Abstract
Background:
Delirium in critically ill patients is independently associated with poor clinical outcomes. There is a scarcity of published data on the prevalence of delirium among critically ill patients in Saudi Arabia. Therefore, we sought to determine, in a multicenter fashion, the prevalence of delirium in critically ill patients in Saudi Arabia and explore associated risk factors.
Methods:
A cross-sectional point prevalence study was conducted on January 28, 2020, at 14 intensive care units (ICUs) across 3 universities and 11 other tertiary care hospitals in Saudi Arabia. Delirium was screened once using the Intensive Care Delirium Screening Checklist. We excluded patients who were unable to participate in a valid delirium assessment, patients admitted with traumatic brain injury, and patients with documented dementia in their medical charts.
Results:
Of the 407 screened ICU patients, 233 patients were enrolled and 45.9% were diagnosed with delirium. The prevalence was higher in mechanically ventilated patients compared to patients not mechanically ventilated (57.5% vs. 33.6%; P < 0.001). In a multivariate model, risk factors independently associated with delirium included age (adjusted odds ratio [AOR], 1.021; 95% confidence interval [CI], 1.01–1.04; P = 0.008), mechanical ventilation (AOR, 2.39; 95% CI, 1.34–4.28; P = 0.003), and higher severity of illness (AOR, 1.01; 95% CI, 1.001–1.021; P = 0.026).
Conclusion:
In our study, delirium remains a prevalent complication, with distinct risk factors. Further studies are necessary to investigate long-term outcomes of delirium in critically ill patients in Saudi Arabia.
Keywords: Cross-sectional studies, delirium, intensive care units, prevalence, Saudi Arabia
INTRODUCTION
Delirium, defined according to the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, fifth edition, is a common neurological disorder typically characterized by fluctuations in inattention, confusion, and disorganized thinking, occurring over a short period of time.[1] It normally develops in 20%–50% of critically ill patients who are not being mechanically ventilated and in 50%–80% of mechanically ventilated patients.[2,3,4,5,6] The variability in the reported rates is highly dependent on the population studied and the diagnostic tools used.
Critically ill patients who develop delirium more often have an increased risk of rehospitalization, longer time in the intensive care unit (ICU) and on a mechanical ventilator, and higher mortality rates; they are also more likely to be discharged to a long-term care facility.[5,6,7,8] Moreover, delirium is frequently linked to increased hospital costs and worsening cognitive function that persists for months to years after discharge.[9,10,11,12]
The risk of developing delirium is dependent on the presence of predisposing and precipitating factors.[13] Among published studies, considerable variability has been cited regarding multiple risk factors for delirium. Evidence suggests strongly that modifiable and nonmodifiable risk factors associated with the occurrence of delirium are benzodiazepine use, blood transfusion, dementia, prior coma, increasing age, pre-ICU emergency surgery or trauma, and an increased acute physiology and chronic health evaluation (APACHE) score.[14,15]
Delirium continues to be under-recognized due to its fluctuating nature and the paucity of routine formal ICU delirium assessments. In fact, it is estimated that the under-recognition rate is 30%–75%.[16] Therefore, and in view of the negative sequelae of delirium, Guidelines issued by the Society of Critical Care Medicine on the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU have endorsed routine delirium screening in the ICU with either the validated Confusion Assessment Method-ICU (CAM-ICU) or Intensive Care Delirium Screening Checklist (ICDSC).[15] The overall agreement between the two delirium assessment tools has been found to be good [kappa coefficient of 0.80 (confidence interval [CI] 95% 0.78–0.84; P < 0.001).[17]
The CAM assesses four features: the presence of an acute onset of symptoms, a fluctuating course, inattention, and either disorganized thinking or an altered level of consciousness. The algorithm screens for delirium in a focused patient assessment approach and takes 2–5 min to complete.[3] In contrast, the 8-domain ICDSC assesses four symptoms – altered level of consciousness, inattention, disorientation, and psychosis – in a focused patient assessment method and four domains that include psychomotor activity, inappropriate speech, sleep disturbance, and fluctuation over the prior and current nursing shift. An ICDSC score ≥4 has been shown to be highly associated with a formal psychiatric diagnosis of delirium.[18]
