Abstract
At all levels of socioeconomic status, Black Americans can expect to live shorter and sicker lives than their White counterparts. This study advances the perspective that anti-Black stigma from Whites precludes Blacks from reaping the full health rewards of higher status, particularly within the context of neighborhoods. To test this hypothesis, I merge census data with rich survey and biomarker data from the Nashville Stress and Health Study, a representative sample of Black and White adults from Davidson County, Tennessee (n = 1,252). Initially, I find that Blacks who reside in higher-status and mostly White communities exhibit lower levels of neuroendocrine stress hormones, relative to their peers living in disadvantaged Black neighborhoods. But Blacks in higher-status areas also report more perceived discrimination. In turn, perceived discrimination is associated with chronic bodily pain, as well as elevated stress hormones and blood pressure tied to high goal-striving stress, or fears of being blocked from reaching life goals. After accounting for racism-related stressors, Blacks exhibit comparable levels of physiological distress regardless of neighborhood context. The inverse is true for Whites, who report fewer stressors in higher-status neighborhoods, and less physiological distress than Blacks overall. Findings are discussed within the context of social evolutionary theories of the human brain and are dovetailed with broader racial health disparities in the United States.
Keywords: diminished returns, goal-striving stress, neighborhoods, health disparities, racism, social pain, vigilance
INTRODUCTION
“Many well-educated, affluent blacks have already found their way out of inner-city ghettos, yet they have not escaped America’s myriad racial demons. Consequently, they remain either estranged or in a state of emotional turmoil.”
– Ellis Cose, The Rage of a Privileged Class
Black Americans live shorter and sicker lives than White Americans. Over the past century, Blacks have suffered between 60,000 to 100,000 premature deaths each year relative to Whites, numbers that equate to a jumbo jet airliner filled with Blacks “crashing without survivors every day, day in and day out, year after year” (Hummer and Hamilton 2019:127). The majority of these early deaths stem from chronic conditions such as heart and kidney disease, stroke, cancer, diabetes, and sepsis (Hummer and Hamilton 2019:133-137). Thus, Black Americans can also expect to live more years than Whites with debilitating illnesses (Crimmins and Seeman 2004).
Accounting for the mechanisms that underlie Black-White health disparities has been an ongoing challenge for researchers. Two major lines of reasoning have prevailed in the literature so far. One hypothesis contends that racial differences in socioeconomic status (SES) could be responsible. Accordingly, Black Americans are often hindered from achieving higher SES and moving into high-status neighborhoods, both of which are considered fundamental social causes of good health. But other scholars have found that Black-White health gaps commonly persist even after accounting for racial differences in SES. These residual gaps are thought to reflect the unique and adverse health effects of racism. Over the past several decades, numerous studies have found varying degrees of support for low SES and racism as mechanisms of poor health among Black Americans (Phelan and Link 2015; Smith 2021; Williams and Collins 2001).
Related research has also discovered that Blacks tend to derive fewer health benefits from higher SES attainment than their White peers (Colen et al. 2006; Colen, Krueger, and Boettner 2018; Farmer and Ferraro 2005; Gaydosh et al. 2018). Moreover, studies consistently find that upwardly mobile Blacks tend to report greater exposure to racism-related stressors from Whites, relative to their less mobile Black peers (Anderson 2015; Assari and Moghani Lankarani 2018; Cole and Omari 2003; Feagin and Sikes 1994; Halanych et al. 2011; Jackson, Thoits, and Taylor 1995; Smith, Allen, and Danley 2007; Smith, Hung, and Franklin 2011). One recent study even suggests that racism-related distress could explain the diminished health returns of higher SES attainment for Black Americans (Colen et al. 2018).
Limitations in theory and measurement have nonetheless precluded population scientists from gaining a clear picture of how racism conditions the health returns of higher status. For the most part, the health consequences of racial discrimination have remained hidden from sociologists within a black box of unsubstantiated stress processes (Goosby, Cheadle, and Mitchell 2018; Harris and Schorpp 2018). Our limited knowledge has largely been due to a lack of granular measures of stress and distress. Indeed, it has taken nearly half a century to design and validate survey instruments that can accurately account for racial disparities in stress exposures (Turner 2013). Likewise, population researchers have only now gained widespread access to biological data that are sensitive enough to detect subclinical effects of chronic stress exposure (Harris and Schorpp 2018; Massey 2015; Turner 2013). Generally, researchers in this area have paid scant attention to the implications of such measurement errors (e.g., Perreira et al. 2005).
The present study aims to address these limitations and advance our understanding of Black-White health disparities in the United States. I merge census data with rich survey and biomarker data from the Nashville Stress and Health Study (NSAHS), a representative sample of Black and White working-age adults from Davidson County, Tennessee. The NSAHS was led by R. Jay Turner, a leading scholar in the sociology of stress, and reflects forty years of accumulated knowledge in the stress process literature (Pearlin et al. 1981; Turner 2013; Turner, Brown, and Hale 2017). Each participant completed a three-hour survey interview, extensive biomarker panel, and was assigned a census block group identifier. With these data, I can test whether exposures to racism-related stressors vary across neighborhood contexts for Black people, and whether such exposures condition the associations between neighborhood status and individual psychophysiology. I can also confirm that I do not find similar patterns among White people.
The fundamental question motivating my study, then, is whether increased exposure to racism-related stressors negates the health benefits of living in high-status neighborhoods for Black Americans. Involuntary residential segregation has long been considered a social determinant of poor health among Black populations (Du Bois 1899; Williams and Collins 2001). Due to legacies of racist zoning policies, segregated Black neighborhoods still tend to be characterized by higher rates of pollution, social disorder, and police surveillance, all of which pose serious health risks for residents (Massey 2004; Rothstein 2017). However, with few exceptions (e.g., Bécares et al. 2012), researchers have overlooked the unique stressors Black residents face in affluent communities.
As I discuss in more detail below, recent advances in neuroscience and biomarker research provide key insights into this question. The field of social neuroscience has demonstrated that experiences of social ostracism—of being viewed and treated as the “black sheep” of a community—can have profound and toxic effects on individual psychophysiology (Eisenberger 2015; MacDonald, Kingsbury, and Shaw 2005). It is also becoming increasingly evident that the numerous health conditions known to plague Black Americans are rooted in similar stress processes tied to the brain and nervous system (Barrett 2017). Thus, although the biomarker outcomes examined in this study do not reflect clinical health measures, per se, they allow me “to peer back earlier into life before illness manifests, and to quantify the tolls exacted by [racist] socioenvironmental conditions” (Goosby et al. 2018:321).
In what follows, I first explain how the brain and body will react to discriminatory episodes. Next, I explain how neighborhood contexts can structure exposures to racism-related stressors for Black residents. I then present my conceptual model, data, analytic strategies, and results. My analyses reveal that racism-related stressors negate much of the health benefits of residing in affluent communities for Black Americans. While Blacks in high-status neighborhoods initially exhibit lower levels of physiological distress, they also report more interpersonal discrimination and anticipatory stress, which predicts increased physiological distress. After accounting for racism-related stressors, Black residents exhibit comparable levels of physiological distress regardless of neighborhood context. I close by discussing how these findings expand our understanding of Black-White health disparities in the United States, and outline avenues for future research.
BACKGROUND
The Psychophysiology of Interpersonal Discrimination
Discrimination experiences are initially encoded in the brain (Goosby et al. 2018) To understand how discrimination impacts the body, it is therefore appropriate to first review the evolutionary functions of the human brain. Our brains are the primary mediators between environmental stimuli and our internal milieu. The job of the brain is to orchestrate the body’s response to environmental demands in real time, and to encode information into long-term memory so we can better anticipate and adapt to similar demands in the future. In short, our brains have evolved to maximize our chances for survival and reproduction through predictive regulation of the body (Sterling 2012).
But we are also social primates, and thus our brains have evolved to remain in concert with other brains. Throughout our evolutionary past, people who could establish reliable connections with a group, effectively anticipating the needs and desires of others, maximized their chances for survival and reproduction, thereby creating selection pressures for humans to develop increasing empathy over time (Massey 2001). Because evolution tends to be conservative, and because ostracism from a group was equivalent to a death sentence in prehistoric times, many of the same neural mechanisms that evolved to encode immediate threats to survival also encode experiences with social rejection (Eisenberger 2015; MacDonald et al. 2005).
The social evolution of the human brain has serious implications for how the body will react to interpersonal discrimination. Such encounters represent to the brain a dire threat to survival requiring an immediate response. Perceptions of social rejection encoded in the brain quickly trigger cascading stress responses that radiate out from the central and peripheral nervous systems, and into the immune, endocrine, and cardiovascular systems, ultimately preparing the body to mount a defense (Cheadle et al. 2020; Goosby et al. 2018). In experimental studies, for example, participants who are subjected to social evaluative threats tend to exhibit increased activity in brain regions that encode perceptions of fear and pain, as well as increased levels of adrenaline, cortisol, pro-inflammatory cytokines, and blood pressure (Eisenberger 2015).
Over the long term, recurring experiences with interpersonal discrimination condition the brain to expect similar confrontations into the future. The training of the brain in this manner can then induce a perpetual state of hypervigilance. For example, studies by Hicken and colleagues find that many Black Americans carry with them constant fears of being mistreated or subjected to anti-Black stigma, a chronic psychological state associated with poor sleep outcomes, higher blood pressure, and increased body weight (Hicken et al. 2013, 2014; Hicken, Lee, and Hing 2018). Studies by Smith and colleagues have also found that racism-related vigilance is particularly high among Black people navigating predominantly White institutions, such as historically White college campuses (Smith et al. 2007, 2011).
