Abstract
Introduction
The exponential growth in health information technology (HIT) presents an immense opportunity for facilitating the data‐to‐knowledge‐to‐performance loop which supports learning health systems. This scoping review addresses the gap in knowledge around HIT implementation contextual factors such as organizational culture and provides a current state assessment.
Methods
A search of 13 databases guided by Arskey and O'Malley's framework identified content on HIT implementations and organizational culture. The Consolidated Framework for Implementation Research (CFIR) was used to assess culture and to develop review criteria. Culture stress, culture effort, implementation climate, learning climate, readiness for implementation, leadership engagement, and available resources were the constructs examined. Rayyan and Qualtrics were used for screening and data extraction.
Results
Fifty two studies included were mainly conducted in Academic Health Centers (n = 18, 35%) and at urban locations (n = 50, 96%). Interviews frequently used for data collection (n = 26, 50%) and guided by multiple frameworks (n = 34). Studies mostly focused on EHR implementations (n = 23, 44%) followed by clinical decision support (n = 9, 17%). About two‐thirds (n = 34, 65%) reflected culture stress theme and 62% (21 of 34) acknowledged it as a barrier. Culture effort identified in 27 studies and was a facilitator in most (78%, 21 of 27). Leadership engagement theme in majority studies (71%, n = 37), with 35% (n = 13) noting it as a facilitator. Eighty percent (42 studies) noted available resources, 12 of which identified this as barrier to successful implementation.
Conclusions
It is vital to determine the culture and other CFIR inner setting constructs that are significant to HIT implementation as facilitators or barriers. This scoping review presents a limited number of empirical studies in this topic highlighting the need for additional research to quantify the effects of culture. This will help build evidence and best practices that facilitate HIT implementations and hence serve as a platform to support robust learning health systems.
Keywords: health information technology, implementation framework, implementation science, learning health systems, organizational culture, review
1. BACKGROUND
1.1. Increasing investments and implementations in Health Information Technology
Since the 2010 multi‐billion dollar investment in health information technology (HIT) through the HITECH Act, 1 the HIT industry has been on a growth trajectory. Subsequent major federal health initiatives (CURES Act in 2016, 2 CARES in 2020 3 ) have included significant provisions leveraging HIT to improve the quality and outcomes in healthcare. While HIT interventions hold a lot of promise for improving healthcare, many HIT solutions are not able to deliver on this promise due to a multitude of factors including adoption and implementation issues. Apart from substantial organizational investment, HIT implementations also suffer from high failure rates, 4 as these systems are complex impacting numerous stakeholders across an organization and requiring buy‐in for success. Given the magnitude of financial capital and human resources being invested, it is vital to understand factors that influence HIT implementations.
1.2. Implementation science framework to understand HIT implementations
Informatics is a socio‐technical field, and there is an increasing need to understand the role of contextual factors such as organizational culture in impacting HIT implementations. Implementation science offers a systematic way to understand the barriers and facilitators to implementing innovations. The Consolidated Framework for Implementation Research (CFIR) 5 , 6 is a state of the science implementation framework which provides a robust method to examine constructs that are associated with effective implementations. The CFIR consists of five main constructs (outer setting, inner setting, intervention characteristics, individual characteristics, and process). 5 Organizational culture, an inner setting construct in CFIR, has been recognized as an important factor in HIT implementations. 7 Culture is defined as the norms, values, and basic assumptions of a given organization. 8 Fernandez et al, assessed various measures related to the inner setting of CFIR and highlighted culture stress and culture effort as sub‐constructs of culture. 9 In addition to culture, CFIR includes implementation climate and readiness to implementation (leadership engagement, available resources) as constructs in inner setting. 5 Table 1 presents the definitions of key concepts related to culture utilized in this study.
TABLE 1.
Definitions of Culture Related Concepts
| Concept | Definition |
|---|---|
| Culture | “Norms, values, and basic assumptions of a given organization” 5 |
| Culture stress | “Perceived strain, stress, and role overload” 9 |
| Culture effort | “How hard people in organizations work toward achieving goals” 9 |
| Implementation climate | “The absorptive capacity for change, shared receptivity of involved individuals to an intervention, and the extent to which use of that intervention will be rewarded, supported, and expected within their organization” 5 |
| Learning climate | “A climate in which: (a) leaders express their own fallibility and need for team members' assistance and input; (b) team members feel that they are essential, valued, and knowledgeable partners in the change process; (c) individuals feel psychologically safe to try new methods; and (d) there is sufficient time and space for reflective thinking and evaluation” 5 |
| Readiness for implementation | “Tangible and immediate indicators of organizational commitment to its decision to implement an intervention” 5 |
| Leadership engagement | “Commitment, involvement, and accountability of leaders and managers with the implementation” 5 |
| Available resources | “The level of resources dedicated for implementation and on‐going operations, including money, training, education, physical space, and time” 5 |
1.3. HIT and implementation science as pillars to support Learning Health Systems
Learning Health Systems (LHS) are organizations that continuously self‐study and adapt using data and analytics to generate knowledge, engage stakeholders and implement changes to transform healthcare delivery. 10 The rapid pace of growth in HIT enables the acceleration of learning cycles that convert data to knowledge (D2K), knowledge to performance (K2P), and performance to data (P2D). 11 A well‐functioning LHS is one wherein science, informatics, incentives, and culture are aligned for continuous improvement and innovation. 12 The intellectual advancement and broad impact of LHS innovations underscore the importance and research to support LHS.
Because of their significant impact on several organizational and team structures across IT and clinical care, HIT implementations can be classified as complex healthcare interventions. 13 Robust evaluation methods are typically needed to understand how complex interventions work in different contexts. Supporting culture is considered a critical infrastructure component for effective LHS. 14 Informatics and implementation science are recognized competencies for LHS researchers. 15 This study brings these domains together and aims to understand the influencing role of organizational culture in the context of informatics and HIT implementations.
1.4. Prior research
Prior scoping reviews of HIT implementations have focused on the concept of “champions” to synthesize their characteristics, behaviors, and impacts on HIT implementations. 16 A subsequent study aimed to understand the breadth of impact of these champions by increasing scope to include implementation leader, opinion leader, facilitator, and change agent. 17 Both reviews found that champions were important positive influences for effective implementations. A recent study by Gui et al, specifically focused on the role of physician champions through qualitative explorations of their challenges and strategies during a large‐scale HIT implementation. 18
1.5. Study objectives
The objective of this scoping review was to summarize current evidence regarding organizational culture in HIT implementations. The aim was to understand the scope and impact of organizational culture by assessing both quantitative and qualitative studies, which addresses a critical gap in knowledge on this important construct. By examining the supporting constructs of the CFIR Inner Setting domain, the review provides added clarity to the impact of organizational culture in HIT implementations.
2. METHODS
The study approach was based on the five‐step framework developed by Arskey and O'Malley 19 : (a) identifying the research question, (b) identifying relevant studies, (c) selecting studies, (d) charting relevant data, and (e) summarizing and reporting the results. The study was registered in the Open Science Framework 20 prior to start of the research.
2.1. Sources and searches
Relevant studies were identified by conducting a comprehensive search incorporating both natural language and controlled vocabulary that reflected the concepts of organizational culture (including change management, organizational culture, and values) and health information technology implementation, including electronic health record implementation. Searches were limited to items published since 2010 and through March 2020. No limits were placed on the language of publication or study design. The search strategy was executed across 13 databases: MEDLINE, PsycINFO and Embase via Ovid; PubMed; Cochrane Library via Wiley; Scopus Web of Science Core Collection; Business Source, CINAHL, Library & Information Science Source and Library, Information Science & Technology Abstracts via EBSCO; CRD Database; and IEEE Xplore. The full search strategy is available in Data S1.
2.2. Selection of studies
Two independent researchers screened each title and abstract using previously defined inclusion and exclusion criteria. Screening was facilitated by Rayyan, 21 a web‐based tool intended for systematic review screening. The HITECH Act definition of HIT was utilized for this study: “hardware, software, integrated technologies, or related licenses, intellectual property, upgrades, or packaged solutions sold as services that are designed for or support the use by health care entities or patients for the electronic creation, maintenance, access, or exchange of health information”. 1 Examples include electronic health records (EHRs), clinical decision support (CDS) tools, and technologies involving clinical notes, medication lists, laboratory results, and telemedicine. We utilized the CFIR definition of culture as “norms, values, and basic assumptions of a given organization.” Culture related definitions and constructs mentioned in CFIR were used to develop inclusion and exclusion criteria.
