Summary
Interventions for obesity prevention can effectively reduce obesity‐related behaviors in young children. Understanding how to leverage and adapt evidence‐based interventions is needed to improve reach among culturally and linguistically diverse families. This systematic review aimed to synthesize the approaches and outcomes of culturally adapted early childhood obesity‐related behavioral prevention interventions. Multiple electronic databases were systematically searched in March 2021. All study designs were included if they reported cultural adaptations of an intervention targeting at least one obesity‐related behavior (infant feeding, nutrition, physical activity, and/or sleep) among children aged 0–5 years. Studies that only conducted language translations or that developed new interventions were excluded. Two authors independently conducted critical appraisals using the Mixed Method Appraisal Tool. Findings were synthesized narratively, based on the Stages of Cultural Adaptation theoretical model and the Framework for Reporting Adaptations and Modifications‐Enhanced. Twelve interventions met the inclusion criteria, with varied study designs. Few reported all aspects of cultural adaptation processes, and the cultural adaptation strategies documented varied. The results suggest that cultural adaptation of obesity‐related behavioral prevention interventions targeting young children increases acceptability among target cultural groups, yet effectiveness is inconclusive due to a lack of trials. More detailed reporting of cultural adaptation processes and further effectiveness trials are needed to evaluate future work.
Keywords: children, cultural adaptation, infants, minority populations
1. INTRODUCTION
Establishing healthy nutrition and physical activity behaviors during a child's early years has lifelong benefits, including preventing obesity, at the individual, intergenerational, and societal levels. 1 , 2 , 3 Worldwide trends in childhood obesity show rising prevalence over recent decades. 4 Childhood obesity prevention is a global priority, including early childhood as a priority area of action. 5
A recent Cochrane systematic review found that early childhood multicomponent interventions that include diet and physical activity behaviors can reduce obesity risk in children 0–5 years. 6 Other reviews have also shown that early individual‐level interventions for obesity prevention that involve parents, families, and health professionals effectively reduce obesity in the short term. 7 , 8 , 9 , 10 Yet, to date, there has been limited focus on minority populations.
Children from culturally and linguistically diverse backgrounds in English‐speaking countries, such as Australia, experience higher prevalence rates of overweight and obesity. 11 , 12 Families from culturally and linguistically diverse backgrounds may face challenges accessing early childhood interventions and services for various reasons, including language barriers and cultural differences. 13 , 14 , 15 To reduce overweight and obesity inequities, there is a pressing need to ensure early childhood interventions supporting healthy growth are culturally relevant and accessible to diverse populations.
Cultural adaptation of interventions to reach new target populations—modifying an intervention to suit different cultures, languages, and contexts—is an established avenue to leverage existing effective evidence‐based interventions. 16 Culturally adapted interventions have been associated with better health outcomes among target populations. 17 Over the past decade particularly, theoretical approaches and guidelines for cultural adaptations have advanced. 17 , 18 , 19 , 20 , 21 In the implementation science field, where the concept of adaptation includes any context (not just cultural) modifications to interventions, reporting frameworks also consider when, who, and why an intervention was adapted. 22
A 2012 review of culturally adapted health promotion interventions promoting healthy eating and physical activity 23 found that interventions primarily focused on adults, with few targeting young children. To date, reviews of culturally adapted obesity prevention interventions targeting children have included interventions for African–American girls (aged 5–18 years) 24 ; African–American youth (aged 6–18 years) 25 ; and minority preschool children in the United States (aged 2–5 years). 26 These reviews did not include literature outside of America and are now 5–10 years since publication. There have been no reviews that include culturally adapted obesity‐related behavioral prevention interventions for children aged 0–2 years. This is of importance given the early years are a critical time for addressing modifiable obesity risk factors. 27
This systematic review aims to identify culturally adapted health programs or interventions targeting obesity‐related behaviors (including infant feeding, nutrition, physical activity, and/or sleep) among children 0–5 years, then analyze the cultural adaptation approaches and outcomes. Our specific research questions were as follows: (a) What processes are used for culturally adapting childhood obesity‐related behavioral prevention interventions and what types of adaptations are made, and (b) how effective are these adaptations in achieving health‐related outcomes?
2. METHODS
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) 2020 guidelines 28 (see Table S1). The review protocol was registered with PROSPERO (CRD42018105596). 29 Three amendments to the registered protocol include (1) no restrictions on search dates to expand search limits; (2) no searches of gray literature to restrict review scope; (3) use of a different quality appraisal tool with criteria for mixed methods studies necessary for this review.
2.1. Study inclusion and exclusion criteria
This review included peer‐reviewed prevention intervention studies published in English that (i) were culturally adapted and explicitly accounted for participants' culture, ethnicity, or race; (ii) targeted healthy children not affected by obesity aged 0–5 years; (iii) included a component related to at least one obesity‐risk related behavior, specifically nutrition, physical activity, sleep, or infant feeding practices (e.g., breastfeeding, introducing solid foods). These behaviors are recognized risk factors for obesity in childhood. 30
Studies that solely undertook language translations of intervention materials or measures and studies that developed new interventions were excluded from this review. Interventions that primarily focused on treatment and/or management of obesity or other health conditions were also excluded, as these interventions recruit a different target group and have a different focus compared with prevention interventions. In addition, interventions targeting children aged over 5 years or children with a specific health condition were excluded. There were no exclusion criteria placed upon study design, study duration, or publication date.
2.2. Search strategy
A preliminary literature search was conducted in July 2018 using Ovid MEDLINE, followed by a comprehensive search using Ovid (MEDLINE(R) and Epub Ahead of Print, Embase, ERIC, Global Health, PsycINFO), CINAHL, Scopus, and Web of Science databases in October 2018, and again in March 2021. The lead author (SM) was a doctoral candidate and sought guidance from the University of Sydney librarians with subject expertise to refine the search terms and map them to appropriate subject headings in each database. The final search terms were limited to human subjects. See the supporting information for the search terms used in each database (Tables S2–S5). Key search terms included (1) infant OR child OR preschool, AND (2) cultur* AND (tailor* OR adapt*), AND (3) trial OR program OR intervention, AND (4) nutrition OR diet OR physical activity OR tummy time OR sleep. Hand searches of reference lists of relevant review articles were also conducted.
2.3. Selection process
All search results were uploaded to Covidence systematic review software 31 to aid the independent screening process. After duplicates were removed, the title and abstract of records were screened by the lead author (SM) and independently by another reviewer (CR, LMW, ST, PL, and ME), with a third independent reviewer resolving any discrepancies (PL or YL). The full article was retrieved if the title and abstract did not provide enough information to inform a final decision. This process was repeated for the full‐text screening (SM screened all records; CR, LMW, ST, PL, and ME independently double screened the records; YL resolved discrepancies). When the full text was required but not accessible (n = 3), 32 , 33 , 34 the authors were contacted for further information. Two responses confirmed the abstracts were outside the review scope, and one did not receive a response, and no information was available in English, so it was also excluded.
2.4. Data extraction and synthesis
Data were extracted from each article using a template in Excel developed for this review. The template was drafted and piloted with six studies, then further refined. Data extracted included details of the study (e.g., design, country, and stated aims), the population (culture or ethnicity of the target group, description of the target group, sample size, sample characteristics, and target group prior to adaptation), the culturally adapted intervention (e.g., name, brief description, setting and mode of delivery, design theories, and target behaviors), a description of the cultural adaptation process, a summary of reported outcomes, and key author conclusions. For study designs that assessed effectiveness or efficacy, data on the health measures and outcomes were also extracted for synthesis.
