Abstract
Objective
This study explored women's perspectives on the acceptability of including new cancer information with an all‐clear breast or cervical screening result letter (using ovarian cancer as a case study).
Methods
In 2016, six focus group discussions were conducted with women aged 25–70 years old, eligible for invitation to the NHS breast or cervical screening programme and resident in England. The focus groups lasted 60–90 min and were held in community venues. Data were analysed using thematic analysis.
Results
Thirty‐eight women aged 25–67 years old participated in the focus groups. Data analysis yielded six descriptive themes: general cancer awareness, taking advantage of a ‘teachable moment’, a double‐edge sword, barriers to accepting and using new cancer information, motivators for accepting and using new cancer information and wider strategies to increase cancer awareness in women. Women welcomed the inclusion of new cancer information in all‐clear screening results but highlighted pertinent lessons to be considered to maximise the usefulness of the approach.
Conclusion
While women perceived this approach as acceptable, it is pertinent to note the potential of the new cancer information to stimulate anxiety and potentially widen inequalities by excluding non‐attenders at screening programmes. Specific complementary and tailored approaches are necessary to mitigate these limitations.
Keywords: cancer screening, qualitative study, theoretical framework of acceptability, teachable moment, women
1. INTRODUCTION
Globally, cancer is a leading cause of death among non‐communicable diseases, and as its incidence continues to increase, it is an important public health concern (Bray et al., 2018). Compared with other western countries (e.g., Canada, Norway), the United Kingdom continues to record lower survival rates for some cancers, such as stomach, colon, pancreas and ovarian cancers (Arnold et al., 2019). Data from the United Kingdom further projects an increase in cancer incidence among females by 0.11% (approximately 65,048 new cancers or 3100–3300 new cancers per year from 2014/2015–2035) between 2015 and 2035, which highlights the crucial need for targeted but innovative strategies to reduce cancer burden among this population (Smittenaar et al., 2016).
Wider collaborative efforts (e.g., awareness campaigns) by policy makers, healthcare providers and cancer charities have led to some successes in stimulating early help‐seeking for worrying cancer symptoms (Green et al., 2015; Lai et al., 2021). While these cancer awareness efforts continue (Cancer Research UK [CRUK], 2021a), there is need for complementary approaches which maximise ‘teachable moments’. Described as an event or circumstance that motivates an individual to take positive actions regarding their health, ‘teachable moments’ have been examined across an array of settings over the years to assess whether health events can motivate risk‐reducing behaviours. For example, HIV treatment initiation and smoking cessation (Vidrine et al., 2018), antenatal care visits and screening for sickle cell and thalassemia (Brown et al., 2011; Tsianakas et al., 2012), COVID‐19 crisis and lifestyle change in cardiovascular disease patients (Brust et al., 2021), ‘cancer worry’ and smoking cessation (McBride et al., 2008) and cancer screening, diagnosis, care and survivorship (Gray et al., 2021; Karvinen et al., 2015; Kathuria et al., 2020; McBride et al., 2017; Neumann et al., 2021).
To promote early diagnosis of breast and cervical cancers, the National Health Service (NHS) routinely invites asymptomatic women aged between 25–64 years and 50–70 years for cervical and breast screening, respectively (CRUK, 2020a). Women are informed of their screening result by letter, which for the majority is often negative (NHS Digital, 2020). Evidence suggests that this contact with the NHS could be perceived as a ‘teachable moment’ (Lawson & Flock, 2009; McBride et al., 2003) to increase women's knowledge and awareness of the symptoms of less common cancers. For example, Scott et al. (2021) explored the acceptability of using breast cancer screening participation as a ‘teachable moment’ to advise women on cancer symptoms and cervical and bowel screening participation and found this was acceptable to the majority of their study participants.
In the current study, ovarian cancer was selected as a case study because it affects women of similar age groups as breast and cervical cancers (CRUK, 2021b) and has the poorest prognosis among the gynaecological cancers (ONS, 2019a). Despite this, symptom awareness for ovarian cancer is low (Low et al., 2013; Reid et al., 2021), and it has high mortality rate due to late diagnosis as outcomes are strongly linked with stage at presentation (Athey et al., 2021; ONS, 2019b). Although ovarian cancer does not have a screening programme (Menon et al., 2021), it is important to increase ovarian cancer symptom awareness to improve help‐seeking behaviour for early diagnosis. However, little is known about the acceptability to women in the United Kingdom if they are informed about the symptoms of new cancers when they receive an all‐clear breast or cervical screening result.
The Theoretical Framework of Acceptability (TFA) (Sekhon et al., 2017) theorises that for a healthcare intervention to be acceptable, users and providers must perceive it as appropriate based on their expected or actual cognitive and emotional responses to the intervention. The seven constructs of the TFA provides a conceptual understanding of intervention acceptability, and they are as follows: affective attitude (individual's feelings about an intervention), burden (effort required to participate in the intervention), ethicality (the extent to which the intervention fits with the individual's value system), intervention coherence (extent of participant's understanding of how the intervention works), opportunity costs (extent to which benefits and values must be given up to partake in the intervention), perceived effectiveness (intervention's achievement of its intended purpose) and self‐efficacy (participant's confidence in their ability to perform the behaviour required in the intervention) (Sekhon et al., 2017).
