Summary
Weight management interventions designed specifically for men have become more common, but the extent to which socioeconomic factors are considered in trials of these interventions is unclear. We synthesized study characteristics, methods, and reporting of interventions with a behavioral component for men that report weight as an outcome, to establish the extent to which socioeconomic factors are considered during intervention design, conduct, and reporting. A comprehensive search was conducted on Medline, Embase, PsycINFO, and CENTRAL for studies published from January 2000 to July 2021. Thirty‐six trials were included. Educational attainment (n = 24) was the most frequently reported socioeconomic characteristic, followed by working status (n = 14) and area level deprivation (n = 12). Seven studies did not report any socioeconomic characteristics. Most studies (n = 20) did not mention the socioeconomic profile of their samples in relation to study strengths or limitations. Few (n = 4) consulted with men from lower socioeconomic groups during intervention design. One study examined potential differential intervention effects across socioeconomic groups, with most not powered to do so. Recent feasibility trials (n = 3) targeting specific socioeconomic groups suggest a potential nascent towards a greater consideration of factors related to equity. To best inform public health policy related to health inequalities, greater consideration of socioeconomic factors is required in trials of men's weight management interventions.
Keywords: inequalities, RCT, socioeconomic characteristics, weight management
Abbreviations
- BMI
Body Mass Index
- FFIT
Football Fans in Training
- HRQoL
Health Related Quality of Life
- Obj
Objective
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta‐Analysis
- RCT
Randomized Controlled Trial
- RoB
Risk of Bias
- SHED‐IT
Self‐Help, Exercise and Diet using Information Technology
- SR
Self‐Report
- VLCD
Very Low Calorie Diet
- Wks
Weeks
- WLM
Weight Loss Maintenance
1. INTRODUCTION
Obesity is a risk factor for morbidity and premature mortality. 1 , 2 Interventions that support individuals living with obesity to modify their diet and physical activity behaviors can result in clinically significant weight reduction and improved health outcomes. 3 , 4 The prevalence of overweight and obesity between men and women is similar. 5 , 6 , 7 However, men are underrepresented in weight management research. 8 , 9 Trials reporting recruitment data disaggregated by gender indicate that women are around twice as likely as men to take up an offer to participate in mixed‐gender weight management programs. 10 , 11 Qualitative research suggests that men perceive some weight management programs as being incompatible with their needs 12 and counter to social ideals of masculinity. 13 Hence, interventions designed specifically to appeal to men are becoming more common. Men residing in lower socioeconomic areas or with lower levels of educational attainment may be particularly unlikely to participate in weight management programs, 10 , 14 but the extent to which socioeconomic factors are considered in the design and evaluation of interventions for men is unknown.
The term socioeconomic status describes the social standing of individuals based on factors such as their place of residence, income, occupation, and educational attainment. 15 Living in lower socioeconomic areas is predictive of poorer quality diet, including lower fruit and vegetable consumption and higher sugar‐sweetened beverage intake. 16 , 17 Similarly, individuals residing in lower socioeconomic areas are less likely to meet recommendations for physical activity, 18 which is likely due to differences in leisure‐time physical activity. 19 , 20 The relationship between socioeconomic status and health outcomes is more strongly mediated by poor diet and physical inactivity in men than women. 21 Social context and socioeconomic status influence the way in which masculinities are constructed. 22 Adherence to particular performances of masculinity linked to poorer health outcomes, 23 , 24 and reduced confidence to seek health information and trust in that information, 25 are prevalent amongst men from lower socioeconomic circumstances. Interventions and engagement strategies that are congruent with masculine identities may be important to engage diverse populations of men. 26 , 27 , 28 , 29
The need for weight management interventions designed to appeal specifically to men is well recognized. 9 , 30 , 31 , 32 The innovation of gender tailoring health interventions has been described as a key development to engage men who may not otherwise participate. 32 Several interventions that have been gender tailored in content, context, mode, and/or style of delivery have proved successful in engaging men living with obesity and supporting positive health behavior change. 33 , 34 , 35 , 36 , 37 , 38 , 39 Qualitative evidence from men's weight management interventions highlights the value men place on programs being developed and targeted specifically for them. 26 , 40 , 41 Systematic reviews indicate that men's weight management interventions can be effective at supporting weight reduction. 31 , 42 However, the characteristics of men who participate in these programs and the extent to which socioeconomic factors are considered in the design and evaluation of these interventions are unknown. Interventions lacking an evidence base to suggest they are appealing and effective across socioeconomic groups may widen health inequities. 43
A systematic review examining government policy impact on socioeconomic inequities in obesity and obesity‐related health behaviors concluded that a broad complement of policies spanning the agency‐structure continuum is required to ameliorate inequities in obesity. 44 Others have posited that behavioral weight management interventions that rely on a high degree of individual agency may augment health inequalities, 43 , 45 with population level approaches potentially more equitable. 46 , 47 Indeed, a recent systematic review concluded that digital interventions targeting physical activity are not effective for individuals with lower socioeconomic status (but are in those more affluent), and that additional efforts or intervention tailoring is required for these types of interventions to be equitable. 48 Possible explanations for this relationship include low socioeconomic status being linked with having lower levels of ehealth literacy, 49 , 50 and potentially fewer opportunities to engage with or act upon intervention content due to limited resources and differences in social and physical environments. 51 Engaging members of disadvantaged communities in intervention design and tailoring of interventions for population subgroups can support positive health outcomes. 52 Public health policy highlights the need for different types of interventions that support health in priority population groups that are most at risk of ill‐health, including those from lower socioeconomic circumstances. 53 , 54
In seminal research published in 2004, senior health policymakers 55 and researchers 56 highlighted a lack of an equity dimension in research evaluations. This has been underlined by systematic review evidence showing that randomized controlled trials (RCTs) examining intervention effectiveness in reducing obesity‐related inequities, particularly in men, are lacking. 57 In 2014, recommendations for research from the “ROMEO” series of systematic reviews on men's obesity concluded that men from diverse backgrounds should be consulted to optimize intervention engagement, and that qualitative research findings should inform all aspects of intervention design, including intervention settings and recruitment processes. 58 In 2017, an extension to the CONSORT guidelines for better reporting of health equity in RCTs was published, with useful recommendations around reporting of participants' characteristics and limitations related to groups that may experience social disadvantage. 59 However, the extent to which RCTs of weight management interventions for men align with these equity‐related recommendations is unclear. Therefore, the aim of this systematic review is to examine RCTs of interventions for men with a behavioral component that report weight as an outcome, to establish the degree to which socioeconomic factors have been considered, including the extent to which
consultations to inform intervention design are undertaken with men from specific socioeconomic groups or with other relevant stakeholders,
trials report participant socioeconomic characteristics,
trials report the socioeconomic profile of their participants in relation to study strengths or limitations statements,
trials target specific socioeconomic groups or conduct subgroup analysis in relation to socioeconomic characteristics.
2. METHODS
This systematic review is reported in line with the Preferred Reporting Items for Systematic Reviews and Meta‐Analysis (PRISMA) guidelines. 60 The review protocol was registered with PROSPERO (CRD42020167282).
2.1. Eligibility criteria
Participants: Men‐only studies were included if they had a mean baseline participant body mass index (BMI) of ≥30 kg/m2 and/or a participant eligibility criterion BMI of ≥25 kg/m2. Studies that included men's partners or family members (e.g., children), where the primary intervention outcome of interest was men's weight, were also included. Studies including any males under 18 years were excluded, except in cases where males under 18 were participating as family members (e.g., in a father‐child intervention).
Interventions: Interventions targeting weight, diet, and/or physical activity with a behavioral component, such as education, behavior change techniques, psychological theories, or counselling, were included. Interventions could include group‐based or individual, face‐to‐face, or e‐health interventions. Surgical or drug interventions, with or without a behavioral component, were excluded.
Comparators: Studies that included a control group (e.g., wait list, usual care, minimal, or no intervention) or that compared two or more active interventions against each other were eligible.
Outcomes: Studies that reported men's weight or BMI as an outcome were eligible. Weight outcomes in the context of this review refer to studies with interventions that may support weight loss, maintenance of weight loss, or weight gain prevention. Both objectively measured and self‐reported weight outcomes were eligible.
Study Designs: Peer‐reviewed individual or cluster RCTs, with any length of follow‐up, published in English since the year 2000 were included.
2.2. Search strategy and information sources
A comprehensive search strategy (Figure S1) was developed for Medline, then adapted for Embase, PsycINFO, and the Cochrane Central Register of Controlled Trials. Groups of terms incorporated into the search strategy related to the (a) outcome of interest (weight), (b) trial design (RCT), and (c) population (men). In line with health equity recommendations, equity‐related search terms were not included. 61 Moreover, the aim of this review was not to assess studies that had a specific focus on equity, rather to examine the extent to which socioeconomic factors were considered in all men's weight management RCTs. The full electronic database search was conducted to include studies from January 2000 to July 2021. This date range captures the period during which seminal research (in 2004) highlighted a lack of an equity dimension in health research and since the innovation of gender‐tailored weight management interventions for men (mid 2000s). Existing systematic reviews relating to men's weight management and physical activity interventions were examined for potentially eligible articles. 30 , 31 , 42 Articles citing and referenced by eligible studies were also examined to see if they were eligible for inclusion. 62
2.3. Study selection
Duplicate records were removed from the Endnote database. One reviewer (MM) screened the titles and abstracts of all remaining records. The full texts of all records identified as potentially relevant were examined against the inclusion and exclusion criteria. Two reviewers (MM and HS) screened five full‐text articles together, to ensure consistent understanding of the inclusion and exclusion criteria. The same two authors (MM and HS) then independently screened the remaining full texts. There was one discrepancy noted, which was ultimately included through discussion with a third researcher (EQ).
2.4. Data collection process
One reviewer (MM) extracted relevant data from eligible studies. Relevant information was extracted from publications reporting RCT outcomes, as well as associated study reports, protocols, intervention development papers, and process evaluations. Additional reviewers (HS and ZM) checked all the primary data reported against the original published research articles.
