Abstract
Objective
Children with leukaemia experience special difficulties adapting to stressful medical procedures and to the adverse effects of chemotherapy, though they can implement their coping strategies.
The aims of the study were to assess whether the coping‐with‐pain strategies could be influenced by a child's personal and illness factors and to render possible comparisons between children with leukaemia and healthy peers. Another aim was to compare parents' and children's reports on coping strategies.
Methods
A total of 125 patients (average age = 6.79 years; SD = 3.40) with acute leukaemia (lymphocytic leukaemia 90.4% and myeloid leukaemia 9.6%) and age‐matched healthy children with their parents were enrolled in the study. A socio‐demographic questionnaire and the Waldon–Varni Pediatric Pain Coping Inventory, parent and self‐report versions, were administered 1 month after diagnosis. Data regarding the therapy's side effects were recorded.
Results
The comparison between proxy‐reports of the two groups of parents found significant differences in terms of social support, self‐cognitive instructions and catastrophising strategies. Children aged 6–10 years relied more heavily on distraction than children of other ages, using more problem‐solving and self‐cognitive instructions. The results indicated moderate parent–child agreement.
Conclusion
Health professionals could help paediatric leukaemic patients in adopting more efficiently pain coping strategies applicable for different ages.
Keywords: control group, paediatric leukaemia, pain coping, parent–child agreement, side effects
1. INTRODUCTION
Acute leukaemias are neoplastic diseases of bone marrow haematopoietic precursors, and they represent the most common neoplasia typology during childhood. Patients must face not only periodical cycles of chemotherapy and their collateral effects but also invasive monitoring procedures. All these factors, together with frequent prolonged periods of hospitalisations, can have serious repercussions for their families and for the paediatric patient's psycho‐emotional well‐being. However, children and adolescents have been shown to adapt themselves to these stressful and painful situations, adopting many coping strategies. Coping represents the set of strategies used to deal with stressful situations as a paediatric tumour represents.
In paediatric oncohematology, the stressful situation can be caused by many factors: communication of the diagnosis, hospitalisation, treatment and its side effects, invasiveness of some diagnostic and therapeutic procedures, parents' concerns and disruption of daily routine. These elements tend to disturb the balance of the children and their family by generating a state of activation (arousal), which is followed by two stages of cognitive assessment of the current situation (Grootenhuis & Last, 2001). In the first phase, defined as primary evaluation, the subject tries to elaborate an assessment of the stressful event (whether it is a situation of damage, loss, threat, or challenge), usually characterised by negative emotions. In the subsequent phase, called secondary evaluation, individuals search for possible tools to deal with the stressful situation; from this second evaluation, the coping process starts. This phase represents the most delicate moment of the process, in which the child is influenced by a variety of factors. Among these, the more relevant factors are as follows: characteristics of the disease, personal characteristics and social context. Depending on how coping evolves, a certain type of adaptation, positive or negative (Grootenhuis & Last, 2001; Zwaanswijk et al., 2011), may be encountered.
In the early 2000s, four coping styles most used by children with cancer were identified: the active one (in which the patient is prone to cognitive restructuring and searches for information and understanding), distraction, seeking support and avoidance. The most frequently used modalities seem to be cognitive reconstruction, distraction and avoidance. Whereas some studies have shown that the third is much more frequent in younger patients, according to others, avoidance is more prevalent than in healthy peers, regardless of patients' age (Tremolada et al., 2015).
In the last 20 years, studies have shown how the attitude adopted by parents in the presence of their children in certain medical conditions can have important repercussions for the emotional status of paediatric patients (Cline et al., 2006; Sobol‐Kwapińska et al., 2020). In paediatric oncohematology, it was found that stress levels experienced by children during invasive procedures (in particular, bone marrow aspirates and lumbar punctures) seem to show a direct correlation with those experienced by their parents. As far as parents concerns, other key elements are as follows: parental health locus of control that can influence a parent's emotional well‐being and may play a role in helping their children coping with the illness (Tremolada, Taverna, et al., 2020) and family routine and time reorganisation that was associated with a major use of problem‐solving and cognitive self‐instructions during the first month of therapy (Tremolada et al., 2015).
The first 6 months from diagnosis are particularly critical for patients' psychological health (Tremolada, Chiavetta, et al., 2020).
2. METHODS
2.1. Research questions
The study was conducted through the collaboration of a multiprofessional team of doctors and psychologists from the University of Padua.
