Abstract
Introduction
Widespread adoption of the human papillomavirus (HPV) vaccine will require population acceptance and tailoring of immunisation services to community needs and preferences. We examined peer‐reviewed publications on the acceptability of and barriers to the HPV vaccine across China.
Methods
We searched English (MEDLINE, Embase, and Web of Science) and Chinese (CNKI, VIP, Wanfang data) databases between 1 January 2006 and 31 December 2017. We adopted a narrative approach for data synthesis.
Results
We identified 73 studies. The overall median acceptability of HPV vaccine was 71.8% (Q1–Q3: 58.6%–81%). Low levels of acceptability (<40%) of HPV vaccine were found in eastern regions of China. The largest differences of acceptability were observed between rural western regions (all >90%) and urban eastern regions (all <35%). Despite these regional variations, common barriers to HPV vaccine acceptance were concerns about vaccine safety, uncertainty over vaccine effectiveness, low perceived risk of cervical cancer and the price of the vaccine. The level of willingness to pay for the HPV vaccine (over 153 US dollars) was very low (<7%).
Conclusion
The acceptability of and attitudes towards HPV vaccine vary by regions and populations across China. HPV vaccination programmes will need to tailor service delivery as well as information materials to take account of regional concerns.
Keywords: HPV vaccine, mainland China, safety concerns, vaccine acceptability, vaccine hesitancy
1. INTRODUCTION
Cervical cancer is the second most common cancer in women aged 15–44 years in China, with an estimated 106,430 new cases and 47,739 deaths occurring annually (Bruni et al., 2018, 2019). The annual increase of incidence and mortality of cervical cancer was the second highest among female cancers in the decade from 2000 to 2011 (Chen et al., 2016; Hu, Zheng, et al., 2014b). In 2018, the World Health Organization (WHO) launched a global strategy towards the elimination of cervical cancer and set three targets for the year 2030—‘90% coverage of HPV vaccination, 70% coverage of twice‐lifetime screening, and 90% access to cervical precancer and cancer treatment services and palliative care’ (Canfell et al., 2020). China's National Health Commission (NHC) has given full support to the WHO's global strategy. The Chinese Government's policy document Health China 2030—signalling the government's commitment to investing in health—included fast‐tracking conditional approval of the nine‐valent HPV vaccine and removing import tariffs on cancer drugs (F. Zhao & Qiao, 2019).
Imported vaccines against Human Papilloma Virus—Cervarix (bivalent vaccine) and Gardasil (quadrivalent and nine‐valent vaccine)—were approved in China in 2016 (Pan et al., 2016), 2017(Yin, 2017) and 2018(Lin et al., 2019), respectively (Cao, 2020; Yin, 2017). A domestic vaccine—Cecolin—was approved in January 2020, with a two‐dose schedule for adolescents aged 9–14 years, and three doses for females aged 15–45 years (Cao, 2020). In May 2020, Cecolin obtained WHO pre‐qualification and was approved by the National Medical Products Administration (NMPA) for shipment of 100,000 doses to mainland China. However, the sole vaccine supply is inadequate to meet demand. Current government policy (Cao, 2020; Y. Xue, 2019) is that individuals can self‐pay for the HPV vaccine through their private or employer insurance (Cao, 2020; Y. Xue, 2019)—a decision that may be determined by an individual perceptions of the HPV vaccine. A review of the global literature has suggested that women's choices over use of the HPV vaccine are influenced by multiple factors including the cost of vaccination, perceived efficacy and safety of the vaccine, and provision of information about vaccination (Santhanes et al., 2018).
Concerns about the safety and effectiveness of the HPV vaccine in China have been influenced by media reports of vaccine safety incidents between 2013 and 2018(Hu et al., 2020; J. Ren et al., 2018; Yang et al., 2014). There is little evidence to support these concerns; however it has been difficult to assuage public doubts about HPV vaccination. Population characteristics affect acceptability; Lin et al. (2019) and You et al. (2020) reported socio‐economic status was associated with a willingness to accept imported HPV vaccines among female undergraduates in China. A subsequent study in Shanghai reported migrants had lower confidence in the vaccine's benefits compared with the urban population, but were not as concerned about safety issues (J. Ren et al., 2018).
Despite an increasing focus on attitudes towards and acceptability of HPV vaccination in China, there is a dearth of comprehensive analysis, and limited data on any variation by demography or geography. To date, only one systematic review and meta‐analysis (Y. Zhang et al., 2016) has been published on the knowledge and acceptability of the HPV vaccine among Chinese populations. The pooled acceptability of the HPV vaccine was 67.25%, with rates varied by sex, ethnicity and geographic regions. Safety of the vaccine was the main concern raised (Y. Zhang et al., 2016). However, variations of attitudes by region and socio‐economic status of populations were not explored. The most recent and comprehensive survey among the Chinese population was a multicenter research study in 136 universities across eastern (78), central (27) and western (31) regions of China in 2019 (You et al., 2020). This study reported moderate acceptance (54%) of the HPV vaccine—the proportion of the sampled population who say they would be willing to receive the HPV vaccine. Living in central and western regions and low socio‐economic status were found to be associated with low levels of willingness to receive the HPV vaccination (You et al., 2020). However, barriers were not presented in terms of regional or socio‐economic status (You et al., 2020).
We have carried out a systematic literature review of the acceptability of the HPV vaccine, and attitudes influencing the uptake of the HPV vaccine, across in the three regions (eastern, central and western) of China, and also reporting on variations in attitudes and acceptability by heterogeneous population groups, in order to inform targeted education strategies.
