Abstract
Recent systematic reviews of plantar warts continue to consider cryotherapy as one of the treatments of choice, but this method appears to have lower cure rates than alternative treatments. A systematic review using meta‐analyses of the efficacy of cryotherapy in plantar warts treatment was performed. Systematic electronic searches were conducted. The primary endpoint was complete clearance of plantar warts. Risk‐of‐bias assessment was based on Cochrane Handbook recommendations. Meta‐analyses used Review Manager v5.4.1 software. Cryotherapy appears to have lower cure rates than other treatments (odds ratio [OR] 0.31, 95% confidence interval [CI] 0.12–0.78) with substantial heterogeneity (I 2 = 80%). A second subgroup analysis had low heterogeneity (I 2 = 28.2%). Subgroup analysis showed that plantar wart cure rates were significantly lower with cryotherapy compared to the physical treatment group (OR 0.05, 95% CI 0.01–0.49) with substantial heterogeneity (I 2 = 79%), and antiviral, chemotherapy, and retinoid group (OR 0.30, 95% CI 0.14–0.66) without heterogeneity (I 2 = 0%). Intralesional versus spray‐on cryotherapy appears to be more effective (OR 0.21, 95% CI 0.09–0.48). No difference in efficacy between two rounds of 10‐s and four rounds of 5‐s freeze–thaw cycles in cryotherapy was found. Evidence of the superiority of antivirals and chemotherapy over cryotherapy in the treatment of plantar warts was found. However, no evidence supports the superiority or inferiority of cryotherapy compared to other treatments.
Keywords: cryotherapy, HPV, human papillomavirus, meta‐analyses, plantar warts, systematic review
1. INTRODUCTION
Plantar warts are benign tumors caused by human papilloma virus (HPV) infection of the epidermal cells 1 with an estimated annual incidence of 14%. 2 The HPV types most frequently detected on the foot are 1, 2, 4, 10, 27, and 57. 1 , 3
A wide variety of treatments, such as cryotherapy, salicylic acid, cantharidin, bleomycin, intralesional immunotherapy, and/or laser are used, but none have been shown to be highly effective in all patients. 3 , 4 The aim of most treatments is to destroy the affected epidermal cells, through a chemical burn or damage of the wart tissue by applying physical methods, which damages healthy perilesional tissue and causes pain in patients. 4 , 5 But sometimes the cell damage is not sufficient to destroy the latent virus in adjacent cells. 4 As a result, treatments sometimes fail, leading to recalcitrant and recurrent warts. 4 This recurrence leads 2% of the general population to seek annual medical attention due to pain and limitation of some activities, aesthetic reasons, and prevention of infections to other areas of the body or other people. 2 , 4 , 6 , 7
Cryotherapy is considered by most of healthcare providing facilities as the treatment of choice in common wart management. 8 It is the most common method for treating warts 9 and it is based on the destruction of infected tissue by the application of liquid nitrogen‐induced cold, producing a sharp, localized freezing, followed by a slow thawing. 9 , 10 The advantages of using cryotherapy are rapid application and cost‐effectiveness 9 although pain, dyspigmentation, scar formation, delayed healing, and/or relapses are potential side effects. 11
Recent systematic reviews of the range of treatments for plantar warts continue to consider cryotherapy together with salicylic acid as one of the treatments of choice. 4 , 12 However, this traditional method appears to produce lower cure rates (45.61%) than alternative treatments, such as laser (79.36%), a combination of cantharidin 1%, podophyllotoxin 5%, and salicylic acid 30% (CPS formulation) (97.82%), or topical antivirals (72.45%). 4
Currently, no specific systematic review using a meta‐analysis of the efficacy of cryotherapy in plantar warts has been published. The objectives of this systematic review and meta‐analysis were to assess cryotherapy efficacy when compared with other interventions to treat plantar warts.
2. MATERIAL AND METHODS
This systematic review and meta‐analyses were performed in accordance with the general guidelines and recommendations made by preferred reporting items for systematic reviews and meta‐analyzes (PRISMA). 13
2.1. Literature search
Pubmed, Cochrane Library, Embase, and Web of Science were systematically searched in July of 2021. The following search terms together with the Boolean operator “AND”: “plantar warts,” “treatment,” and “cryotherapy” were used.
2.2. Article selection
Inclusion criteria were randomized controlled clinical trials (RCTs) of the effects of cryotherapy of plantar warts, in male and/or female patients of any age, published in English or Spanish, from the first article published until July 2021.
Title and abstract review were performed independently by two reviewers. Any discrepancies between the two reviewers were discussed with a third reviewer. Articles were excluded in which the treatment was carried out on common and/or genital warts and in which the cure rate of any of the topical treatment was not recorded.
2.3. Data extraction
Two reviewers independently reviewed full texts for inclusion, and data extraction of the included articles was performed. The following outcomes were collected from each study: (1) type of study, (2) demographic data (number subjects, age, and sex), (3) topical interventions, (4) type of treatment (chemical, physical, antiviral, and immunotherapy), (5) complete cure rate (%), and (6) the number of treatment sessions.