The first research question concerned a comparison between pain coping strategies implemented by the paediatric patients with those of healthy peers, in relation to age. The second question focused on whether the use of these strategies in the clinical group was somehow associated with socio‐demographic and family factors or with the child's diagnosis and treatments after the first month from diagnosis.
The third question focused on the evaluation of parent–child agreement, regarding the patients' coping strategies (Sheffler et al., 2009).
2.2. Procedure
The study was conducted at the Pediatric Oncohematology Clinic, Department of Child and Woman Health, University of Padua. All personal data were collected and processed in accordance with current legislation regarding the protection of personal data, after parents signed the parental consent form. The data collection relating to the self‐report and proxy‐report questionnaires was conducted 1 month after communication of the diagnosis by the psychologist at the Clinic and approved by the local Ethics Committee. The time to administer the questionnaires has a mean of 15–20 min.
The data collected refer to two cohorts of patients, the first diagnosed in the period between 2003 and 2007 and the second between 2010 and early 2015 matched for gender and age with a control group of healthy peers. The costs were represented by the psychologist's clinical work in administering the questionnaires. The psychologist was a Ph.D. student and then a Research fellow, so the economical fare of the study is free of charge. At the first hospitalisation of the child, 1 week after the diagnosis communication, social and demographic information of the child's family was collected. One month after diagnosis (at Day +33), both patient and one of his parent (generally mother) were administered the Waldron–Varni Pediatric Pain Coping Inventory (PPCI; Bonichini & Axia, 2000, Varni et al., 1996). Eligibility criteria included being in the first month of treatment for leukaemias and age<18 years. We excluded the patients with learning or sensory problems or genetic syndromes and those who were unable to complete the questionnaires by themselves.
We matched the patients with a control group with 125 patient‐healthy peer couples with the same gender and age. Control group participants met the following eligibility criteria: no history of life‐threatening or chronic illness or injury and absence of learning or sensory problems and other pathological aspects. The control group of healthy peers was enrolled at schools in the same region of the paediatric clinic.
2.3. Instruments
2.3.1. PPCI (Varni et al., 1996; Italian version by Bonichini & Axia, 2000)
PPCI is a patient‐report and parent‐report instrument with 41 items designed to provide a standardised assessment of the child's and parents' perception of the strategies that the child utilises to cope with physical pain. A 3‐point Likert‐type scale was developed for clarity and ease of administration, and its scores ranged from 0 (never, not at all) to 1 (sometimes) to 2 (often, a lot).
According to the authors, children in pain can adopt five different coping strategies, which represent five subscales of the questionnaire, as follows:
Cognitive self‐instruction (α = 0.74): This scale includes internal self‐statements that deal with the child's pain at a cognitive level (seven items).
Problem‐solving (α = 0.67): This scale includes overt acts that are intended to manage pain (10 items).
Distraction (α = 0.66): This scale includes items that shift the child's attention to things other than pain (nine items).
Seeking social support (α = 0.66): This scale includes items in which the child seeks aid, comfort or understanding from parents, peers and others (nine items).
Catastrophising/helplessness (α = 0.57): This scale includes items that assess feelings of victimisation and powerlessness over the pain (six items).
2.3.2. SES questionnaire
Parental education and occupational status were measured. In particular, the following variables were considered: number of years of school achievement, type and average hours of job, economical status and number of familiars and sons in the family.
2.3.3. Patient's medical chart
The patient data related only to the first month of therapy were collected in a special form referring to the following: disease diagnosis (type of leukaemia, central nervous system [CNS] involvement in diagnosis, presence of metastases and risk group) and response to therapy (response to steroids on Day +8 for ALL, clinical course such as days of hospitalisation within the first 33 days, no of hospitalisations, no of pain episodes, fever, nausea, infections and mucositis). This phase was carried out by viewing all the clinical documentation available in the hospital paper archives (hospitalisation and day hospital records within the first 33 days of diagnosis) and the clinical graphics of the sedation procedures that can be consulted in the online archive of analgesic therapy.
2.4. Statistics
To answer the first question, data from the leukaemic children self‐reports were compared with the self‐reports of their healthy peers; the same procedure was performed for the comparison with parental proxy‐reports. These analyses were conducted using the Student's t‐test for paired samples, after verifying the condition of normality based on the Kolmogorov and Smirnov tests.
