Abstract
A careful history and evaluation of men with chronic orchialgia elucidates the aetiology in some men to be a hyperactive cremaster muscle reflex with testicular retraction as the cause. The objective is to evaluate outcomes in men who underwent microsurgical subinguinal cremaster muscle release (MSCMR) with a retrospective chart review between September 2011 and April 2019. Nineteen men with hyperactive cremaster muscle reflex in 25 spermatic cord units underwent MSCMR, six bilateral and thirteen unilateral. Candidacy for MSCMR included answering yes to the question: “at times of testicular pain, does the testicle retract up in the groin to the extent that you have to milk it back down to the scrotum?”, normal digital rectal examinations, negative urinalyses, negative scrotal Doppler ultrasounds, vigorous retraction of testis with Valsalva on examination and pain without an anatomic or pathologically identifiable aetiology except testicular retraction. Of the men who underwent MSCMR, 100% (25/25) of spermatic cord units had resolution of testicular retraction and 92% (23/25) of spermatic cord units had complete resolution of orchialgia. There was one complication, a small scrotal hematoma which resolved. MSCMR is an effective option for men with orchialgia secondary to testicular retraction due to a hyperactive cremaster muscle reflex.
Keywords: cremaster muscle release, orchialgia, testicular retraction
1. INTRODUCTION
Chronic orchialgia, defined as unilateral or bilateral scrotal pain lasting at least 3 months in duration, is one of the most common complaints seen in the urologist's office and continues to be a challenging entity to diagnose and to treat (Costabile, Hahn, & McLeod, 1991; Davis, Noble, Weigel, Foret, & Mebust, 1990). Identifiable aetiologies for orchialgia must be ruled out and treated when they are present. A thorough evaluation for aetiologies should include a thorough history, genital examination, digital rectal examination, scrotal Doppler ultrasound and urinalysis. Testicular retraction to the external inguinal ring is an underdiagnosed aetiology of orchialgia which may be directly treated. A previous clinical option for this dilemma was scrotal orchiopexy; however, this often resulted in continuation of orchialgia with testicular retraction due to the hyperactive cremaster muscle while pulling the scrotum anchored to the inferior pole of the testis upwards with the testis with retraction. Our goal was to assess the clinical response and complications of microsurgical subinguinal cremaster muscle release (MSCMR) for orchialgia secondary to hyperactive cremaster muscle reflex resulting in testicular retraction.
2. MATERIALS AND METHODS
After institutional review board exemption was obtained, a retrospective chart review was performed to assess the outcomes and complications of men who underwent MSCMR by a single microsurgeon between September 2011 and April 2019.
Microsurgical subinguinal cremaster muscle release was performed by making a 1.5‐cm, transverse, subinguinal incision overlying the external inguinal ring, dissecting through the subcutaneous tissues, incising Scarpa's fascia and isolating spermatic cord. Then, under microsurgical magnified visualisation, the cremaster muscle was divided circumferentially with electrocautery, leaving all veins, nerves, gonadal arteries, lymphatics and the vas deferens intact. Great care was taken to divide all muscle fibres of the cremaster muscle circumferentially under microsurgical visualisation, as leaving some muscle fibres intact may result in failure and continued retraction (Figure 1). Upon completion of division of the cremaster fibres, the spermatic cord was dropped back into the anatomic position and the incision was closed in layers. Results are presented as means ± standard deviations.
Figure 1.