2.4. Quality assessment and risk of bias
The type of study was also recorded and classified according to levels of evidence and grades of recommendation proposed by the Oxford Center for Evidence‐Based Medicine (OCEBM). 14
The risk of bias was estimated for two experienced reviewers independently (SGO and FJAA) using the Cochrane Collaboration's tool 15 for assessing risk of bias, according to six specific domains: (1) random‐sequence generation (selection bias), (2) allocation concealment (selection bias), (3) blinding (performance bias and detection bias), (4) incomplete outcome data (attrition bias), (5) selective reporting (reporting bias), and (6) other biases (including supposed financial support). Each domain was evaluated for low, high, or unclear risk for bias. Any discrepancies between the two reviewers were discussed with a third reviewer.
2.5. Statistical analysis
The patient was the unit of analysis for all studies. Studies reporting similar interventions were combined for meta‐analysis. Thus, the meta‐analysis was conducted in four subgroups: (1) keratolytics; (2) physical treatments; (3) antivirals, chemotherapy, and retinoids; and (4) placebo and others treatments. Review Manager v5.4.1 (http://ims.cochrane.org/revman) 16 was used to analyze the data with the Mantel–Haenszel method for dichotomous outcomes according to a fixed‐effect or random‐effects model. Estimates of the intervention's effects are expressed as odd ratio (OR) (95% CI). Heterogeneity was estimated clinically and methodologically, and when Higgins' I 2 exceeded 50%, a random‐effects model was used. 17
The significance of any discrepancies in the estimates of the treatment effects from the different trials was assessed by means of the Cochrane test for heterogeneity and the I 2 statistic.
3. RESULTS
3.1. Literature search
One‐hundred‐fifty‐three non‐duplicate articles were identified in the initial search strategy. Title and abstract review excluded 127 articles, while a full‐text review excluded an additional 17 articles. Fourteen RCTs were included in this systematic review as outlined in the PRISMA flow diagram (Figure 1). 13
FIGURE 1.
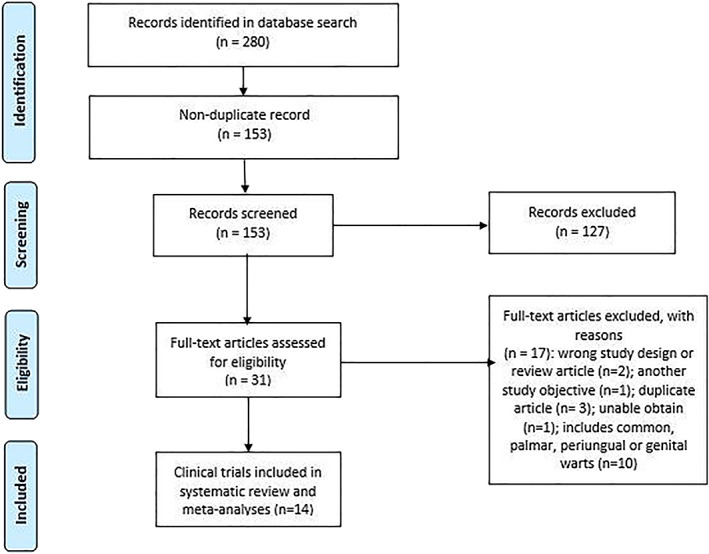
Preferred reporting items for systematic reviews and meta‐analyzes (PRISMA) flow diagram of the literature search and study selection for the systematic review of cryotherapy in plantar warts
3.2. Study characteristics and risk of bias
The 14 RCTs included 1084 participants with a mean of 77 subjects per study. All studies were published between 1984 and 2020. Only two studies reported the total number of warts treated.
Cryotherapy was compared with 40% trichloroacetic acid solution (TCA) 9 , 18 or laser 19 , 20 in two trials, duct tape, 8 intralesional bleomycin, 21 topical 10% formaldehyde soaks, 22 adapalene 0.1% gel, 23 CPS formulation, 24 radiofrequency ablation, 25 salicylic acid, 6 acyclovir cream, 26 or placebo 26 in one trial. In addition, studies carried out by Albalat et al. 11 and Leow et al. 27 compared the efficacy of two modalities of cryotherapy.
All studies were randomized controlled trials and therefore had a level of evidence of 1b and grade of recommendation A according to the Oxford Center for Evidence‐Based Medicine (OCEBM) classification 14 (Table 1).
TABLE 1.