The data extraction items related to the cultural adaptation process were informed by Barrera and colleagues' Stages of Cultural Adaptation theoretical model 35 and the Framework for Reporting Adaptations and Modifications‐Enhanced (FRAME). 22 Barrera's model outlines the stages of the cultural adaptation process, which relates to study design. The FRAME assists with characterizing modifications to interventions, including cultural adaptations. The cultural sensitivity dimensions of surface or deep structure from Resnicow et al. 36 , 37 were used to classify the reported adaptations. These key cultural adaptation data extraction items are described in Table 1.
TABLE 1.
Data extraction items related to cultural adaptation process and strategies
| Data item heading | Description of item and definitions, where relevant |
|---|---|
| Stage(s) of cultural adaptation (design) | Which stages of adaptation are presented, according to the Stages of Cultural Adaptation process model? 35 The stages include Stage 1: Information gathering; Stage 2: Preliminary adaptation design; Stage 3: Preliminary adaptation tests; Stage 4 Adaptation refinement; Stage 5: Cultural adaptation trial. |
| Cultural adaptation theory or framework (design) | Were there references to any cultural adaptation theories or frameworks? If yes, which one(s)? |
| Description of process for adaptation (how) | What process was undertaken to make cultural adaptations to the intervention? Was this described? |
| Description of cultural adaptations made/cultural adaptation strategies (what) | What cultural adaptations were made to the intervention content and/or contextual factors (such as delivery setting and mode)? What (If any) other changes were made to the original intervention? |
| Surface or deep structure cultural adaptations (what) | Were the cultural adaptations made at the surface or deep structure level according to Resnicow and colleagues' cultural sensitivity dimensions? 36 , 37 Surface structure adaptations include modifications to the observable characteristics of a target population, such as people, language, music, and foods. Deep structure adaptations involve incorporating relevant cultural, social, historical, and environmental factors that influence health behaviors. |
| Who made the adaptations (who) | Who determined that the adaptations should be made? Who led and who undertook the cultural adaptations? |
| Involvement of the target group (who) | To what extent were members from the target population group involved in making and/or informing the cultural adaptation process and strategies? What was the approach to involvement? |
| When adaptations were made (when) | When in the cultural adaptation process were the adaptations made? Were there multiple time points? |
| The rationale for adaptation (why) | What were the reasons provided for undertaking the cultural adaptation? What were the influences on the decision? |
Note: Informed by the Framework for Reporting Adaptations and Modifications‐Enhanced (FRAME). 22
The lead author (SM) extracted and coded the data using the data extraction template, and another author independently cross‐checked and edited for accuracy and completeness (CR, LMW, ST, PL, and YL). For three articles, published reports and supplementary material related to the study were referred to when extracting data. Missing or unclear information in the articles was recorded as such in the data extraction template. To assist with data presentation and synthesis, the lead author coded the level of detail reported about the cultural adaptation process and strategies for each intervention. The level of detail reported was coded as “detailed description,” “some description,” “limited description,” or “not presented, not described” (see Table 3).
TABLE 3.
Cultural adaptations of included interventions
| Intervention information | Cultural adaptation | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention name | Primary author, year, reference, country | Target cultural group | Stage(s) of cultural adaptation a reported | Cultural adaptation theory or framework | Process of cultural adaptation described | Description of cultural adaptations made | Target group involved | Surface or deep structure adaptations b | Brief description of cultural adaptations |
| Reach Up and Thinking Healthy |
Akter et al. (2020), 46 Bangladesh |
Bangladeshi, rural families | Stages 1–4 | Yes | +++ | +++ | Yes | Surface and deep | Adjusted visual cues, modified interactive activities and motivational meetings with family members, tailored intervention contents, and translated materials into Bangladeshi. |
| CHAMP |
Armstrong (2019) 47 USA |
Mid‐Atlantic, urban families | Stage 5 | − | + | + | − | Surface | Modified vocabulary used, promotion of culturally relevant foods and replaced activities with increased cultural relevance. |
| NEAT AT2 |
Broyles (2011), 48 USA |
Latino, Spanish‐speaking parents | Stages 1–4 | Yes | ++ | ++ | Yes | Surface and deep | Inclusion of traditional and affordable foods, reinforced the Latino cultural practice of preparing meals at home and eating together as a family, translated materials into Spanish and involvement of bilingual‐bicultural educators. |
| Hip‐Hop to Health Jr. |
Fitzgibbon (2006), 49 , 50 , 51 USA |
African‐American and Latino families | Stage 5 | − | +++ | +++ | Yes | Surface and deep | Strategies to increase access to the program; addressing cognitive and environmental influencing factors; including behavioral demonstrations; delivering the intervention in Spanish and English. |
| Tribal MIECHV Programs |
Hiratsuka (2018), 52 USA |
American Indian and Alaska Native families | Stages 1‐2 | Yes | +++ | +++ | Yes | Surface and deep | Review of underpinning concepts and ideas; adjusted visuals, language, and relevant content; inclusion of traditional practices, values and beliefs. Adaptation aims included language and culture preservation. |
| ToyBox |
Malaysia |
Malaysian children | Stage 5 | − | + | ++ | Yes | Surface | Changes to activities and language to suit cultural norms and the local physical environment; resources translated into Bahasa Malaysia; delivered by local teachers. |
| Healthy Balance |
Linville (2020), 55 USA |
Latino immigrant families | Stages 3–5 | − | ++ | ++ | Yes | Surface and deep | Embedded sociocultural norms and traditions within the intervention; all study materials translated in English and Spanish; at least half of the interventionists were bilingual. |
| Healthy Beginnings |
Marshall (2021), 56 Australia |
Arabic and Chinese speaking migrant families | Stages 1–3 | Yes | +++ | +++ | Yes | Surface and deep | Adaptation and translation of materials into Arabic and Chinese, including modified visuals, language and content; delivered by bilingual‐bicultural nurse educators. |
| HAPPY |
United Kingdom |
South Asian‐origin (predominantly Pakistani) populations | Stages 1–5 | Yes | +++ | +++ | Yes | Surface and deep | Modified language, interactive activities, resources and content according to information needs, consideration of cultural/religious values. |
| Fit 5 Kids |
Mendoza (2016), 59 USA |
Latino or Hispanic children | Stage 5 | − | ++ | + | Yes | Surface | Adjusted visuals, language, and concepts, e.g., substitution of songs and poetry that were known by and relevant to local Latino families. |
| LEAPS |
Murtha (2020), 60 Australia |
Aborigina and Torres Strait Islander communities |
Stages 1–4 | − | ++ | ++ | Yes | Surface and deep | Adjusted visuals, language, format and core content, e.g., use of a strengths‐based approach; changes to suit remote location and context; involvement of local facilitators. |
| Tummy Time |
Nitsos (2017), 61 USA |
Latino or Hispanic parents |
Stages 1–4 | − | ++ | ++ | − | Surface | Adjusted visuals and language; materials translated into Spanish; delivered by two bilingual (English‐Spanish) and bicultural (Mexico–USA) research assistants. |
Note: Level of reporting: +++, detailed description; ++, some description; +, limited description; −, not presented, not described.
