Abstract
This study examines how perceived information overload and misinformation affect vaccine hesitancy and how this is moderated by structural and cultural factors. By applying and extending the fundamental cause theory, this study proposes a contextualized impact model to analyze a cross-national survey of 6034 residents in six societies in Asia, Europe and North America in June 2021. The study finds that (1) Older and highly-educated participants were less susceptible to COVID-19 information overload and belief in vaccine misinformation. (2) Perceived information overload led to an increase in vaccine acceptance and uptake, whereas belief in vaccine misinformation caused a decrease. (3) The structural differentiation of vaccine hesitancy was salient and higher socioeconomic status could buffer the negative impact of misinformation on vaccine acceptance. (4) Cultural factors such as collectivism and authoritarian mentality also served as buffers against the misinformation that reduced vaccine acceptance and uptake. These findings add nuanced footnotes to the fundamental causes theory and contribute to the discussion on the global recovery from the infodemic. Besides fact-checking and improving individual information literacy, effective and long-term information management and health policies must pay attention to stratified information gaps across socioeconomic groups, and to contextualize the communication and intervention strategies in different cultures.
Keywords: Infodemic, Information overload, Misinformation, COVID-19 vaccine hesitancy, fundamental causes theory, Socioeconomic status, Culture, Cross-national survey
1. Introduction
In the current stage of the global anti-pandemic battles, governments around the world are facing the challenge of high COVID-19 vaccine hesitancy – “[a] delay in acceptance or refusal of the vaccine despite the availability of the vaccination services” (MacDonald, 2015, p.4136) – due to the spread of infodemic worldwide. The World Health Organization defined the term “infodemic” as “an overabundance of information – some accurate and some not – that makes it hard for people to find trustworthy sources and reliable guidance when they need it” (World Health Organization [WHO], 2020). This term has flourished in journalistic, academic, and political discourses since the pandemic (Choukou et al., 2022; Pian et al., 2021; Ries, 2022; van der Linden 2022). Empirical studies further show that anti-vaccination disinformation and misinformation have significantly increased vaccine hesitancy in various societies (Allintong et al., 2021; Daly & Robinson, 2021; Loomba et al., 2021; Romer & Jamieson, 2020; Wilson & Wiysonge, 2020). An analysis of around 100 million Facebook users across several countries revealed anti-vaccination clusters become deeply intertwined with undecided clusters, leaving the pro-vaccination clusters on the sidelines (Johnson et al., 2020). Thus, taming the infodemic could be one of crucial steps on the path to global recovery from the COVID-19 pandemic.
However, most discussions on the impact of the infodemic on protective measures focus on cognitive and psychological mechanisms of individuals’ information processing in a single society, which offers insightful suggestions on the anti-infodemic practices but leaves the impacts of structural and cultural factors systemically underexamined. A recent survey of US households in 2021 reported that 18.4% of those surveyed were unwilling to take a COVID-19 vaccine (Tram et al., 2022). A survey in UK in 2020 reported a vaccine hesitancy rate of 18% (Robertson et al., 2021). While Asian societies, where the pandemic seems to be better controlled, have much higher percentages of vaccine hesitancy: in 2020, it was 25.5% in Hong Kong (Luk et al., 2021), and in January 2021, the hesitancy was high as 37.9% in Japan (Machida et al., 2021). Such variations demand empirical studies on the impact of the infodemic on vaccine hesitancy to go beyond the individual level and beyond a single culture context.
Thus, this study aims to investigate how the infodemic impacts vaccine hesitancy and how such impacts are moderated by social structure (measured by the socioeconomic status, SES) and cultural orientation (collectivism and authoritarian mentality). The data of this study were obtained from a cross-national online survey of public attitudes and responses toward COVID-19 in six societies in Asia, Europe and North America in June 2021. The findings of this study speak to the global recovery. Following the peak of the Omicron variant, many countries have begun to move beyond restrictive policies and adopt protective measures (Edwards, et al., 2021; Petherick et al., 2021). However, managing pandemic fatigue and securing compliance with protective measures are highly contingent on information management and dissemination. Incorporating structural and cultural factors when designing protective policies may improve the effectiveness of such interventions and help battle misinformation, thus making the recovery more sustainable.
In the following, we first discuss the nuanced definition of infodemic and clarify two types of infodemic – information overload and misinformation. We synergize the existing studies and propose a contextualized impact model to analyze the impact of the infodemic on vaccine willingness and uptake. We then outline specific research questions and introduce the data and measures. Lastly, we report the findings which are followed by a brief conclusion and discussion.
2. Literature review
2.1. Multi-layers of the infodemic and its impact on vaccination
During the severe acute respiratory syndrome (SARS) outbreak in 2003, David J. Rothkopf, a political analysist in The Washington Post, coined the term “infodemic” to describe an information epidemic where “a few facts, mixed with fear, speculation and rumor, amplified and relayed swiftly worldwide by modern information technologies, have affected national and international economies, politics and even security in ways that are utterly disproportionate with the root realities” (Rothkopf, 2003). Even though it is not new that public health crises are often accompanied by rumors and false information, the recent coronavirus marks the first social media infodemic (Hao & Basu, 2020). Given the participatory nature of online platforms, the scale and speed of spreading information have created turbulence in processing and managing information during the pandemic, thereby triggering an economic, social and even political debacle.
When the WHO (2020) defined “infodemic” as “an overabundance of information”, it lacks specificity. Most existing empirical studies on “infodemic” often center around two types of information: information overload and misinformation. The former occurs when the amount and complexity of information exceed cognitive capacity; while the latter type is due to fake news, conspiracies, pseudoscience, and rumours.
Research concerning information overload (Bawden & Robinson, 2009; Rathore & Farooq, 2020) focuses on infodemic that arises when the information an individual is exposed to is much more than what they can process. Information overabundance is common in the modern new media ecosystem (Van Aelst et al., 2017). Some survey studies adapted the perceived information overload scale (Misra & Stokols, 2012) or the cancer information overload scale (Jensen et al., 2014) to the COVID-19 pandemic, and asked informants to rate their agreement with statements regarding the intensity and trustworthiness of the sources of information (e.g., Chen et al., 2022; Hong & Kim, 2020; Sarkhel et al., 2020). During the COVID-19 pandemic, a study in South Korea found no significant association between perceived information overload and intentions to take preventative measures (Hong & Kim, 2020). Other studies revealed perceived information overload tended to increase psychological distress (Chen et al., 2022). However, there is scarce systematic investigation on the impact of perceived information overload on vaccine willingness and uptake in a cross-national setting.
Studies on misinformation concern the lack of quality and accuracy of information. Although defining what misinformation is remains a challenge, a growing scholarly discussion has defined misinformation as the information that contradicts the best available expertise at the time (Vraga & Bode, 2020). Riddled with decontextualization, pseudoscience, fake news, rumors and conspiracies, social media platforms became the main sources of disseminating misinformation in various societies during the pandemic (Brennen et al., 2021; Jamieson & Albarracín, 2020; Li et al., 2020; Pulido et al., 2020). Analyzing 30.80 million tweets further revealed four primary themes on Twitter: political bias, reliability, conspiracy, and clickbait (Sharma et al., 2020).
Empirical studies often measure misinformation by asking informants if they believe the statements on false information about the virus and preventative measures (e.g., Jolley & Paterson, 2020; Romer & Jamieson, 2020; Roozenbeek et al., 2020). Research has revealed that conspiracy beliefs and susceptibility to rumors are contributing factors to low intensions of vaccination in many societies. For example, Roozenbeek et al. (2020) demonstrated that, after controlling demographic features and political ideology, increased susceptibility to misinformation reduced people's vaccine intention in the USA, the UK, Ireland, Mexico and Spain. Romer and Jamieson (2020) found that conspiracy believers were less likely to take the MMR vaccine because they were more likely to believe the MMR vaccine was harmful. In the U.K., three studies also found a negative association between COVID-19 conspiracy beliefs and COVID-19 health-protective behaviours (Allington et al., 2020). However, existing studies on vaccine hesitancy mostly reported vaccine intention. As the vaccine availability has increased, this study thus aims to extend the investigation of the impacts of the infodemic to vaccine uptake as well.
2.2. Fundamental cause theory and contextualized impacts of the infodemic
When explaining how health disparity emerges and persists over time, fundamental cause theory (FCT) argues that those with higher socioeconomic status (SES), both individually and collectively, “avoid risks and adopt protective strategies using flexible resources: knowledge, money, power, prestige, and beneficial social connections” (Clouston & Link, 2021; Link & Phelan, 1995; Phelan et al., 2010). FCT research has long focused on vaccine deployment (Clouston et al., 2014; Polonijo & Carpiano, 2013). In the case of COVID-19, studies indicate that global inequalities emerge as wealthy countries and individuals have more access to vaccines (Painter et al., 2021). However, as information and knowledge also serve as “a mechanism for disparities” (Clouston et al., 2016), the effects of the infodemic on vaccination uptake have not been fully examined in the context of COVID-19.
Existing studies also reveal two countervailing processes that lead to paradoxical results from a FCT vantage point: choice constraints and competitive valuations (Clouston & Link, 2021). The choice constraint hypothesis argues that social contexts functioning at multiple levels affect individuals’ health choices in varying degrees, ranging from family, social communities, policies and institutions (e.g., Assari, 2018; Bird & Rieker, 2008). The competitive valuation process suggests that people might value other ends more than health. There is evidence that health concerns can be overridden by competing values of importance to an individual (e.g., Christy et al., 2014; Courtenay, 2000; Rothgerber, 2013). During the pandemic, these two processes may suggest that the impact of the infodemic on vaccine hesitancy could be moderated by socioeconomic status and cultural orientations.
