Abstract
Empirical research regarding the health benefits of positive psychological well‐being (e.g., positive emotions, life satisfaction, purpose in life, and optimism) has flourished in recent years, particularly with regard to cardiovascular disease. This paper reviews the state of evidence for well‐being's association with cardiovascular disease in both healthy individuals and those diagnosed with a disease. Prospective studies consistently indicate well‐being reduces cardiovascular events in healthy and, to a lesser extent, patient populations. Potential pathways that link well‐being with cardiovascular disease are discussed (including health behaviors, physiological processes, and stress buffering), although the existing evidence is mostly cross‐sectional which limits conclusions about directionality. Issues related to development across the lifespan are considered and childhood is identified as a crucial period for establishing healthy cardiovascular trajectories. Outstanding questions for future research are provided with recommendations to focus on well‐powered and prospective study designs with rigorous assessment of both well‐being and cardiovascular‐related outcomes.
1. INTRODUCTION
In the last 30 years, empirical research related to positive psychological well‐being (hereafter shortened to well‐being) has exploded. Well‐being is distinct from markers of psychological distress such as depression and anxiety, the latter of which may indicate the presence of poor psychological functioning. By contrast, well‐being is defined as the “positive feelings, cognitions, and strategies of individuals who function well in their life and evaluate their life favorably” (Boehm & Kubzansky, 2012, p. 656). Rather than signaling a deficit or problem to be solved, well‐being signals that life is going well or that psychological resources are present. Well‐being is a broad concept that encompasses constructs from various theoretical traditions including positive emotions, life satisfaction, purpose in life, and optimism. Different taxonomies of well‐being have been proposed (Diener, Suh, et al., 1999; Keyes et al., 2002; Ryan & Deci, 2001; Steptoe, 2019), the most prominent of which include hedonic well‐being (colloquially referred to as happiness and assessed via positive emotions and satisfaction with life) and eudaimonic well‐being (fulfilling one's potential and assessed via purpose in life).
Well‐being feels good in its own right, but is also associated with beneficial outcomes including supportive social relationships (Algoe, 2019; Diener et al., 2018), career success (Walsh et al., 2018), and healthier and longer lives (Boehm & Kubzansky, 2012; Martin‐Maria et al., 2017; Steptoe, 2019). Perhaps the most robust evidence for the latter comes from the area of cardiovascular disease (CVD), which is the leading cause of death worldwide and includes diagnoses such as coronary heart disease and stroke (Virani et al., 2020). Although a robust association exists between psychological distress and increased risk of CVD (Suls, 2018), only recently has well‐being demonstrated its own independent associations with CVD. Research in this area has caught the attention of the American Heart Association, which identified well‐being as “an important frontier of knowledge” in its 2030 goal to promote healthier lives for all members of the population (Angell et al., 2020, p. e127). As such, this is a key time to evaluate the current state of evidence for well‐being's connection to CVD.
The primary hypothesis guiding this work is that people with greater levels of well‐being have reduced risk of CVD. Moreover, any apparent association may be due to underlying processes related to health behaviors, physiological function, and buffering against stress. The overarching theoretical framework for these associations is depicted in Figure 1. To evaluate these connections, this paper first reviews the evidence for an association between well‐being and CVD, as depicted by the green rectangle and red diamond in Figure 1. Next, well‐being's association with pathways that potentially link well‐being with CVD (represented by the blue double‐headed arrow and yellow triangle in Figure 1) will be examined. These associations are discussed within a development context (represented by the unidirectional arrow at the bottom of Figure 1) and issues related to the social and physical environment are briefly considered. Finally, outstanding questions for future research are discussed.
FIGURE 1.
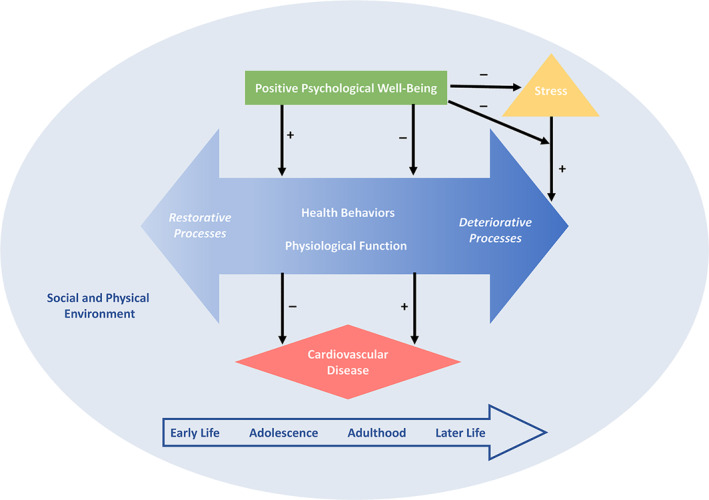
Model of the underlying pathways linking positive psychological well‐being with cardiovascular disease across the lifespan. Adapted and reprinted from Kubzansky, Huffman, et al. (2018) and Boehm and Kubzansky (2012)
2. ASSESSING AND CONCEPTUALIZING WELL‐BEING
Although well‐being is displayed concisely in Figure 1, its assessment and theoretical conceptualization are not straightforward in practice. There is substantial debate about which measure of well‐being should be prioritized for assessment and how well‐being should be optimally assessed (Ryff et al., 2020; VanderWeele et al., 2020). Oftentimes, there are even moderately strong intercorrelations between different indicators of well‐being (Kashdan et al., 2008), so strict theoretical distinctions in well‐being may not be adequately captured with current assessment methods. Moreover, most research in this area has been based on large epidemiological cohorts that assess thousands of people over time to determine who develops CVD. Until recently, such epidemiological cohorts had only limited assessments of psychological factors and even more rare, assessments of well‐being. Thus, researchers have been somewhat constrained by the specific indicators of well‐being that were assessed (often single items, sometimes shortened or unvalidated scales). Given that one indicator of well‐being is not consistently used in this area of research and evidence is not clear regarding which indicator of well‐being is most relevant, the review that follows considers a variety of common well‐being indicators including life satisfaction (an overall evaluation of one's life; Pavot & Diener, 2008), positive affect (the experience of positive emotions; Pressman et al., 2018), life purpose (having valued goals and activities in one's life; McKnight & Kashdan, 2009), and optimism (favorable expectations for the future; Carver et al., 2010). Whenever possible, the specific indicator of well‐being used in each study is noted.
3. WELL‐BEING'S LONGITUDINAL ASSOCIATION WITH CVD
The association between well‐being and cardiovascular outcomes may look different depending on whether well‐being is assessed when people are initially healthy or after they have been diagnosed with CVD. Indeed, cardiovascular outcomes and study methodologies (e.g., size and length of investigation) may also differ between these groups. For people who start a study healthy, researchers tend to measure well‐being at baseline and then follow participants across years or decades to see which baseline characteristics were associated with the first diagnosis of CVD. CVD can be defined in a variety of ways, but often include physician‐diagnosed heart attack or stroke, or death from a cardiovascular‐related cause. The relevant question for these types of studies is whether baseline levels of well‐being reduce the risk of initial CVD diagnoses during a subsequent time period (i.e., incident CVD). For people diagnosed with CVD prior to a study's baseline, the outcome of interest is typically a secondary event like another heart attack, hospitalization, or death. The question then becomes whether well‐being reduces risk of these secondary CVD events (i.e., whether well‐being delays disease processes that are already underway). Because well‐being's role may differ in these two scenarios, we review the evidence published to date separately. In general, however, strong evidence for well‐being's association with reduced risk of CVD is characterized by longitudinal studies that assess well‐being with a validated measure, follow individuals across multiple years to see who goes on to experience an objectively assessed cardiovascular event, and statistically adjust for potential confounders or mechanisms such as socioeconomic status, health behaviors, and psychological distress (Boehm & Kubzansky, 2012).
3.1. Well‐being's longitudinal association with CVD in initially healthy individuals
Consistent with the primary hypothesis guiding this work, evidence from the studies of initially healthy people show that higher levels of well‐being tend to be associated with reduced risk of incident CVD (i.e., the first diagnosis of CVD). For example, in one study with nearly 8000 British civil servants, those with the highest baseline levels of life satisfaction had 13% reduced risk of coronary heart disease 5 years later (Boehm et al., 2011). These findings were robust to confounders including psychological distress. In addition, among nearly 7000 older adults in the United States, those with low versus high levels of purpose in life had higher risk of death due to heart‐related conditions (Alimujiang et al., 2019). Two meta‐analyses have summarized existing work and found that higher levels of optimism and life purpose were each associated with 35% reduced risk of experiencing a first‐time cardiovascular event (Cohen et al., 2015; Rozanski et al., 2019). Thus, it appears that well‐being is prospectively associated with better cardiovascular outcomes among people who start studies healthy.
3.2. Well‐being's longitudinal association with CVD in individuals diagnosed with CVD
In line with evidence from initially healthy individuals, well‐being appears to be related to reduced risk of a secondary CVD event in those people with a pre‐existing CVD diagnosis. One systematic review has examined studies of people with known heart disease to determine whether well‐being was associated with reduced risk for cardiovascular events such as re‐hospitalizations and death (DuBois et al., 2015). Although participant characteristics (e.g., diagnosis type) and study methodologies (e.g., outcomes, sample sizes, duration of follow‐up, and control for confounders) differed, individuals with higher versus lower levels of well‐being had 11% reduced risk of mortality and 19% reduced risk of re‐hospitalization (DuBois, et al., 2015). For example, one study assessed positive emotions in more than 800 cardiac patients and then re‐assessed them 11 years later (Brummett et al., 2005). Individuals with higher levels of positive emotions had 20% reduced risk of mortality. However, when depression was considered alongside positive emotions, associations were attenuated.
The association between well‐being and longevity among CVD patients may exist because well‐being is related to better treatment adherence (Bassett et al., 2019). For example, among more than 600 people with coronary heart disease, increases in positive emotions across 5 years co‐occurred with improved medication adherence when accounting for sociodemographic characteristics, body mass index (BMI), lipids, and depressive symptoms. In another study, 400 individuals reported their positive emotions and optimism within 1 month of percutaneous coronary intervention (a non‐surgical procedure to open blood vessels near the heart). Higher levels of optimism and positive emotions were each associated with better self‐reported adherence to recommended treatments 6 months later; however, only optimism's association was maintained when adjusting for covariates like psychological distress (van Montfort et al., 2016).
3.2.1. Summary of findings for well‐being's longitudinal association with CVD
Prospective longitudinal studies of initially healthy individuals provide the most robust evidence to date that well‐being may precede and reduce CVD risk. However, such observational studies may be subject to residual confounding by unmeasured variables and cannot establish causality. Future work that examines changes in well‐being over time in relation to CVD (Martin‐Maria, et al., 2017) or that targets well‐being in randomized trials (Kubzansky, Huffman, et al., 2018) are necessary next steps.
In general, well‐being also seems to play a role in the progression of CVD (i.e., experiencing subsequent cardiovascular events after a CVD diagnosis). However, these associations may not be as large or as robust as those in healthy populations, perhaps because disease processes are well‐underway once a diagnosis is received. Moreover, well‐being's relatively small effects may not be enough to counter entrenched disease trajectories. It is also possible that well‐being and psychological distress may be more closely intertwined in patient populations relative to healthy populations.