2. MATERIALS AND METHODS
2.1. Search strategy and selection criteria
We searched English‐language databases: MEDLINE, Embase, and Web of Science and Chinese‐language databases: China National Knowledge Infrastructure (CNKI), VIP Database for Chinese Technical Periodicals (VIP) and Wanfang data for relevant articles published between 1 January 2006 and 31 December 2017. The search terms are provided in Table S1. We included research studies if they included Chinese populations, assessed the acceptability of HPV vaccine and factors that may affect this level and were carried out in Mainland China, not in Hong Kong, Macao and Taiwan. Studies were excluded if they did not present original data (e.g., review), outcomes were not completely presented preventing data extraction, or only reported data on either knowledge or awareness of HPV and vaccine but did not report on acceptability and attitudes. The study selection followed Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) guidelines (Moher et al., 2009) and the selection process is displayed in Figure 1.
FIGURE 1.
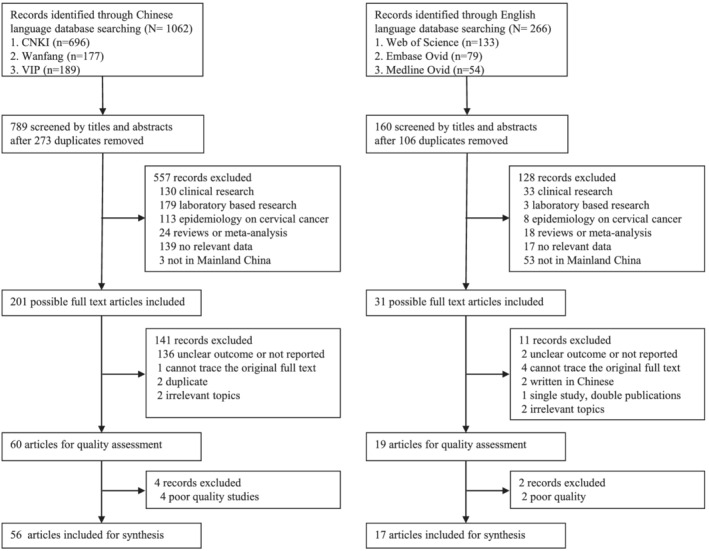
Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) flow diagram for selection of studies
DuW, JD and BT independently reviewed the titles and abstracts in the Chinese databases. HO and DuW reviewed the English titles and abstracts. Disagreement on the records were discussed and clarified by DuW. The final decision was made by DuW for the inclusion of articles in the systematic review.
2.2. Data synthesis
A standardised data extraction form was used (variables included study date, setting, participant characteristics, and the outcomes of each study). When identifying reported reasons for not accepting the HPV vaccine, we extracted the exact wording from English published papers, and translated Chinese wording into English from Chinese published papers. Four authors (DuW, HO, JD and BT) extracted the information from included studies and any disagreements were resolved through discussion. Study populations described in more than one paper were included as one research study, with any duplicate data excluded.
An adapted version of Zaza's validated checklist (Zaza et al., 2000) (Table S2) was used to assess the quality of included studies. The checklist was translated from English into Chinese for quality assessment of the Chinese language studies, and assessed according to the checklist by three authors (DuW, JD and BT). Studies in English were assessed by HO and DuW; disagreements were resolved through discussion. Each study was graded as ‘good’, ‘fair’ or ‘low’ quality based on the scores generated by Zaza's checklist (Zaza et al., 2000). The outcome was presented in the Quality Assessment Tables (Table S3). ‘Low’ quality studies were removed for data synthesis.
A narrative approach was used to synthesise data (Ryan & Cochrane Consumers and Communication Review Group, 2020). Given the heterogeneity between studies (e.g., geographical regions, study populations and methods), and analytical strategies (adjustment for different confounders), meta‐analysis of data was not feasible. The rationale for using narrative synthesis instead of meta‐analysis is summarised in Table S4. We reported HPV vaccine acceptability and reasons for not taking HPV vaccine among people across geographical regions (eastern, central and western China). Table S5 summaries socio‐demographic characteristics of the regions in China. The full results from each study, including stratification by rurality, by gender, by population subgroups (i.e., undergraduates, parents and medical providers) were summarised in supplementary materials, grouped according to whether studies presented acceptability for oneself, or for a daughter or son, willingness to pay for the HPV vaccine by price ranges, and the reasons for not accepting the HPV vaccine. We used box plots to describe regional variation. For each region, we presented summary figures (the median with the first quantile and the third quantile) showing the acceptability of the HPV vaccine by rural/urban residence, and gender. For studies reporting results on reasons to accept or decline the HPV vaccine, we extracted the exact wording of reasons from English language papers and translated the wording of reasons into English from Chinese language papers and then summarised the results by multiple/single choice answers, populations and region. There was sufficient similarity in wording across studies to allow collation and comparison of findings. For studies reporting results of acceptability variation by the price of the vaccine, we extracted data that provided the acceptability by price ranges (i.e., under 15.3(¥100), 15.3–45.9(¥300), 45.9–76.5 (¥500), 76.5–153(¥1,000), and over 153 US dollars), grouping data by the lowest threshold of paying for the HPV vaccine (<3.06(¥20), <7.65(¥50), <15.3, <45.9, <76.5 US dollars), and summarised the results by the most commonly used price range (>15.3, >153 US dollars). For studies exploring acceptability of domestic versus imported vaccines, we summarised the result by the most commonly used price range (<76.5, >76.5 US dollars).
The protocol of this study is registered with PROSPERO, number CRD42018085894. R software (version 3.5.2; https://www.r-project.org/) was used for descriptive analysis.
3. RESULTS
3.1. Characteristics of included studies
A total of 1062 records from Chinese language and 266 from English language searches were identified. Seventy‐three studies (56 Chinese language and 17 English language), covering 24 provincial regions across mainland China and presenting data for 110,754 individuals, were selected for inclusion in the review (Figure 1).