2.2.1. The impact of structural factor: SES as choice constraints
The complexity of COVID-19 information (e.g., contains much scientific jargon) contributes to information turbulence as processing COVID-19 information requires great cognitive resources. Previous studies have shown that older adults (Chan & Huang, 2013) and females (Ji et al., 2014; Lagoe & Atkin, 2015; York, 2013) experienced greater information overload. Also, those who are less educated (Chae et al., 2016; Chan & Huang, 2013; Obamiro & Leek, 2019) and of lower SES (Jiang & Beaudoin, 2016; Kim et al. 2007) were more prone to feel overburdened by information. Previous studies also show that the elderly, minorities and those with a lower social status were more susceptible to fake news and conspiracy theories (Goertzel, 1994; Grinberg et al., 2019; Van Prooijen, 2017). Even though individuals could have developed skills and strategies to cope with the overabundance of true and false information (Hargittai et al., 2012; Mercier, 2020; Neuman, 2016), people with lower levels of education are less capable of developing skills and strategies to buffer against infodemic (Georgiou et al., 2019; Swami & Furnham, 2012; Van Prooijen, 2017). Thus, following this line of logic, it seems reasonable to speculate that the impact of an infodemic might be stronger for individuals in lower SES group as they might have less resources to buffer against it.
However, as the COVID-19 pandemic is the first social media infodemic (Hao & Basu, 2020), the younger, the better-educated and those in higher SES are more capable to adapt to the social media communication. A study across six societies in Asia revealed that respondents who were younger, and with higher socioeconomic status were not only more likely to feel COVID-19 information overload but also experienced stronger impacts of information overload on their psychological distress (Chen et al., 2022). If following this line of logic, it might also be plausible that the impacts of the infodemic on vaccination might be stronger among those high SES groups.
2.2.2. The impact of cultural orientation: competitive valuations
Culture is essential to understand the variations of health behaviors across groups (Kreuter & McClure, 2004; Pasick et al., 1996). During a crisis, individuals tend to form risk perceptions that are in line with their values and such “cultural cognition of risk” shapes the way individuals process and manage information (Kahan, 2008). Even though health is a substantial outcome, individuals might ignore the implications of risky behaviours to maintain or achieve the shared value. Hence, a relatively stable set of values and practices in a community could not only link to a group's health decisions and behaviours (Dutta, 2007; Kreuter & McClure, 2004; Pasick et al., 1996), and but also moderate how an infodemic shapes health-related behaviour.
The cultural orientation in the spectrum of individualism-collectivism is highly relevant in the context of the COVID-19 pandemic. “Individualism pertains to societies in which the ties between individuals are loose: everyone is expected to look after him- or herself and his or her immediate family. Collectivism as its opposite pertains to societies in which people from birth onward are integrated into strong, cohesive in-groups, which throughout people's lifetime continue to protect them in exchange for unquestioning loyalty” (Hofstede et al., 2010, p.92). Many COVID-19 preventative measures, such as mask-wearing, social distancing and vaccination, have simultaneous impacts on individuals, others and the society at large (Yu et al., 2021). Collectivists might be more willing to take preventive actions that require personal sacrifices; while individualists might perceive lockdown polices, the use of contract-tracking devices and mandatory vaccination as a threat to individual freedom and personal rights. Recent studies in U.K. have shown that individuals who have a stronger sense of individualism have lower intention to engage in protective measures, while individuals with a higher sense of collectivism are more likely to adopt these measures (Biddlestone et al., 2020; Schneider et al., 2021). Another survey study in Hong Kong corroborated this pattern: individualism increased vaccination hesitancy by directly or indirectly adjusting perceived personal and societal benefits (Yu et al., 2021). Researchers also found that the inherent cultural difference in individualism/collectivism further contributed to the narrative discrepancy between American and Chinese social media users: Twitter users were more likely to tweet personal vaccination experience while Weibo users rarely discussed their vaccination experience and feelings (Luo et al., 2021).
Another dimension of cultural traits that have been studied during crises concerns how people perceive power and the authorities (Perea & Slater, 1999). People who score high in authoritarian mentality (World Values Survey Association, 2012) have stronger faith in the intentions of the authorities. Authoritarian mentality is “a preference for order and homogeneity and a belief that these outcomes should be achieved by force if necessary” (Ballard-Rosa et al., 2018, p. 1). Classic literature on authoritarianism generally construes such mentality as a multi-dimensional construct in which deterrence to dissenters and reliance on authority and a strong political leader emerge as key characteristics (Adorno et al., 1950; Altemeyer, 1981; Todosijević & Enyedi, 2008). During a crisis, the paternalistic leadership and vertical guidance might better manage individuals who are accustomed to obeying authority and embracing the hierarchy (Aycan, 2006; Gelfand et al., 2007).
During the COVID-19 pandemic, a comparative study on Chinese and American social media users found that Weibo users paid more attention to the WHO and presented more positive sentiments toward the COVID-19 vaccine; while Twitters users adopted more neutral tones in their tweets. Such variation was traced back to the different attitudes towards the authorities in these two cultures (Luo et al., 2021). These findings are consistent with the global survey on vaccination intention: the intention rate was 89% in China, much higher than the 75% in United States of America (Lazarus et al., 2021).
3. Research questions and objectives
Since existing studies on the impacts of infodemic on vaccine hesitancy across SES groups are inconclusive, we thus plan to explore:
RQ1: To what extent do the perceived information overload and vaccine misinformation affect an individual's vaccination willingness and uptake?
There is also no direct empirical evidence of the structural differences of the infodemic's impact on vaccination, thus this study aims to explore:
RQ2: To what extent and how an individual's socioeconomic status can moderate the impacts of the infodemic on his/her vaccination willingness and uptake?
Existing studies mainly focus on how cultural orientations affect protective measures, leaving their moderating effects unexamined. Given that existing studies have shown a negative association between misinformation and vaccination acceptance, and people who hold stronger collectivist and authoritarian mentality have stronger vaccination intention, we thus suspect:
H1: The negative association between infodemic and vaccination uptake might be mitigated by collectivism.
H2: The negative association between infodemic and vaccination uptake might be mitigated by the authoritarian orientation.
4. Data and methods
4.1. Data collection
We conducted a cross-national online survey of public attitudes and responses toward the COVID-19 pandemic in six societies including Hong Kong, Japan, South Korea, Singapore, the UK, and the US between June 15 and June 30, 2021. As detailed in the supplemented materials, the surveys used online panels provided by a globally-renowned data company whose panels contained an opt-in list of 56,000 to 2,350,000 individuals relative to the population size in these jurisdictions. The survey targeted residents aged 18 or above and adopted a quota sampling strategy to ensure that the selected samples match the population's geographical and demographic characteristics released by the latest available census in each jurisdiction. The questionnaire was available in English, Chinese, Korean, Japanese for participants from different jurisdictions. A total number of 6764 representative respondents were collected, with approximately 1,100 individuals in each jurisdiction. Responses with incomplete information were deleted (n = 730) and therefore the final sample size was 6034. Ethical approval was obtained from the Human Subject Ethics Committee of the City University of Hong Kong (Ref No: 8-2020-04-E295-18). All necessary participant consent was obtained.
4.2. Measures
Vaccine hesitancy was assessed by both willingness to accept COVID-19 vaccines and actual vaccination behaviour. Willingness to be vaccinated was measured by the question: “A few vaccines are developed to prevent coronavirus; would you accept it for yourself? The response ranged from 1 = “Definitely no” to 7 = “Definitely yes”, with a higher value indicating a higher level of vaccine willingness. Participants were also asked whether they had received the COVID-19 vaccine (at least one jab) at the time of the survey (yes/no).
Exposure to COVID-19 infodemic was assessed by two dimensions: (1) perceived information overload about COVID-19 vaccines and (2) belief in misinformation. The measure of perceived information overload was adapted from Farooq et al. (2020) which included two items: “I receive too much information regarding COVID-19 vaccine to form a coherent picture of what is happening in the past four weeks;” and “I am often distracted by the excessive amount of information and news on multiple sources about COVID-19 vaccine.” The responses ranged from 1= “Strongly disagree” to 7 = “Strongly agree.” The scores of the three items were averaged, with higher values representing a higher level of perceived information overload.
Susceptibility to misinformation was gauged by asking the participants to rate on a 7-Likert scale whether they agreed with the following statements about COVID-19 vaccines: (1) “The real purpose of a mass vaccination program against COVID-19 is to track and control the population.” (2) “The COVID‐19 vaccine will alter human DNA.” and (3) “The only reason the COVID-19 vaccine is being developed is to make money for pharmaceutical companies.” (1= “Strongly disagree” to 7 = “Strongly agree”) These statements were widespread false claims about the COVID-19 vaccines (The Policy Institute, 2020). The mean score of the three items was calculated to represent the level of belief in COVID-19 vaccine misinformation, with higher values indicating belief in more vaccine misinformation (pooled data: alpha = 0.85; alpha in individual regions: 0.82 - 0.93; details shown in the supplemental materials).
Collectivism was measured with a six-item subscale of collectivism-individualism from Hofstede's cultural dimension (Hofstede,1983,1984; Hofstede et al., 2010). Participants were asked to rate on a 7-point scale their agreement with the following statements (1 = “Strongly disagree” to 7 = “Strongly agree”): (1) Individuals should sacrifice self-interest for the group; (2) Individuals should stick with the group even through difficulties; (3) Group welfare is more important than individual rewards; (4) Group success is more important than individual success; (5) Individuals should only pursue their goals after considering the welfare of the group; and (6) Group loyalty should be encouraged even if individual goals suffer. A composite score of “collectivism” was created by averaging the six items (pooled data: alpha = 0.91; alpha in individual regions: 0.88-0.92).
