Abstract
Objective:
To assess relationships between material hardships, shortened sleep duration, and suboptimal sleep practices across infancy and toddlerhood in low-income Hispanic families.
Methods:
We analyzed longitudinal data of 451 low-income Hispanic mother-child pairs from a child obesity prevention trial. During infancy and toddlerhood, we used adjusted linear regression to assess associations between material hardship (financial difficulty, food insecurity, housing disrepair, multiple hardships), sleep duration (24-hour, night), and the number of suboptimal sleep practices (e.g., later bedtime, co-sleeping). We used adjusted linear regression to assess the longitudinal association between the number of suboptimal sleep practices in infancy and toddlerhood, and tested whether specific or multiple hardships moderated this association.
Results:
In infants, financial difficulty and multiple hardships were associated with decreased night sleep (B=−0.59 hours, 95% CI: −1.04, −0.14; and B=−0.54 hours, 95% CI: −1.00, −0.08). Housing disrepair was associated with decreased 24-hour sleep (B=−0.64 hours, 95% CI: −1.29, −0.01). In toddlers, each additional suboptimal sleep practice was associated with a decrease in night sleep (B=−0.19 hours, 95% CI: −0.29, −0.09). Each additional suboptimal sleep practice in infancy was associated with a 0.30 increase in the number of suboptimal sleep practices in toddlerhood (p<0.001), with greater increases for those with food insecurity or multiple hardships.
Conclusion:
Specific and multiple hardships shortened sleep duration during infancy, and moderated the increase of suboptimal sleep behaviors between infancy and toddlerhood. Future studies should consider these early critically sensitive periods for interventions to mitigate material hardships and establish healthy sleep practices.
Keywords: Social Determinants of Health, Bedtime Routine, Food Insecurity, Housing Disrepair, Financial Difficulty
INTRODUCTION
Poverty-related disparities in sleep emerge during infancy and toddlerhood.1,2 Shortened night sleep is linked to long-term adverse outcomes such as lack of school readiness,3 slowed language development,4 behavior problems,5 and child obesity.6 Adjusting for income reduced the gap in night sleep duration between Hispanic and white infants, suggesting that poverty has specific relationships with sleep early in life.1 While research has identified poverty-related disparities in sleep,1,2,6 less is known about the mechanisms behind how poverty affects sleep in infants and toddlers.
The American Academy of Pediatrics (AAP) has endorsed recommendations around sleep duration and practices in young children. While total 24-hour sleep indicates overall sleep adequacy in this age group,7,8 night sleep duration, which increases incrementally in the first 4 to 12 months of life,9 indicates sleep maturation.10 In toddlers, setting an appropriate and consistent bedtime,11 implementing a bedtime routine,12 and decreasing nighttime awakenings13,14 are all practices associated with longer night sleep. Environmental practices detrimental to night sleep include sleep arrangements (co-sleeping),15 sleep location (sleeping in parent’s room),16 or the presence of a television where the child sleeps.6,17
Material hardship, or the inability of families to meet basic needs such as financial difficulty, housing disrepair or food insecurity, may represent a mechanism linking poverty to poor sleep outcomes. Material hardships have effects on child health that extend beyond the effect of low income alone.18 Specific material hardships have been associated with adverse outcomes like infant and toddler wellness,19 regulatory capacity,20 and maternal locus of control,21 and thus may impact sleep as well. Poor housing conditions limit a parent’s perceived options on where the baby can sleep,22 directly impacting the baby’s physical sleep space. Food insecurity during pregnancy has been linked to a decreased maternal locus of control and a belief in greater control by others, which in turn may decrease maternal confidence in implementing healthy sleep practices.21 Financial difficulties, previously associated with short sleep trajectories in young children,23 may result in increased family stress. Finally, while multiple hardships have negative effects on parenting outcomes,19,21 less is known about whether the additive impact of multiple hardships have similar impacts on early sleep.
The AAP recommends establishing healthy sleep practices in infancy to avoid sleep problems in toddlerhood and beyond.24,25 However, less is known about whether material hardships affect the trajectory of suboptimal sleep practices from infancy through toddlerhood. Children living in poverty develop differently than children not in poverty with regards to well-being,26 and the way sleep practices evolve between infancy and toddlerhood may be different based on exposure to material hardships.
To fill these gaps, we assessed relationships between material hardships, shortened sleep duration, and suboptimal sleep practices across infancy and toddlerhood in low-income Hispanic families. We hypothesized that: 1) having specific hardships (financial difficulties, housing disrepair, food insecurity) and having multiple material hardships (2 or more) would be associated with shortened sleep duration and suboptimal sleep practices; and 2) material hardships would moderate the longitudinal association between the number of suboptimal sleep practices from infancy and toddlerhood.
METHODS
Study Design
We analyzed longitudinal data from the Starting Early Program (StEP) randomized controlled trial. StEP is a primary care-based child obesity prevention program designed to promote healthy infant growth. The trial enrolled pregnant women between August 2012 and December 2014, ending in June 2018. This trial was approved by the Institutional Review Board of New York University School of Medicine, by the New York City Health + Hospitals, and was registered on clinicaltrials.gov (NCT01541761).