Range of stages of cultural adaptation, as described by Barrera and colleagues 35 : Stage 1, information gathering; Stage 2, preliminary adaptation design; Stage 3, preliminary adaptation tests; Stage 4, adaptation refinement; Stage 5, trial.
In this review, with multiple study designs included, we used a segregated design, 38 where qualitative and quantitative data were considered separately but complementarily to answer the two key review research questions. Qualitative data and descriptions were used to understand cultural adaptation processes, and quantitative data were used to understand intervention effectiveness for achieving health‐related outcomes. Data from this systematic review were synthesized and reported narratively to summarize and explain the findings.
2.5. Critical appraisals
As all study designs were included in this review, the quality appraisals were conducted using a tool for varied designs; the Mixed Method Appraisal Tool (MMAT). 39 The MMAT is a reliable and valid tool for assessing the methodological quality. 40 , 41 MMAT focuses on core items representing the overall quality of evidence and risk of bias, which may impact the validity of the study findings. The MMAT includes two screening questions and five criteria according to the relevant study methodology category (qualitative research, quantitative randomized controlled trials, quantitative nonrandomized studies, quantitative descriptive, and mixed method studies). Each item is rated “yes,” “no,” or “can't tell.” For each of the included interventions, the peer‐reviewed publication that included key behavioral outcomes was assessed by the lead author (SM) and independently by another author (CR, LMW, ST, YL, PL) using separate Excel files. Ratings were then compared, and discrepancies were resolved through author group discussion. The results of the assessments were considered during data synthesis but did not result in exclusions from this review.
3. RESULTS
3.1. Study selection
The searches generated 8,322 records, and after removing duplicates, 4,708 records were independently double screened by title and abstract (95.1% interrater agreement). The full texts of 107 records were evaluated against the inclusion and exclusion criteria. A total of 16 articles representing 12 unique interventions were included in this review (Figure 1).
FIGURE 1.
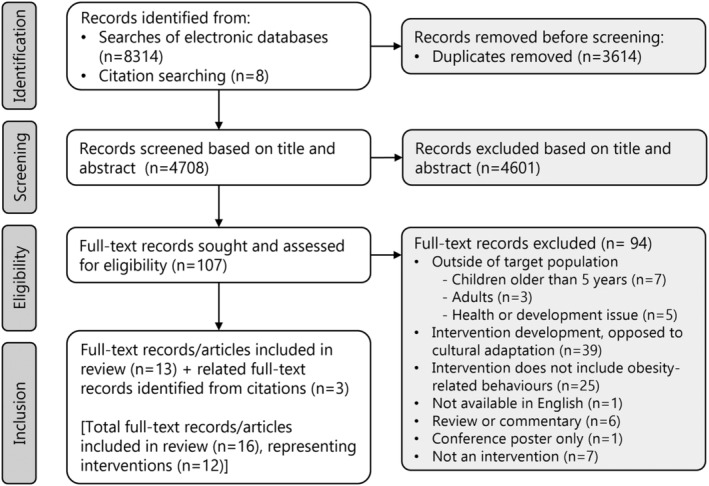
Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) diagram of systematic search findings and study selection
Notable exclusions that might appear to meet the criteria of this review included interventions that referred to cultural adaptation literature; however, they were designed or developed specifically for a particular cultural population group rather than adapting an existing intervention (e.g., 42 , 43 ). Another notable exclusion was an intervention for childhood obesity prevention in Europe, 44 which was developed with the intention of context and cultural adaptations during implementation; however, the cultural adaptations have not been documented. 45
3.2. Description of studies
Table 2 summarizes the included interventions (n = 12) and articles (n = 16). 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 Detailed intervention characteristics are available in Table S6. Included interventions primarily aimed to prevent childhood obesity (n = 5) or improve obesity‐related behaviors (n = 5), and most included content to promote multiple obesity‐related behaviors (n = 7). Most were from the United States of America (n = 7), with others from Australia, Bangladesh, Malaysia, and the United Kingdom (n = 5).
TABLE 2.
Main characteristics of included interventions (n = 12)
| Intervention characteristics | n | Reference numbers |
|---|---|---|
| Stated aim | ||
| Obesity prevention | 5 | 47 , 49 / 50 / 51 , 55 , 56 , 57 / 58 |
| Improving specific behavior(s) | 5 | 48 , 53 / 54 , 59 , 60 , 61 |
| Child development | 2 | 46 , 52 |
| Target obesity‐related behavior(s) | ||
| Multiple lifestyle behaviors | 7 | 47 , 49 / 50 / 51 , 52 , 55 , 56 , 57 / 58 , 60 |
| Activity and sedentary behaviors | 3 | 53 / 54 , 59 , 61 |
| Feeding and nutrition | 2 | 46 , 48 |
| Target child age | ||
| In utero until 2 years | 4 | 46 , 56 , 57 / 58 , 61 |
| 2–5 years | 7 | 47 , 48 , 49 / 50 / 51 , 52 , 53 / 54 , 55 , 59 |
| 0–5 years | 1 | 60 |
| Engaged in intervention | ||
| Child | 3 | 53 / 54 , 59 , 60 |
| Parent/caregiver and child | 9 | 46 , 47 , 48 , 49 / 50 / 51 , 52 , 55 , 56 , 57 / 58 , 61 |
| Setting b | ||
| Early education and care settings | 5 | 47 , 49 / 50 / 51 , 53 / 54 , 59 , 60 |
| Community venue | 3 | 52 , 59 , 61 |
| Home | 3 | 48 , 52 , 56 |
| Healthcare clinic or hospital | 3 | 55 , 57 / 58 , 61 |
| Community health center | 2 | 46 , 48 |
| Mode of delivery b | ||
| Face‐to‐face, groups | 10 | 46 , 47 , 48 , 49 / 50 / 51 , 53 / 54 , 55 , 59 , 60 , 57 / 58 , 61 |
| Face‐to‐face, individual | 2 | 48 , 52 |
| Telephone, individual | 1 | 56 |
| Online component | 1 | 47 |
| Provider/facilitator | ||
| Health professional | 4 | 46 , 52 , 55 , 56 |
| Childcare staff member | 3 | 47 , 49 / 50 / 51 , 53 / 54 |
| Parents or peers | 3 | 48 , 60 , 57 / 58 |
| Research assistant | 2 | 59 , 61 |
| Theory of intervention | ||
| Described/referred to | 7 | 47 , 48 , 49 / 50 / 51 , 55 , 56 , 59 , 57 / 58 |
| Not described | 5 | 46 , 52 , 53 / 54 , 60 , 61 |
Multiple categories applied to some interventions; therefore, the sum is greater than 12.
Of the included interventions, most were family‐based, involving parents/caregivers and children (n = 9). Some specifically targeted physical activity behaviors, 61 sedentary behaviors, 53 , 59 or nutrition and feeding behaviors. 46 , 48 Most interventions focused on when children were aged 2–5 years (n = 7), with four interventions focused on the earlier years in life (pregnancy to child aged 2 years). One intervention targeted children aged 0–5 years attending childcare services. 60
The delivery setting varied within and across interventions, based within the home, healthcare, community and early education and care settings (e.g., preschool and childcare). The mode of delivery was predominately face‐to‐face group sessions (n = 10), with three interventions delivered individually, 48 , 52 , 56 and one of these was via telephone. 56 The intervention providers also varied and included health professionals, childcare staff members, other parents or peers, and research assistants. Some included interventions (n = 7) described or referred to the interventions' underpinning theories, most commonly social cognitive theory (n = 4). 47 , 49 , 56 , 59 Further details are included in Table S6.