Another critical though less studied form of racism-related vigilance is goal-striving stress. People with high goal-striving stress perceive a large gap between their current and ideal statuses, strongly desire to bridge this gap, but perceive a low likelihood of future success (DeAngelis 2020; Sellers and Neighbors 2008). The scale used to measure goal-striving stress was developed by sociologists during the Civil Rights movement. The theory behind this scale was that continued exposure to racial discrimination, despite the passing of the Civil Rights Act, would trigger deep feelings of ostracism and despair for Black Americans striving for upward mobility during this pivotal turning point in United States history (Parker and Kleiner 1966).
Contemporary studies find that fears of blocked strivings remain pervasive in the lives of Black Americans, who still tend to report significantly higher goal-striving stress than their White peers (DeAngelis 2020). High goal-striving stress, in turn, predicts low-quality sleep, higher blood pressure, poor kidney functioning, and elevated neuroendocrine hormones for Black people (Cain et al. 2019; Cain-Shields et al. 2020; DeAngelis 2020). Parallel research also suggests that exposure to interpersonal racism can elicit higher goal-striving stress. For instance, Hochschild (1995:102) reviewed decades of research and found that upwardly mobile Black Americans continue to report regular racist encounters, which predict wider achievement-aspiration gaps. A more recent study found that Black people who report greater exposures to interpersonal racism also tend to exhibit increased hopelessness, or a “cognitive state characterized by negative expectations toward the future and the belief that one cannot achieve sought after goals” (Mitchell et al. 2020:2).
Interpersonal discrimination, in sum, can impact the brain and body in two main ways. First, racist encounters can elicit immediate social pain responses. Second, recurring exposures to discrimination can condition the brain to anticipate similar encounters in the future. The need to constantly anticipate future racist encounters could then perpetuate a vigilant state of high goal-striving stress and hyperactivity of physiological stress responses. In the next section, I consider how neighborhood environments structure exposures to discrimination for Black residents.
Neighborhood Context and Racism-Related Stressors
A key tenet of the sociological study of stress is that distributions of social stressors, including interpersonal discrimination, are stratified across social groups and contexts (Pearlin 1989; Pearlin et al. 1981). This same logic is applicable to neighborhood contexts. Neighborhoods in the United States have operated historically as racially stratified, meso-level organizations wherein social and environmental stressors have been disproportionately concentrated among urban Black communities (Massey and Denton 1993; Ray 2019; Rothstein 2017). This could explain why the vast majority of research exploring the effects of neighborhood environments on the health of Black Americans has focused exclusively on stressors unique to segregated Black neighborhoods (Phelan and Link 2015; Williams and Collins 2001).
Studies of urban Black communities find that racist lending and zoning policies have had long-term, adverse impacts on the physical and social infrastructures of these areas. Continuing legacies of systemic disinvestment in Black neighborhoods have created unstable social contexts characterized by fast residential turnover, high rates of violent crime, and intense police surveillance (Massey 2001; Massey 2004; McFarland et al. 2018). Through similar redlining initiatives, polluting industries have also been given free rein to target Black communities as primary sites for the disposal of industrial waste discharges (Rothstein 2017). Studies find that residents of segregated Black neighborhoods tend to exhibit elevated levels of psychophysiological distress, presumably from having to adapt to such toxic environments on a regular basis (e.g., Barber et al. 2016; Hill, Ross, and Angel 2005; Massey 2004; Mayne et al. 2019).
Researchers in this area have paid less attention, however, to area-level risks of racist encounters. To be sure, a few studies have found that marginalized racial groups sometimes exhibit better health outcomes when they live in communities with a greater concentration of residents belonging to their own racial-ethnic group (Bécares et al. 2012; Pickett and Wilkinson 2008). Feelings of diminished stigma and increased social cohesion are thought to explain these patterns. Nonetheless, we still lack a clear picture of how differential exposures to interpersonal racism are contributing to place-based health disparities between Black and White Americans.
Several parallel literatures support the hypothesis that Black residents of affluent areas will be subjected to more discrimination from White neighbors. The same historical processes that led to segregated Black neighborhoods have also created areas of concentrated White affluence. Indeed, neighborhood redlining was enacted during the Roosevelt administration to assist White families not only in recovering from the Great Depression, but in more fundamentally achieving racial seclusion and hegemony (Massey and Denton 1993; Rothstein 2017). As a result of these and other historical initiatives, allocations of property and wealth have been inextricably linked to Whiteness (Harris 1993), and the majority of high-status neighborhoods still remain populated mostly by White residents (Goetz, Damiano, and Hicks 2019; Massey 1996).
Public opinion polling has revealed that Whites still express preferences for living in mostly White areas and tend to view the presence of Black neighbors as a threat to their safety and status (Bobo and Zubrinsky 1996; Lewis, Emerson, and Klineberg 2011; Yancey 2003). Population studies have found similar patterns. For example, an increasing percentage of Black residents in a given area predicts greater fears of victimization and perceptions of social disorder among White residents (Chiricos, McEntire, and Gertz 2001; Schieman 2009).
Black residents of high-status communities are likely to be viewed by White neighbors with concern and skepticism, then, if not outright disdain. Among a sample of Black women, Hunt and colleagues uncovered a positive association between the percentage of White neighbors and self-reports of interpersonal racism (Hunt et al. 2007). In their interviews with over 200 upwardly mobile Black Americans, Feagin and Sikes (1994) revealed that participants had regular run-ins with White neighbors and police officers, who were convinced the participants did not belong in their own neighborhoods. Anderson (2015:14) has also noted that affluent communities commonly form neighborhood watch groups to monitor for “suspicious-looking” people, a term that White residents tacitly assume to mean Black people. Such widespread suspicion of Black people in high-status areas often motivates Black residents to limit the amount of time they spend outside of their own homes, lest they be caught “jogging while Black,” for example (Beauchamp 2020; Ray 2017).
Conceptual Model
The weight of evidence indicates that Black residents of higher-status neighborhoods will be exposed to more racist encounters with White neighbors. In turn, chronic exposure to interpersonal discrimination could predict elevated physiological distress directly, or indirectly via increased goal-striving stress. Recall that discrimination can spark immediate physiological pain responses, and also condition the brain to remain vigilant to racist encounters into the future. Although adaptive in the short term, dogged goal-striving in the face of anticipated racist barriers could lead to hyperactive physiological stress responses (DeAngelis 2020). Residents of segregated Black neighborhoods should also exhibit elevated stress responses, albeit for reasons other than interpersonal racism, such as increased exposures to crime, police surveillance, or pollution.
These empirical expectations are visually depicted below in Figure 1. First, I hypothesize a direct inverse association between neighborhood status and physiological stress response. Second, I expect to find a direct positive association between higher neighborhood status and discrimination. Exposure to interpersonal discrimination should then predict elevated physiological stress directly, or indirectly via goal-striving stress. Third, I expect that the direct inverse association between neighborhood status and stress response will be attenuated by the indirect positive associations via discrimination and goal-striving stress. Thus, Figure 1 represents a suppression or inconsistent mediation model, with discrimination and goal-striving stress operating as countervailing mechanisms (MacKinnon, Krull, and Lockwood 2000; Wheaton 1985).
Figure 1.
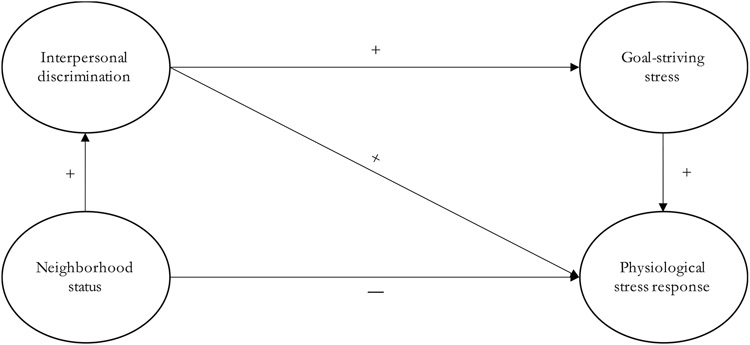
Conceptual model.
The Historical Contexts of Nashville
Several historical features of Nashville make it an appropriate location for testing this model. Nashville was a cradle of Black intellectual life and political causes following emancipation and into the Civil Rights era (Briggs 2015). For example, Nashville houses many of the country’s earliest and most prominent Black universities, including Walden, Fisk, and Meharry Medical College. As early as 1960, James Lawson and the Nashville Student Movement also helped to spearhead nonviolent protests of Jim Crow segregation laws throughout the South (Halberstam 1998).
As a result, the contemporary Black population of Nashville is now economically diverse and integrated with Whites more so than in many other metropolitan areas across the United States (Turner et al. 2017). As of the 2010 census, for instance, the Nashville-Davidson metropolitan area had a Black-White dissimilarity score of 56 (Frey 2011). This number reflects the percentage of Black residents who would need to move to other census tracts before the Black and White populations of Nashville would be evenly distributed. To put this score into national perspective, the average dissimilarity score for the 102 largest metropolitan areas was 55, with a high score of 82 (Milwaukee) and a low score of 22 (Provo).
White residents of Nashville have also been noted for espousing a distinctly Southern, pseudo-aristocratic racial etiquette that would seem to invite the types of racist encounters mentioned before. In his book, The Nashville Way: Racial Etiquette and the Struggle for Social Justice in a Southern City, Benjamin Houston shows that Whites in Nashville have historically emphasized “moderation” in race relations, or an “upper-class emphasis on manners, decorum, and a hypersensitive avoidance of civic unrest.” This type of racialized ideology, according to Houston, has led White Nashville residents to adopt a “sympathy for Black advancement undergirded by deeply felt assumptions of Black inferiority and White superiority” (Houston 2012:13).