Both scales are validated in several languages, including Arabic and English.[3,18,19,20] The Arabic CAM-ICU and ICDSC were shown to be valid and reliable for delirium assessment among critically ill patients.[3,18] The Richmond Agitation–Sedation Scale (RASS) is commonly utilized to evaluate sedation and agitation in critically ill patients and is commonly used with the CAM-ICU or ICDSC to detect delirium.[21,22]
Studies reporting the prevalence of delirium and related risk factors among critically ill patients in Saudi Arabia are scarce. In fact, only a few reports have been published so far. A survey conducted in one ICU in Saudi Arabia showed that 54% of the ICU clinicians including nurses and physicians rate their knowledge and skills with regard to delirium assessment and management as fair to poor.[23] Another group of investigators detected delirium, via psychiatrist assessments, in 63% of patients.[19] Moreover, the Arabic ICDSC was recently established, demonstrating an acceptable validity and reliability in detecting delirium among the critically ill Arabic-speaking population. In this particular study, the incidence of delirium was 21% using psychiatrist evaluations and 17% using the Arabic ICDSC.[20] Finally, another group has investigated the risk factors associated with ICU delirium development and detected a strong association with sedation, mechanical ventilation, and a baseline Glasgow Coma Scale score of <15. The incidence of ICU delirium using the CAM-ICU was 17.3%.[24]
The results obtained from these studies are considerably lower than those reported from international studies (45%–87%).[25,26] Whether this is due to sampling error alone or actual distinctions between the studied populations such as demographics, mixed ethnicities, or comorbidities remains to be determined through larger studies in Saudi Arabia. Therefore, the objectives of this first Saudi Arabian multicenter cross-sectional study of delirium in ICUs were to (1) determine the point prevalence of ICU delirium among a cohort of critically ill patients in Saudi Arabia and to (2) identify the risk factors associated with the development of delirium.
METHODS
Study design
We conducted a 1-day cross-sectional multicenter study in 14 ICUs across 3 universities and 11 other tertiary care teaching hospitals in Saudi Arabia. The size of the units ranged between 6 and 75 ICU beds. Hospitals were selected after seeking an expression of interest and no incentives were provided to the participants. To augment the representation of large tertiary care hospitals, secondary and private hospitals were not included. Geographical representation was also considered. We included a convenience sample of hospitals located in the Central (C), Eastern (E), and Western (W) regions (R) of Saudi Arabia. All the ICUs are closed, multidisciplinary units, and have well-established pain and sedation protocols. On January 28, 2020, eligible patients who were expected to stay in the ICU for at least 24 h and had a RASS score ≥−3 were screened for possible enrollment. We excluded patients admitted to the ICU following a traumatic brain injury, those with documented dementia in their medical chart as defined by the patient's primary care physician/psychiatrist, and those who were unable to participate in a valid delirium assessment (e.g., ICU admission because of acute or chronic neurologic disease and/or severe electrolyte disturbance). The ICDSC was used as the delirium screening tool. While the time of assessment was not standardized across sites, trained ICU physicians and/or critical care clinical pharmacists who were part of the research study completed the scale in the morning. The evaluations utilized included information from the last 24 h. Delirious patients were defined as those with an ICDSC score of ≥4. We used the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement to draft this manuscript.[27] The study was conducted in accordance with the Declaration of Helsinki and the International Council for Harmonisation–Good Clinical Practice. It was reviewed and approved by the local Institutional Review Board at each site.
Data collection and management
An electronic case report form was used for data collection using a secure online web-based Research Electronic Data Capture (REDCap®) tool (Vanderbilt, Nashville, USA).[28] For each study site, investigators received training on data entry and management. Each facility had independent access secured with user-authorized credentials. No protected health information was shared between the sites. Hard copies of the data collection forms were made available to all study investigators as needed. Site investigators were instructed and trained on how to use the ICDSC through online educational materials on delirium. An independent delirium expert was available to answer the questions of study investigators. A conference call explaining the application and pitfalls of the ICDSC and the REDCap® electronic data capture system was scheduled with all investigators 1 week before the commencement of the study.