3.3. Cultural adaptation processes and strategies
The included articles described various stages of the cultural adaptation process, defined according to the Stages of Cultural Adaptation theoretical model 35 (see Table 3). The detailed cultural adaptation data extracted is presented in Table S7. Most interventions (n = 8) included reporting on cultural adaptation Stages 1–4, and four reported on Stage 5 only.
Five of the culturally adapted interventions 46 , 48 , 52 , 56 , 57 referred to cultural adaptation theories or frameworks. These included process models or frameworks 35 , 62 , 63 that informed the steps for undertaking the cultural adaptation and theoretical guidance for the types of cultural adaptation strategies or content. 23 , 36 , 37 , 64 , 65 The cultural sensitivity theory by Resnicow et al. 36 , 37 was referred to by three of the interventions 48 , 52 , 56 and was used to inform and categorize the types of cultural adaptations undertaken (surface versus deep structure).
There was wide variation in the detail presented about the cultural adaptation process and the strategies used. This may be partly due to the stage of cultural adaptation reported; there was generally more explicit information presented if the preliminary stages of cultural adaptation design were the focus (Stages 1–4). Thorough descriptions were offered by some studies, 46 , 52 , 56 with others providing few details. 47 , 53 All reports gave some information about the adaptations made; however, again, the level of detail varied greatly. More commonly, interventions included both surface and deep structure adaptations (n = 7), where both the observable characteristics and a deeper understanding of the target cultural group are incorporated into the adaptations made. The most common adaptations were modifying language and translations (surface structure), altering activities to improve suitability (surface structure), addressing cultural values in the intervention content (deep structure), and involving culturally matched intervention facilitators (surface and deep structure).
Most intervention adaptations involved members of the target cultural group to some extent (n = 10); however, the level of engagement varied, from input from staff who identified with the target group (e.g., Nitsos et al. 61 ) to community member involvement in project steering committees (e.g., Hiratsuka et al. and Murtha et al. 52 , 60 ). The project leadership was not always explicitly stated; however, from the information presented, it is likely that ultimately researchers led the projects and adaptations of the included interventions.
3.4. Culturally adapted intervention effectiveness
Of the 12 included interventions, six described assessing behavioral or health outcomes. 47 , 49 , 53 , 55 , 57 , 59 However, one was a protocol report only, 47 and another 53 was a case–control design. The remaining four were randomized controlled trials. Meta‐analyses could not be undertaken due to the differences in the interventions, study designs, and outcome measures. The synthesis is described here and summarized in Table S8.
Two interventions were randomized controlled pilot or feasibility trials with high‐quality reporting and directionally positive behavioral results, but were not powered to detect definitive effects upon behavioral outcomes. 55 , 57 The Healthy Balance intervention for Latino immigrant families 55 provided a strong example of adaptations, refinement, and feasibility testing of the culturally adapted intervention in two pilot studies. Although there were no significant intervention effects for children, changes in adult outcomes were observed (significantly reducing body mass index [BMI], neck circumference, and diastolic blood pressure for parent/caregiver participants). Similarly, the HAPPY intervention 57 did not find significant outcome measurements, yet notably, this was not the study's primary aim. HAPPY 57 offers a strong example of exploring the acceptability of the adapted intervention and the feasibility of a full‐scale trial evaluation.
Two interventions were randomized controlled trials statistically powered to assess the effectiveness of the culturally adapted intervention. 49 , 59 The Hip‐Hop to Health Jr. 49 , 50 , 51 diet and physical activity intervention among African–American and Latino preschool children and parents included a large sample size with primary and secondary outcomes assessed up to 2 years of post‐intervention. The authors found no significant differences between intervention and control group outcomes among the Latino children, 49 , 50 , 51 yet an effective reduction of BMI among the African–American children in the intervention. Conversely, the culturally adapted Fit 5 Kids intervention effectively reduced television viewing time among children in the intervention group (n = 90) by nearly 3 fewer hours/week than children in the control group (n = 70). 59
3.5. Quality appraisal
The quality appraisals using the MMAT 39 are available in full in Table S9. One article included in this review was written by the authors of this review (Marshall et al. 56 ); therefore, two external assessors (BM and AR, public health doctoral candidates experienced in early life interventions) independently conducted the MMAT scoring for this article there was 100% agreement. For the other 11 intervention studies, there was 75% scoring consistency between two independent author assessments (SM another author CR, LMW, ST, YL, or PL).
All met the MMAT initial screening questions indicating clear research questions or aims and appropriate data collection methods to answer the research questions. The five MMAT method categories classified included intervention studies as qualitative research, 46 , 52 , 56 randomized controlled trials, 47 , 49 , 55 , 57 , 59 quantitative nonrandomized studies, 48 , 53 or mixed method studies. 60 , 61
Three intervention studies met all five MMAT criteria for their study design, 46 , 56 , 57 therefore suggesting higher methodological quality with lower risk of bias. Two met all but one of the criteria for their study design. 52 , 59 While the included protocol article 47 was scored, the scoring was based only on the authors' proposed work. The remaining six interventions did not meet several of the MMAT criteria, with some reports missing information for conclusively scoring as “yes” or “no,” making it difficult to fully assess the methodological quality.
4. DISCUSSION
This systematic review aimed to identify culturally adapted interventions targeting obesity‐related behaviors (including infant feeding, nutrition, physical activity, and/or sleep) among children aged 0–5 years. The research questions related specifically to the processes undertaken, types, and effectiveness of the cultural adaptations. This review identified 12 behavioral interventions, most of which were published in the last 5 years (n = 10) and from high‐income, English‐speaking countries (n = 10). Few interventions reported all aspects of the cultural adaptation processes, and the cultural adaptation strategies documented varied. Synthesis of the findings indicates improved acceptability among target populations after cultural adaptation of the intervention. Yet, with only four interventions delivered as part of a controlled trial, there is currently limited evidence to demonstrate the effectiveness of culturally adapted interventions for behavioral outcomes among young children.
Interventions identified varied in their design, quality, and reporting, making comparisons challenging. Only half of the included interventions reported using cultural adaptation guidance and theories. Some reported on the preliminary cultural adaptation stages in detail (e.g., Akter et al., Hiratsuka, et al., and Marshall et al. 46 , 52 , 56 ), whereas others reported the trial and summarized the initial cultural adaptation stages in the methods writing (e.g., Hon et al. and Mendoza et al. 53 , 59 ). Although most described a stepwise approach to cultural adaptation, it is evident that more consistency is needed for undertaking and reporting cultural adaptation studies. Our findings are consistent with other reviews of culturally adapted interventions, 20 , 24 , 26 calling for more rigorous and consistent use of theory and reporting standards. This may partly be because processes and frameworks for cultural adaptation of health promotion and prevention interventions are still developing. 23 , 64
Most of the culturally adapted early childhood behavioral interventions identified in this review involved the target population in some way. This is promising as involvement of the target population is recognized as essential throughout the cultural adaptation process for improving intervention cultural relevance and engagement. 66 , 67 The extent to which the interventionists engaged constituents did vary, however. Some consulted with target cultural group members before adaptations (e.g., Linville et al. 55 ), while others engaged them throughout the process (e.g., Hiratsuka et al. 52 ). There was also the varied engagement of other key stakeholders such as community leaders, experts, and health professionals.