Therefore, this study aimed to explore women's perspectives on the acceptability of including new cancer information with an all‐clear breast or cervical screening result letter (this will be referred to as INCLUSION throughout this manuscript). The INCLUSION approach would facilitate contact with a population appropriate to the particular cancer information included in a cost‐effective manner (using ovarian cancer as a case study). Insights gleaned from this study will also be useful to inform policy and practice in developing user‐centred and acceptable interventions to improve cancer awareness and early help‐seeking among at‐risk populations.
2. METHODS
This study is reported following the Consolidated Reporting of Qualitative Studies (COREQ) guidelines (Tong et al., 2007). See checklist in Supporting Information.
2.1. Study design
We conducted a qualitative study using focus group discussions, which enabled us to triangulate data from diverse perspectives at once, leading to the collection of rich data and an in‐depth understanding of the research topic (Bryman, 2015). Purposive sampling was used to recruit women eligible for invitation to the NHS breast or cervical screening programme (aged 25–70 years), able to give informed consent and resident in England (Hull, Leeds, London and Newcastle) in 2016. Using maximum variation sampling, we targeted a mix of affluent and deprived populations in these areas. Participants were accessed via a specialist recruitment agency in England and received a £20 gift voucher to thank them for participating in the study
2.2. Data collection
Although we initially intended to recruit eight women for each focus group, we recruited 38 women across the six groups (there were 10 non‐attenders across the six groups, who had either cancelled or did not attend on the scheduled date). Consenting women participated in six focus group discussions (four groups had six women; two groups had seven women) held at mutually convenient community venues in Hull, Leeds, London and Newcastle in 2016 (Table 1). The focus group discussions were audio‐recorded, lasted 60–90 min and were facilitated by TG and ST (female postdoctoral researchers with social scientist and health psychologist backgrounds, respectively, and without prior relationship with any of the study participants). A topic guide was used to stimulate discussions. Informed by the research aim and the literature (e.g., McBride et al., 2008), sample open‐ended questions on the topic guide included women's perceptions of the concept of including new cancer information within their all‐clear breast or cervical screening result, perceived advantages and disadvantages of this approach and suggestions on novel ways of creating acceptable cancer awareness among the general population. To contextualise the discussions, ovarian cancer was used as a case study for the new cancer information to be included and an information leaflet was circulated to each participant before the focus group discussions. Field notes were written after each discussion.
TABLE 1.
Demographic information of study participants
| N = 38 (100%) | |
|---|---|
| Age (in years) | |
| 25–35 | 8 (21%) |
| 36–45 | 7 (18%) |
| 46–55 | 11 (29%) |
| 56–65 | 9 (24%) |
| >65 | 3 (8%) |
| Ethnicity | |
| White | 29 (76%) |
| Black African | 3 (8%) |
| Black Caribbean | 2 (5%) |
| Indian | 2 (5%) |
| Euro Asian | 1 (3%) |
| Black Other | 1 (3%) |
| Marital status | |
| Married | 17 (45%) |
| Single | 14 (37%) |
| Co‐habiting | 4 (10%) |
| Divorced | 3 (8%) |
| Work status | |
| Paid full‐time employment | 18 (47%) |
| Paid part‐time employment | 7 (18%) |
| Retired/unemployed | 11 (29%) |
| Self‐employed | 2 (5%) |
| Job type (for those in employment) a | |
| Managerial/professional | 16 (42%) |
| Intermediate | 10 (26%) |
| Routine/manual | 1 (3%) |
| Attendance at cancer screening | |
| Cervical | 27 (71%) |
| Breast | 18 (47%) |
| Both breast and cervical | 14 (37%) |
| Not attended any | 6 (16%) |
Using the Office for National Statistics classification (ONS 2010).
2.3. Ethical considerations
Ethical approval was received from Hull York Medical School (HYMS) Ethics Committee. Each participant provided written informed consent before participating in a focus group discussion. Participants' confidentiality was addressed by asking all discussants to keep the discussion private. All transcripts were anonymised.
2.4. Data analysis
Data were analysed using thematic analysis as described by Clark and Braun (2017), which involved identification, analysis and interpretation of patterns of meanings (themes) within the data in relation to the research aim and objectives. Following data familiarisation, descriptive codes were generated using words which described participants' views and meanings within the data. Themes were then constructed from the codes by iteratively engaging with the data and exploring the codes for patterns, similarities and differences. The themes were iteratively reviewed in relation to the research aim and objectives and labelled accordingly. Data analysis was undertaken by two authors (OB and JW) and discussed with a third author (UM) to enhance credibility and trustworthiness. Data analysis was managed using NVivo 12.
3. RESULTS
3.1. Overview
Thirty‐eight women aged between 25 and 67 years old, participated in the focus group discussions (Table 1). The majority were as follows: White (76%), married or co‐habitating (55%) and over 45 years old (61%).
Data analysis yielded six descriptive themes (Figure 1): (i) general cancer awareness, (ii) taking advantage of a ‘teachable moment’, (iii) a double‐edge sword, (iv) barriers to accepting and using new cancer information, (v) motivators for accepting and using new cancer information and (v) wider strategies to increase cancer awareness in women.
FIGURE 1.