4. PATHWAYS LINKING WELL‐BEING AND CVD
Given evidence pointing to an association between well‐being and CVD, researchers have proposed underlying pathways linking the two together. These include an indirect pathway via health behaviors, a direct pathway through physiological processes, and buffering against the detrimental effects of stress (Figure 1). Well‐being is expected to bolster restorative processes like sleep and high‐density lipoprotein cholesterol (HDL‐C; i.e., “good” cholesterol that removes “bad” cholesterol like low‐density lipoprotein cholesterol [LDL‐C] from the bloodstream; Robles & Carroll, 2011) as well as diminish deteriorative processes like cigarette smoking and atherosclerosis (i.e., buildup of plaque in the arteries). In turn, restorative processes are expected to reduce the risk of CVD while deteriorative processes are expected to increase the risk of CVD. Evidence for well‐being's association with each potential pathway appears in the subsequent subsections.
4.1. Well‐being's association with health behaviors
Well‐being may reduce risk of CVD by encouraging individuals to engage in restorative, health‐promoting behaviors (e.g., eating fruits and vegetables) and avoid deteriorative, health‐diminishing behaviors (e.g., cigarette smoking). In other words, well‐being may foster a healthy lifestyle (Trudel‐Fitzgerald, James, et al., 2019). A meta‐analysis examining optimism's association with three health behaviors critical for CVD—physical activity, dietary consumption, and cigarette smoking (Virani, et al., 2020)—found that individuals with higher versus lower levels of optimism tended to engage in more frequent exercise, ate healthier foods, and were less likely to smoke cigarettes (Boehm, Chen, et al., 2018). Two notable conclusions emerged (see similar conclusions from a systematic review regarding the association between positive emotions and better sleep; Ong et al., 2017). First, the magnitude of association between optimism and health behaviors was relatively modest (r = 0.07–0.12). Second, most evidence was cross‐sectional. As an example of cross‐sectional evidence, a representative sample of more than 2.5 million people in the United States showed that higher levels of positive emotions and life satisfaction were each associated with eating fruits and vegetables and exercising 30 min a day (Kushlev et al., 2020). However, cross‐sectional evidence cannot establish whether greater well‐being precedes healthier behavior or whether healthier behaviors precede greater well‐being. Although it is likely that bi‐directional relationships exist, evaluating the direction of associations presented in Figure 1 will help determine whether well‐being could serve as an intervention target for fostering restorative health behaviors, minimizing deteriorative health behaviors, and reducing risk of CVD (Boehm et al., 2012). Thus, to establish temporal order, the next sections review longitudinal evidence that well‐being precedes restorative and deteriorative health behaviors.
4.1.1. Well‐being's longitudinal association with restorative health behaviors
In the few longitudinal studies published to date, greater well‐being precedes restorative or health‐promoting behaviors. For example, higher versus lower levels of well‐being co‐occurred with more fruit and vegetable consumption in older English adults. Although fruit and vegetable consumption declined across the 7‐year study, older adults with higher baseline well‐being also showed slower declines in fruit and vegetable consumption (Boehm, Soo, et al., 2018). Additionally, greater baseline levels of purpose in older US adults were associated with lower likelihood of experiencing disrupted sleep across 4–8 years when accounting for numerous confounders (Kim et al., 2015a; Kim, Shiba, et al., 2020). Longitudinal evidence from another US cohort similarly found that optimism was linked to better self‐reported sleep quality across 5 years, but not objectively assessed sleep parameters (Hernandez et al., 2019).
Well‐being also shows longitudinal associations with physical activity, another health‐promoting behavior. In two different cohorts of older adults who engaged in physical activity at baseline, those with greater well‐being had approximately 20%–24% reduced risk of becoming sedentary across 8–11 years (Kim et al., 2017; Kim, Shiba, et al., 2020). Similarly, the most versus least optimistic postmenopausal women were 15% more likely to engage in vigorous physical activity, even when controlling for sociodemographic characteristics, health status, other health behaviors, and depression (Progovac, Donohue, et al., 2017).
Individuals with greater well‐being may also be more likely to use preventive health services that delay the onset of disease. For example, among adults over 50 years, both satisfaction and purpose were associated with increased use of cholesterol tests, colonoscopies, mammograms and pap smears for women, and prostate exams for men during 6 years of follow‐up (Kim et al., 2014, 2015b).
4.1.2. Well‐being's longitudinal association with deteriorative health behaviors
The most prominent deteriorative or health‐diminishing behavior relevant for CVD is cigarette smoking. Although cross‐sectional associations between well‐being and cigarette smoking are evident (e.g., Kelloniemi et al., 2005; Morimoto et al., 2018), longitudinal associations have not been reliably confirmed. For example, among older US adults, higher levels of baseline purpose in life were associated with reduced likelihood of cigarette smoking across 8 years in age‐adjusted analyses, but associations did not hold when other covariates were taken into account (Kim, Shiba, et al., 2020). Similarly, among older women smokers, age‐adjusted analyses showed only a modest association between optimism and smoking cessation during a 6‐year period; multivariable‐adjusted analyses showed no association (Progovac, Chang, et al., 2017). Other evidence from young Finnish adults showed that optimism was not associated with being a non‐smoker across 6 years; these findings rigorously controlled for baseline smoking status and pessimism (Serlachius et al., 2015). Thus, existing longitudinal evidence does not support a robust association between well‐being and cigarette smoking.
4.2. Well‐being's association with physiological function
Well‐being may be tied to physiological processes relevant to CVD such as autonomic cardiac control, lipids, atherosclerosis, inflammation, glucose regulation, and blood pressure (BP; Castelli et al., 1986; Chobanian et al., 2004; Herrington et al., 2016; Khaw et al., 2004; Pearson et al., 2003; Thayer & Lane, 2007). Although most of these processes are considered deteriorative such that the presence of higher levels may signal poor functioning, a few restorative indicators of physiological function such as heart rate variability and the previously mentioned HDL‐C also exist. Figure 1 posits that well‐being precedes more restorative physiological function and less deteriorative physiological function. Relevant evidence is reviewed in the next sections; due to a dearth of longitudinal findings, results from both cross‐sectional and longitudinal studies are included.
4.2.1. Well‐being's association with restorative physiological function
Although fewer restorative physiological processes have been identified relative to deteriorative processes (Kubzansky et al., 2015), existing evidence suggests possible links with well‐being. The restorative lipid of HDL‐C, which carries other cholesterols out of the bloodstream, has shown the most robust associations. For example, in a middle‐age cohort of US adults, greater optimism was cross‐sectionally associated with higher (i.e., healthier) levels of HDL‐C (Boehm et al., 2013). Using the same cohort and building on those findings, continuously high levels of eudaimonic well‐being across 9–10 years were also associated with high levels of HDL‐C (Radler et al., 2018). Finally, in a prospective longitudinal study of older adults in England, baseline well‐being was associated with healthier trajectories of HDL‐C over 9 years, controlling for multiple covariates (Soo et al., 2018). Thus, greater well‐being is linked with higher levels of HDL‐C.
Besides HDL‐C, well‐being may also foster enhanced regulation of the autonomic nervous system, which can be assessed via heart rate variability (HRV). Early work by Oveis et al. (2009) reported both positive emotions and optimism were positively associated with HRV in students (see also Geisler et al., 2010; Lü & Wang, 2018; Wang et al., 2013). Yet, neither positive emotions nor eudaimonic well‐being were related to HRV in a representative sample of nearly 1000 US adults (Sloan et al., 2017). In another study of more than 2500 women, HRV was tested as a potential pathway in optimism's relationship with heart disease. However, baseline optimism was not linked with HRV 3 years later and HRV did not attenuate optimism's association with heart disease, suggesting HRV may not mediate associations between well‐being and CVD (Salmoirago‐Blotcher et al., 2019). Certain conditions may explain inconsistent findings for well‐being's association with HRV. For example, a nonlinear relationship may exist such that moderate but not high levels of well‐being correlate with vagal tone (Duarte & Pinto‐Gouveia, 2017; Kogan et al., 2013). Moreover, distinct positive emotions (e.g., amusement, awe) and, more broadly, different indicators of well‐being may show different associations with vagal activity (Duarte & Pinto‐Gouveia, 2017; Shiota et al., 2011). Thus, more research is necessary before firm conclusions are drawn about well‐being's association with HRV.
4.2.2. Well‐being's association with deteriorative physiological function
Besides showing consistent relationships with the restorative lipid of HDL‐C, well‐being also appears to be associated with deteriorative lipids and other indicators of deteriorative physiology (i.e., those where lower levels indicate better health). For example, in middle‐age adults, greater optimism and eudaimonic well‐being were associated with lower (i.e., healthier) levels of triglycerides, but no associations were evident for LDL‐C (Boehm, Williams, et al., 2013; Radler, et al., 2018). In the related process of atherosclerosis (a pre‐disease indicator of CVD characterized by plaque buildup in the arteries; Folsom et al., 2008), cross‐sectional findings are somewhat mixed for an association with well‐being (Matthews, Owens, et al., 2006; Shahabi et al., 2016). However, longitudinal analyses found that relative to the less optimistic, the most optimistic middle‐age women showed less progression in carotid atherosclerosis across 3 years (Matthews, Raikkonen, Sutton‐Tyrrell, & Kuller, 2004).
Cross‐sectional studies have also reported associations between reduced inflammation and positive emotions (Ironson et al., 2018; Stellar et al., 2015; Steptoe et al., 2008), purpose in life (Steptoe & Fancourt, 2019), and optimism (Roy et al., 2010). Yet longitudinal studies provide conflicting evidence. In more than 300 older men, inflammatory markers were assessed up to four times across as many as 8 years (Ikeda et al., 2011). Optimistic men had lower baseline levels of interleukin‐6, but optimism was not associated with changes in inflammation over time. In another longitudinal study of older adults, greater initial well‐being was associated with lower levels of C‐reactive protein; furthermore, increases in well‐being over time were associated with decreases in C‐reactive protein levels over time (Okely et al., 2017). Finally, in nearly 9000 older English adults, hedonic well‐being, eudaimonic well‐being, and inflammatory markers were each assessed three times across 8 years (Fancourt & Steptoe, 2020). Increases in eudaimonic well‐being were related to lower levels of interleukin‐6, C‐reactive protein, and white blood cell count. Associations persisted when adjusting for distress but were attenuated when adjusting for chronic conditions, BMI, and cigarette smoking.
Well‐being has also been examined in relation to glucose regulation, which is measured via glycosylated hemoglobin (HbA1c), a marker of long‐term glucose control and a diagnostic criterion for type 2 diabetes. Although there are some null cross‐sectional findings for an association between well‐being and HbA1c (Ryff, Dienberg Love, et al., 2006), other cross‐sectional studies have reported inverse associations (Boylan et al., 2017; Tindle, Duncan, et al., 2018). In longitudinal work among older women without diabetes, higher levels of positive emotions—but not eudaimonic well‐being—were inversely associated with HbA1c 2 years later when controlling for baseline HbA1c (Tsenkova et al., 2007). However, in older adults who started another study without prediabetes or type 2 diabetes, those with high versus low levels of purpose in life had lower levels of HbA1c after 4 years (Hafez et al., 2018). Findings held when adjusting for sociodemographics, physical health and functioning, and depressive symptoms. Thus, well‐being may be linked with glucose regulation over time.