Study Sample
Pregnant women were recruited in a large urban public hospital in New York City. Inclusion criteria included pregnant adult women who self-identified as Hispanic or Latina, were fluent in English or Spanish, had a singleton pregnancy, with available contact information, and who intended to receive pediatric care at the study site.27 Exclusion criteria included women with severe illness, pregnancy complications, homelessness, or substance use disorders.
Five hundred and thirty-three pregnant women were randomized into the trial. For our analysis, we included 451 mother-child pairs (85%) who had complete data at the prenatal and 2 year timepoints. Material hardship variables were collected prenatally (third trimester of pregnancy) and in early toddlerhood (19 months). Sleep duration and suboptimal sleep practice variables were collected in infancy (3 months) and in late toddlerhood (2 years).
Measures
Sleep Duration
Our team adapted questions from the Brief Infant Sleep Questionnaire (BISQ), a clinically and cross-culturally validated survey for infants and toddlers.28,29 From the BISQ,28 we assessed total daytime sleep duration with “How much total time does your baby sleep during the day?” Night sleep, our indicator of night sleep duration, was an assessment of night sleep opportunity or time in bed. To assess night sleep, we asked, “What time does your baby/child go to bed on a typical night?” and “What time does your baby/child wake up on a typical day?” We calculated night sleep as the number of hours between bedtime and wake time. Total 24-hour sleep was calculated by adding total daytime nap duration and night sleep. Our adaptation of the BISQ underwent a formal process where questions were translated, back-translated, then culturally adapted by a native Spanish speaking team of community providers and nutritionists.
Suboptimal Sleep Practices
Suboptimal sleep practices were coded 1–7 (infants) or 1–8 (toddlers) by summing the total number of suboptimal sleep practices and treated as a continuous variable, allowing each suboptimal sleep practice to contribute equally to the score: 1) later bedtime,11 2) no regular bedtime,12 3) no regular bedtime routine12 (toddler only), 4) increased night awakenings,13 5) sleep arrangements (co-sleeping),15 6) suboptimal sleep location (sleeping in parent’s room),16 7) television in room where baby sleeps,6,17 and 8) perception of sleep problems.28
We assessed later bedtime with the BISQ item, “What time do you put your baby to bed?” We categorized later bedtime as 9PM or later based on prior literature.11,14 We assessed regular bedtime and regular bedtime routine using adapted questions from the Bright Futures guidelines,25 “Does your child have a regular bedtime?” and “Does your child have a regular bedtime routine?” Responses were categorized as “yes” or “no.” We assessed increased night time awakenings using the BISQ item, “What is the average number of times your baby wakes up each night?” We categorized increased night awakenings as a parent reported average of more than one awakening per night.14
In the infant period, we assessed both sleep arrangements and location using an adapted BISQ item, “Where does your baby usually sleep?” Options included “infant crib in a separate room,” “infant crib in the parent’s room,” “in parents’ bed,” “infant crib in a room with sibling,” and “other.” We categorized co-sleeping as “in parents’ bed” vs. all others. We categorized “infant crib in the parents’ room” as the optimal sleep arrangement vs. all others.
In the toddler period, we assessed sleep arrangements and location using an adapted BISQ item, “Where does your child usually sleep?” Options included, “crib in a separate room,” “crib in your room,” “crib in a room with sibling,” “in his/her own bed in a separate room,” “in his/her own bed in your room,” “in his/her own bed in a room with a sibling,” “in your bed,” and “other.” We categorized co-sleeping as “in your bed” vs. all others. In toddlerhood, we categorized suboptimal sleep location as any answer that was not “crib/bed in separate room” or “crib/bed in room with sibling.” We assessed having a television in the room where the baby sleeps with the BISQ item, “Is there a television in the room where the child sleeps?” We categorized answers as “yes” or “no.” We assessed sleep problems with the BISQ item, “Do you consider your child’s sleep to be a problem?” We categorized the answers as “A very big problem” and “A small problem” together vs. “Not a problem at all.”
Material Hardships
Financial Difficulties was assessed using 2 questions from the United States Census Bureau’s Survey of Income and Program Participation (SIPP).30 The questions assessed whether in the last 12 months, mothers experienced: 1) serious financial problems or were unable to pay monthly bills, rent or mortgage; or 2) having service turned off by the gas, electric or telephone company. We coded financial difficulties as responding “yes” to either one or both questions.
Housing Disrepair was also assessed using the SIPP.30 The questions assessed whether any of the following conditions were present in the home: 1) rats, mice, roaches or other insects; 2) a leaking roof or ceiling; 3) a toilet, hot water heater or other plumbing that doesn’t work; 4) broken windows; 5) exposed electric wires; 6) holes in the floor (large enough to trip in); and 7) open cracks or holes in the walls or ceiling. We coded housing disrepair as an answer of “yes” to one or more of the above conditions.
Food Insecurity was assessed using the United States Department of Agriculture’s Core Food Security Module,31 which consists of 10 questions assessing adult food insecurity in the prior 12 months. While the survey’s validated guidelines list 4 categories, our sample did not have a broad range across the categories. For our analysis, we coded those who had low or very low food security as food insecure.21,30
We created the multiple hardships variable by totaling the number of hardships, and dichotomizing 2 or more hardships vs. 0–1 hardships. This cutpoint was based on prior literature about the impact of multiple hardships on child outcomes.19–21
Covariates
Maternal characteristics included age, education, marital status, and US born status. Child characteristics included sex and firstborn status. Maternal depressive symptoms were measured in pregnancy and early toddlerhood using the Patient Health Questionnaire-9. We used the recommended scoring, 5–27 as “yes” and 0–4 as “no.”32 We included intervention group status as a covariate because while the intervention did not target sleep, parenting groups likely promote parental self-efficacy around routines, which could impact sleep knowledge.