Articles were excluded if they did not include some component of organizational culture, did not involve a HIT implementation, were based outside of the United States, or described projects primarily completed prior to 2010. Articles also were excluded if they were focused on health information exchange (HIE) implementation or described a technology such as mobile apps aimed at patient self‐management. The initial screening process was followed with full‐text screening using previously established criteria. Three authors (SR, GH, CB) were involved in all aspects of screening process (title/abstract and full text reviews). Any discrepancies in screening decisions were resolved through discussion or by a senior faculty researcher (GM) where necessary. Reasons for exclusion were recorded to be reported in accordance with PRISMA‐ScR standards. 22
2.3. Data extraction and synthesis
Relevant data for charting was first identified collaboratively by the researchers. A data charting form using survey software (Qualtrics, Provo, UT) was developed by one researcher (GH) and tested by other researchers (CB, SR) for any potential further refinement or clarification. Every study was reviewed by two researchers and discrepancies in the data extracted were resolved through consensus. As this is a scoping review rather than a systematic review or meta‐analysis, formalized risk of bias assessment was not undertaken.
The type of HIT implemented was recorded along with any HIT vendor to capture the predominance of studies around any particular HIT. Next, the factors related to culture (culture stress, culture effort) were identified, along with implementation climate, learning climate, readiness for implementation, leadership engagement, and available resources. These seven constructs were chosen for this study due to the availability of tools/measures as validated by Fernandez et al. 9 The definitions presented in this paper were used as guidelines to code culture and related constructs. Relevant text from studies were highlighted and captured in the form so that additional analysis could be performed. Two researchers reviewed all qualitative data to code each construct identified in a paper as being a barrier to implementation, facilitator to implementation, both a barrier and a facilitator, or to have an unclear role or impact. Following extraction of needed information, the results were synthesized, and findings summarized through iterative discussions in the research team (SR, GH, CB, and GM).
3. RESULTS
3.1. Study selection
The literature search results are presented in Figure 1 using the PRISMA flow chart. The searches across various databases yielded 3787 articles and no additional papers were brought in through other sources. After the removal of duplicate articles, 2178 articles remained which met the criteria for initial screening. After title and abstract review, 1845 of these were excluded and 333 articles met the criteria for full text review. The full text screening led to exclusion of 278 articles (reasons listed in Figure 1) with 55 papers for inclusion in the detailed analysis. Three of those used the same data as selected ones and so a final count of 52 studies are included. A listing of these studies with relevant information is provided in Data S2.
FIGURE 1.
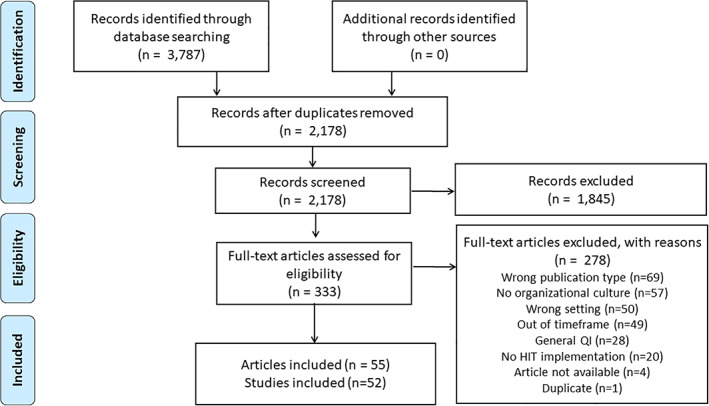
PRISMA diagram for literature search on culture in HIT implementations
3.2. Study characteristics
3.2.1. Publication timeframe
The years 2015 (n = 8) and 2018 (n = 8) had the most publications of the 52 selected studies. It should be noted that data for the year 2020 included only the months of January through March but had 6 studies published by then. The inclusion of culture and related concepts over the years is represented in Figure 2. Culture stress was predominant in 2015 (n = 6) and culture effort was also a strongly identified theme that year (n = 8). Implementation Climate (n = 19), Leadership Engagement (n = 19) and Available Resources (n = 29) have been consistent factors identified in most articles since 2017.
FIGURE 2.
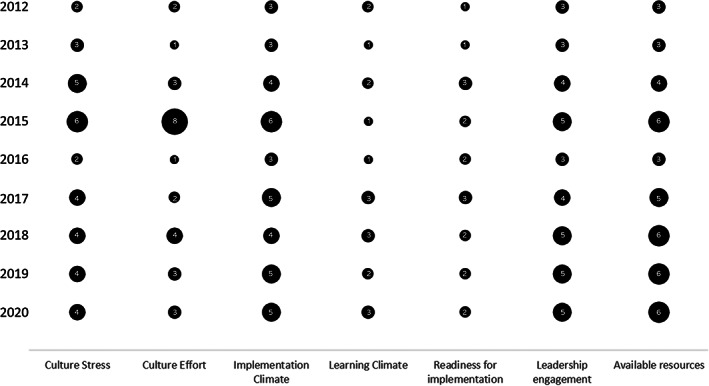
Representation of culture concepts in citations over the study period
3.2.2. Study location and health system
Studies were most frequently conducted in Academic Health Centers (n = 18, 35%), followed by studies conducted in multiple settings/systems (n = 16, 31%) as presented in Table 1. Three studies were conducted in the setting of the Veteran's Administration and only 2 studies were conducted in Federally Qualified Health Centers (FQHC). Smaller settings had fewer studies (independent clinics = 2, outpatient clinics = 2) and only 1 study had a focus on critical access hospitals. Almost all studies predominantly were conducted in urban locations (n = 50, 96%) and only 2 studies (4%) were done exclusively in rural locations. In terms of the geographic representation, 19 studies (37%) included settings nationwide across the US, with Massachusetts being the most represented (n = 6, 12%).
3.2.3. Study data collection and implementation phase
Given the need to gather detailed information on implementations, half of the studies (n = 26, 50%) collected data using interviews. This was followed by data collection using surveys (n = 16, 30%) and field studies/observations (n = 12, 23%). A large number of studies included more than one data collection method. A majority (n = 38, 73%) of papers were on the implementation phase of the HIT cycle along with elements of evaluation (n = 34, 65%). Fourteen papers (27%) had some aspects of planning along with emphasis on implementation.
3.3. Frameworks used
A total of 34 frameworks were used across these studies (Figure 3). Some studies (n = 8) utilized more than one framework to guide their research and its interpretation. Frameworks were primarily drawn from the field of implementation science, including the CFIR and Reach, Effectiveness, Adoption, Implementation and Maintenance (RE‐AIM). The sample of studies also included frameworks from the fields of organizational science, strategic management, change management, social science, information systems, psychology, communications, work redesign and quality improvement.
FIGURE 3.
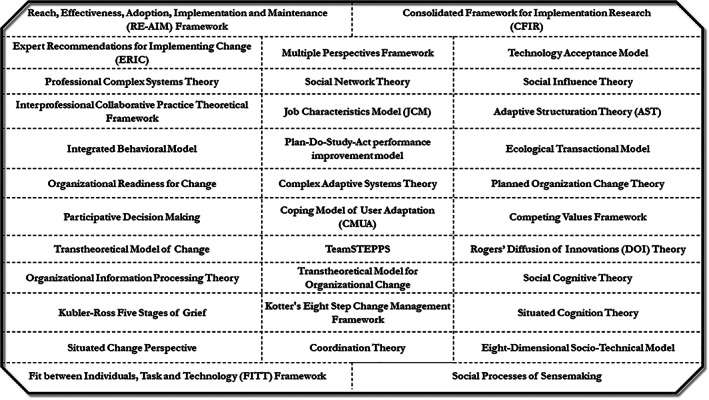
Frameworks used to study and represent culture
3.3.1. Type of HIT and vendor
Table 2 presents the details of the type of HIT implemented in the selected studies. Approximately half of studies (n = 23, 44%) were focused on EHR implementations (both new and switching from legacy EHRs). This was followed by the implementation of CDS tools (CDS/CPOE/alert), which comprised 9 studies (17%). The next set of implementations focus on patient facing tools (PROM, PHR, patient portal) and included 6 studies (11%). The most frequently mentioned EHR vendor in these studies was Epic (n = 10), and in 18 studies no vendor was described as associated with the HIT.