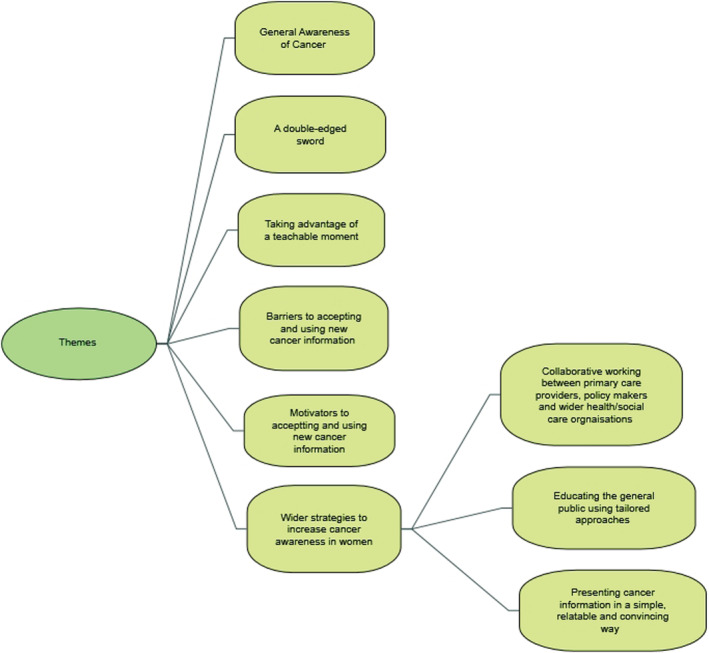
Map showing the themes
3.2. General cancer awareness
Most of the study participants reported having general cancer awareness which they attributed to information received through their GPs, previous attendance at routine breast and cervical screening programmes, personal experience of a cancer diagnosis (self, family or friend) or through work/volunteering activities in a cancer charity. Some participants reported being prompted by the experience of potential cancer symptoms to seek information, mostly through their doctors or through personal research:
… I think if something's wrong me with me or they said you've got, this is what's happening with your body, I'll go on and I'll find out exactly all about all ifs, you know, like my sister had, ovarian cancer, I thought okay, I'm going to have, I'm going to have to read up on it … (Participant, FG3)
When probed about ovarian cancer as an example of a cancer for which information might be presented, participants perceived it as a silent killer due to its limited public awareness, difficulty in symptom recognition and appraisal. This perception was further attributed to a current lack of routine ovarian cancer screening programme, confusion over the body part it affects (some women reported mixing it up with cervical cancer), and the complexity of differentiating ovarian cancer symptoms from other diseases with related symptoms:
… but I think the danger with the ovarian cancer is that the symptoms are so vague, really aren't they … ? (Participant, FG6)
3.3. Taking advantage of a ‘teachable moment’
This theme resonated across all the focus group discussions as women reiterated that receiving new cancer information with all‐clear screening results would increase their sensitivity to body changes which may be indicative of potential cancer and motivate them to promptly seek help:
…I'm certainly going to be saying something to the doctor on Friday because… I'm going a bit of a flare‐up with the fibroids[?] so I'm assuming that the IBS is because of that, so it's been like the last year, but the weeing, it's like, that's just started and I just think it's summer, I'm drinking loads and, so…. now I've read this, I'm going to mention it to the doctor, it's as simple … (Participant, FG1)
Some women added they are more likely to read cancer information sent this way as opposed to receiving it via their letterboxes which they may just treat it as junk mail. A recurring theme was the perception that this approach would save on cost for the health service, empower individuals to take personal responsibility for their own health, be assertive in their help‐seeking for suspected symptoms and stimulate conversation with their doctor regarding any concerns they might have which they may otherwise not feel confident to bring up:
… one of the things I like about it is it says take this to your doctor, so you've got the beginnings of a discussion because not everybody's confident about going and talking to the doctor … (Participant, FG1)
… The cost thing again and it's cheaper to do that and then actually send you for the tests that you need to start off with … (Participant, FG1)
3.4. A double‐edged sword
Participants highlighted some pros and cons of the INCLUSION approach. Some women reported they would be positively inclined towards receiving new cancer information this way because of being in ‘taking care of myself mode’ (Participant, FG1), increased sensitivity to their health due to ageing (older participants) and concern for what would happen to their dependent family particularly their children, if they had poorer chances of survival from cancer because it was picked up late:
… I think since I've had children … I've got like two dependents and think I've got to be around for them and how would they be, how would they live their lives without me? Wanting to see how they progress and like finish school and … There's all that sort of ahead and if I wasn't to go for the screening then they pick something up that was preventable then that would be my regret … (Participant, FG2)
In contrast, some participants said that receiving such information at that time could stimulate anxiety and worry due to their perceptions of cancer fatality and a potential misunderstanding of such information as indicative of an impending diagnosis:
… And I think sometimes sort of too much knowledge can be quite frightening, so I don't know if there's an easier, a better way of getting that knowledge across that isn't so utterly terrifying … (Participant, FG5)
Some participants identified that the consequence of this approach would also be to exclude women with positive breast/cervical screening results or those who had not undergone any screening at all, so potentially widening inequality in cancer knowledge and awareness:
… just looking at the wider picture, if people with a negative result get this as you were suggesting, what about people who haven't? It feels a bit discriminatory … (Participant, FG6)
Other concerns related to compromising individuals' autonomous preferences on how they may wish to receive health information (e.g., through verbal communication with GP) and the infrequent opportunity to disseminate new cancer information in this way (due to the 3‐year interval in breast/cervical screening invitations).