Authoritarian mentality was assessed by participants’ level of agreement with four statements about political governance preference adapted from the World Values Survey (World Values Survey Association, 2012), so that higher values indicate higher levels of identification with authoritarianism. Sample questions included “A government shall be led by a political strongman” and “A government led by elites is more effective in governance than a government led by public opinions.” (Pooled data: alpha = 0.69; alpha in individual region: 0.62 – 0.77)
We included a series of socioeconomic factors, including education (secondary school or below, college or above, or unknown), income (from lowest to highest quartile), and rural/urban residence.
In all regression models, we adjusted for additional sociodemographic variables, such as age (18-29, 30-59, ≥60), sex (male vs. female), industry (professional/service vs. manual labor/ other), and jurisdiction; health status (with or without chronic diseases); and whether living with vulnerable population (pregnant women or elderly aged over 65). We further controlled for institutional trust in the government and in public health departments (1 = “Totally do not trust” to 7 = “Totally trust”), information-seeking behavior (assessed by the frequency of accessing COVID-19 information from social media;1 = “Never” to 7 = “Very frequently”), and conspiracy mentality that was assessed by a validated five-item scale of general conspiracy mentality thinking (Bruder et al., 2013). Since the willingness to be vaccinated could be related to the severity of the pandemic in a given jurisdiction, we also included a set of dummy variables to control jurisdiction.
4.3. Data handling and analysis
Descriptive statistics were used to characterize the study population. We ran OLS regression models to investigate which subpopulations were more susceptible to infodemic during the pandemic. We then used OLS and logistic regression models to examine the effects of perceived information overload and misinformation on vaccine willingness (continuous) and vaccine uptake (binary), after adjusting for various background variables. Lastly, two-way interaction terms were computed between perceived information overload/belief in misinformation and each SES and culture measurements. The variance inflation factor for each of the predictors was well below 10 (ranged from 1.04 to 2.98); suggesting no extreme interrelations between covariates. All the analyses were performed using Stata 16.0. Unstandardized coefficients with 95% confidence intervals were reported. A p value of 0.05 was set as the level of statistical significance.
5. Results
5.1. Sample characteristics
The sample characteristics are displayed in Table 1 . There were slightly more females (50.1%) than males (49.9%). About one-fifth of participants were aged between 18 and 29 (21.7%) and 60 or older (22.8%); the remaining 55.5% were aged between 30 and 59. About 22.0% of participants had secondary education or below and nearly 46% of participants received tertiary education or above; the remainder did not disclose their educational level. A majority of respondents lived in urban areas (79.6%) and worked in the professional and service industry (65.6%). About 16.4% of participants had a chronic illness. More than one in five (21.5%) participants resided with elderly (aged over 65) or pregnant women who were relatively vulnerable during the COVID-19 pandemic.
Table 1.
Descriptive statistics.
| Variable | Variable | ||||
|---|---|---|---|---|---|
| Sociodemographics | Living with vulnerable populations, N (%) | ||||
| Age, N (%) | No | 4706 | (78.0%) | ||
| 18-29 | 1308 | (21.7%) | Yes | 1298 | (21.5%) |
| 30-59 | 3351 | (55.5%) | Unknown | 30 | (0.5%) |
| >=60 | 1375 | (22.8%) | Jurisdiction, N (%) | ||
| Sex, N (%) | Hong Kong | 1013 | (16.8%) | ||
| Male | 3011 | (49.9%) | Japan | 997 | (16.5%) |
| Female | 3023 | (50.1%) | Singapore | 1077 | (17.8%) |
| Education, N (%) | South Korea | 1054 | (17.5%) | ||
| Secondary or below | 1325 | (22.0%) | UK | 954 | (15.8%) |
| Tertiary or above | 2757 | (45.7%) | US | 939 | (15.6%) |
| Unknown/refuse to disclose | 1952 | (32.3%) | Dependent variables | ||
| Income, N (%) | Vaccine willingness, Mean (SD) | 5.56 | (1.72) | ||
| Lowest quartile | 1474 | (24.4%) | Vaccine uptake, N (%) | ||
| 2nd quartile | 1496 | (24.8%) | Yes | 2868 | (47.5%) |
| 3rd quartile | 1819 | (30.2%) | No | 3166 | (52.5) |
| Highest quartile | 926 | (15.5%) | Independent variables | ||
| Unknown/refuse to disclose | 309 | (5.1%) | Perceived information overload, Mean (SD) | 4.18 | (1.49) |
| Area, N (%) | Misinformation, Mean (SD) | 3.67 | (1.66) | ||
| Urban | 4803 | (79.6%) | Cultural variables | ||
| Rural | 1231 | (20.4%) | Collectivism, Mean (SD) | 4.57 | (1.18) |
| Industry, N (%) | Authoritarianism, Mean (SD) | 4.25 | (1.19) | ||
| Manufacture/other | 3956 | (65.6%) | Other covariates | ||
| Professional/service | 2078 | (34.4%) | Social media use, Mean (SD) | 4.43 | (1.96) |
| Chronic diseases, N (%) | Social media use, Mean (SD) | 4.43 | (1.96) | ||
| No | 4927 | (81.7%) | Trust in government, median (IQR) | 5 | (3-6) |
| Yes | 987 | (16.4%) | Trust in public health, median (IQR) | 5 | (4-6) |
| Unknown/refuse to disclose | 120 | (2.0%) | Conspiracy mentality, Mean (SD) | 4.85 | (1.06) |
5.2. Descriptive statistics of key covariates
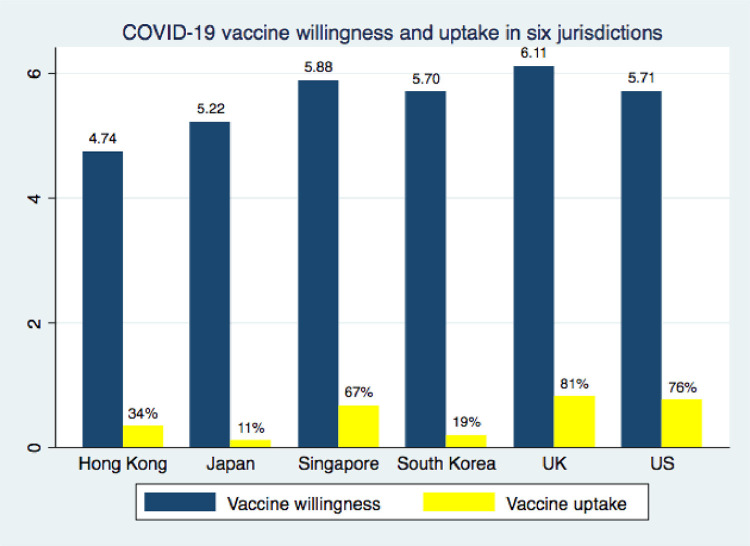
Overall, the participants reported a high level of vaccine willingness (M = 5.56, SD = 1.72). Nearly half of the participants (47.5%) had received at least one jab of the COVID-19 vaccines. The mean scores of vaccine willingness and rate of vaccine uptake in each jurisdiction were presented in Fig. 1 . The level of vaccine acceptance was highest in the UK (M = 6.11) and lowest in Hong Kong (M = 4.74), with Singapore (M = 5.88), the US (M = 5.71), and South Korea (M = 5.70) in between. Similarly, the rate of vaccine uptake was higher in the UK (81%) and US (76%), followed by Singapore (67%), Hong Kong (34%), South Korea (19%), and Japan (11%).
Fig. 1.
COVID-19 vaccine willingness and uptake in six jurisdictions.
The mean of perceived information overload was 4.18 (SD = 1.49). Specifically, about 41.4% of respondents agreed (somewhat agree/agree/strongly agree) that they had been receiving too much information regarding COVID-19 vaccines and about 46.0% agreed that they were often distracted by the excessive amount of information regarding COVID-19 vaccines. Also, belief in COVID-19-vaccine-related misinformation was prevalent (Mean = 3.67; SD =1.66). More than one in three participants thought that the real purpose of a mass vaccination program against COVID-19 is to track and control the population (35.9%), believed that the COVID‐19 vaccine would alter human DNA (33.1%), and agreed that the only reason the COVID-19 vaccine was being developed was to make money for pharmaceutical companies (34.0%). As for cultural variables, the mean of collectivism and authoritarianism were 4.57 (SD = 1.18) and 4.25 (SD = 1.19), respectively.
5.3. Who were more susceptible to COVID-19 infodemic?
Table 2 displays the results of the associations between sociodemographic variables and two aspects of infodemic, i.e., perceived information overload and belief in misinformation. The results showed that participants who were older (vs. those aged 18−29) and had college education (vs. those with secondary education) were less likely to experience perceived information overload during the pandemic and less likely to believe in misinformation about COVID-19 vaccines. Besides, females, and people with higher income were less likely to believe in vaccine misinformation.
Table 2.