Legacies of Black intellectualism and desegregation efforts in Nashville have allowed Blacks to integrate into affluent areas more so than in many other cities. At the same time, Nashville appears to be replete with Southern White moderates who view Blacks with paternalistic anxiety. This distinct blend of sociohistorical currents is important to consider for analytic purposes, as Black Nashville residents will likely experience a wide range of neighborhood environments and exposures to interpersonal racism (Turner et al. 2017).
METHODS
Data
Data come from Vanderbilt University’s Nashville Stress and Health Study (NSAHS), a cross-sectional probability survey of non-Hispanic Black and White working-age adults who lived in Davidson County, Tennessee between 2011 and 2014 (n = 1,252). The NSAHS sample was collected using multistage, stratified cluster sampling techniques, with census block groups as the primary sampling unit (n = 194). The total sample was stratified by race and gender to ensure equal representations of Black and White women and men. Fifty-nine percent of contacted persons ultimately agreed to participate in the study. All analyses are weighted for the probability of selection during the household screening phase, and for nonresponse during the interviewing phase. Poststratification weights are incorporated into the final design weight to permit generalizability to Davidson County’s population of Black and White adults.
The average survey interview lasted around three hours. Interviews were computer-assisted and conducted in the respondent’s home or on the Vanderbilt campus. Interviewers were professionally trained and matched to respondents based on race. Interviewers also provided respondents with instructions and materials for biomarker collection, including directions to fast before collection. The morning following the survey interview, clinicians visited respondents’ homes to collect fasting 12-hour urine samples, intravenous blood samples, blood pressure measurements, and anthropometric measures of height, weight, and hip and waist circumferences. Respondents received $50 each for participating in the survey and biomarker phases of the interview. Less than 2% of respondents refused to provide biomarker data (for more information on NSAHS data collection, see Turner et al. 2017).
Measurement
Analyses include a combination of observed and latent variables. Latent variables refer to abstract constructs that are inferred from other observed or indicator variables, rather than being directly observed in the data (Bollen 1989). Indicator variables can be conceptualized as effects or causes of latent variables (Bollen and Bauldry 2011). All indicator variables in this study are assumed to be effects of latent causes. Researchers typically make this same assumption, albeit implicitly, whenever they construct multi-item scales. The only difference in the current case is that the relationships between latent and indicator variables are explicitly modeled, and the error terms associated with indicator variables are purged from the latent variable estimates.
Physiological Stress Response.
I gauge physiological stress response with four latent variables comprised of biomarker and self-report indicators. I settled on a four-factor solution because this provided a far superior fit to the data compared to a one-factor solution (see the online supplement). NSAHS biomarkers originate from the MacArthur Studies of Successful Aging (Turner et al. 2017). These included measures of neuroendocrine stress hormones and cardiometabolic biomarkers. However, NSAHS researchers did not collect biomarkers of inflammation. To measure pro-inflammatory stress response, I rely on self-reports of bodily pain, one of the most common symptoms of chronic inflammation (Barrett 2017:199-209).
The first latent factor is neuroendocrine stress response, reflected by 12-hour urine levels of epinephrine, norepinephrine, and cortisol. Respondents who score higher on this latent variable are assumed to be under chronic neurological stress burdens, which cause them to secrete higher concentrations of neuroendocrine hormones in their urine throughout their waking hours. Epinephrine and norepinephrine are measured in micrograms per milliliter of urine (μg/mL). Cortisol is measured in micrograms per liter of urine (μg/L). I took the natural log of each biomarker to adjust for extreme skewness and kurtosis (see the online supplement).
Pro-inflammatory stress response is gauged with a second latent factor of self-reported bodily pain. Respondents were asked four questions about their bodily pain during the survey interview. The first item asked, “On average, how bad has your bodily pain been during the past 4 weeks?” The second item asked, “How often during the past 4 weeks have you had pain or discomfort?” The third item asked, “During the past 4 weeks, how many days did pain interfere with the things you usually do?” The fourth and final item asked, “How much bodily pain do you feel right now?” These questions originate from the 36-item Short-Form Health Survey (SF-36). Following the SF-36 coding guidelines, all responses are ordinal and coded such that 0 = total absence of pain and 100 = maximum pain (see Ware and Sherbourne 1992). To facilitate model convergence, however, final scores are divided by 100 with a resulting range of 0 to 1.
I also gauge cardiovascular stress response with two latent variables of systolic and diastolic blood pressure. Blood pressure was recorded as three separate readings spaced two minutes apart. All readings were recorded in millimeters of mercury (mmHg). Blood pressure readings are also divided by 100 to allow for model convergence.
Neighborhood Status.
Neighborhood status is reflected by four continuous measures of block group-level (1) proportion of White residents, (2) proportion of residents with at least a bachelor’s degree, (3) median household income in dollars, and (4) proportion of residents living above the poverty line. These measures were taken from American Community Survey five-year estimates that overlapped with the NSAHS study period (2010–2014). To facilitate model convergence, I rescaled median household income by dividing all values by the maximum income. This allowed for all block group indicators to have a consistent range of 0 to 1.
Neighborhood status is assumed to lie on a latent scale of extremes, with concentrated privilege and disadvantage on the high and low ends, respectively (e.g., Massey 2001b).1 Higher values on the latent variable capture simultaneous increases in the proportion of residents who are White, college educated, earning higher incomes, and living above the poverty line. Conversely, lower values capture increases in the proportion of residents who are Black, less than college educated, earning lower incomes, and living below the poverty line. To reiterate, these indicators are assumed to be the effects of an underlying latent cause. The latent variable is conceptualized this way to emphasize the historical agency of White-dominated institutions, which have actively conspired to create racially stratified areas of affluence and poverty across the United States. I refer to this latent variable as “concentrated privilege” moving forward, to reflect the fact that higher values are associated with a greater concentration of privileged residents.
Perceived Discrimination.
Exposure to interpersonal racism is gauged with the following five indicators of perceived discrimination: (1) “You are treated with less respect than you deserve,” (2) “You are treated with less courtesy than other people,” (3) “People act as if they think you are not smart,” (4) “People act as if they think you are dishonest,” and (5) “People act as if they are better than you are.” Response choices range from 1 = never to 5 = almost always. These items are chosen for their face validity as indicators of aversive forms of interpersonal discrimination. According to literature on aversive racism, high-status Whites will tend to denounce overt expressions of racism yet still harbor implicit biases that lead them to stereotype Black people (Dovidio and Gaertner 2004). Higher scores on this latent variable capture respondents who perceive more chronic exposure to aversive types of interpersonal discrimination.
Goal-Striving Stress.
Goal-striving stress is reflected by three indicators. Respondents were first shown an image of a ladder with rungs numbered from zero to nine. They were then told that “the steps on the ladder stand for the ten possible steps in your life. Level nine stands for the best possible way of life for you, and the first step stands for the worst possible way of life for you.” Respondents were then asked to report the rung they felt they currently occupied, the rung they aspired to reach in a few years, and their attitudes toward their aspired rung.
The first indicator is the respondent’s subjective distance from aspirations, calculated by subtracting the respondent’s achieved rung from their aspired rung (0 = no distance, 9 = maximum distance). Respondents who reported no achievement-aspiration gap were not asked any follow-up questions and were given a score of zero for all indicators (11% of the sample). The second indicator is the respondent’s subjective likelihood of reaching aspirations (0 = no distance, 4 = highly unlikely). The third indicator is the respondent’s emotional attachment to aspirations (0 = no distance, 4 = unmet aspirations would be very disappointing). Higher scores on this latent variable capture respondents who feel further away from their aspirations, more attached to their aspirations, but less optimistic about future attainment.2
Control Variables.
Analyses control for age (in years), gender (1 = female, 0 = male), educational attainment (in years), and household income (ordinal, 0 = none, 15 = $135k or more). Studies find that Black Americans tend to exhibit signs of premature morbidity as they attain higher levels of individual SES and transition into older age, presumably from distress related to overcoming racist barriers to attainment over the life course (Allen et al. 2019; Gaydosh et al. 2018).
Research on stress proliferation processes also suggests that experiences with neighborhood disorder, racial discrimination, or goal-striving stress could cluster with other role-related stressors (e.g., Turney 2014). To account for stress clustering, models include added controls for job strain (stably employed = reference, non-employed, precariously employed), and relationship strain (stable relationship = reference, single, precarious relationship). To measure precarious jobs, employed respondents were asked, “Thinking about the next 12 months, how likely do you think it is that you will lose your job or be laid off?” Precarious relationships were measured by asking respondents, “Realistically, how likely do you think it is that you and your spouse/partner will spend the rest of your lives together?” Respondents who answered very/somewhat likely to the first question, and not very/not at all likely to the second question, were assigned precarious statuses.3
Structural Equation Model
Figure 2 depicts the full structural equation model with latent variables. Latent variables are enclosed within circles, indicator variables are enclosed within squares, and error terms are unenclosed (Bollen 1989:32). The full model consists of separate measurement and path components. The measurement model refers to the relationships between latent variables and their respective indicators. Arrows run from the latent variables to their indicators, signaling effect indicators. The path model refers to the relationships among latent variables. Controls are treated as exogenous observed variables in the path model, which are allowed to correlate with concentrated privilege and to predict the other endogenous latent variables (not depicted).
Figure 2.