Characteristics of the plantar warts treatment studies included in this review
| First author, year | Target population | Topical interventions | Type of study | Levels of evidence | Grades of recommendation |
|---|---|---|---|---|---|
| Albalat, 11 2020 | >18 years | Arm 1: intralesional cryotherapy | RCT | 1b | A |
| Arm 2: cryotherapy spray | |||||
| Karrabi, 9 2020 | 8–40 years | Arm 1: 40% trichloroacetic acid | RCT | 1b | A |
| Arm 2: cryotherapy with a cotton swab | |||||
| Abdel‐Latif, 8 2019 | All | Arm 1: duct tape | RCT | 1b | A |
| Arm 2: cryotherapy spray | |||||
| Muhammad, 21 2019 | 20–50 years | Arm 1: intralesional bleomycin 0.1% | RCT | 1b | A |
| Arm 2: cryotherapy with a cotton swab | |||||
| Hemmatian Boroujeni, 19 2018 | >18 years | Arm 1: cryotherapy | RCT | 1b | A |
| Arm 2: CO2 laser | |||||
| Ahmad, 22 2018 | >12 years | Arm 1: topical 10% formaldehyde soaks | RCT | 1b | A |
| Arm 2: cryotherapy spray | |||||
| Leow, 27 2017 | ≥21 years | Cryotherapy spray | RCT | 1b | A |
| Arm 1: two rounds of 10‐s sustained freeze | |||||
| Arm 2: four rounds of 5‐s sustained freeze | |||||
| Cengiz, 18 2016 | >18 years | Arm 1: cryotherapy spray | RCT | 1b | A |
| Arm 2: trichloroacetic acid 40% solution | |||||
| Gupta, 23 2015 | All | Arm 1: adapalene 0.1% gel twice daily under occlusion using plastic wrap | RCT | 1b | A |
| Arm 2: cryotherapy spray | |||||
| Kaçar, 24 2011 | >18 years | Arm 1: topical preparation of cantharidin (1%), podophylline (5%), salicylic acid (30%) | RCT | 1b | A |
| Arm 2: cryotherapy spray | |||||
| Arora, 25 2014 | All | Arm 1: cryotherapy spray | RCT | 1b | A |
| Arm 2: radiofrequency ablation | |||||
| Cockayne, 6 2011 | >12 years | Arm 1: cryotherapy | RCT | 1b | A |
| Arm 2: daily patient self‐treatment with 50% salicylic acid | |||||
| El‐Tonsy, 20 1999 | All | Arm 1: Nd:YAG laser | RCT | 1b | A |
| Arm 2: cryotherapy with cotton‐tipped applicator | |||||
| Gibson, 26 1984 | All | Arm 1: 5% acyclovir cream | RCT | 1b | A |
| Arm 2: placebo cream | |||||
| Arm 3: cryotherapy spray |
Abbreviation: RCT, randomized control trial.
Figures 2 and 3 summarize the risk‐of ‐bias assessment of the studies included.
FIGURE 2.
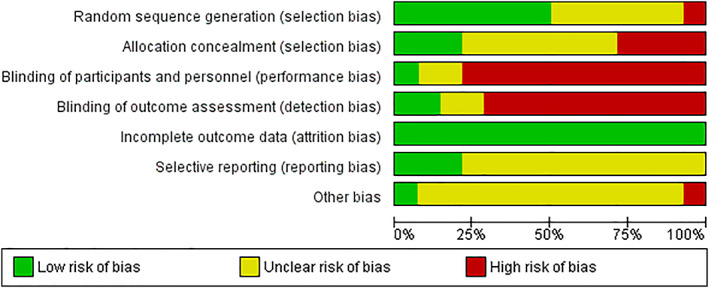
Risk of bias graph: review authors' judgments about each risk of bias item presented as percentages across all included studies
FIGURE 3.
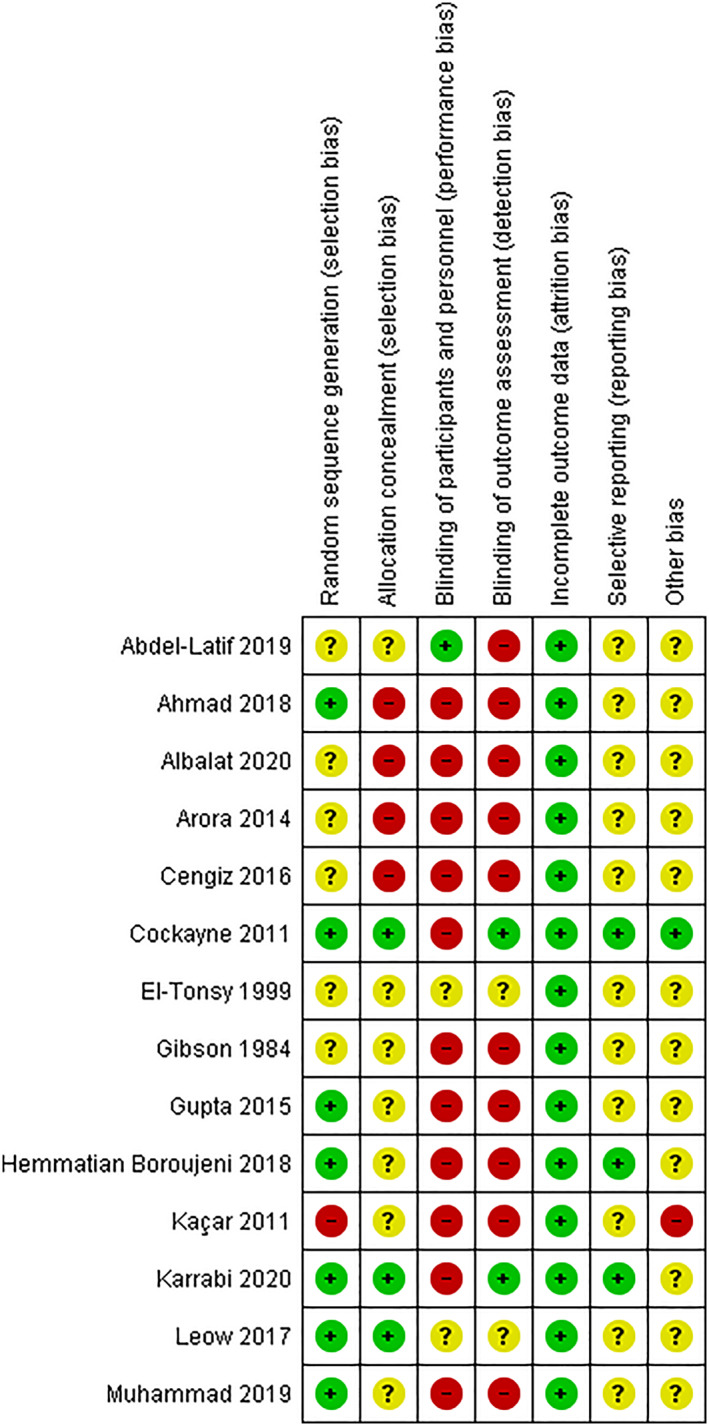
Risk of bias summary: review authors' judgments about each risk of bias item for each included study
3.3. Plantar warts clearance postintervention: Cryotherapy versus other treatments
Table 2 presents the information on the number of patients included in each study, the cure rates of the different analyze treatments, the follow‐up periods, and the number of sessions applied for each treatment.