Data analysis
Statistical analysis was performed using the Windows-based IBM Statistical Package for the Social Sciences (SPSS) Version 24.0 (IBM, Armonk, NY, USA) program. Descriptive and inferential statistics were used to characterize the study sample and test hypotheses. Descriptive results (including graphical displays) for all quantitative/continuous variables were presented as means ± standard deviations for normally distributed data or as medians with inter-quartile range for nonparametric data. Frequencies, proportions, and their 95% CI were used to describe the qualitative categorical variables. Bivariate analysis was performed using either the independent sample t-test or Mann–Whitney U-test, as appropriate, to compare quantitative/continuous variables, while Pearson Chi-square analysis or Fisher's exact test was used, as appropriate, to compare all qualitative categorical variables between those with delirium versus those without delirium. A multiple logistic regression model was generated and tested to identify significant independent factors associated with the presence of delirium among patients, after adjusting for potentially confounding factors. The Wald test was computed on each predictor to determine its significance. The adjusted odds ratios and 95% CIs for the adjusted odds ratio have also been reported. Two-tailed P < 0.05 was considered statistically significant.
RESULTS
A total of 14 ICUs were involved in the study, of which 6 participated from the Central Region (CR) (1 university and 5 tertiary care hospitals) and 4 from each the Western Region (WR) (1 university and 3 tertiary care hospitals) and the Eastern Region (ER) (1 university and 3 tertiary care hospitals). On the study day, 407 patients were screened for possible enrollment; 174 patients were excluded. The most common reason for exclusion was a low level of consciousness (RASS <−3), which was found in 82 screened patients [Figure 1]. The enrolled 233 patients who met the inclusion criteria were assessed for the presence of delirium. The overall prevalence of delirium was 45.9% [Figure 2]. Of the 107 patients with delirium, 49 (45.8%) had hypoactive delirium and 58 (54.2%) had hyperactive delirium. Most patients who were not diagnosed with delirium (123/126, 98%) developed subsyndromal delirium (ICDSC 1–3).
Figure 1.
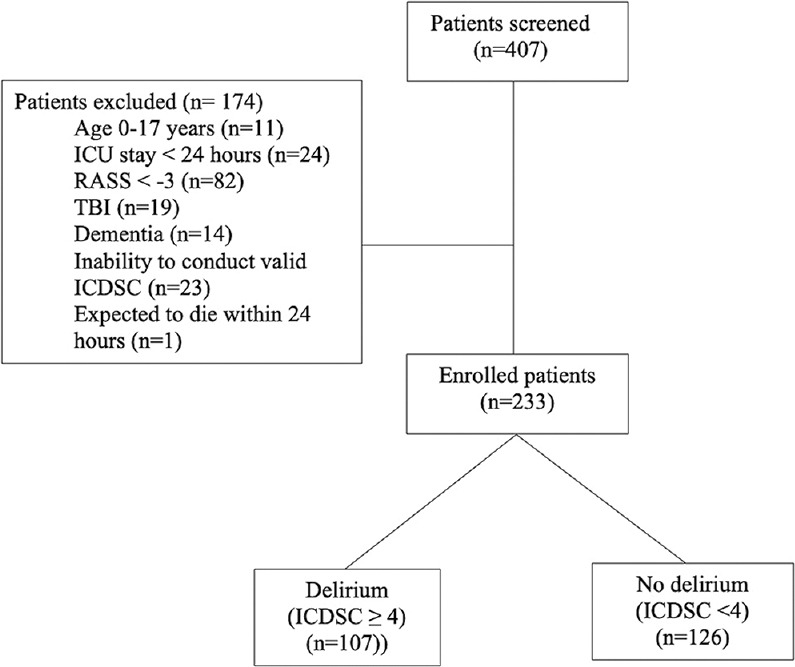
Flowchart of patients in the study. ICU: Intensive care unit, RASS: Richmond Agitation–Sedation Scale, TBI: Traumatic brain injury, ICDSC: Intensive Care Delirium Sscreening Checklist
Figure 2.