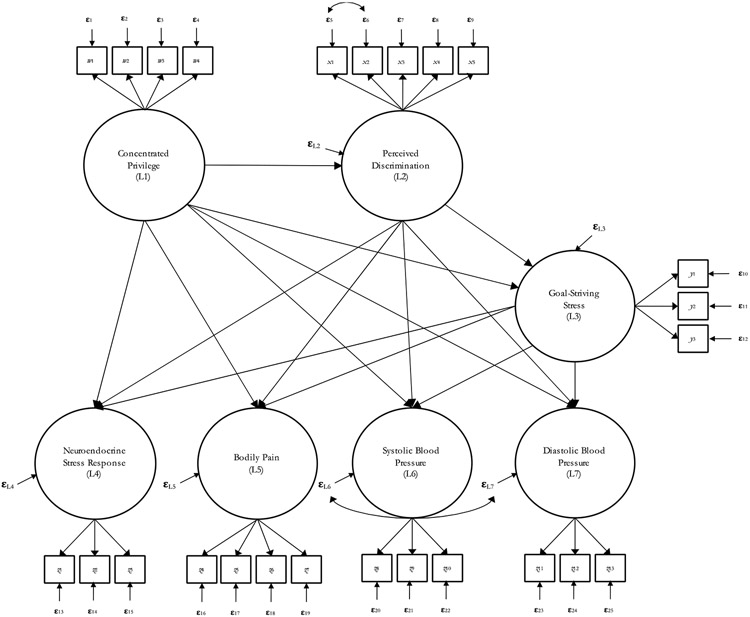
Structural equation model with latent variables.
All endogenous variables have unique error terms. I allow the errors for systolic and diastolic blood pressure to correlate. I also correlate the errors for the first two perceived discrimination indicators. These correlations represent measurement artifacts. Systolic and diastolic blood pressure were measured simultaneously and with the same instrument. The first two discrimination indicators also gauged similar experiences and were asked in succession during the survey interview. Recall that x1 asks respondents how often they are treated with “less respect than they deserve,” while x2 asks how often they are treated with “less courtesy than other people.”
The full model is tested in Mplus version 7. Main analyses are limited to Black respondents. Findings for White respondents are presented in the online supplement and briefly discussed in this manuscript. Results for the measurement model are also presented in the online supplement, along with global model fit indices. Estimates are derived using full information maximum likelihood (FIML) procedures, with probability weights and robust standard errors clustered by block group. FIML is chosen because it is superior to listwise deletion and multiple imputation for recovering missing observations in structural equation models (Enders and Bandalos 2001). Findings generated with FIML are comparable to the results after listwise deletion (see the online supplement). There is at least one missing observation for 19 out of 33 observed variables. Proportions of missing data vary from 32% for block group-level indicators, to less than 1% for indicators of discrimination and goal-striving stress (see Table 1).
Table 1.
Weighted descriptive statistics of observed variables: NSAHS, Black subsample.
| Mean/ Proportion |
S.D. | Skewness | Kurtosis | N | % missing |
|
|---|---|---|---|---|---|---|
| Concentrated Privilege | ||||||
| Proportion of White residents in block group (w1) | .56 | .34 | −.42 | 1.78 | 426 | 32 |
| Proportion of college educated residents in block group (w2) | .20 | .15 | .42 | 1.52 | 426 | 32 |
| Median household income of block group (w3) | 42,391.63 | 18,881.67 | −.14 | 1.68 | 424 | 32 |
| Proportion of residents living above the poverty line (w4) | .93 | .06 | −.73 | 2.09 | 426 | 32 |
| Perceived Discrimination | ||||||
| "You are treated with less respect than you deserve" (x1) | 2.38 | .97 | .36 | 2.79 | 627 | 0 |
| "You are treated with less courtesy than other people" (x2) | 2.39 | .93 | .30 | 2.95 | 626 | <1 |
| "People act as if they think you are not smart" (x3) | 2.41 | 1.01 | .33 | 2.72 | 624 | <1 |
| "People act as if they think you are dishonest" (x4) | 1.76 | .83 | .95 | 3.79 | 625 | <1 |
| "People act as if they are better than you are" (x5) | 2.82 | 1.03 | .17 | 2.91 | 627 | 0 |
| Goal-Striving Stress | ||||||
| Subjective distance from aspirations (y1) | 2.53 | 1.42 | .74 | 4.88 | 625 | <1 |
| Subjective low likelihood of reaching aspirations (y2) | 1.53 | .79 | .49 | 4.04 | 627 | 0 |
| Emotional attachment to aspirations (y3) | 2.35 | 1.24 | −.14 | 1.97 | 626 | <1 |
| Neuroendocrine Stress Response | ||||||
| Logged epinephrine (z1) | −6.18 | .99 | −.35 | 3.19 | 577 | 8 |
| Logged norepinephrine (z2) | −3.77 | .72 | −.17 | 3.05 | 601 | 4 |
| Logged cortisol (z3) | 2.12 | .91 | .01 | 2.62 | 565 | 10 |
| Bodily Pain | ||||||
| "How bad has bodily pain been in past 4 weeks?" (z4) | .33 | .34 | .38 | 1.69 | 627 | 0 |
| "How often have you had pain in past 4 weeks?" (z5) | .33 | .37 | .72 | 2.06 | 627 | 0 |
| "How many days did pain interfere in past 4 weeks?" (z6) | .22 | .28 | 1.62 | 5.02 | 627 | 0 |
| "How much bodily pain do you feel right now?" (z7) | .11 | .24 | 1.97 | 5.59 | 627 | 0 |
| Systolic Blood Pressure | ||||||
| Reading #1 (z9) | 126.11 | 15.16 | .79 | 5.11 | 606 | 3 |
| Reading #2 (z8) | 125.44 | 15.16 | .84 | 5.24 | 603 | 4 |
| Reading #3 (z10) | 125.46 | 15.30 | .94 | 4.89 | 596 | 5 |
| Diastolic Blood Pressure | ||||||
| Reading #1 (z12) | 80.24 | 10.53 | .27 | 3.54 | 606 | 3 |
| Reading #2 (z11) | 80.27 | 9.91 | .13 | 3.44 | 603 | 4 |
| Reading #3 (z13) | 80.49 | 9.66 | .39 | 3.71 | 596 | 5 |
| Control Variables | ||||||
| Age (in years) | 43.57 | 11.43 | .10 | 1.80 | 627 | 0 |
| Female (vs. male) | .55 | 627 | 0 | |||
| Education (in years) | 13.40 | 2.76 | −.37 | 5.65 | 627 | 0 |
| Household income (1 = under $5k, 15 = $135k or more) | 6.72 | 3.63 | .26 | 2.51 | 607 | 3 |
| Job strain | ||||||
| Stable employment (reference) | .59 | 627 | 0 | |||
| Non-employed | .30 | 627 | 0 | |||
| Precarious employment | .11 | 627 | 0 | |||
| Relationship strain | ||||||
| Stable relationship (reference) | .53 | 627 | 0 | |||
| Single | .40 | 627 | 0 | |||
| Precarious relationship | .07 | 627 | 0 |
Note: NSAHS = Nashville Stress and Health Study (2011-2014). N = number of original observations. S.D. = standard deviation.
Note: N = number of original observations. S.D. = standard deviation.
RESULTS
Characteristics of the NSAHS Black Subsample
Table 1 provides weighted descriptive statistics of observed variables. In short, the typical Black respondent resides in a racially mixed or majority (56%) White neighborhood, experiences some racism-related stressors, and exhibits some bodily pain and early signs of cardiovascular disease. For instance, average blood pressure readings are around 125 over 80, indicating prehypertension. Black respondents also tend to have at least one year of education beyond high school, and between $35–$45,000 in annual household income (= 7), which is roughly equivalent to the average Black American family income in 2010 (Semega et al. 2020).
Neighborhood Status and Physiological Stress Response
Is neighborhood status directly associated with physiological stress levels among Black residents? Results in Table 2 suggest this is the case, but only when considering the neuroendocrine system. A one-unit increase in concentrated privilege, which is equivalent to the difference between living in areas of total disadvantage (= 0) versus total privilege (= 1), predicts an expected decrease in neuroendocrine hormones by .369 logged units (b = −.369; p < .01). This gap is comparable to the average difference in hormone levels between respondents who are 8 years apart in educational attainment. This finding provides partial support for my first hypothesis. Black residents in areas of concentrated Black disadvantage exhibit signs of hyperactive neuroendocrine systems, likely from having to navigate precarious social environments on a regular basis.
Table 2.