2.5. Risk of bias in individual studies
One researcher (MM) assessed risk of bias (RoB) domains using the Cochrane RoB tool. 63 Individual RoB domains were assigned as being “low risk,” “some concerns,” or “high risk” for each study. A second reviewer (JB) independently assessed RoB domains for 50% of the included studies to ensure consistent interpretation across studies (k = 0.80). Any discrepancies were resolved through discussion, with a third researcher consulted if required. The “other” bias category was used to capture information on potential conflicts of interest between the funder and the researchers.
2.6. Data items
Baseline data (i.e., means and standard deviations of age and BMI), study descriptors (i.e., sample sizes, inclusion criteria, and recruitment strategies), participant socioeconomic characteristics (i.e., education level, area level deprivation, income, and employment status), and other associated factors (i.e., ethnicity and rurality) were extracted. The term “area level deprivation” refers to an index that categorizes zipcode/postcode areas of residence by deprivation, relative to the level of deprivation nationally (e.g., postcode areas classified as being in quintile 1 are in the 20% most deprived areas and those in quintile 5 are in the 20% least deprived areas nationally). These indexes typically account for multiple indicators of deprivation, including income levels, employment, housing, health, education, and crime. 64 Information on consultations (i.e., with men from the target group or other stakeholders) undertaken to inform intervention design and statements made about the socioeconomic profile of study samples being a study strength or limitation were also extracted.
2.7. Data synthesis
The number and proportion of studies reporting specific participant socioeconomic characteristics were calculated. From this, the total number of socioeconomic characteristics reported in each study was determined. We calculated the number and proportion of studies that reported consulting with men from the target group and other relevant stakeholders during intervention design. Data on whether consultations targeted men from specific socioeconomic groups were collated. The number and proportion of interventions tailored specifically for men were also computed. Due to the heterogeneity of socioeconomic characteristic measures across studies and countries, moderation analysis of socioeconomic status on weight outcomes and retention was not undertaken.
The number and proportion of trials that reported the socioeconomic profiles of their participants in relation to study strengths or limitations were calculated. Examining study strength and limitation statements gives some indication as to whether study authors may have considered the importance of the socioeconomic characteristics of their sample in relation to the potential for their intervention to impact health inequalities. These statements were categorized as being specific to the socioeconomic profile of the sample if they mentioned socioeconomic groups, educational attainment, area level deprivation, income levels, or similar terms. Statements clearly referring to strengths were documented as such. Due to the potential for differential interpretation of whether some statements could be deemed a limitation, a strength, or neither, we simply documented that the socioeconomic profile was mentioned. Statements focusing on diversity related to ethnic groups were classified separately if there was no mention of specific socioeconomic characteristics. Nonspecific statements about study diversity or generalizability were also classified separately. All data were synthesized narratively.
3. RESULTS
3.1. Study selection
A summary of the study selection process is outlined in Figure 1. The search strategy identified 15,104 articles, with 12,706 remaining after duplicates were excluded. Eighty‐six articles were eligible for full‐text screening, of which 36 trials were ultimately included. No additional studies were deemed eligible from included studies citation and reference lists, or from existing systematic reviews. Common reasons for exclusion, after full‐text review, were a failure to meet the BMI eligibility criteria and weight not being reported as an outcome.
FIGURE 1.
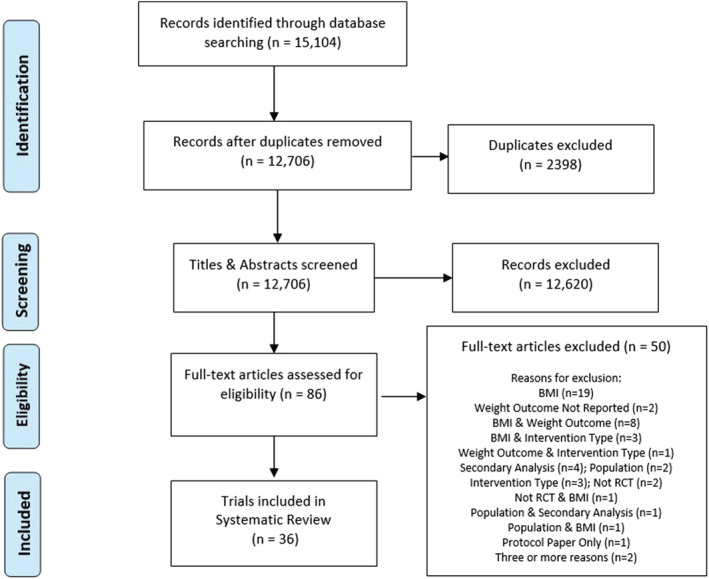
PRISMA flow diagram
3.2. Study characteristics
Table 1 reports selected characteristics of the included RCTs. Most trials were conducted in the United States (n = 9), Australia (n = 8), Scotland (n = 5), or other European countries (n = 7). The number of study participants ranged from 18 to 1113. Most studies (n = 21) had less than 100 participants, 12 had between 100 and 200, and 4 had over 200. Ten studies completed longer term follow‐up measures with participants (12–24 m: n = 6; >24 m: n = 4). 33 , 38 , 39 , 65 , 66 , 67 , 68 , 69 , 70 , 71 Twenty studies were pilot or feasibility studies. 33 , 35 , 37 , 38 , 65 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 Weight loss was the main intervention outcome in most studies (n = 28), with maintenance of weight lost the focus in two trials. 66 , 67 Four studies were published between the years 2000 and 2009. One study reported post‐intervention results in 2009, 87 with longer‐term outcomes reported in 2011. 38 Twelve studies were published between 2010 and 2015, with a further 19 published more recently (2016–2021).
TABLE 1.
Study characteristics
| Primary source | Country | N | Study arms | Controls | Primary outcome of intervention | Intervention duration (months) | Intervention type | Measures (months post‐baseline) | Weight change (kg) |
|---|---|---|---|---|---|---|---|---|---|
| Aguiar et al 2016 a | Australia | 101 | 2 | Wait list | Weight | 6 | Remote, individual | 3 and 6 | −5.5 |
| Alick et al 2017 a | USA | 40 | 2 | Active intervention | Weight | 2.8 | F2F, group | 1.4 and 2.8 | −1.3 |
| Azar et al 2015 a | USA | 64 | 2 | Wait list | Weight | 2.8 | Remote, group | 3 | −3.2 |
| Borg et al 2002 | Finland | 90 | 3 | Minimal intervention | Weight (WLM) | 6 | F2F, group | 6 and 29 | +0.2, −1.3 |
| Crane et al 2015 | USA | 107 | 2 | Wait list | Weight | 6 | Combination | 3 and 6 | −4.7 |
| Demark‐Wahnefried et al 2017 a | USA | 40 | 2 | Wait list (post‐surgery intervention) |
Weight |
Varied up to prostate surgery | F2F, individual | Varied post‐intervention | −2.5 |
| De Melo et al 2021 | Brazil | 45 | 2 | Low protein diet | Sleep apnoea and metabolic parameters | 1 | F2F, individual | 1 | −0.3 |
| Dombrowski et al 2020 a | Scotland | 105 | 3 | Wait list | Weight | 12 | Remote, individual | 12 | −2.1, −0.4 |
| Esposito et al 2004 | Italy | 110 | 2 | Minimal intervention | Erectile/endothelial function | 24 | Combination | 24 | −13.0 |
| Garcia et al 2019 a | USA | 50 | 2 | Wait list (12 wks) | Weight | 2.8 | F2F, individual | 2.8 | −5.5 |
| Gray et al 2013 a | Scotland | 103 | 2 | Wait list | Weight | 2.8 | F2F, Group | 2.8 | −4.8 |
| Griffin et al 2019 a | England | 43 | 2 | Minimal intervention | Weight | 2.8 | F2F, group | 3 and 6 | −0.9 |
| Hunt et al 2014 | Scotland | 747 | 2 | Wait list | Weight | 2.8 | F2F, group | 2.8 and 12 | −4.8 |
| Irvine et al 2017 a | Scotland | 69 | 2 | Minimal intervention | Alcohol consumption and weight | 2 | Remote, individual | 5 | +1.1 |
| Johansson et al 2009 | Sweden | 62 | 2 | Wait list | Sleep apnoea | 2.1 | F2F, group, with VLCD | 0.2, 0.7, 1.2, 1.6, and 2.1 | −19.8 |
|
Kaukua et al 2002 |
Finland | 38 | 2 | Wait list | Weight loss on HRQoL | 3.9 | F2F, group, with VLCD | 2.5, 3.9, and 7.4 | −17.1 |
| Kim et al 2015 | South Korea | 205 | 2 | Minimal intervention | Weight | 6 | Remote, individual | 1, 3, and 6 | −0.1 |
| Kwasnicka et al 2020a | Australia | 130 | 2 | Wait list | Weight | 2.8 | F2F, group | 3 | −3.3 |
| Maddison et al 2019 a | New Zealand | 96 | 2 | Wait list | Weight | 2.8 | F2F, group | 2.8 | −2.5 |
| Mohamad et al 2019 a | Scotland | 62 | 2 | Wait list (12 wks), then minimal intervention | Weight | 2.8 | Remote, individual | 2.8 (Obj), 6, and 12 (SR) | −2.4 |
| Mollentze et al 2019 a | South Africa | 18 | 2 | Standard intervention | Weight | 6 | Combination, with VLCD | 3 and 6 | −8.1 |
| Morgan et al 2013 |
Australia |
159 | 3 | Wait list | Weight | 3 | Remote, individual | 3 and 6 | −3.2, −4.2 |
| Morgan et al 2014 |
Australia |
93 | 2 | Wait list | Weight | 1.6 | F2F, group | 3.2 | −3.4 |
| Morgan et al 2011a a | Australia | 110 | 2 | Wait list | Weight | 3 | Combination | 3.2 | −4.3 |
| Morgan et al 2011b a | Australia | 53 | 2 | Wait list | Weight | 3 | F2F, group | 3 and 6 | −7.6 |
| Morgan et al 2011c a | Australia | 65 | 2 | Minimal intervention | Weight | 3 | Remote, individual | 3 and 12 | −2.2 |
| O'Connor et al 2020 a | USA | 36 | 2 | Wait list | Weight | 2.3 | F2F, group | 4 |
−1.7 |
| Ozaki et al 2019 | Japan | 71 | 3 | Wait list | Weight | 2.8 | Remote, individual | 2.8 | −2.2, −4.3 |
| Patrick et al 2011 | USA | 441 | 2 | Wait list | Weight | 12 | Remote, individual | 6 and 12 | −0.7 |
| Petrella et al 2017 a | Canada | 80 | 2 | Wait list | Weight |
2.8 |
F2F, group | 2.8 | −3.6 |
| Puhkala et al 2015 | Finland | 113 | 2 | Wait list | Weight | 12 | Combination | 12 and 24 | −4.0 |
| Rounds et al 2020 | USA | 102 | 2 | Intervention without incentives | Weight | 2.8 | Remote, individual | 2.8 and 5.5 | −2.2 |
| Shin et al 2017 a | South Korea | 105 | 3 | Minimal intervention | Weight | 2.8 | Remote, individual | 0.9, 1.8, and 2.8 | −0.7, −2.7 |
| Ventura Marra et al 2019 a | USA | 59 | 2 | Minimal intervention | Weight | 2.8 | Remote, individual | 1.4 and 2.8 | −3.3 |
| Wyke et al 2019 | England, Netherlands, Norway. and Portugal | 1,113 | 2 | Wait list | Sedentary time and physical activity | 2.8 | F2F, group | 2.8 and 12 | −2.4 |
| Young et al 2017 |
Australia |
92 | 2 | No intervention | Weight (WLM) | 6 | Remote, individual | 6, 12, and 36 | −1.6 |
Primary outcome of intervention: For pilot and feasibility studies, the intended primary outcome of the intervention or potential future full RCT is listed (i.e., not feasibility related outcomes).