TABLE 2.
A summary of the reported efficacy of topical treatments against plantar warts
| First author, year | Topical interventions | No of participants (no of lesions) | Cure rate (%) | Follow up/evaluation period | No of treatment required |
|---|---|---|---|---|---|
| Albalat, 11 2020 |
Arm 1: intralesional cryotherapy Arm 2: cryotherapy spray |
Arm 1: 60 Arm 2: 59 Total: 119 |
Arm 1: 50/60 (83.3) Arm 2: 30/59 (50.8) |
6 months | Maximum five sessions |
| Karrabi, 9 2020 |
Arm 1: 40% trichloroacetic acid Arm 2: cryotherapy with a cotton swab |
Arm 1: 30 Arm 2: 30 Total: 60 |
Arm 1: 26/30 (86.67) Arm 2: 23/30 (76.67) |
6 months |
Arm1: 4 sessions Arm 2: 4 sessions |
| Abdel‐Latif, 8 2019 |
Arm 1: duct tape Arm 2: cryotherapy with cryo‐gun |
Arm 1: 50 Arm 2: 50 Total: 100 |
Arm 1: 10/50 (20) Arm 2: 29/50 (58) |
Arm 1: 8 weeks Arm 2: 8–12 weeks. |
Arm 1: the tape was removed after 6 days. Arm 2: 4 sessions. |
| Muhammad, 21 2019 |
Arm 1: intralesional bleomycin 0.1% Arm 2: cryotherapy with a cotton swab |
Arm 1: 80 Arm 2: 80 Total: 160 |
Arm 1: 72/80 (90) Arm 2: 58/80 (72.5) |
6 weeks | One session |
| Hemmatian Boroujeni, 19 2018 |
Arm 1: cryoteraphy Arm 2: CO2 laser |
Arm 1: 27 Arm 2: 29 Total: 56 |
Arm 1: 19/27 (70.4) Arm 2: 26/29 (89.7) |
3 months |
Arm 1: 3 sessions (maximum 12 weeks) Arm 2: 1 session (maximum 3 sessions) |
| Ahmad, 22 2018 |
Arm 1: topical 10% formaldehyde soaks Arm 2: cryotherapy spray |
Arm 1: 13 Arm 2: 15 Total: 28 |
Arm 1: 6/13 (46.2) Arm 2: 7/15 (46.7) |
3 months |
Arm 1: applied by the patients at home twice daily. Arm 2: applied by the physician every 2 weeks |
| Leow, 27 2017 |
Cryotherapy spray Arm 1: two rounds of 10‐s sustained freeze Arm 2: four rounds of 5‐s sustained freeze |
Arm 1: 25 Arm 2: 24 Total: 49 |
Arm 1: 25/25 (100) Arm 2: 23/24 (95.8) |
— | Maximum 12 sessions |
| Cengiz, 18 2016 |
Arm 1: cryotherapy spray Arm 2: trichloroacetic acid 40% solution |
Arm 1: 30 Arm 2: 30 Total: 60 |
Arm 1: 1/30 (3.3) Arm 2: 6/30 (20) |
Arm 1: 8 weeks Arm 2: 4 weeks |
Four sessions |
| Gupta, 23 2015 |
Arm 1: adapalene 0.1% gel twice daily under occlusion using plastic wrap Arm 2: cryotherapy spray |
Arm 1: 25 Arm 2: 25 Total: 50 (424) |
Arm 1: 24/25 (96) Arm 2: 24/25 (96) |
6 months |
Arm 1: 36.71 ± 19.24 days Arm 2: 52.17 ± 30.06 days (1–4 sessions) |
| Kaçar, 24 2011 |
Arm 1: topical preparation of cantharidin (1%), podophylline (5%), salicylic acid (30%) Arm 2: cryotherapy spray |
Arm 1: 14 Arm 2: 12 Total: 26 |
Arm 1: 14/14 (100) Arm 2: 5/12 (41.7) |
— | Maximum five sessions |
| Arora, 25 2014 |
Arm 1: cryotherapy spray Arm 2: radiofrequency ablation |
Arm 1: 25 (77) Arm 2: 25 (132) Total: 50 |
Arm 1: 8/25 (32) Arm 2: 21/25 (84) |
12 weeks | Average of 5.63 sessions |
| Cockayne, 6 2011 |