Statistical Analysis
Statistical analyses were performed using Stata/SE version 15 (Stata Corp, College Station, TX). We used descriptive statistics to summarize sample characteristics including material hardships, sleep practices, and sleep duration.
To investigate the effects of material hardship on sleep duration in infants and toddlers, we performed separate adjusted linear regression models to study the association between material hardship variables (financial difficulty, housing disrepair, food insecurity, multiple hardships) and sleep duration variables (night sleep and total 24-hour sleep), adjusting for covariates listed above along with intervention status. Next, we performed adjusted linear regressions to assess associations between material hardship variables and the number of suboptimal sleep practices in each age group.
We then performed an adjusted linear regression to study the association between the number of suboptimal sleep practices in infancy and the number in toddlerhood. Next, using stratified analyses and by adding interaction terms to the regression models, we investigated whether the presence or absence of material hardship variables moderated this association. Moderation was analyzed in separate models through inclusion of an interaction term calculated by multiplying together the dichotomous variables defined for the moderator (material hardship) and the predictor (suboptimal sleep practices in infancy). We conducted simple slope analyses to see whether the association between the number of suboptimal sleep practices in infancy and toddlerhood was significant in the presence and in the absence of each material hardship variable.
RESULTS
Study Sample
Table 1 summarizes our sample characteristics. We had a retention rate of 84.6%, and those lost to follow-up were more likely to be first born (48.8% lost vs. 35.3% followed, p<0.05), more likely to have finished high school (76.8% lost vs. 65.0% followed, p<0.05), more likely to be US born (30.4% lost vs. 18.1% followed, p<0.01). There were no significant differences in material hardships between these two groups.
Table 1:
Study Sample Characteristics (n=451)
| Sociodemographic Information, N (%) | |
|---|---|
| Mother | |
| Mean Maternal Age (years) (median, interquartile range) | 28.6 (28.0, 23.7–33.0) |
| Maternal Education Less than High School | 158 (35.0%) |
| Married or Living as Married | 324 (71.8%) |
| Birth Country | |
| United States | 83 (18.4%) |
| Mexico | 227 (50.3%) |
| Ecuador | 73 (16.2%) |
| Dominican Republic | 21 (4.7%) |
| Central America (Guatemala, Colombia, El Salvador, Honduras, Nicaragua, Panama, Costa Rica) | 37 (8.2%) |
| South America (Peru, Bolivia, Paraguay, Venezuela) | 10 (2.2%) |
| Depressive Symptoms | 143 (31.8%) |
| On WIC | 396 (87.8%) |
| Child | |
| First Child | 159 (35.3%) |
| Female | 227 (50.3%) |
| Study Variables Across 2 Timepoints, N (%) | ||
|---|---|---|
| Material Hardships | Prenatal | Early Toddler 1 |
| Financial Difficulties | 120 (26.6%) | 102 (26.4%) |
| Housing Disrepair | 156 (34.6%) | 131 (33.9%) |
| Food Insecurity | 143 (31.7%) | 65 (16.8%) |
| Multiple Hardships (2+) | 116 (25.7%) | 80 (20.7%) |
| Sleep Duration | Infant | Toddler |
| Mean 24 Hour Sleep (median, IQR) | 14.1 (14.0, 12.0–16.0) | 11.8 (12.0, 11.0–12.5) |
| Mean Night Sleep (median, IQR) | 9.2 (9.0, 8.0–10.5) | 10.7 (11.0, 10.0–12.0) |
| Suboptimal Sleep Practices | Infant | Toddler |
| Awakenings (>1 overnight) | 231 (51.3%) | 24 (6.5%) |
| Sleep Onset (9PM or after) | 372 (83.4%) | 212 (56.8%) |
| Sleep Arrangements (co-sleeping) | 35 (7.8%) | 100 (27.3%) |
| Sleep Location2 | 69 (15.3%)2 | 307 (83.7%) |
| Sleep as a Problem | 69 (15.3%) | 61 (16.4%) |
| TV in Room | 340 (75.4%) | 261 (70.9%) |
| No Regular Bedtime | 159 (35.3%) | 73 (19.8%) |
| No Regular Bedtime Routine3 | - | 117 (31.5%) |
Material hardships data available for 386 toddlers.
In infants, suboptimal sleep practice for sleep location is to sleep separately from parents. In toddlers, suboptimal sleep practice is to room in with parents.
Regular bedtime routine information not available for infants.
As would be expected, night sleep was shorter and total 24-hour sleep was longer for infants when compared to toddlers. Infants also had more night awakenings (51.3% infants vs. 6.3% toddlers, p<0.001), later bedtimes (83.5% infants vs. 57.4% toddlers, p<0.001), were less likely to have a regular bedtime (62.5% infants vs. 80.2% toddlers, p<0.001) and less likely to be co-sleeping (8.0% infants vs. 27.3% toddlers). There were no significant differences in whether there was a television where the baby slept or whether sleep was a problem.