Intervention type: Whether the intervention is predominantly delivered face‐to‐face or remotely, and mostly individually or group based. Some studies are listed as “combination” where the predominant intervention type is mixed and difficult to classify. If interventions involve a very low calorie diet, this is also listed.
Weight change (kg): Intervention group(s) versus comparison group weight change reported at final follow‐up. Different analysis methods used across studies and in some cases, we have calculated weight change between groups or converted pound into kilogram for reporting in this paper.
Abbreviations: kg, kilograms; VLCD, very low calorie diet; F2F, face to face; HRQoL, health related quality of life; WLM, weight loss maintenance; Obj, objective; SR, self‐report; wks, weeks.
Pilot/feasibility studies: Starred studies (n = 20) are either self‐described as pilot/feasibility studies and/or report on feasibility related outcomes.
Four studies involved fathers and their primary school‐aged children. 37 , 77 , 82 , 88 Two of these studies were of the Healthy Dads Healthy Kids intervention in Australia, 37 , 88 and two were of cultural adaptations of the same program in the UK 77 and the USA. 82 One study examined the effects of a group‐based intervention with and without spousal support in African American men. 72 All other studies involved only men. Two studies examined interventions for men who had experienced prostate cancer, 65 , 74 two for men with moderate or severe sleep apnoea, 89 , 90 one for men with erectile dysfunction, 68 and one for men consuming high levels of alcohol. 78 Three worksite‐related studies specifically recruited long distance truck or bus drivers, 69 those working at company headquarters, 91 and men working in private companies and local government agencies, 92 respectively. Thirteen studies included remote individual level interventions utilizing technology, and 12 studies were face‐to‐face group‐based interventions. The remote individual level interventions included five studies linked to the Self‐Help, Exercise and Diet using Information Technology (SHED‐IT) intervention in Australia. 38 , 66 , 83 , 86 , 93 The face‐to‐face group‐based RCTs included the pilot, 76 full‐scale trial, 39 and international adaptations 35 , 70 , 85 , 94 of the Football Fans in Training (FFIT) intervention. Three trials were of interventions utilizing very low calorie diets. 79 , 90 , 95
3.3. Risk of bias
The full list of studies and designated RoB for each domain can be found in the supporting information (Figure S2). Most studies had a low RoB for the randomization process (n = 28, 77.8%), missing outcome data (n = 29; 80.6%), and measurement of outcome (n = 33; 91.7%). Most studies (n = 32, 88.9%) had “some concerns” for deviations from intended interventions due to a lack of blinding in the intervention types considered in this review. For selection of reported result, most studies (n = 24; 66.7%) had “some concerns” due to a lack of information on whether the analysis methods were pre‐planned. Four studies had a high risk of other bias due to potential conflicts of interest around how the study was funded or interventions provided, which included the three studies of a very low calorie diet intervention.
3.4. Study socioeconomic characteristics
Table 2 provides an overview of information related to intervention design, study socioeconomic characteristics, and statements related to the socioeconomic profile of studies. Measures of socioeconomic characteristics were heterogeneous across studies and countries. Seven (19.4%) studies reported no socioeconomic characteristics, 14 (38.9%) studies reported 1, and 15 (41.7%) reported 2 or more socioeconomic characteristic at baseline. Twenty‐four (66.7%) studies reported education level and 14 (38.9%) studies reported working status or occupation. Twelve (33.3%) studies reported area level deprivation, all of which were from Australia or the UK. For two of the trials of worksite specific interventions, other than the targeted occupations, neither study reported other socioeconomic factors. 69 , 91 Four recent studies aimed to engage the following specific groups: men from more deprived areas, 33 men from low‐income Hispanic families, 82 men from socioeconomically disadvantaged and ethnically diverse localities, 77 and men in the workplace with 2 years or less of college education, 96 respectively. Fifteen (41.7%) studies reported participant ethnicity. Three of these trials were intended for and had an inclusion criterion relating to specific ethnic groups. 72 , 75 , 82 One pilot study reported on the urban‐rural classification of their sample, with all participants (n = 54) residing in areas classified as “rural.” 81
TABLE 2.
Intervention design, socioeconomic characteristics and strength and limitation statements
| Studies | Intervention design | Socioeconomic characteristics reported | Strength and limitation statements | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Primary intervention type | Total | Tailored for men | Men consulted | Stakeholders consulted | No tailoring for men or consultations | Education level | Area level deprivation | Working status/occupation | Income | None reported | Socioeconomic profile mentioned | No mention of socioeconomic profile |
| N | N | N | N | N | N | N | N | N | N | N | N | |
| Face to face group | 12 | 10 | 5 | 4 | 2 | 9 | 5 | 6 | 4 | 1 | 8 | 4 |
| Face to face individual | 3 | 1 | 1 | 0 | 2 | 2 | 0 | 1 | 0 | 1 | 0 | 3 |
| Remote group | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 |
| Remote individual | 13 | 8 | 3 | 2 | 2 | 10 | 6 | 4 | 1 | 2 | 6 | 7 |
| Very low calorie diet | 3 | 0 | 0 | 0 | 3 | 1 | 0 | 1 | 0 | 2 | 0 | 3 |
| Combination | 4 | 3 | 0 | 0 | 1 | 1 | 1 | 2 | 0 | 1 | 1 | 3 |
| Total | 36 | 22, 61.1% | 9, 25.0% | 6, 16.7% | 11, 30.6% | 24, 66.7% | 12, 33.3% |
14, 38.9% |
5, 13.9% | 7, 19.4% | 16, 44.4% | 20, 55.6% |
Primary intervention type: Whether the intervention is predominantly delivered face‐to‐face or remotely, and mostly individually or group based. Some studies are listed as “combination” where the predominant intervention type is mixed and difficult to classify. If interventions involve a very low calorie diet, this is also listed.
Detailed information on the socioeconomic characteristics of study samples and related statements about study strengths or limitations are provided in Table S1. Twenty (55.6%) studies did not specifically mention the socioeconomic profile of their study sample. Of these 20 studies, 3 provided a broad statement about a lack of generalizability, 68 , 80 , 97 1 provided a broad statement about sample diversity being a study strength, 71 1 made a statement about the lack of generalizability to other ethnic groups, 75 another reported the reach across ethnic groups as a strength, 84 and the remaining 14 made no statement about sample diversity or reach. Three studies that had designed their intervention or recruitment strategies to reach specific socioeconomic groups reported the socioeconomic profile of their sample as a strength. 33 , 77 , 82
The FFIT intervention and recruitment strategies were not designed to specifically engage lower socioeconomic groups. However, the study papers did report reaching men from across the socioeconomic spectrum in both the pilot and full‐scale trials. 39 , 76 In the full trial (n = 747 participants), this was reported as a study strength as it facilitated subgroup analysis examining potential differential intervention effects across socioeconomic groups. 98 In the pre‐specified analysis, intervention effects on weight outcomes at 12 months did not vary significantly by participant education, employment status, or area level deprivation. 98 No other studies included in this review conducted subgroup analysis in relation to socioeconomic characteristics.