Coefficients for the path model: NSAHS, Black subsample (n = 627).
| Endogenous Latent Variables |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Perceived discrimination |
Goal-striving stress |
Neuroendocrine stress response |
Bodily pain |
Systolic bloodpressure |
Diastolic blood pressure |
|||||||
| Exogenous Latent Variables | ||||||||||||
| Concentrated privilege | .469 | (.115) *** | .307 | (.188) | −.369 | (.121) ** | .038 | (.056) | −.038 | (.030) | .002 | (.024) |
| Perceived discrimination | – | .422 | (.076) *** | .089 | (.082) | .070 | (.027) ** | −.008 | (.013) | .002 | (.008) | |
| Goal-striving stress | – | – | .094 | (.037) * | .019 | (.015) | .013 | (.008) | .015 | (.005) ** | ||
| Control Variables | ||||||||||||
| Age | −.006 | (.005) | −.005 | (.007) | −.017 | (.008) * | .002 | (.003) | .003 | (.001) *** | .001 | (.000)** |
| Female (vs. male) | .048 | (.076) | −.173 | (.131) | −.559 | (.094) *** | .102 | (.036) ** | −.012 | (.020) | −.019 | (.012) |
| Education | .002 | (.012) | .028 | (.017) | −.047 | (.015)** | .009 | (.006) | −.006 | (.003) * | −.003 | (.002) |
| Household income | −.030 | (.017) | −.096 | (.021) *** | .036 | (.016) * | −.003 | (.009) | −.003 | (.003) | .001 | (.002) |
| Non-employed a | .007 | (.103) | −.086 | (.158) | −.126 | (.171) | .160 | (.044) *** | −.029 | (.021) | −.020 | (.009) * |
| Precarious job a | .263 | (.122) * | .045 | (.301) | −.193 | (.215) | .020 | (.032) | −.037 | (.040) | −.024 | (.024) |
| Single b | −.113 | (.096) | .007 | (.181) | .163 | (.102) | −.063 | (.050) | −.014 | (.017) | −.001 | (.007) |
| Precarious relationship b | .252 | (.241) | .537 | (.317) | .260 | (.195) | .029 | (.061) | −.002 | (.032) | −.006 | (.020) |
| Intercept | 2.518 | (.227) *** | 1.907 | (.513) *** | −5.062 | (.462) *** | −.183 | (.195) | 1.248 | (.062) *** | .763 | (.034) *** |
| R-squared | .077 | .158 | .207 | .151 | .106 | .077 | ||||||
Notes: Unstandardized regression coefficients are presented with robust standard errors in parentheses. Estimates are derived using full information maximum likelihood procedures, with post-stratification weights and robust standard errors clustered by block group. NSAHS = Nashville Stress and Health Study (2011-2014).
Reference = has a stable job.
Reference = in a stable relationship.
p < .05
p < .01
p < .001 (two-tailed).
Racism-Related Stressors as Countervailing Mechanisms
Table 2 provides evidence that increased discrimination and goal-striving stress indirectly predict higher physiological stress levels for Black residents of higher-status areas. First, concentrated privilege predicts greater perceived discrimination (b = .469; p < .001). In turn, perceived discrimination predicts higher goal-striving stress (b = .422; p < .001) and chronic bodily pain (b = .070; p < .01). Higher goal-striving stress also predicts increased levels of neuroendocrine stress hormones (b = .094; p < .05) and diastolic blood pressure (b = .015; p < .01). There is also a positive though marginally significant association between goal-striving stress and systolic blood pressure (b = .013; p < .10). Taken together, these findings provide preliminary support for my second hypothesis. Blacks in higher-status White neighborhoods report more perceived discrimination, which then predicts increased goal-striving and physiological stress response.
Table 3 reports results from the decomposition of direct, indirect, and total associations between concentrated privilege and dimensions of physiological stress response. Significance tests for indirect associations are calculated using the delta method (Sobel 1982). Table 3 confirms there are significant indirect pathways between concentrated privilege and higher physiological stress levels. The fifth row of the first column shows there is a significant pathway leading from concentrated privilege to perceived discrimination, then to goal-striving stress, and finally to neuroendocrine response (b = .019; p < .05). The sixth row of the first column reveals that the total indirect association between concentrated privilege and neuroendocrine response—that is, the sum of specific indirect paths listed in rows three through five—is also positive and statistically significant (b = .089; p < .05). After taking all indirect paths into account, the direct inverse association between concentrated privilege and neuroendocrine response is attenuated by 24%, suggesting suppression effects of perceived discrimination and goal-striving stress.
Table 3.
Decomposition of associations between concentrated privilege (CP) and stress response latent variables: NSAHS, Black subsample (n = 627).
| Neuroendocrine stress response |
Bodily pain |
Diastolic blood pressure |
||||
|---|---|---|---|---|---|---|
| Direct | −.369 | (.121) ** | .038 | (.056) | .002 | (.024) |
| Specific Indirect: | ||||||
| CP ➝ PD ➝ | .042 | (.041) | .033 | (.016) * | .001 | (.004) |
| CP ➝ GSS ➝ | .029 | (.024) | .006 | (.006) | .005 | (.003) |
| CP ➝ PD ➝ GSS ➝ | .019 | (.009) * | .004 | (.003) | .003 | (.002) |
| Total Indirect | .089 | (.044) * | .043 | (.014) ** | .009 | (.004) * |
| Total | −.280 | (.132) * | .081 | (.053) | .011 | (.023) |
| Percent Mediated | 24% | 53% | 82% | |||
Notes: Unstandardized coefficients are reported with robust standard errors in parentheses. Systolic blood pressure is excluded because there were no significant paths (see Table 2). NSAHS = Nashville Stress and Health Study (2011-2014). PD = Perceived discrimination. GSS = Goal-striving stress.
p < .05
p < .01 (two-tailed).
Similar patterns surface for pain and diastolic blood pressure. The indirect path from concentrated privilege to perceived discrimination and then pain is positive and significant (b = .033; p < .05). The sum total of indirect paths leading from concentrated privilege to pain, through discrimination and goal-striving stress, is also positive and significant (b = .043; p < .01). For diastolic blood pressure, the total of indirect paths is positive and significant (b = .009; p < .05). Moreover, the paths leading from concentrated privilege to pain and diastolic blood pressure are entirely indirect, and largely mediated by perceived discrimination and goal-striving stress—53% of the association with pain and 82% for diastolic blood pressure.
Table 3 supports my conceptual model. Living in high-status areas indirectly predicts higher physiological stress levels for Blacks, via perceived discrimination and goal-striving stress. Racism-related stressors also suppress the inverse association between higher neighborhood status and physiological stress response, particularly related to the neuroendocrine system.
Sensitivity Analyses
I also tested the model depicted in Figure 2 among White respondents. The results of these analyses are presented in the online supplement. In short, Whites report less perceived discrimination in higher-status neighborhoods, and there is only one significant pathway leading from higher neighborhood status to lower levels of discrimination, goal-striving stress, and then bodily pain. Among Black respondents, I also did not find any further variations by gender, age, or skin tone (see Hargrove 2018). Finally, I included additional metabolic biomarkers as outcomes, such as blood triglyceride levels, cholesterol, HbA1C, and waist-to-hip ratio. I did not find any significant paths among these biomarkers. Thus, results are limited to neuroendocrine hormones, bodily pain, and blood pressure. I discuss the implications of these findings below.
DISCUSSION
Black Americans who live in areas of concentrated Black disadvantage throughout Nashville exhibit elevated levels of neuroendocrine stress hormones, relative to their Black peers residing in communities of concentrated White privilege. But residents of higher-status White neighborhoods also report more perceived discrimination, which predicts chronic bodily pain and increased goal-striving stress. Goal-striving stress, in turn, is associated with higher levels of stress hormones and blood pressure. The end result is that living in high-status communities is indirectly associated with amplified physiological stress levels for Black residents, and racism-related stressors appear to suppress much of the potential health benefits of living in these areas.
The links between discrimination, goal-striving stress, and physiological stress response also reveal important nuances. While perceived discrimination only predicts chronic bodily pain for Black residents, higher goal-striving stress is associated with elevated stress hormones and blood pressure, particularly diastolic blood pressure. Neither of these stressors are predictive of metabolic biomarkers such as cholesterol or blood glucose levels.
Interpersonal discrimination represents an instance of social rejection to the brain, and research in the emerging field of social neuroscience shows that these episodes can illicit pro-inflammatory pain responses. Proponents of “social pain theory” suggest that this is because our brains have evolved overlapping neural mechanisms that encode experiences of physical and social pain in similar manners (Eisenberger 2015; MacDonald et al. 2005). Although these interrelated mechanisms served us well in prehistoric social contexts, when securing our place within a larger group was a life-or-death matter, the same processes can become toxic whenever we are repeatedly subjected to harsh treatment. Applied to the current context, social pain theory suggests that perceived discrimination triggered inflammatory stress responses for Black residents of high-status neighborhoods, which eventually surfaced as perceptible bodily pain.
The brain not only reacts to discrimination in real time, but also encodes information about how to better respond to similar encounters moving forward (Barrett 2017; Sterling 2012). Thus, chronic exposure to discrimination can train the brain to expect harsh encounters indefinitely, leading to a vigilant state of high goal-striving stress. The felt need to always be “on point,” constantly pushing back against obstacles to major life goals, can drive the release of neuroendocrine hormones akin to a “fight-or-flight” response. This could explain the positive association between goal-striving stress and neuroendocrine hormones for Blacks (DeAngelis 2020). When extended over longer periods, high-effort coping with barriers to goals can also impact cardiovascular systems (James 1994). In this study, goal-striving stress mainly predicts elevated diastolic blood pressure for Blacks, a notable precursor to cardiovascular disease and mortality (Flint et al. 2019).
The fact that neighborhood status and stressors have direct and robust links to pain and neuroendocrine hormones, but inconsistent or no associations with blood pressure or metabolic biomarkers, suggests there may be something unique about the NSAHS sample. According to notions of “allostatic load,” for example, chronic high levels of stress hormones and inflammation should eventually lead to arterial plaque buildup and an overabundance of glucose and fat in the blood (McEwen 1998). The age distribution of NSAHS respondents is one plausible reason for these observed patterns. Recall that the NSAHS is a cross-sectional survey of working-age Black and White adults, ranging from 22 to 69 years old with a mean age of 44. If we could follow respondents over a longer period of time, we might begin to observe more cardiometabolic abnormalities linked to chronic neighborhood stressors.