Associations between sociodemographic variables and COVID-19 infodemic.
| Perceived information overload | Belief in vaccine misinformation | |||
|---|---|---|---|---|
| b | [95% CI] | b | [95% CI] | |
| Age | ||||
| 18−29 | Ref | Ref | ||
| 30−59 | -0.28⁎⁎⁎ | [-0.37,-0.19] | -0.32⁎⁎⁎ | [-0.42,-0.22] |
| >=60 | -0.85⁎⁎⁎ | [-0.96,-0.74] | -1.09⁎⁎⁎ | [-1.21,-0.96] |
| Sex | ||||
| Male | Ref | Ref | ||
| Female | -0.06 | [-0.13,0.02] | -0.16⁎⁎⁎ | [-0.25,-0.08] |
| Education | ||||
| Secondary or below | Ref | Ref | ||
| Tertiary or above | -0.13* | [-0.23,-0.03] | -0.31⁎⁎⁎ | [-0.42,-0.20] |
| Unknown | 0.18⁎⁎ | [0.07,0.29] | 0.09 | [-0.03,0.22] |
| Income | ||||
| Lowest quartile | Ref | Ref | ||
| 2nd quartile | -0.01 | [-0.11,0.10] | -0.10 | [-0.22,0.01] |
| 3rd quartile | -0.04 | [-0.14,0.06] | -0.22⁎⁎⁎ | [-0.33,-0.10] |
| Highest quartile | -0.00 | [-0.12,0.12] | -0.09 | [-0.23,0.04] |
| Unknown | -0.13 | [-0.31,0.05] | -0.12 | [-0.32,0.08] |
| Area | ||||
| Urban | Ref | Ref | ||
| Rural | 0.03 | [-0.06,0.13] | -0.03 | [-0.14,0.08] |
| Industry | ||||
| Manufacture/other | Ref | Ref | ||
| Professional/service | 0.25⁎⁎⁎ | [0.16,0.33] | 0.28⁎⁎⁎ | [0.18,0.37] |
| Chronic diseases | ||||
| No | Ref | Ref | ||
| Yes | 0.27⁎⁎⁎ | [0.17,0.37] | 0.23⁎⁎⁎ | [0.12,0.34] |
| Unknown | 0.14 | [-0.13,0.41] | 0.19 | [-0.11,0.49] |
| Living with vulnerable populations | ||||
| No | Ref | Ref | ||
| Yes | -0.02 | [-0.11,0.08] | -0.05 | [-0.15,0.05] |
| Unknown | -0.07 | [-0.59,0.46] | -0.21 | [-0.79,0.37] |
| Jurisdiction | ||||
| Hong Kong | Ref | Ref | ||
| Japan | 0.22⁎⁎ | [0.08,0.35] | -0.03 | [-0.18,0.11] |
| Singapore | 0.26⁎⁎⁎ | [0.13,0.39] | -0.13 | [-0.27,0.01] |
| South Korea | 0.29⁎⁎⁎ | [0.16,0.42] | -0.42⁎⁎⁎ | [-0.56,-0.28] |
| UK | 0.07 | [-0.07,0.21] | -0.64⁎⁎⁎ | [-0.79,-0.49] |
| US | 0.13 | [-0.01,0.27] | -0.19* | [-0.34,-0.04] |
CI = confidence intervals
p < 0.05
p < 0.01
p < 0.001
5.4. Impact of infodemic on vaccine acceptance/uptake
Table 3 presented the effect of perceived information overload and belief in vaccine misinformation on vaccine willingness and uptake, after adjusting for sociodemographic variables, information seeking behaviour, institutional trust, and cultural variables. Model 1 revealed a positive effect of perceived information overload (b = 0.09, 95% CI = [0.06,0.12], p < 0.001) and a negative effect of vaccine misinformation (b = -0.32, 95% CI = [-0.35, -0.29], p < 0.001) on willingness to accept COVID-19 vaccines. Similarly, participants who believe vaccine misinformation to be true were less likely to receive COVID-19 vaccines (b = -0.19, 95% CI = [-0.25, -0.14], p < 0.001). Perceived information overload was not significantly associated with vaccine uptake. Besides, when other conditions are equal, collectivism and authoritarian values were positively associated with COVID-19 vaccine willingness and uptake.
Table 3.
Associations between infodemic and vaccine acceptance and uptake.
| Vaccine willingness | Vaccine uptake | |||
|---|---|---|---|---|
| b | [95% CI] | b | [95% CI] | |
| Information overload (IO) | 0.09⁎⁎⁎ | [0.06,0.12] | 0.05 | [-0.00,0.11] |
| Misinformation (MI) | -0.32⁎⁎⁎ | [-0.35,-0.29] | -0.19⁎⁎⁎ | [-0.25,-0.14] |
| Collectivism | 0.29⁎⁎⁎ | [0.25,0.33] | 0.28⁎⁎⁎ | [0.21,0.35] |
| Authority | 0.08⁎⁎⁎ | [0.04,0.12] | 0.10* | [0.02,0.18] |
| Seeking COVID-19 information from social media | 0.02 | [-0.01,0.04] | -0.04 | [-0.08,0.00] |
| Trust in government | 0.15⁎⁎⁎ | [0.12,0.18] | 0.09⁎⁎ | [0.03,0.15] |
| Trust in public health | 0.15⁎⁎⁎ | [0.12,0.19] | 0.11⁎⁎ | [0.04,0.18] |
Note: The models adjusted for sociodemographic variables, including age, sex, education, income, rural/urban area, industry, chronic diseases, living the vulnerable populations, and jurisdiction.
CI = confidence intervals
p < 0.05
p < 0.01
p < 0.001
5.5. Socioeconomic and cultural differences in the effects of infodemic
Next, we assessed whether the impacts of the COVID-19 infodemic on vaccine outcomes varied by different socioeconomic status and cultural orientations. A series of two-way interaction terms between two aspects of infodemic (i.e., perceived information overload and belief in vaccine misinformation) and each of these SES variable (i.e., education, income, and urban/rural residence) and cultural variables (i.e., collectivism and authoritarian mentality) were computed and included in the regression models.
Table 4 presents the results of vaccine willingness on interactions between infodemic and SES and cultural factors, after controlling for background variables. A significant and positive interaction term between tertiary education and belief in vaccine misinformation emerged (Model 1a; b = 0.11, 95% CI = [0.04,0.17], p < 0.01), suggesting that higher education may attenuate the negative effect of vaccine misinformation on vaccine acceptance. Similarly, the interactions between vaccine misinformation and higher income (Model 2a; 3rd quartile: b = 0.09, 95% CI = [0.02,0.16], p < 0.01; highest quartile: b = 0.09, 95% CI = [0.01,0.18], p < 0.05), as well as the interaction between misinformation and urban residence (Model 3a; b = 0.10, 95% CI = [0.04,0.17], p < 0.01) were significant. These results suggested that the association between belief in vaccine misinformation and vaccine willingness was weaker among professionals, urban residents, and individuals with higher income than their counterparts. In other words, higher SES may buffer the adverse effect of vaccine misinformation on willingness to take COVID-19 vaccines.
Table 4.
Moderating effect of sociodemographic and cultural variables on the relationship between infodemic and vaccination willingnes
| Model 1a | Model 2a | Model 3a | ||||||
|---|---|---|---|---|---|---|---|---|
| b | [95% CI] | b | [95% CI] | b | [95% CI] | |||
| IO | 0.13⁎⁎⁎ | [0.06,0.19] | IO | 0.13⁎⁎⁎ | [0.07,0.19] | IO | 0.13⁎⁎⁎ | [0.07,0.19] |
| MI | -0.42⁎⁎⁎ | [-0.47,-0.36] | MI | -0.39⁎⁎⁎ | [-0.45,-0.34] | MI | -0.42⁎⁎⁎ | [-0.47,-0.36] |
| Education (ref: ≤Secondary education) | Income (ref: Lowest quartile) | Area (ref: Urban) | ||||||
| ≥ Tertiary education | 0.01 | [-0.29,0.30] | 2nd quartile | 0.07 | [-0.26,0.40] | Urban | -0.08 | [-0.36,0.19] |
| Unknown education | -0.14 | [-0.44,0.17] | 3rd quartile | 0.14 | [-0.17,0.45] | IO × Rural | -0.06 | [-0.13,0.01] |
| IO × ≥ Tertiary education | -0.06 | [-0.13,0.02] | Highest quartile | 0.15 | [-0.20,0.50] | MI × Rural | 0.10⁎⁎ | [0.04,0.17] |
| IO × ≥ Unknown education | -0.03 | [-0.11,0.06] | Unknown | 0.21 | [-0.40,0.83] | |||
| MI × ≥ Tertiary education | 0.11⁎⁎ | [0.04,0.17] | IO × 2nd quartile | -0.04 | [-0.13,0.04] | |||
| MI × ≥ Unknown education | 0.10⁎⁎ | [0.03,0.18] | IO × 3rd quartile | -0.07 | [-0.14,0.01] | |||
| IO ×Highest quartile | -0.06 | [-0.15,0.04] | ||||||
| IO × Unknown | -0.06 | [-0.20,0.08] | ||||||
| MI × 2nd quartile | 0.07 | [-0.01,0.14] | ||||||
| MI × 3rd quartile | 0.09⁎⁎ | [0.02,0.16] | ||||||
| MI ×Highest quartile | 0.09* | [0.01,0.18] | ||||||
| MI × Unknown | 0.04 | [-0.09,0.16] | ||||||
| Model 4a | Model 5a | |||||||
| b | [95% CI] | b | [95% CI] | |||||
| IO | 0.15⁎⁎ | [0.05,0.25] | IO | 0.02 | [-0.08,0.12] | |||
| MI | -0.85⁎⁎⁎ | [-0.95,-0.76] | MI | -0.67⁎⁎⁎ | [-0.77,-0.57] | |||
| Collectivism | -0.02 | [-0.11,0.06] | Authoritarianism | -0.25⁎⁎⁎ | [-0.34,-0.16] | |||
| IO × Collectivism | -0.02 | [-0.04,0.01] | IO × Authoritarianism | 0.02 | [-0.01,0.04] | |||
| MI × Collectivism | 0.11⁎⁎⁎ | [0.09,0.13] | MI × Authoritarianism | 0.08⁎⁎⁎ | [0.05,0.10] | |||
Note: The models adjusted for sociodemographic variables, including age, sex, education, income, rural/urban area, industry, chronic diseases, living the vulnerable populations, and jurisdiction.