A normal distribution was found both for children's and parents' reports variables. Nonparametric tests were used for some analyses (see below), without normal distribution.
As the literature has shown that, among all social and demographic variables, age is an important predictive factor (Holdsworth et al., 2006; Kestler & LoBiondo‐Wood, 2012; Nunes et al., 2017), it has been considered as an independent variable, identifying four ranges and taking into account psychophysical development stages (respectively, 2–4, >4–6, >6–10 and >10 years). Analyses of variance (ANOVAs) and Bonferroni's post hoc test were carried out to make multiple comparisons between the means in the different age groups.
To answer the question about possible gender or familiar factors associated with coping‐with‐pain strategies, Pearson's correlations (if the independent variable is dichotomous) or ANOVAs (if the independent variable is multilevel ordinal) were run.
To answer the question relating to parent–patient agreement, we compared the self‐reports of the leukaemic children and the proxy‐reports of their parents using the contingency tables with Cohen's kappa and an interrater correlation coefficient. We run Spearman's t‐test for paired samples with normal distribution for the possible difference between the means.
In all analyses, the level of significance considered was equal to p < 0.05.
3. RESULTS
3.1. Participants characteristics
The average age of the 125 patients with leukaemia was 6.79 years (SD = 2.86; range 2–18 years). With reference to the categorised age, the group was distributed as follows: 17.6% between 2 and 4 years, 39.2% between 4.01 and 6 years, 27.2% between 6.01 and 10 years and 16% over 10 years. Males were 56.8%. Almost all participants (97.6%) were Caucasian.
Most of the participants (90.4%) were newly diagnosed with acute lymphoblastic leukaemia (ALL), whereas 9.6% were diagnosed with acute myeloid leukaemia (AML). Among patients, 24% were classified as standard risk, 50.4% as intermediate and 23.2% as high risk (the remaining 2.4% was unknown).
Most of the paediatric patients (97.6%) did not have CNS involvement at diagnosis, and leukaemia was associated with metastases (lymph nodes, mediastinum other or with multiple presentations) in only 13.6% of cases.
In the sample of ALL patients examined (n = 113), 53.1% were treated according to the AIEOP ALL 2000 protocol, 25.7% according to the R2006 version, 16.8% followed the AIEOP ALL 2009 protocol and 4.4% were treated according to the EsPhALL protocol for the presence of the t (9; 22) translocation. As for patients diagnosed with AML (n = 12), 91.7% were treated according to the AIEOP 2002/2001 protocol for myeloid leukaemia, whereas only one patient was treated following the GINEMA protocol.
In the group of patients with ALL, a good response to cortisone at Day +8 (PGR) was found in 80.8% of cases, and in both leukaemic forms, almost all experienced a first complete remission (99.2%).
As regards the responding parents, the largest percentage was represented by mothers (89.6%). In terms of education, 10.4% of parents obtained a 3‐year degree and only 2% completed a specialist degree course or a postgraduate course. Concerning employment, 48% of parents reported being on leave or out of work, and 58.4% reported to work for an average of 30 to 50 or more hours per week. Among the sample of parents, 33.6% declared a barely sufficient economic condition, 50.4% an adequate availability of resources, whereas only 16% claimed to be in a good situation; 77.6% owned a home (with or without a mortgage), whereas 17.6% had a rental contract. Regarding additional offspring, 17.6% reported having only one child, 46.4% had two to three children and the remaining 43.2% had more than four children.
3.2. Child's coping strategies
The relationship between PPCI scales and demographic variables shows that age correlates significantly with the factor seeking social support (r = −0.41, p < 0.001) and the factor distraction (r = −0.27, p < 0.001).
Seeking social support resulted as the most used coping strategy (F (3,288) = 13.40; p < 0.001). Distraction was more used by children hospitalised for surgery than the other strategies (F (1,98) = 2.90; p < 0.01). Cognitive self‐instruction was preferred according with increasing number of hospitalisation days (F (1,98) = 4.86; p < 0.01); seeking social support was used more by hospitalised children than by healthy ones (t (284) = 4.77; p = 0.001).
3.3. Pain coping strategies comparisons
The comparison between the proxy‐reports of the parents of children with leukaemia and healthy children found statistically significant differences for the use of social support, cognitive self‐instruction and noncatastrophising strategies (Table 1).
TABLE 1.