Twenty‐two studies reported that their interventions were tailored specifically for men based on the literature, and six reported stakeholder (not including target group men) consultations during pre‐trial intervention design. Nine (25%) of the studies 33 , 39 , 65 , 75 , 76 , 77 , 78 , 82 , 84 included in this review reported consulting with men from the target during intervention design. Consultation methods undertaken to inform the intervention design process varied across studies, including focus groups, workshops, survey data, and various patient and public involvement activities. Of the nine studies that consulted men, four specifically reported engaging with lower socioeconomic groups. 99 , 100 , 101 , 102 In the cultural adaptation of the Healthy Dads Healthy Kids intervention for men and children from low‐income Hispanic communities in the United States, family members participated in focus groups, online surveys, and interviews with findings reviewed by stakeholder experts to inform the adaptation. 101 Garcia and colleagues undertook semi‐structured qualitative interviews with men in the United States, including those “less acculturated” (e.g., Spanish‐speaking, foreign‐born, low educational attainment), to inform the gender and cultural tailoring of a face‐to‐face individual intervention. 100 In the Healthy Dads Healthy Kids feasibility study in the UK, individual and focus group interviews with fathers and other family members from a range of ethnic, religious, and socioeconomic groups informed the cultural adaptation of the programs, with patient and public involvement also integrated throughout. 99 In the “Game of Stones” feasibility trial of a remotely delivered individual intervention in Scotland, a focus group with men from lower socioeconomic areas informed the recruitment strategies; with a large survey, and patient and public involvement activities undertaken to inform the intervention design and study processes. 41 , 102 Eleven (30.6%) trials did not report intervention tailoring for men or undertake stakeholder or target group consultations.
4. DISCUSSION
4.1. Summary of evidence
This systematic review highlights that in RCTs of interventions with a behavioral component for men that report weight as an outcome, socioeconomic factors were inconsistently reported, few were specifically designed for men from lower socioeconomic groups, and subgroup analysis by socioeconomic status was rarely undertaken or planned. Thus, there is currently limited evidence on the reach and effectiveness of interventions across the socioeconomic spectrum, or for interventions designed specifically for men from lower socioeconomic circumstances. However, some recent feasibility studies did aim to engage specific socioeconomic and ethnic groups.
Counter to recommendations for involving men from diverse backgrounds during intervention design, 58 only nine (25%) of the trials included in this review reported consulting with men from the target group, of which four specifically reported engaging with lower socioeconomic groups. 99 , 100 , 101 , 102 Of note, eight of the nine studies that reported consulting with men from the target group have been published since the ROMEO review recommendations in 2014. 58 Four of the most recent RCTs (published since 2019) included in this review were aimed at specific socioeconomic groups, 33 , 77 , 82 , 96 suggesting that there may be a recent shift towards a greater focus on equity and diversity, and the importance of adaptation and targeting to specific groups. One of these studies, the “Gutbusters” trial in the United States, initially targeted men in the workplace with 2 years or less college education; but due to poor enrolment rates the recruitment methods and the inclusion criteria were altered, resulting in a highly educated sample of men. 14 , 96 Indeed, lower socioeconomic groups are typically difficult to engage in research due to a variety of barriers, including a lack of trust in research, a lack of perceived benefit from participating, gatekeepers preventing access to the target group, gender roles, cultural factors, and stigma related to participating. 103 Recruitment of men from diverse backgrounds is particularly challenging in the context of weight management. 10
Rigorous feasibility studies and piloting, with pre‐specified progression criteria, are required before undertaking definitive RCTs, 58 , 104 and this stage may be of particular importance to ensure that prospective trials are likely to reach, engage, and be acceptable to men from lower socioeconomic groups. The “Game of Stones” feasibility trial targeted recruitment activities in postcode areas with higher levels of deprivation, meeting a‐priori enrolment, and feasibility targets. 33 Furthermore, in a feasibility trial of the culturally adapted version of the Healthy Dads Healthy Kids intervention for low‐income Hispanic families, pre‐specified feasibility criteria were largely met, with some modifications to the recruitment strategies suggested. 82 However, in a recent feasibility RCT of the UK adaptation of the same program, which targeted socioeconomically disadvantaged and ethnically diverse localities, a‐priori trial feasibility progression criteria relating to recruitment, attendance, and follow‐up were not met. 77 , 99 These examples highlight the importance of robust assessment of feasibility for interventions targeted at specific socioeconomic or ethnic groups, to best inform decisions around resource allocation for definitive RCTs that have the potential to have a positive effect on health inequalities.
Eleven studies did not report undertaking consultations to inform intervention design or being tailored specifically for men. A qualitative evidence synthesis highlights that program features that help attract and retain men in weight management interventions include having autonomy over dietary intake, some focus on physical activity, social support, and the use of humor. 13 In addition, men may be motivated to attend programs that are in culturally and physically accessible, and that are delivered in non‐threatening settings that align with their masculine identities. 13 For example, in the gender tailored Australian Football themed Aussie‐Fans in Training program, 426 men registered their interest in participating within 3 days of advertising. 35 Despite the clear program appeal, the authors reported limited sample diversity in terms of socioeconomic status and ethnicity. 35 , 105 In the FFIT RCT in Scotland, without specific targeting of recruitment efforts beyond the location of professional football clubs known to attract people from a wide range of socioeconomic backgrounds in their fan base, the program recruited men from across the socioeconomic spectrum. 26 Gender‐tailoring and aligning interventions with men's interests can engage men who would not otherwise participate; however, depending on the context, specific targeting (e.g., in lower socioeconomic areas or regional towns) and tailoring (e.g., for specific ethnic groups) may be required to reach more diverse populations more representative of the burden of obesity‐related disease.
There are concerns that interventions that rely on a high degree of individual agency may exacerbate inequalities. Inequalities can occur at any stage of trials (i.e., during recruitment, adherence, or outcomes) of weight management programs. 106 For example, in a large RCT of brief opportunistic primary care interventions, participants from lower socioeconomic backgrounds that were assigned to the behavioral weight management program referral group, on average, lost less weight than their counterparts from higher socioeconomic backgrounds. 107 This was attributed to those from lower socioeconomic backgrounds attending fewer program sessions (i.e., inequalities related to intervention adherence). 107 Differential effectiveness was only examined in one of the studies included in this review, the FFIT trial. 98 In pre‐specified subgroup analysis, no significant predictors of the interventions effect on weight (the primary outcome) were observed, including for education level, area disadvantage, and employment status. 98 The delivery of FFIT via professional football clubs (a traditionally working‐class game), and alignment to culturally valued masculine identities, may have supported the positive intervention outcomes reported across socioeconomic groups, despite the high levels of agency required from men participating.
RCTs can be classified as “health equity relevant” if they either exclusively focus on a single disadvantaged population subgroup or they assess potential differential effects across the socioeconomic spectrum. 108 No full‐scale studies included in this review targeted specific lower socioeconomic or other disadvantaged groups. Studies are typically designed based on having the power to detect differences in outcomes between intervention and control groups; they often will not be sufficiently powered to assess differential effectiveness. Furthermore, any such subgroup analysis should only be undertaken if they are pre‐specified. 109 In the current review, study sample size was not an inclusion criterion, and most studies were pilot or feasibility studies (n = 20). Only four studies included had a sample size of over 200. Thus, in most of the studies included in this review, subgroup analysis would not be appropriate.
A recent UK study has developed a core outcome set looking to standardize reporting of behavioral weight management interventions for adults to help better understand which interventions work best for which segments of the population. 110 Area level deprivation category was considered a “core” outcome for behavioral weight management interventions, 110 highlighting the importance of measuring, and reporting a measure of socioeconomic status. In the current review, 12 studies reported area level deprivation, all of which were based in either Australia or the UK. However, educational attainment and other potentially relevant socioeconomic characteristics were neither considered “core” nor “optional” outcomes. 110 A key dimension of the RE‐AIM framework, which is commonly used to assess the public health impact of interventions, is intervention reach. 111 If effective programs do not adequately reach lower socioeconomic groups, they may not have a positive effect on health equity. Ideally, studies should consider socioeconomic factors from the outset, when designing interventions. But, where evidence for intervention effectiveness exists, alternative study designs may be considered to more closely examine factors related to intervention reach. For example, in the Healthy Dads Healthy Kids intervention that has been tested in two RCTs in Australia, 37 , 88 the intervention was subsequently trialled in a nonrandomized dissemination study targeting lower socioeconomic regional communities. 112 This study demonstrated that the Healthy Dads Healthy Kids intervention could be delivered by trained local facilitators in lower socioeconomic regional communities, and prior positive trial weight outcomes were largely replicated in this context, including up to 12 months. 112
While a policy priority in many countries, 53 , 54 socioeconomic factors may not always be a top priority for researchers who design and evaluate (weight management) interventions. A recent qualitative study found that although trial Chief Investigators deemed matters relating to equity to be important, the majority were primarily motivated by a commitment to delivering successful trials efficiently. 113 Undertaking trials in less research‐active sites, with higher disease prevalence and lower socioeconomic status, could be seen as a risk to trial success. 113 In the current review, this may be reflected by the majority (n = 20) of trials making no specific mention of the socioeconomic profile of their study sample in relation to strengths or limitations. Moreover, this could also point to the need for a shift in the way that researchers report on the socioeconomic profiles of study samples, and how this information is contextualized in relation to intervention reach, trial outcomes, and the potential for interventions to positively (or negatively) impact health inequalities. Drawing on the CONSORT‐Equity extension guidelines 59 and the studies collated in this review, we propose that researchers reporting on the socioeconomic profiles of study samples
collect characteristic data on and report a minimum of two measures of socioeconomic status that enable, as far as possible, comparison to the wider literature and national population data,
contextualize this data in relation to who the intervention has reached, the trial outcomes, and the potential for impact on health inequalities, and
highlight how this information can inform future research and/or policy
4.2. Strengths and limitations
No previous reviews have a specific focus on socioeconomic factors in men's weight management RCTs. This review included RCTs only and was pre‐registered on PROSPERO, and PRISMA reporting guidelines were adhered to throughout. Usefully, this review includes studies with smaller sample sizes assessing pilot and feasibility outcomes, providing insight into whether studies are designed with equity in mind, targeted to specific socioeconomic groups or have demonstrated feasibility of reaching particular socioeconomic groups for future larger trials.