IO = perceived information overload; MI = belief in misinformation; CI = confidence intervals
p < 0.05
p < 0.01
p < 0.001
As for the moderating effect of cultural variables, we found significant interactive effects between belief in vaccine misinformation with collectivism (Model 4a; b = 0.11, 95% CI = [0.09,0.13], p < 0.001) and authoritarian mentality (Model 5a; b = 0.08, 95% CI = [0.05,0.10], p < 0.001) on vaccine willingness. Specifically, participants identified with higher levels of collectivism and authoritarian orientation were more likely to accept COVID-19 vaccines when believing misinformation about COVID-19 vaccines, compared to those with lower levels of collectivism and authoritarian mentality. Thus, the results confirmed the buffering effect of collectivism and authoritarian orientation on the relationship between vaccine misinformation and vaccine willingness. In addition, there were no significant interactions between perceived information overload and SES/cultural factors, suggesting that the effect of perceived information overload on vaccine willingness was not conditional on either SES or cultural factors.
The interactive effects between infodemic and ssocioeconomic and cultural variables on vaccine uptake are shown in Table 5 . Similar to the results of vaccine acceptance, the effect of misinformation on vaccine uptake were weaker among individuals with higher SES, such as those with higher education (Model 1b; b = 0.20, 95%CI = [0.07,0.33], p < 0.01) and higher income quartiles (Model 2b; 3rd quartile: b = 0.16, 95% CI = [0.03,0.29], p < 0.05; highest quartile: b = 0.21, 95% CI = [0.05,0.36], p < 0.01). Also, collectivism (Model 4b; b = 0.07, 95% CI = [0.03,0.11], p < 0.01) and authoritarian mentality (Model 5b; b = 0.05, 95% CI =[0.01,0.09], p < 0.01) tended to diminish the negative impact of belief in vaccine misinformation on vaccine uptake.
Table 5.
Moderating effect of sociodemographic and cultural variables on the relationship between infodemic and vaccination uptake
| Model 1b | Model 2b | Model 3b | ||||||
|---|---|---|---|---|---|---|---|---|
| b | [95% CI] | b | [95% CI] | b | [95% CI] | |||
| IO | 0.09 | [-0.02,0.21] | IO | 0.13* | [0.02,0.23] | IO | 0.08 | [-0.04,0.20] |
| MI | -0.32⁎⁎⁎ | [-0.43,-0.21] | MI | -0.28⁎⁎⁎ | [-0.38,-0.18] | MI | -0.26⁎⁎⁎ | [-0.38,-0.15] |
| Education (ref: ≤Secondary education) | Income (ref: Lowest quartile) | Area (ref: Urban) | ||||||
| ≥ Tertiary education | -0.32 | [-0.87,0.23] | 2nd quartile | 0.33 | [-0.28,0.93] | Urban | -0.17 | [-0.71,0.37] |
| Unknown education | 0.09 | [-0.49,0.67] | 3rd quartile | 0.09 | [-0.49,0.66] | IO × Rural | -0.04 | [-0.17,0.10] |
| IO × ≥ Tertiary education | -0.05 | [-0.19,0.10] | Highest quartile | 0.32 | [-0.33,0.98] | MI × Rural | 0.09 | [-0.03,0.21] |
| IO × ≥ Unknown education | -0.06 | [-0.21,0.09] | Unknown | -0.13 | [-1.33,1.07] | |||
| MI × ≥ Tertiary education | 0.20⁎⁎ | [0.07,0.33] | IO × 2nd quartile | -0.05 | [-0.20,0.11] | |||
| MI × ≥ Unknown education | 0.13 | [-0.01,0.27] | IO × 3rd quartile | -0.11 | [-0.25,0.04] | |||
| IO ×Highest quartile | -0.19 | [-0.37,0.00] | ||||||
| IO × Unknown | -0.07 | [-0.35,0.20] | ||||||
| MI × 2nd quartile | 0.01 | [-0.13,0.15] | ||||||
| MI × 3rd quartile | 0.16* | [0.03,0.29] | ||||||
| MI ×Highest quartile | 0.21⁎⁎ | [0.05,0.36] | ||||||
| MI × Unknown | 0.20 | [-0.04,0.45] | ||||||
| Model 4b | Model 5b | |||||||
| b | [95% CI] | b | [95% CI] | |||||
| IO | 0.02 | [-0.18,0.21] | IO | 0.00 | [-0.19,0.19] | |||
| MI | -0.50⁎⁎⁎ | [-0.69,-0.31] | MI | -0.41⁎⁎⁎ | [-0.59,-0.22] | |||
| Collectivism | 0.03 | [-0.14,0.19] | Authoritarianism | -0.12 | [-0.30,0.05] | |||
| IO × Collectivism | 0.01 | [-0.04,0.05] | IO × Authoritarianism | 0.01 | [-0.03,0.06] | |||
| MI × Collectivism | 0.07⁎⁎ | [0.03,0.11] | MI × Authoritarianism | 0.05* | [0.01,0.09] | |||
Note: The models adjusted for sociodemographic variables, including age, sex, education, income, rural/urban area, industry, chronic diseases, living the vulnerable populations, and jurisdiction.
IO = perceived information overload; MI = belief in misinformation; CI = confidence intervals
p < 0.05
p < 0.01
p < 0.001
6. Discussion and conclusion
This study proposes a contextualized impact model to examine how the impacts of perceived information overload and misinformation on vaccine hesitancy are moderated by structural and cultural factors. Extending the fundamental cause theory, our study emphasizes the importance of information that functions as a “mechanism of disparity” in shaping health decisions and outcomes. On the one hand, the findings showed that the fundamental cause for health inequality remains unfortunately robust during the pandemic, as the systematic relationships between SES-related resources and health decisions results (vaccine hesitancy) has been reproduced across different societies. On the other hand, our findings also presented evidence to support the argument that cultural values would shape individuals’ health choices, which suggests long-term potential strategies of the global recovery. In this sense, our findings add nuanced mechanisms not only to understand how a system of relationship could be reproduced over time and across societies, but also to explore the possibility to modify such reproduction of inequality and disparity.
6.1. On defining infodemic
Our study first differentiates two different types of infodemic: information overload and misinformation. Our findings suggest that these two types of infodemic function through different mechanisms to shape individuals’ preventative measures during the pandemic. When holding an individual's belief in vaccine misinformation equal, perceived information overload actually increases the individual's vaccine willingness. Existing studies have shown that perceived information overload increases individuals’ psychological distress (Chen et al., 2022). Worried and stressed people might perceive the pandemic as threatening and thus are more likely to take protective measures. However, misinformation functions on the opposite direction: misinformation significantly decreases individuals’ vaccine intention. People who believe in conspiracy theories tend to think that vaccines are harmful (e.g., Allington et al., 2020), and doubt their effectiveness, thus have lower vaccine acceptance and update.
It is worth noticing that more often the term “infodemic” is used loosely as a metaphor in many journalistic, political and scholarly discussion (Simon & Camargo, 2021). By comparing the information-sharing with virus-spreading during the pandemic, such analogy might misleadingly oversimplify the complex mechanism of information processing when the intention, the sources and consequences of information-spreading are not well investigated (Simon & Camargo, 2021). This study is a humble effort to unpack “infodemic” and to explore different, even competing information processing mechanisms involved in the “infodemic”. Further empirical studies might engage in more nuanced scrutinization of information processing mechanisms during a crisis.
6.2. Implications for global recovery
The findings of this study have implications on global recovery amidst the uncertainties and impacts associated with the COVID-19 pandemic. Following the peaks of the Omicron variant, many countries have begun to move beyond restrictive policies and adopt protective measures (Edwards et al., 2021; Petherick et al., 2021). However, the effectiveness of policy interventions, as revealed in our findings, is often associated with stratified information gaps across socioeconomic groups, and is moderated by cultural factors such as collectivism and authoritarian mentality. These factors can buffer against vaccine hesitancy in certain cultures and socio-economic groups, but are likely to induce more resistance in others. To manage pandemic fatigue while mitigating the pressure on medical systems, protective measures that are less costly and less disruptive, such as rapid mass testing and periodic vaccination for the vulnerable, may be easier to adopt and to be adapted.
Moreover, the levels of compliance with protective measures are highly contingent on information management and dissemination. To reduce pandemic fatigue over regulative measures, policymakers need to work closely with trusted and influential partners to transmit targeted and accurate information. Great efforts have been spent on fact-checking which is crucial. The WHO has assembled a team of “myth busters” to work with social media giants such as Facebook, Twitter, Tencent and Tiktok and to routinely correct false information and debunk the myths surrounding the pandemic (WHO, 2022). Although such reactive responses are important, research suggests the persuasiveness of information correction is limited (Lewandowsky et al., 2012). Thus, these measures are necessary but insufficient in battling misinformation (Chou et al., 2021). Our findings suggest that, besides fact-checking and improving individual information literacy, effective information and health intervention policies shall also address the impacts of social structures, culture and media environments. Successful cooperation between scientific experts and the tech giants managing social media platforms may help to battle misinformation and make the recovery sustainable.
Our findings further recommend stratified strategies to achieve the global recovery. The socially disadvantaged groups might suffer more from the infodemic once they are “infected” by it. As the lower SES groups have less capacity to handle misinformation (Georgiou et al., 2019; Swami & Furnham, 2012; Van Prooijen, 2017), conspiracy theories might become a rational coping strategy to understand their structural disadvantage in the chaos (Van Prooijen & Douglas, 2017). Since the pandemic, the world has become digitalized at an accelerating speed. It is likely that the enlarging digital and information divide will be translated into further health disparities in the post-pandemic society. Thus, to achieve “recovery equity”, our findings call for an urgent attention to the structural gaps embedded in interventions and information policies.