Material Hardships and Sleep Outcomes (Table 2)
Table 2:
Material Hardships and Sleep Duration in Infancy and Toddlerhood (n = 451)
| Prenatal Material Hardships | Infant Total 24 Hour Sleep1 B (95% CI)2 | Infant Night Sleep1 B (95% CI)2 |
|---|---|---|
| Financial Difficulties | 0.28 (−0.42, 0.97) | −0.59 (−1.04, −0.14)* |
| Housing Disrepair | −0.64* (−1.29, 0.01) | −0.18 (−0.59, 0.23) |
| Food Insecurity | 0.29 (−0.38, 0.96) | −0.33 (−0.76, −0.10) |
| Multiple Hardships | −0.23 (−0.94, 0.49) | −0.54* (−1.00, −0.08) |
| Toddler Material Hardships | Toddler Total 24 Hour Sleep1 B (95% CI)2 | Toddler Night Sleep1 B (95% CI)2 |
| Financial Difficulties | 0.16 (−0.18, 0.51) | 0.06 (−0.27, 0.38) |
| Housing Disrepair | 0.07 (−0.25, 0.40) | 0.005 (−0.30, 0.31) |
| Food Insecurity | −0.29 (−0.70, 0.13) | −0.02 (−0.42, 0.37) |
| Multiple Hardships | −0.05 (−0.44, 0.33) | 0.006 (−0.36, 0.37) |
Linear regression adjusting for maternal age, high school education, first born child, child gender, marital status, US born, maternal depressive symptoms, and intervention group status.
Unstandardized coefficients in hours.
p<0.05
Infant Sleep
Financial difficulty was associated with decreased night sleep (B=−0.59 hours, 95% CI: −1.04, −0.14). Multiple hardships had a similar effect size as financial difficulty on decreasing night sleep (B=−0.54 hours, 95% CI: −1.00, −0.08). Housing disrepair was associated with decreased total 24-hour sleep (B=−0.64 hours, 95% CI: −1.29, −0.01).
In infants, there were no significant associations between material hardships and the number of suboptimal sleep practices. There was also no association between the number of suboptimal sleep practices and sleep duration.
Toddler Sleep
In toddlers, there were no significant associations between material hardships and sleep duration. In adjusted linear regression models, multiple hardships was associated with an increase in suboptimal sleep behaviors (B=0.44 behaviors, 95% CI: 0.03, 0.84). As expected, each additional suboptimal sleep practice was associated with an additional decrease in night sleep (B=−0.19 hours, 95% CI: −0.29, −0.09).
Longitudinal Association Between Suboptimal Sleep Practices from Infancy to Toddlerhood
In adjusted linear regression, each additional suboptimal sleep practice reported in the infant period was associated with an increase in the number of suboptimal sleep practices in toddlerhood (B=0.30 behaviors, 95% CI: 0.17, 0.43).
Moderation of Longitudinal Association of Suboptimal Sleep Behaviors by Material Hardships
In toddlers not exposed to food insecurity, each suboptimal sleep practice in infancy was associated with a 0.21 (p<0.01) increase in the number of practices reported in toddlerhood (Table 3). In toddlers exposed to food insecurity, each suboptimal sleep practice in infancy was associated with a 0.53 (p<0.01) increase in the number of practices in toddlerhood (interaction term B=0.31, p=0.06). In simple slope analysis, the p-values for both slopes (exposed and not exposed to food insecurity) were <0.001. In toddlers not exposed to multiple hardships, each suboptimal sleep practice in infancy was associated with a 0.20 (p<0.05) increase in the number of practices in toddlerhood (Figure 1). In toddlers exposed to multiple hardships, each suboptimal sleep practice in infancy was associated with a 0.49 (p<0.01) increase in the number of practices in toddlerhood (interaction term, B=0.28, p=0.06). In simple slope analysis, the p-values for both slopes (exposed and not exposed to multiple hardships) were <0.001. Financial difficulty or housing disrepair did not moderate the longitudinal association between suboptimal sleep practices in infancy and toddlerhood.
Table 3:
Subgroup Analysis, Association of # of Suboptimal Sleep Practices From Infancy to Toddlerhood
| Material Hardship | Change in # of Suboptimal Sleep Practices (Infancy to Toddlerhood) B2 (95% CI) | |
|---|---|---|
| Full Sample | 0.30 (0.17, 0.43)*** | |
| Food Insecurity | Present | 0.53 (0.22, 0.85)** |
| Absent | 0.21 (0.06, 0.36)** | |
| Multiple Hardships | Present | 0.49 (0.22, 0.76)** |
| Absent | 0.20 (0.04, 0.35)* | |
Linear regression adjusted for maternal age, high school education, first born child, child gender, marital status, US born, maternal depressive symptoms, and intervention group status.