Arm 1: cryotherapy Arm 2: daily patient self‐treatment with 50% salicylic acid |
Arm 1: 119 Arm 2: 110 Total: 229 |
Arm 1: 17/119 (14.3) Arm 2: 15/110 (13.6) |
12 weeks and 6 months |
Arm 1: four sessions Arm 2: daily patient self‐treatment for a maximum of 8 weeks |
| El‐Tonsy, 20 1999 |
Arm 1: Nd:YAG laser Arm 2: cryotherapy with a cotton‐tipped applicator |
Arm 1: 25 Arm 2: 25 Total: 50 |
Arm 1: 24/25 (96) Arm 2: 0/25 (0) |
8 weeks | Three sessions |
| Gibson, 26 1984 |
Arm 1: 5% acyclovir cream Arm 2: placebo cream Arm 3: cryotherapy spray |
Arm 1: 18 Arm 2: 18 Arm 3: 11 Total: 47 |
Arm 1: 7/18 (38,8) Arm 2: 5/18 (27,7) Arm 3: 1/11 (9) |
8 weeks |
Arm 1: applied once daily for 6 weeks Arm 2: applied once daily for 6 weeks Arm 3: four sessions (on entry into the study and at weeks 2, 4, and 6) |
A first meta‐analysis with 12 studies including 927 patients compared the effects of cryotherapy versus other treatments 6 , 8 , 9 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 (Figure 4). Meta‐analysis of this data estimated the pooled odds ratio (OR) at 0.31 (95% confidence interval [CI] 0.12–0.78) with substantial heterogeneity (x 2 = 60.85, df = 12, p = 0.01, I 2 = 80%).
FIGURE 4.
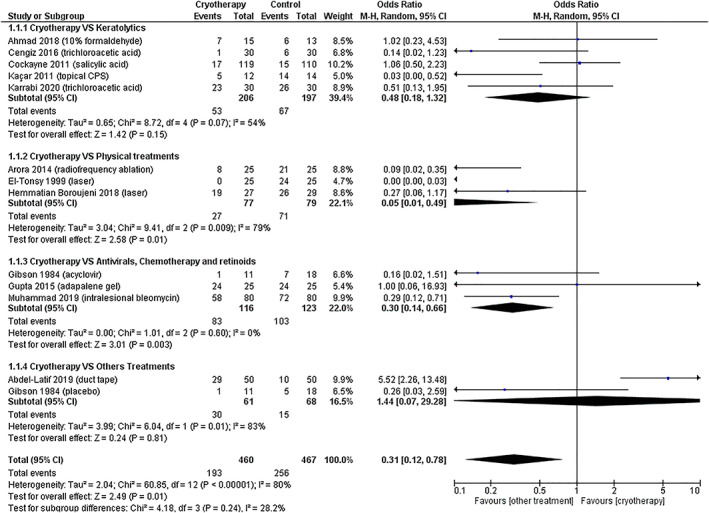
Forest plot of comparison: 1 cure rate, outcome: 1.1 cryotherapy versus other treatments
Subsequently, a second analysis by subgroups was performed with low heterogeneity (x 2 = 4.18, df = 3, p = 0.24, I 2 = 28.2%). Five studies included 403 patients compared the effects of cryotherapy versus keratolytic agents (daily patient self‐treatment with 50% salicylic acid, 40% trichloroacetic acid, and 10% formaldehyde and topical CPS). 6 , 9 , 18 , 22 , 24 Meta‐analysis of this data estimated the pooled OR at 0.48 (95% CI 0.18–1.32) with substantial heterogeneity (x 2 = 8.72, df = 4, p = 0.07, I 2 = 54%). Three studies including 156 patients compared the effects of cryotherapy versus physical treatments (laser and radiofrequency ablation). 19 , 20 , 25 Meta‐analysis of this data estimated the pooled OR at 0.05 (95% CI 0.01–0.49) with substantial heterogeneity (x 2 = 9.41, df = 2, p = 0.009, I 2 = 79%). Three studies with 239 patients compared the effects of cryotherapy versus antivirals (5% acyclovir cream), chemotherapy (intralesional bleomycin), and retinoids (adapalene 0.1% gel). 21 , 23 , 26 Meta‐analysis of this data estimated the pooled OR at 0.30 (95% CI 0.14–0.66), favoring antivirals and chemotherapy without heterogeneity (x 2 = 1.01, df = 6, p = 0.60, I 2 = 0%). Two studies with 129 patients compared the effects of cryotherapy versus placebo and others (duct tape). 19 , 20 , 25 Meta‐analysis of this data estimated the pooled OR at 1.44 (95% CI 0.07–29.28) with substantial heterogeneity (x 2 = 6.04, df = 1, p = 0.01, I 2 = 83%).