Comparison parameters between the means of use of the five coping strategies based on what is reported by the parents of ill and healthy children
| Coping strategies | t | df | p‐value |
|---|---|---|---|
| Distraction | −3.74 | 121 | 0.0001 |
| Problem‐solving | 1.46 | 121 | 0.15 |
| Seek for social support | −2.7 | 121 | 0.01 |
| Cognitive self‐instruction | 2.91 | 121 | 0.004 |
| Noncatastrophising | −2.78 | 121 | 0.01 |
| Total efficacy | −0.78 | 121 | 0.44 |
As reported by the parents, the group of children with leukaemia was more inclined towards strategies such as cognitive self‐instruction (M ill = 0.84; SS ill = 0.37 and M healthy = 0.71; SD healthy = 0.36), whereas controls tended to prefer distraction (M health y = 0.77; SD healthy = 0.34 and M ill = 0.61; SD ill = 0.36), catastrophising (M healthy = 1; SD healthy = 0.29 and M ill = 0.89; SD ill = 0.38) and social support (M healthy = 1.2; SD healthy = 0.30 and M ill = 1.09; SD ill = 0.37) (Figure 1).
FIGURE 1.
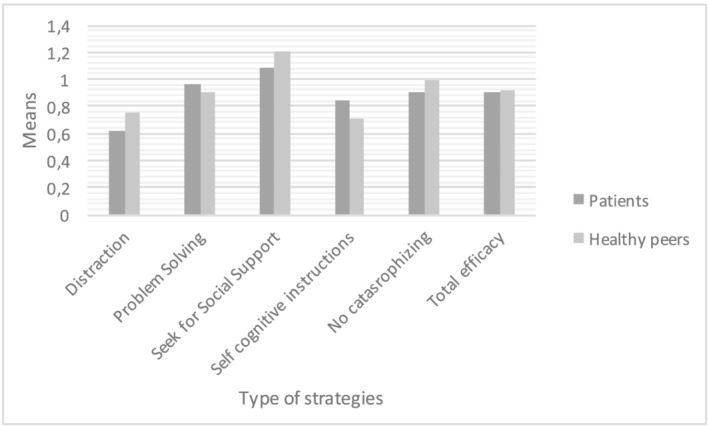
Comparison by paired samples t‐tests between the means of each of the five coping strategies reported by parents of the ill and healthy children
The same type of comparison was carried out on the two samples of children (clinical vs. control) divided by age‐levels (Group 1: 2–4 years; Group 2: 4–6 years; Group 3: 6–10 years; Group 4: 10–18 years).
From the analyses of the samples of Group 1 (n = 22 pairs), significant differences were found in the distraction subscale (t = −2.49; p = 0.02), and in catastrophising (t = −2.04; p = 0.05), the first group of strategies was more frequent in the control group (M control = 0.75; SD control = 0.33 and M clinic = 0.53; SD clinic = 0.33), whereas leukaemic children had a tendency to catastrophise (for catastrophising: M clinic = 0.9; SD clinic = 0.28 and M control = 1.06; SD control = 0.28).
As regards Group 2 (n = 49 couples), a significant difference was found in the use of distraction (t = −3.03; p = 0.004; M control = 0.75; SD control = 0.39 and M clinic = 0.53; SD clinic = 0.3), social support (t = −2.01; p = 0.05; M control = 1.19; SD control = 0.28 and M clinic = 1.06; SD clinic = 0.38), catastrophising (t = −2.3; p = 0.03; M control = 0.95; SD clinic = 0.26 and M clinic = 0.82; SD clinic = 0.38) and cognitive self‐instructions (t = 2.3; p = 0.03; M ill = 0.83; SD clinic = 0.38 and M control = 0.66; SD control = 0.36): The first three strategies showed higher scores in the control group, while cognitive self‐instruction was more used by children with leukaemia.
From the analyses of Group 3 (n = 34 couples), a statistically significant difference was found in the use of cognitive self‐instructions (t = 2.25; p = 0.03) with greater use by patients (M clinic = 0.94, SD clinic = 0.32) compared with healthy peers (M control = 0.74; SD control = 0.38).
No significant differences were found in the comparison between means in subjects with age >10 years (n = 20 couples).
3.4. Socio‐demographic and illness variables related to children's coping strategies
Univariate ANOVA and Bonferroni's post hoc procedure for multiple comparisons were used to determine whether the children's adoption of coping strategies differed significantly across the four age groups.