Our findings also suggest the importance of contextualizing the health communication in different cultures in the global fight against the infodemic. During a crisis, culture could be an immediate repertoire of developing coping strategies. Behavioural science advisors in the U.K have proposed to enhance a sense of collectivism in individuals in order to promote appropriate protective behaviours against the COVID-19 pandemic (Scientific Advisory Group for Emergencies, 2020). However, values and worldviews are the core of culture, which is relatively stable and slow to change. Thus, adopted culturalized practices might be more realistic in the shorter term to enhance the effectiveness when communicating health information to different groups (Luo et al. 2021).
In addition, different from previous studies (e.g., Chan & Huang, 2013), our study found that younger groups were more likely to experience the infodemic during the COVID-19 pandemic. Such difference invites further concerns on how to build a responsible digital and media environment as social media is a major source of misinformation (Hao & Basu, 2020). During pandemics before the social media era, such as the SARS outbreak in 2003, information went through a multi-layered information gatekeeping process involving experts, authorities and journalists before reaching the public. Such mechanisms have been compromised during the COVID-19 pandemic as social media has become the dominant information-releasing and sharing process. This calls for policy and legal regulations to effectively define social media's accountability and construct a responsible digital infrastructure.
6.3. Limitations and future studies
Several limitations of the study merit comment. (1) Even though our measures of both perceived information overload and misinformation were exacted from existing scales and studies, a cross-section survey is still facing the challenge of measuring the evolving nature of the infodemic for at least two reasons. As the COVID-19 virus is newly emerged, the expert consensus is difficult to reach and the evidence is also evolving. As the anti-pandemic measures have often tangled with politics in different societies, the consensus between the experts and authorities might also change at a later stage of the pandemic. Facing such uncertainty, the measurements of perceived information overload and misinformation would vary by time. It is likely the associations that are identified at a single time point of the pandemic might evolve along with the pandemic. In addition, survey studies usually rely on self-reports, rather than objective media logs, to measure the exposure of the infodemic. Thus, well-designed longitudinal studies with more objective measures of the infodemic will be needed and valuable in future studies.
(2) This study has not explained the gap between individuals’ vaccine acceptance and uptake. There are several reasons for the gap between acceptance and uptake. Some might be due to availability of vaccine stockpiles by the time we conducted the survey. Others might be rooted in individuals’ information-sharing process, peer-pressure, or specific vaccine policies in a given society. Even though this study is among the first to link vaccine intention and behavior, it has not gone in depth to explore underlying mechanisms to explain the gap between vaccine intention and behavior, which might deserve further examination.
(3) This study only explores two dimensions of cultural factors: collectivism and authoritarian mentality, leaving many other cultural values unexamined. In addition, the reliability of authoritarian mentality in this study was a little below the frequently cited acceptable level of 0.7, as the Cronbach's alpha for the authoritarian mentality was 0.69 and alpha in individual regions ranged from 0.62 to 0.77. Even though some authors consider 0.6 to 0.7 acceptable for Cronbach's alpha coefficient (DeVellis & Thorpe, 2021; Hair et al., 2006; Loewenthal & Lewis, 2018), the relatively low reliability of authoritarian mentality suggests that this scale in this study might not be unidimensional. In other words, future studies could either explore more cultural values or deepen the analysis on various layers of one cultural orientation.
(4) This study used dummies to control the regional influence, which leaves the mechanisms of regional difference underexamined. Our findings show that when believing in vaccine misinformation, an individual's socioeconomic status plays a more significant role than cultural factors in explaining the variation of vaccine uptake among Asian residents. In contrast, among Western residents, cultural orientation plays a more significant role than socioeconomic status in moderating the effects of infodemic on vaccine uptake. Unfortunately, so far, all these regional differences remain descriptive. In addition, we have not investigated the “collective healthy agency” (Freese & Lutfey, 2011): how the communal pooling of resources shapes regional differences. The collective agency's implications for the global recovery also deserve further investigation.
6.4. Conclusion
By analyzing a cross-national survey of 6034 residents in six societies in Asia, Europe and North America in June 2021, the study finds that the older and highly-educated participants were less susceptible to COVID-19 information overload and belief in vaccine misinformation. The data also reveals that perceived information overload led to an increase in vaccine acceptance and uptake, whereas belief in vaccine misinformation may cause a decrease. In addition, the structural and cultural differentiations of vaccine hesitancy were salient, in which both higher socioeconomic status and cultural orientation towards collectivism and authoritarian mentality can buffer the negative impact of vaccine misinformation on the vaccine willingness and uptake. These findings contribute to nuanced understanding of the fundamental cause theory of health inequality and the discussion on the global recovery from the infodemic.
Author statement
This work was supported by the Research Grants Council of the Hong Kong Special Administrative Region, China (grant no. CityU 11609219), and by the Center for Public Affairs and Law at City University of Hong Kong (project no. 9609002), as well as a Knowledge Transfer Earmarked Fund from Hong Kong University Grants Commission (6354048). Ethical approval was obtained from the Human Subject Ethics Committee of the City University of Hong Kong (Ref No: 8-2020-04-E295-18).
All authors do not have any financial interests and ethical conflicts influencing this research. Authors of this article had access to all study data, are responsible for all contents of the article, and had authority over manuscript preparation and the decision to submit the manuscript for publication. All listed authors have approved of the submission of the manuscript to the journal.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ipm.2022.103013.
Appendix. Supplementary materials
References
- Adorno T., Frenkel-Brenswik E., Levinson D.J., Sanford R.N. Harper and Row; 1950. The Authoritarian Personality. [Google Scholar]
- Allington D., Duffy B., Wessely S., Dhavan N., Rubin J. Health-protective behaviour, social media usage and conspiracy belief during the COVID-19 public health emergency. Psychological Medicine. 2021;51(10):1763–1769. doi: 10.1017/S003329172000224X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altemeyer B. University of Manitoba Press; 1981. Right-wing Authoritarianism. [Google Scholar]
- Assari S. Life expectancy gain due to employment status depends on race, gender, education, and their intersections. Journal of Racial and Ethnic Health Disparities. 2018;5(2):375–386. doi: 10.1007/s40615-017-0381-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aycan Z. Indigenous and cultural psychology: Understanding people in context. Kim U., Yang K.-S., Hwang K.-K., editors. Indigenous and cultural psychology: Understanding people in contextSpringer Science + Business Media. 2006:445–466. doi: 10.1007/0-387-28662-4_20. Paternalism: Towards Conceptual Refinement and Operationalization. [DOI] [Google Scholar]
- Ballard-Rosa C., Jensen A., Scheve K. Economic decline, social identity, and authoritarian values in the United States. International Studies Quarterly. 2018;66(1) https://ces.fas.harvard.edu/uploads/files/events/Scheve_for_SC_2018.pdf sqab027. [Google Scholar]
- Bawden D., Robinson L. The dark side of information: overload, anxiety and other paradoxes and pathologies. Journal of Information Science. 2009;35(2):180–191. doi: 10.1177/0165551508095781. [DOI] [Google Scholar]
- Biddlestone M., Green R., Douglas K.M. Cultural orientation, power, belief in conspiracy theories, and intentions to reduce the spread of COVID-19. British Journal of Social Psychology. 2020;59(3):663–673. doi: 10.1111/bjso.12397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird C.E., Rieker P.P. Cambridge University Press; 2008. Gender and Health: The Effects of Constrained Choices and Social Policies. [Google Scholar]
- Brennen J.S., Simon F.M., Nielsen R.K. Beyond (mis) representation: Visuals in COVID-19 misinformation. The International Journal of Press/Politics. 2021;26(1):277–299. doi: 10.1177/1940161220964780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruder M., Haffke P., Neave N., Nouripanah N., Imhoff R. Measuring individual differences in generic beliefs in conspiracy theories across cultures: Conspiracy Mentality Questionnaire. Frontiers in Psychology. 2013;4:225. doi: 10.3389/fpsyg.2013.00225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chae J., Lee C.J., Jensen J.D. Correlates of cancer information overload: Focusing on individual ability and motivation. Health Communication. 2016;31(5):626–634. doi: 10.1080/10410236.2014.986026. [DOI] [PubMed] [Google Scholar]
- Chan Y.M., Huang H. Weight management information overload challenges in 2007 HINTS: Socioeconomic, health status and behaviors correlates. Journal of Consumer Health On the Internet. 2013;17(2):151–167. doi: 10.1080/15398285.2013.780540. [DOI] [Google Scholar]
- Chen X., Lee W., Lin F. Infodemic, Institutional Trust, and COVID-19 Vaccine Hesitancy: A Cross-National Survey. International Journal of Environmental Research and Public Health. 2022;19(13):8033. doi: 10.3390/ijerph19138033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X., Lin F., Cheng E.W. Stratified Impacts of the Infodemic During the COVID-19 Pandemic: Cross-sectional Survey in 6 Asian Jurisdictions. Journal of Medical Internet Research, 2022;24(3):e31088. doi: 10.2196/31088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou W.S., Gaysynsky A., Vanderpool R.C. The COVID-19 misinfodemic: Moving beyond fact-checking. Health Education & Behavior. 2021;48(1):9–13. doi: 10.1177/1090198120980675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choukou, M. A., Sanchez-Ramirez, D. C., Pol, M., Uddin, M., Monnin, C., & Syed-Abdul, S. (2022). COVID-19 infodemic and digital health literacy in vulnerable populations: A scoping review. Digital Health, 8, 10.1177/20552076221076927. [DOI] [PMC free article] [PubMed]
- Christy S.M., Mosher C.E., Rawl S.M. Integrating men's health and masculinity theories to explain colorectal cancer screening behavior. American Journal of Men's Health. 2014;8(1):54–65. doi: 10.1177/1557988313492171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clouston S., Kidman R., Palermo T. Social inequalities in vaccination uptake among children aged 0–59 months living in Madagascar: An analysis of Demographic and Health Survey data from 2008 to 2009. Vaccine. 2014;32(28):3533–3539. doi: 10.1016/j.vaccine.2014.04.030. [DOI] [PubMed] [Google Scholar]