… then you're going to waste three years in between each screening … (Participant, FG6)
3.5. Barriers to accepting and using new cancer information
Participants identified barriers such as young age (perceptions that older women are generally more receptive to health information compared with younger ones), cultural avoidance of discussions on intimate body parts and stigma emanating from perceptions that some cancers (such as ovarian cancer) are sexually transmitted:
… because people might think it's sexually transmitted, it's down in the parts we don't talk about … (Participant, FG3)
The women also described the current healthcare structure and processes as barriers. For example, they perceived the current lack of routine screening for some cancers (e.g., ovarian) within the current service provision is aggravated by prioritisation of funding allocation and budget to high‐risk areas and populations:
… So, I think it's all got to do with the funding, and it seems to be much better here so whether they get more money (Participant, FG3)
… Is it a matter of cost that women are not scanned after a certain age? … You can't go and have a blood test if you needed, if you wanted one … (Participant, FG6)
Additional barriers related to communication challenges in patient‐provider relationship (for example, anticipated dismissive attitude from their GP if women acted on the information and ask for a blood test), difficulty in getting a GP appointment and perceptions that GPs are already under pressure and should not be burdened with non‐urgent requests:
… but I waited until it got a lot worse, so I'd have to be quite ill because it's, difficult to get an appointment.… (Participant, FG4)
3.6. Motivators for accepting and using new cancer information
Participants highlighted that they would be motivated to accept new cancer information if it were presented in an educative, ethical and engaging format using language that is ‘very easy to understand’ (Participant, FG2), clearly describe the symptoms to look out for and signpost women to avenues to access further information. Other motivators included: knowing it is a simple blood test and women describing themselves as being proactive in seeking help (actively seeking out information and taking prompt action regarding their health). There was a recurring theme that concern for their families' health and wellbeing would further motivate women to accept and act on the included new cancer information:
… For anything, you know, there's always that anxiety, for me definitely there is, because once upon a time I would have just ignored it but then once you become a mother and things, your lifestyle changes and you think well no, because I've got to be there for them … although I'm frightened to death still, but thinking about not just me and other people in my life would make me sort of, go get this screening now … (Participant, FG1).
Some women added they would act on the new information to ensure early diagnosis and avoid any decisional regret that may be associated with a delayed diagnosis:
… and if I wasn't to go for the screening then they pick something up that was preventable then that would be my regret… (Participant, FG2)
3.7. Wider strategies to increase cancer awareness in women
Participants suggested alternative ways of increasing cancer awareness to enhance wider coverage, especially the less common cancers. This theme is reported under the following sub‐themes: ‘collaborative working between primary care providers, policy makers and wider health/social care organisations’, ‘educating the general public using tailored approaches’ and ‘presenting cancer information in a simple, relatable and convincing way’.
3.7.1. Collaborative working between primary care providers, policy makers and wider health/social care organisations
Participants suggested collaborative working among primary care providers, policy makers and wider health and social care organisations to disseminate cancer messages and provide support through avenues that women frequently patronise. These include gyms, pharmacies, libraries, playgroups, dentists, well women clinics, cancer charities, cultural community groups and health/wellbeing companies:
… Well what about, contacting, slimming companies? They might want to help because they're involved in helping women improve their health, you know, like Slimming World, Weightwatchers, there's a load … and I would think that they might, … feel altruistically that they would like to carry these leaflets and say has anybody seen these, you know, if you would like to, erm, take a leaflet before you go home then have a good read of it?… (Participant, FG2)
There were also reiterations around the need to maximise the use of online platforms to spread cancer information via cancer websites which are accessible to the public, for example, NHS, Macmillan and Cancer Research UK websites. Participants highlighted the need for primary care providers and policy makers to include cancers whose symptoms are difficult to recognise (e.g., ovarian cancer) in routine screening programmes, reduce waiting times for test procedures and provide up‐to‐date cancer information at GP surgeries and A/E walk‐in clinics:
… Yeah, yeah, just go to the walk‐in centre, wait two hours … now I definitely think this information should be there … I think that would be great there. So you're sitting in the waiting room and you've looked at this wall, you've looked at that wall, oh I'll start with, oh right, do you know what I mean … (Participant, FG2)
3.7.2. Educating the general public using tailored approaches
A common theme which resonated across all the focus group discussions was the need to adopt a tailored approach to cancer education by considering diversities in women's demographics (such as age, ethnicity and literacy levels):
… the only thing would be to do different leaflets for different age groups and statistically probably someone under thirty might not read all of that, I don't know if I'm generalising too much but I think they'd probably read a one‐page thing … but maybe an older person might be more inclined to read the whole thing and you might even want different digital for different age groups… (Participant, FG3)
Suggested tailored approaches included targeting areas where women congregate, incorporating body and cancer awareness information in school curriculum, including family members in awareness campaigns, engaging women in discussion groups at their natural setting, promoting survivorship stories to reduce people's anxiety regarding perceived cancer fatality, and pitching cancer information to ethnic minority women in their language and community settings:
… If you want to measure the success or see if it gets results … depending on the ethnicity, you will get women to attend or, or they can't read it or, so I think that's got to go to communities where you've got ethnicity to discuss what is the best way we can promote this to your culture?… (Participant, FG1)
3.7.3. Presenting cancer information in a simple, relatable and convincing way
Participants identified the importance of framing cancer awareness messages in a language that will stimulate women's interest and engagement. They emphasised that information leaflets should be presented in a clear, simple and non‐medical language such that it is not perceived as intended to stimulate fear but positive help‐seeking for prompt diagnosis. To achieve this, they recommended using an everyday analogy or metaphor that women can relate with:
… Remember when I was at university, I was training to be a PE teacher and …. the men there were doing sport as well and there was a huge poster in the doctor's surgery, it says men, boys, check your balls …. Rugby balls and footballs and all sort of stuff, and that, was like 1996 and I've never forgotten that because it was just really eye catching, it was really quite funny … but it just made all the blokes think, and I've never seen it since, but I thought that was the best cancer poster, I've, because I can still remember it, it's like twenty years on… (Participant, FG5)
4. DISCUSSION
This study aimed to explore women's perspectives on the acceptability of including new cancer information (e.g., ovarian cancer) in all‐clear breast or cervical screening result letter. We used focus groups to generate discussion related to this topic. Findings showed that women found the INCLUSION approach acceptable as they perceived it to be a ‘teachable moment’ which presents an opportunity to increase their awareness of potential cancer symptoms and take positive action to seek help. Women attributed this positive response to being in their ‘taking care of yourself mode’. This highlights the applicability of the concept of ‘teachable moment’ (Lawson & Flock, 2009; McBride et al., 2003) to this context. However, our participants also highlighted some pertinent lessons (e.g., information stimulating fear and anxiety; potential to widen inequalities by excluding non‐attenders) to be considered if the approach is to maximise its intended outcome. TFA further provides a conceptual understanding of study findings and implications particularly in relation to affective attitude, perceived effectiveness, ethicality and self‐efficacy.
Relating their ‘affective attitude’, women in this study mostly felt positive about the INCLUSION approach, but had concerns about its emotional implications in stimulating anxiety or fear which could impede their acceptance and use of new cancer information. Previous studies have also shown fear of diagnosis as a barrier to early presentation for suspected cancer symptoms (Al‐Aziz et al., 2021; Macleod et al., 2009) or screening uptake (Bamidele et al., 2017), which highlights the importance of providing cancer information in a clear and reassuring way, to avoid women confusing it with an impending diagnosis.
Describing their ‘perceived effectiveness’ of the INCLUSION approach to achieve the intended outcome, our study participants identified some barriers such as age, confusion about female anatomy and difficulty in booking appointments with their GPs, all of which have practical implications. For example, the influence of age disparities on symptom recognition and help‐seeking has been recognised in previous studies (Macleod et al., 2009; Mwaka et al., 2021). In the current study, participants perceived older women to be more receptive to health messages because of their concern about age‐related body changes and associated illnesses. While older age remains an important risk factor for most cancers, evidence shows that younger women are not altogether immune from some cancer types (e.g., cervical, ovarian) (CRUK, 2020b) and should therefore be likewise targeted in preventative interventions.
The ethicality of the INCLUSION approach is also worthy of attention. For example, participants perceived it may lead to unforeseen burden on screening services and potentially widen inequalities as it is only being offered to women who have attended for screening who may be the most likely to attend with new symptoms (Lorenc et al., 2013). A construct of the TFA (Sekhon et al., 2017), ethicality highlights that for an intervention to be acceptable, it must have a good fit with the user's value system. Many cancer interventions, although appropriate, seem to inadvertently widen inequalities due to the exclusion of certain demographics (Ellis et al., 2021). To address this concern, specific interventions need to be developed to encourage screening non‐attenders (Moen et al., 2020). For example, using targeted approaches tailored for diverse demographics as appropriate (e.g., pitching cancer information to ethnic minority women in their language and community settings).
Although recognising the included information as empowering them to take personal responsibility for their health and start off conversations with their GPs, our study participants indicated the existence of power imbalance in patient‐GP consultations which often makes it difficult for them to book appointments to get a test done, despite the simplicity of the test procedure. Sekhon et al. (2017) highlights the centrality of self‐efficacy (an individual's confidence in their ability to perform the required behaviour) to the acceptability of an intervention. Previous findings (Jefferson et al., 2019) also identified difficulty booking a GP appointment as a barrier to early help‐seeking for suspected cancer symptoms. This suggests the need to examine the dynamics of patient‐provider communications while addressing the important elements that could facilitate or impede how ‘teachable moment’ is maximised in this context.
4.1. Implications
Noting the potential of the INCLUSION approach to widen inequalities by focusing on active help‐seekers, there is need for specific interventions targeted at those who do not attend cancer screening. The importance of presenting new cancer information materials in an appropriate language which would not elicit fear or anxiety cannot be undermined. As recommended by study participants, this can be achieved by using simple but relatable language (e.g., metaphors), conspicuously highlighting the simplicity of the test procedure and explaining the importance of early diagnosis to improve survival if diagnosed. Additionally, there is need to consider the use of role models and/or ‘peer leaders’ in promoting cancer screening (Ahmad et al., 2017; Hulme et al., 2016); or share success stories of relatable individuals from the similar background or language.