Due to the heterogeneity of socioeconomic measures across studies and countries, moderation analysis of socioeconomic status on weight outcomes and retention rates was not undertaken. In addition, heterogeneity of measures makes it difficult to make conclusions about the socioeconomic profiles of study samples. Hence, in this review, we did not deviate from how authors reported their studies or look to categorize the degree to which studies may have reached socioeconomic groups. Inequalities can also occur across a range of characteristics that may not be related to socioeconomic status (e.g., race/ethnicity, religion, sexual orientation, and social capital). In this review, we were unable to focus on all of these characteristics, but studies were considered where factors overlapped with a measure of socioeconomic status (e.g., a study targeting low‐income men from a specific ethnic group). 82 Most included studies were from high‐income countries, with little representation from lower‐income countries. This may be partly attributed to the fact that only studies published in English were included. The risk of obesity associated disease is increased in Asian populations at a lower BMI compared to other ethnic groups, 114 , 115 with lower BMI cutoffs for overweight and obesity across Asian‐Pacific countries. 116 , 117 , 118 The inclusion criterion for this review rendered several studies targeted at addressing overweight and obesity in men from Asian countries ineligible due to having a lower BMI criterion. 119 , 120 , 121 , 122 , 123 , 124 , 125 , 126
5. CONCLUSIONS
In trials of interventions with a behavioral component for men that report weight as an outcome, socioeconomic factors are inconsistently reported, men from lower socioeconomic circumstances are rarely targeted or consulted during intervention design, and there is scant evidence that interventions reach or are effective in lower socioeconomic groups. Recent feasibility trials of interventions with a focus on specific socioeconomic and ethnic groups suggest a potential nascent towards a greater consideration of factors related to equity. To best inform public health policy related to health inequalities, in trials of weight management interventions for men, a greater consideration of socioeconomic factors is required during intervention design, conduct, analysis, and reporting.
CONFLICT OF INTEREST
MDM was employed on the Game of Stones feasibility trial, is named as a collaborator on the Game of Stones full‐scale trial as a consultant, contributed to the Aussie‐Fans in Training pilot process evaluation, and his PhD is linked to the Aussie‐Fans in Training intervention. KH was the co‐principal investigator on the FFIT pilot and full‐scale trial, and co‐investigator on the Aussie‐Fans in Training pilot, Hockey Fans in Training pilot, Rugby Fans in Training New Zealand pilot and current full‐scale trial, the EURO‐Fans in Training full‐scale trial, and the current Game of Stones full‐scale trial. NN and DK were co‐investigators, and EQ was the chief‐investigator on the Aussie‐Fans in Training pilot. AA was the chief investigator on the ROMEO systematic review with research recommendations and a co‐investigator on the Game of Stones feasibility and the current full‐scale trial.
AUTHOR CONTRIBUTIONS
MDM conceived the research idea, developed the review protocol, undertook the literature search and study selection process, extracted and synthesized the data, conducted the risk of bias assessment, and managed all aspects of manuscript preparation and submission. KH, DK, AA, and NN helped develop the initial research idea and protocol. HS assisted with study selection and data extraction. JMB assisted with risk of bias assessment. EQ helped develop the initial research idea and protocol and assisted with study selection. All authors reviewed and provided comments on the manuscript, and approved the final version.
FUNDING INFORMATION
Matthew D McDonald is doing a PhD at Curtin University supported by an Australian Government Research Training Program Scholarship. Alison Avenell is employed at the Health Services Research Unit, which is funded by the Chief Scientist Office of the Scottish Government Health and Social Care Directorates. Jack M Birch is supported by the Medical Research Council (MRC) (Grant MC_UU_00006/6).
Supporting information
Figure S1 Example search strategy (Medline, Ovid)
Table S1 Study information, socioeconomic characteristics and related strength or limitation statements
Figure S2 Risk of bias assessment
ACKNOWLEDGMENTS
The authors acknowledge the Wadjuk Nyungar people as the traditional owners of the land on which Curtin University's Bentley campus sits, and we would like to pay respects to elders' past, present, and future. The authors would like to thank the Curtin University librarians Diana Blackwood and Claire Murphy for their advice on developing the search strategy. The authors also thank Zibu Moyo for his assistance with data extraction checking. Open access publishing facilitated by Curtin University, as part of the Wiley ‐ Curtin University agreement via the Council of Australian University Librarians.
McDonald MD, Hunt K, Sivaramakrishnan H, et al. A systematic review examining socioeconomic factors in trials of interventions for men that report weight as an outcome. Obesity Reviews. 2022;23(7):e13436. doi: 10.1111/obr.13436
Funding information Australian Government Research Training Program Scholarship
REFERENCES
- 1. Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all‐cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta‐analysis. Jama. 2013;309(1):71‐82. doi: 10.1001/jama.2012.113905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Di Angelantonio E, Bhupathiraju SN, Wormser D, et al. Body‐mass index and all‐cause mortality: individual‐participant‐data meta‐analysis of 239 prospective studies in four continents. Lancet. 2016;388(10046):776‐786. doi: 10.1016/s0140-6736(16)30175-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ma C, Avenell A, Bolland M, et al. Effects of weight loss interventions for adults who are obese on mortality, cardiovascular disease, and cancer: systematic review and meta‐analysis. BMJ. 2017;359:j4849. doi: 10.1136/bmj.j4849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. LeBlanc ES, Patnode CD, Webber EM, Redmond N, Rushkin M, O'Connor EA. Behavioral and pharmacotherapy weight loss interventions to prevent obesity‐related morbidity and mortality in adults: updated evidence report and systematic review for the US Preventive Services Task Force. Jama. 2018;320(11):1172‐1191. doi: 10.1001/jama.2018.7777 [DOI] [PubMed] [Google Scholar]
- 5. NHS Digital . Statistics on obesity, physical activity and diet, England. 2020. https://digital.nhs.uk/data-and-information/publications/statistical/statistics-on-obesity-physical-activity-and-diet/england-2020
- 6. Scottish Government . Obesity indicators, Scotland. 2018. https://www.gov.scot/publications/obesity-indicators/
- 7. Australian Institute of Health and Welfare . Australia's Health 2020: in brief, Australia. 2020. https://www.aihw.gov.au/reports/australias-health/australias-health-2020-in-brief/contents/summary
- 8. Pagoto SL, Schneider KL, Oleski JL, Luciani JM, Bodenlos JS, Whited MC. Male Inclusion in randomized controlled trials of lifestyle weight loss interventions. Obesity. 2012;20(6):1234‐1239. doi: 10.1038/oby.2011.140 [DOI] [PubMed] [Google Scholar]
- 9. Robertson C, Avenell A, Boachie C, et al. Should weight loss and maintenance programmes be designed differently for men? A systematic review of long‐term randomised controlled trials presenting data for men and women: the ROMEO project. Obes Res Clin Pract. 2016;10(1):70‐84. doi: 10.1016/j.orcp.2015.04.005 [DOI] [PubMed] [Google Scholar]
- 10. Ahern AL, Aveyard P, Boyland EJ, Halford JC, Jebb SA. Inequalities in the uptake of weight management interventions in a pragmatic trial: an observational study in primary care. Br J Gen Pract. 2016;66(645):e258‐e263. doi: 10.3399/bjgp16x684337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Punt SE, Kurz DL, Befort CA. Recruitment of men into a pragmatic rural primary care weight loss trial. Am J Mens Health. 2020;14(6):1557988320971917. doi: 10.1177/1557988320971917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Elliott M, Gillison F, Barnett J. Exploring the influences on men's engagement with weight loss services: a qualitative study. BMC Public Health. 2020;20(1):1‐11. doi: 10.1186/s12889-020-8252-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Archibald D, Douglas F, Hoddinott P, et al. A qualitative evidence synthesis on the management of male obesity. BMJ Open. 2015;5(10):e008372. doi: 10.1136/bmjopen-2015-008372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rounds T, Harvey J. Enrollment challenges: recruiting men to weight loss interventions. Am J Mens Health. 2019;13(1):155798831983212. doi: 10.1177/1557988319832120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Baker EH. Socioeconomic status, definition. In: The Wiley Blackwell Encyclopedia of Health, Illness, Behavior, and Society; 2014:2210‐2214. [Google Scholar]
- 16. Patel L, Alicandro G, La Vecchia C. Dietary approach to stop hypertension (DASH) diet and associated socioeconomic inequalities in the United Kingdom. Brit J Nutr. 2020;1‐24(10):1076‐1085. doi: 10.1017/s0007114520001087 [DOI] [PubMed] [Google Scholar]
- 17. Barton KL, Wrieden WL, Sherriff A, Armstrong J, Anderson AS. Trends in socio‐economic inequalities in the Scottish diet: 2001–2009. Public Health Nutr. 2015;18(16):2970‐2980. doi: 10.1017/s1368980015000361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. NHS Digital . Health survey for England 2016: physical activity in adults. England, 2017. https://files.digital.nhs.uk/publication/m/3/hse16-adult-phy-act.pdf