Current findings can speak to why Black Americans, regardless of socioeconomic status, tend to live shorter and sicker lives than their White peers. Maintaining health and longevity requires living in environments that do not command constant, high-effort regulation of physiological systems (Sterling 2012). On the one hand, Blacks with fewer resources often must live and work in segregated, high-stress areas characterized by crime, police surveillance, and pollution (Massey 2001a; Sharkey 2013). On the other, Blacks who achieve socioeconomic success, and attempt to integrate into higher-status workplaces or neighborhoods, are then subjected to anti-Black racism from Whites (Feagin and Sikes 1994; Ray 2017; Smith et al. 2007). In either scenario, Blacks experience harsher social environments than their White peers, which can tax their brains and bodies and eventually lead to earlier morbidity and mortality (Massey 2017).
The biomarker patterns uncovered in this study could thus reflect broader patterns of chronic illnesses commonly observed among Black populations in the United States. For example, studies suggest that constant high levels of neuroendocrine stress hormones and pro-inflammatory cytokines can atrophy the brain and lead to dementia or stroke (Goosby et al. 2018; Lebedeva et al. 2018). Chronic inflammation can also accelerate biological aging processes via increased oxidative stress and DNA methylation, a phenomenon referred to as “inflammaging” (Franceschi and Campisi 2014). Recent nationwide estimates indicate that relative to Whites, Blacks are 44% more likely to die prematurely from cerebrovascular disease, and also live four years less on average (Hummer and Hamilton 2019:132-137). My analyses suggest that chronic inflammation and neuroendocrine distress, tied to recurring exposures to neighborhood stressors, can help to explain these broader Black-White gaps in health and longevity.
I also find unique patterns among White residents. First, the association between neighborhood status and discrimination is inverted for Whites, suggesting that Whites perceive more discrimination when they reside in disadvantaged and mostly Black areas. Much like their Black peers, perceptions of discrimination also predict higher goal-striving stress for Whites. Unlike Black respondents, however, goal-striving stress—and, less consistently, perceived discrimination—only predicts chronic bodily pain for Whites.
These findings are consistent with a prior study of mine, which tested for Black-White differences in the effects of goal-striving stress among the NSAHS sample (DeAngelis 2020). I found that higher goal-striving stress predicted low self-esteem, depression, anxiety, and passive coping only among Whites. For Blacks, however, goal-striving stress did not predict self-reported mental health but rather increased blood pressure, neuroendocrine stress hormones, and high-effort coping (i.e., John Henryism). Drawing from theories of racial socialization and Whiteness, I proposed that racial privilege conditions White Americans to expect success, and when met with barriers to their goals, Whites are inclined to internalize perceived failures and retreat from society. Black Americans, on the other hand, learn from a young age to expect barriers and, instead of retreating, tend to double down on their strivings and push themselves even harder—hence, the increased stress hormones, blood pressure, and John Henryism.
Racial differences in the health effects of discrimination and blocked goals are striking, especially in light of prior discussions of the human brain. Legacies of slavery, Jim Crow, and mass incarceration have created deep and enduring traumas for Black communities, serving as a perpetual reminder of the high stakes involved in securing freedom in a White supremacist society (Mohatt et al. 2014). Thus, daily or mundane racist encounters, as innocuous as they may seem to White people, reflect centuries of historical pains for Black people, and often signal dangerous status threats that demand extreme vigilance (James 1994). In the current study, perceived discrimination has direct links to bodily pain for Blacks, but not to stress hormones or blood pressure. The more immediate impacts of discrimination, then, appear to be on the immune system via social pain responses. Racist encounters also appear to affect neuroendocrine and cardiovascular systems, but only by first triggering fears of blocked aspirations and related high-effort strivings.
White Americans have not been subjected to centuries of racial oppression, and therefore seem more inclined to interpret unfair treatment or strained goals as a sign of personal deficiency. Again, this is reflected by the fact that goal-striving stress only predicts increased pain for Whites, but not neuroendocrine or cardiovascular distress. Whites do not appear inclined, in other words, to double down on their strivings. Instead, Whites seem more likely to internalize experiences with blocked goals and perceive themselves as social rejects who cannot live up to individualist ideals of achievement (DeAngelis 2020). This could also explain why Whites report more discrimination, goal-striving stress, and pain whenever they live in low-status Black areas. Residing in these kinds of neighborhoods, isolated from their high-status White compatriots, may be interpreted as a sign of failure to participate in the “American Dream” (Hochschild 1995). The internalization of perceived failures could then lead to deep feelings of social pain, despair, and, in more extreme cases, even substance addiction or suicide (see Case and Deaton 2017; Metzl 2019).
CONCLUSION
This study is not without limitations. First, the data used in this study are restricted to Black and White working-age adults residing in urban and suburban areas across Nashville. Although I offered reasons for why Nashville is an appropriate location for my study, I also acknowledge that the unique historical and cultural evolution of Nashville could mean findings are not generalizable beyond this area. Future studies should test similar conceptual models in rural areas or in metropolitan areas with different historical patterns of racial segregation.
Future work could also determine whether the conceptual model tested in this study can be extended to other social environments, including schools, workplaces, or churches (e.g., Assari and Moghani Lankarani 2018). Social pain theory also suggests that vicarious exposure to racism on social media, or through word-of-mouth from loved ones, will trigger similar stress responses as those experienced in direct racist encounters (Cheadle et al. 2020). Moreover, tracking respondents’ social interactions with real-time smartphone data would provide richer accounts of daily activity spaces in future studies (see York Cornwell and Goldman 2020). To better account for temporal precision in the discrimination-stress relationship, researchers could then triangulate activity space data with real-time stress response data harnessed through newer bio-signal technologies (see Cheadle et al. 2020). Indeed, another main limitation of the current study design is that data are cross-sectional and respondent reports of discrimination are general and retrospective. My analyses therefore cannot establish temporal ordering between stressors and biomarker outcomes.
Despite these limitations, the present study advances our understanding of racial and place-based health disparities in the United States. By merging survey, biomarker, and census data from a representative sample of Black and White adults, I revealed the hidden health costs of neighborhood attainment for Black Americans. When Blacks reside in involuntarily segregated Black areas, they are subjected to higher degrees of social disorder, policing, and pollution. When Blacks reside in high-status neighborhoods, however, their minds and bodies have to adapt to anti-Black racism from White neighbors. Racial disparities in health and longevity will likely persist, then, for as long as Black Americans are forced to contend with White racism.
Supplementary Material
Acknowledgements
The author thanks the following persons for providing invaluable feedback on earlier drafts of this study: Allison Aiello, Ken Bollen, Esther Chung, Barbara Entwisle, Christy Erving, Bridget Goosby, Iliya Gutin, Taylor Hargrove, Kathie Harris, Bob Hummer, Adam Lilly, and Liana Richardson. Any errors or omissions are the fault of the author and not of the reviewers. I also thank John Taylor for granting me access to the Nashville Stress and Health Study data. Finally, I would like to acknowledge the 1,252 participants of the Nashville Stress and Health Study who endured three-hour survey interviews, 12-hour fasting sessions, and extensive biomarker panels for the sake of advancing health disparities research.
Funding and Data
This research uses data from the Nashville Stress and Health Study, a project led by the late R. Jay Turner and funded by the National Institute on Aging (R01AG034067). The author received support from the Population Research Infrastructure Program (P2C-HD050924) and the Biosocial Training Program (T32-HD091058) awarded to the Carolina Population Center at the University of North Carolina at Chapel Bill by the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Footnotes
Block group percentages of Black and White residents are almost perfectly collinear in the NSAHS sample (r = −.97). The other indicators are also highly correlated with neighborhood racial composition (see online supplement).
Researchers typically combine these three items into an observed scale. The most common formula for this scale weights the respondent’s subjective distance from aspirations by the product of their emotional attachment and subjective likelihood scores (e.g., Sellers and Neighbors 2008). Preliminary analyses included scaled scores instead of the latent variable and findings were comparable.
Preliminary analyses also included controls for home values, liquid financial assets, polynomials for age, and the perceived racial compositions of respondents’ workplaces and churches. These controls were excluded from the final model because they did not account for unique variance.