The characteristics and results of the studies are summarised in Tables 1 and S6. All 73 included studies used a cross‐sectional survey approach. The median sample size was 757 participants (range 104–13,024), with the majority of studies (73, 80.2%) having less than 2000 participants. Articles were published from 2007 to 2017. Many studies examined multiple topics including awareness of HPV, and understanding of the HPV vaccine. We report on acceptability, and barriers influencing acceptability of the vaccine.
TABLE 1.
Characteristics of included studies
| Study | Region | Study setting | People | Sex |
|---|---|---|---|---|
| Feng SW 2010 (S. Feng et al., 2012) | Eastern | Rural/urban hospital | Rural/urban women outpatients | Female |
| Hong Y, 2013 (Hong et al., 2013) | Eastern | Community | Female sex workers | Female |
| Zhao FH, 2012 (F. H. Zhao et al., 2012) | Mixed | Urban/rural hospital | General population, government officials and healthcare providers | Mixed |
| Zhou YQ 2016 (Y. Q. Zhou, Yang, & Wu, 2016b) | Eastern | Urban hospital | Healthcare providers | Female |
| Ma D 2012 (X. J. Ma, Meng, et al., 2013b) | Eastern | Urban hospital | Healthcare providers | Mixed |
| Wang HQ 2011 | Eastern | Urban hospital | Healthcare providers | NA |
| Gao J 2017 (Gao, Zhen, & Liu, 2017a) | Central | Urban community | Healthcare providers | NA |
| Li J 2011(J. Li, 2011) | Eastern | Rural/urban hospital | Healthcare providers and government officials | Mixed |
| Fu CJ, 2014(Fu et al., 2014) | Western | Medical university | Medical students | Mixed |
| Ma D 2013 (D. Ma, Wei, et al., 2013a) | Eastern | College | Medical students | Mixed |
| Gu C, 2015 (Gu et al., 2015) | Central | Medical university | Medical students | Female |
| Pan XF, 2014 (Pan et al., 2014) | Western | Medical university | Medical students | Mixed |
| Zou H, 2016 (Zou, Meng, et al., 2016a) | Eastern | Sexual health clinic | Men | Male |
| Zhang YY 2016 (Y. Y. Zhang, 2016) | Eastern | School | Parents of children | Female |
| Zhang SK, 2015 (S. K. Zhang et al., 2015) | Mixed | Middle school, junior | Parents of teenagers | Mixed |
| Hu HS 2014 (Hu, Ren, et al., 2014a) | Eastern | Middle school | Parents of teenagers | Mixed |
| Zhang H 2014 (H. Zhang, Yu, et al., 2014a) | Central | School | Parents of teenagers | Mixed |
| Wang W, 2015 (W. Wang, Ma, et al., 2015b) | Eastern | Middle school, junior | Parents of teenagers | Mixed |
| Yu Y, 2016 (Y. Yu et al., 2016) | Eastern | High school, primary, junior, senior | Parents of teenagers | Female |
| Yan J 2013 (J. Yan et al., 2013) | Western | Rural community | Rural adult women | Female |
| Ye JR 2011 (Ye, 2011) | Eastern | Rural community | Rural adult women | Female |
| Zhang XX 2014 (X. X. Zhang, Zhao, et al., 2014c) | Eastern | Rural hospital | Rural adult women | Female |
| Cheng Y 2017 (Cheng et al., 2017) | Central | Rural community | Rural adult women | Female |
| Song D 2007 (Song, 2007) | Central | Rural community | Rural adult women | Female |
| Li J, 2015 (J. Li et al., 2015) | Central | Villages | Rural adult women | Female |
| Yu J 2013 (J. Yu et al., 2013) | Western | Rural/urban community | Rural adult women, government officials and healthcare providers | Mixed |
| Wang XM 2012 (X. M. Wang et al., 2012) | Central | Rural community/urban hospital | Rural women residents/urban women outpatients | Female |
| Cui B 2010 (Cui, 2010) | Eastern | Rural community/urban hospital | Rural women/urban women patients | Female |
| Xue L, 2018 (L. Xue et al., 2018) | Eastern | Middle school, junior | Teenagers | Mixed |
| Wang SM, 2014 (S. M. Wang, Zhang, et al., 2014a) | Mixed | University | Undergraduate students | Mixed |
| Zeng XM 2015 (Zeng et al., 2015) | Eastern | College | Undergraduate students | Mixed |
| He X 2010 (X. He et al., 2010) | Central | College | Undergraduate students | Mixed |
| Zhu YR 2017 (Y. R. Zhu et al., 2017) | Central | College | Undergraduate students | Mixed |
| Zhou Y 2012 (Y. Zhou et al., 2012) | Central | College | Undergraduate students | Mixed |
| Gong FQ 2014 (Gong, 2014) | Eastern | College | Undergraduate students | Mixed |
| Xu J 2014 (Xu & Li, 2014) | Western | College | Undergraduate students | Mixed |
| Yang J 2016 (J. Yang et al., 2016) | Western | College | Undergraduate students | Female |
| Zou H, 2016 (Zou, Wang, et al., 2016b) | Eastern | University | Undergraduate students | Mixed |
| Huang H 2013 (H. Huang et al., 2013) | Western | College | Undergraduate students | Mixed |
| Liu RJ 2017 (R. J. Liu et al., 2017) | Eastern | College | Undergraduate students | Mixed |