Somewhat more consistent associations are evident for well‐being and BP. A cross‐sectional study of older Mexican Americans indicated that higher versus lower levels of well‐being were associated with lower levels of systolic and diastolic BP (Ostir et al., 2006). Ikigai, a Japanese term related to purpose in life, was cross‐sectionally associated with lower levels of systolic BP in Japanese adults, but hedonic well‐being was not (Boylan et al., 2017). In a prospective study of British adults who were healthy at baseline, greater initial emotional vitality (a composite of energized and engaged positive emotions) was associated with reduced risk of incident hypertension across 12 years (Trudel‐Fitzgerald, Boehm, et al., 2014). Findings held when accounting for sociodemographic factors and health, but a single‐item measure of optimism was not associated with incident hypertension in the same cohort. Other research with a large cohort of US army members did find that baseline levels of optimism were associated with reduced risk of hypertension across an average of 3.5 years of follow‐up (Kubzansky, Boehm, Allen, et al., 2020).
4.3. Well‐being's association with stress buffering
Positive emotions and related markers of well‐being may be associated with reduced risk of CVD by buffering against stress and developing other psychosocial resources (shown in Figure 1 with the solid black lines pointing to and away from the yellow triangle). To start, the presence of well‐being may reduce perceptions or experiences of stress, which means less physiological activation that could harm the body (Folkman & Moskowitz, 2000; Pressman, et al., 2018). Furthermore, when stress is encountered, well‐being may facilitate more effective regulation or coping (Schaefer et al., 2013). For example, in one study of 200 stressed postdoctoral researchers, the relationship between positive emotions and resilience was partially mediated by adaptive coping responses such as positive reframing and planning (Gloria & Steinhardt, 2016). Moreover, a meta‐analysis showed that optimism was positively associated with approach‐oriented coping strategies that help to manage or reduce stressors (and associated emotions) as well as inversely associated with avoidance‐oriented coping strategies that tend to ignore stressors (Nes & Segerstrom, 2006). These approaches to coping may foster better adjustment to stress among those who initially have greater well‐being.
Furthermore, well‐being may foster an adaptive stress response by capitalizing on pre‐existing resources. The Broaden‐and‐Build Model posits that positive emotions build physical, intellectual, and social resources that can be used during challenging times (Fredrickson, 1998). Indeed, well‐being is intimately tied with social integration and supportive relationships (Diener, Seligman, et al., 2018; Feeney & Collins, 2015). In turn, social relationships are critical for health and longevity (Holt‐Lunstad et al., 2010). Thus, well‐being may foster other resources—including coping skills and social relationships—that may help people manage stress and reduce its harmful consequences on deteriorative health behaviors (e.g., sedentary behavior, overeating) and physiology (e.g., inflammation, BP).
Summary of findings for pathways linking well‐being and CVD
Overall, some research supports the idea that restorative and deteriorative behavioral and physiological processes, as well as stress buffering, may underlie well‐being's association with CVD. However, well‐being may not be related to all processes under consideration. For example, well‐being seems consistently related to indicators such as the restorative markers of healthy diet and HDL‐C, but the evidence is less robust or null for deteriorative processes such as cigarette smoking and LDL‐C.
Moreover, the evidence to date is characterized by several limitations. First, research findings come from predominantly cross‐sectional studies which do not allow for conclusions about temporal order or causality. This is particularly apparent when considering well‐being's association with physiological function as few longitudinal or experimental studies are available. Second, associations from observational studies may be subject to concerns about third variables that are not accounted for (e.g., people with restricted mobility may have limited access to fruits and vegetables because they cannot visit grocery stores easily). Third, many studies are characterized by small samples sizes and homogeneous participants (e.g., older, white individuals). Finally, in the case of health behaviors, both well‐being and the behaviors under investigation are most frequently self‐reported. This shared method may inflate associations, so objective measurements of health behaviors may yield more realistic associations. Research suggests objectively assessed physical activity is associated with life purpose in much the same way that self‐reported physical activity is (Hooker & Masters, 2016), but this may not be the case with all behaviors (e.g., sleep quality and duration; Hernandez, et al., 2019). On the whole, future research with well‐powered and diverse samples as well as prospective longitudinal designs are necessary.
5. EARLY‐LIFE CONSIDERATIONS FOR WELL‐BEING'S ASSOCIATION WITH CARDIOVASCULAR OUTCOMES
The overarching framework driving this paper (Figure 1) is expected to operate across the life course. Yet most of the cardiovascular‐related research discussed thus far has assessed adults in midlife as this is when diagnoses of CVD are likely to occur and overall health begins to decline. Although well‐being indicators such as optimism are tied to healthy aging (remaining free of chronic disease, memory impairment, and physical impairment) and exceptional longevity (living to 85 years or older; James et al., 2019; Kim, James, et al., 2019; Lee et al., 2019) in later life, by mid to late adulthood health‐related processes are often well‐entrenched and difficult to change. Thus, trajectories toward CVD and other chronic diseases are underway long before the second half of life, even as early as the fetal environment (Barker et al., 1993). Combined with recent trends showing that cardiovascular risk factors such as obesity are prevalent in youth (Shay et al., 2013), childhood is increasingly viewed as a key period for CVD prevention (Fernandez‐Jimenez et al., 2018; Steinberger et al., 2016; Weintraub et al., 2011).
Consequently, research is starting to look earlier in the lifespan to determine whether well‐being's association with cardiovascular‐related outcomes is apparent at younger ages. This parallels interest in adverse childhood experiences (Appleton, Holdsworth, et al., 2017; Bellis et al., 2019; Hughes et al., 2017) but asks not whether traumatic life experiences are detrimental to health, but rather whether protective factors such as well‐being can promote health. In other words, is youth a sensitive period during which individuals establish trajectories toward or away from CVD later in life? Preliminary evidence from children and adolescents suggests this may be the case. Cross‐sectional and longitudinal studies find that childhood well‐being is linked with subsequent healthy behavior including balanced diets, physical activity, and non‐smoking (Booker et al., 2014; Hoyt et al., 2012). Moreover, cross‐sectional studies of racially diverse adolescents showed that higher levels of optimism and other positive attributes were associated with healthier levels of cardiovascular‐relevant biomarkers such as HDL‐C, as well as composite measures of cardiometabolic health (Midei & Matthews, 2014; Oreskovic & Goodman, 2013).
Although most prospective longitudinal studies in youth have not specifically focused on well‐being, two are informative. In one, more than 3,000 English youth had their cardiometabolic health (defined by levels of lipids, BP, insulin resistance, C‐reactive protein, and BMI) assessed at 9 and 17 years old. Children with the most psychosocial assets (i.e., executive functioning, prosocial behaviors, and infrequent emotional or social problems) had the best cardiometabolic health when they were on the cusp of adulthood at age 17 (Qureshi et al., 2019). Similarly, children with the presence of three psychosocial assets (emotion regulation, cognitive ability, and positive home environment) had substantially higher odds of experiencing cardiometabolic health (i.e., being diabetes‐free and a non‐smoker, as well as having healthy levels of BP, total cholesterol, and BMI) in adulthood relative to individuals without any childhood assets (Appleton, Buka, et al., 2013). Thus, childhood psychosocial assets that are closely related to well‐being predict better health years later.
6. FUTURE RESEARCH QUESTIONS
Taken together, well‐being is prospectively linked with reduced risk of experiencing a cardiovascular event in people who are initially healthy. The association seems weaker (albeit still evident) among people already diagnosed with CVD. Proposed underlying pathways related to health behaviors, physiological function, and stress buffering have received some support but are characterized by relatively weak cross‐sectional evidence. As such, additional research with large and diverse cohorts that explicitly test the direction of effects between well‐being and underlying pathways as well as control for confounding variables is necessary.
There are also other questions to ask with regards to the potential pathways that might explain well‐being's association with CVD. For example, does well‐being have differential associations with the restorative versus deteriorative processes proposed as underlying pathways? In the case of restorative health behaviors, researchers posit that when positive emotions are associated with health‐promoting behaviors (e.g., physical activity), nonconscious motivations to engage in those behaviors are generated, which in turn support the growth of personal resources such as social connections (Van Cappellen et al., 2018). This may foster an upward spiral by which individuals are able to maintain restorative behaviors. Such mechanisms may not occur with health‐diminishing behaviors (e.g., cigarette smoking), reflecting their weaker associations with well‐being. Thus, it is feasible that well‐being's relationship with underlying pathways may be stronger for restorative versus deteriorative processes.
Another consideration for longitudinal investigations of health behaviors and potentially physiological function is how initial status should be taken into account. Baseline and subsequent assessments of behaviors and biomarkers could be strongly correlated, which may not leave much variance to be explained by well‐being. Furthermore, the distinction between the maintenance of health behaviors versus the initiation or decline of health behaviors may also matter for associations with well‐being. The likelihood of starting a behavior may have different correlates than the correlates of maintaining an existing behavior (Kim, Shiba, et al., 2020). Thus, how underlying behavioral and physiological processes are conceptualized in study designs may have important implications.
In addition, most studies have only investigated potential pathways in relation to well‐being without also considering cardiovascular‐related outcomes (cf. Salmoirago‐Blotcher, et al., 2019). Even when prospective studies of well‐being and CVD statistically adjust for potential pathway variables such as cigarette smoking, often those variables are assessed at baseline only (e.g., Tindle, Chang, et al., 2009). If well‐being and potential mechanisms are measured simultaneously, such timing cannot provide a strong test of underlying pathways. Thus, future work should consider possible mechanisms with data that has well‐being measured at baseline, CVD measured at a later point, and pathway‐related variables measured during an intermediary period. This may require data across several years or even decades but would provide greater understanding of the pathways linking well‐being with CVD.
It is not clear which indicator of well‐being matters most for cardiovascular‐related outcomes. Much work has capitalized on existing epidemiological cohorts and secondary data analyses, so researchers have been limited by the measures that were originally included. That is, the type of well‐being under investigation may have been less theoretically driven and more opportunistic, thereby prohibiting firm conclusions for one indicator or another. In addition, well‐being is typically measured via self‐report. Some of these self‐report measures show good psychometric properties (e.g., the widely used Satisfaction With Life Scale or Life Orientation Test‐Revised; Diener, Emmons, et al., 1985; Pavot & Diener, 2008; Scheier et al., 1994), but others have weaker or unknown psychometric properties (e.g., single items). Thus, it is unclear whether a lack of association for some well‐being indicators may be partially explained by poor or unavailable assessments. A key direction for future researchers is determining which specific indicator of well‐being is most pertinent for better cardiovascular outcomes. This would require adding well‐validated measures to epidemiological cohorts so that direct comparisons between associations of interest (e.g., optimism and CVD vs. life satisfaction and CVD) can be assessed.