On the other hand, one RCT enrolled 119 patients and compared the effects of cryotherapy spray versus intralesional cryotherapy, 11 and other RCT enrolled 49 patients and compared two different liquid nitrogen cryotherapy regimes. 27 Clinical improvement differed significantly favoring the intralesional cryotherapy (OR 0.21, 95% CI 0.09–0.48), and no differences in efficacy between two rounds of 10‐s and four rounds of 5‐s freeze–thaw cycles in cryotherapy (OR 3.26, 95% CI 0.13–83.90) were found.
4. DISCUSSION
To our knowledge, this study is the first systematic review consisting of a meta‐analysis that evaluates the efficacy of cryotherapy for the treatment of plantar warts.
This systematic review with meta‐analysis of the efficacy of cryotherapy in patients with plantar warts indicated that cryotherapy appears to have lower cure rates than other treatments in most randomized clinical trials published so far. However, the high heterogeneity (I 2 = 80%) allowed us to conclude that no evidence supports the superiority or inferiority of cryotherapy when compared to other treatments. When we performed a meta‐analysis by subgroups (keratolytics, physical treatments, antiviral, chemotherapy, and retinoids, and placebo and others), heterogeneity between subgroups was low (I 2 = 28.2%), and the cure rates of plantar warts were significantly lower with cryotherapy compared to the physical treatment group and the antiviral, chemotherapy, and retinoids group. The high heterogeneity (I 2 = 79%) of the results of the meta‐analysis of the physical treatment subgroup allowed us to conclude that no evidence supports the superiority of this group over cryotherapy. In contrast, the zero heterogeneity (I 2 = 0) found in the meta‐analysis of the antiviral and chemotherapy treatment subgroup does provide evidence for the superiority of these treatments over cryotherapy. In both the keratolytic and placebo groups, no statistically significant findings to support the superiority or inferiority of cryotherapy was found, but these results are also inconclusive due to the high heterogeneity found in both groups (I 2 = 54% and I 2 = 83%, respectively).
In addition, intralesional cryotherapy appears to be more effective than spray‐on cryotherapy, and no differences in efficacy between two rounds of 10‐s and four rounds of 5‐s freeze–thaw cycles in cryotherapy were found.
A 2011 systematic review and meta‐analysis on the efficacy of topical treatments for skin warts concluded that cryotherapy (cure rate: 45%–75%) should be considered as second‐line treatment with salicylic acid (cure rate: 0%–87%) as the first‐line treatment. 28 By contrast, in a recent systematic review, cure rates in plantar warts were found to be higher with cryotherapy (45.61%) than salicylic acid (13.6%). 4 This difference might also be due to the different characteristics of plantar skin and plantar warts. 4 Moreover, cure rates with cryotherapy were also higher than with tape (15%) but low compared to other treatments such as CPS formulation (97.82%), immunotherapy (68.14%), laser (79.36%), topical antivirals (72.45%), and intralesional bleomycin (83.37%). 4 In another recent systematic review of large interventional and observational studies (more than 100 patients per study), the authors concluded that cryotherapy and salicylic acid remain the first‐choice treatments despite having lower efficacy than novel treatments such as laser. 12 Other novel treatments, such as intralesional injections including intralesional immunotherapy, are promising but were not represented owing to lack of large studies. 12 The paucity of RCTs included in each comparison is a limitation in drawing conclusions on the efficacy of cryotherapy compared to other treatments.
Regarding the level of evidence and the degree of recommendation of the included studies, all were controlled and RCTs with a level of evidence of 1b and degree of recommendation A. In 10/14 and 11/14 of the included studies, a high risk‐of‐bias in the blinding of results and of participants and/or professionals respectively was found. A high risk‐of‐bias in the allocation concealment in 4/14 studies and high risk of bias in the random sequency in 1/14 studies was found. In general, in all studies a medium or high risk of bias in some of the items was observed, mainly due to lack of information. Even though all studies were randomized clinical trials, the high risk of bias in the blinding of patients and professionals together with the lack of information in most of the studies limits the conclusions of this review with meta‐analysis. In the meta‐analysis by Bertolotti et al. 29 concerning the efficacy of cryotherapy for anogenital warts, they also found a high risk of bias in blinding. The authors consider blinding of the practitioner applying a non‐pharmacological treatment to be difficult and recommend the design of strategies for future RCTs, such as not informing participants of the study objectives until the end of the study. 29
Another limitation of the present study is the total cure rate was only analyzed and other aspects, such as partial clearance, number of sessions, time to cure, patient satisfaction, quality of life during treatment, and cost‐effectiveness ratios were not considered. Many of these variables were also not reported in most other studies. In addition, the intensity of cryotherapy and duration of application or form of application (spray or swab) was not sufficiently standardized in the RCTs. The lack of studies of each treatment was another limitation when making the subgroups since not enough articles could be found to be able to analyze each intervention separately from cryotherapy. Therefore, we grouped the treatments into four major subgroups (keratolytics, physical treatments, antiviral, chemotherapy, and retinoids, and placebo and others). For this reason, heterogeneity was high in most of the subgroups.