| Li M 2013 (M. Li et al., 2013) | Eastern | NA | Undergraduate students and parents of teenagers | Mixed |
| Liu Q 2015 (Q. Liu et al., 2015) | Central | College | Undergraduate students and parents of teenagers | Mixed |
| Lu J 2016 (Lu et al., 2016) | Eastern | College/urban community/hospital | Undergraduate students/government/HCPs | Mixed |
| Tian T 2017 (Tian, 2017) | Western | NA | Urban adult men | Male |
| Zhu JH 2016 (J. H. Zhu et al., 2016) | Eastern | Urban CDC | Urban adult men | Male |
| Huang YH 2014 (Y. H. Huang et al., 2014) | Eastern | Urban community | Urban adult men and women | Mixed |
| Li J 2008 (J. Li et al., 2009) | Eastern | Urban community | Urban adult women | Female |
| Zhang SK 2014 (S. K. Zhang, Huang, et al., 2014b) | Mixed | NA | Urban adult women | Female |
| Lei JH 2015 (Lei & Zhong, 2015) | Eastern | Urban hospital | Urban adult women | Female |
| Meng LP 2015 (Meng et al., 2015) | Eastern | Urban community | Urban adult women | Female |
| Yang GQ 2013 (G. Q. Yang et al., 2013) | Eastern | Urban hospital | Urban adult women | Female |
| Zhou YQ 2016 (Y. Q. Zhou, Yang, & Wu, 2016b) | Eastern | Urban community | Urban adult women | Female |
| Ran LM 2014 (Ran et al., 2014) | Western | Urban hospital | Urban adult women | Female |
| Liu XW 2016 (X. W. Liu et al., 2016) | Eastern | Urban hospital | Urban adult women | Female |
| Ma XJ 2013 (X. J. Ma, Meng, et al., 2013b) | Eastern | Urban hospital | Urban adult women | Female |
| Zhao DJ 2010 (D. J. Zhao et al., 2010) | Eastern | Urban community | Urban adult women | Female |
| Shao SJ 2013 (Shao et al., 2013) | Eastern | Urban hospital | Urban adult women | Female |
| Hu SY, 2011 (S. Y. Hu et al., 2011) | Eastern | Rural (Binhai), suburban (Jintan) and urban (Xuzhou) | Urban and rural women | Female |
| Li J, 2009 (J. Li et al., 2009) | Mixed | Urban community cluster and rural areas | Urban and rural women | Female |
| Feng S, 2012 (S. Feng et al., 2012) | Eastern | Urban/rural hospital | Urban and rural women | Female |
| Wu Y 2011 (Wu, 2011) | Eastern | NA | Urban women adults | Female |
| Chang IJ, 2013 (Chang et al., 2013) | Mixed | Companies and universities | Urban women and undergraduate students | Female |
| He M 2011 (M. He et al., 2011) | Mixed | Urban hospital | Urban women outpatients/urban hps | Female |
| Xiao W 2010 (Xiao & Bian, 2009) | Eastern | Urban hospital | Urban women patients | Female |
| Huang GF 2011 (G. F. Huang, 2011) | Eastern | Urban hospital | Urban women patients | Female |
| Xie WL 2015 (Xie et al., 2015) | Central | Urban hospital | Urban women patients | Female |
| Fan BJ 2009 (Fan, 2009) | Eastern | Urban hospital | Urban women patients | Female |
| Su Q 2016 (Su et al., 2016) | Western | Urban hospital | Urban women patients | Female |
| Wang X 2014 (X. Wang, Lei, et al., 2014b) | Western | Urban hospital | Urban women patients | Female |
| Zhu QY 2015 (Q. Y. Zhu et al., 2015) | Eastern | Urban hospital | Urban women patients | Female |
| Fatima 2014 (Fatima, 2014) | Western | Rural community | Uyghur rural adult women | Female |
| Ren CL 2011 (C. L. Ren et al., 2011) | Western | NA | Uyghur/Hui/Han women adults | Female |
| Wang L 2015 (L. Wang, Ouyang, & Wang, 2015a) | Central | Urban hospital | Medical students | Female |
3.1.1. Geographical distribution
Of the 73 studies, the majority (40) were conducted in eastern China (Guangdong, Beijing, Hebei, Zhejiang, Liaoning, Shandong, Shanghai, Tianjin and Jiangsu), 13 studies in western China (Xinjiang, Yunnan, Chongqing, Shaanxi, Gansu, Inner Mongolia, Guizhou and Sichuan) and 13 in central China (Hunan, Jiangxi, Shanxi, Hubei and Henan). Seven studies were multicenter, recruiting participants across two or three regions of China. Publications from three areas—Beijing, Guangdong and Zhejiang—predominated (27 in total) (Figure 2).
FIGURE 2.
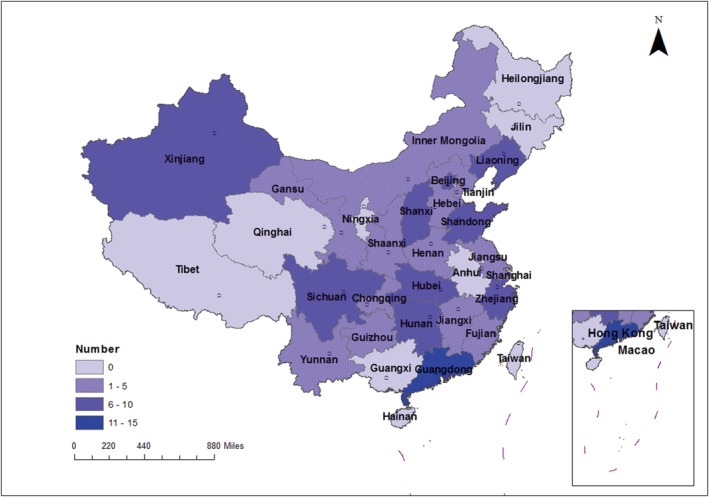
Map of mainland China, showing the number of studies in each province and region
3.1.2. Study participants
The majority of studies (39 in total) were conducted among adult women, 20 among undergraduate students, seven among parents of teenagers, six among healthcare providers, four among adult men, two among Uyghur people and one among teenagers (aged 11–18 years). Studies examining the views of ethnic minority groups (Uyghur, Mongolian and Hui peoples) were only found from western China (Tables 1 and S6). Most studies (38) were undertaken in urban areas, with 10 in rural areas, and 9 in both urban and rural areas (Table S7).