Differences emerged in the use of distraction (F 3,? = 3.87; p = 0.01), problem‐solving (F 3,? = 4.13; p = 0.01) and cognitive self‐instruction (F 3,? = 3.01; p = 0.03) and in the total score (F 3,? = 2.71; p = 0.05).
Thanks to Bonferroni's procedure for multiple comparisons, the differences for each individual age group were explored (n group1 = 22; n group2 = 49; n group3 = 34; n group4 = 20), showing that distraction was adopted more by children aged 6–10 years than by children in the preceding age bands. Problem‐solving and cognitive self‐instruction strategies were used more by older children, (Table 2 and Figure 2).
TABLE 2.
Bonferroni post hoc test (p ≤ 0.05) of childs coping strategies by child's age bands
| Age bands | ||||
|---|---|---|---|---|
| Coping strategies |
(1) 2–4 years |
(2) 4.01–6 years |
(3) 6.01–10 years |
(4) >10 years |
| Distraction | ns | I‐J = −0.24 (3); p = 0.01 | I‐J = 0.24 (2); p = 0.01 | ns |
| Problem‐solving |
I‐J = −0.23 (2); p = 0.04 I‐J = −0.29 (3); p = 0.01 I‐J = −0.29 (4); p = 0.03 |
I‐J = 0.23 (1); p = 0.04 |
I‐J = 0.29 (1); p = 0.01 |
I‐J = 0.29 (1); p = 0.03 |
| Seek for social support | ns | ns | ns | ns |
| Cognitive self‐instruction |
I‐J = −0.28(3); p = 0.03 |
ns |
I‐J = 0.28(3); p = 0.03 |
ns |
| Noncatastrophising | ns | ns | ns | ns |
| Total efficacy | ns | ns | ns | ns |
Note: Means for each age bands are reported. The numbers in parentheses refer to the significant comparisons between the different pairs of age bands.
Abbreviation: ns, nonsignificant.
FIGURE 2.
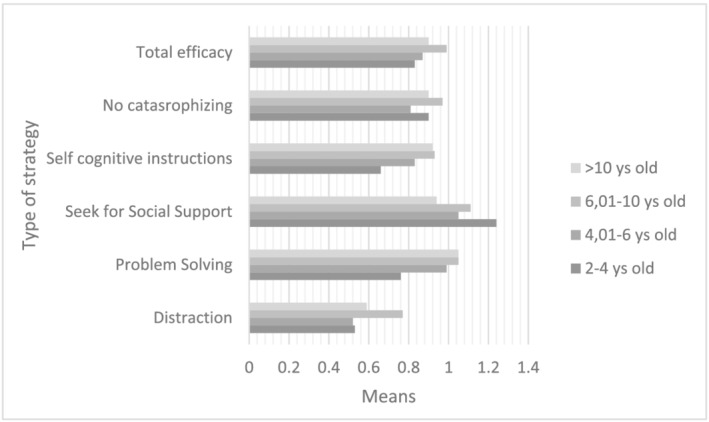
Comparison between the averages of the items of each of the five coping strategies considered based on the reports of the parents of ill children categorised according to the age of the patients
There were no significant differences based on gender, and all the medical variables were considered in the clinical group (type of diagnosis and protocol, the risk group, the CNS involvement or the presence of metastases, the use of cortisone or the response to therapy).
In the clinical group, a negative correlation (Table 3) emerged between the use of distraction and the number of days of hospitalisation (r = −0.19; p = 0.04), number of episodes of fever (r = −0.22; p = 0.02) and mucositis (r = −0.24; p = 0.01), whereas a positive one with the episodes of nausea (r = 0.18; p = 0.04). Cognitive self‐instruction resulted to be associated with the number of hospitalisations (r = −0.19; p = 0.03) and the number of mucositis episodes (r = −0.029; p = 0.001).
TABLE 3.