REFERENCES
- Allen Amani M., Thomas Marilyn D., Michaels Eli K., Reeves Alexis N., Okoye Uche, Price Melisa M., Hasson Rebecca E., Syme S. Leonard, and Chae David H.. 2019. “Racial Discrimination, Educational Attainment, and Biological Dysregulation among Midlife African American Women.” Psychoneuroendocrinology 99:225–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson Elijah. 2015. “‘The White Space.’” Sociology of Race and Ethnicity 1(1):10–21. [Google Scholar]
- Assari Shervin, and Lankarani Maryam Moghani. 2018. “Workplace Racial Composition Explains High Perceived Discrimination of High Socioeconomic Status African American Men.” Brain Sciences 8(8):139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber Sharrelle, Hickson DeMarc A., Kawachi Ichiro, Subramanian SV, and Earls Felton. 2016. “Neighborhood Disadvantage and Cumulative Biological Risk Among a Socioeconomically Diverse Sample of African American Adults: An Examination in the Jackson Heart Study.” Journal of Racial and Ethnic Health Disparities 3(3):444–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett Lisa Feldman. 2017. How Emotions Are Made. Boston, MA: Houghton Mifflin Harcourt. [Google Scholar]
- Beauchamp Zack. 2020. “Ahmaud Arbery and the Dangers of Running While Black.” Vox. Retrieved April 5, 2020 (https://www.vox.com/policy-and-politics/2020/5/8/21250914/ahmaud-arbery-mcmichael-arrest-black-men-exercise). [Google Scholar]
- Bécares Laia, Shaw Richard, Nazroo James, Stafford Mai, Albor Christo, Atkin Karl, Kiernan Kathleen, Wilkinson Richard, and Pickett Kate. 2012. “Ethnic Density Effects on Physical Morbidity, Mortality, and Health Behaviors: A Systematic Review of the Literature.” American Journal of Public Health 102(12):e33–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bobo Lawrence, and Zubrinsky Camille L.. 1996. “Attitudes on Residential Integration: Perceived Status Differences, Mere In-Group Preference, or Racial Prejudice?” Social Forces 74(3):883–909. [Google Scholar]
- Bollen Kenneth A. 1989. Structural Equations with Latent Variables. New York, NY: John Wiley & Sons. [Google Scholar]
- Bollen Kenneth A., and Bauldry Shawn. 2011. “Three Cs in Measurement Models: Causal Indicators, Composite Indicators, and Covariates.” Psychological Methods 16(3):265–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs Gabriel A. 2015. The New Negro in the Old South. New Brunswick, NJ: Rutgers University Press. [Google Scholar]
- Cain Loretta R., Glover LáShauntá, Young Bessie, and Sims Mario. 2019. “Goal-Striving Stress Is Associated with Chronic Kidney Disease Among Participants in the Jackson Heart Study.” Journal of Racial and Ethnic Health Disparities 6(1):64–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cain-Shields Loretta R., Johnson Dayna A., Glover LáShauntá, and Sims Mario. 2020. “The Association of Goal-Striving Stress with Sleep Duration and Sleep Quality among African Americans in the Jackson Heart Study.” Sleep Health 6(1):117–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case Anne, and Deaton Angus. 2017. “Mortality and Morbidity in the 21st Century.” Brookings Papers on Economic Activity 2017(1):397–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheadle Jacob E., Goosby Bridget J., Jochman Joseph C., Tomaso Cara C., Yancey Chelsea B. Kozikowski, and Nelson Timothy D.. 2020. “Race and Ethnic Variation in College Students’ Allostatic Regulation of Racism-Related Stress.” Proceedings of the National Academy of Sciences 117(49):31053–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiricos Ted, McEntire Ranee, and Gertz Marc. 2001. “Perceived Racial and Ethnic Composition of Neighborhood and Perceived Risk of Crime.” Social Problems 48(3):322–40. [Google Scholar]
- Cole Elizabeth R., and Omari Safiya R.. 2003. “Race, Class and the Dilemmas of Upward Mobility for African Americans.” Journal of Social Issues 59(4):785–802. [Google Scholar]
- Colen Cynthia G., Geronimus Arline T., Bound John, and James Sherman A.. 2006. “Maternal Upward Socioeconomic Mobility and Black–White Disparities in Infant Birthweight.” American Journal of Public Health 96(11):2032–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colen Cynthia G., Krueger Patrick M., and Boettner Bethany L.. 2018. “Do Rising Tides Lift All Boats? Racial Disparities in Health across the Lifecourse among Middle-Class African-Americans and Whites.” SSM - Population Health 6:125–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins Eileen M., and Seeman Teresa E.. 2004. “Integrating Biology into the Study of Health Disparities.” Population and Development Review 30:89–107. [Google Scholar]
- DeAngelis Reed T. 2020. “Striving While Black: Race and the Psychophysiology of Goal Pursuit.” Journal of Health and Social Behavior 61(1):24–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dovidio John F., and Gaertner Samuel L.. 2004. “Aversive Racism.” Pp. 1–51 in Vol. 36, Advances in Experimental Social Psychology. San Diego, CA: Academic Press. [Google Scholar]
- Du Bois WEB 1899. The Philadelphia Negro: A Social Study. Philadelphia, PA: University of Pennsylvania Press. [Google Scholar]
- Eisenberger Naomi I. 2015. “Social Pain and the Brain: Controversies, Questions, and Where to Go from Here.” Annual Review of Psychology 66(1):601–29. [DOI] [PubMed] [Google Scholar]
- Enders Craig, and Bandalos Deborah. 2001. “The Relative Performance of Full Information Maximum Likelihood Estimation for Missing Data in Structural Equation Models.” Structural Equation Modeling: A Multidisciplinary Journal 8(3):430–57. [Google Scholar]
- Farmer Melissa M., and Ferraro Kenneth F.. 2005. “Are Racial Disparities in Health Conditional on Socioeconomic Status?” Social Science & Medicine 60(1):191–204. [DOI] [PubMed] [Google Scholar]
- Feagin Joe R., and Sikes Melvin P.. 1994. Living with Racism: The Black Middle-Class Experience. Boston, MA: Beacon Press. [Google Scholar]
- Flint Alexander C., Conell Carol, Ren Xiushui, Banki Nader M., Chan Sheila L., Rao Vivek A., Melles Ronald B., and Bhatt Deepak L.. 2019. “Effect of Systolic and Diastolic Blood Pressure on Cardiovascular Outcomes.” New England Journal of Medicine 381(3):243–51. [DOI] [PubMed] [Google Scholar]
- Franceschi C, and Campisi J. 2014. “Chronic Inflammation (Inflammaging) and Its Potential Contribution to Age-Associated Diseases.” The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 69(Suppl 1):S4–9. [DOI] [PubMed] [Google Scholar]
- Frey William H. 2011. “The New Metro Minority Map: Regional Shifts in Hispanics, Asians, and Blacks from Census 2010.” Brookings Papers on Metropolitan Policy 1–18. [Google Scholar]
- Gaydosh Lauren, Schorpp Kristen M., Chen Edith, Miller Gregory E., and Harris Kathleen Mullan. 2018. “College Completion Predicts Lower Depression but Higher Metabolic Syndrome among Disadvantaged Minorities in Young Adulthood.” Proceedings of the National Academy of Sciences 115(1):109–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goetz Edward G., Damiano Tony, and Hicks Jason. 2019. “Racially Concentrated Areas of Affluence: A Preliminary Investigation.” Cityscape 21(1):99–124. [Google Scholar]
- Goosby Bridget J., Cheadle Jacob E., and Mitchell Colter. 2018. “Stress-Related Biosocial Mechanisms of Discrimination and African American Health Inequities.” Annual Review of Sociology 44(1):319–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halanych Jewell H., Safford Monika M., Shikany James M., Cuffee Yendelela, Person Sharina D., Scarinci Isabel C., Kiefe Catarina I., and Allison Jeroan J.. 2011. “The Association Between Income, Education, and Experiences of Discrimination in Older African American and European American Patients.” Ethnicity & Disease 21(2):223–29. [PMC free article] [PubMed] [Google Scholar]
- Halberstam David. 1998. The Children. New York, NY: Ballantine Books. [Google Scholar]
- Hargrove Taylor W. 2018. “BMI Trajectories in Adulthood: The Intersection of Skin Color, Gender, and Age among African Americans.” Journal of Health and Social Behavior 59(4):501–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris Cheryl I. 1993. “Whiteness as Property.” Harvard Law Review 106(8):1707–91. [Google Scholar]
- Harris Kathleen Mullan, and Schorpp Kristen M.. 2018. “Integrating Biomarkers in Social Stratification and Health Research.” Annual Review of Sociology 44(1):361–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicken Margaret T., Lee Hedwig, Ailshire Jennifer, Burgard Sarah A., and Williams David R.. 2013. “‘Every Shut Eye, Ain’t Sleep’: The Role of Racism-Related Vigilance in Racial/Ethnic Disparities in Sleep Difficulty.” Race and Social Problems 5(2):100–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicken Margaret T., Lee Hedwig, and Hing Anna K.. 2018. “The Weight of Racism: Vigilance and Racial Inequalities in Weight-Related Measures.” Social Science & Medicine 199:157–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicken Margaret T., Lee Hedwig, Morenoff Jeffrey, House James S., and Williams David R.. 2014. “Racial/Ethnic Disparities in Hypertension Prevalence: Reconsidering the Role of Chronic Stress.” American Journal of Public Health 104(1):117–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill Terrence D., Ross Catherine E., and Angel Ronald J.. 2005. “Neighborhood Disorder, Psychophysiological Distress, and Health.” Journal of Health and Social Behavior 46(2):170–86. [DOI] [PubMed] [Google Scholar]
- Hochschild Jennifer L. 1995. Facing Up to the American Dream: Race, Class, and the Soul of the Nation. Princeton, N.J: Princeton University Press. [Google Scholar]
- Houston Benjamin. 2012. The Nashville Way: Racial Etiquette and the Struggle for Social Justice in a Southern City. Athens, GA: University of Georgia Press. [Google Scholar]
- Hummer Robert A., and Hamilton Erin R.. 2019. Population Health in America. Oakland, CA: University of California Press. [Google Scholar]