3.2. Quality of included studies
Overall, 23 studies were of ‘good’ quality, 50 were ‘fair’ and 14 were ‘low’ (Table S3). Low quality studies were excluded from data synthesis. Studies carried out in western China were more likely to be of lower quality whereas those reporting data from eastern China were more likely to clearly describe the study population, outcomes, statistical tests and study instruments. Full details are available in Tables S3 and S4.
3.3. Acceptability of the HPV vaccine
Fifty‐eight studies assessed the level of acceptability of the HPV vaccine. Acceptability of HPV vaccine was generally defined as the proportion of people willing to have HPV vaccine.
The overall median rate of acceptability of the HPV vaccine was 71.8% (Q1‐Q3: 58.6%–81%). Regional variation was observed: studies from western China reported a higher acceptability (median: 84.7%, Q1–Q3: 74.3%–94.1%) compared with those from eastern China (median: 68.4%, Q1–Q3: 56.8%–76.4%) and central China (median: 59.9%, Q1–Q3: 50.6%–75.5%) (Figure 3). In 52 of 58 studies, the acceptability of the HPV vaccine was over 50% (Table S7). Ten studies reported over 80% baseline acceptability of HPV vaccine (Fan, 2009; Fatima, 2014; Fu et al., 2014; He et al., 2011; Liu et al., 2016; Ren et al., 2011; Tian, 2017; Yan et al., 2013; Zhao et al., 2012). In contrast, eight studies from eastern China reported low levels of acceptability of HPV vaccine (less than 40% willingness) (Hong et al., 2013; Hu, Ren, et al., 2014a; Ma et al., 2012; Ma, Meng, et al., 2013b; Y. Yu et al., 2016; S. K. Zhang et al., 2015; Y. Y. Zhang, 2016; Zou, Meng, et al., 2016a) across various population groups including female sex workers (Hong et al., 2013), healthcare providers (D. Ma et al., 2012), parents of teenagers (Y. Yu et al., 2016; S. K. Zhang et al., 2015; Y. Y. Zhang, 2016) and urban men (Y. H. Huang et al., 2014; Zou, Meng, et al., 2016a) and women (Ma, Meng, et al., 2013b). For example, Yu et al. (2016), Zhang (2016) and Ma, Meng, et al. (2013b) found that 24.7%–33% of respondents indicated that they would be willing to take the HPV vaccine in urban and rural areas of Shandong and Fujian. Ma et al. (2012) found that 25%–37% healthcare providers in urban Hebei indicated a willingness to accept the vaccine. Zhang et al. (2015) found low overall intention of accepting the HPV vaccine (36.2%) in seven provinces in both western and eastern China: however, it is not possible to disaggregate the results by region (S. K. Zhang et al., 2015) (Table S7).
FIGURE 3.
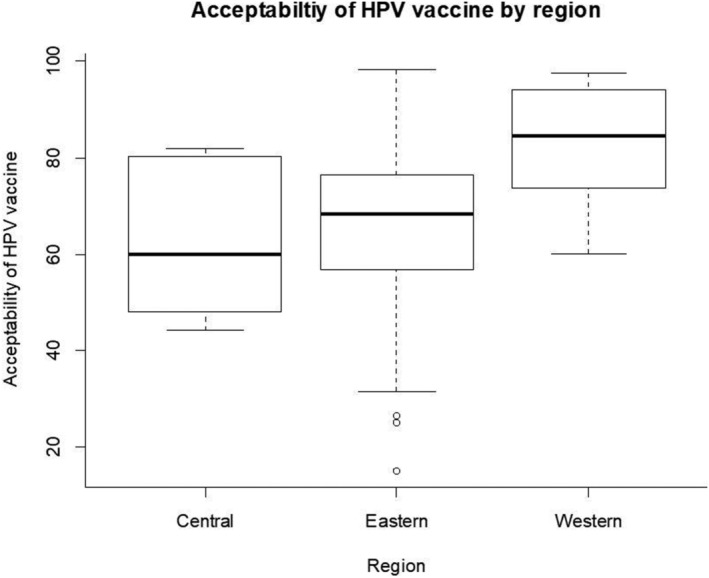
Acceptability of human papillomavirus (HPV) vaccine by region
When taking account of rurality and regional location, the largest differences in acceptability were observed between rural western and urban eastern groups. For example, Fatima (2014), Yan et al. (2013) and Yu et al. (2013) reported high levels of acceptability of HPV vaccine (exceeding 90%) in rural western China, whereas Yu Y 2016, Zhang YY 2016 and Ma XJ 2013 reported levels of acceptability of HPV vaccine of no more than 35% in urban eastern China (Table S7).
Five studies (Fatima, 2014; Fu et al., 2014; Y. H. Huang et al., 2014; Wang, Zhang, et al., 2014a; L. Xue et al., 2018) stratified level of acceptability of the HPV vaccine by gender. In each study, the authors found women were more likely to express a willingness to be vaccinated than men. Two studies among undergraduates found that 73.2%–87.5% of females and 68.3%–81.8% of males would accept the HPV vaccine (Fu et al., 2014; Wang, Zhang, et al., 2014a) (Table S7).