Although it is agreed that stakeholders should be involved in adaptation efforts, 21 there is no explicit agreement or guidance on how to conduct this. Similar to our findings, a recent scoping review of culturally adapted health interventions for Indigenous peoples found that stakeholder involvement was common, but ownership and direction from the community were less so. 68 This may be a common finding given the nature of culturally adapting an existing evidence‐based intervention as opposed to designing an intervention with a community from the ground up.
Community‐based participatory research approaches describe community participation and decision making throughout research efforts. 69 The Healthy Migrant Families Initiative, a culturally competent obesity prevention intervention for African migrants (Australia), 70 is an example of community‐based participatory research to create and develop (opposed to adapt) a tailored intervention. Although few of the interventions included in this review referred to participatory design approaches, 46 , 52 this is an emerging area in research and practice that warrants further consideration in the context of culturally adapting interventions to enable deeper engagement with target communities. Particularly as the level of participation from target communities may be predictive of the level of the desired behavior changes. 22
Cultural adaptations of interventions have been associated with better outcomes among target populations in other fields 17 and in lifestyle behavioral interventions. 71 However, the findings are inconsistent. In this review, only two interventions were statistically powered to assess the effectiveness of the culturally adapted intervention; therefore, it was not possible to conduct a meta‐analysis or definitively draw conclusions about how effective cultural adaptations were in achieving behavioral or health‐related outcomes among children 0–5 years. There is a need for increased research beyond formative evaluation and feasibility trials to assess effects and validate the investment of culturally adapted interventions.
Further to this, significant resources are required to conduct appropriately designed effectiveness trials of culturally adapted interventions. This may partly explain why few studies of this kind were identified. Research designs that include multiple versions of the culturally adapted program can investigate what (if any) adaptations are needed to achieve behavioral outcomes. 20 Noting that direct comparisons between a mainstream/nonadapted intervention and a culturally adapted intervention are ideal for assessing effect, however, may be challenging to implement. For example, target community members who may access a culturally adapted intervention may not access a mainstream intervention due to language barriers; therefore, setting up a randomized trial in this way may not be appropriate. Further consideration of research designs for outcome evaluation is essential for progressing cultural adaptation science. 18 , 72
4.1. Strengths and limitations
This is the first systematic review to investigate worldwide cultural adaptations of obesity‐related behavioral interventions focused on children under 5 years. The strengths of our review include the rigorous review process, prospective review registration, comprehensive search strategy across multiple databases, dual independent reviewer processes, and synthesis based on cultural adaptation stages and reporting frameworks. Our review was limited to peer‐reviewed literature in English, thereby reducing the scope of our findings. Our review was also complicated by the differences in cultural adaptation approaches, study designs, and reporting presented in the included articles, which made comparing results difficult. Furthermore, as our review synthesized reported findings, it is possible that cultural adaptations were conducted but details of adaptations were not reported. The limited report length and formatting imposed by research journals may contribute to this. Due to time constraints, we did not contact the interventionists for more information, which could have enhanced this synthesis and reduced potential reporting biases. Similarly, a more extensive review of gray literature could illuminate other cultural adaptation processes and outcomes with on‐the‐ground applications for cultural and country context adaptations, particularly for low‐resource settings.
4.2. Implications for practice and policy
Working with families from minority cultural groups, including culturally and linguistically diverse populations, remains a global priority to reduce health inequities and improve support for populations at higher risk of experiencing obesity. Although this review cannot offer definitive conclusions for the effectiveness of culturally adapted early obesity‐related behavioral prevention interventions, the findings provide process guidance for what and how to adapt established interventions for specific cultural groups. It is important to thoroughly document and report on each stage of the cultural adaptation process for transparency and replicability. The use of established cultural adaptation evidence, frameworks, and guidance (e.g., Movsisyan et al., Barrera et al., and Resnicow et al. 21 , 35 , 36 ) will strengthen the cultural adaptation of interventions. Cultural adaptations of interventions should ensure involvement with target populations and consider underpinning program theories to implement deep structure adaptations that are meaningful and acceptable to the target populations.
Cultural adaptation of early childhood obesity‐related behavioral prevention interventions is a promising strategy for improving engagement, acceptability, and health outcomes among minority cultural groups. Addressing cultural fit and subgroup differences is essential for population‐level impacts and should be a priority for practice and policy. 73 Although acknowledging there can be practical constraints to undertaking cultural adaptation projects (such as finances, resources, and time), actions toward cultural adaptations of evidence‐based early life health interventions being implemented and sustained in practice are recommended. 74 , 75
4.3. Implications for research
The findings of this review highlight the need for further research regarding (a) cultural adaptation processes and strategies for early childhood health promotion and obesity prevention interventions targeting specific cultural communities, (b) sufficiently powered trials to assess the effects of the adapted interventions on target behaviors and health outcomes, and (c) culturally adapted interventions targeting children aged 0–2 years, which is a crucial period for establishing healthy behaviors and supporting families early in life. Additionally, there is emerging evidence about obesity risk factors in early childhood and those most pertinent for minority populations, 76 , 77 , 78 , 79 which should continue to inform obesity prevention interventions targeting specific cultural communities. Positively, much work is occurring in the United States of America, yet more research is needed globally, for other countries and specific minority populations.
5. CONCLUSION
This is the first systematic review investigating worldwide cultural adaptations of obesity‐related behavioral interventions targeting children under 5 years among culturally and linguistically diverse communities. The cultural adaptation strategies documented were varied and the use of cultural adaptation guidance and involvement of target communities were inconsistent. These results suggest that cultural adaptation of early childhood obesity‐related behavioral prevention interventions may increase acceptability among target populations. Yet, there needs to be more detailed reporting of cultural adaptation processes for further evaluation of this work. Additionally, few studies assess the effectiveness of cultural adaptations for obesity‐related behavioral outcomes; therefore, this should focus on future research efforts to ultimately reduce health inequities.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.
Supporting information
Table S1. PRISMA 2020 item checklist and abstracts checklist
Table S2. Final search terms for database searches: Ovid (MEDLINE[R] and Epub Ahead of Print, Embase, ERIC, Global Health, PsychINFO)
Table S3. Final search terms for database searches: Ebscohost CINAHL
Table S4. Final search terms for database searches: Scopus
Table S5. Final search terms for database searches: Web of Science
Table S6. Summary characteristics of included interventions
Table S7. Cultural adaptation data extracted for included interventions
Table S8. Effectiveness of culturally adapted intervention quantitative trials
Table S9. Final Mixed Method Appraisal Tool (MMAT) scoring for included interventions
ACKNOWLEDGMENTS
We would like to thank Bernadette Carr and Roderick Dyson, librarians from the University of Sydney, who assisted with refining the search terms. We would also like to thank Mahalakshmi Ekambareshwar for contributing toward the title and abstract screening and Brittany Markides and Ana Renda for their independent assessment of one study included in this review. Authors SM, ST, PL, LMW, CR are affiliated with, and SM receives a postgraduate scholarship from the National Health and Medical Research Council Centre for Research Excellence in The Early Prevention of Obesity in Childhood (EPOCH CRE) (GNT1101675).