- Clouston S.A., Rubin M.S., Phelan J.C., Link B.G. A social history of disease: Contextualizing the rise and fall of social inequalities in cause-specific mortality. Demography. 2016;53(5):1631–1656. doi: 10.1007/s13524-016-0495-5. [DOI] [PubMed] [Google Scholar]
- Clouston S.A.P., Link B.G. A retrospective on fundamental cause theory: state of the literature and goals for the future. Annual Review of Sociology. 2021;47(1):131–156. doi: 10.1146/annurev-soc-090320-094912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtenay W.H. Constructions of masculinity and their influence on men's well-being: a theory of gender and health. Social Science & Medicine. 2000;50(10):1385–1401. doi: 10.1016/s0277-9536(99)00390-1. [DOI] [PubMed] [Google Scholar]
- Daly M., Robinson E. Willingness to vaccinate against COVID-19 in the US: Representative longitudinal evidence from April to October 2020. American Journal of Preventive Medicine. 2021;60(6):766–773. doi: 10.1016/j.amepre.2021.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeVellis R.F., Thorpe C.T. Sage publications; 2021. Scale development: Theory and applications. [Google Scholar]
- Dutta M.J. Communicating about culture and health: Theorizing culture-centered and cultural sensitivity approaches. Communication Theory. 2007;17(3):304–328. doi: 10.1111/j.1468-2885.2007.00297.x. [DOI] [Google Scholar]
- Edwards B., Biddle N., Gray M., Sollis K. COVID-19 vaccine hesitancy and resistance: Correlates in a nationally representative longitudinal survey of the Australian population. PloS One. 2021;16(3) doi: 10.1371/journal.pone.0248892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farooq A., Laato S., Islam A.N. Impact of online information on self-isolation intention during the COVID-19 pandemic: Cross-sectional study. Journal of Medical Internet Research. 2020;22(5):e19128. doi: 10.2196/19128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freese J., Lutfey K. Springer; New York, NY: 2011. Fundamental causality: Challenges of an animating concept for medical sociology. In Handbook of the sociology of health, illness, and healing; pp. 67–81. [Google Scholar]
- Gelfand M.J., Erez M., Aycan Z. Cross-cultural organizational behavior. Annual Review of Psychology. 2007;58(1):479–514. doi: 10.1146/annurev.psych.58.110405.085559. [DOI] [PubMed] [Google Scholar]
- Georgiou N., Delfabbro P., Balzan R. Conspiracy beliefs in the general population: The importance of psychopathology, cognitive style and educational attainment. Personality and Individual Differences. 2019;151 doi: 10.1016/j.paid.2019.109521. [DOI] [Google Scholar]
- Goertzel T. Belief in conspiracy theories. Political Psychology. 1994:731–742. doi: 10.2307/3791630. [DOI] [Google Scholar]
- Grinberg N., Joseph K., Friedland L., Swire-Thompson B., Lazer D. Fake news on Twitter during the 2016 US presidential election. Science. 2019;363(6425):374–378. doi: 10.1126/science.aau2706. [DOI] [PubMed] [Google Scholar]
- Hair J.F., Black W.C., Babin B.J., Anderson R.E., Tatham R.L. Pearson Prentice Hall Upper Saddle River; 2006. Multivariate data analysis (Vol. 6) [Google Scholar]
- Hao K., Basu T. The coronavirus is the first true social-media infodemic. MTI Technology Review. 2020 https://www.technologyreview.com/2020/02/12/844851/the-coronavirus-is-the-first-true-social-media-infodemic/ [Google Scholar]
- Hargittai E., Neuman W.R., Curry O. Taming the information tide: Perceptions of information overload in the American home. The Information Society. 2012;28(3):161–173. doi: 10.1080/01972243.2012.669450. [DOI] [Google Scholar]
- Hofstede, G. (1983). National cultures in four dimensions: A research-based theory of cultural differences among nations. International Studies of Management & Organization, 13(1-2), 46-74. 10.1080/00208825.1983.11656358. [DOI]
- Hofstede G. Vol. 5. Sage; 1984. (Culture's Consequences: International Differences in Work-related Values). [Google Scholar]
- Hofstede G., Hofstede G.J., Minkov M. 3rd edition. Mcgraw-hill; 2010. Cultures and Organizations: Software of the Mind; p. 9. [Google Scholar]
- Hong H., Kim H.J. Antecedents and consequences of information overload in the COVID-19 pandemic. International Journal of Environmental Research and Public Health. 2020;17(24):9305. doi: 10.3390/ijerph17249305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamieson, K. H., & Albarracin, D. (2020). The relation between media consumption and misinformation at the outset of the SARS-CoV-2 pandemic in the US. The Harvard Kennedy School Misinformation Review, 42(2), 265-277. 10.37016/mr-2020-012. [DOI]
- Jensen J.D., Carcioppolo N., King A.J., Scherr C.L., Jones C.L., Niederdeppe J. The cancer information overload (CIO) scale: Establishing predictive and discriminant validity. Patient Education and Counseling. 2014;94(1):90–96. doi: 10.1016/j.pec.2013.09.016. [DOI] [PubMed] [Google Scholar]
- Ji Q., Ha L., Sypher U. The role of news media use and demographic characteristics in the possibility of information overload prediction. International Journal of Communication. 2014;8:16. [Google Scholar]
- Jiang S., Beaudoin C.E. Health literacy and the internet: An exploratory study on the 2013 HINTS survey. Computers in Human Behavior. 2016;58:240–248. doi: 10.1016/j.chb.2016.01.007. [DOI] [Google Scholar]
- Johnson N.F., Velásquez N., Restrepo N.J., Leahy R., Gabriel N., El Oud S., Zheng M., Manrique P., Wuchty S., Lupu Y. The online competition between pro-and anti-vaccination views. Nature. 2020;582(7811):230–233. doi: 10.1038/s41586-020-2281-1. [DOI] [PubMed] [Google Scholar]
- Jolley D., Paterson J.L. Pylons ablaze: Examining the role of 5G COVID-19 conspiracy beliefs and support for violence. British Journal of Social Psychology. 2020;59(3):628–640. doi: 10.1111/bjso.12394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahan D.M. Handbook of risk theory. Springer; 2008. Cultural cognition as a conception of the cultural theory of risk; pp. 725–759. S. Roeser, R. Hillerbrand, P. Sandin & M. Peterson. [DOI] [Google Scholar]
- Kim K., Lustria M.L.A., Burke D., Kwon N. Predictors of cancer information overload: findings from a national survey. Information Research. 2007;12(4):12–14. [Google Scholar]
- Kreuter M.W., McClure S.M. The role of culture in health communication. Annual Review of Public Health. 2004;25:439–455. doi: 10.1146/annurev.publhealth.25.101802.123000. [DOI] [PubMed] [Google Scholar]
- Lagoe C., Atkin D. Health anxiety in the digital age: An exploration of psychological determinants of online health information seeking. Computers in Human Behavior. 2015;52:484–491. doi: 10.1016/j.chb.2015.06.003. [DOI] [Google Scholar]
- Lazarus J.V., Ratzan S.C., Palayew A., Gostin L.O., Larson H.J., Rabin K., Kimball S., El-Mohandes A. A global survey of potential acceptance of a COVID-19 vaccine. Nature Medicine. 2021;27(2):225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewandowsky S., Ecker U.K., Seifert C.M., Schwarz N., Cook J. Misinformation and its correction: Continued influence and successful debiasing. Psychological Science in the Public Interest. 2012;13(3):106–131. doi: 10.1177/1529100612451018. [DOI] [PubMed] [Google Scholar]
- Link, B. G., & Phelan, J. (1995). Social conditions as fundamental causes of disease. Journal of Health and Social Behavior, 80-94. 10.1177/0022146510383498. [DOI] [PubMed]
- Li H.O., Bailey A., Huynh D., Chan J. YouTube as a source of information on COVID-19: A pandemic of misinformation? BMJ Global Health. 2020;5(5) doi: 10.1136/bmjgh-2020-002604. Article e002604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loewenthal K., Lewis C.A. Psychology press; 2018. An introduction to psychological tests and scales. [Google Scholar]
- Loomba S., de Figueiredo A., Piatek S.J., de Graaf K., Larson H.J. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nature Human Behaviour. 2021;5(3):337–348. doi: 10.1038/s41562-021-01056-1. [DOI] [PubMed] [Google Scholar]
- Luk T.T., Zhao S., Wu Y., Wong J.Y.H., Wang M.P., Lam T.H. Prevalence and determinants of SARS-CoV-2 vaccine hesitancy in Hong Kong: A population-based survey. Vaccine. 2021;39(27):3602–3607. doi: 10.1016/j.vaccine.2021.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo C., Chen A., Cui B., Liao W. Exploring public perceptions of the COVID-19 vaccine online from a cultural perspective: Semantic network analysis of two social media platforms in the United States and China. Telematics and Informatics. 2021;65 doi: 10.1016/j.tele.2021.101712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonald N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- Machida M., Nakamura I., Kojima T., Saito R., Nakaya T., Hanibuchi T., Takamiya T., Odagiri Y., Fukushima N., Kikuchi H., Amagasa S., Watanabe H., Inoue S. Acceptance of a COVID-19 vaccine in Japan during the COVID-19 pandemic. Vaccines. 2021;9(3):210. doi: 10.3390/vaccines9030210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercier H. Princeton University Press; 2020. Not Born Yesterday: The Science of Who We Trust and What We Believe. [Google Scholar]
- Misra S., Stokols D. Psychological and health outcomes of perceived information overload. Environment and Behavior. 2012;44(6):737–759. doi: 10.1177/0013916511404408. [DOI] [Google Scholar]
- Neuman W.R. Harvard University Press; Cambridge, MA: 2016. The Digital Difference: Media Technology and the Theory of Communication Effects. [Google Scholar]
- Obamiro K., Lee K. Information overload in patients with atrial fibrillation: Can the cancer information overload (CIO) scale be used? Patient Education and Counseling. 2019;102(3):550–554. doi: 10.1016/j.pec.2018.10.005. [DOI] [PubMed] [Google Scholar]
- Painter E.M., Ussery E.N., Patel A., Hughes M.M., Zell E.R., Moulia D.L., Scharf L.G., Lynch M., Ritchey M.D., Toblin L.R., Murthy B.P., Harris L.Q., Wasley A., Rose D.A., Cohn A., Messonnier N.E. Demographic characteristics of persons vaccinated during the first month of the COVID-19 vaccination program—United States, December 14, 2020–January 14, 2021. Morbidity and Mortality Weekly Report. 2021;70(5):174. doi: 10.15585/mmwr.mm7005e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasick R.J., D'onofrio C.N., Otero-Sabogal R. Similarities and differences across cultures: Questions to inform a third generation for health promotion research. Health Education Quarterly. 1996;23(1_suppl):142–161. doi: 10.1177/109019819602301S11. [DOI] [Google Scholar]
- Perea A., Slater M.D. Power distance and collectivist/individualist strategies in alcohol warnings: Effects by gender and ethnicity. Journal of Health Communication. 1999;4(4):295–310. doi: 10.1080/108107399126832. [DOI] [PubMed] [Google Scholar]
- Petherick A., Goldszmidt R., Andrade E.B., Furst R., Hale T., Pott A., Wood A. A worldwide assessment of changes in adherence to COVID-19 protective behaviours and hypothesized pandemic fatigue. Nature Human Behaviour. 2021;5(9):1145–1160. doi: 10.1038/s41562-021-01181-x. [DOI] [PubMed] [Google Scholar]
- Phelan J.C., Link B.G., Tehranifar P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. Journal of Health and Social Behaviour. 2010;51(1_suppl):S28–S40. doi: 10.1177/0022146510383498. [DOI] [PubMed] [Google Scholar]
- Pian, W., Chi, J., & Ma, F. (2021). The causes, impacts and countermeasures of COVID-19 “Infodemic”: A systematic review using narrative synthesis. Information Processing & Management, 58(6), 102713. 10.1016/2Fj.ipm.2021.102713. [DOI] [PMC free article] [PubMed]
- Policy Institute. (2020, January 2). Coronavirus: vaccine misinformation and the role of social media.https://www.kcl.ac.uk/policy-institute/assets/coronavirus-vaccine-misinformation.pdf.