Unstandardized coefficient in # of behaviors.
p<0.05,
p<0.01,
p<0.001
Figure 1:
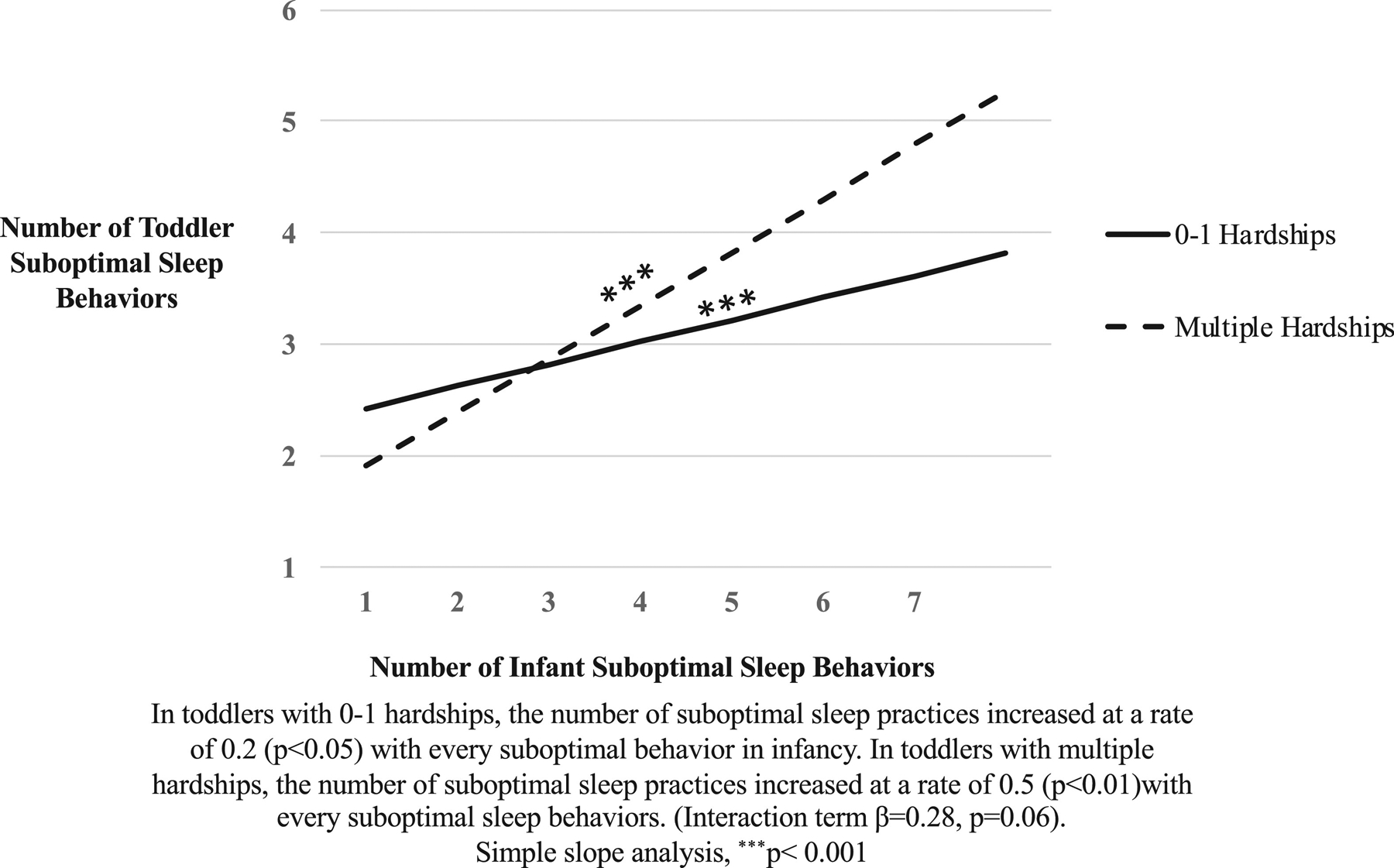
Multiple Hardships Moderate Longitudinal Change in Suboptimal Sleep Behaviors
DISCUSSION
In this sample of low-income Hispanic families with young children, we examined relationships between material hardships, sleep duration, and sleep practices. For our first hypothesis, we were able to show during infancy that financial difficulty and multiple hardships were inversely associated with night sleep and that housing disrepair was inversely associated with total 24-hour sleep. While we were unable to show similar associations during toddlerhood, we found in toddlers that multiple hardships were associated with an increased number of suboptimal sleep practices. For our second hypothesis, we identified an association between the number of suboptimal sleep practices in infancy and the number of suboptimal sleep practices in toddlerhood. This relationship increased with food insecurity and multiple hardships.
Our study strengthens existing literature about poverty and sleep duration in children,1,2 by identifying associations between material hardships and infant sleep duration. Financial difficulties, or the inability to pay bills, may be due to unsteady employment, increasing parental stress or disrupting parent night sleep, which has been found to shorten night sleep in other age groups.33 While we found a similar association between multiple hardships and night sleep, no associations was detected between these two variables with total 24-hour sleep, suggesting that high levels of parental stress may interfere with night sleep consolidation, but not overall infant sleep adequacy.
Our finding that housing disrepair was associated with shortened total 24-hour sleep extends prior literature linking poor home environments and sleep quality in school-aged children,34 by extending the age range to include infants. The relationship between housing disrepair and total 24-hour sleep, but not night sleep, may be related to concrete challenges in the sleep environment, such as noise, that impact overall sleep adequacy. Food insecurity was not associated with any sleep duration variable in infancy. Our food insecurity measure was on the adult level, and prior literature has found that food insecurity is not consistently linked with child-level outcomes because parents often shield their children from food insecurity,35 and they may be even more likely to guard infants.