Future clinical trials with low risk of bias, using control groups, with clear randomization and blinding of results could help clarify our conclusions. In addition, it is recommended that the sample size of each treatment group be calculated and that results of total and partial clearances, number of sessions, healing times, patient satisfaction, and quality of life during treatment be recorded. We also consider that a subsequent follow‐up is necessary to evaluate the occurrence of relapses and whether they are related to each treatment in addition to an evaluation of the efficiency of the treatments. Stamuli et al. 30 in 2012 and Thomas et al. 31 in 2006 analyzed the cost‐effectiveness of cryotherapy and salicylic acid and concluded that cryotherapy is more expensive and less effective than self‐treatment with 50% salicylic acid. Finally, we believe that more clinical trials, such as the one by Albalat et al. 11 comparing the different forms of cryotherapy application and the one by Leow et al. 27 comparing application times and cycles on plantar skin would be of interest for clinicians in daily clinical practice.
In conclusion, evidence of the superiority of antivirals and chemotherapy over cryotherapy in the treatment of plantar warts. However, no evidence supports the superiority or inferiority of cryotherapy compared to other treatments.
This review with meta‐analysis should stimulate high quality clinical trials comparing cryotherapy with more aggressive treatments for compassionate use, such as intralesional bleomycin or the CPS formulation, which appear to have higher cure rates in addition to research into the different modalities and timing of cryotherapy.
CONFLICT OF INTEREST
This review was written independently. The authors did not receive financial or professional help with the preparation of the manuscript.
AUTHOR CONTRIBUTIONS
Sara García‐Oreja, Francisco Javier Álvaro‐Afonso, and José Luis Lázaro‐Martínez had full access to all data in the study and were responsible for their integrity. Mateo López‐Moral and Aroa Tardáguila‐García provided the study concept and design. Sara García‐Oreja and Marta García‐Madrid obtained the data. Sara García‐Oreja and Francisco Javier Álvaro‐Afonso statistically analyzed the data. All authors analyzed and interpreted the data, drafted the manuscript, and critically revised the manuscript.
García‐Oreja S, Álvaro‐Afonso FJ, Tardáguila‐García A, López‐Moral M, García‐Madrid M, Lázaro‐Martínez JL. Efficacy of cryotherapy for plantar warts: A systematic review and meta‐analysis. Dermatologic Therapy. 2022;35(6):e15480. doi: 10.1111/dth.15480
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Hashmi F, Bristow I. Treating plantar warts: utilising natural immunity to induce wart regression. Dermatol Nurs. 2014;13(1):42‐46. [Google Scholar]
- 2. Witchey D, Witchey N, Roth‐kauffman M, Kauffman M. Plantar warts: epidemiology, pathophysiology, and clinical management. J Am Osteopath Assoc. 2018;118(2):92‐105. [DOI] [PubMed] [Google Scholar]
- 3. Viennet C, Gheit T, Muret P, et al. Assessment of the efficacy of a new formulation for plantar wart mummification: new experimental design and human papillomavirus identification. Clin Exp Dermatol. 2013;38(1):85‐88. doi: 10.1111/ced.12025 [DOI] [PubMed] [Google Scholar]
- 4. García‐Oreja S, Álvaro‐Afonso FJ, García‐Álvarez Y, García‐Morales E, Sanz‐Corbalán I, Lázaro Martínez JL. Topical treatment for plantar warts: a systematic review. Dermatol Ther. 2021;34:e14621. [DOI] [PubMed] [Google Scholar]
- 5. Aldana‐Caballero A, Marcos‐Tejedor F, Mayordomo R. Diagnostic techniques in HPV infections and the need to implement them in plantar lesions: a systematic review. Exp Rev Mol Diagn. 2021;21(12):1341‐1348. [DOI] [PubMed] [Google Scholar]
- 6. Cockayne S, Curran M, Denby G, et al. EVerT: cryotherapy versus salicylic acid for the treatment of verrucae ‐ A randomised controlled trial. Health Technol Assess. 2011;15(32):1‐170. [DOI] [PubMed] [Google Scholar]
- 7. Gibbs S, Harvey I. Topical treatments for cutaneous warts (review). Cochrane Database Syst Rev. 2006;(3). doi: 10.1002/14651858.CD001781.pub2 [DOI] [PubMed] [Google Scholar]
- 8. Abdel‐Latif AA, El‐Sherbiny AF, Omar AH. Silver duct tape occlusion in treatment of plantar warts in adults: is it effective? Dermatol Ther. 2020;33:1‐6. [DOI] [PubMed] [Google Scholar]
- 9. Karrabi M, Kheirkhah M, Shahrestanaki E, Thomas S, Sahebkar M. Comparison of 40% trichloroacetic acid and cryotherapy for the treatment of plantar warts: a single‐blind, randomized clinical trial. Dermatol Ther. 2020;33(4):e13559. [DOI] [PubMed] [Google Scholar]