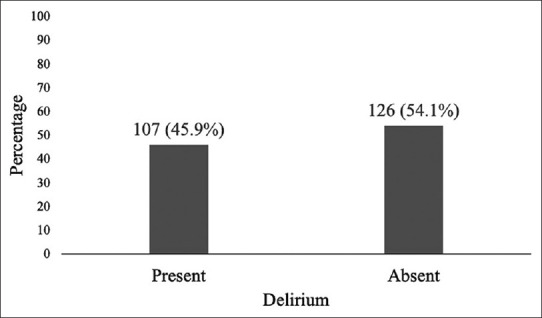
Overall prevalence of delirium
Of the 14 participating sites, the prevalence of delirium was highest at Site 3-ER (78.6%; 11/14) and Site 1-WR (72.2%; 13/18) and lowest at Site 1-ER (0%; 0/2) and Site 2-ER (0%; 0/1). It is worth noting that the prevalence of ICU delirium varied markedly between sites, these findings might be spurious due to low sample size in some hospitals [Figure 3]. Table 1 summarizes baseline characteristics of the study subjects, stratified by delirium status. Among the delirious group, 55 (46.6%) were males. The mean age of the patients with delirium was 60.3 ± 18.2 years. Delirious patients were more likely to be older (P = 0.001), have more severe illness (P = 0.005), and be on mechanical ventilation (P < 0.001) compared to nondelirious patients. There was a trend toward having lower median RASS scores in the delirious group, relative to the nondelirious group (P = 0.051).
Figure 3.
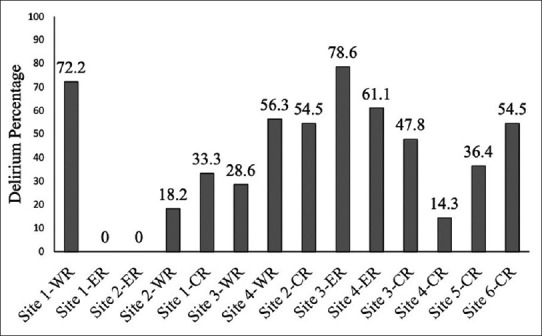
Prevalence of delirium by hospital. WR: Western Region, ER: Eastern Region, CR: Central Region
Table 1.
Baseline characteristics of patients with and without delirium
| Clinical characteristic | Delirium (n=107) | No delirium (n=126) | P $ |
|---|---|---|---|
| Age (years), mean±SD | 60.30±18.15 | 51.52±20.16 | 0.001‡ |
| Gender, n (%) | |||
| Male | 55 (46.6) | 63 (53.4) | 0.831 |
| Female | 52 (45.2) | 63 (54.8) | |
| RASS at enrollment, median (IQR) | −1 (−2–0) | 0 (0–0) | 0.051† |
| APACHE IV, median (IQR) | 54 (28–87) | 40 (26–68) | 0.009† |
| Mechanically ventilation at time of assessment, n (%) | |||
| Mechanically ventilated | 69 (57.5) | 51 (42.5) | <0.001 |
| Nonmechanically ventilated | 38 (33.6) | 75 (66.4) | |
| Received blood transfusion (n) | 47 | 54 | 0.870 |
| ICU type (n) | |||
| Medical | 79 | 78 | |
| Surgical | 22 | 29 | |
| Neurological | 6 | 13 | |
| Other | 0 | 6 | |
| Primary admitting diagnosis to ICU (n) | |||
| Sepsis | 28 | 22 | |
| Respiratory | 47 | 41 | |
| Neurologic | 15 | 14 | |
| Cardiac | 5 | 8 | |
| Surgery | 3 | 11 | |
| Other | 9 | 30 | |
| Location immediately prior to ICU admission (n) | |||
| Emergency department | 56 | 65 | |
| Hospital ward | 37 | 38 | |
| Operating room following surgery | 5 | 9 | |
| ICU at outside hospital | 6 | 9 | |
| Ward at outside hospital | 1 | 3 | |
| Medications received (n) | |||
| Fentanyl | 31 | 36 | |
| Propofol | 5 | 6 | |
| Dexmedetomidine | 9 | 5 | |
| Midazolam | 8 | 11 |
$P value has been calculated using Pearson Chi-Square test, ‡P value has been calculated using Independent sample t-test, †P value has been calculated using nonparametric Mann–Whitney U-test, ^P value has been calculated using Fisher’s exact test. SD: Standard deviation, RASS: Richmond Agitation–Sedation Scale, APACHE: Acute physiology and chronic health evaluation, ICU: Intensive care unit, IQR: Interquartile range
Delirium was more prevalent in mechanically ventilated patients (P < 0.001) compared to patients who were not being mechanically ventilated [Figure 4]. In contrast, delirium prevalence was not affected by admitting service, medical or surgical ICU, hospital ward or emergency room admission, presence of sepsis on admission, blood transfusion, or medication use for analgesia or sedation.