TABLE 2.
Details on Health Information Technology Implementations in Selected Studies
| ID | Year | Study citation | Study emphasis/type of HIT | Study data collection | Study location | Study health system type and name | Study focus/Phase of HIT cycle | Study HIT vendor info | |
|---|---|---|---|---|---|---|---|---|---|
| Urban/Rural | Region/State | ||||||||
| 1 | 2020 | Bachmann et al 23 | Patient reported outcomes system | Stakeholder feedback | Urban | Southeast (TN) | Academic Health Center | Planning; Implementation | Epic |
| 2 | Businger et al 24 | Patient portal, Patient interactive platform, EHR dashboard | Stakeholder feedback, Systems/chart review | Urban | Northeast (MA) | Academic Health Center (Brigham and Women's Hospital) | Implementation | Epic | |
| 3 | Cartier et al 25 | Platform for referral to social services | Review existing literature, Market/vendor analysis | Urban | Nationwide | Multiple | Planning; Implementation | Multiple referral tools a | |
| 4 | Chipps et al 26 | General EHR optimization | Focus group | Urban | Nationwide | Multiple | Evaluation | Multiple | |
| 5 | Heinze and Heinze 27 | EHR | Survey, Interview | Urban | Nationwide | Multiple | Implementation; Evaluation | Multiple | |
| 6 | Sieck et al 28 | EHR | Interview | Urban | Midwest | Academic Health Center | Implementation; Evaluation | Epic | |
| 7 | 2019 | Angoff et al 29 | EHR | Systems/chart review | Urban | Northeast (MA) | Federally Qualified Health Center (Boston Health Care for the Homeless Program [BHCHP]) | Implementation | Epic |
| 8 | Chaturvedi et al 30 | Intravenous clinical integration (IVCI) to allow bidirectional communication between EHRs and infusion pumps | Interview, Field studies/observation | Urban | Westcoast (CA) | Academic Health Center (Cedars‐Sinai Medical Center) | Planning; Implementation | EHR: Epic, Dispensing cabinet: Pyxis, Smart pump vendor: CareFusion | |
| 9 | Orenstein et al 31 | CDS for refugee health | Stakeholder feedback | Urban | Nationwide | Multiple | Planning; Implementation | Epic | |
| 10 | Pittman et al 32 | eScreening patient self ‐assessment tool | Survey, Interview, Focus Group | Urban | Westcoast (CA) | VA/Military (VA San Diego Healthcare System [VASDHS]) | Implementation | Not specified | |
| 11 | Rangachari et al 33 | Social Networking System | Interview, Systems/chart review | Urban | Southeast (GA) | Academic Health Center (AU Health [Augusta University's Health System]) | Planning; Implementation; Evaluation | EHR: Cerner, Message system: Yammer | |
| 12 | Zhang et al 34 | Patient Reported Outcomes System | Interview | Urban | Midwest (IL) | Academic Health Center (Northwestern Medicine) | Evaluation | Epic | |
| 13 | 2018 | Anderson et al 35 | EHR based communication tool | Survey, systems/chart review | Urban | Midwest | Academic Health Center | Planning; Implementation | Not specified |
| 14 | Barrett 36 | EHR | Survey | Urban | Southwest | Federally Qualified Health Center | Evaluation | Epic | |
| 15 | Campione et al 37 | EHR, E‐reporting | Survey | Urban | Nationwide | Multiple | Planning; Implementation | Multiple | |
| 16 | Chung et al 38 | CPOE for chemotherapy | Survey, stakeholder feedback, systems/chart review | Urban | Southwest (TX) | Academic Health Center (Harris Health System) | Implementation; Evaluation | Epic | |
| 17 | Creber et al 39 | CDS tool for pediatric head trauma | Interview, Existing literature, Market/vendor analysis | Urban | Westcoast (CA) | Integrated Health System (Kaiser) | Evaluation | Epic | |
| 18 | Giuliano et al 40 | Clinical decision support for antimicrobial stewardship | Interview | Urban | Nationwide | Integrated Health System (Ascension Health) | Evaluation | CDS: SENTRI7 | |
| 19 | Hao and Padman 41 | Wireless personal digital assistant based tool for online access to clinical data for phsticians | Systems/chart review | Urban | Northeast (PA) | Integrated Health System | Implementation; Evaluation | Not specified | |
| 20 | Rao‐Gupta et al 42 | Patient Interactive Platform | Survey, systems/chart review, Field studies/observation | Urban | Midwest (IL) | Academic Health Center (Ann & Robert H. Lurie Children's Hospital of Chicago) | Implementation | Patient Interactive Platform: GetWellNetwork | |
| 21 | 2017 | Kim et al 43 | General HIT | Survey | Urban | Nationwide | Multiple | Evaluation | Multiple |
| 22 | Kooienga and Singh 44 | e‐prescribing | Interview, field studies/observation | Rural | West | Independent Clinic | Evaluation | e‐prescribing tool: Surescripts | |
| 23 | Leslie et al 45 | General HIT | Field studies/observation | Urban | Nationwide | Academic Health Center | Evaluation | Not specified | |
| 24 | Mason et al 46 | EHR | Interview | Rural | Midwest (MO) | Outpatient Clinic | Implementation; Evaluation | Not specified | |
| 25 | Reidy et al 47 | Internet based tool for advanced care planning, integrated into the EHR | Case study | Urban | Northeast (MA) | Academic Health Center (UMass Memorial Medical Center) | Planning; Implementation; Evaluation | Advanced Care planning tool: Luminat | |
| 26 | Saleem et al 48 | EHR | Case study | Urban | Southwest (TX) | Inpatient Hospital | Implementation; Evaluation | Not specified | |
| 27 | Tobler et al 49 | EHR | Interview, Field studies/observation | Urban | West (UT) | Outpatient Clinic | Planning; Implementation | Not specified | |
| 28 | 2016 | Ballaro and Washington 50 | EHR | Survey | Urban | Nationwide | VA/Military (Military Healthcare System [MHS]) | Implementation | Not specified |
| 29 | Bentley et al 51 | EHR | Case study | Urban | Midwest (OH) | Academic Health Center (Ohio State Wexner Medical Center) | Planning; Implementation; Evaluation | Not specified | |
| 30 | Gross et al 52 | EHR | Case study | Urban | Northeast (MA) | Academic Health Center (Dana‐Farber Cancer Institute) | Implementation; Evaluation | Not specified | |
| 31 | Lin et al 53 | Electronic drug–disease alert for patients with CKD | Interview | Urban | West (WA, AK, MT, ID) | Multiple | Planning | Multiple | |
| 32 | Queenan and Devaraj 54 | CPOE | Survey | Urban | Nationwide | Inpatient Hospital (Multiple) | Evaluation | Multiple | |
| 33 | Ramsey et al 55 | General HIT | Survey | Urban | Nationwide | Multiple | Implementation | Multiple | |