- 19. O'Donoghue G, Kennedy A, Puggina A, et al. Socio‐economic determinants of physical activity across the life course: a "DEterminants of DIet and physical ACtivity" (DEDIPAC) umbrella literature review. PLoS ONE. 2018;13(1):e0190737. doi: 10.1371/journal.pone.0190737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Beenackers MA, Kamphuis CBM, Giskes K, et al. Socioeconomic inequalities in occupational, leisuretime, and transport related physical activity among European adults: a systematic review. Int J Behav Nutr Phys Act. 2012;9(1):116‐139. doi: 10.1186/1479-5868-9-116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Whitley E, Batty GD, Hunt K, Popham F, Benzeval M. The role of health behaviours across the life course in the socioeconomic patterning of all‐cause mortality: the west of Scotland twenty‐07 prospective cohort study. Ann Behav Med. 2013;47(2):148‐157. doi: 10.1007/s12160-013-9539-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Evans J, Frank B, Oliffe JL, Gregory D. Health, illness, men and masculinities (HIMM): a theoretical framework for understanding men and their health. J Mens Health. 2011;8(1):7‐15. doi: 10.1016/j.jomh.2010.09.227 [DOI] [Google Scholar]
- 23. Dolan A. ‘You can't ask for a Dubonnet and lemonade!’: working class masculinity and men's health practices. Sociol Health Illn. 2011;33(4):586‐601. doi: 10.1111/j.1467-9566.2010.01300.x [DOI] [PubMed] [Google Scholar]
- 24. Taylor Smith A, Dumas A. Class‐based masculinity, cardiovascular health and rehabilitation. Sociol Health Illn. 2019;41(2):303‐324. doi: 10.1111/1467-9566.12827 [DOI] [PubMed] [Google Scholar]
- 25. Richardson A, Allen JA, Xiao H, Vallone D. Effects of race/ethnicity and socioeconomic status on health information‐seeking, confidence, and trust. J Health Care Poor U. 2012;23(4):1477‐1493. doi: 10.1353/hpu.2012.0181 [DOI] [PubMed] [Google Scholar]
- 26. Hunt K, Gray CM, Maclean A, Smillie S, Bunn C, Wyke S. Do weight management programmes delivered at professional football clubs attract and engage high risk men? A mixed‐methods study. BMC Public Health. 2014;14(1):50. doi: 10.1186/1471-2458-14-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Grace B, Richardson N, Carroll P. “... If you're not part of the institution you fall by the wayside”: service providers' perspectives on moving young men from disconnection and isolation to connection and belonging. Am J Mens Health. 2018;12(2):252‐264. doi: 10.1177/1557988316634088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Oliffe JL, Bottorff JL, McKenzie MM, Hislop TG, Gerbrandt JS, Oglov V. Prostate cancer support groups, health literacy and consumerism: are community‐based volunteers re‐defining older men's health? Health. 2011;15(6):555‐570. doi: 10.1177/1363459310364156 [DOI] [PubMed] [Google Scholar]
- 29. Lefkowich M, Richardson N, Robertson S. “If we want to get men in, then we need to ask men what they want”: pathways to effective health programing for men. Am J Mens Health. 2017;11(5):1512‐1524. doi: 10.1177/1557988315617825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sharp P, Spence JC, Bottorff JL, et al. One small step for man, one giant leap for men's health: a meta‐analysis of behaviour change interventions to increase men's physical activity. Brit J Sport Med. 2020;54(20):1208‐1216. doi: 10.1136/bjsports-2019-100912 [DOI] [PubMed] [Google Scholar]
- 31. Young M, Morgan P, Plotnikoff R, Callister R, Collins C. Effectiveness of male‐only weight loss and weight loss maintenance interventions: a systematic review with meta‐analysis. Obes Rev. 2012;13(5):393‐408. doi: 10.1111/j.1467-789X.2011.00967.x [DOI] [PubMed] [Google Scholar]
- 32. Bottorff JL, Seaton CL, Johnson ST, et al. An updated review of interventions that include promotion of physical activity for adult men. Sports Med. 2015;45(6):775‐800. doi: 10.1007/s40279-014-0286-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Dombrowski SU, McDonald M, Van Der Pol M, et al. Game of Stones: feasibility randomised controlled trial of how to engage men with obesity in text message and incentive interventions for weight loss. BMJ Open. 2020;10(2):e032653. doi: 10.1136/bmjopen-2019-032653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sharp P, Stolp S, Bottorff JL, Oliffe JL, Hunt K, Caperchione CM. Can lifestyle interventions improve Canadian men's mental health? Outcomes from the HAT TRICK programme. Health Promot Int. 2020;36(4):943‐951. doi: 10.1093/heapro/daaa120 [DOI] [PubMed] [Google Scholar]
- 35. Kwasnicka D, Ntoumanis N, Hunt K, et al. A gender‐sensitised weight‐loss and healthy living program for men with overweight and obesity in Australian football league settings (Aussie‐FIT): a pilot randomised controlled trial. PLoS Med. 2020;17(8):e1003136. doi: 10.1371/journal.pmed.1003136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Aguiar EJ, Morgan PJ, Collins CE, Plotnikoff RC, Young MD, Callister R. Process evaluation of the type 2 diabetes mellitus PULSE program randomized controlled trial: recruitment, engagement, and overall satisfaction. Am J Mens Health. 2017;11(4):1055‐1068. doi: 10.1177/1557988317701783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Morgan PJ, Lubans DR, Callister R, et al. The ‘Healthy Dads, Healthy Kids’ randomized controlled trial: efficacy of a healthy lifestyle program for overweight fathers and their children. Int J Obes (Lond). 2011;35(3):436‐447. doi: 10.1038/ijo.2010.151 [DOI] [PubMed] [Google Scholar]
- 38. Morgan PJ, Lubans DR, Collins CE, Warren JM, Callister R. 12‐month outcomes and process evaluation of the SHED‐IT RCT: an Internet‐based weight loss program targeting men. Obesity. 2011;19(1):142‐151. doi: 10.1038/oby.2010.119 [DOI] [PubMed] [Google Scholar]
- 39. Hunt K, Wyke S, Gray CM, et al. A gender‐sensitised weight loss and healthy living programme for overweight and obese men delivered by Scottish Premier League football clubs (FFIT): a pragmatic randomised controlled trial. Lancet. 2014;383(9924):1211‐1221. doi: 10.1016/S0140-6736(13)62420-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Morgan PJ, Warren JM, Lubans DR, Collins CE, Callister R. Engaging men in weight loss: experiences of men who participated in the male only SHED‐IT pilot study. Obes Res Clin Pract. 2011;5(3):e239‐e248. doi: 10.1016/j.orcp.2011.03.002 [DOI] [PubMed] [Google Scholar]
- 41. McDonald MD, Dombrowski SU, Skinner R, et al. Recruiting men from across the socioeconomic spectrum via GP registers and community outreach to a weight management feasibility randomised controlled trial. BMC Med Res Methodol. 2020;20(1):1‐15. doi: 10.1186/s12874-020-01136-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Robertson C, Avenell A, Stewart F, et al. Clinical effectiveness of weight loss and weight maintenance interventions for men: a systematic review of men‐only randomized controlled trials (The ROMEO project). Am J Mens Health. 2017;11(4):1096‐1123. doi: 10.1177/1557988315587550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. White M, Adams J, Heywood P. How and why do interventions that increase health overall widen inequalities within populations. In: Social Inequality and Public Health. Vol. 65; 2009:82. [Google Scholar]
- 44. Olstad D, Teychenne M, Minaker L, et al. Can policy ameliorate socioeconomic inequities in obesity and obesity‐related behaviours? A systematic review of the impact of universal policies on adults and children. Obes Rev. 2016;17(12):1198‐1217. doi: 10.1111/obr.12457 [DOI] [PubMed] [Google Scholar]
- 45. Adams J, Mytton O, White M, Monsivais P. Why are some population interventions for diet and obesity more equitable and effective than others? The role of individual agency. PLoS Med. 2016;13(4):e1001990. doi: 10.1371/journal.pmed.1002045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Boelsen‐Robinson T, Peeters A, Beauchamp A, Chung A, Gearon E, Backholer K. A systematic review of the effectiveness of whole‐of‐community interventions by socioeconomic position. Obes Rev. 2015;16(9):806‐816. doi: 10.1111/obr.12297 [DOI] [PubMed] [Google Scholar]
- 47. McGill R, Anwar E, Orton L, et al. Are interventions to promote healthy eating equally effective for all? Systematic review of socioeconomic inequalities in impact. BMC Public Health. 2015;15(1):457. doi: 10.1186/s12889-015-1781-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Western MJ, Armstrong ME, Islam I, Morgan K, Jones UF, Kelson MJ. The effectiveness of digital interventions for increasing physical activity in individuals of low socioeconomic status: a systematic review and meta‐analysis. Int J Behav Nutr Phy. 2021;18(1):1‐21. doi: 10.1186/s12966-021-01218-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Neter E, Brainin E. eHealth literacy: extending the digital divide to the realm of health information. J Med Internet Res. 2012;14(1):e19. doi: 10.2196/jmir.1619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Yoon H, Jang Y, Vaughan PW, Garcia M. Older adults' internet use for health information: digital divide by race/ethnicity and socioeconomic status. J Appl Gerontol. 2018;39(1):105‐110. doi: 10.1177/0733464818770772 [DOI] [PubMed] [Google Scholar]
- 51. Pampel FC, Krueger PM, Denney JT. Socioeconomic disparities in health behaviors. Annu Rev Sociol. 2010;36(1):349‐370. doi: 10.1146/annurev.soc.012809.102529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. O'Mara‐Eves A, Brunton G, Oliver S, Kavanagh J, Jamal F, Thomas J. The effectiveness of community engagement in public health interventions for disadvantaged groups: a meta‐analysis. BMC Public Health. 2015;15(1):1‐23. doi: 10.1186/s12889-015-1352-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Department of Health and Social Care . Prevention is better than cure: our vision to help you live well for longer. England, 2018. https://www.gov.uk/government/publications/prevention-is-better-than-cure-our-vision-to-help-you-live-well-for-longer