No association was identified between suboptimal sleep practices and sleep duration in infancy, though in toddlers we found an eleven minute decrease in night sleep for each suboptimal sleep practice. This may be due to the more prominent role of sleep practices for toddlers, after sleep consolidation in infancy is complete. We also identified an association between multiple hardships and an increase in the number of suboptimal sleep practices in toddlers, suggesting an additive effect of material hardships on outcomes.
Our findings have clinical implications. Prior evidence in slightly older children has found that a 30 minute decrease in night sleep was associated with not meeting kindergarten educational standards,36 and that a 65 minute decrease in toddler night sleep was associated with eating in the absence of hunger as well as emotional overeating.37 Reinforcing prior evidence about the advantage of starting early to establish key behaviors,38 we identified an association between the number of suboptimal sleep practices in infancy and the number in toddlerhood. Furthermore, we found that material hardships modify the change in suboptimal sleep practices between infancy and toddlerhood. Children exposed to food insecurity had a steeper increase in the number of suboptimal sleep practices between infancy and toddlerhood compared to children not exposed to food insecurity. Food insecurity has been associated with indulgent feeding styles,39 which may extend to indulgent bedtime parenting and therefore suboptimal sleep practices. We found a similar interaction with our multiple hardships variable, which reinforces prior work showing that families with food insecurity or housing disrepair are less likely to implement a nightly bedtime.2
Overall, these results represent a framework to study how specific social determinants relate to sleep practices during critical periods in early childhood. The association between social determinants and health has already led to the development of clinical screening programs to connect families to services.40 Medical homes have the ability to advocate on the behalf of families by writing letters to landlords or connecting families to social services. This study not only supports social needs screening and connection to resources to directly mitigate hardships, but also suggests social needs screening early in life so knowledge about a family’s social needs can be folded into anticipatory guidance7 about establishing optimal sleep practices. Prior evidence has already identified sleep routines as a potential source of resilience for at-risk children,41 and our study strengthens this body of work by emphasizing the importance of targeting early behaviors.
Study limitations relate to our parent-reported measures, loss to follow-up, and generalizability. Our measure of night sleep was a calculation between bedtime and wake time, which represents night sleep opportunity rather than true night sleep duration. Sophisticated sleep studies rely on direct actigraphy. However, infant studies show that actigraphy can overestimate night-waking given active infant sleep and self-soothing, limiting its validity in this age group.42 Next, our measure for suboptimal sleep practices weighed each sleep practice equally. While it was beyond the scope of this study, research should continue to elucidate the differential impact of each suboptimal sleep behavior on sleep duration. Based on the characteristics of our patients excluded from these analyses due to missing data (~15% of the original sample), those excluded were more likely to have higher education and be US born. However, there was no difference in the prevalence of material hardships between those followed and those lost, so our sample is likely still be representative. Due to the inability of a cross-sectional design to infer causality to any extent, we balanced the increased degree of causal inference against the potential bias of follow-up loss in a longitudinal design.
Finally, our findings may not be generalizable to all families experiencing material hardships. Our sample lived in an urban setting, where housing disrepair likely takes place in small apartments, while housing disrepair in rural and suburban settings may occur in larger spaces with potentially different environmental impacts on sleep. Furthermore, due to the diverse Hispanic composition of our sample, there may be unmeasured cultural beliefs around sleep that could affect practices.
CONCLUSION
Specific and multiple hardships were associated with indicators of shortened sleep duration in infancy but not in toddlerhood. The association between the number of suboptimal sleep practices in infancy and in toddlerhood varied according to the presence or absence of specific and multiple hardships. Programs and policies that aim to prevent poverty-related disparities should not only consider how material hardships may affect sleep outcomes, but also recognize early critically sensitive periods for interventions to establish healthy sleep practices and mitigate material hardships.
WHAT’S NEW.
Material hardships are associated with shortened infant sleep duration, and moderate the longitudinal change in suboptimal sleep practices between infancy and toddlerhood. These findings identify early critical periods to mitigate material hardships and establish healthy sleep practices.
ACKNOWLEDGEMENTS
We thank the Starting Early Program staff who contributed to this project. This work was supported by: the National Institute of Food and Agriculture, USDA# 2011-68001-30207 (Drs. Messito, Gross); HRSA T32HP22238 and CTSI NCATS 1UL 1TR001445 training grants (Dr. Duh-Leong); and a K23 Mentored Patient-Oriented Research Career Development Award NICHD K23HD081077 (Dr. Gross). These funding sources had no involvement in conducting the research or in preparing this article.
Financial Disclosure Statement: The authors have no financial relationships relevant to this article to disclose.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Potential Conflicts of Interest: The authors have no conflicts of interest relevant to this article to disclose.