| 34 | 2015 | Callahan et al 56 | Sexual orientation and gender identity fields in EHR | Interview, Field studies/observation, systems/chart review | Urban | Westcoast (CA) | Academic Health Center (University of California Davis Health System) | Implementation; Evaluation | Not specified |
| 35 | Collins et al 57 | EHR | Interview | Urban | Nationwide | Multiple | Implementation; Evaluation | Multiple | |
| 36 | Elias et al 58 | EHR | Field studies/observation | Urban | Southeast | Independent Clinic | Planning; Implementation | Not specified | |
| 37 | McAlearney et al 59 | EHR | Interview, Focus group | Urban | Nationwide | Multiple | Evaluation | Multiple | |
| 38 | Sherer et al 60 | EHR | Interview, Systems/chart review | Urban | Northeast (PA) | Academic Health Center (Lehigh Valley Health Network) | Implementation; Evaluation | GE Centricity | |
| 39 | Wright et al 61 | CDS | Interview | Urban | Nationwide (MA, IN, OR, NJ) | Multiple | Implementation; Evaluation | Multiple | |
| 40 | Wright et al 62 | Problem lists in EHRs | Survey, Interview, Systems/chart review | Urban | Nationwide (OR, TX, NY, UT) | Multiple | Evaluation | Multiple | |
| 41 | Yuan et al 63 | EHR | Survey, Interview, field studies/observation | Urban | Not Stated | Academic Health Center | Implementation | Not specified | |
| 42 | 2014 | Chase et al 64 | EHR | Interview, field studies/observation | Urban | Nationwide | Multiple | Implementation; Evaluation | Multiple |
| 43 | Fairbrother et al 65 | General HIT | Interview | Urban | Midwest (OH) | Multiple | Implementation; Evaluation | Multiple | |
| 44 | Muslin et al 66 | CPOE | Survey | Rural | Southeast | Inpatient Hospital | Implementation; Evaluation | Not specified | |
| 45 | Shea et al 67 | General HIT | Survey | Urban | Southeast | Academic Health Center (University of North Carolina Health Care System) | Implementation; Evaluation | Not specified | |
| 46 | Wells et al 68 | Personal health record | Survey, Interview | Urban | Nationwide | Multiple | Evaluation | Multiple | |
| 47 | 2013 | Boswell 69 | EHR | Interview | Urban | Northeast (PA) | Multispecialty ambulatory care organization | Planning; Implementation | Not specified |
| 48 | Craven et al 70 | EHR | Interview | Rural | Nationwide | Critical Access Hospitals (Multiple) | Planning; Implementation | Multiple | |
| 49 | Kitzmiller et al 71 | Electronic nursing documentation system | Field studies/observation | Urban | Southeast | Academic Health Center | Implementation; Evaluation | Not specified | |
| 50 | 2012 | Ash et al 72 | CDS, specifically focused on CDS for providers with ordering authority | Survey, Interview, Field studies/observation | Urban | Nationwide (OR, CA, MA, IN, NJ) | Multiple sites b | Evaluation | Multiple |
| 51 | Lanham et al 73 | EHR | Interview, Field studies/observation | Urban | Southwest (TX) | Multispecialty ambulatory care organization | Implementation; Evaluation | Not specified | |
| 52 | McAlearney et al 74 | EHR | Interview, Focus group | Urban | Nationwide | Multiple | Implementation; Evaluation | Multiple | |
Multiple Referral Tools: Aunt Bertha, CharityTracker, CrossTx, Healthify, Pieces Iris, NowPow, One Degree, TAVConnect (now Signify Community), and Unite Us.
Multiple (Providence Portland Medical Center, El Camino Hospital, Partners HealthCare, Wishard Memorial Hospital Clinics, Roudebush Veterans Health Administration, Mid‐Valley IPA, RWJ) Medical Group.
3.4. Culture and inner setting constructs
Table 3 presents the representation of culture and related inner setting constructs across the selected studies. Apart from identifying the presence of these constructs (culture stress, culture effort, implementation climate, learning climate, readiness for implementation, leadership engagement, and available resources), the table also identifies the role of construct as a barrier, facilitator, both or not stated. These are also depicted graphically in Figure 4.
TABLE 3.
Representation of organizational culture and inner setting constructs in selected studies
| Year | Citation | Culture Stress | Culture Effort | Implementation Climate | Learning Climate | Readiness for implementation | Leadership engagement | Available resources |
|---|---|---|---|---|---|---|---|---|
| 2020 | Bachmann et al 23 | ♢ | ♢ | ♢ | ||||
| Businger et al 24 | ○ | ☐ | ☐ | ☐ | ♢ | |||
| Cartier et al 25 | ○ | ♢ | ☐ | ☐ | ♢ | ○ | ||
| Chipps et al 26 | △ | ☐ | △ | |||||
| Heinze and Heinze 27 | ☐ | ○ | ☐ | ♢ | ☐ | |||
| Sieck et al 28 | ○ | ☐ | ☐ | ☐ | △ | ○ | ||
| 2019 | Angoff et al 29 | ☐ | ☐ | ☐ | ♢ | |||
| Chaturvedi et al 30 | △ | ☐ | ☐ | △ | ☐ | |||
| Orenstein et al 31 | ♢ | ♢ | ♢ | |||||
| Pittman et al 32 | ○ | ☐ | △ | ○ | ||||
| Rangachari et al 33 | △ | △ | ♢ | ☐ | ♢ | ♢ | ♢ | |
| Zhang et al 34 | △ | ☐ | ○ | ○ | ||||
| 2018 | Anderson et al 35 | ☐ | ♢ | ♢ | ♢ | |||
| Barrett 36 | ○ | ☐ | ♢ | |||||
| Campione et al 37 | ♢ | ♢ | ♢ | |||||
| Chung et al 38 | ○ | ☐ | ☐ | ☐ | ♢ | |||
| Creber et al 39 | ☐ | ☐ | ☐ | ☐ | ☐ | ☐ | ||
| Giuliano et al 40 | ○ | ☐ | △ | |||||
| Hao and Padman 41 | ☐ | ☐ | ||||||
| Rao‐Gupta et al 42 | ♢ | ♢ | ||||||
| 2017 | Kim et al 43 | ♢ | ♢ | ♢ | ||||
| Kooienga and Singh 44 | △ | ☐ | ○ | △ | ||||
| Leslie et al 45 | △ | △ | ♢ | |||||
| Mason et al 46 | △ | △ | ||||||
| Reidy et al 47 | ♢ | ☐ | ☐ | ♢ | △ | |||
| Saleem et al 48 | △ | ☐ | △ | ♢ | ||||
| Tobler et al 49 | △ | ☐ | △ | ○ | ○ | |||
| 2016 | Ballaro and Washington 50 | ○ | ♢ | |||||
| Bentley et al 51 | ♢ | ☐ | ☐ | ☐ | ♢ | |||
| Gross et al 52 | ○ | ☐ | ♢ | |||||
| Lin et al 53 | △ | ♢ | ||||||
| Queenan and Devaraj 54 | ||||||||
| Ramsey et al 55 | △ | ♢ | ○ | |||||
| 2015 | Callahan et al 56 | △ | ○ | ♢ | ♢ | ○ | ♢ | |
| Collins et al 57 | ☐ | △ | ♢ | △ | ||||
| Elias et al 58 | △ | ♢ | △ | △ | ||||
| McAlearney et al 59 | △ | ♢ | ♢ | ☐ | ♢ | ♢ | ||
| Sherer et al 60 | △ | ♢ | ♢ | |||||
| Wright et al 61 | △ | ☐ | △ | |||||
| Wright et al 62 | ☐ | ☐ | ||||||
| Yuan et al 63 | △ | ☐ | ○ | ☐ | △ | |||
| 2014 | Chase et al 64 | △ | ☐ | ♢ | ♢ | |||
| Fairbrother et al 65 | ○ | ☐ | ☐ | △ | ||||
| Muslin et al 66 | △ | △ | △ | △ | ○ | △ | ||
| Shea et al 67 | ○ | ☐ | ♢ | ♢ | ☐ | |||
| Wells et al 68 | △ | ☐ | △ | ♢ | ☐ | ♢ | ||
| 2013 | Boswell 69 | ○ | ☐ | ☐ | ☐ | ♢ | ☐ | ☐ |
| Craven et al 70 | △ | ♢ | ♢ | ♢ | ||||
| Kitzmiller et al 71 | △ | ☐ | ☐ | △ | ||||
| 2012 | Ash et al 72 | △ | ☐ | ♢ | ☐ | ♢ | △ | |
| Lanham et al 73 | ♢ | ☐ | ♢ | ♢ | ||||
| McAlearney et al 74 | ☐ | ☐ | ○ | ♢ | ☐ | ♢ |
Note: ☐, Facilitator; △, Barrier; ○, Both; ♢, Not stated.
FIGURE 4.