The consistent evidence for well‐being's association with CVD in adulthood is also evident for pre‐disease indicators in youth. Thus, early life may be an essential period for cultivating well‐being and setting up healthy trajectories that endure across the lifespan. In particular, adolescence and young adulthood may be a prime candidate for establishing healthy trajectories because it is a period of increasing independence, cognitive capacity, and identity formation (Arnett, 2000; Geller & Boehm, 2020). What is not well understood, however, is how well‐being is initially developed across early life (Coffey, 2018; Luhmann, 2017; Renaud et al., 2019). Higher levels of well‐being in childhood establish optimal psychosocial functioning in adulthood (Coffey et al., 2015; Richards & Huppert, 2011), yet how do youth become more or less happy, satisfied, or optimistic? A portion of well‐being is heritable (Bartels, 2015; Carver & Scheier, 2014; Røysamb & Nes, 2018; Stubbe et al., 2005), but the social context is also relevant. For example, childhood attachment and relationships with caregivers may play a critical role either via the modeling of adaptive strategies or the presence of trust to explore one's world (Carver & Scheier, 2014; Coffey, 2018; Ek et al., 2004). Indeed, more parental warmth is related to greater optimism during adolescence (Yu et al., 2019). Socioeconomic status may also shape certain indicators of well‐being (Robb et al., 2009). In one study, lower socioeconomic status in childhood was associated with lower levels of optimism in adulthood (Heinonen et al., 2006). Relative to higher socioeconomic environments, lower socioeconomic environments may be characterized by stressful experiences that require greater vigilance, which in turn develop tendencies to expect the worse or evaluate experiences negatively (Gallo & Matthews, 2003; Heinonen, et al., 2006). Other adverse experiences may operate in similar ways (Sheikh et al., 2016). Determining the complex ways in which well‐being may give rise in early life is an area ripe for further investigation.
Well‐being is often conceptualized as a stable characteristic that does not change, but this is not the case when a broad view of the life course is taken (Lucas et al., 2008). Although the exact trajectory of well‐being from early life to later life is debated and large scale investigations of well‐being's trajectory during early childhood are non‐existent, most people report experiencing well‐being (Diener & Diener, 1996). A typical pattern is that levels of life satisfaction and positive emotions are relatively low during young adulthood, increase from middle age to early old age, and then diminish in the oldest old as individuals approach the end of life (Gerstorf et al., 2008; Hudson et al., 2019; Luhmann, 2017). These average trajectories are subject to individual variability too. In one study of more than 3,000 Germans who were repeatedly assessed across 17 years, nearly a quarter showed substantial change in life satisfaction (Fujita & Diener, 2005). Thus, although well‐being may be somewhat stable over time (Hudson, et al., 2019; Renaud, et al., 2019), it can change over the life course and in response to impactful life events such as unemployment or widowhood (Lucas et al., 2003, 2004, 2004).
Well‐being's malleability has led numerous researchers to develop experimental interventions to enhance well‐being. These interventions vary in participant characteristics, content, method of delivery, and duration. For example, most interventions have targeted university students or older individuals with chronic disease; fewer involve healthy youth or midlife to older adults. Some interventions focus on just one indicator of well‐being (e.g., optimism) in a single session whereas others target well‐being more generally in a variety of activities that take place across multiple sessions. Finally, some interventions are conducted online, whereas others are conducted in‐person either individually or in a group setting. Although well‐being interventions tend to be relatively brief, administered during a short period of time (4–12 weeks), and characterized by relatively small sample sizes, they have yielded small to moderate increases in well‐being when compared with control groups (Carrillo et al., 2019; Malouff & Schutte, 2017; Weiss et al., 2016; White et al., 2019).
However, whether or not these interventions have long‐term effects on well‐being or influence downstream health behaviors, physiology, or even CVD remains to be seen. Preliminary findings from small samples of individuals diagnosed with CVD indicate well‐being interventions may lead to greater physical activity (Duque et al., 2019; Huffman et al., 2019; Peterson et al., 2012), increased medication adherence (Ogedegbe et al., 2012), and reduced inflammation (Mohammadi et al., 2020; Nikrahan et al., 2016; Redwine et al., 2016). Moreover, one randomized control trial found that among approximately 100 community members (presumably free from CVD), a 12‐week well‐being intervention was associated not only with improvements in well‐being over time, but also significantly fewer self‐reported sick days relative to a waitlist control (Kushlev et al., 2020). Notably, however, effects were not evident for objective outcomes like BMI or blood pressure. Further intervention work would be bolstered by larger sample sizes and objectively assessed outcomes assessed across time.
Most studies assume that higher levels of well‐being are better for cardiovascular‐related outcomes. However, more is not always better and “the optimal levels of happiness are likely to depend on a person's resources, the challenges and dangers they face, the behavioral domain in question, and the type of well‐being under consideration” (Oishi et al., 2007, p. 358). Thus, it is important for both epidemiological and intervention studies to more thoroughly pinpoint what level of well‐being may have the most potent effects on CVD and if too much well‐being is detrimental. This may require moving beyond linear models to investigate non‐linear associations.
Just as certain levels of well‐being may not be optimal in all cases, well‐being may not be good for health in every context. For example, Japanese adults with high levels of positive emotions but low levels of social connectedness had unhealthy levels of HDL‐C (Yoo et al., 2016). By contrast, high levels of positive emotions in US adults were associated with healthy levels of HDL‐C, regardless of social connectedness. Thus, high levels of well‐being may conflict with cultural norms to maintain social harmony and cultural context may be an important moderating factor. Most research in this area has assessed predominantly White individuals from Western countries (cf. Sone et al., 2008), so well‐being's intricate relationships with health may not be fully specified and generalizability to other racial and ethnic backgrounds, regions of the world, and cultural backgrounds is limited. Given the important role that the social and physical environment plays in health outcomes (Diez Roux & Mair, 2010; Olvera Alvarez et al., 2018) as well as the social patterning of well‐being (Boehm et al., 2015), it will be important for future research to consider such factors.
7. CONCLUDING REMARKS
Positive psychological well‐being is consistently and independently associated with better health, particularly in the cardiovascular domain. The American Heart Association's encouragement to incorporate well‐being into cardiovascular‐related research has merit. However, high‐quality research that further explores underlying pathways and how associations operate across the lifespan (especially in childhood) and in different social contexts are needed for a more comprehensive understanding of well‐being's links with CVD. Such work may build on preliminary efforts to develop targeted well‐being interventions that bolster the restorative processes and minimize the deteriorative processes that contribute to the burden and expense of CVD.
ACKNOWLEDGMENT
This work was supported by American Heart Association grant #18AIREA33960394 to Julia K. Boehm.
Biography
Julia K. Boehm is an associate professor of Psychology at Chapman University. She received her PhD degree in psychology from the University of California, Riverside and was a postdoctoral fellow at Harvard T. H. Chan School of Public Health. Dr. Boehm's research examines whether positive psychological well‐being is associated with cardiovascular disease and related behavioral and biological processes. She has published extensive reviews on these topics in top psychology and cardiovascular journals including Psychological Bulletin, Journal of the American College of Cardiology, and Circulation Research. Her work has been funded by the National Institute on Aging and the American Heart Association.
REFERENCES
- Algoe, S. B. (2019). Positive interpersonal processes. Current Directions in Psychological Science, 28, 183–188. 10.1177/0963721419827272 [DOI] [Google Scholar]
- Alimujiang, A. , Wiensch, A. , Boss, J. , Fleischer, N. L. , Mondul, A. M. , McLean, K. , Mukherjee, B. , & Pearce, C. L. (2019). Association between life purpose and mortality among US adults older than 50 years. JAMA Network Open, 2, e194270. 10.1001/jamanetworkopen.2019.4270.e194270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angell, S. Y. , McConnell, M. V. , Anderson, C. A. M. , Bibbins‐Domingo, K. , Boyle, D. S. , Capewell, S. , Ezzati, M. , de Ferranti, S. , Gaskin, D. J. , Goetzel, R. Z. , Huffman, M. D. , Jones, M. , Khan, Y. M. , Kim, S. , Kumanyika, S. K. , McCray, A. T. , Merritt, R. K. , Milstein, B. , Mozaffarian, D. , … Warner, J. J. (2020). The American Heart Association 2030 impact goal: A presidential advisory from the American Heart Association. Circulation, 141, e120–e138. 10.1161/cir.0000000000000758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appleton, A. A. , Buka, S. L. , Loucks, E. B. , Rimm, E. B. , Martin, L. T. , & Kubzansky, L. D. (2013). A prospective study of positive early‐life psychosocial factors and favorable cardiovascular risk in adulthood. Circulation, 127, 905–912. 10.1161/circulationaha.112.115782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appleton, A. A. , Holdsworth, E. , Ryan, M. , & Tracy, M. (2017). Measuring childhood adversity in life course cardiovascular research: A systematic review. Psychosomatic Medicine, 79, 434–440. 10.1097/psy.0000000000000430 [DOI] [PubMed] [Google Scholar]
- Arnett, J. J. (2000). Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist, 55, 469–480. 10.1037/0003-066X.55.5.469 [DOI] [PubMed] [Google Scholar]
- Barker, D. J. P. , Godfrey, K. M. , Gluckman, P. D. , Harding, J. E. , Owens, J. A. , & Robinson, J. S. (1993). Fetal nutrition and cardiovascular disease in adult life. The Lancet, 341, 938–941. 10.1016/0140-6736(93)91224-a [DOI] [PubMed] [Google Scholar]