Figure 4.
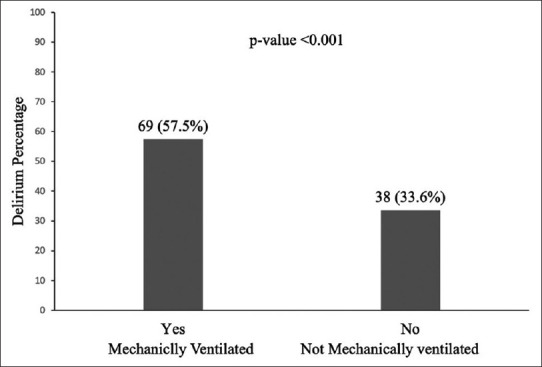
Prevalence of delirium by mechanically ventilated
Multiple logistic regression analysis identified age (P = 0.008), higher severity of illness (P = 0.026), and the presence of mechanical ventilation (P = 0.003) as independent predictors of delirium in critically ill patients after adjusting for gender, blood transfusion, and medication use. We did not find a significant independent relationship between ICU delirium and other variables [Table 2]. Likewise, no independent effect of hospitals on the prevalence of delirium in critically ill patients was noted.
Table 2.
Multiple binary logistic regression model to identify significant independent factors associated with delirium
| Factor | AOR* (95% CI for AOR) | P |
|---|---|---|
| Mechanically ventilated | 2.206 (1.090-4.464) | 0.028 |
| Age (years) | 1.021 (1.004-1.038) | 0.014 |
| APACHE IV | 1.013 (1.002-1.023) | 0.022 |
| Gender | 1.098 (0.591-2.040) | 0.767 |
| Blood transfusion | 0.918 (0.486-1.736) | 0.793 |
| Fentanyl | 0.636 (0.274-1.476) | 0.292 |
| Propofol | 1.445 (0.377-5.548) | 0.591 |
| Dexmedetomidine | 2.203 (0.656-7.393) | 0.201 |
| Midazolam | 2.037 (0.528-7.857) | 0.302 |
| RASS at enrollment | 0.944 (0.715-1.248) | 0.687 |
*AOR of delirium presence versus absent. Hosmer and Lemeshow goodness-of-fit test, χ2=7.87, df=8 and P=0.446. Results are expressed as AOR and 95% CI for AOR. APACHE IV: Acute physiology and chronic health evaluation IV, AOR: Adjusted odds ratio, CI: Confidence interval, RASS: Richmond Agitation–Sedation Scale
DISCUSSION
This is the first multicenter study to explore the prevalence of delirium in critically ill patients in Saudi Arabia over a single day. Our findings suggest that the overall prevalence of ICU delirium is high, at 45.9%, with a higher prevalence in mechanically ventilated patients (57.5%). These results are consistent with other studies that have evaluated delirium in critically ill mechanically ventilated patients.[2,3,4,5,6] In addition, in one other meta-analysis, critically ill patients on mechanical ventilation were found to be at higher risk of developing delirium than those not being mechanically ventilated (odds ratio = 4.51 [95% CI: 1.41–14.39]).[29] One possible reason for this may be that mechanically ventilated ICU patients are predisposed to hypoxemia and lung infections, both of which increase their risk of developing delirium.[30] In our study, we noticed wide variations in the reported frequencies of delirium among participating sites, ranging from 0% to almost 79%, which raises important questions regarding the type of patients enrolled, severity of illness, depth of sedation, and delirium assessment practices across sites.
Moreover, on multivariable analysis, after adjusting for factors such as gender, blood transfusion, and medication use, we identified age, more severe illness, and the presence of mechanical ventilation as independently associated with a higher odds of delirium.
Previously published literature has shown that patients with delirium are usually above 65 years of age and have an APACHE II score ≥20.[14,31,32,33,34,35] Likewise, other studies have documented the mean age of patients with delirium ranging between 64 and 70.7 years.[36,37,38] In contrast, the severity of illness between study populations has varied widely; for example, in a study by Kanova et al., among patients with a lower risk of mortality upon admission and a median APACHE II score of 12, the prevalence of delirium was just 20.3%. Conversely, in the study by Agarwal's group, which consisted of burn ICU patients with a higher risk of mortality and a median APACHE II score of 27, the prevalence of delirium was 71%.[33,38] In our cohort, the mean age of patients with delirium was 60 years and the median APACHE IV score was 54.