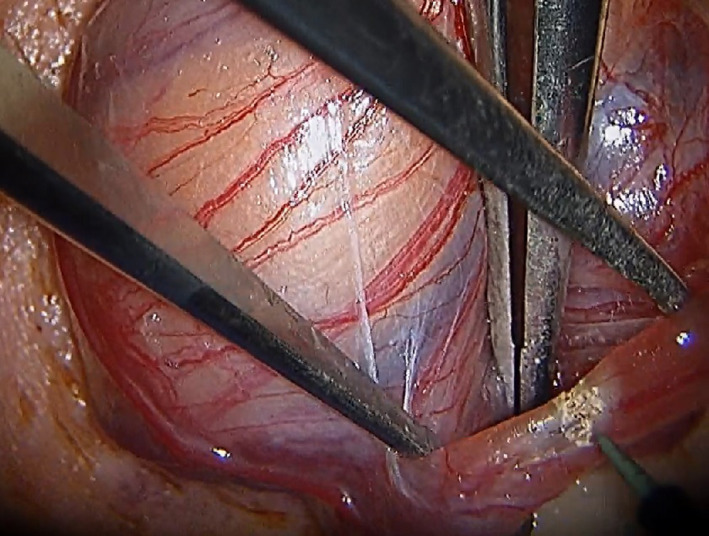
Microsurgical view of cremaster muscle fibre being divided with electrocautery
3. RESULTS
Between September 2011 and April 2019, nineteen men who presented with chronic orchialgia secondary to a hyperactive cremaster muscle reflex underwent MSCMR. Their mean visual analogue pain score preoperatively when asked the level of pain at times of retraction was six. Eleven of the men were married, five were not married but in stable relationships, and three were not in consistent relationships. All the men were heterosexual. A total of 25 spermatic cord units underwent MSCMR, as six of the men presented with bilateral testicular retraction and thirteen with unilateral retraction requiring MSCMR. The mean age of the men was 38.5 years ± 10.2. Consideration for candidacy for MSCMR included answering ‘yes’ to the clinical question: ‘at times of testicular pain, does the testicle retract up in the groin to the extent that you have to milk it back down to the scrotum?’ The pain was typically described as a dull, heavy ache which would commonly worsen with intercourse and with exercise. None of the men had a history of a retractile testis in childhood, none were previously treated for any issues with a contralateral retractile testis, nor did they have a history of childhood testicular trauma. On physical examination, the testicle must have vigorously retracted with Valsalva manoeuvre. Cases where the history and physical examination eliciting a vigorous cremaster reflex on Valsalva were not demonstrable were excluded. The men must also have had normal digital rectal examinations, negative urinalyses and negative scrotal Doppler ultrasounds, and had pain localised to the testicle, epididymis or spermatic cord, without an anatomic or pathologically identifiable aetiology other than testicular retraction.
Of the men who underwent MSCMR, 100% of the spermatic cord units (25/25) had complete resolution of testicular retraction and 92% (23/25) of spermatic cord units had complete resolution of orchialgia. The two men who had persistent pain despite resolution of testicular retraction had a mean visual analogue pain score of four. There was a complication in one out of 25 testicular units (4%) which was a small scrotal haematoma which resolved with conservative management. None of the patients suffered serious complications with long‐term sequelae such as a surgical infection, development of a hydrocele or testicular atrophy. Men were followed out for 6 months after MSCMR.
4. DISCUSSION
The evaluation of men with chronic orchialgia is a challenging diagnostic and therapeutic dilemma, as there is not always an identifiable aetiology for orchialgia. When no aetiology is identified, conservative therapy is the first‐line treatment. When conservative treatment fails, surgical intervention may be warranted. Surgical intervention for chronic orchialgia was advanced with the use of the operative microscope in the 1970s to perform microsurgical spermatic cord denervation (MSCD; Devine & Schellhammer, 1978). Although MSCD has progressed from a full skeletonisation of the spermatic cord to a more targeted approach to MSCD, a retractile testis secondary to a hyperactive cremaster muscle reflex as the clear cause of orchialgia can even further simplify the surgical approach (Kavoussi, 2018; Levine, Matkov, & Lubenow, 1996; Parekattil et al., 2013). A careful history and physical examination may elicit testicular retraction secondary to a hyperactive cremaster muscle as the aetiology for orchialgia which allows for a less complex and less time‐consuming surgical procedure with favourable outcomes, which essentially avoids risk to important microsurgical anatomic structures within the spermatic cord such as lymphatic channels, gonadal arteries and the vas deferens.
There is a paucity of data on hyperactive cremaster muscle resulting in orchialgia due to testicular retraction. As early as 1885, a case of a 25‐year‐old man having testicular retraction into the abdomen was reported (Retraction of Testicle into Abdomen, 1885). A case series of six patients with testicular retraction due to hyperactive cremaster muscles was reported in 1956, which was termed ‘cremasteric cramp with testicular retraction’. These patients underwent excision of the ilioinguinal nerve and cremaster muscle with good reported success rates (Baty, 1956). A thorough physical examination should rule out an indirect inguinal hernia in men with a retractile testis as a source for the retraction (Heller, 1988). It has been reported that men with an attenuated or obliterated external oblique aponeurosis who failed orchiopexy may have severe testicular retraction treated by reconstruction of the external inguinal ring with a GORE‐TEX mesh, which can reduce testicular retraction into the external inguinal ring (Deck & Berger, 1999). Although this was reported to be effective in three men, and none of the patients in the current study undergoing MSCMR were found to have an obliterated external ring by examination, patients with an obliterated external ring may presumably respond to MSCMR as well based on the physiology of the cremaster reflex and testicular retraction, avoiding a more time‐consuming, complex surgery, obviating the need for placement of mesh. A case of post‐coital painful testicular retraction associated with the tricyclic antidepressant desipramine has also been reported, so this should be a point of suspicion in the history of men with orchialgia secondary to testicular retraction (Sorvino, 1986).