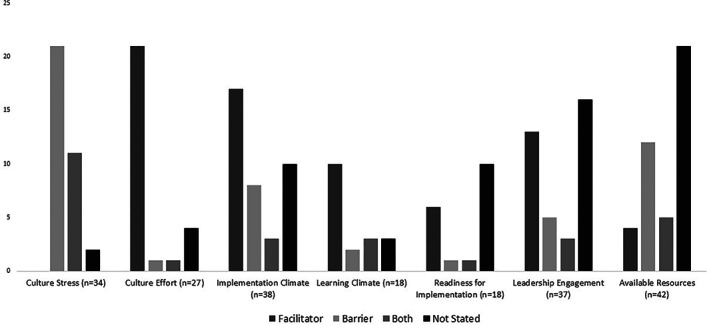
Culture and inner setting context themes by code
3.4.1. Culture stress
Culture stress as defined by Fernandez et al, refers to “Perceived strain, stress, and role overload”. 9 Out of the 52 chosen studies, about two thirds (n = 34, 65%) included the construct culture stress. Approximately two‐thirds of these studies (21 of 34) were identified as barriers and no study listed stress as a facilitator. In the recent publications, about 50% had stress‐related concepts in both 2020 (4 out of 6) and in 2019 (4 out of 6). This construct was not connected with a specific vendor or the type of health system.
3.4.2. Culture effort
Approximately 50% of studies addressed culture effort, defined as “How hard people in organizations work toward achieving goals”. 9 Culture effort was coded as a facilitator in three fourth of these studies (21 of 27). In most of these studies (23 out of 27), culture effort co‐occurred with the construct of implementation climate. Half of studies in recent years (3 out of 6 in 2020 and 3 out of 6 in 2019) were coded for this construct.
3.4.3. Implementation climate
Implementation climate was defined as “the absorptive capacity for change, shared receptivity of involved individuals to an intervention and the extent to which use of that intervention will be rewarded, supported, and expected within their organization”. 5 Approximately three‐fourths of the studies (n = 38, 73%) mentioned this construct, of which 17 (45%) were identified as a facilitators and 8 (21%) identified as barriers and in 10 studies (26%) this was not stated or was unclear.
3.4.4. Learning climate
A learning climate is “a climate in which (a) leaders express their own fallibility and need for team members' assistance and input; (b) team members feel that they are essential, valued, and knowledgeable partners in the change process; (c) individuals feel psychologically safe to try new methods; and (d) there is sufficient time and space for reflective thinking and evaluation (in general, not just in a single implementation)”. 5 Eighteen studies (35%) were coded as representative of this construct, of which 10 (56%) were facilitators and 2 (11%) were barriers.
3.4.5. Readiness for implementation
“Tangible and immediate indicators of organizational commitment to its decision to implement an intervention” is referred as the readiness for implementation”. 5 Eighteen studies (35%) were coded to be representative of this construct of which 6 were coded as facilitators, 1 was a barrier, 1 had both listed and 10 studies did not state if it was a barrier or a facilitator or was unclear.
3.4.6. Leadership engagement
Engagement of the leadership of an organization in the HIT implementation process is an indicator of readiness for implementation and is defined as “Commitment, involvement, and accountability of leaders and managers”. 5 Close to three‐fourths of studies (n = 37, 71%) had identified this construct, of which 13 studies were noted to be a facilitator, 5 as a barrier, 3 were stated to be both and 16 studies did not state if it was a barrier or a facilitator or was unclear.
3.4.7. Available resources
Eighty percent (42 out of 52 studies) had mentioned available resources as part of the HIT life cycle process (planning, implementation, evaluation), as shown in Table 2. This indicates the “level of resources dedicated for implementation and on‐going operations including money, training, education, physical space, and time”. 5 Of these, 4 studies had identified available resources as facilitator to implementation efforts, 12 studies as a barrier, 5 indicated both and 12 studies did not state if it was a barrier or a facilitator or was unclear.
3.5. Impact of organizational culture in HIT implementations
Of all the inner setting constructs, culture stress was most frequently noted as a barrier (21/34 studies), followed by lack of available resources (12/42). Representative quotes (as shown in Table 3) describe the high volume of work and understaffing as issues in implementations. Culture effort (21 studies), implementation climate (17 studies), and leadership engagement (13 studies) were more frequently noted as facilitators. Quotes presented in Table 4 point to shared responsibility, management support, and financial commitment as facilitators related to these constructs. As shown in Table 3, insufficient training programs, perception of roles as passive implementers, and lack of enthusiasm/communication from the top were some of the barriers related to learning climate, readiness for implementation and leadership engagement respectively.
TABLE 4.
Representative quotes on culture related concepts in health information technology implementations
| Theme | Sub‐theme | Sample quote |
|---|---|---|
| Culture stress (n = 34) | Facilitator (n = 0) | NA |
| Barrier (n = 21) | “[The participants] articulated that the volume of work shifted to [the staff] was very high and that they were understaffed … Overall, participants felt that there was not a sufficient numbers of [staff] in their organization and that these [staff] were under‐resourced.” (Chipps et al 26 ) | |
| Both (n = 11) | “The informant reported that initially there was ‘anticipatory panic’ expressed by medical assistants about fitting the additional work into the clinical workflow. However, once staff started using the platform and were able to see positive effects on patients' lives, they became more enthusiastic about the technology.” (Cartier et al 25 ) | |
| Not Stated or Unclear (n = 2) | “In practices where communication patterns are more fragmented, EHR support staff may need to work with each individual to achieve EHR use goals set by the larger organization.” (Lanham et al 73 ) | |
| Culture effort (n = 27) | Facilitator (n = 21) | “both primary care providers and specialists considered themselves to have shared responsibility for problem list maintenance” (Wright et al 62 ) |
| Barrier (n = 1) | “I have seen prescribers simply ‘not act’ to reconcile a medication because there was insufficient information or they were not sure” (Rangachari et al 33 ) | |
| Both (n = 1) | “[The authors] viewed this resistance as an invitation to educate leaders, providers, and staff about LGBT health disparities and to expose providers to techniques” (Callahan et al 56 ) | |
| Not Stated or Unclear (n = 4) | “Managing the culture, it is what it is. The most you can do is find, like a good physician champion, find a strong practice leader.” (McAlearney et al 59 ) | |
| Implementation climate (n = 38) | Facilitator (n = 17) | “…the decision to pursue [an HIT implementation] stemmed from a culture of innovation, particularly regarding initiatives to improve patient safety and organizational efficiency” (Chaturvedi et al 30 ) |
| Barrier (n = 8) | “…physicians did not view their role as active translators of the technology to their local setting. In other words, because physicians felt that the [HIT implementation] was not customized to local needs, resistance was engendered, rather than acceptance” (Muslin et al 66 ) | |
| Both (n = 3) | “In our case, oncologists were not incentivized to review PROs, whereas surgeons could receive additional payment for including PRO assessment” (Zhang et al 34 ) | |
| Not Stated or Unclear (n = 10) | “Cultural shifts within a clinical area are required to promote sustained practice change. The cultural shift toward early mobility started in 2010 … yet integration of early mobility as a cultural norm continued to be a work in progress” (Anderson et al 35 ) | |
| Learning climate (n = 18) | Facilitator (n = 10) | “The importance of institution wide educational efforts in resolving user workflow problems cannot be emphasized enough.” (Chung et al 38 ) |
| Barrier (n = 2) | “a lesson here is simply having a training program is not sufficient; providing physicians with a set of instructions for using the ordering software will not necessarily create buy‐in” (Muslin et al 66 ) | |
| Both (n = 3) | “One clinician commented, ‘occasionally things pop up and I have to learn how to do it but after a few times, you learn how to make it faster.’ Another felt she navigated the [new] screen quite well and adapted the screen to meet her needs.” (Tobler et al 49 ) | |
| Not Stated or Unclear (n = 3) | “The first phase of implementation consisted of staff participation in an online educational module … Although completion of the eMobility module was not tracked by individual staff participants, the postimplementation survey asked whether the module was viewed and helpful.” (Anderson et al 35 ) | |
| Readiness for implementation (n = 18) | Facilitator (n = 6) | “organizational innovativeness is likely associated with more forums associated with the technology, including workshops, seminars, and email groups. These outlets create opportunities for employees to ask each other for advice and help” (Barrett 36 ) |
| Barrier (n = 1) | “Physicians here viewed their role simply as passive implementers of a standardized technology package. A physician stated: “The training and implementation left much to be desired.” (Queenan and Devaraj 54 ) | |
| Both (n = 1) | “One practice was very engaged about change and implementation of technology, while the other was somewhat resistant to change and wary of e‐prescribing feeling it was not make prescribing safer with less prescribing errors.” (Kooienga and Singh 44 ) | |
| Not Stated or Unclear (n = 10) | “Informants at all our sites recognized that some potential EHR users, mainly clinicians, did not have basic computer literacy and skills. Several of the sites recognized this need and developed pre‐implementation skills assessments.” (McAlearney et al 74 ) | |