Possible associations through Pearson correlations between the means of use of the five coping strategies based on what was reported by the parents of the sick children and specific characteristics of hospitalisation within the first month of diagnosis
| Coping strategies | Medical variables | ||||||
|---|---|---|---|---|---|---|---|
| Days of hospitalisation | Number of recoveries | Pain episodes | Fever episodes | Nausea episodes | Mucositi | ||
| Distraction | r | −0.19 * | −0.15 | −0.09 | −0.22 * | 0.18 * | −0.24 * |
| p‐value | 0.04 | 0.1 | 0.31 | 0.02 | 0.04 | 0.01 | |
| Problem‐solving | r | −0.002 | 0.04 | 0.09 | 0.1 | 0.05 | −0.03 |
| p‐value | 0.98 | 0.04 | 0.31 | 0.28 | 0.59 | 0.79 | |
| Seek for social support | r | −0.07 | −0.03 | 0.15 | −0.11 | 0.09 | 0.01 |
| p‐value | 0.43 | 0.71 | 0.1 | 0.24 | 0.35 | 0.9 | |
| Cognitive self‐instruction | r | −0.15 | −0.19 * | −0.06 | −0.14 | −0.05 | −0.29 * |
| p‐value | 0.1 | 0.03 | 0.53 | 0.12 | 0.8 | 0.001 | |
| Noncatastrophising | r | 0.06 | −0.02 | 0.18 | 0.07 | −0.03 | 0.1 |
| p‐value | 0.40 | 0.85 | 0.08 | 0.45 | 0.75 | 0.26 | |
| Total efficacy | r | −0.11 | −0.09 | 0.09 | −0.11 | 0.09 | −0.15 |
| p‐value | 0.21 | 0.31 | 0.36 | 0.24 | 0.32 | 0.11 | |
Note: Values in bold emphasis are significant results.
p value < 0.05.
3.5. Parent–patient agreement
From the analyses carried out with Student's t‐test for paired samples (n = 49 pairs of leukaemic children and their parents), a significant difference emerged in social support (t = 1.45, df = 47, p = 0.05): The child required social support more frequently according to parents' reports than children's reports (M parent = 1.19; SD parent = 0.33 and M child = 1.05; SD child = 0.35). Another significant difference was found for self‐cognitive instructions (t = −2.36, df = 47, p = 0.02), which were reported higher by children (M child = 0.94; SD child = 0.41) than their parents (M parent = 0.77; SD parent = 0.35) (Figure 3).
FIGURE 3.
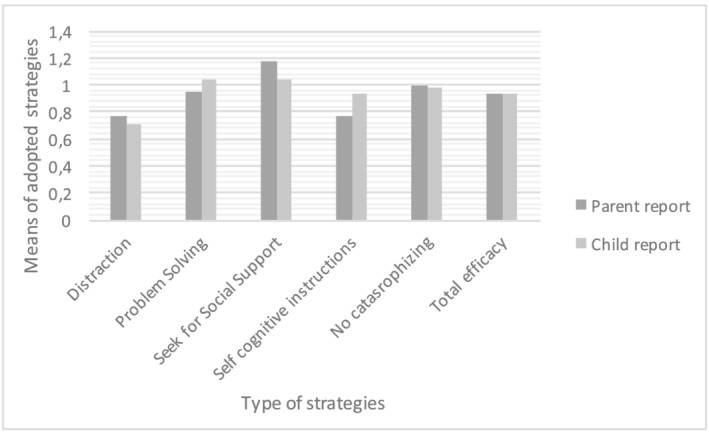
Comparison by means adopting t‐tests for paired samples between the means of the five coping strategies reported by children themselves with those reported by parents
4. DISCUSSION
Children's coping with pain is crucial for the adaptation of paediatric patients with leukaemia to hospitalisations and treatments. Several short‐term stressful complications can happen, such as nausea, vomiting and mucositis, and these negative effects may negatively impact children's emotive well‐being.
The findings of this study showed that coping was influenced by child's age: Distraction, problem‐solving and cognitive self‐instruction were adopted mostly by children aged 6–10 years. Children aged 2–6 years used less strategies, especially problem‐solving and distraction, whereas all children used social support more than all the other ones independently from age.
Paediatric cancer patients (especially <6 years) experienced greater difficulty in using distraction than their healthy peers and tended to prefer different types of strategies. From the analyses carried out, this difficulty seems to be correlated directly with a prolongation of hospitalisation (typical of AML) or with an increase in the frequency of hospitalisations (especially high in ALL). In addition, distraction and cognitive self‐instruction strategies were reported less if episodes of pain, fever and mucositis were more frequent, whereas distraction was reported as higher in presence of multiple episodes of nausea.