Marshall S, Taki S, Laird Y, Love P, Wen LM, Rissel C. Cultural adaptations of obesity‐related behavioral prevention interventions in early childhood: A systematic review. Obesity Reviews. 2022;23(4):e13402. doi: 10.1111/obr.13402
Funding information National Health and Medical Research Council Centre for Research Excellence in The Early Prevention of Obesity in Childhood (EPOCH CRE), Grant/Award Number: GNT1101675
REFERENCES
- 1. Baur LA, Garnett SP. Early childhood—a critical period for obesity prevention. Nat Rev Endocrinol. 2018;15(1):5‐6. 10.1038/s41574-018-0131-0 [DOI] [PubMed] [Google Scholar]
- 2. Black RE, Victora CG, Walker SP, et al. Maternal and child undernutrition and overweight in low‐income and middle‐income countries. Lancet. 2013;382(9890):427‐451. 10.1016/S0140-6736(13)60937-X [DOI] [PubMed] [Google Scholar]
- 3. Simmonds M, Llewellyn A, Owen CG, Woolacott N. Predicting adult obesity from childhood obesity: a systematic review and meta‐analysis. Obes Rev. 2016;17(2):95‐107. 10.1111/obr.12334 [DOI] [PubMed] [Google Scholar]
- 4. NCD Risk Factor Collaboration (NCD‐RisC) . Worldwide trends in body‐mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population‐based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627‐2642. 10.1016/S0140-6736(17)32129-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. World Health Organization . Report of the Commission on Ending Childhood Obesity: implementation plan: executive summary. World Health Organization. 2017. Available at: https://apps.who.int/iris/handle/10665/259349. Accessed 06 August 2021.
- 6. Brown T, Moore TH, Hooper L, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2019;7(7):CD001871. Published 2019 Jul 23. 10.1002/14651858.CD001871.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Blake‐Lamb TL, Locks LM, Perkins ME, Woo Baidal JA, Cheng ER, Taveras EM. Interventions for Childhood Obesity in the First 1,000 Days A Systematic Review. Am J Prev Med. 2016;50(6):780‐789. 10.1016/j.amepre.2015.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hennessy M, Heary C, Laws R, et al. The effectiveness of health professional‐delivered interventions during the first 1000 days to prevent overweight/obesity in children: a systematic review. Obes Rev. 2019;20(12):1691‐1707. 10.1111/obr.12924 [DOI] [PubMed] [Google Scholar]
- 9. Ash T, Agaronov A, Young T, Aftosmes‐Tobio A, Davison KK. Family‐based childhood obesity prevention interventions: a systematic review and quantitative content analysis. Int J Behav Nutr Phys Act. 2017;14(1):113. 10.1186/s12966-017-0571-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Askie LM, Espinoza D, Martin A, et al. Interventions commenced by early infancy to prevent childhood obesity‐The EPOCH Collaboration: An individual participant data prospective meta‐analysis of four randomized controlled trials. Pediatr Obes. 2020;15(6):e12618. 10.1111/ijpo.12618 [DOI] [PubMed] [Google Scholar]
- 11. Dixon B, Peña MM, Taveras EM. Lifecourse approach to racial/ethnic disparities in childhood obesity. Adv Nutr. 2012;3(1):73‐82. 10.3945/an.111.000919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hardy LL, Jin K, Mihrshahi S, Ding D. Trends in overweight, obesity, and waist‐to‐height ratio among Australian children from linguistically diverse backgrounds, 1997 to 2015. Int J Obes (Lond). 2019;43(1):116‐124. 10.1038/s41366-018-0139-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. De Freitas C, Massag J, Amorim M, Fraga S. Involvement in maternal care by migrants and ethnic minorities: a narrative review. Public Health Rev. 2020;41(1):5. Published 2020 Apr 7. 10.1186/s40985-020-00121-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Au M, Anandakumar AD, Preston R, Ray RA, Davis M. A model explaining refugee experiences of the Australian healthcare system: a systematic review of refugee perceptions. BMC Int Health Hum Rights. 2019;19(1):22. Published 2019 Jul 18. 10.1186/s12914-019-0206-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Benza S, Liamputtong P. Pregnancy, childbirth and motherhood: a meta‐synthesis of the lived experiences of immigrant women. Midwifery. 2014;30(6):575‐584. 10.1016/j.midw.2014.03.005 [DOI] [PubMed] [Google Scholar]
- 16. Bernal G, Bonilla J, Bellido C. Ecological validity and cultural sensitivity for outcome research: issues for the cultural adaptation and development of psychosocial treatments with Hispanics. J Abnorm Child Psychol. 1995;23(1):67‐82. 10.1007/BF01447045 [DOI] [PubMed] [Google Scholar]
- 17. Ferrer‐Wreder L, Sundell K, Mansoory S. Tinkering with perfection: theory development in the intervention cultural adaptation field. Child Youth Care Forum. 2012;41(2):149‐171. 10.1007/s10566-011-9162-6 [DOI] [Google Scholar]
- 18. Castro FG, Barrera M Jr, Holleran Steiker LK. Issues and challenges in the design of culturally adapted evidence‐based interventions. Annu Rev Clin Psychol. 2010;6(1):213‐239. 10.1146/annurev-clinpsy-033109-132032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Domenech Rodríguez MM, Bernal G. Frameworks, models, and guidelines for cultural adaptation. In: Bernal G, Domenech Rodríguez MM, eds. Cultural Adaptations: Tools for Evidence‐Based Practice with Diverse Populations. 2012. 10.1037/13752-002 [DOI] [Google Scholar]
- 20. Baumann AA, Powell BJ, Kohl PL, et al. Cultural adaptation and implementation of evidence‐based parent‐training: a systematic review and critique of guiding evidence. Child Youth Serv Rev. 2015;53:113‐120. 10.1016/j.childyouth.2015.03.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Movsisyan A, Arnold L, Evans R, et al. Adapting evidence‐informed complex population health interventions for new contexts: a systematic review of guidance. Implement Sci. 2019;14(1):105. Published 2019 Dec 17. 10.1186/s13012-019-0956-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wiltsey Stirman S, Baumann AA, Miller CJ. The FRAME: an expanded Framework for Reporting Adaptations and Modifications to evidence‐based interventions. Implement Sci. 2019;14(1):58. Published 2019 Jun 6. 10.1186/s13012-019-0898-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Liu J, Davidson E, Bhopal R, et al. Adapting health promotion interventions to meet the needs of ethnic minority groups: mixed‐methods evidence synthesis. Health Technol Assess. 2012;16(44):1‐469. 10.3310/hta16440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Barr‐Anderson DJ, Adams‐Wynn AW, DiSantis KI, Kumanyika S. Family‐focused physical activity, diet and obesity interventions in African‐American girls: a systematic review. Obes Rev. 2013;14(1):29‐51. 10.1111/j.1467-789X.2012.01043.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lofton S, Julion WA, McNaughton DB, Bergren MD, Keim KS. A systematic review of literature on culturally adapted obesity prevention interventions for African American youth. J Sch Nurs. 2016;32(1):32‐46. 10.1177/1059840515605508 [DOI] [PubMed] [Google Scholar]
- 26. Bender MS, Clark MJ. Cultural adaptation for ethnic diversity: a review of obesity interventions for preschool children. Calif J Health Promot. 2011;9(2):40‐60. [PMC free article] [PubMed] [Google Scholar]