Limitations to this study include the retrospective nature and the small sample size; however, to our knowledge, this is the largest study evaluating treatment of the retractile testis secondary to hyperactive cremaster muscle reflex and the first study demonstrating the effectiveness of MSCMR for chronic orchialgia secondary to testicular retraction due to a hyperactive cremaster muscle reflex, although it has been previously described (Kavoussi & Costabile, 2013).
5. CONCLUSION
Microsurgical subinguinal cremaster muscle release is an effective option with a relatively low complication rate for men when chronic orchialgia is clearly identified as being secondary to testicular retraction due to a hyperactive cremaster muscle reflex when other aetiologies of orchialgia have been ruled out.
CONFLICT OF INTEREST
Author is on the speaker bureau for AYTU BioSciences, no relevant to this work.
Kavoussi PK. Microsurgical subinguinal cremaster muscle release for chronic orchialgia secondary to hyperactive cremaster muscle reflex in adults. Andrologia. 2020;52:e13493. 10.1111/and.13493
REFERENCES
- Baty, J. A. (1956). Cremasteric cramp with testicular retraction. British Medical Journal, 1(4974), 1014–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costabile, R. A. , Hahn, M. , & McLeod, D. G. (1991). Chronic orchialgia in the pain prone patient: The clinical perspective. Journal of Urology, 146(6), 1571–1574. 10.1016/S0022-5347(17)38169-7 [DOI] [PubMed] [Google Scholar]
- Davis, B. E. , Noble, M. J. , Weigel, J. W. , Foret, J. D. , & Mebust, W. K. (1990). Analysis and management of chronic testicular pain. Journal of Urology, 143(5), 936–939. 10.1016/S0022-5347(17)40143-1 [DOI] [PubMed] [Google Scholar]
- Deck, A. J. , & Berger, R. E. (1999). Pain associated with testicular retraction treated with Gore‐Tex external inguinal ring reconstruction. Techniques in Urology, 5(4), 219–222. [PubMed] [Google Scholar]
- Devine, C. J. Jr , & Schellhammer, P. F. (1978). The use of microsurgical denervation of the spermatic cord for orchialgia. Transactions of the American Association of Genito‐Urinary Surgeons, 70, 149–151. [PubMed] [Google Scholar]
- Heller, J. E. (1988). Intraabdominal retraction and entrapment of testicle associated with indirect inguinal hernia. Journal of Adolescent Health Care, 9(4), 335–336. 10.1016/0197-0070(88)90261-6 [DOI] [PubMed] [Google Scholar]
- Kavoussi, P. K. (2018). Validation of targeted microsurgical spermatic cord denervation: Comparison of outcomes to traditional complete microsurgical spermatic cord denervation. Asian Journal of Andrology, 21(4), 319. 10.4103/aja.aja_87_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavoussi, P. K. , & Costabile, R. A. (2013). Orchialgia and the chronic pelvic pain syndrome. World Journal of Urology, 31(4), 773–778. 10.1007/s00345-013-1092-5 [DOI] [PubMed] [Google Scholar]
- Levine, L. A. , Matkov, T. G. , & Lubenow, T. R. (1996). Microsurgical denervation of the spermatic cord: A surgical alternative in the treatment of chronic orchialgia. Journal of Urology, 155(3), 1005–1007. 10.1016/S0022-5347(01)66369-9 [DOI] [PubMed] [Google Scholar]
- Parekattil, S. J. , Gudeloglu, A. , Brahmbhatt, J. V. , Priola, K. B. , Vieweg, J. , & Allan, R. W. (2013). Trifecta nerve complex: Potential anatomical basis for microsurgical denervation of the spermatic cord for chronic orchialgia. Journal of Urology, 190(1), 265–270. 10.1016/j.juro.2013.01.045 [DOI] [PubMed] [Google Scholar]
- Retraction of Testicle into Abdomen. (1885). The British Medical Journal, 1(1263), 536. [PMC free article] [PubMed] [Google Scholar]
- Sorvino, A. R. (1986). Painful postcoital testicular retraction linked with desipramine. American Journal of Psychiatry, 143(5), 682–683. [DOI] [PubMed] [Google Scholar]