| Leadership engagement (n = 37) | Facilitator (n = 13) | “Support from high level management was instrumental to success and played a critical role in communicating the organizational vision, the expectation for clinician engagement, and that the PHR implementation was the organization's policy” (Wells et al 68 ) |
| Barrier (n = 5) | “Though most leadership expressed strong support for eScreening in individual interviews, many staff focus group participants sensed a lack of enthusiasm for the project either because of little to no communication from the top.” (Pittman et al 32 ) | |
| Both (n = 3) | “Several of the primary barriers (eg, openness/buy‐in) were centered on collective attitudes and perspectives of those within the organization, such as leaders in the position of making clinical care (and therefore adoption) decisions, about technology‐based approaches…. Successful implementation is more likely in climates with motivation to change, that are flexible for embracing innovation, and that have leadership support and infrastructure resources to support the innovation.” (Ramsey et al 55 ) | |
| Not Stated or Unclear (n = 16) | “Specifically, top‐down communication must clearly delineate strategies and tactics for achieving system standardization, processes for change management decisions, the capability of the EHR, and expectations for professional competencies.” (Collins et al 57 ) | |
| Available resources (n = 42) | Facilitator (n = 4) | “However, leadership reported making an early decision to commit the necessary financial requirements for implementation—even when it became clear that the staff time investment was significantly larger than initially expected.” (Creber et al 39 ) |
| Barrier (n = 12) | “A challenge at all four demonstration sites was securing the technical, clinical and informatics resources needed to complete the implementation.” (Wright et al 61 ) | |
| Both (n = 5) | “Physicians noted that training tailored to their role helped them to adapt to using the EHR. For example, as one physician told us, “I think if it's very specific, and it's sort of triggered by the provider… then they think, they'd probably accept it pretty well. But, if it's sort of imposed, probably not.” (Sieck et al 28 ) | |
| Not Stated or Unclear (n = 21) | “The organization mobilized over 600 super users who received extra training and were pulled out of staffing to offer at‐the‐elbow support 24/7 for the first 2 weeks.” (Bentley et al 51 ) |
4. DISCUSSION
The studies provide insight into the range of different types of HIT implementations and the work done to understand the impact of organizational culture on its success across different health systems and geographic locations over the last decade. Despite the breadth of implementations and settings represented, the total number of empirical studies examining organizational culture in this context is limited. Nevertheless, this scoping review yields important insights.
The predominance of EHR implementations in these studies may be due to the timeframe of the study and the influence of the HITECH Act when large numbers of organizations were adopting EHRs or switching from legacy systems. Based on the publication date, it appears that other HIT tools such as patient facing technology (patient portals for capturing PROM) are increasingly being studied once basic functionalities were established. Likewise, Epic being the predominant vendor in these studies is reflective of the fact that this HIT vendor being used by many health systems across the US. 75 , 76
With respect to the study design and data collection methods utilized in these studies, a majority of studies used multiple data collection methods with half of them using interviews with a qualitative approach to gather more contextual data. Most of the published studies are from academic health centers as these entities may be more involved in research and tend to publish due to their academic context.
Overall, 34 frameworks were used across 10 different fields to represent the concepts of culture and other inner setting constructs. Culture stress, culture effort, implementation climate, learning climate, readiness for implementation, leadership engagement, and available resources were all represented in this body of literature. However, the influence of these constructs in implementations appears to be varied. All these constructs can be either a barrier or a facilitator in for a particular HIT implementation. This demonstrates how constructs do not exist in isolation, with these constructs often co‐occurring and, presumably, influencing each other. Individuals and organizations involved in HIT implementations should consider not only the role of single constructs in serving as barriers or facilitators, but instead may wish to consider the role and interplay of these constructs.
This review points to current gaps in the literature and additional studies are needed to build evidence and develop best practices for effective implementations. Studies which presents contextual information around HIT implementation (objectives, funding, market dynamics, project influencers, decision‐makers) will provide valuable insights. More in‐depth research is needed to present a set of recommendations that point to optimal criteria that should be in place to ensure successful HIT implementations. Although the intention of a scoping review is to provide an overview of the landscape, this project identifies that this field is well‐positioned to move toward research of efficacy. This could include the use of validated measures, such as those identified by Fernandez et al, 9 to assess the role of organizational culture in HIT implementations. Only a few academic health centers are the main contributors for publications, and efforts should be made to widen the scope of this research to other institutions and settings, so that findings are generalizable. Robust studies will need to be based on theories and as such guidance on frameworks to be used for studying these HIT implementations is needed.
Findings from this review on organizational culture and HIT implementation can be applicable to the evolving concept of LHS, as informatics is an integral element of LHS. The journey to being effective LHS is iterative characterized by strong leadership, along with a culture and workforce committed to continuous learning and improvement. 15 McGinnis et al, 77 noted in a recent perspective that the digital revolution with HIT and advanced analytics has the potential to increase the scale, speed, and sophistication of LHS. These advances along with a supportive organizational culture will facilitate the adoption of best practices in care processes and generate new knowledge as part of healthcare delivery and support the continuous learning loop of an effective LHS.
4.1. Limitations
This scoping review has some limitations. The study sample is restricted to only US‐based implementations and so results may not be generalizable to other contexts or settings. The review content was limited to studies where the data were mostly gathered post‐2010 and so the portrayal of the role of organizational culture in HIT implementations is restricted to a single decade. All the identified publications focused on the process of HIT implementations and included culture and inner settings concepts as part of that research. The culture and related constructs were inferenced by the researchers and were not measured explicitly in the studies. Data abstraction from these publications required significant effort on the part of the researchers with ongoing discussion and reaching consensus. Finally, this review did not specifically examine other factors related to implementation failures or successes; so, additional research is needed to identify cultural constructs related to implementation outcomes.
5. CONCLUSION
Supported by a detailed analysis of 52 studies, this scoping review provides insights into the current state of the science around HIT implementation and the inner settings of an organization including culture. This study also underscores the need to recognize organizational culture as an important element during implementations of HIT. Our findings point to the need for additional research to facilitate the understanding of the role of organizational culture, specifically the characteristics that facilitate HIT implementation and hence serve as a platform to support LHS.
CONFLICT OF INTEREST
The authors declare that they do not have any competing interests.
AUTHOR CONTRIBUTIONS
Genevieve B. Melton provided guidance throughout the review and writing process. Sripriya Rajamani, Gretchen Hultman, and Caitlin Bakker participated in all stages of the review process from conceptualization, screening, data extraction and analysis. Sripriya Rajamani led the drafting of the manuscript and all authors read and approved the final version.
Supporting information
Data S1. Supporting information.
Data S2. Supporting information.
Rajamani S, Hultman G, Bakker C, Melton GB. The role of organizational culture in health information technology implementations: A scoping review. Learn Health Sys. 2022;6(3):e10299. doi: 10.1002/lrh2.10299
REFERENCES
- 1. Centers for Medicare and Medicaid Services . EHR Incentive Programs. 2010 [cited March 9, 2021]. Available from: http://www.cms.gov/ehrincentiveprograms
- 2. Office of the National Coordinator for Health Information Technology. 21st Century Cures Act 2020 [cited January 23, 2021]. Available from: https://www.healthit.gov/curesrule/
- 3. HIMSS . CARES Act Provisions for Healthcare and Health IT 2020 [cited January 16, 2021]. Available from: https://www.himss.org/news/cares-act-provisions-healthcare-and-health-it
- 4. HIMSS . HIT or Miss: Lessons Learned from Health Information Technology Projects. (HIMSS Book Series) 3rd Edition. 2019.