Our study has several notable strengths, including its prospective multicenter design and the inclusion of a large number of patients from multiple ICUs in numerous regions across Saudi Arabia. As such, we believe that our results have high internal and external validity, thereby increasing the generalizability of our findings. In addition, the study is the first to rigorously assess the prevalence of delirium in critically ill patients in Saudi Arabia. Moreover, for delirium detection, we used the ICDSC tool, a validated tool for delirium detection in the ICU.
Our study also has a few limitations. First, the participation of hospitals was voluntary; hence, the participating ICUs might not be representative of all ICUs; in other words, the ICUs we studied might differ from those not engaged in the study. Second, the delirium assessment occurred just once during the ICU stay and, as such, episodes of delirium could have been missed. In addition, delirium severity was not included in our data collection. Third, this 1-day point prevalence study may be subject to potential seasonal selection bias. Moreover, variables such as baseline health status, presence of natural versus artificial light,[39] baseline religiosity,[40] and ambient noise might have confounded our results and affected delirium incidence and severity across study sites. Finally, while we did not study the interrater reliability of the ICDSC, we provided adequate training and practice on the instrument during the introductory phase of the study. Further evidence from randomized, prospective clinical trials is needed to confirm the relationship between ICU delirium and individual risk factors and to characterize delirium outcomes in critically ill patients in Saudi Arabia.
CONCLUSION
In summary, this is, so far, the largest point prevalence study of ICU delirium in Saudi Arabia, revealing a prevalence of 45.9% across different ICUs. Mechanical ventilation, age, and high severity of illness were independent risk factors of delirium. Our findings highlight the importance of delirium detection, specifically in more severely ill and higher-risk patients. Further randomized prospective clinical trials are needed to confirm the relationship between ICU delirium and identifiable risk factors and to characterize the delirium outcomes in this patient population.
Research quality and ethics statement
This study was approved by the Institutional Review Board/Ethics Committee at the King Fahad Specialist Hospital-Dammam (Approval #ICU0306; Approval date December 1, 2019). The authors followed the applicable EQUATOR Network (http://www.equator-network.org/) guidelines, specifically the STROBE Guidelines, during the conduct of this research project.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We wish to thank the ICU staff at all cohort sites for making this study possible. We also express our appreciation to the Saudi Critical Care Trial group for their support in this work.
REFERENCES
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington DC: American Psychiatric Association; 2013. [Google Scholar]
- 2.Ely EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L, et al. Delirium in mechanically ventilated patients: Validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU) JAMA. 2001;286:2703–10. doi: 10.1001/jama.286.21.2703. [DOI] [PubMed] [Google Scholar]
- 3.Ely EW, Margolin R, Francis J, May L, Truman B, Dittus R, et al. Evaluation of delirium in critically ill patients: Validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) Crit Care Med. 2001;29:1370–9. doi: 10.1097/00003246-200107000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Pun BT, Ely EW. The importance of diagnosing and managing ICU delirium. Chest. 2007;132:624–36. doi: 10.1378/chest.06-1795. [DOI] [PubMed] [Google Scholar]
- 5.Ely EW, Gautam S, Margolin R, Francis J, May L, Speroff T, et al. The impact of delirium in the intensive care unit on hospital length of stay. Intensive Care Med. 2001;27:1892–900. doi: 10.1007/s00134-001-1132-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell FE, Jr, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291:1753–62. doi: 10.1001/jama.291.14.1753. [DOI] [PubMed] [Google Scholar]