- Bartels, M. (2015). Genetics of wellbeing and its components satisfaction with life, happiness, and quality of life: A review and meta‐analysis of heritability studies. Behavior Genetics, 45, 137–156. 10.1007/s10519-015-9713-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bassett, S. M. , Schuette, S. A. , O'Dwyer, L. C. , & Moskowitz, J. T. (2019) Positive affect and medication adherence in chronic conditions: A systematic review. Health Psychology, 38, 960–974. 10.1037/hea0000778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellis, M. A. , Hughes, K. , Ford, K. , Ramos Rodriguez, G. , Sethi, D. , & Passmore, J. (2019) Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: A systematic review and meta‐analysis. The Lancet Public Health, 4, e517–e528. 10.1016/s2468-2667(19)30145-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boehm, J. K. , Chen, Y. , Koga, H. , Mathur, M. B. , Vie, L. L. , & Kubzansky, L. D. (2018). Is optimism Associated with Healthier cardiovascular‐related behavior? Circulation Research, 122, 1119–1134. 10.1161/circresaha.117.310828 [DOI] [PubMed] [Google Scholar]
- Boehm, J. K. , Chen, Y. , Williams, D. R. , Ryff, C. , & Kubzansky, L. D. (2015). Unequally distributed psychological assets: Are there social disparities in optimism, life satisfaction, and positive affect? PLoS One, 10, e0118066. 10.1371/journal.pone.0118066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boehm, J. K. , & Kubzansky, L. D. (2012). The heart's content: The association between positive psychological well‐being and cardiovascular health. Psychological Bulletin, 138, 655–691. 10.1037/a0027448 [DOI] [PubMed] [Google Scholar]
- Boehm, J. K. , Peterson, C. , Kivimaki, M. , & Kubzansky, L. D. (2011). Heart health when life is satisfying: Evidence from the Whitehall II cohort study. European Heart Journal, 32, 2672–2677. 10.1093/eurheartj/ehr203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boehm, J. K. , Soo, J. , Zevon, E. S. , Chen, Y. , Kim, E. S. , & Kubzansky, L. D. (2018b). Longitudinal associations between psychological well‐being and the consumption of fruits and vegetables. Health Psychology, 37, 959–967. 10.1037/hea0000643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boehm, J. K. , Vie, L. L. , & Kubzansky, L. D. (2012). The promise of well‐being interventions for improving health risk behaviors. Current Cardiovascular Risk Reports, 6, 511–519. 10.1007/s12170-012-0273-x [DOI] [Google Scholar]
- Boehm, J. K. , Williams, D. R. , Rimm, E. B. , Ryff, C. , & Kubzansky, L. D. (2013). Relation between optimism and lipids in midlife. The American Journal of Cardiology, 111, 1425–1431. 10.1016/j.amjcard.2013.01.292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booker, C. L. , Skew, A. J. , Sacker, A. , & Kelly, Y. J. (2014). Well‐being in Adolescence‐An Association with Health‐related behaviors. The Journal of Early Adolescence, 34, 518–538. 10.1177/0272431613501082 [DOI] [Google Scholar]
- Boylan, J. M. , Tsenkova, V. K. , Miyamoto, Y. , & Ryff, C. D. (2017). Psychological resources and glucoregulation in Japanese adults: Findings from MIDJA. Health Psychology, 36, 449–457. 10.1037/hea0000455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brummett, B. H. , Boyle, S. H. , Siegler, I. C. , Williams, R. B. , Mark, D. B. , & Barefoot, J. C. (2005). Ratings of positive and depressive emotion as predictors of mortality in coronary patients. International Journal of Cardiology, 100, 213–216. 10.1016/j.ijcard.2004.06.016 [DOI] [PubMed] [Google Scholar]
- Carrillo, A. , Rubio‐Aparicio, M. , Molinari, G. , Enrique, Á. , Sánchez‐Meca, J. , & Baños, R. M. (2019). Effects of the best possible self intervention: A systematic review and meta‐analysis. PLoS One, 14, e0222386. 10.1371/journal.pone.0222386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver, C. S. , & Scheier, M. F. (2014). Dispositional optimism. Trends in Cognitive Sciences, 18, 293–299. 10.1016/j.tics.2014.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver, C. S. , Scheier, M. F. , & Segerstrom, S. C. (2010). Optimism. Clinical Psychology Review, 30, 879–889. 10.1016/j.cpr.2010.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castelli, W. P. , Garrison, R. J. , Wilson, P. W. , Abbott, R. D. , Kalousdian, S. , & Kannel, W. B. (1986). Incidence of coronary Heart disease and lipoprotein cholesterol levels. Journal of the American Medical Association, 256, 2835–2838. 10.1001/jama.1986.03380200073024 [DOI] [PubMed] [Google Scholar]
- Chobanian, A. V. , Bakris, G. L. , Black, H. R. , Cushman, W. C. , Green, L. A. , Izzo, J. L., Jr , & Wright, J. T., Jr (2004). The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. U.S. Department of Health and Human Services. [DOI] [PubMed] [Google Scholar]
- Coffey, J. K. (2018). Positive psychology of infancy and early childhood. In Snyder C. R., Lopez S. J., Edwards L. M., & Marques S. C. (Eds.), The Oxford handbook of positive psychology (3rd ed.). Oxford University Press. [Google Scholar]
- Coffey, J. K. , Warren, M. T. , & Gottfried, A. W. (2015). Does infant happiness forecast adult life satisfaction? Examining subjective well‐being in the first quarter century of life. Journal of Happiness Studies, 16, 1401–1421. 10.1007/s10902-014-9556-x [DOI] [Google Scholar]
- Cohen, R. , Bavishi, C. , & Rozanski, A. (2016). Purpose in life and its relationship to All‐cause mortality and cardiovascular events. Psychosomatic Medicine, 78, 122–133. 10.1097/psy.0000000000000274 [DOI] [PubMed] [Google Scholar]
- Diener, E. , & Diener, C. (1996). Most people are happy. Psychological Science, 7, 181–185. 10.1111/j.1467-9280.1996.tb00354.x [DOI] [Google Scholar]
- Diener, E. , Emmons, R. A. , Larsen, R. J. , & Griffin, S. (1985). The satisfaction with life scale. Journal of Personality Assessment, 49, 71–75. 10.1207/s15327752jpa4901_13 [DOI] [PubMed] [Google Scholar]
- Diener, E. , Seligman, M. E. P. , Choi, H. , & Oishi, S. (2018). Happiest people revisited. Perspectives on Psychological Science, 13, 176–184. 10.1177/1745691617697077 [DOI] [PubMed] [Google Scholar]
- Diener, E. , Suh, E. M. , Lucas, R. E. , & Smith, H. L. (1999). Subjective well‐being: Three decades of progress. Psychological Bulletin, 125, 276–302. 10.1037/0033-2909.125.2.276 [DOI] [Google Scholar]
- Diez Roux, A. V. , & Mair, C. (2010). Neighborhoods and health. Annals of the New York Academy of Sciences, 1186, 125–145. 10.1111/j.1749-6632.2009.05333.x [DOI] [PubMed] [Google Scholar]
- Duarte, J. , & Pinto‐Gouveia, J. (2017). Positive affect and parasympathetic activity: Evidence for a quadratic relationship between feeling safe and content and heart rate variability. Psychiatry Research, 257, 284–289. 10.1016/j.psychres.2017.07.077 [DOI] [PubMed] [Google Scholar]
- DuBois, C. M. , Lopez, O. V. , Beale, E. E. , Healy, B. C. , Boehm, J. K. , & Huffman, J. C. (2015). Relationships between positive psychological constructs and health outcomes in patients with cardiovascular disease: A systematic review. International Journal of Cardiology, 195, 265–280. 10.1016/j.ijcard.2015.05.121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duque, L. , Brown, L. , Celano, C. M. , Healy, B. , & Huffman, J. C. (2019). Is it better to cultivate positive affect or optimism? Predicting improvements in medical adherence following a positive psychology intervention in patients with acute coronary syndrome. General Hospital Psychiatry, 61, 125. 10.1016/j.genhosppsych.2019.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ek, E. , Remes, J. , & Sovio, U. (2004). Social and developmental predictors of optimism from infancy to early adulthood. Social Indicators Research, 69, 219–242. 10.1023/b:soci.0000033591.80716.07 [DOI] [Google Scholar]
- Fancourt, D. , & Steptoe, A. (2020). The longitudinal relationship between changes in wellbeing and inflammatory markers: Are associations independent of depression? Brain, Behavior, and Immunity, 83, 146–152. 10.1016/j.bbi.2019.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feeney, B. C. , & Collins, N. L. (2015). A new look at social support. Personality and Social Psychology Review, 19, 113–147. 10.1177/1088868314544222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez‐Jimenez, R. , Al‐Kazaz, M. , Jaslow, R. , Carvajal, I. , & Fuster, V. (2018). Children present a window of opportunity for promoting Health. Journal of the American College of Cardiology, 72, 3310–3319. 10.1016/j.jacc.2018.10.031 [DOI] [PubMed] [Google Scholar]
- Folkman, S. , & Moskowitz, J. T. (2000). Positive affect and the other side of coping. American Psychologist, 55, 647–654. 10.1037//0003-066x.55.6.647 [DOI] [PubMed] [Google Scholar]
- Folsom, A. R. , Kronmal, R. A. , Detrano, R. C. , O'Leary, D. H. , Bild, D. E. , Bluemke, D. A. , & Burke, G. L. (2008). Coronary Artery calcification compared with carotid intima‐media thickness in the prediction of cardiovascular disease IncidenceThe Multi‐ethnic study of Atherosclerosis (MESA). Archives of Internal Medicine, 168, 1333–1339. 10.1001/archinte.168.12.1333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson, B. L. (1998). What good are positive emotions? Review of General Psychology, 2, 300–319. 10.1037/1089-2680.2.3.300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujita, F. , & Diener, E. (2005). Life satisfaction set point: Stability and change. Journal of Personality and Social Psychology, 88, 158–164. 10.1037/0022-3514.88.1.158 [DOI] [PubMed] [Google Scholar]
- Gallo, L. C. , & Matthews, K. A. (2003). Understanding the association between socioeconomic status and physical health: Do negative emotions play a role? Psychological Bulletin, 129, 10–51. 10.1037/0033-2909.129.1.10 [DOI] [PubMed] [Google Scholar]
- Geisler, F. C. M. , Vennewald, N. , Kubiak, T. , & Weber, H. (2010). The impact of heart rate variability on subjective well‐being is mediated by emotion regulation. Personality and Individual Differences, 49, 723–728. 10.1016/j.paid.2010.06.015 [DOI] [Google Scholar]
- Geller, M. B. , & Boehm, J. K. (2020). It's for their health: Encouraging autonomy during emerging adulthood. PsiChiJournal, 25, 54. 10.24839/2325-7342.JN25.1.54 [DOI] [Google Scholar]
- Gerstorf, D. , Ram, N. , Estabrook, R. , Schupp, J. , Wagner, G. G. , & Lindenberger, U. (2008). Life satisfaction shows terminal decline in old age: Longitudinal evidence from the German Socio‐Economic Panel Study (SOEP). Developmental Psychology, 44, 1148–1159. 10.1037/0012-1649.44.4.1148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gloria, C. T. , & Steinhardt, M. A. (2016). Relationships among positive emotions, coping, resilience and mental health. Stress and Health, 32, 145–156. 10.1002/smi.2589 [DOI] [PubMed] [Google Scholar]