- 5. CFIR Research Team . Consolidated Framework for Implementation Research (CFIR). 2009 [cited March 23, 2021]. Available from: https://cfirguide.org/
- 6. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implem Sci. 2009;4(1):50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Li S‐A, Jeffs L, Barwick M, Stevens B. Organizational contextual features that influence the implementation of evidence‐based practices across healthcare settings: a systematic integrative review. Syst Rev. 2018;7(1):72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gershon RR, Stone PW, Bakken S, Larson E. Measurement of organizational culture and climate in healthcare. J Nurs Adm. 2004;34(1):33‐40. [DOI] [PubMed] [Google Scholar]
- 9. Fernandez ME, Walker TJ, Weiner BJ, et al. Developing measures to assess constructs from the inner setting domain of the consolidated framework for implementation research. Implement Sci. 2018;13(1):52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. University of Michigan Learning Health Sciences . Learning Health Systems. 2015. [cited May 29, 2021]. Available from: https://medicine.umich.edu/dept/lhs/service-outreach/learning-health-systems
- 11. Friedman CP, Rubin JC, Sullivan KJ. Toward an information infrastructure for Global Health improvement. Yearb Med Inform. 2017;26(1):16‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. National Academy of Medicine (NAM) . The Learning Healthcare System: Workshop Summary. Washington, DC: The National Academies Press; 2007. [cited May 29, 2021]. Available from:. doi: 10.17226/11903 [DOI] [PubMed] [Google Scholar]
- 13. Wienert J. Understanding health information technologies as complex interventions with the need for thorough implementation and monitoring to sustain patient safety. Front ICT. 2019;6(9):1–5. [Google Scholar]
- 14. Vinson A. Culture as infrastructure in learning health systems. Learn Health Syst. 2021;5:e10267. doi: 10.1002/lrh210267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Agency for Healthcare Research and Quality (AHRQ) . Learning Health Systems. 2017. [cited May 29, 2021]. Available from: https://www.ahrq.gov/learning-health-systems/index.html.
- 16. Shea CM, Belden CM. What is the extent of research on the characteristics, behaviors, and impacts of health information technology champions? A scoping review. BMC Med Inform Decis Mak. 2016;16:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Miech EJ, Rattray NA, Flanagan ME, Damschroder L, Schmid AA, Damush TM. Inside help: an integrative review of champions in healthcare‐related implementation. SAGE Open Med. 2018;6:2050312118773261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gui X, Chen Y, Zhou X, Reynolds TL, Zheng K, Hanauer DA. Physician champions' perspectives and practices on electronic health records implementation: challenges and strategies. JAMIA Open. 2020;3(1):53‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19‐32. [Google Scholar]
- 20. Foster ED, Deardorff A. Open science framework (OSF). J Med Libr Assoc. 2017;105(2):203‐206. [Google Scholar]
- 21. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan ‐ a web and mobile app for systematic reviews. Syst Rev. 2016;5:210. doi: 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tricco A, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA‐ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467‐473. doi: 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 23. Bachmann JM, Posch DR, Hickson GB, et al. Developing an implementation strategy for systematic measurement of patient‐reported outcomes at an academic health center. J Healthc Manag. 2020;65(1):15‐28. [DOI] [PubMed] [Google Scholar]
- 24. Businger AC, Fuller TE, Schnipper JL, et al. Lessons learned implementing a complex and innovative patient safety learning laboratory project in a large academic medical center. J Am Med Inform Assoc. 2020;27(2):301‐307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cartier Y, Fichtenberg C, Gottlieb LM. Implementing community resource referral technology: facilitators and barriers described by early adopters. Health Aff. 2020;39(4):662‐669. [DOI] [PubMed] [Google Scholar]
- 26. Chipps E, Tucker S, Labardee R, et al. The impact of the electronic health record on moving new evidence‐based nursing practices forward. Worldviews Evid Based Nurs. 2020;17(2):136‐143. [DOI] [PubMed] [Google Scholar]
- 27. Heinze KL, Heinze JE. Individual innovation adoption and the role of organizational culture. Rev Manag Sci. 2020;14(3):561‐586. [Google Scholar]
- 28. Sieck CJ, Pearl N, Bright TJ, Yen PY. A qualitative study of physician perspectives on adaptation to electronic health records. BMC Med Inform Decis Mak. 2020;20(1):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Angoff GH, O'Connell JJ, Gaeta JM, et al. Electronic medical record implementation for a healthcare system caring for homeless people. JAMIA Open. 2019;2(1):89‐98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chaturvedi RR, Etchegaray JM, Raaen L, Jackson J, Friedberg MW. Technology Isn't the half of it: integrating electronic health records and infusion pumps in a large hospital. Jt Comm J Qual Patient Saf. 2019;45(10):649‐661. [DOI] [PubMed] [Google Scholar]
- 31. Orenstein EW, Yun K, Warden C, et al. Development and dissemination of clinical decision support across institutions: standardization and sharing of refugee health screening modules. J Am Med Inform Assoc. 2019;26(12):1515‐1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Pittman JOE, Afari N, Floto E, et al. Implementing eScreening technology in four VA clinics: a mixed‐method study. BMC Health Serv Res. 2019;19(1):604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rangachari P, Dellsperger KC, Rethemeyer RK. A qualitative study of interprofessional learning related to electronic health record (EHR) medication reconciliation within a social knowledge networking (SKN) system. J Healthc Leadersh. 2019;11:23‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zhang R, Burgess ER, Reddy MC, et al. Provider perspectives on the integration of patient‐reported outcomes in an electronic health record. JAMIA Open. 2019;2(1):73‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Anderson RJ, Sparbel K, Barr RN, Doerschug K, Corbridge S. Electronic health record tool to promote team communication and early patient mobility in the intensive care unit. Crit Care Nurse. 2018;38(6):23‐34. [DOI] [PubMed] [Google Scholar]
- 36. Barrett AK. Technological appropriations as workarounds: integrating electronic health records and adaptive structuration theory research. Inf Technol People. 2018;31(2):368‐387. [Google Scholar]
- 37. Campione JR, Mardon RE, McDonald KM. Patient safety culture, health information technology implementation, and medical office problems that could lead to diagnostic error. J Patient Saf. 2019;15(4):267‐273. [DOI] [PubMed] [Google Scholar]
- 38. Chung C, Patel S, Lee R, et al. Implementation of an integrated computerized prescriber order‐entry system for chemotherapy in a multisite safety‐net health system. Am J Health Syst Pharm. 2018;75(6):398‐406. [DOI] [PubMed] [Google Scholar]
- 39. Masterson Creber RM, Dayan PS, Kuppermann N, et al. Applying the RE‐AIM framework for the evaluation of a clinical decision support tool for pediatric head trauma: a mixed‐methods study. Appl Clin Inform. 2018;9(3):693‐703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Giuliano CA, Binienda J, Kale‐Pradhan PB, Fakih MG. “I never would have caught that before”: pharmacist perceptions of using clinical decision support for antimicrobial stewardship in the United States. Qual Health Res. 2018;28(5):745‐755. [DOI] [PubMed] [Google Scholar]
- 41. Hao H, Padman R. An empirical study of opinion leader effects on mobile technology implementation by physicians in an American community health system. Health Informatics J. 2018;24(3):323‐333. [DOI] [PubMed] [Google Scholar]
- 42. Rao‐Gupta S, Kruger D, Leak LD, Tieman LA, Manworren RCB. Leveraging interactive patient care technology to improve pain management engagement. Pain Manag Nurs. 2018;19(3):212‐221. [DOI] [PubMed] [Google Scholar]
- 43. Kim J, Ohsfeldt RL, Gamm LD, Radcliff TA, Jiang L. Hospital characteristics are associated with readiness to attain stage 2 meaningful use of electronic health records. J Rural Health. 2017;33(3):275‐283. [DOI] [PubMed] [Google Scholar]