- 7.Ouimet S, Kavanagh BP, Gottfried SB, Skrobik Y. Incidence, risk factors and consequences of ICU delirium. Intensive Care Med. 2007;33:66–73. doi: 10.1007/s00134-006-0399-8. [DOI] [PubMed] [Google Scholar]
- 8.van den Boogaard M, Schoonhoven L, van der Hoeven JG, van Achterberg T, Pickkers P. Incidence and short-term consequences of delirium in critically ill patients: A prospective observational cohort study. Int J Nurs Stud. 2012;49:775–83. doi: 10.1016/j.ijnurstu.2011.11.016. [DOI] [PubMed] [Google Scholar]
- 9.Milbrandt EB, Deppen S, Harrison PL, Shintani AK, Speroff T, Stiles RA, et al. Costs associated with delirium in mechanically ventilated patients. Crit Care Med. 2004;32:955–62. doi: 10.1097/01.ccm.0000119429.16055.92. [DOI] [PubMed] [Google Scholar]
- 10.Witlox J, Eurelings LS, de Jonghe JF, Kalisvaart KJ, Eikelenboom P, van Gool WA. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: A meta-analysis. JAMA. 2010;304:443–51. doi: 10.1001/jama.2010.1013. [DOI] [PubMed] [Google Scholar]
- 11.Girard TD, Jackson JC, Pandharipande PP, Pun BT, Thompson JL, Shintani AK, et al. Delirium as a predictor of long-term cognitive impairment in survivors of critical illness. Crit Care Med. 2010;38:1513–20. doi: 10.1097/CCM.0b013e3181e47be1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bickel H, Gradinger R, Kochs E, Förstl H. High risk of cognitive and functional decline after postoperative delirium.A three-year prospective study. Dement Geriatr Cogn Disord. 2008;26:26–31. doi: 10.1159/000140804. [DOI] [PubMed] [Google Scholar]
- 13.Vasilevskis EE, Han JH, Hughes CG, Ely EW. Epidemiology and risk factors for delirium across hospital settings. Best Pract Res Clin Anaesthesiol. 2012;26:277–87. doi: 10.1016/j.bpa.2012.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zaal IJ, Devlin JW, Peelen LM, Slooter AJ. A systematic review of risk factors for delirium in the ICU. Crit Care Med. 2015;43:40–7. doi: 10.1097/CCM.0000000000000625. [DOI] [PubMed] [Google Scholar]
- 15.Devlin JW, Skrobik Y, Glélinas C, Needham D, Slooter AJ, Pandharipande P, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility and sleep disruption in adult patients in the ICU. Crit Care Med. 2018;46:e825–73. doi: 10.1097/CCM.0000000000003299. [DOI] [PubMed] [Google Scholar]
- 16.Collins N, Blanchard MR, Tookman A, Sampson EL. Detection of delirium in the acute hospital. Age Ageing. 2010;39:131–5. doi: 10.1093/ageing/afp201. [DOI] [PubMed] [Google Scholar]
- 17.Plaschke K, von Haken R, Scholz M, Engelhardt R, Brobeil A, Martin E, et al. Comparison of the confusion assessment method for the intensive care unit (CAM-ICU) with the Intensive Care Delirium Screening Checklist (ICDSC) for delirium in critical care patients gives high agreement rate (s) Intensive Care Med. 2008;34:431–6. doi: 10.1007/s00134-007-0920-8. [DOI] [PubMed] [Google Scholar]
- 18.Bergeron N, Dubois MJ, Dumont M, Dial S, Skrobik Y. Intensive care delirium screening checklist: Evaluation of a new screening tool. Intensive Care Med. 2001;27:859–64. doi: 10.1007/s001340100909. [DOI] [PubMed] [Google Scholar]
- 19.Aljuaid MH, Deeb AM, Dbsawy M, Alsayegh D, Alotaibi M, Arabi YM. Psychometric properties of the Arabic version of the confusion assessment method for the intensive care unit (CAM-ICU) BMC Psychiatry. 2018;18:91. doi: 10.1186/s12888-018-1676-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.AlQadheeb NS, Nazer LH, Aisa TM, Osman H, Rugaan A, Alzahrani A, et al. Arabic intensive delirium screening checklist's validity andreliability: A multicenter study. J Crit Care. 2019;54:170–4. doi: 10.1016/j.jcrc.2019.08.025. [DOI] [PubMed] [Google Scholar]
- 21.Riker RR, Picard JT, Fraser GL. Prospective evaluation of the sedation-agitation scale for adult critically ill patients. Crit Care Med. 1999;27:1325–9. doi: 10.1097/00003246-199907000-00022. [DOI] [PubMed] [Google Scholar]
- 22.Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O’Neal PV, Keane KA, et al. The richmond agitation-sedation scale: Validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. 2002;166:1338–44. doi: 10.1164/rccm.2107138. [DOI] [PubMed] [Google Scholar]