- Hafez, D. , Heisler, M. , Choi, H. , Ankuda, C. K. , Winkelman, T. , & Kullgren, J. T. (2018). Association between purpose in life and glucose control among older adults. Annals of Behavioral Medicine, 52, 309–318. 10.1093/abm/kax012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinonen, K. , Raikkonen, K. , Matthews, K. A. , Scheier, M. F. , Raitakari, O. T. , Pulkki, L. , & Keltikangas‐Jarvinen, L. (2006). Socioeconomic status in childhood and adulthood: Associations with dispositional optimism and pessimism over a 21‐year follow‐up. Journal of Personality, 74, 1111–1126. 10.1111/j.1467-6494.2006.00404.x [DOI] [PubMed] [Google Scholar]
- Hernandez, R. , Vu, T.‐H. T. , Kershaw, K. N. , Boehm, J. K. , Kubzansky, L. D. , Carnethon, M. , Trudel‐Fitzgerald, C. , Knutson, K. L. , Colangelo, L. A. , & Liu, K. (2019). The association of optimism with sleep duration and quality: Findings from the coronary artery risk and development in young adults (CARDIA) study. Behavioral Medicine, 46, 100–111. 10.1080/08964289.2019.1575179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrington, W. , Lacey, B. , Sherliker, P. , Armitage, J. , & Lewington, S. (2016). Epidemiology of atherosclerosis and the potential to reduce the global burden of atherothrombotic disease. Circulation Research, 118, 535–546. 10.1161/circresaha.115.307611 [DOI] [PubMed] [Google Scholar]
- Holt‐Lunstad, J. , Smith, T. B. , & Layton, J. B. (2010). Social relationships and mortality risk: A meta‐analytic review. PLoS Medicine, 7, e1000316. 10.1371/journal.pmed.1000316.e1000316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooker, S. A. , & Masters, K. S. (2016). Purpose in life is associated with physical activity measured by accelerometer. Journal of Health Psychology, 21, 962–971. 10.1177/1359105314542822 [DOI] [PubMed] [Google Scholar]
- Hoyt, L. T. , Chase‐Lansdale, P. L. , McDade, T. W. , & Adam, E. K. (2012). Positive youth, healthy adults: Does positive well‐being in adolescence predict better perceived health and fewer risky health behaviors in young adulthood? Journal of Adolescent Health, 50, 66–73. 10.1016/j.jadohealth.2011.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson, N. W. , Lucas, R. E. , & Donnellan, M. B. (2019). The development of subjective well‐being across the lifespan. In McAdams D. P., Shiner R. L., & Tackett J. L. (Eds.), Handbook of personality development (pp. 503–517). The Guilford Press. [Google Scholar]
- Huffman, J. C. , Feig, E. H. , Millstein, R. A. , Freedman, M. , Healy, B. C. , Chung, W.‐J. , Amonoo, H. L. , Malloy, L. , Slawsby, E. , Januzzi, J. L. , & Celano, C. M. (2019). Usefulness of a positive psychology‐motivational interviewing Intervention to promote positive affect and physical activity after an acute coronary syndrome. The American Journal of Cardiology, 123, 1906–1914. 10.1016/j.amjcard.2019.03.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes, K. , Bellis, M. A. , Hardcastle, K. A. , Sethi, D. , Butchart, A. , Mikton, C. , … , Dunne, M. P. (2017). The effect of multiple adverse childhood experiences on health: A systematic review and meta‐analysis. The Lancet Public Health, 2, e356‐e366. 10.1016/s2468-2667(17)30118-4 [DOI] [PubMed] [Google Scholar]
- Ikeda, A. , Schwartz, J. , Peters, J. L. , Fang, S. , Spiro, A. , Sparrow, D. , Vokonas, P. , & Kubzansky, L. D. (2011). Optimism in relation to inflammation and endothelial dysfunction in older men. Psychosomatic Medicine, 73, 664–671. 10.1097/PSY.0b013e3182312497 [DOI] [PubMed] [Google Scholar]
- Ironson, G. , Banerjee, N. , Fitch, C. , & Krause, N. (2018). Positive emotional well‐being, health behaviors, and inflammation measured by C‐reactive protein. Social Science & Medicine, 197, 235–243. 10.1016/j.socscimed.2017.06.020 [DOI] [PubMed] [Google Scholar]
- James, P. , Kim, E. S. , Kubzansky, L. D. , Zevon, E. S. , Trudel‐Fitzgerald, C. , & Grodstein, F. (2019). Optimism and healthy aging in women. American Journal of Preventive Medicine, 56, 116–124. 10.1016/j.amepre.2018.07.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashdan, T. B. , Biswas‐Diener, R. , & King, L. A. (2008). Reconsidering happiness: The costs of distinguishing between hedonics and eudaimonia. The Journal of Positive Psychology, 3, 219–233. 10.1080/17439760802303044 [DOI] [Google Scholar]
- Kelloniemi, H. , Ek, E. , & Laitinen, J. (2005). Optimism, dietary habits, body mass index and smoking among young Finnish adults. Appetite, 45, 169–176. 10.1016/j.appet.2005.05.001 [DOI] [PubMed] [Google Scholar]
- Keyes, C. L. M. , Shmotkin, D. , & Ryff, C. D. (2002). Optimizing well‐being: The empirical encounter of two traditions. Journal of Personality and Social Psychology, 82, 1007–1022. 10.1037/0022-3514.82.6.1007 [DOI] [PubMed] [Google Scholar]
- Khaw, K.‐T. , Wareham, N. , Bingham, S. , Luben, R. , Welch, A. , & Day, N. (2004). Association of hemoglobin A1c with cardiovascular disease and mortality in adults: The European Prospective Investigation into Cancer in Norfolk. Annals of Internal Medicine, 141, 413–420. 10.7326/0003-4819-141-6-200409210-00006 [DOI] [PubMed] [Google Scholar]
- Kim, E. S. , Hershner, S. D. , & Strecher, V. J. (2015a). Purpose in life and incidence of sleep disturbances. Journal of Behavioral Medicine, 38, 590–597. 10.1007/s10865-015-9635-4 [DOI] [PubMed] [Google Scholar]
- Kim, E. S. , James, P. , Zevon, E. S. , Trudel‐Fitzgerald, C. , Kubzansky, L. D. , & Grodstein, F. (2019). Optimism and healthy aging in women and men. American Journal of Epidemiology, 188, 1084–1091. 10.1093/aje/kwz056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, E. S. , Kubzansky, L. D. , & Smith, J. (2015b). Life satisfaction and use of preventive health care services. Health Psychology, 34, 779–782. 10.1037/hea0000174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, E. S. , Kubzansky, L. D. , Soo, J. , & Boehm, J. K. (2017). Maintaining healthy behavior: A prospective study of psychological well‐being and physical activity. Annals of Behavioral Medicine, 51, 337–347. 10.1007/s12160-016-9856-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, E. S. , Shiba, K. , Boehm, J. K. , & Kubzansky, L. D. (2020). Sense of purpose in life and five health behaviors in older adults. Preventive Medicine, 139, 106172. 10.1016/j.ypmed.2020.106172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, E. S. , Strecher, V. J. , & Ryff, C. D. (2014). Purpose in life and use of preventive health care services. Proceedings of the National Academy of Sciences of the United States of America, 111, 16331–16336. 10.1073/pnas.1414826111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kogan, A. , Gruber, J. , Shallcross, A. J. , Ford, B. Q. , & Mauss, I. B. (2013). Too much of a good thing? Cardiac vagal tone's nonlinear relationship with well‐being. Emotion, 13, 599–604. 10.1037/a0032725 [DOI] [PubMed] [Google Scholar]
- Kubzansky, L. D. , Boehm, J. K. , Allen, A. R. , Vie, L. L. , Ho, T. E. , Trudel‐Fitzgerald, C. , Koga, H. K. , Scheier, L. M. , & Seligman, M. E. P. (2020). Optimism and risk of incident hypertension: A target for primordial prevention. Epidemiology and Psychiatric Sciences, 29, e157. 10.1017/s2045796020000621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubzansky, L. D. , Boehm, J. K. , & Segerstrom, S. C. (2015). Positive psychological functioning and the biology of health. Social and Personality Psychology Compass, 9, 645–660. 10.1111/spc3.12224 [DOI] [Google Scholar]
- Kubzansky, L. D. , Huffman, J. C. , Boehm, J. K. , Hernandez, R. , Kim, E. S. , Koga, H. K. , Feig, E. H. , Lloyd‐Jones, D. M. , Seligman, M. E. P. , & Labarthe, D. R. (2018). Positive psychological well‐being and cardiovascular disease. Journal of the American College of Cardiology, 72, 1382–1396. 10.1016/j.jacc.2018.07.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushlev, K. , Drummond, D. M. , & Diener, E. (2020a). Subjective well‐being and Health behaviors in 2.5 million Americans. Applied Psychology. Health and Well‐Being, 12, 166–187. 10.1111/aphw.12178 [DOI] [PubMed] [Google Scholar]
- Kushlev, K. , Heintzelman, S. J. , Lutes, L. D. , Wirtz, D. , Kanippayoor, J. M. , Leitner, D. , & Diener, E. (2020b). Does happiness improve health? Evidence from a randomized controlled trial. Psychological Science, 31, 807–821. 10.1177/0956797620919673 [DOI] [PubMed] [Google Scholar]
- Lee, L. O. , James, P. , Zevon, E. S. , Kim, E. S. , Trudel‐Fitzgerald, C. , Spiro, A., 3rd&, Kubzansky, L. D. , (2019). Optimism is associated with exceptional longevity in 2 epidemiologic cohorts of men and women. Proceedings of the National Academy of Sciences of the United States of America, 116, 18357–18362. 10.1073/pnas.1900712116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lü, W. , & Wang, Z. (2018). Associations between resting respiratory sinus arrhythmia, intraindividual reaction time variability, and trait positive affect. Emotion, 18, 834–841. 10.1037/emo0000392 [DOI] [PubMed] [Google Scholar]
- Lucas, R. E. , Clark, A. E. , Georgellis, Y. , & Diener, E. (2003). Reexamining adaptation and the set point model of happiness: Reactions to changes in marital status. Journal of Personality and Social Psychology, 84, 527–539. 10.1037/0022-3514.84.3.527 [DOI] [PubMed] [Google Scholar]
- Lucas, R. E. , Clark, A. E. , Georgellis, Y. , & Diener, E. (2004). Unemployment alters the set point for life satisfaction. Psychological Science, 15, 8–13. 10.1111/j.0963-7214.2004.01501002.x [DOI] [PubMed] [Google Scholar]
- Lucas, R. E. , Dyrenforth, P. S. , & Diener, E. (2008). Four myths about subjective well‐being. Social and Personality Psychology Compass, 2, 2001–2015. 10.1111/j.1751-9004.2008.00140.x [DOI] [Google Scholar]
- Luhmann, M. (2017). The development of subjective well‐being. In Specht J., & Specht J. (Eds.), Personality development across the lifespan (pp. 197–218). Elsevier Academic Press. [Google Scholar]
- Malouff, J. M. , & Schutte, N. S. (2017). Can psychological interventions increase optimism? A meta‐analysis. The Journal of Positive Psychology, 12, 594–604. 10.1080/17439760.2016.1221122 [DOI] [Google Scholar]
- Martín‐María, N. , Miret, M. , Caballero, F. F. , Rico‐Uribe, L. A. , Steptoe, A. , Chatterji, S. , & Ayuso‐Mateos, J. L. (2017). The impact of subjective well‐being on mortality: A meta‐analysis of longitudinal studies in the general population. Psychosomatic Medicine, 79, 565–575. 10.1097/psy.0000000000000444 [DOI] [PubMed] [Google Scholar]
- Matthews, K. A. , Owens, J. F. , Edmundowicz, D. , Lee, L. , & Kuller, L. H. (2006). Positive and negative attributes and risk for coronary and aortic calcification in healthy women. Psychosomatic Medicine, 68, 355–361. 10.1097/01.psy.0000221274.21709.d0 [DOI] [PubMed] [Google Scholar]