- 54. Australian Government . National Men's Health Strategy 2020–2030, Australia, 2019. https://www.health.gov.au/resources/publications/national-mens-health-strategy-2020-2030
- 55. Petticrew M, Whitehead M, Macintyre SJ, Graham H, Egan M. Evidence for public health policy on inequalities: 1: the reality according to policymakers. J Epidemiol Commun H. 2004;58(10):811‐816. doi: 10.1136/jech.2003.015289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Whitehead M, Petticrew M, Graham H, Macintyre SJ, Bambra C, Egan M. Evidence for public health policy on inequalities: 2: assembling the evidence jigsaw. J Epidemiol Commun H. 2004;58(10):817‐821. doi: 10.1136/jech.2003.015297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Bambra C, Hillier F, Cairns J, Kasim A, Moore H, Summerbell C. How effective are interventions at reducing socioeconomic inequalities in obesity among children and adults? Two systematic reviews. Public Health Res. 2015;3(1):1‐446. doi: 10.3310/phr03010 [DOI] [PubMed] [Google Scholar]
- 58. Robertson C, Archibald D, Avenell A, et al. Systematic reviews of and integrated report on the quantitative, qualitative and economic evidence base for the management of obesity in men. Health Technol Assess. 2014;18(35). doi: 10.3310/hta18350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Welch VA, Norheim OF, Jull J, Cookson R, Sommerfelt H, Tugwell P. CONSORT‐Equity 2017 extension and elaboration for better reporting of health equity in randomised trials. BMJ. 2017;359:j5085. doi: 10.1136/bmj.j5085 [DOI] [PubMed] [Google Scholar]
- 60. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Welch VA, Petticrew M, O'Neill J, et al. Health equity: evidence synthesis and knowledge translation methods. Syst Rev. 2013;2(1):1‐10. doi: 10.1186/2046-4053-2-43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Hinde S, Spackman E. Bidirectional citation searching to completion: an exploration of literature searching methods. Pharmacoeconomics. 2015;33(1):5‐11. doi: 10.1007/s40273-014-0205-3 [DOI] [PubMed] [Google Scholar]
- 63. Sterne JA, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 64. Payne RA, Abel GA. UK indices of multiple deprivation—a way to make comparisons across constituent countries easier. Health Stat Q. 2012;53(22):2015‐2016. https://www.proquest.com/scholarly-journals/uk-indices-multiple-deprivation-way-make/docview/1054966975/se-2?accountid=10382 [Google Scholar]
- 65. Mohamad H, Ntessalen M, Craig L, et al. A self‐help diet and physical activity intervention with dietetic support for weight management in men treated for prostate cancer: pilot study of the Prostate Cancer Weight Management (PRO‐MAN) randomised controlled trial. Brit J Nutr. 2019;122(5):592‐600. doi: 10.1017/S0007114519001090 [DOI] [PubMed] [Google Scholar]
- 66. Young MD, Callister R, Collins CE, Plotnikoff RC, Aguiar EJ, Morgan PJ. Efficacy of a gender‐tailored intervention to prevent weight regain in men over 3 years: A weight loss maintenance RCT. Obesity. 2017;25(1):56‐65. doi: 10.1002/oby.21696 [DOI] [PubMed] [Google Scholar]
- 67. Borg P, Kukkonen‐Harjula K, Fogelholm M, Pasanen M. Effects of walking or resistance training on weight loss maintenance in obese, middle‐aged men: a randomized trial. Int J Obes (Lond). 2002;26(5):676‐683. doi: 10.1038/sj.ijo.0801962 [DOI] [PubMed] [Google Scholar]
- 68. Esposito K, Giugliano F, Di Palo C, et al. Effect of lifestyle changes on erectile dysfunction in obese men: a randomized controlled trial. Jama. 2004;291(24):2978‐2984. doi: 10.1001/jama.291.24.2978 [DOI] [PubMed] [Google Scholar]
- 69. Puhkala J, Kukkonen‐Harjula K, Mansikkamäki K, et al. Lifestyle counseling to reduce body weight and cardiometabolic risk factors among truck and bus drivers—a randomized controlled trial. Scand J Work Environ Health. 2015;41(1):54‐64. doi: 10.5271/sjweh.3463 [DOI] [PubMed] [Google Scholar]
- 70. Wyke S, Bunn C, Andersen E, et al. The effect of a programme to improve men's sedentary time and physical activity: the European Fans in Training (EuroFIT) randomised controlled trial. PLoS Med. 2019;16(2):e1002736. doi: 10.1371/journal.pmed.1002736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Patrick K, Calfas KJ, Norman GJ, et al. Outcomes of a 12‐month web‐based intervention for overweight and obese men. Ann Behav Med. 2011;42(3):391‐401. doi: 10.1007/s12160-011-9296-7 [DOI] [PubMed] [Google Scholar]
- 72. Alick C, Samuel‐Hodge C, Ward D, Ammerman A, Rini C, Tate D. Together Eating & Activity Matters (TEAM): results of a pilot randomized‐clinical trial of a spousal support weight loss intervention for Black men. Obes Sci Pract. 2018;4(1):62‐75. doi: 10.1002/osp4.142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Azar KM, Aurora M, Wang EJ, Muzaffar A, Pressman A, Palaniappan LP. Virtual small groups for weight management: an innovative delivery mechanism for evidence‐based lifestyle interventions among obese men. Transl Behav Med. 2015;5(1):37‐44. doi: 10.1007/s13142-014-0296-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Demark‐Wahnefried W, Rais‐Bahrami S, Desmond RA, et al. Presurgical weight loss affects tumour traits and circulating biomarkers in men with prostate cancer. Brit J Cancer. 2017;117(9):1303‐1313. doi: 10.1038/bjc.2017.303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Garcia DO, Valdez LA, Aceves B, et al. A gender‐and culturally sensitive weight loss intervention for Hispanic men: results from the animo pilot randomized controlled trial. Health Educ Behav. 2019;46(5):763‐772. doi: 10.1177/1090198119853011 [DOI] [PubMed] [Google Scholar]
- 76. Gray CM, Hunt K, Mutrie N, Anderson AS, Treweek S, Wyke S. Weight management for overweight and obese men delivered through professional football clubs: a pilot randomized trial. Int J Behav Nutr Phy. 2013;10(1):1‐17. doi: 10.1186/1479-5868-10-121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Griffin T, Sun Y, Sidhu M, et al. Healthy Dads, Healthy Kids UK, a weight management programme for fathers: feasibility RCT. BMJ Open. 2019;9(12):e033534. doi: 10.1136/bmjopen-2019-033534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Irvine L, Crombie IK, Cunningham KB, et al. Modifying alcohol consumption to reduce obesity: a randomized controlled feasibility study of a complex community‐based intervention for men. Alcohol Alcohol. 2017;52(6):677‐684. doi: 10.1093/alcalc/agx067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Mollentze WF, Joubert G, Prins A, van der Linde S, Marx GM, Tsie KG. The safety and efficacy of a low‐energy diet to induce weight loss, improve metabolic health, and induce diabetes remission in insulin‐treated obese men with type 2 diabetes: a pilot RCT. Int J Diabetes Dev C. 2019;39(4):618‐625. doi: 10.1007/s13410-019-00734-1 [DOI] [Google Scholar]
- 80. Shin DW, Yun JM, Shin JH, et al. Enhancing physical activity and reducing obesity through smartcare and financial incentives: a pilot randomized trial. Obesity. 2017;25(2):302‐310. doi: 10.1002/oby.21731 [DOI] [PubMed] [Google Scholar]
- 81. Ventura Marra M, Lilly CL, Nelson KR, Woofter DR, Malone J. A pilot randomized controlled trial of a telenutrition weight loss intervention in middle‐aged and older men with multiple risk factors for cardiovascular disease. Nutrients. 2019;11(2):229. doi: 10.3390/nu11020229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. O'Connor TM, Beltran A, Musaad S, et al. Feasibility of targeting Hispanic fathers and children in an obesity intervention: Papás Saludables Niños Saludables. Child Obes. 2020;16(6):379‐392. doi: 10.1089/chi.2020.0006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Aguiar EJ, Morgan PJ, Collins CE, Plotnikoff RC, Young MD, Callister R. Efficacy of the type 2 diabetes prevention using lifestyle education program RCT. Am J Prev Med. 2016;50(3):353‐364. doi: 10.1016/j.amepre.2015.08.020 [DOI] [PubMed] [Google Scholar]
- 84. Maddison R, Hargreaves EA, Wyke S, et al. Rugby Fans in Training New Zealand (RUFIT‐NZ): a pilot randomized controlled trial of a healthy lifestyle program for overweight men delivered through professional rugby clubs in New Zealand. BMC Public Health. 2019;19(1):166. doi: 10.1186/s12889-019-6472-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Petrella RJ, Gill DP, Zou G, et al. Hockey fans in training: a pilot pragmatic randomized controlled trial. Med Sci Sports Exerc. 2017;49(12):2506‐2516. doi: 10.1249/MSS.0000000000001380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Morgan PJ, Collins CE, Plotnikoff RC, et al. Efficacy of a workplace‐based weight loss program for overweight male shift workers: the Workplace POWER (Preventing Obesity Without Eating like a Rabbit) randomized controlled trial. Prev Med. 2011;52(5):317‐325. doi: 10.1016/j.ypmed.2011.01.031 [DOI] [PubMed] [Google Scholar]
- 87. Morgan PJ, Lubans DR, Collins CE, Warren JM, Callister R. The SHED‐IT randomized controlled trial: evaluation of an Internet‐based weight‐loss program for men. Obesity. 2009;17(11):2025‐2032. doi: 10.1038/oby.2009.85 [DOI] [PubMed] [Google Scholar]
- 88. Morgan PJ, Collins CE, Plotnikoff RC, et al. The ‘Healthy Dads, Healthy Kids’ community randomized controlled trial: a community‐based healthy lifestyle program for fathers and their children. Prev Med. 2014;61:90‐99. doi: 10.1016/j.ypmed.2013.12.019 [DOI] [PubMed] [Google Scholar]
- 89. de Melo CM, dos Santos Quaresma MVL, Del Re MP, et al. One‐month of a low‐energy diet, with no additional effect of high‐protein, reduces obstructive sleep apnea severity and improve metabolic parameters in obese males. Clin Nutr ESPEN. 2021;42:82‐89. doi: 10.1016/j.clnesp.2020.12.028 [DOI] [PubMed] [Google Scholar]