In younger patients (2–4 years), the prevalence of strategies, such as seeking social support and catastrophising, was found. Unlike what happened among the population of healthy children, patients between 4 and 6 years began to adopt problem‐solving techniques and cognitive self‐instruction, although these strategies are normally used more from school age (Garmezy & Rutter, 1983). This anticipation of the use of such strategies in the clinic group, that are generally more frequent in adolescence, can probably be associated with the situation of serious difficulty in which these subjects found themselves. In this same age group, children also have the highest level of use of distraction, so it is necessary for health professionals to help children in this regard, by offering them, for instance, advice on adopting relaxation techniques. The treatment's negative effects may dampen the effectiveness of coping strategies, and it is necessary to enhance the training of cognitive strategies.
Another finding derives from the comparison between patients and healthy peers in their adoption of coping strategies: Children with leukaemia used more cognitive strategies and catastrophising, whereas the healthy peers preferred distraction and social support to cope with pain.
It was found that the average total efficacy reaches its peak in the pre‐adolescent period, which is in line with findings of other studies in the literature. In fact, many studies have shown that, starting from the age of 7 years, children begin overcoming crying and screaming phase gaining greater self‐control and request for support from the people around them (Ellis & Spanos, 1994), experimenting with what are defined as cognitive strategies.
As far as agreement between parents' and children's reports in the clinical group concerns, although no specific studies have been found on the parent–patient agreement on pain coping strategies, the research carried out on the comparison of proxy and self‐reports in the context of HRQOL has, in fact, revealed how often informants' disagreements are anchored to parents' anxious and worried states (Cremeens et al., 2006) or may vary according to patients' age with a lower agreement between adolescents and their parents (Chang & Yeh, 2005).
Children reported seeking social support less frequently than parents did in their reports, whereas they reported self‐cognitive instructions more. Interestingly, parents judged their help contribution as more important than their children's estimations.
Basing on these results, there are some clinical suggestions that can be derived:
Administer these questionnaires on children's coping with pain to screen the specific strategies adopted by paediatric patients in their hospitalisation for leukaemia treatment
Empower coping with strategies less adopted in children with leukaemia, such as distraction, for example, with mindfulness, relaxation, guidance visualisation or virtual experiences.
The adoption of problem‐solving techniques and cognitive self‐instructions in children aged 4–6 years could be adapted in these preschoolers using an educative approach, through cartoon, role playing and emotional communication. These interventions could be proposed by clinical psychologists, nurses or educators during the hospitalisation of the children not only during stress conditions but also during their daily life in the clinic.
Parenting support should be provided to implement parents' capacity to help children in their adoption of efficacious pain coping strategies. Parental training could be proposed to ameliorate their efficacy in taking care of their children during medical procedures.
CONFLICT OF INTEREST
The authors have no conflict to declare.
AUTHOR CONTRIBUTION
All the authors contributed equally to this work.
ETHICS STATEMENT
The project “Family factors predicting short‐ and long‐term adaptation and quality of life in children with leukaemia. A longitudinal study” was approved by the Ethics Committee of University Hospital of Padua.
ACKNOWLEDGEMENT
The study is supported by the Istituto della Ricerca Pediatrica Città della Speranza. Open Access Funding provided by Universita degli Studi di Padova within the CRUI‐CARE Agreement.
Tremolada, M. , Tasso, G. , Bonichini, S. , Taverna, L. , Tumino, M. , Putti, M. C. , Biffi, A. , & Pillon, M. (2022). Pain coping strategies in paediatric patients newly diagnosed with leukaemia compared with healthy peers. European Journal of Cancer Care, 31(3), e13575. 10.1111/ecc.13575
[Correction added on 20 May 2022, after first online publication: CRUI funding statement has been added.]