- Matthews, K. A. , Räikkönen, K. , Sutton‐Tyrrell, K. , & Kuller, L. H. (2004). Optimistic attitudes protect against progression of carotid atherosclerosis in healthy middle‐aged women. Psychosomatic Medicine, 66, 640–644. 10.1097/01.psy.0000139999.99756.a5 [DOI] [PubMed] [Google Scholar]
- McKnight, P. E. , & Kashdan, T. B. (2009). Purpose in life as a system that creates and sustains health and well‐being: An integrative, testable theory. Review of General Psychology, 13, 242–251. [Google Scholar]
- Midei, A. J. , & Matthews, K. A. (2014). Positive attributes protect adolescents from risk for the metabolic syndrome. Journal of Adolescent Health, 55, 678–683. 10.1016/j.jadohealth.2014.05.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohammadi, N. , Aghayousefi, A. , Nikrahan, G. R. , King, F. , Alipour, A. , Sadeghi, M. , Roohafza, H. , Celano, C. M. , Gomez, P. R. , & Huffman, J. C. (2020). The impact of an optimism training intervention on biological measures associated with cardiovascular health: Data from a randomized controlled trial. Psychosomatic Medicine, 82, 634–640. 10.1097/psy.0000000000000834 [DOI] [PubMed] [Google Scholar]
- Morimoto, Y. , Yamasaki, S. , Ando, S. , Koike, S. , Fujikawa, S. , Kanata, S. , Endo, K. , Nakanishi, M. , Hatch, S. L. , Richards, M. , Kasai, K. , Hiraiwa‐Hasegawa, M. , & Nishida, A. (2018). Purpose in life and tobacco use among community‐dwelling mothers of early adolescents. BMJ Open, 8, e020586. 10.1136/bmjopen-2017-020586.e020586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nes, L. S. , & Segerstrom, S. C. (2006). Dispositional optimism and coping: A meta‐analytic review. Personality and Social Psychology Review, 10, 235–251. 10.1207/s15327957pspr1003_3 [DOI] [PubMed] [Google Scholar]
- Nikrahan, G. R. , Laferton, J. A. C. , Asgari, K. , Kalantari, M. , Abedi, M. R. , Etesampour, A. , Rezaei, A. , Suarez, L. , & Huffman, J. C. (2016). Effects of positive psychology interventions on risk biomarkers in coronary patients: A randomized, wait‐list controlled pilot trial. Psychosomatics, 57, 359–368. 10.1016/j.psym.2016.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogedegbe, G. O. , Boutin‐Foster, C. , Wells, M. T. , Allegrante, J. P. , Isen, A. M. , Jobe, J. B. , & Charlson, M. E. (2012). A randomized controlled trial of positive‐affect intervention and medication adherence in hypertensive African Americans. Archives of Internal Medicine, 172, 322–326. 10.1001/archinternmed.2011.1307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oishi, S. , Diener, E. , & Lucas, R. E. (2007). The optimum level of well‐being: Can people be too happy? Perspectives on Psychological Science, 2, 346–360. 10.1111/j.1745-6916.2007.00048.x [DOI] [PubMed] [Google Scholar]
- Okely, J. A. , Weiss, A. , & Gale, C. R. (2017). Well‐being and arthritis incidence: The role of inflammatory mechanisms. Findings from the English Longitudinal Study of Ageing. Psychosomatic Medicine, 79, 742–748. 10.1097/psy.0000000000000480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olvera Alvarez, H. A. , Appleton, A. A. , Fuller, C. H. , Belcourt, A. , & Kubzansky, L. D. (2018). An integrated socio‐environmental model of health and well‐being: A conceptual framework exploring the joint contribution of environmental and social exposures to health and disease over the life span. Current Environmental Health Reports, 5, 233–243. 10.1007/s40572-018-0191-2 [DOI] [PubMed] [Google Scholar]
- Ong, A. D. , Kim, S. , Young, S. , & Steptoe, A. (2017). Positive affect and sleep: A systematic review. Sleep Medicine Reviews, 35, 21–32. 10.1016/j.smrv.2016.07.006 [DOI] [PubMed] [Google Scholar]
- Oreskovic, N. M. , & Goodman, E. (2013). Association of optimism with cardiometabolic risk in adolescents. Journal of Adolescent Health, 52, 407–412. 10.1016/j.jadohealth.2012.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostir, G. V. , Berges, I. M. , Markides, K. S. , & Ottenbacher, K. J. (2006). Hypertension in older adults and the role of positive emotions. Psychosomatic Medicine, 68, 727–733. 10.1097/01.psy.0000234028.93346.38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oveis, C. , Cohen, A. B. , Gruber, J. , Shiota, M. N. , Haidt, J. , & Keltner, D. (2009). Resting respiratory sinus arrhythmia is associated with tonic positive emotionality. Emotion, 9, 265–270. 10.1037/a0015383 [DOI] [PubMed] [Google Scholar]
- Pavot, W. , & Diener, E. (2008). The Satisfaction with Life Scale and the emerging construct of life satisfaction. The Journal of Positive Psychology, 3, 137–152. 10.1080/17439760701756946 [DOI] [Google Scholar]
- Pearson, T. A. , Mensah, G. A. , Alexander, R. W. , Anderson, J. L. , Cannon, R. O., 3rd , Criqui, M. , Fadl, Y. Y. , Fortmann, S. P. , Hong, Y. , Myers, G. L. , Rifai, N. , Smith, S. C. , Taubert, K. , Tracy, R. P. , & Vinicor, F. (2003). Markers of inflammation and cardiovascular disease. Circulation, 107, 499–511. 10.1161/01.cir.0000052939.59093.45 [DOI] [PubMed] [Google Scholar]
- Peterson, J. C. , Charlson, M. E. , Hoffman, Z. , Wells, M. T. , Wong, S. C. , Hollenberg, J. P. , & Allegrante, J. P. (2012). A randomized controlled trial of positive‐affect induction to promote physical activity after percutaneous coronary intervention. Archives of Internal Medicine, 172, 329–336. 10.1001/archinternmed.2011.1311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pressman, S. D. , Jenkins, B. N. , & Moskowitz, J. T. (2019). Positive affect and health: What do we know and where next should we go? Annual Review of Psychology, 70, 627. 10.1146/annurev-psych-010418-102955 [DOI] [PubMed] [Google Scholar]
- Progovac, A. M. , Chang, Y.‐F. , Chang, C.‐C. H. , Matthews, K. A. , Donohue, J. M. , Scheier, M. F. , Habermann, E. B. , Kuller, L. H. , Goveas, J. S. , Chapman, B. P. , Duberstein, P. R. , Messina, C. R. , Weaver, K. E. , Saquib, N. , Wallace, R. B. , Kaplan, R. C. , Calhoun, D. , Smith, J. C. , & Tindle, H. A. (2017a). Are optimism and cynical hostility associated with smoking cessation in older women? Annals of Behavioral Medicine, 51, 500–510. 10.1007/s12160-016-9873-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Progovac, A. M. , Donohue, J. M. , Matthews, K. A. , Chang, C.‐C. H. , Habermann, E. B. , Kuller, L. H. , Saquib, J. , LaMonte, M. J. , Salmoirago‐Blotcher, E. , Zaslavsky, O. , & Tindle, H. A. (2017b). Optimism predicts sustained vigorous physical activity in postmenopausal women. Preventive Medicine Reports, 8, 286–293. 10.1016/j.pmedr.2017.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qureshi, F. , Koenen, K. C. , Tiemeier, H. , Williams, M. A. , Misra, S. , & Kubzansky, L. D. (2019). Childhood assets and cardiometabolic health in adolescence. Pediatrics, 143, e20182004. 10.1542/peds.2018-2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radler, B. T. , Rigotti, A. , & Ryff, C. D. (2018). Persistently high psychological well‐being predicts better HDL cholesterol and triglyceride levels: Findings from the midlife in the U.S. (MIDUS) longitudinal study. Lipids in Health and Disease, 17, 1. 10.1186/s12944-017-0646-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redwine, L. S. , Henry, B. L. , Pung, M. A. , Wilson, K. , Chinh, K. , Knight, B. , Jain, S. , Rutledge, T. , Greenberg, B. , Maisel, A. , & Mills, P. J. (2016). Pilot randomized study of a gratitude journaling intervention on heart rate variability and inflammatory biomarkers in patients with stage B heart failure. Psychosomatic Medicine, 78, 667–676. 10.1097/psy.0000000000000316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renaud, J. , Barker, E. T. , Hendricks, C. , Putnick, D. L. , & Bornstein, M. H. (2019). The developmental origins and future implications of dispositional optimism in the transition to adulthood. International Journal of Behavioral Development, 43, 221–230. 10.1177/0165025418820629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards, M. , & Huppert, F. A. (2011). Do positive children become positive adults? Evidence from a longitudinal birth cohort study. The Journal of Positive Psychology, 6, 75–87. 10.1080/17439760.2011.536655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robb, K. A. , Simon, A. E. , & Wardle, J. (2009). Socioeconomic disparities in optimism and pessimism. International Journal of Behavioral Medicine, 16, 331–338. 10.1007/s12529-008-9018-0 [DOI] [PubMed] [Google Scholar]
- Robles, T. F. , & Carroll, J. E. (2011). Restorative biological processes and health. Social and Personality Psychology Compass, 5, 518–537. 10.1111/j.1751-9004.2011.00368.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy, B. , Diez‐Roux, A. V. , Seeman, T. , Ranjit, N. , Shea, S. , & Cushman, M. (2010). Association of optimism and pessimism with inflammation and hemostasis in the Multi‐Ethnic Study of Atherosclerosis (MESA). Psychosomatic Medicine, 72, 134–140. 10.1097/PSY.0b013e3181cb981b [DOI] [PMC free article] [PubMed] [Google Scholar]
- Røysamb, E. , & Nes, R. B. (2018). The genetics of well‐being. In Diener E., Oishi S., & Tay L. (Eds.), Handbook of well‐being. DEF Publishers. [Google Scholar]
- Rozanski, A. , Bavishi, C. , Kubzansky, L. D. , & Cohen, R. (2019). Association of optimism with cardiovascular events and All‐cause mortality. JAMA Network Open, 2, e1912200. 10.1001/jamanetworkopen.2019.12200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan, R. M. , & Deci, E. L. (2001). On happiness and human potentials: A review of research on hedonic and eudaimonic well‐being. Annual Review of Psychology, 52, 141–166. 10.1146/annurev.psych.52.1.141 [DOI] [PubMed] [Google Scholar]
- Ryff, C. D. , Boylan, J. M. , & Kirsch, J. A. (2020). Disagreement about recommendations for measurement of well‐being. Preventive Medicine, 139, 106049. 10.1016/j.ypmed.2020.106049 [DOI] [PubMed] [Google Scholar]
- Ryff, C. D. , Dienberg Love, G. , Urry, H. L. , Muller, D. , Rosenkranz, M. A. , Friedman, E. M. , Davidson, R. J. , & Singer, B. (2006). Psychological well‐being and ill‐being: Do they have distinct or mirrored biological correlates? Psychotherapy and Psychosomatics, 75, 85–95. 10.1159/000090892 [DOI] [PubMed] [Google Scholar]
- Salmoirago‐Blotcher, E. , Hovey, K. M. , Andrews, C. A. , Allison, M. , Brunner, R. L. , Denburg, N. L. , Eaton, C. , Garcia, L. , Sealy‐Jefferson, S. M. , Zaslavsky, O. , Kang, J. , López, L. , Post, S. G. , Tindle, H. , & Wassertheil‐Smoller, S. (2019). Psychological traits, heart rate variability, and risk of coronary heart disease in healthy aging women‐The Women's Health Initiative. Psychosomatic Medicine, 81, 256–264. 10.1097/psy.0000000000000672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaefer, S. M. , Morozink Boylan, J. , van Reekum, C. M. , Lapate, R. C. , Norris, C. J. , Ryff, C. D. , & Davidson, R. J. (2013). Purpose in life predicts better emotional recovery from negative stimuli. PLoS One, 8, e80329. 10.1371/journal.pone.0080329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheier, M. F. , Carver, C. S. , & Bridges, M. W. (1994). Distinguishing optimism from neuroticism (and trait anxiety, self‐mastery, and self‐esteem): A reevaluation of the life orientation test. Journal of Personality and Social Psychology, 67, 1063–1078. 10.1037//0022-3514.67.6.1063 [DOI] [PubMed] [Google Scholar]