It is also pertinent to note the women's perceptions regarding the reasons for lack of routine ovarian screening. While they perceived it was due to funding limitations, evidence suggest this is due to lack of a test with sufficient sensitivity and specificity to pick ovarian cancer up in its early stage (CRUK, 2021c). Thus, there is need for targeted educational interventions to increase women's understanding of screening provision and implementation (e.g., through community education sessions; Hulme et al., 2016). This will enhance intervention coherence (extent to which the participant understands how the intervention works) (Sekhon et al., 2017). It is also imperative for primary care providers to consider diversities in women's demographics (such as age, ethnicity and literacy levels) and collaborate with policy makers and wider health/social care organisation to design and tailor cancer education approaches as appropriate.
4.2. Study limitations and directions for future research
The strength of this study is in using focus group discussions to gain an in‐depth understanding of an under‐researched phenomenon. However, there some limitations. Most of the participants being middle class White women who already attend breast or cervical screening, may have contributed to their generally receptive behaviour and seemingly knowledgeable views on the research topic. Although we used maximum variation sampling to target women across different socio‐economic backgrounds, most of the recruited participants were from more affluent areas and majority white ethnic backgrounds. Future studies should target women from more deprived areas, ethnic minority groups and non‐attenders at cancer screening programmes to elicit their perceptions. Using TFA in this study provided a conceptual understanding of the topic from users' perspectives. Future studies should explore the feasibility of this approach from both patients' and healthcare providers' perspectives, particularly primary care providers (seeing their central role in implementing the intervention if adopted into policy and practice).
5. CONCLUSION
This study explored women's perspectives on the acceptability of including new cancer information (e.g., ovarian cancer) in all‐clear breast or cervical screening result letter, using six focus group discussions with 38 women. Overall, findings showed that this approach is an acceptable and relatively inexpensive way of raising cancer awareness and information. However, there is need to be aware of the potential of the new cancer information to stimulate anxiety and potentially widen inequalities by excluding non‐attenders at screening programmes. Specific complementary and tailored approaches are necessary to mitigate these limitations.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Supporting information
Data S1. COREQ Checklist.
ACKNOWLEDGEMENTS
The authors wish to thank Dr. Jo Waller for her helpful contribution to the study. We also appreciate all the women who kindly took time to participate in the study.
This study was funded by the NIHR Policy Research Unit in Cancer Awareness, Screening and Early Diagnosis (2010–2018). The Unit received funding for a research programme from the Department of Health Policy Research Programme. It was a collaboration between researchers from seven institutions (Queen Mary University of London, UCL, King's College London, London School of Hygiene and Tropical Medicine, Hull York Medical School, Durham University and Exeter University). Trish Green was funded by this programme.
Bamidele, O. O. , Green, T. , Tookey, S. , Walabyeki, J. , & Macleod, U. (2022). A qualitative exploration of women's perspectives and acceptability of including new cancer awareness information in all‐clear breast or cervical screening results. European Journal of Cancer Care, 31(3), e13574. 10.1111/ecc.13574
Funding information Department of Health Policy Research Programme; NIHR Policy Research Unit in Cancer Awareness, Screening and Early Diagnosis
DATA AVAILABILITY STATEMENT
The datasets generated during and/or analysed during the current study are not publicly available due to privacy or ethical restrictions but are available upon reasonable request from the University of Hull Repository through the last author.
REFERENCES
- Ahmad, F. , Ferrari, M. , Moravac, C. , Lofters, A. , & Dunn, S. (2017). Expanding the meaning of ‘being a peer leader’: Qualitative findings from a Canadian community‐based cervical and breast cancer screening programme. Health & Social Care in the Community, 25(2), 630–640. 10.1111/hsc.12352 [DOI] [PubMed] [Google Scholar]
- Al‐Aziz, M. , Al‐Baimani, K. , Al‐Awaisi, H. , Al‐Mandhari, Z. , Al‐Khamayasi, J. , Al‐Lawati, Y. , & Panchatcharam, S. (2021). Knowledge of symptoms, time to presentation and barriers to medical help‐seeking among Omani women diagnosed with breast cancer: A cross‐sectional study. BMJ Open, 11, e043976. 10.1136/bmjopen-2020-043976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold, M. , Rutherford, M. J. , Bardot, A. , Ferlay, J. , Andersson, T. M. , Myklebust, T. Å. , Tervonen, H. , Thursfield, V. , Ransom, D. , Shack, L. , & Woods, R. R. (2019). Progress in cancer survival, mortality, and incidence in seven high‐income countries 1995–2014 (ICBP SURVMARK‐2): A population‐based study. The Lancet Oncology, 20(11), 1493–1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Athey, R. A. , Macdonald, M. C. , & Jha, S. (2021). Stage of ovarian cancer at diagnosis. Does presentation as an emergency make a difference? European Journal of Obstetrics & Gynecology and Reproductive Biology, 261, 7–11. 10.1016/j.ejogrb.2021.04.001 [DOI] [PubMed] [Google Scholar]