Twenty‐five studies assessed the level of parental acceptability of the HPV vaccine for a child (Chang et al., 2013; Cui, 2010; Fan, 2009; Fatima, 2014; Fen, 2010; M. He et al., 2011; Hong et al., 2013; Hu, Ren, et al., 2014a; Lei & Zhong, 2015; J. Li, 2011; J. Li et al., 2015; J. Li et al., 2009; M. Li et al., 2013; D. Ma et al., 2012; Pan et al., 2014; C. L. Ren et al., 2011; Su et al., 2016; Wang, Ma, et al., 2015b; Xiao & Bian, 2009; Xie et al., 2015; Zhang, Yu, et al., 2014a; Zhang, Huang, et al., 2014b; S. K. Zhang et al., 2015; Y. Y. Zhang, 2016; Zhao et al., 2010; F. H. Zhao et al., 2012; Zhou, Fan, et al., 2016a; Zou, Wang, et al., 2016b). The majority of studies (19 of 25) reported levels of acceptability of the HPV vaccine for either a daughter or a son exceeded 50%. Seven studies (Fan, 2009; Fatima, 2014; M. He et al., 2011; J. Li, 2011; J. Li et al., 2015; J. Li et al., 2009; C. L. Ren et al., 2011) reported high levels of acceptability of the HPV vaccine (over 80% acceptability). However, it is important to note that many of these studies (19 of 25) were carried out among health care providers, gynaecology patients, or undergraduates, with respondents having either adult daughters or sons, or no children at present. Only six studies were carried out among parents of teenagers: among these studies, the level of acceptability of the HPV vaccine was lower, ranging from 8.2% to 42.8%; (Hu, Ren, et al., 2014a; M. Li et al., 2013; Wang, Ma, et al., 2015b; H. Zhang, Yu, et al., 2014a; S. K. Zhang et al., 2015; Y. Y. Zhang, 2016). One study in Fujian(Y. Y. Zhang, 2016) reported a higher acceptability of 58% for their daughters (Table S8).
3.4. Barriers to uptake of the HPV vaccine
Studies reporting barriers affecting the acceptability of HPV vaccine are summarised in Table S9. The four most commonly reported barriers to HPV vaccine acceptance were concerns about vaccine safety, questions regarding vaccine effectiveness, low perceived risk of cervical cancer, and the price of the vaccine.
Thirty‐seven studies reported the reasons people would not be willing to accept the HPV vaccine (Table S10). In general, the level of concerns about vaccine varied widely across different populations and regions. Undergraduates (Gong, 2014; Gu et al., 2015; H. Huang et al., 2013; Lu et al., 2016; Pan et al., 2014; Zeng et al., 2015; Zou, Wang, et al., 2016b), parents of teenagers (Chang et al., 2013; Hu, Ren, et al., 2014a; W. Wang, Ma, et al., 2015b; Y. Yu et al., 2016; H. Zhang, Yu, et al., 2014a; S. K. Zhang, Huang, et al., 2014b) and urban adult women (Chang et al., 2013; Cui, 2010; Fan, 2009; S. Feng et al., 2012; M. He et al., 2011; Y. H. Huang et al., 2014; Lei & Zhong, 2015; X. W. Liu et al., 2016; Wu, 2011; S. K. Zhang, Huang, et al., 2014b; D. J. Zhao et al., 2010; F. H. Zhao et al., 2012) reported high levels of worry about vaccine safety, concerns about the vaccine's effectiveness and concerns that the vaccine has not been widely used in China. Higher levels of worry about the vaccine's safety were found among undergraduates (Zou, Wang, et al., 2016b) in Shandong and by Gong FQ 2014(Gong, 2014) in Liaoning (83.3% and 92.1% respectively). Two studies (H. Huang et al., 2013, and Chang et al., 2013) reported lower rates (57.5% and 58.3% respectively), with lower rates among male undergraduates (safety: male vs. female: 49.3% vs. 67.7%; effectiveness: male vs. female: 19.7% vs. 36.5%) (H. Huang et al., 2013). However, other studies reported inconsistent gender differences (Fu et al., 2014; Pan et al., 2014; Zou, Wang, et al., 2016b) (Table S10). Parents of teenagers (Hu, Ren, et al., 2014a; W. Wang, Ma, et al., 2015b; Y. Yu et al., 2016; H. Zhang, Yu, et al., 2014a; S. K. Zhang et al., 2015) also reported high levels of concern about the vaccine's safety and the rates varied less widely from 62.4% to 78.2%; these studies were from urban areas of seven provinces. Zhang SK (S. K. Zhang et al., 2015) noted that mothers worried more than fathers about the vaccine's safety (67.9% vs. 62.4%), but this gender difference in parental attitudes was not reported in other studies (Table S11).
Patterns of concerns about HPV vaccine among rural adult women were inconsistent and differed from other populations. Of the eight studies exploring attitudes among rural women (Cui, 2010; Cheng et al., 2017; Fatima, 2014; S. Feng et al., 2012; J. Li et al., 2009; Song, 2007; J. Yan et al., 2013; F. H. Zhao et al., 2012), five (Cui, 2010; Fatima, 2014; J. Li et al., 2015; Song, 2007; J. Yan et al., 2013) reported an unwillingness based on a low perceived risk of cervical cancer, followed by concerns about the vaccine's safety, and the high price of the vaccine. The levels of perceived low risk for cervical cancer among rural women varied widely across regions: 34.8% in Liaoning (Cui, 2010), 67.8% in Shanxi (Song, 2007), 78.4% in Gansu (J. Yan et al., 2013), 84.3% in Xinjiang (Fatima, 2014) and 31.8% for daughters in Shanxi (J. Li et al., 2015). Two studies (Cheng et al., 2017, and F. H. Zhao et al., 2012) found rural women reported different patterns of concerns about the HPV vaccine in comparison with urban women—the high price of the vaccine was the major concern of rural women, while concerns about the vaccine's safety was more predominant among urban women (Table S10).