- 10. Walczuk I, Eertmans F, Rossel B, et al. Efficacy and safety of three cryotherapy devices for wart treatment: a randomized, controlled, investigator‐blinded, comparative study. Dermatol Ther. 2018;8(2):203‐216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Albalat W, Attwa E, Ebrahim HM. Intralesional cryotherapy versus cryotherapy spray for the treatment of recalcitrant plantar warts: a prospective, randomized study. J Dermatolog Treat. 2020;26:1‐7. [DOI] [PubMed] [Google Scholar]
- 12. Hekmatjah J, Farshchian M, Grant‐Kels JM, Mehregan D. The status of treatment for plantar warts in 2021: no definitive advancements in decades for a common dermatology disease. Clin Dermatol. 2021;39:688‐694. [DOI] [PubMed] [Google Scholar]
- 13. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group . Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. CEBM. Centre for Evidence Based Medicine: Levels of Evidence (March 2009) [Internet]. CEBM: The centre for evidence‐based medicine develops, promotes and disseminates better evidence for healthcare. 2021 [Cited July 2021]. https://www. cebm.net/2009/06/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/
- 15. Cochrane Handbook ‐ Your Guide To Health [Internet] [Cited 2021 Aug 25]. https://www.cochrane-handbook.org/
- 16. Download and installation RevMan 5|Cochrane Training [Internet] [Cited 2021 Aug 25]. https://training.cochrane.org/online-learning/core-software-cochrane-reviews/revman/revman-5-download/download-and-installation
- 17. JPT H, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Stat Med. 2002;21(11):1539‐1558. doi: 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 18. Cengiz FP, Emiroglu N, Su O, Onsun N. Effectiveness and safety profile of 40% trichloroacetic acid and cryotherapy for plantar warts. J Dermatol. 2016;43(9):1059‐1061. [DOI] [PubMed] [Google Scholar]
- 19. Hemmatian Boroujeni N, Handjani F. Cryotherapy versus CO2 laser in the treatment of plantar warts: a randomized controlled trial. Dermatol Pract Concept. 2018;8(3):168‐173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. El‐Tonsy MH, Anbar TED, El‐Domyati M, Barakat M. Density of viral particles in pre and post Nd:YAG laser hyperthermia therapy and cryotherapy in plantar warts. Int J Dermatol. 1999;38(5):393‐398. [DOI] [PubMed] [Google Scholar]
- 21. Muhammad J, Akhtar N, Ahmad MK, Anwar MI. Comparison of efficacy between intralesional bleomycin and cryotherapy in plantar warts. J Pakistan Assoc Dermatol. 2019;29(1):35‐39. [Google Scholar]
- 22. Ahmad HM, Abdel‐Azim ES, Abdel‐Aziz RT. Clinical, histopathologic, and viral load study after treatment of plantar warts with 10% formaldehyde soaks versus liquid nitrogen cryotherapy. J Egypt Women's Dermatol Soc. 2018;15(3):165‐171. [Google Scholar]
- 23. Gupta S. Topical adapalene in the treatment of plantar warts; randomized comparative open trial in comparison with cryo‐therapy. Indian J Dermatol. 2015;60(1):102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kaçar N, Taşli L, Korkmaz S, Ergin Ş, Erdoǧan BŞ. Cantharidin‐podophylotoxin‐salicylic acid versus cryotherapy in the treatment of plantar warts: a randomized prospective study. J Eur Acad Dermatol Venereol. 2012;26(7):889‐893. [DOI] [PubMed] [Google Scholar]
- 25. Kaur Arora A, Dogra A, Kumar Gupta S. Efficacy of cryotherapy versus radiofrequency ablation in the treatment of plantar warts. Iran J Dermatol. 2014;17(3):85‐90. [Google Scholar]
- 26. Gibson JR, Harvey SG, Barth J, Darley CR, Reshad H, Burke CA. A comparison of acyclovir cream versus placebo cream versus liquid nitrogen in the treatment of viral plantar warts. Dermatologica. 1984;168:178‐181. [DOI] [PubMed] [Google Scholar]
- 27. Leow MQH, Tan EST. Efficacy of two different liquid nitrogen cryotherapy regimes in the treatment of plantar viral warts: A prospective comparative study. J Dermatol Nurses Assoc. 2017;9(4):E1‐E5. [Google Scholar]
- 28. Kwok CS, Holland R, Gibbs S. Efficacy of topical treatments for cutaneous warts: a meta‐analysis and pooled analysis of randomized controlled trials. Br J Dermatol. 2011;165(2):233‐246. [DOI] [PubMed] [Google Scholar]
- 29. Bertolotti A, Dupin N, Bouscarat F, Milpied B, Derancourt C. Cryotherapy to treat anogenital warts in nonimmunocompromised adults: systematic review and meta‐analysis. J Am Acad Dermatol. 2017;77(3):518‐526. [DOI] [PubMed] [Google Scholar]
- 30. Stamuli E, Cockayne S, Hewitt C, et al. Cost‐effectiveness of cryotherapy versus salicylic acid for the treatment of plantar warts: economic evaluation alongside a randomised controlled trial (EVerT trial). J Foot Ankle Res. 2012;5(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Thomas KS, Keogh‐Brown MR, Chalmers JR, et al. Effectiveness and cost‐effectiveness of salicylic acid and cryotherapy for cutaneous warts. An economic decision model. Health Technol Assess. 2006;10(25):9–87. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