- 27. Woo Baidal JA, Locks LM, Cheng ER, Blake‐Lamb TL, Perkins ME, Taveras EM. Risk factors for childhood obesity in the first 1,000 days: a systematic review. Am J Prev Med. 2016;50(6):761‐779. 10.1016/j.amepre.2015.11.012 [DOI] [PubMed] [Google Scholar]
- 28. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. Published 2021 Mar 29. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Marshall S, Rissel C, Wen LM, Love P, Taki S, Laird Y. Culturally‐adapted childhood obesity prevention interventions: a systematic narrative review. PROSPERO: International Prospective Register of Systematic Reviews. 2018. CRD42018105596. Available at: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42018105596? [Google Scholar]
- 30. Hawkins SS, Cole TJ, Law C, Millennium Cohort Study Child Health Group . An ecological systems approach to examining risk factors for early childhood overweight: findings from the UK millennium cohort study. J Epidemiol Community Health. 2009;63(2):147‐155. 10.1136/jech.2008.077917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Covidence Systematic Review Software . Melbourne, Australia: Veritas Health Innovation; 2021. Available at https://www.covidence.org
- 32. Milbrath G, Gopinath V, Constance C, Ogendi A, Compton M, Plews‐Ogan J. Implementing and evaluating a sustainable early child development program in Limpopo, South Africa: A pilot study. Ann Glob Health. 2015;81(1):162. 10.1016/j.aogh.2015.02.870 [DOI] [Google Scholar]
- 33. Burmaz T, Villani M, Cattaneo A, Milinco M, Romero S. Compliance to preventive interventions in infancy among immigrants: a randomised trial. Quad ACP. 2007;14(2):50‐55. [Google Scholar]
- 34. Gallois KM, de Henauw S, Hassel H, Hebestreit A, Pigeot I, Zeeb H. Standardisierte Entwicklung der IDEFICS‐Intervention und Implementierung in Deutschland [Standardized development of the IDEFICS intervention and its implementation in Germany]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2011;54(3):330‐338. 10.1007/s00103-010-1220-y [DOI] [PubMed] [Google Scholar]
- 35. Barrera M Jr, Castro FG, Strycker LA, Toobert DJ. Cultural adaptations of behavioral health interventions: a progress report. J Consult Clin Psychol. 2013;81(2):196‐205. 10.1037/a0027085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: defined and demystified. Ethn Dis. 1999;9(1):10‐21. [PubMed] [Google Scholar]
- 37. Resnicow K, Soler R, Braithwaite RL, Ahluwalia JS, Butler J. Cultural sensitivity in substance use prevention. J Community Psychol. 2000;28(3):271‐290. [DOI] [Google Scholar]
- 38. Sandelowski M, Voils CI, Barroso J. Defining and designing mixed research synthesis studies. Res Sch. 2006;13(1):29. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2809982/ [PMC free article] [PubMed] [Google Scholar]
- 39. Hong QN, Gonzalez‐Reyes A, Pluye P. Improving the usefulness of a tool for appraising the quality of qualitative, quantitative and mixed methods studies, the Mixed Methods Appraisal Tool (MMAT). J Eval Clin Pract. 2018;24(3):459‐467. 10.1111/jep.12884 [DOI] [PubMed] [Google Scholar]
- 40. Pace R, Pluye P, Bartlett G, et al. Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. Int J Nurs Stud. 2012;49(1):47‐53. 10.1016/j.ijnurstu.2011.07.002 [DOI] [PubMed] [Google Scholar]
- 41. Hong QN, Pluye P, Fàbregues S, et al. Improving the content validity of the mixed methods appraisal tool: a modified e‐Delphi study. J Clin Epidemiol. 2019;111:49‐59.e1. 10.1016/j.jclinepi.2019.03.008 [DOI] [PubMed] [Google Scholar]
- 42. Bender MS, Nader PR, Kennedy C, Gahagan S. A culturally appropriate intervention to improve health behaviors in Hispanic mother‐child dyads. Child Obes. 2013;9(2):157‐163. 10.1089/chi.2012.0118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Barkin SL, Gesell SB, Po'e EK, Escarfuller J, Tempesti T. Culturally tailored, family‐centered, behavioral obesity intervention for Latino‐American preschool‐aged children. Pediatrics. 2012;130(3):445‐456. 10.1542/peds.2011-3762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. de Henauw S, Verbestel V, Mårild S, et al. The IDEFICS community‐oriented intervention programme: a new model for childhood obesity prevention in Europe? Int J Obes (Lond). 2011;35(Suppl 1):S16‐S23. 10.1038/ijo.2011.31 [DOI] [PubMed] [Google Scholar]
- 45. Baranowski T, Lytle L. Should the IDEFICS outcomes have been expected? Obes Rev. 2015;16(Suppl 2):162‐172. 10.1111/obr.12359 [DOI] [PubMed] [Google Scholar]
- 46. Akter F, Rahman M, Pitchik HO, et al. Adaptation and integration of psychosocial stimulation, maternal mental health and nutritional interventions for pregnant and lactating women in rural Bangladesh. Int J Environ Res Public Health. 2020;17(17):6233. Published 2020 Aug 27. 10.3390/ijerph17176233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Armstrong B, Trude ACB, Johnson C, et al. CHAMP: A cluster randomized‐control trial to prevent obesity in child care centers. Contemp Clin Trials. 2019;86:105849. 10.1016/j.cct.2019.105849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Broyles SL, Brennan JJ, Burke KH, Kozo J, Taras HL. Cultural adaptation of a nutrition education curriculum for Latino families to promote acceptance. J Nutr Educ Behav. 2011;43(4 Suppl 2):S158‐S161. 10.1016/j.jneb.2011.02.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Fitzgibbon ML, Stolley MR, Schiffer L, van Horn L, KauferChristoffel K, Dyer A. Hip‐Hop to Health Jr. for Latino preschool children. Obesity (Silver Spring). 2006;14(9):1616‐1625. 10.1038/oby.2006.186 [DOI] [PubMed] [Google Scholar]
- 50. Fitzgibbon ML, Stolley MR, Dyer AR, VanHorn L, KauferChristoffel K. A community‐based obesity prevention program for minority children: rationale and study design for Hip‐Hop to Health Jr. Prev Med. 2002;34(2):289‐297. 10.1006/pmed.2001.0977 [DOI] [PubMed] [Google Scholar]
- 51. Fitzgibbon ML, Stolley MR, Schiffer L, van Horn L, KauferChristoffel K, Dyer A. Two‐year follow‐up results for Hip‐Hop to Health Jr.: a randomized controlled trial for overweight prevention in preschool minority children. J Pediatr. 2005;146(5):618‐625. 10.1016/j.jpeds.2004.12.019 [DOI] [PubMed] [Google Scholar]
- 52. Hiratsuka VY, Parker ME, Sanchez J, et al. Cultural adaptations of evidence‐based home‐visitation models in tribal communities. Infant Ment Health J. 2018;39(3):265‐275. 10.1002/imhj.21708 [DOI] [PubMed] [Google Scholar]
- 53. Hon KY, Chua BS, Hashmi SI. Effectiveness of ToyBox intervention to reduce sedentary behaviour among pre‐school children: a case in Malaysia. Pertanika J Soc Sci Humanit. 2018;26(1):425–440. Available at: http://www.pertanika.upm.edu.my/pjssh/browse/regular-issue?article=JSSH-1975-2016 Accessed 06 August 2021 [Google Scholar]
- 54. Reeves S, Poh BK, Cheah WL, et al. ToyBox Study Malaysia: a feasibility study to improve healthy energy balance and obesity‐related behaviour. Proceedings of the Nutrition Society. 2020;79(OCE2):E313. 10.1017/S002966512000261X [DOI] [Google Scholar]
- 55. Linville D, Mintz B, Martinez C, Gau JM, Shune S, Stice E. Preliminary effects of tailoring an obesity prevention intervention program for Latino immigrant families. Fam Community Health. 2020;43(2):118‐130. 10.1097/FCH.0000000000000252 [DOI] [PubMed] [Google Scholar]