- Hunt Matthew O., Wise Lauren A., Jipguep Marie-Claude, Cozier Yvette C., and Rosenberg Lynn. 2007. “Neighborhood Racial Composition and Perceptions of Racial Discrimination: Evidence from the Black Women’s Health Study.” Social Psychology Quarterly 70(3):272–89. [Google Scholar]
- Jackson Pamela Braboy, Thoits Peggy A., and Taylor Howard F.. 1995. “Composition of the Workplace and Psychological Well-Being: The Effects of Tokenism on America’s Black Elite.” Social Forces 74(2):543–57. [Google Scholar]
- James Sherman A. 1994. “John Henryism and the Health of African-Americans.” Culture, Medicine and Psychiatry 18(2):163–82. [DOI] [PubMed] [Google Scholar]
- Lebedeva A, Sundström A, Lindgren L, Stomby A, Aarsland D, Westman E, Winblad B, Olsson T, and Nyberg L. 2018. “Longitudinal Relationships among Depressive Symptoms, Cortisol, and Brain Atrophy in the Neocortex and the Hippocampus.” Acta Psychiatrica Scandinavica 137(6):491–502. [DOI] [PubMed] [Google Scholar]
- Lewis VA, Emerson MO, and Klineberg SL. 2011. “Who We’ll Live With: Neighborhood Racial Composition Preferences of Whites, Blacks and Latinos.” Social Forces 89(4):1385–1407. [Google Scholar]
- MacDonald Geoff, Kingsbury Rachell, and Shaw Stephanie. 2005. “Adding Insult to Injury: Social Pain Theory and Response to Social Exclusion.” Pp. 77–90 in The Social Outcast: Ostracism, Social Exclusion, Rejection, and Bullying, edited by Williams KD, Forgas JP, and von Hippel W. UK: Taylor & Francis. [Google Scholar]
- MacKinnon David P., Krull Jennifer L., and Lockwood Chondra M.. 2000. “Equivalence of the Mediation, Confounding and Suppression Effect.” Prevention Science 1(4):173–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massey Douglas S. 1996. “The Age of Extremes: Concentrated Affluence and Poverty in the Twenty-First Century.” Demography 33(4):395. [PubMed] [Google Scholar]
- Massey Douglas S. 2001. “A Brief History of Human Society: The Origin and Role of Emotion in Social Life.” American Sociological Review 67(1):1–29. [Google Scholar]
- Massey Douglas S. 2001a. “Segregation and Violent Crime in Urban America.” Pp. 317–44 in Problem of the Century: Racial Stratification in the United States, edited by Anderson E and Massey DS. New Haven, CT: Yale University Press. [Google Scholar]
- Massey Douglas S. 2001b. “The Prodigal Paradigm Returns: Ecology Comes Back to Sociology.” Pp. 41–47 in Does it Take a Village? Community Effects on Children, Adolescents, and Families, edited by Booth A and Crouter AC. Mahwah, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Massey Douglas S. 2004. “Segregation and Stratification: A Biosocial Perspective.” Du Bois Review: Social Science Research on Race 1(1):7–25. [Google Scholar]
- Massey Douglas S. 2015. “Brave New World of Biosocial Science.” Criminology 53(1):127–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massey Douglas S. 2017. “Why Death Haunts Black Lives.” Proceedings of the National Academy of Sciences 114(5):800–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massey Douglas S., and Denton Nancy A.. 1993. American Apartheid: Segregation and the Making of the Underclass. Cambridge, MA: Harvard University Press. [Google Scholar]
- Mayne Stephanie L., Hicken Margaret T., Merkin Sharon Stein, Seeman Teresa E., Kershaw Kiarri N., Do D. Phuong, Hajat Anjum, and Roux Ana V. Diez. 2019. “Neighbourhood Racial/Ethnic Residential Segregation and Cardiometabolic Risk: The Multiethnic Study of Atherosclerosis.” Journal of Epidemiology and Community Health 73(1):26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen Bruce S. 1998. “Stress, Adaptation, and Disease: Allostasis and Allostatic Load.” Annals of the New York Academy of Sciences 840(1):33–44. [DOI] [PubMed] [Google Scholar]
- McFarland Michael J., Taylor John, McFarland Cheryl A. S., and Friedman Katherine L.. 2018. “Perceived Unfair Treatment by Police, Race, and Telomere Length: A Nashville Community-Based Sample of Black and White Men.” Journal of Health and Social Behavior 59(4):585–600. [DOI] [PubMed] [Google Scholar]
- Metzl Jonathan M. 2019. Dying of Whiteness: How the Politics of Racial Resentment Is Killing America’s Heartland. New York, NY: Basic Books. [Google Scholar]
- Mitchell Uchechi A., Gutierrez-Kapheim Melissa, Nguyen Ann W., and Al-Amin Nadia. 2020. “Hopelessness Among Middle-Aged and Older Blacks: The Negative Impact of Discrimination and Protecting Power of Social and Religious Resources” edited by Sands LP. Innovation in Aging 4(5):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohatt Nathaniel Vincent, Thompson Azure B., Thai Nghi D., and Tebes Jacob Kraemer. 2014. “Historical Trauma as Public Narrative: A Conceptual Review of How History Impacts Present-Day Health.” Social Science & Medicine 106:128–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker Seymour, and Kleiner Robert J.. 1966. Mental Illness in the Urban Negro Community. New York, NY: Free Press. [Google Scholar]
- Pearlin Leonard I. 1989. “The Sociological Study of Stress.” Journal of Health and Social Behavior 30(3):241–56. [PubMed] [Google Scholar]
- Pearlin Leonard I., Menaghan Elizabeth G., Lieberman Morton A., and Mullan Joseph T.. 1981. “The Stress Process.” Journal of Health and Social Behavior 22(4):337–56. [PubMed] [Google Scholar]
- Perreira Krista M., Deeb-Sossa Natalia, Harris Kathleen Mullan, and Bollen Kenneth. 2005. “What Are We Measuring? An Evaluation of the CES-D Across Race/Ethnicity and Immigrant Generation*.” Social Forces 83(4):1567–1601. [Google Scholar]
- Phelan Jo C., and Link Bruce G.. 2015. “Is Racism a Fundamental Cause of Inequalities in Health?” Annual Review of Sociology 41(1):311–30. [Google Scholar]
- Pickett Kate E., and Wilkinson Richard G.. 2008. “People like Us: Ethnic Group Density Effects on Health.” Ethnicity & Health 13(4):321–34. [DOI] [PubMed] [Google Scholar]
- Ray Rashawn. 2017. “Black People Don’t Exercise in My Neighborhood: Perceived Racial Composition and Leisure-Time Physical Activity among Middle Class Blacks and Whites.” Social Science Research 66:42–57. [DOI] [PubMed] [Google Scholar]
- Ray Victor. 2019. “A Theory of Racialized Organizations.” American Sociological Review 84(1):26–53. [Google Scholar]
- Rothstein Richard. 2017. The Color of Law: A Forgotten History of How Our Government Segregated America. New York, NY: Liveright Publishing. [Google Scholar]
- Schieman Scott. 2009. “Residential Stability, Neighborhood Racial Composition, and the Subjective Assessment of Neighborhood Problems Among Older Adults.” The Sociological Quarterly 50(4):608–32. [Google Scholar]
- Sellers Sherrill L., and Neighbors Harold W.. 2008. “Effects of Goal-Striving Stress on the Mental Health of Black Americans.” Journal of Health and Social Behavior 49(1):92–103. [DOI] [PubMed] [Google Scholar]
- Semega Jessica, Kollar Melissa, Shrider Emily A., and Creamer John F.. 2020. “Income and Poverty in the United States: 2019.” Pp. 60–270 in U.S. Census Bureau, Current Population Reports. Washington, D.C: U.S. Government Publishing Office. [Google Scholar]
- Sharkey Patrick. 2013. Stuck in Place: Urban Neighborhoods and the End of Progress toward Racial Equality. Chicago, IL: University of Chicago Press. [Google Scholar]
- Smith Nicholas C. 2021. “Black-White Disparities in Women’s Physical Health: The Role of Socioeconomic Status and Racism-Related Stressors.” Social Science Research Online first. [DOI] [PubMed] [Google Scholar]
- Smith William A., Allen Walter R., and Danley Lynette L.. 2007. “‘Assume the Position … You Fit the Description’: Psychosocial Experiences and Racial Battle Fatigue Among African American Male College Students.” American Behavioral Scientist 51(4):551–78. [Google Scholar]
- Smith William A., Hung Man, and Franklin Jeremy D.. 2011. “Racial Battle Fatigue and the MisEducation of Black Men: Racial Microaggressions, Societal Problems, and Environmental Stress.” The Journal of Negro Education 80(1):63–82. [Google Scholar]
- Sobel Michael E. 1982. “Asymptotic Confidence Intervals for Indirect Effects in Structural Equation Models.” Sociological Methodology 13:290–312. [Google Scholar]
- Sterling Peter. 2012. “Allostasis: A Model of Predictive Regulation.” Physiology & Behavior 106(1):5–15. [DOI] [PubMed] [Google Scholar]
- Turner R. Jay. 2013. “Understanding Health Disparities: The Relevance of the Stress Process Model.” Society and Mental Health 3(3):170–86. [Google Scholar]
- Turner R. Jay, Brown Tony N., and Hale William Beardall. 2017. “Race, Socioeconomic Position, and Physical Health: A Descriptive Analysis.” Journal of Health and Social Behavior 58(1):23–36. [DOI] [PubMed] [Google Scholar]
- Turney Kristin. 2014. “Stress Proliferation across Generations? Examining the Relationship between Parental Incarceration and Childhood Health.” Journal of Health and Social Behavior 55(3):302–19. [DOI] [PubMed] [Google Scholar]
- Ware John E., and Sherbourne Cathy Donald. 1992. “The MOS 36-Item Short-Form Health Survey (SF-36): I. Conceptual Framework and Item Selection.” Medical Care 30(6):12. [PubMed] [Google Scholar]
- Wheaton Blair. 1985. “Models for the Stress-Buffering Functions of Coping Resources.” Journal of Health and Social Behavior 26(4):352–64. [PubMed] [Google Scholar]
- Williams David R., and Collins Chiquita. 2001. “Racial Residential Segregation: A Fundamental Cause of Racial Disparities in Health.” Public Health Reports 116:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yancey George. 2003. Who Is White? Latinos, Asians, and the New Black/Nonblack Divide. Boulder, Colorado: Lynne Rienner Publishers. [Google Scholar]
- York Cornwell Erin, and Goldman Alyssa W.. 2020. “Neighborhood Disorder and Distress in Real Time: Evidence from a Smartphone-Based Study of Older Adults.” Journal of Health and Social Behavior 61(4):523–41. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