- Polonijo A.N., Carpiano R.M. Social inequalities in adolescent human papillomavirus (HPV) vaccination: a test of fundamental cause theory. Social Science & Medicine. 2013;82:115–125. doi: 10.1016/j.socscimed.2012.12.020. [DOI] [PubMed] [Google Scholar]
- Pulido C.M., Villarejo-Carballido B., Redondo-Sama G., Gómez A. COVID-19 infodemic: More retweets for science-based information on coronavirus than for false information. International Sociology. 2020;35(4):377–392. doi: 10.1177/0268580920914755. [DOI] [Google Scholar]
- Rathore F.A., Farooq F. Information overload and infodemic in the COVID-19 pandemic. The Journal of the Pakistan Medical Association. 2020;70(5):162–165. doi: 10.5455/jpma.38. [DOI] [PubMed] [Google Scholar]
- Ries, M. (2022). The COVID-19 Infodemic: Mechanism, Impact, and Counter-Measures—A Review of Reviews. Sustainability, 14(5), 2605. 10.3390/su14052605. [DOI]
- Robertson E., Reeve K.S., Niedzwiedz C.L., Moore J., Blake M., Green M., Katikireddi S.V., Benzeval M.J. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain, Behavior, and Iimmunity. 2021;94:41–50. doi: 10.1016/j.bbi.2021.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romer D., Jamieson K.H. Conspiracy theories as barriers to controlling the spread of COVID-19 in the US. Social Science & Medicine. 2020;263 doi: 10.1016/j.socscimed.2020.113356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roozenbeek J., Schneider C.R., Dryhurst S., Kerr J., Freeman A.L., Recchia G., Van Der Bles A.M., Van Der Linden S. Susceptibility to misinformation about COVID-19 around the world. Royal Society Open Science. 2020;7(10) doi: 10.1098/rsos.201199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothgerber H. Real men don't eat (vegetable) quiche: Masculinity and the justification of meat consumption. Psychology of Men & Masculinity. 2013;14(4):363. doi: 10.1037/a0030379. [DOI] [Google Scholar]
- Rothkopf D.J. When the buzz bites back. The Washington Post. 2003 https://www.washingtonpost.com/archive/opinions/2003/05/11/when-the-bzz-bites-back/bc8cd84f-cab6-4648-bf58-0277261af6cd/ [Google Scholar]
- Sarkhel S., Bakhla A.K., Praharaj S.K., Ghosal M.K. Information overload regarding COVID-19: Adaptation and validation of the cancer information overload scale. Indian Journal of Psychiatry. 2020;62(5):481. doi: 10.4103/psychiatry.indianjpsychiatry_974_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider C.R., Dryhurst S., Kerr J., Freeman A.L., Recchia G., Spiegelhalter D., van der Linden S. COVID-19 risk perception: A longitudinal analysis of its predictors and associations with health protective behaviours in the United Kingdom. Journal of Risk Research. 2021;24(3-4):294–313. doi: 10.1080/13669877.2021.1890637. [DOI] [Google Scholar]
- Scientific Advisory Group for Emergencies (SAGE) (2020). SPI-B return on risk of public disorder. GOV.UK. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/887660/08-spi-b-return-on-risk-of-public-disorder.pdf.
- Sharma, K., Seo, S., Meng, C., Rambhatla, S., Dua, A. & Liu, Y. (2020). Coronavirus on social media: Analyzing misinformation in Twitter Conversations 2019. http://arxiv.org/abs/2003.12309.
- Simon F.M., Camargo C.Q. Autopsy of a metaphor: The origins, use and blind spots of the ‘infodemic’. New Media & Society. 2021 doi: 10.1177/14614448211031908. 14614448211031908. [DOI] [Google Scholar]
- Swami V., Furnham A. Examining conspiracist beliefs about the disappearance of Amelia Earhart. The Journal of General Psychology. 2012;139(4):244–259. doi: 10.1080/00221309.2012.697932. [DOI] [PubMed] [Google Scholar]
- Todosijević B., Enyedi Z. Authoritarianism without dominant ideology: Political manifestations of authoritarian attitudes in Hungary. Political Psychology. 2008;29(5):767–787. doi: 10.1111/j.1467-9221.2008.00663.x. [DOI] [Google Scholar]
- Tram K.H., Saeed S., Bradley C., Fox B., Eshun-Wilson I., Mody A., Geng E. Deliberation, dissent, and distrust: understanding distinct drivers of coronavirus disease 2019 vaccine hesitancy in the United States. Clinical Infectious Diseases. 2022;74(8):1429–1441. doi: 10.1093/cid/ciab633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Aelst P., Strömbäck J., Aalberg T., Esser F., De Vreese C., Matthes J., Hopmann D., Salgado S., Hubé N., Stępińska A., Papathanassopoulos S., Berganza R., Legnante G., Reinemann C., Sheafer T., Stanyer J. Political communication in a high-choice media environment: a challenge for democracy? Annals of the International Communication Association. 2017;41(1):3–27. doi: 10.1080/23808985.2017.1288551. [DOI] [Google Scholar]
- Van der Linden S. Misinformation: susceptibility, spread, and interventions to immunize the public. Nature Medicine. 2022;28(3):460–467. doi: 10.1038/s41591-022-01713-6. [DOI] [PubMed] [Google Scholar]
- Van Prooijen J.W. Why education predicts decreased belief in conspiracy theories. Applied Cognitive Psychology. 2017;31(1):50–58. doi: 10.1002/acp.3301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Prooijen J.W., Douglas K.M. Conspiracy theories as part of history: The role of societal crisis situations. Memory Studies. 2017;10(3):323–333. doi: 10.1177/1750698017701615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vraga E.K., Bode L. Defining misinformation and understanding its bounded nature: Using expertise and evidence for describing misinformation. Political Communication. 2020;37(1):136–144. doi: 10.1080/10584609.2020.1716500. [DOI] [Google Scholar]
- Wilson S.L., Wiysonge C. Social media and vaccine hesitancy. BMJ Global Health. 2020;5(10) doi: 10.1136/bmjgh-2020-004206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2020). Novel coronavirus (2019-nCov): Situation report-13. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200202-sitrep-13-ncov-v3.pdf.
- World Health Organization. (2022). Coronavirus disease (COVID-19) advice for the public: Mythbusters. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters.
- World Values Survey Association. (2012). World Values Survey Wave 6, Official Questionnaire v4 June 2012. https://www.worldvaluessurvey.org/WVSDocumentationWV6.jsp.
- York C. Overloaded by the news: Effects of news exposure and enjoyment on reporting information overload. Communication Research Reports. 2013;30(4):282–292. doi: 10.1080/08824096.2013.836628. [DOI] [Google Scholar]
- Yu, Y., Lau, M., & Lau, J. T. F. (2021). Positive association between individualism and vaccination resistance against COVID-19 vaccination among Chinese adults: Mediations via perceived personal and societal benefits. Vaccines, 9(11), 1225. 10.3390/2Fvaccines9111225. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.