- 56. Marshall S, Taki S, Love P, et al. The process of culturally adapting the Healthy Beginnings early obesity prevention program for Arabic and Chinese mothers in Australia. BMC Public Health. 2021;21(1):284. Published 2021 Feb 4. 10.1186/s12889-021-10270-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. McEachan RRC, Santorelli G, Bryant M, et al. The HAPPY (Healthy and Active Parenting Programmme for early Years) feasibility randomised control trial: acceptability and feasibility of an intervention to reduce infant obesity. BMC Public Health. 2016;16(1):211. Published 2016 Mar 1. 10.1186/s12889-016-2861-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Taylor NJ, Sahota P, Sargent J, et al. Using intervention mapping to develop a culturally appropriate intervention to prevent childhood obesity: the HAPPY (Healthy and Active Parenting Programme for Early Years) study. Int J Behav Nutr Phys Act. 2013;10:142. Published 2013 Dec 28. 10.1186/1479-5868-10-142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Mendoza JA, Baranowski T, Jaramillo S, et al. Fit 5 Kids TV reduction program for Latino preschoolers: a cluster randomized controlled trial. Am J Prev Med. 2016;50(5):584‐592. 10.1016/j.amepre.2015.09.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Murtha K, Thompson K, Cleland P, Gallegos D. Adaptation and evaluation of a nutrition and physical activity program for early childhood education settings in Aboriginal and Torres Strait Islander communities in remote Far North Queensland. Health Promot J Austr. 2021;32(2):163‐171. 10.1002/hpja.352 [DOI] [PubMed] [Google Scholar]
- 61. Nitsos A, Estrada RD, Messias DKH. Tummy time for Latinos with limited English proficiency: evaluating the feasibility of a cultural and linguistically adapted parent education intervention. J Pediatr Nurs. 2017;36:31‐36. 10.1016/j.pedn.2017.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Netto G, Bhopal R, Lederle N, Khatoon J, Jackson A. How can health promotion interventions be adapted for minority ethnic communities? Five principles for guiding the development of behavioural interventions. Health Promot Int. 2010;25(2):248‐257. 10.1093/heapro/daq012 [DOI] [PubMed] [Google Scholar]
- 63. Goldstein NE, Kemp KA, Leff SS, Lochman JE. Guidelines for adapting manualized interventions for new target populations: a step‐wise approach using anger management as a model. Clin Psychol (New York). 2012;19(4):385‐401. 10.1111/cpsp.12011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Kreuter MW, Lukwago SN, Bucholtz RD, Clark EM, Sanders‐Thompson V. Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health Educ Behav. 2003;30(2):133‐146. 10.1177/1090198102251021 [DOI] [PubMed] [Google Scholar]
- 65. Castro FG, Barrera M Jr, Martinez CR Jr. The cultural adaptation of prevention interventions: resolving tensions between fidelity and fit. Prev Sci. 2004;5(1):41‐45. 10.1023/b:prev.0000013980.12412.cd [DOI] [PubMed] [Google Scholar]
- 66. Movsisyan A, Arnold L, Copeland L, et al. Adapting evidence‐informed population health interventions for new contexts: a scoping review of current practice. Heal Res Policy Syst. 2021;19(1):13. 10.1186/s12961-020-00668-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Kumpfer K, Magalhães C, Xie J. Cultural adaptation and implementation of family evidence‐based interventions with diverse populations. Prev Sci. 2017;18(6):649‐659. 10.1007/s11121-016-0719-3 [DOI] [PubMed] [Google Scholar]
- 68. Vincze L, Barnes K, Somerville M, et al. Cultural adaptation of health interventions including a nutrition component in Indigenous peoples: a systematic scoping review. Int J Equity Health 2021;20(1):125. Published 2021 May 22. 10.1186/s12939-021-01462-x, 20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Wallerstein NB, Duran B. Using community‐based participatory research to address health disparities. Health Promot Pract. 2006;7(3):312‐323. 10.1177/1524839906289376 [DOI] [PubMed] [Google Scholar]
- 70. Renzaho AM, Halliday JA, Mellor D, Green J. The Healthy Migrant Families Initiative: development of a culturally competent obesity prevention intervention for African migrants. BMC Public Health. 2015;15(1):272. Published 2015 Mar 19. 10.1186/s12889-015-1628-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Nierkens V, Hartman MA, Nicolaou M, et al. Effectiveness of cultural adaptations of interventions aimed at smoking cessation, diet, and/or physical activity in ethnic minorities. a systematic review. PLoS One. 2013;8(10):e73373. Published 2013 Oct 7. 10.1371/journal.pone.0073373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Lau Anna S. Making the case for selective and directed cultural adaptations of evidence‐based treatments: examples from parent training. Clinical Psychology: Science and Practice.. 2006;13(4):295‐310. 10.1111/j.1468-2850.2006.00042.x [DOI] [Google Scholar]
- 73. Gonzales NA. expanding the cultural adaptation framework for population‐level impact. Prev Sci. 2017;18(6):689‐693. 10.1007/s11121-017-0808-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Moore G, Campbell M, Copeland L, et al. Adapting interventions to new contexts‐the ADAPT guidance. BMJ. 2021;374:n1679. 10.1136/bmj.n1679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Barrera M Jr, Berkel C, Castro FG. Directions for the advancement of culturally adapted preventive interventions: local adaptations, engagement, and sustainability. Prev Sci. 2017;18(6):640‐648. 10.1007/s11121-016-0705-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Peña MM, Dixon B, Taveras EM. Are you talking to ME? The importance of ethnicity and culture in childhood obesity prevention and management. Child Obes. 2012;8(1):23‐27. 10.1089/chi.2011.0109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Chatham RE, Mixer SJ. Cultural influences on childhood obesity in ethnic minorities: a qualitative systematic review. J Transcult Nurs. 2020;31(1):87‐99. 10.1177/1043659619869428 [DOI] [PubMed] [Google Scholar]
- 78. Taveras EM, Gillman MW, Kleinman KP, Rich‐Edwards JW, Rifas‐Shiman SL. Reducing racial/ethnic disparities in childhood obesity: the role of early life risk factors. JAMA Pediatr. 2013;167(8):731‐738. 10.1001/jamapediatrics.2013.85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Isong IA, Rao SR, Bind MA, Avendaño M, Kawachi I, Richmond TK. Racial and ethnic disparities in early childhood obesity. Pediatrics. 2018;141(1):e20170865. 10.1542/peds.2017-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. PRISMA 2020 item checklist and abstracts checklist
Table S2. Final search terms for database searches: Ovid (MEDLINE[R] and Epub Ahead of Print, Embase, ERIC, Global Health, PsychINFO)
Table S3. Final search terms for database searches: Ebscohost CINAHL
Table S4. Final search terms for database searches: Scopus
Table S5. Final search terms for database searches: Web of Science
Table S6. Summary characteristics of included interventions
Table S7. Cultural adaptation data extracted for included interventions
Table S8. Effectiveness of culturally adapted intervention quantitative trials
Table S9. Final Mixed Method Appraisal Tool (MMAT) scoring for included interventions