REFERENCES
- 1.Ash T, Davison KK, Haneuse S, et al. Emergence of racial/ethnic differences in infant sleep duration in the first 6 months of life. Sleep Medicine: X Published online May 18, 2019:100003. doi: 10.1016/j.sleepx.2019.100003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Covington LB, Rogers VE, Armstrong B, Storr CL, Black MM. Toddler bedtime routines and associations with nighttime sleep duration and maternal and household factors. JCSM 2019;15(06):865–871. doi: 10.5664/jcsm.7838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berger RH, Diaz A, Valiente C, et al. Sleep duration moderates the association between children’s temperament and academic achievement. Early Education and Development 2018;29(5):624–640. doi: 10.1080/10409289.2017.1404884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dionne G, Touchette E, Forget-Dubois N, et al. Associations between sleep-wake consolidation and language development in early childhood: a longitudinal twin study. Sleep 2011;34(8):987–995. doi: 10.5665/SLEEP.1148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sadeh A, Marcas GD, Guri Y, Berger A, Tikotzky L, Bar-Haim Y. Infant sleep predicts attention regulation and behavior problems at 3–4 years of age. Developmental Neuropsychology 2015;40(3):122–137. doi: 10.1080/87565641.2014.973498 [DOI] [PubMed] [Google Scholar]
- 6.Taveras EM, Gillman MW, Kleinman KP, Rich-Edwards JW, Rifas-Shiman SL. Reducing racial/ethnic disparities in childhood obesity: the role of early life risk factors. JAMA Pediatr 2013;167(8):731–738. doi: 10.1001/jamapediatrics.2013.85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Academy of Pediatrics supports childhood sleep guidelines. AAP.org. Accessed October 9, 2019. http://www.aap.org/en-us/about-the-aap/aap-press-room/Pages/American-Academy-of-Pediatrics-Supports-Childhood-Sleep-Guidelines.aspx [Google Scholar]
- 8.Paruthi S, Brooks LJ, D’Ambrosio C, et al. Consensus Statement of the American Academy of Sleep Medicine on the Recommended Amount of Sleep for Healthy Children: Methodology and Discussion. J Clin Sleep Med 2016;12(11):1549–1561. doi: 10.5664/jcsm.6288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Henderson JMT, France KG, Owens JL, Blampied NM. Sleeping through the night: the consolidation of self-regulated sleep across the first year of life. Pediatrics 2010;126(5):e1081–1087. doi: 10.1542/peds.2010-0976 [DOI] [PubMed] [Google Scholar]
- 10.Henderson JMT, France KG, Blampied NM. The consolidation of infants’ nocturnal sleep across the first year of life. Sleep Medicine Reviews 2011;15(4):211–220. doi: 10.1016/j.smrv.2010.08.003 [DOI] [PubMed] [Google Scholar]
- 11.Mindell JA, Meltzer LJ, Carskadon MA, Chervin RD. Developmental aspects of sleep hygiene: Findings from the 2004 National Sleep Foundation Sleep in America Poll. Sleep Medicine 2009;10(7):771–779. doi: 10.1016/j.sleep.2008.07.016 [DOI] [PubMed] [Google Scholar]
- 12.Mindell JA, Williamson AA. Benefits of a bedtime routine in young children: Sleep, development, and beyond. Sleep Medicine Reviews 2018;40:93–108. doi: 10.1016/j.smrv.2017.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weinraub M, Bender RH, Friedman SL, et al. Patterns of developmental change in infants’ nighttime sleep awakenings from 6 through 36 months of age. Developmental Psychology 2012;48(6):1511–1528. doi: 10.1037/a0027680 [DOI] [PubMed] [Google Scholar]
- 14.Hager ER, Calamaro CJ, Bentley LM, Hurley KM, Wang Y, Black MM. Nighttime sleep duration and sleep behaviors among toddlers from low-income families: associations with obesogenic behaviors and obesity and the role of parenting. Childhood Obesity. 2016;12(5):392–400. doi: 10.1089/chi.2015.0252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mao A, Burnham MM, Goodlin-Jones BL, Gaylor EE, Anders TF. A comparison of the sleep–wake patterns of cosleeping and solitary-sleeping infants. Child Psychiatry Hum Dev 2004;35(2):95–105. doi: 10.1007/s10578-004-1879-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paul IM, Hohman EE, Loken E, et al. Mother-infant room-sharing and sleep outcomes in the insight study. Pediatrics 2017;140(1). doi: 10.1542/peds.2017-0122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cespedes EM, Gillman MW, Kleinman K, Rifas-Shiman SL, Redline S, Taveras EM. Television viewing, bedroom television, and sleep duration from infancy to mid-childhood. Pediatrics. 2014;133(5):e1163–e1171. doi: 10.1542/peds.2013-3998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gershoff ET, Aber JL, Raver CC, Lennon MC. Income is not enough: incorporating material hardship into models of income associations with parenting and child development. Child Development 2007;78(1):70–95. doi: 10.1111/j.1467-8624.2007.00986.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Frank DA, Casey PH, Black MM, et al. Cumulative hardship and wellness of low-income, young children: multisite surveillance study. Pediatrics 2010;125(5):e1115–1123. doi: 10.1542/peds.2009-1078 [DOI] [PubMed] [Google Scholar]