- Serlachius, A. , Pulkki‐Råback, L. , Elovainio, M. , Hintsanen, M. , Mikkilä, V. , Laitinen, T. T. , Jokela, M. , Rosenström, T. , Josefsson, K. , Juonala, M. , Lehtimäki, T. , Raitakari, O. , & Keltikangas‐Järvinen, L. (2015). Is dispositional optimism or dispositional pessimism predictive of ideal cardiovascular health? The young Finns study. Psychology and Health, 30, 1221–1239. 10.1080/08870446.2015.1041394 [DOI] [PubMed] [Google Scholar]
- Shahabi, L. , Karavolos, K. , Everson‐Rose, S. A. , Lewis, T. T. , Matthews, K. A. , Sutton‐Tyrrell, K. , & Powell, L. H. (2016). Associations of psychological well‐being with carotid intima media thickness in African American and white middle‐aged women. Psychosomatic Medicine, 78, 511–519. 10.1097/psy.0000000000000293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shay, C. M. , Ning, H. , Daniels, S. R. , Rooks, C. R. , Gidding, S. S. , & Lloyd‐Jones, D. M. (2013). Status of cardiovascular Health in US Adolescents. Circulation, 127, 1369–1376. 10.1161/CIRCULATIONAHA.113.001559 [DOI] [PubMed] [Google Scholar]
- Sheikh, M. A. , Abelsen, B. , & Olsen, J. A. (2016). Clarifying associations between childhood adversity, social support, behavioral factors, and mental health, health, and well‐being in adulthood: A population‐based study. Frontiers in Psychology, 7, 727. 10.3389/fpsyg.2016.00727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiota, M. N. , Neufeld, S. L. , Yeung, W. H. , Moser, S. E. , & Perea, E. F. (2011). Feeling good: Autonomic nervous system responding in five positive emotions. Emotion, 11, 1368–1378. 10.1037/a0024278 [DOI] [PubMed] [Google Scholar]
- Sloan, R. P. , Schwarz, E. , McKinley, P. S. , Weinstein, M. , Love, G. , Ryff, C. , Mroczek, D. , Choo, T.‐H. , Lee, S. , & Seeman, T. (2017). Vagally‐mediated heart rate variability and indices of well‐being: Results of a nationally representative study. Health Psychology, 36, 73–81. 10.1037/hea0000397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sone, T. , Nakaya, N. , Ohmori, K. , Shimazu, T. , Higashiguchi, M. , Kakizaki, M. , Kikuchi, N. , Kuriyama, S. , & Tsuji, I. (2008). Sense of life worth living (ikigai) and mortality in Japan: Ohsaki Study. Psychosomatic Medicine, 70, 709–715. 10.1097/PSY.0b013e31817e7e64 [DOI] [PubMed] [Google Scholar]
- Soo, J. , Kubzansky, L. D. , Chen, Y. , Zevon, E. S. , & Boehm, J. K. (2018). Psychological well‐being and restorative biological processes: HDL‐C in older English adults. Social Science & Medicine, 209, 59–66. 10.1016/j.socscimed.2018.05.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberger, J. , Daniels, S. R. , Hagberg, N. , Isasi, C. R. , Kelly, A. S. , Lloyd‐Jones, D. , Pate, R. R. , Pratt, C. , Shay, C. M. , Towbin, J. A. , Urbina, E. , Van Horn, L. V. , & Zachariah, J. P. (2016). Cardiovascular health promotion in children: Challenges and opportunities for 2020 and beyond: A scientific statement from the American Heart Association. Circulation, 134, e236–255. 10.1161/cir.0000000000000441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stellar, J. E. , John‐Henderson, N. , Anderson, C. L. , Gordon, A. M. , McNeil, G. D. , & Keltner, D. (2015). Positive affect and markers of inflammation: Discrete positive emotions predict lower levels of inflammatory cytokines. Emotion, 15, 129–133. 10.1037/emo0000033 [DOI] [PubMed] [Google Scholar]
- Steptoe, A. (2019). Happiness and health. Annual Review of Public Health, 40, 339–359. 10.1146/annurev-publhealth-040218-044150 [DOI] [PubMed] [Google Scholar]
- Steptoe, A. , & Fancourt, D. (2019). Leading a meaningful life at older ages and its relationship with social engagement, prosperity, health, biology, and time use. Proceedings of the National Academy of Sciences of the United States of America, 116, 1207–1212. 10.1073/pnas.1814723116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe, A. , O'Donnell, K. , Badrick, E. , Kumari, M. , & Marmot, M. (2008). Neuroendocrine and inflammatory factors associated with positive affect in healthy men and women: The Whitehall II study. American Journal of Epidemiology, 167, 96–102. 10.1093/aje/kwm252 [DOI] [PubMed] [Google Scholar]
- Stubbe, J. H. , Posthuma, D. , Boomsma, D. I. , & De Geus, E. J. C. (2005). Heritability of life satisfaction in adults: A twin‐family study. Psychological Medicine, 35, 1581–1588. 10.1017/S0033291705005374 [DOI] [PubMed] [Google Scholar]
- Suls, J. (2018). Toxic affect: Are anger, anxiety, and depression independent risk factors for cardiovascular disease? Emotion Review, 10, 6–17. 10.1177/1754073917692863 [DOI] [Google Scholar]
- Thayer, J. F. , & Lane, R. D. (2007). The role of vagal function in the risk for cardiovascular disease and mortality. Biological Psychology, 74, 224–242. 10.1016/j.biopsycho.2005.11.013 [DOI] [PubMed] [Google Scholar]
- Tindle, H. A. , Chang, Y.‐F. , Kuller, L. H. , Manson, J. E. , Robinson, J. G. , Rosal, M. C. , Siegle, G. J. , & Matthews, K. A. (2009). Optimism, cynical hostility, and incident coronary heart disease and mortality in the Women's Health Initiative. Circulation, 120, 656–662. 10.1161/CIRCULATIONAHA.108.827642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tindle, H. A. , Duncan, M. S. , Liu, S. , Kuller, L. H. , Fugate Woods, N. , Rapp, S. R. , Kroenke, C. H. , Coday, M. , Loucks, E. B. , Lamonte, M. J. , Progovac, A. M. , Salmoirago‐Blotcher, E. , Walitt, B. T. , Yuo, N.‐C. Y. , & Freiberg, M. S. (2018). Optimism, pessimism, cynical hostility, and biomarkers of metabolic function in the Women's Health Initiative. Journal of Diabetes, 10, 512–523. 10.1111/1753-0407.12584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trudel‐Fitzgerald, C. , Boehm, J. K. , Kivimaki, M. , & Kubzansky, L. D. (2014). Taking the tension out of hypertension. Journal of Hypertension, 32, 1222–1228. 10.1097/hjh.0000000000000175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trudel‐Fitzgerald, C. , James, P. , Kim, E. S. , Zevon, E. S. , Grodstein, F. , & Kubzansky, L. D. (2019). Prospective associations of happiness and optimism with lifestyle over up to two decades. Preventive Medicine, 126, 105754. 10.1016/j.ypmed.2019.105754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsenkova, V. K. , Love, G. D. , Singer, B. H. , & Ryff, C. D. (2007). Socioeconomic status and psychological well‐being predict cross‐time change in glycosylated hemoglobin in older women without diabetes. Psychosomatic Medicine, 69, 777–784. 10.1097/PSY.0b013e318157466f [DOI] [PubMed] [Google Scholar]
- Van Cappellen, P. , Rice, E. L. , Catalino, L. I. , & Fredrickson, B. L. (2018). Positive affective processes underlie positive health behaviour change. Psychology and Health, 33, 77–97. 10.1080/08870446.2017.1320798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Montfort, E. , Denollet, J. , Widdershoven, J. , & Kupper, N. (2016). Interrelation and independence of positive and negative psychological constructs in predicting general treatment adherence in coronary artery patients ‐ results from the THORESCI study. Journal of Psychosomatic Research, 88, 1–7. 10.1016/j.jpsychores.2016.06.009 [DOI] [PubMed] [Google Scholar]
- VanderWeele, T. J. , Trudel‐Fitzgerald, C. , Allin, P. , Farrelly, C. , Fletcher, G. , Frederick, D. E. , Hall, J. , Helliwell, J. F. , Kim, E. S. , Lauinger, W. A. , Lee, M. T. , Lyubomirsky, S. , Margolis, S. , McNeely, E. , Messer, N. , Tay, L. , Viswanath, V. , Węziak‐Białowolska, D. , & Kubzansky, L. D. (2020). Current recommendations on the selection of measures for well‐being. Preventive Medicine, 133, 106004. 10.1016/j.ypmed.2020.106004 [DOI] [PubMed] [Google Scholar]
- Virani, S. S. , Alonso, A. , Benjamin, E. J. , Bittencourt, M. S. , Callaway, C. W. , Carson, A. P. , Chamberlain, A. M. , Chang, A. R. , Cheng, S. , Delling, F. N. , Djousse, L. , Elkind, M. S. V. , Ferguson, J. F. , Fornage, M. , Khan, S. S. , Kissela, B. M. , Knutson, K. L. , Kwan, T. W. , Lackland, D. T. , Lewis, T. T. , Lichtman, J. H. , Longenecker, C. T. , Loop, M. S. , Lutsey, P. L. , Martin, S. S. , Matsushita, K. , Moran, A. E. , Mussolino, M. E. , Perak, A. M. , Rosamond, W. D. , Roth, G. A. , Sampson, U. K. A. , Satou, G. M. , Schroeder, E. B. , Shah, S. H. , Shay, C. M. , Spartano, N. L. , Stokes, A. , Tirschwell, D. L. , VanWagner, L. B. , & Tsao, C. W. (2020). Heart disease and stroke statistics‐2020 update: A report from the American Heart Association. Circulation, 141, e139–e596. 10.1161/cir.0000000000000757 [DOI] [PubMed] [Google Scholar]
- Walsh, L. C. , Boehm, J. K. , & Lyubomirsky, S. (2018). Does happiness promote career success? Revisiting the evidence. Journal of Career Assessment, 26, 199–219. 10.1177/1069072717751441 [DOI] [Google Scholar]
- Wang, Z. , Lü, W. , & Qin, R. (2013). Respiratory sinus arrhythmia is associated with trait positive affect and positive emotional expressivity. Biological Psychology, 93, 190–196. 10.1016/j.biopsycho.2012.12.006 [DOI] [PubMed] [Google Scholar]
- Weintraub, W. S. , Daniels, S. R. , Burke, L. E. , Franklin, B. A. , Goff, D. C., Jr , Hayman, L. L. , Lloyd‐Jones, D. , Pandey, D. K. , Sanchez, E. J. , Schram, A. P. , & Whitsel, L. P. (2011). Value of primordial and primary prevention for cardiovascular disease. Circulation, 124, 967–990. 10.1161/CIR.0b013e3182285a81 [DOI] [PubMed] [Google Scholar]
- Weiss, L. A. , Westerhof, G. J. , & Bohlmeijer, E. T. (2016). Can we increase psychological well‐being? The effects of interventions on psychological well‐being: A meta‐analysis of randomized controlled trials. PLoS One, 11, e0158092. 10.1371/journal.pone.0158092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White, C. A. , Uttl, B. , & Holder, M. D. (2019). Meta‐analyses of positive psychology interventions: The effects are much smaller than previously reported. PLoS One, 14, e0216588. 10.1371/journal.pone.0216588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo, J. , Miyamoto, Y. , & Ryff, C. D. (2016). Positive affect, social connectedness, and healthy biomarkers in Japan and the U.S. Emotion, 16, 1137–1146. 10.1037/emo0000200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu, J. , Putnick, D. L. , Hendricks, C. , & Bornstein, M. H. (2019). Long‐term effects of parenting and adolescent self‐competence for the development of optimism and neuroticism. Journal of Youth and Adolescence, 48, 1544–1554. 10.1007/s10964-018-0980-9 [DOI] [PMC free article] [PubMed] [Google Scholar]