- Bamidele, O. , Ali, N. , Papadopoulos, C. , & Randhawa, G. (2017). Exploring factors contributing to low uptake of the NHS breast cancer screening programme among Black African women in the UK. Diversity and Equality in Health and Care, 14(4), 212–219. [Google Scholar]
- Bray, F. , Ferlay J., Soerjomataram I., Siegel. R. , Torre, L. A. , & Jemal, A. (2018). Global Cancer Statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians, 68, 394–424. [DOI] [PubMed] [Google Scholar]
- Brown, K. , Dormandy, E. , Reid, E. , Gulliford, M. , & Marteau, T. (2011). Impact on informed choice of offering antenatal sickle cell and thalassaemia screening in primary care: A randomized trial. Journal of Medical Screening, 18(2), 65–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brust, M. , Gebhardt, W. A. , Numans, M. E. , & Kiefte‐de Jong, J. C. (2021). The COVID‐19 crisis as a teachable moment for lifestyle change in Dutch cardiovascular disease patients. Frontiers in Psychology, 12, 678513. 10.3389/fpsyg.2021.678513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryman, A. (2015). Social research methods (5th ed.). Oxford University Press. [Google Scholar]
- Cancer research UK . (2020a). Cancer screening. https://www.cancerresearchuk.org/about-cancer/screening/understanding-cancer-screening
- Cancer Research UK . (2020b). Risk and causes. https://www.cancerresearchuk.org/about-cancer/cervical-cancer/risks-causes
- Cancer Research UK . (2021a). Be clear on cancer. https://www.cancerresearchuk.org/health-professional/awareness-and-prevention/be-clear-on-cancer#bcoclanding0
- Cancer Research UK . (2021b), Ovarian cancer incidence by age. https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/ovarian-cancer/incidence#heading-One
- Cancer Research UK . (2021c). Screening for ovarian cancer. https://www.cancerresearchuk.org/about-cancer/ovarian-cancer/getting-diagnosed/screening
- Clark, V. , & Braun, V. (2017). Thematic analysis. The Journal of Positive Psychology, 12(3), 297–298. 10.1080/17439760.2016.1262613 [DOI] [Google Scholar]
- Ellis, K. , Raji, D. , Olaniran, M. , Alick, C. , Nichols, D. , & Allicock, M. (2021). A systematic scoping review of post‐treatment lifestyle interventions for adult cancer survivors and family members. Journal of Cancer Survivorship. 10.1007/s11764-021-01013-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray, D. M. , Emerson, B. , Reddy, M. , Zimmermann, B. J. , Hashi, A. , Shoben, A. , Reiter, P. L. , & Katz, M. L. (2021). A teachable moment: Colorectal cancer screening among companions waiting for outpatients undergoing a colonoscopy. Journal of Cancer Education, 36, 1163–1169. 10.1007/s13187-020-01745-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green, T. , Atkin, K. , & Macleod, U. (2015). GPs' perceptions and experiences of public awareness campaigns for cancer: A qualitative enquiry. Health Expectations, 19, 377–387. 10.1111/hex.12362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hulme, J. , Moravac, C. , Ahmad, F. , Cleverly, S. , Lofters, A. , Ginsburg, O. , & Dunn, S. (2016). “I want to save my life”: Conceptions of cervical and breast cancer screening among urban immigrant women of South Asian and Chinese origin. BMC Public Health, 16(1), 1077. 10.1186/s12889-016-3709-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jefferson, L. , Atkin, K. , Sheridan, R. , Oliver, S. , Macleod, U. , Hall, G. , Forbes, S. , Green, T. , Allgar, V. , & Knapp, P. (2019). Non‐attendance at urgent referral appointments for suspected cancer: A qualitative study to gain understanding from patients and GPs. British Journal of General Practice, 69(689), e850–e859. 10.3399/bjgp19X706625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karvinen, K. , Bruner, B. and Truant, T. , (2015, November). The teachable moment after cancer diagnosis: perceptions from oncology nurses. In Oncology nursing forum (Vol. 42, No. 6, pp. 602‐609). Oncology Nursing Society. [DOI] [PubMed] [Google Scholar]
- Kathuria, H. , Koppelman, E. , Borrelli, B. , Slatore, C. G. , Clark, J. A. , Lasser, K. E. , & Wiener, R. S. (2020). Patient–physician discussions on lung cancer screening: A missed teachable moment to promote smoking cessation. Nicotine and Tobacco Research, 22(3), 431–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai, J. , Mak, V. , Bright, C. J. , Lyratzopoulos, G. , Elliss‐Brookes, L. , & Gildea, C. (2021). Reviewing the impact of 11 national Be Clear on Cancer public awareness campaigns, England, 2012 to 2016: A synthesis of published evaluation results. International Journal of Cancer, 148(5), 1172–1182. [DOI] [PubMed] [Google Scholar]
- Lawson, P. J. , & Flock, S. A. (2009). Teachable moments for health behaviour change: A concept analysis. Patient Education and Counselling, 76, 25–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorenc, T. , Petticrew, M. , Welch, V. , & Tugwell, P. (2013). What types of interventions generate inequalities? Evidence from systematic reviews. Journal of Epidemiological Community Health, 67, 190–193. [DOI] [PubMed] [Google Scholar]
- Low, E. L. , Waller, J. , Menon, U. , Jones, A. , Reid, F. , & Simon, A. E. (2013). Ovarian cancer symptom awareness and anticipated time to help‐seeking for symptoms among UK women. Journal of Family Planning and reproductive health care, 39(3), 163–171. [DOI] [PubMed] [Google Scholar]