- 20.Fuller A, Messito MJ, Mendelsohn AL, Oyeku SO, Gross RS. Prenatal Material Hardships and Infant Regulatory Capacity at 10 Months Old in Low-Income Hispanic Mother-Infant Pairs. Academic Pediatrics 2018;18(8):897–904. doi: 10.1016/j.acap.2018.04.134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gross RS, Mendelsohn AL, Gross MB, Scheinmann R, Messito MJ. Material hardship and internal locus of control over the prevention of child obesity in low-income hispanic pregnant women. Academic Pediatrics. 2016;16(5):468–474. doi: 10.1016/j.acap.2016.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chu T, Hackett M, Kaur N. Housing influences among sleep-related infant injury deaths in the USA. Health Promot Int 2016;31(2):396–404. doi: 10.1093/heapro/dav012 [DOI] [PubMed] [Google Scholar]
- 23.Magee CA, Gordon R, Caputi P. Distinct Developmental Trends in Sleep Duration During Early Childhood. Pediatrics 2014;133(6):e1561–e1567. doi: 10.1542/peds.2013-3806 [DOI] [PubMed] [Google Scholar]
- 24.Bathory E, Tomopoulos S. Sleep regulation, physiology and development, sleep duration and patterns, and sleep hygiene in infants, toddlers, and preschool-age children. Current Problems in Pediatric and Adolescent Health Care 2017;47(2):29–42. doi: 10.1016/j.cppeds.2016.12.001 [DOI] [PubMed] [Google Scholar]
- 25.Duncan PM. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents Fourth edition. (JFHJM FAAP, JSSEMR FAAP, PMDM FAAP, eds.). American Academy of Pediatrics; 2017. [Google Scholar]
- 26.Chaudry A, Wimer C. Poverty is not just an indicator: the relationship between income, poverty, and child well-being. Academic Pediatrics 2016;16(3, Supplement): S23–S29. doi: 10.1016/j.acap.2015.12.010 [DOI] [PubMed] [Google Scholar]
- 27.Gross RS, Mendelsohn AL, Gross MB, Scheinmann R, Messito MJ. Randomized controlled trial of a primary care-based child obesity prevention intervention on infant feeding practices. The Journal of Pediatrics 2016;174:171–177.e2. doi: 10.1016/j.jpeds.2016.03.060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sadeh A A brief screening questionnaire for infant sleep problems: validation and findings for an internet sample. Pediatrics 2004;113(6):e570–e577. doi: 10.1542/peds.113.6.e570 [DOI] [PubMed] [Google Scholar]
- 29.Mindell JA, Sadeh A, Wiegand B, How TH, Goh DYT. Cross-cultural differences in infant and toddler sleep. Sleep Med 2010;11(3):274–280. doi: 10.1016/j.sleep.2009.04.012 [DOI] [PubMed] [Google Scholar]
- 30.Bureau UC. Survey of Income and Program Participation. Accessed September 12, 2019. https://www.census.gov/sipp/
- 31.Household U.S. Food Security Survey Module. SNAP Education Connection Accessed November 17, 2019. https://snaped.fns.usda.gov/library/materials/us-household-food-security-survey-module
- 32.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9. Journal of General Internal Medicine 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang J, Li AM, Fok TF, Wing YK. Roles of parental sleep/wake patterns, socioeconomic status, and daytime activities in the sleep/wake patterns of children. J Pediatr 2010;156(4):606–612.e5. doi: 10.1016/j.jpeds.2009.10.036 [DOI] [PubMed] [Google Scholar]
- 34.Bagley EJ, Kelly RJ, Buckhalt JA, El-Sheikh M. What keeps low-SES children from sleeping well: the role of presleep worries and sleep environment. Sleep Med 2015;16(4):496–502. doi: 10.1016/j.sleep.2014.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hanson KL, Connor LM. Food insecurity and dietary quality in US adults and children: a systematic review. Am J Clin Nutr 2014;100(2):684–692. doi: 10.3945/ajcn.114.084525 [DOI] [PubMed] [Google Scholar]
- 36.Ravid S, Afek I, Suraiya S, Shahar E, Pillar G. Kindergarten Children’s Failure to Qualify for First Grade Could Result From Sleep Disturbances. J Child Neurol 2009;24(7):816–822. doi: 10.1177/0883073808330766 [DOI] [PubMed] [Google Scholar]
- 37.Miller AL, Miller SE, LeBourgeois MK, Sturza J, Rosenblum KL, Lumeng JC. Sleep duration and quality are associated with eating behavior in low-income toddlers. Appetite 2019;135:100–107. doi: 10.1016/j.appet.2019.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Winsper C, Wolke D. Infant and toddler crying, sleeping and feeding problems and trajectories of dysregulated behavior across childhood. J Abnorm Child Psychol 2014;42(5):831–843. doi: 10.1007/s10802-013-9813-1 [DOI] [PubMed] [Google Scholar]
- 39.Gross RS, Mendelsohn AL, Messito MJ. Additive effects of household food insecurity during pregnancy and infancy on maternal infant feeding styles and practices. Appetite 2018;130:20–28. doi: 10.1016/j.appet.2018.07.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chung EK, Siegel BS, Garg A, et al. Screening for social determinants of health among children and families living in poverty: a guide for clinicians. Current Problems in Pediatric and Adolescent Health Care 2016;46(5):135–153. doi: 10.1016/j.cppeds.2016.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bocknek EL, Richardson PA, van den Heuvel MI, Qipo T, Brophy-Herb HE. Sleep moderates the association between routines and emotion regulation for toddlers in poverty. Journal of Family Psychology 2018;32(7):966–974. doi: 10.1037/fam0000433 [DOI] [PubMed] [Google Scholar]
- 42.Hall WA, Liva S, Moynihan M, Saunders R. A Comparison of Actigraphy and Sleep Diaries for Infants’ Sleep Behavior. Front Psychiatry 2015;6. doi: 10.3389/fpsyt.2015.00019 [DOI] [PMC free article] [PubMed] [Google Scholar]