3.5. Cost of the HPV vaccine
Twenty‐eight studies examined respondents' willingness to pay for the HPV vaccine. The level of willingness of paying over 100 Chinese yuan (15.3 US dollars) for the HPV vaccine varied widely. Low levels of willingness (range: 6.1%–16.2%) were found in seven studies (Li et al., 2008; Song, 2007; Su et al., 2016; Xiao & Bian, 2009; J. Yang et al., 2016; D. J. Zhao et al., 2010): three (range: 7.8%–16.2%) in the western region (two in Shaanxi (Su et al., 2016; J. Yang et al., 2016), one in Xinjiang (Fatima, 2014)) with the lowest threshold of paying less than 50 Chinese yuan (7.65 US dollars); four (6.1%–15.8%) published before 2010 (J. Li et al., 2008; Song, 2007; Xiao & Bian, 2009; D. J. Zhao et al., 2010) with the lowest threshold of paying less than 20 Chinese yuan (3.06 US dollars). Higher rates (19.2%–51.1%) of willingness of paying over 100 Chinese yuan (15.3 US dollars) were found in the other three studies in central and eastern regions (two in Hebei (X. W. Liu et al., 2016; D. Ma et al., 2012), one in Shanxi (X. M. Wang et al., 2012)), published after 2010 with the lowest threshold of paying less than 50 Chinese yuan (7.65 US dollars) (Table S12).
For the willingness of paying over 1,000 Chinese yuan (153 US dollars) for the HPV vaccine, all (Fu et al., 2014; H. Huang et al., 2013; W. Wang, Ma, et al., 2015b; Wu, 2011; Y. Y. Zhang, 2016; Zou, Wang, et al., 2016b) but two (Lu et al., 2016; Y. R. Zhu et al., 2017) reported very low levels of willingness: less than 7% people (range: 2.0%–6.5%) would be willing to pay over 1000 Chinese yuan (153 US dollars) for the HPV vaccine. The exceptions were undergraduates in Hunan where the level of willingness to pay over 1000 Chinese yuan (153 US dollars) ranged from 8.2% to 17.7% for domestic and 38.1%–41.4% for imported vaccines.(Y. R. Zhu et al., 2017). Another study, health providers and government officials (Lu et al., 2016) in Shanghai also reported acceptability of a high cost (Table S12).
Ten studies compared domestic and imported HPV vaccines and found that people would be willing to pay more for imported vaccines (Table S12) (M. He et al., 2011; H. Huang et al., 2013; M. Li et al., 2013; Lu et al., 2016; Pan et al., 2014; Wang, Zhang, et al., 2014a; W. Wang, Ma, et al., 2015b; J. H. Zhu et al., 2016; Y. R. Zhu et al., 2017; Zou, Wang, et al., 2016b). For example, Zhu YR 2017(Y. R. Zhu et al., 2017) found that if the vaccine was less than 500 Chinese yuan (76.5 US dollars), 27.2% versus 62.8% of undergraduates were willing to pay for imported and domestic vaccines respectively, but if the vaccine was over 1000 Chinese yuan (153 US dollars), the willingness increased to 39.8% for imported vaccines and dropped to 12.6% for domestic ones. Zhu JH 2016 (J. H. Zhu et al., 2016) reported the acceptable price for imported HPV vaccine was 755 Chinese yuan (115.5 US dollars) but 604 Chinese yuan (92.4 US dollars) for domestic vaccine.
4. DISCUSSION
This review explored the acceptability of and attitudes towards HPV vaccine among 110,754 Chinese people living in 24 provinces across mainland China, from 73 included studies, from both the Chinese‐ and English‐ language literature. The acceptability of and barriers to HPV vaccination vary across regions (eastern, central and western) and different demographic populations in China. The most common barriers affecting acceptability of the HPV vaccine include concerns about the vaccine's safety, effectiveness, price and an individual's perceived risk.
Compared with a previous systematic review(Y. Zhang et al., 2016), we have reported variation of acceptability of the HPV vaccine by region, different populations and by price range. Zhang et al published a meta‐analysis of 58 studies in Mainland China in 2016, showing a pooled willingness to take the HPV vaccine of 67.25% of studies' participants—very close to our overall estimate. However, comparison should be made with caution given the differences in inclusion criteria. In our review, low levels of acceptability of the HPV vaccine were most commonly found in eastern China irrespective of population groups, while studies from western China showed much higher acceptance levels. When rurality is considered, participants from rural western regions had nearly three times the level of HPV vaccine acceptability compared to urban eastern people (who are mostly better‐educated and with higher income) (Table S5). This finding was consistent with Liu et al.'s research who found that people who were ‘relatively well‐educated, had higher incomes and lived in urban areas’ had more vaccine hesitancy (D. Hu et al., 2020). Papers published since 2017 report similar or contradictory findings. Wagner AL (Wagner et al., 2019) and Lin Y (Lin et al., 2019) reported similar findings—people in low and middle‐income regions were less vaccine hesitant and had fewer safety concerns than people in high‐income regions of China. However, this contrasts with You D's finding that low level of willingness was found in lower income groups and rural residents in central and western regions of China (You et al., 2020). However, we also noted variations in reasons for concern about HPV vaccine among different populations. Vaccine safely was the greatest concern raised by urban women, and those in the eastern provinces.