- Macleod, U. , Mitchell, E. , Burgess, C. , Macdonald, S. , & Ramirez, A. J. (2009). Risk factors for delayed presentation and referral of symptomatic cancer: Evidence for common cancers. British Journal of Cancer, 101, S92–S101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride, C. M. , Blocklin, M. , Lipkus, I. M. , Klein, W. M. , & Brandon, T. H. (2017). Patient's lung cancer diagnosis as a cue for relatives' smoking cessation: Evaluating the constructs of the teachable moment. Psycho‐oncology, 26(1), 88–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride, C. M. , Emmons, K. M. , & Lipkus, I. M. (2003). Understanding the potential of teachable moments: The case of smoking cessation. Health Education Research, 18(2), 156–170. [DOI] [PubMed] [Google Scholar]
- McBride, C. M. , Puleo, E. , Pollak, K. I. , Clipp, E. C. , Woolford, S. , & Emmons, K. M. (2008). Understanding the role of cancer worry in creating a “teachable moment” for multiple risk factor reduction. Social Science & Medicine, 66, 790–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menon, U. , Gentry‐Maharaj, A. , Burnell, M. , Singh, N. , Ryan, A. , Karpinskyj, C. , Carlino, G. , Taylor, J. , Massingham, S. K. , Raikou, M. , Kalsi, J. K. , Woolas, R. , Manchanda, R. , Arora, R. , Casey, L. , Dawnay, A. , Dobbs, S. , Leeson, S. , Mould, T. , … Parmar, M. (2021). Ovarian cancer population screening and mortality after long‐term follow‐up in the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS): A randomised controlled trial. Lancet, 397(10290), 2182–2193. 10.1016/S0140-6736(21)00731-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moen, K. , Kumar, B. , Igland, J. , & Diaz, E. (2020). Effect of an Intervention in general practice to increase the participation of immigrants in cervical cancer screening—A cluster randomized clinical trial. JAMA Network Open, 3(4), e201903. 10.1001/jamanetworkopen.2020.1903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mwaka, A. , Walter, F. , Scott, S. , Harries, J. , Wabinga, H. , & Moodley, J. (2021). Symptom appraisal, help‐seeking and perceived barriers to healthcare seeking in Uganda: An exploratory study among women with potential symptoms of breast and cervical cancer. BMJ Open, 11, e041365. 10.1136/bmjopen-2020-041365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumann, M. , Murphy, N. , & Seetharamu, N. (2021). Impact of family and social network on tobacco cessation amongst cancer patients. Cancer Control, 28, 10732748211056691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NHS Digital . (2020). Test results overview (Data Table 8, KC53, NHS Digital) Cervical Screening Programme, England‐2019‐20 [NS], Official statistics, National statistics. https://digital.nhs.uk/data-and-information/publications/statistical/cervical-screening-annual/england---2019-20/section-1-call-and-recall
- Office for National Statistics . (2019a) Cancer survival in England: Adult, stage at diagnosis and childhood ‐ patients followed up to 2018. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/cancersurvivalinengland/stageatdiagnosisandchildhoodpatientsfollowedupto2018
- Office for National Statistics . (2019b), Cancer survival by stage at diagnosis for England, 2019. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/datasets/cancersurvivalratescancersurvivalinenglandadultsdiagnosed
- Reid, F. , Bhatla, N. , Oza, A. M. , Blank, S. V. , Cohen, R. , Adams, T. , Benites, A. , Gardiner, D. , Gregory, S. , Suzuki, M. , & Jones, A. (2021). The World Ovarian Cancer Coalition Every Woman Study: Identifying challenges and opportunities to improve survival and quality of life. International Journal of Gynecologic Cancer, 31(2), 238. [DOI] [PubMed] [Google Scholar]
- Scott, S. E. , Rauf, B. , & Waller, J. (2021). “Whilst you are here …” Acceptability of providing advice about screening and early detection of other cancers as part of the breast cancer screening programme. Health Expect, 24, 1868–1878. 10.1111/hex.13330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sekhon, M. , Cartwright, M. , & Francis, J. J. (2017). Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC health services research, 17(1), 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smittenaar, C. R. , Petersen, K. A. , Stewart, K. , & Moitt, N. (2016). Cancer incidence and mortality projections in the UK until 2035. British Journal of Cancer, 115, 1147–1155. 10.1038/bjc.2016.304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong, A. , Sainsbury, P. , & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32‐item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–397. [DOI] [PubMed] [Google Scholar]
- Tsianakas, V. , Atkin, K. , Calnan, M. W. , Dormandy, E. , & Marteau, T. M. (2012). Offering antenatal sickle cell and thalassaemia screening to pregnant women in primary care: A qualitative study of women's experiences and expectations of participation. Health Expectations, 15(2), 115–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vidrine, D. J. , Frank, S. , Savin, M. J. , Waters, A. J. , Li, Y. , Chen, S. , Fletcher, F. , Arduino, R. , & Gritz, E. (2018). HIV care initiation: A teachable moment for smoking cessation. Nicotine & Tobacco Research, 20(9), 1109–1116. 10.1093/ntr/ntx218 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. COREQ Checklist.
Data Availability Statement
The datasets generated during and/or analysed during the current study are not publicly available due to privacy or ethical restrictions but are available upon reasonable request from the University of Hull Repository through the last author.