Funding information Istituto della Ricerca Pediatrica Città della Speranza
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Bonichini, S. , & Axia, G. (2000). La valutazione delle strategie di coping al dolore fisico nei bambini di età scolare. Psicologia Clinica dello Sviluppo, 1, 97–123. [Google Scholar]
- Chang, P. C. , & Yeh, C. H. (2005). Agreement between child self‐report and parent proxy‐report to evaluate quality of life in children with cancer. Psychooncology, 14, 125–134. [DOI] [PubMed] [Google Scholar]
- Cline, R. J. , Harper, F. W. , Penner, L. A. , Peterson, A. M. , Taub, J. W. , & Albrecht, T. L. (2006). Parent communication and child pain and distress during painful pediatric cancer treatments. Social Science & Medicine, 63(4), 883–898. 10.1016/j.socscimed.2006.03.007 [DOI] [PubMed] [Google Scholar]
- Cremeens, J. , Eiser, C. , & Blades, M. (2006). Factors influencing agreement between child self‐report and parent proxy‐reports on the Pediatric Quality of Life Inventory 4.0 (PedsQL) generic core scales. Health and Quality of Life Outcomes, 30(4), 58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis, J. A. , & Spanos, N. P. (1994). Cognitive‐behavioral interventions for children's distress during bone marrow aspirations and lumbar punctures: A critical review. Journal of Pain and Symptom Management, 9(2), 96–108. 10.1016/0885-3924(94)90162-7 [DOI] [PubMed] [Google Scholar]
- Garmezy, N. , & Rutter, M. (1983). Stress, Coping, and Development in Children. McGraw‐Hill. [Google Scholar]
- Grootenhuis, M. A. , & Last, B. F. (2001). Children with cancer with different survival perspectives: Defensiveness, control strategies, and psychological adjustment. Psychooncology, 10(4), 305–314. 10.1002/pon.529 [DOI] [PubMed] [Google Scholar]
- Holdsworth, M. T. , Raisch, D. W. , & Frost, J. (2006). Acute and delayed nausea and emesis control in pediatriconcology patients. Cancer, 106(4), 931–940. 10.1002/cncr.21631 [DOI] [PubMed] [Google Scholar]
- Kestler, S. A. , & LoBiondo‐Wood, G. (2012. Mar‐Apr). Review of symptom experiences in children and adolescents with cancer. CancerNurs, 35(2), E31–E49. 10.1097/NCC.0b013e3182207a2a [DOI] [PubMed] [Google Scholar]
- Nunes, M. D. R. , Jacob, E. , Bomfim, E. O. , Lopes‐Junior, L. C. , De Lima, R. A. G. , Floria‐Santos, M. , & Nascimento, L. C. (2017). Fatigue and health related quality of life in children and adolescents with cancer. Eur J OncolNurs, 29, 39–46. 10.1016/j.ejon.2017.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheffler, L. C. , Hanley, C. , Bagley, A. , Molitor, F. , & James, M. A. (2009). Comparison of self‐reports and parent proxy‐reports offunctionandqualityoflifeofchildrenwithbelow‐the‐elbowdeficiency. The Journal of Bone and Joint Surgery. American Volume, 91(12), 2852–2859. 10.2106/JBJS.H.01108 [DOI] [PubMed] [Google Scholar]
- Sobol‐Kwapińska, M. , Sobol, M. , & Woźnica‐Niesobska, E. (2020). Parental behavior and child distress and pain during pediatric medical procedures: Systematic review and meta‐analysis. Health Psychology, 39(7), 558–572. 10.1037/hea0000864 [DOI] [PubMed] [Google Scholar]
- Tremolada, M. , Bonichini, S. , Basso, G. , & Pillon, M. (2015). Coping with pain in children with leukemia. International Journal of Cancer Research and Prevention, 8, 451–466. [Google Scholar]
- Tremolada, M. , Taverna, L. , Chiavetta, I. T. , Bonichini, S. , Putti, M. C. , & Biffi, A . (2020). Psychological wellbeing in adolescents with leukaemia: A comparative study with typical development peers. International Journal of Environmental Research and Public Health, 17, 567–579. 10.3390/ijerph17020567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tremolada, M. , Taverna, L. , Bonichini, S. , Putti, M. C. , Pillon, M. , & Biffi, A. (2020). Health locus of control in parents of children with leukemia and associations with their life perceptions and depression symptomatology. Children, 7(5), 40–52. 10.3390/children7050040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varni, J. W. , Waldron, S. A. , Gragg, R. A. , Rapoff, M. A. , Bernstein, B. H. , Lindsley, C. B. , & Newcomb, M. D. (1996). Development of the Waldron/Varni pediatric pain coping inventory. Pain, 67(1), 141–150. 10.1016/0304-3959(96)03077-1 [DOI] [PubMed] [Google Scholar]
- Zwaanswijk, M. , Tates, K. , van Dulmen, S. , Hoogerbrugge, P. M. , Kamps, W. A. , Beishuizen, A. , & Bensing, J. M . (2011). Communicating with young patients in pediatric oncology consultations: A vignette study on patients', parents', and survivors' communication preferences. Psycho‐Oncology, 20(3), 269–276. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