- 23.Aljuaid M. The role of Saudi Critical Care Trials Group in advancing delirium prevention and management. Saudi Crit Care J. 2019;3:48–51. [Google Scholar]
- 24.Rasheed AM, Amirah M, Abdallah M, Awajeh AM, Parameaswari PJ, Al Harthy A. Delirium incidence and risk factors in adult critically Ill patients in Saudi Arabia. J Emerg Trauma Shock. 2019;12:30–4. doi: 10.4103/JETS.JETS_91_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–9. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 26.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde J. Research electronic data capture (REDCap®)-a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huai J, Ye X. A meta-analysis of critically ill patients reveals several potential risk factors for delirium. Gen Hosp Psychiatry. 2014;36:488–96. doi: 10.1016/j.genhosppsych.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 28.Elpern EH, Scott MG, Petro L, Ries MH. Pulmonary aspiration in mechanically ventilated patients with tracheostomies. Chest. 1994;105:563–6. doi: 10.1378/chest.105.2.563. [DOI] [PubMed] [Google Scholar]
- 29.Arumugam S, El-Menyar A, Al-Hassani A, Strandvik G, Asim M, Mekkodithal A, et al. Delirium in the Intensive Care Unit. J Emerg Trauma Shock. 2017;10:37–46. doi: 10.4103/0974-2700.199520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pandharipande P, Shintani A, Peterson J, Pun BT, Wilkinson GR, Dittus RS, et al. Lorazepam is an independent risk factor for transitioning to delirium in intensive care unit patients. Anesthesiology. 2006;104:21–6. doi: 10.1097/00000542-200601000-00005. [DOI] [PubMed] [Google Scholar]
- 31.Zhang Z, Pan L, Deng H, Ni H, Xu X. Prediction of delirium in critically ill patients with elevated C-reactive protein. J Crit Care. 2014;29:88–92. doi: 10.1016/j.jcrc.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 32.McNicoll L, Pisani MA, Zhang Y, Ely EW, Siegel MD, Inouye SK. Delirium in the intensive care unit: Occurrence and clinical course in older patients. J Am Geriatr Soc. 2003;51:591–8. doi: 10.1034/j.1600-0579.2003.00201.x. [DOI] [PubMed] [Google Scholar]
- 33.Kanova M, Sklienka P, Roman K, Burda M, Janoutova J. Incidence and risk factors for delirium development in ICU patients a prospective observational study. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2017;161:187–96. doi: 10.5507/bp.2017.004. [DOI] [PubMed] [Google Scholar]
- 34.Salluh JI, Soares M, Teles JM, Ceraso D, Raimondi N, Nava VS, et al. Delirium epidemiology in critical care (DECCA): An international study. Crit Care. 2010;14:R210. doi: 10.1186/cc9333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ryan DJ, O’Regan NA, Caoimh RÓ, Clare J, O’Connor M, Leonard M, et al. Delirium in an adult acute hospital population: Predictors, prevalence and detection. BMJ Open. 2013;3:e001772. doi: 10.1136/bmjopen-2012-001772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grover S, Lahariya S, Bagga S, Sharma A. Incidence, prevalence and risk factors for delirium in elderly admitted to a coronary care unit. J of Geriatr Ment Health. 2014;1:45–53. [Google Scholar]
- 37.Kalish VB, Gillham JE, Unwin BK. Delirium in older persons: Evaluation and management. Am Fam Physician. 2014;90:150–8. [PubMed] [Google Scholar]
- 38.Agarwal V, O’Neill PJ, Cotton BA, Pun BT, Haney S, Thompson J, et al. Prevalence and risk factors for development of delirium in burn intensive care unit patients. J Burn Care Res. 2010;31:706–15. doi: 10.1097/BCR.0b013e3181eebee9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vahedian-Azimi A, Bashar FR, Khan AM, Miller AC. Natural versus artificial light exposure on delirium incidence in ARDS patients. Ann Intensive Care. 2020;10:15. doi: 10.1186/s13613-020-0630-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Farzanegan B, Elkhatib THM, Elgazzar AE, Moghaddam KG, Torkaman M, Zarkesh M, et al. Impact of religiosity on delirium severity among critically Ill Shi’a Muslims: A prospective multi-center observational study. J Relig Health. 2021;60:816–40. doi: 10.1007/s10943-019-00895-7. [DOI] [PubMed] [Google Scholar]