- 44. Kooienga S, Singh RL. Pharmacy and primary care perspectives on e‐prescribing in a rural community: a focused ethnography. Res Social Adm Pharm. 2017;13(4):820‐830. [DOI] [PubMed] [Google Scholar]
- 45. Leslie M, Paradis E, Gropper MA, Kitto S, Reeves S, Pronovost P. An ethnographic study of health information technology use in three intensive care units. Health Serv Res. 2017;52(4):1330‐1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Mason P, Mayer, R ., Chien, W ., & Monestime, J. P. (2017). Overcoming barriers to implementing electronic health Records in Rural Primary Care Clinics. Qualitat Rep, 22(11), 2943–2955. Retrieved from https://nsuworks.nova.edu/tqr/vol22/iss11/7. [Google Scholar]
- 47. Reidy J, Halvorson J, Makowski S, et al. Health system advance care planning culture change for high‐risk patients: the promise and challenges of engaging providers, patients, and families in systematic advance care planning. J Palliat Med. 2017;20(4):388‐394. [DOI] [PubMed] [Google Scholar]
- 48. Saleem N, Steel D, Gercek G, Chandra A. Significance of user participation in a hospital information system success: insights from a case study. Health Care Manag. 2017;36(2):199‐205. [DOI] [PubMed] [Google Scholar]
- 49. Tobler N, Colvin J, Rawlins NW. Longitudinal analysis and coping model of user adaptation. J Comput Inf Syst. 2017;57(2):97‐105. [Google Scholar]
- 50. Ballaro J, Washington ER. The impact of organizational culture and perceived organizational support on successful use of electronic healthcare record (EHR). Organiz Dev J. 2016;34:11. [Google Scholar]
- 51. Bentley T, Rizer M, McAlearney AS, et al. The journey from precontemplation to action: transitioning between electronic medical record systems. Health Care Manage Rev. 2016;41(1):22‐31. [DOI] [PubMed] [Google Scholar]
- 52. Gross AH, Leib RK, Tonachel A, et al. Teamwork and electronic health record implementation: a case study of preserving effective communication and mutual trust in a changing environment. J Oncol Pract. 2016;12(11):1075‐1083. [DOI] [PubMed] [Google Scholar]
- 53. Lin C‐P, Guirguis‐Blake J, Keppel GA, et al. Using the diffusion of innovations theory to assess socio‐technical factors in planning the implementation of an electronic health record alert across multiple primary care clinics. J Innov Health Inform. 2016;23(1):450‐458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Queenan CCKT, Devaraj S. Complements or substitutes? Culture–technology interactions in healthcare. Decis Sci. 2016;47(5):851‐880. doi: 10.1111/deci.12199 [DOI] [Google Scholar]
- 55. Ramsey A, Lord S, Torrey J, Marsch L, Lardiere M. Paving the way to successful implementation: identifying key barriers to use of technology‐based therapeutic tools for behavioral health care. J Behav Health Serv Res. 2016;43(1):54‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Callahan EJ, Sitkin N, Ton H, Eidson‐Ton WS, Weckstein J, Latimore D. Introducing sexual orientation and gender identity into the electronic health record: one academic health center's experience. Acad Med. 2015;90(2):154‐160. [DOI] [PubMed] [Google Scholar]
- 57. Collins SA, Alexander D, Moss J. Nursing domain of CI governance: recommendations for health IT adoption and optimization. J Am Med Inform Assoc. 2015;22(3):697‐706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Elias B, Barginere M, Berry PA, Selleck CS. Implementation of an electronic health records system within an interprofessional model of care. J Interprof Care. 2015;29(6):551‐554. [DOI] [PubMed] [Google Scholar]
- 59. McAlearney AS, Hefner JL, Sieck CJ, Huerta TR. The journey through grief: insights from a qualitative study of electronic health record implementation. Health Serv Res. 2015;50(2):462‐488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Sherer SA, Meyerhoefer CD, Sheinberg M, Levick D. Integrating commercial ambulatory electronic health records with hospital systems: an evolutionary process. Int J Med Inform. 2015;84(9):683‐693. [DOI] [PubMed] [Google Scholar]
- 61. Wright A, Sittig DF, Ash JS, et al. Lessons learned from implementing service‐oriented clinical decision support at four sites: a qualitative study. Int J Med Inform. 2015;84(11):901‐911. [DOI] [PubMed] [Google Scholar]
- 62. Wright A, McCoy AB, Hickman TT, et al. Problem list completeness in electronic health records: a multi‐site study and assessment of success factors. Int J Med Inform. 2015;84(10):784‐790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Yuan CT, Bradley EH, Nembhard IM. A mixed methods study of how clinician ‘super users’ influence others during the implementation of electronic health records. BMC Med Inform Decis Mak. 2015;15:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Chase DA, Ash JS, Cohen DJ, Hall J, Olson GM, Dorr DA. The EHR's roles in collaboration between providers: a qualitative study. AMIA Annu Symp Proc. 2014;2014:1718‐1727. [PMC free article] [PubMed] [Google Scholar]
- 65. Fairbrother G, Trudnak T, Christopher R, Mansour M, Mandel K. Cincinnati Beacon community program highlights challenges and opportunities on the path to care transformation. Health Aff. 2014;33(5):871‐877. [DOI] [PubMed] [Google Scholar]
- 66. Muslin IS, Vardaman JM, Cornell PT. Fostering acceptance of computerized physician order entry: insights from an implementation study. Health Care Manag. 2014;33(2):165‐171. [DOI] [PubMed] [Google Scholar]
- 67. Shea CM, Reiter KL, Weaver MA, et al. Stage 1 of the meaningful use incentive program for electronic health records: a study of readiness for change in ambulatory practice settings in one integrated delivery system. BMC Med Inform Decis Mak. 2014;14(1):119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Wells S, Rozenblum R, Park A, Dunn M, Bates DW. Organizational strategies for promoting patient and provider uptake of personal health records. J Am Med Inform Assoc. 2015;22(1):213‐222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Boswell RA. Implementing electronic health records: implications for HR professionals. Strateg HR Rev. 2013;12(5):262‐268. [Google Scholar]
- 70. Craven CK, Sievert MC, Hicks LL, Alexander GL, Hearne LB, Holmes JH. Experts speak: advice from key informants to small, rural hospitals on implementing the electronic health record system. Stud Health Technol Inform. 2013;192:608‐612. [PubMed] [Google Scholar]
- 71. Kitzmiller Rebecca R, McDaniel Reuben R, Johnson Constance M, Lind EA, Anderson Ruth A. Exploring interpersonal behavior and team sensemaking during health information technology implementation. Leading in Health Care Organizations: Improving Safety, Satisfaction and Financial Performance. Advances in Health Care Management. 14: Emerald Group Publishing Limited; 2013. p. 119–44. [DOI] [PubMed]
- 72. Ash JS, Sittig DF, Guappone KP, et al. Recommended practices for computerized clinical decision support and knowledge management in community settings: a qualitative study. BMC Med Inform Decis Mak. 2012;12:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Lanham HJ, Leykum LK, McDaniel RR Jr. Same organization, same electronic health records (EHRs) system, different use: exploring the linkage between practice member communication patterns and EHR use patterns in an ambulatory care setting. J Am Med Inform Assoc. 2012;19(3):382‐391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. McAlearney AS, Robbins J, Kowalczyk N, Chisolm DJ, Song PH. The role of cognitive and learning theories in supporting successful EHR system implementation training: a qualitative study. Med Care Res Rev. 2012;69(3):294‐315. [DOI] [PubMed] [Google Scholar]
- 75. Office of the National Coordinator for Health Information Technology . Certified Health IT Developers and Editions Reported by Hospitals Participating in the Medicare EHR Incentive Program, Health IT Quick‐Stat #29. dashboard.healthit.gov/quickstats/pages/FIG-Vendors-of-EHRs-to-Participating-Hospitals.php. July 2017.
- 76. Office of the National Coordinator for Health Information Technology . ‘Certified Health IT Developers and Editions Reported by Health Care Professionals Participating in the Medicare EHR Incentive Program,’ Health IT Quick‐Stat #30. dashboard.healthit.gov/quickstats/pages/FIG-Vendors-of-EHRs-to-Participating-Professionals.php. July 2017.
- 77. McGinnis JM, Fineberg HV, Dzau VJ. Advancing the learning health system. N Engl J Med. 2021;385(1):1‐5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Supporting information.
Data S2. Supporting information.