- 90. Johansson K, Neovius M, Lagerros YT, et al. Effect of a very low energy diet on moderate and severe obstructive sleep apnoea in obese men: a randomised controlled trial. BMJ. 2009;339:b4609. doi: 10.1136/bmj.b4609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Kim JY, Oh S, Steinhubl S, et al. Effectiveness of 6 months of tailored text message reminders for obese male participants in a worksite weight loss program: randomized controlled trial. JMIR Mhealth Uhealth. 2015;3(1):e3949. doi: 10.5271/sjweh.3463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Ozaki I, Watai I, Nishijima M, Saito N. Randomized controlled trial of Web‐based weight‐loss intervention with human support for male workers under 40. J Occup Health. 2019;61(1):110‐120. doi: 10.1002/1348-9585.12037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Morgan PJ, Callister R, Collins CE, et al. The SHED‐IT community trial: a randomized controlled trial of internet‐and paper‐based weight loss programs tailored for overweight and obese men. Ann Behav Med. 2013;45(2):139‐152. doi: 10.1007/s12160-012-9424-z [DOI] [PubMed] [Google Scholar]
- 94. Maddison R, Hargreaves EA, Jiang Y, et al. Rugby Fans in Training New Zealand (RUFIT‐NZ): protocol for a randomized controlled trial to assess the effectiveness and cost‐effectiveness of a healthy lifestyle program for overweight men delivered through professional rugby clubs in New Zealand. Trials. 2020;21(1):139. doi: 10.1186/s13063-019-4038-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Kaukua J, Pekkarinen T, Sane T, Mustajoki P. Health‐related quality of life in WHO Class II–III obese men losing weight with very‐low‐energy diet and behaviour modification: a randomised clinical trial. Int J Obes (Lond). 2002;26(4):487‐495. doi: 10.1038/sj.ijo.0801953 [DOI] [PubMed] [Google Scholar]
- 96. Rounds T, Crane M, Harvey J. The impact of incentives on weight control in men: a randomized controlled trial. Am J Mens Health. 2020;14(1):1557988319895147. doi: 10.1177/1557988319895147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Crane MM, Lutes LD, Ward DS, Bowling JM, Tate DF. A randomized trial testing the efficacy of a novel approach to weight loss among men with overweight and obesity. Obesity. 2015;23(12):2398‐2405. doi: 10.1002/oby.21265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Wyke S, Hunt K, Gray C, et al. Football fans in training (FFIT): a randomised controlled trial of a gender‐sensitised weight loss and healthy living programme for men. Public Health Res. 2015;3(2):1‐130. doi: 10.3310/phr03020 [DOI] [PubMed] [Google Scholar]
- 99. Jolly K, Griffin T, Sidhu M, et al. A weight management programme for fathers of children aged 4–11 years: cultural adaptation and the Healthy Dads, Healthy Kids UK feasibility RCT. Public Health Res. 2020;8(2):1‐166. doi: 10.3310/phr08020 [DOI] [PubMed] [Google Scholar]
- 100. Garcia DO, Valdez LA, Bell ML, et al. A gender‐and culturally‐sensitive weight loss intervention for Hispanic males: The ANIMO randomized controlled trial pilot study protocol and recruitment methods. Contemp Clin Trials. 2018;9:151‐163. doi: 10.1016/j.conctc.2018.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. O'Connor TM, Perez O, Beltran A, et al. Cultural adaptation of ‘Healthy Dads, Healthy Kids’ for Hispanic families: applying the ecological validity model. Int J Behav Nutr Phy. 2020;17(1):1‐18. doi: 10.1186/s12966-020-00949-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Dombrowski SU, McDonald M, Van Der Pol M, et al. Text messaging and financial incentives to encourage weight loss in men with obesity: the Game of Stones feasibility RCT. Public Health Res. 2020;8(11):1‐224. doi: 10.3310/phr08110 [DOI] [PubMed] [Google Scholar]
- 103. Bonevski B, Randell M, Paul C, et al. Reaching the hard‐to‐reach: a systematic review of strategies for improving health and medical research with socially disadvantaged groups. BMC Med Res Methodol. 2014;14(1):1‐29. doi: 10.1186/1471-2288-14-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Eldridge SM, Chan CL, Campbell MJ, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. Pilot Feasibility Stud. 2016;2(1):64. doi: 10.1136/bmj.i5239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Kwasnicka D, Donnachie C, Thøgersen‐Ntoumani C, et al. The Aussie‐FIT process evaluation: feasibility and acceptability of a weight loss intervention for men, delivered in Australian Football League settings. Psychol Health. 2021;1‐20. doi: 10.1080/08870446.2021.1890730 [DOI] [PubMed] [Google Scholar]
- 106. Birch JM, Griffin SJ, Kelly MP, Ahern AL. Inequalities in the uptake of, adherence to and effectiveness of behavioural weight management interventions: systematic review protocol. BMJ Open. 2020;10(11):e039518. doi: 10.1136/bmjopen-2020-039518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Graham J, Tudor K, Jebb S, et al. The equity impact of brief opportunistic interventions to promote weight loss in primary care: secondary analysis of the BWeL randomised trial. BMC Med. 2019;17(1):1‐9. doi: 10.1186/s12916-019-1284-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Jull J, Whitehead M, Petticrew M, et al. When is a randomised controlled trial health equity relevant? Development and validation of a conceptual framework. BMJ Open. 2017;7(9):e015815. doi: 10.1136/bmjopen-2016-015815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Petticrew M, Tugwell P, Kristjansson E, Oliver S, Ueffing E, Welch V. Damned if you do, damned if you don't: subgroup analysis and equity. J Epidemiol Community Health. 2012;66(1):95‐98. doi: 10.1136/jech.2010.121095 [DOI] [PubMed] [Google Scholar]
- 110. Mackenzie RM, Ells LJ, Simpson SA, Logue J. Core outcome set for behavioural weight management interventions for adults with overweight and obesity: standardised reporting of lifestyle weight management interventions to aid evaluation (STAR‐LITE). Obes Rev. 2020;21(2):e12961. doi: 10.1111/obr.12961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Glasgow RE, Harden SM, Gaglio B, et al. RE‐AIM planning and evaluation framework: adapting to new science and practice with a 20‐year review. Front Public Health. 2019;7:64. doi: 10.3389/fpubh.2019.00064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Morgan PJ, Collins CE, Lubans DR, et al. Twelve‐month outcomes of a father–child lifestyle intervention delivered by trained local facilitators in underserved communities: the Healthy Dads Healthy Kids dissemination trial. Transl Behav Med. 2019;9(3):560‐569. doi: 10.1093/tbm/ibz031 [DOI] [PubMed] [Google Scholar]
- 113. Rai T, Dixon S, Ziebland S. Shifting research culture to address the mismatch between where trials recruit and where populations with the most disease live: a qualitative study. BMC Med Res Methodol. 2021;21(1):1‐10. doi: 10.1186/s12874-021-01268-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Ding J, Chen X, Bao K, et al. Assessing different anthropometric indices and their optimal cutoffs for prediction of type 2 diabetes and impaired fasting glucose in Asians: the Jinchang cohort study. J Diabetes. 2020;12(5):372‐384. doi: 10.1111/1753-0407.13000 [DOI] [PubMed] [Google Scholar]
- 115. World Health Organisation Expert Commission . Appropriate body‐mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157‐163. doi: 10.1016/S0140-6736(03)15268-3 [DOI] [PubMed] [Google Scholar]
- 116. Misra A, Chowbey P, Makkar B, et al. Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management. Japi. 2009;57(2):163‐170. [PubMed] [Google Scholar]
- 117. Ogawa W, Miyazaki S. Diagnosis criteria for obesity and obesity disease. Health Eval Prom. 2015;42(2):301‐306. doi: 10.7143/jhep.42.301 [DOI] [Google Scholar]
- 118. Pan W‐H, Yeh W‐T. How to define obesity? Evidence‐based multiple action points for public awareness, screening, and treatment: an extension of Asian‐Pacific recommendations. Asia Pac J Clin Nutr. 2008;17(3):370‐374. [PubMed] [Google Scholar]
- 119. Tanaka M, Adachi Y, Adachi K, Sato C. Effects of a non‐face‐to‐face behavioral weight‐control program among Japanese overweight males: a randomized controlled trial. Int J Behav Med. 2010;17(1):17‐24. doi: 10.1007/s12529-009-9057-1 [DOI] [PubMed] [Google Scholar]
- 120. Nanri A, Tomita K, Matsushita Y, et al. Effect of six months lifestyle intervention in Japanese men with metabolic syndrome: randomized controlled trial. J Occup Health. 2012;54(3):215‐222. doi: 10.1539/joh.11-0238-OA [DOI] [PubMed] [Google Scholar]
- 121. Muto T, Yamauchi K. Evaluation of a multicomponent workplace health promotion program conducted in Japan for improving employees' cardiovascular disease risk factors. Prev Med. 2001;33(6):571‐577. doi: 10.1006/pmed.2001.0923 [DOI] [PubMed] [Google Scholar]
- 122. Maruyama C, Kimura M, Okumura H, Hayashi K, Arao T. Effect of a worksite‐based intervention program on metabolic parameters in middle‐aged male white‐collar workers: a randomized controlled trial. Prev Med. 2010;51(1):11‐17. doi: 10.1016/j.ypmed.2010.04.008 [DOI] [PubMed] [Google Scholar]
- 123. Iriyama Y, Murayama N. Effects of a worksite weight‐control programme in obese male workers: a randomized controlled crossover trial. Health Ed J. 2014;73(3):247‐261. doi: 10.1177/0017896912471038 [DOI] [Google Scholar]
- 124. Dong F, Zhang Y, Huang Y, et al. Long‐term lifestyle interventions in middle‐aged and elderly men with nonalcoholic fatty liver disease: a randomized controlled trial. Sci Rep. 2016;6(1):1‐8. doi: 10.1038/srep36783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Tan X, Alén M, Wang K, et al. Effect of six‐month diet intervention on sleep among overweight and obese men with chronic insomnia symptoms: a randomized controlled trial. Nutrients. 2016;8(11):751. doi: 10.3390/nu8110751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Kang JY, Cho SW, Sung SH, Park YK, Paek YM, Choi TI. Effect of a continuous diabetes lifestyle intervention program on male workers in Korea. Diabetes Res Clin Pract. 2010;90(1):26‐33. doi: 10.1016/j.diabres.2010.06.006 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 Example search strategy (Medline, Ovid)
Table S1 Study information, socioeconomic characteristics and related strength or limitation statements
Figure S2 Risk of bias assessment