Interpretation of our findings should take into account different immunisation services in respective populations and regions (Hu, Ren, et al., 2014a; W. Wang, Ma, et al., 2015b; Y. Yu et al., 2016). For example, eastern China, including Guangdong and Shandong, should consider providing a focus of health education on the vaccine's safety particularly to parents; while provinces in western China such as Xinjiang and Gansu should consider subsidising part of the cost of the vaccine, or initiate a two‐dose instead of a three‐dose schedule to reduce the cost. Overall, there is little research on the relationship between vaccine acceptability and socio‐economic status in China; therefore, the findings should be interpreted according to the specific context.
Additionally, many studies did not take account of vaccine price in examining the overall acceptability of HPV vaccine, and results may reflect an expectation that the vaccine would be free of charge. In those studies that did include price, the level of acceptability was 6.1%–51.1% if the price was over 15.3 US dollars, lower (6.1%–16.2%) in people in Shaanxi (Su et al., 2016; J. Yang et al., 2016) and Xinjiang (Fatima, 2014), particular lower (2%–6.5%) (Fu et al., 2014; H. Huang et al., 2013; W. Wang, Ma, et al., 2015b; Wu, 2011; Y. Y. Zhang, 2016) if the vaccine's price was over 153 US dollars—but the price was still much lower than the market price in China (Yin, 2017). A similar downward trend was shown in a study based in Hong Kong (Z. Wang et al., 2018), where acceptability dropped to 14.9%–27.4% from 51.6%–63.0% if the vaccine was at a market price. Moreover, we found that when the vaccine price was over 76.5 US dollars, Chinese people preferred to pay more for imported vaccines than domestic ones (Figure 4). This is a common cost threshold in a number of Chinese studies which is close to the cost‐effective price per vaccinated woman (≤$50 [¥350]) suggested by Levin CE (Levin et al., 2015). However, in China, the imported HPV vaccine costs as much as $271–571 (¥1806–4,000) (Cao, 2020; Yin, 2017 ), compared to $94–170 (¥658–987) for the domestic HPV vaccine (Cecolin) (Cao, 2020). This gap between the acceptable or cost‐effective price, and the real cost, highlights the need for strategies to reduce the HPV vaccine cost, particularly in rural areas and less resourced provinces.
FIGURE 4.
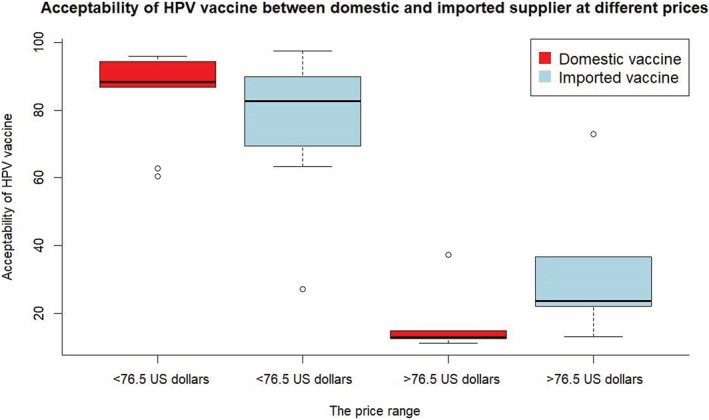
Acceptability of human papillomavirus (HPV) vaccine between domestic and imported supplier at different prices
Economic development varies within each region/province and may contribute to the variation in HPV vaccine acceptability. In addition, the respective region/province's vaccine safety history must be taken into account (R. T. Yang et al., 2014). HPV vaccine safety events in Shenzhen (Guangdong) in 2013 (R. T. Yang et al., 2014), in Shandong in 2016, and in Changchun Changsheng Biotechnology company in 2018 (D. Hu et al., 2020) led to a public trust crisis, resulting in a decline in the vaccination rate afterwards and documented vaccine hesitancy (D. Hu et al., 2020; X. L. Yan, 2016). Some vaccine safety events were misrepresented (and exaggerated) in the media (R. T. Yang et al., 2014), some arose from lack of supervision and professional management of cold chain logistics (R. T. Yang et al., 2014). That these safety events occurred mostly in eastern provinces may partially explain our findings in this region: the lowest level of acceptability of vaccine and high levels of worries about the vaccine's safety were in eastern China (a more affluent region). Well educated people and those on higher incomes (female undergraduates and parents of teenagers in urban areas) were groups with the most hesitancy. Similarly, Liu et al. reported people who were ‘relatively well‐educated, had higher incomes and lived in urban areas’ had more vaccine hesitancy(D. Hu et al., 2020). However, we note that information on the vaccine's safety and effectiveness may not have been available to parents of teenagers in studies from western China, and there is a need to investigate whether the safety incidents will affect acceptability of HPV vaccine in the long term. At present, concerns about vaccine safety are relatively limited, and better public understanding of the HPV vaccine (including evidence of effectiveness, safety profile, informing health care providers of health status prior to vaccination), is needed, particularly in eastern China (e.g., Shandong and Guangdong). Public health officials should provide transparent evidence‐based information following any vaccine scares and tailor public health messages to individuals with different education levels.
Our study was comprehensive and systematic, but did have some limitations. Firstly, we focused our analysis on regional variations across China because government policy or national programmes are mostly frequently launched or located by region and province: the three regions themselves represent socio‐economic inequalities because they were originally divided based on disparities in economic progress (Gao, Zhou, et al., 2017b). However, region‐level data are crude, and variation within region based on rurality and sex could not always be assessed because of lack of data on these subgroups in the included studies. Secondly, we used median, first quantile and third quantile for our estimates of regional level of acceptability because studies are heterogeneous in population groups. Median, first, and third quantiles are not weighted by sample size, and region‐level data require cautious interpretation. However, our review was carried out according to PRISMA guidance, following a registered protocol and assessing the quality using modified quality assessment criteria. Most of the studies included in this review used quantitative study designs with robust sample sizes. Additionally, comparable results among subpopulations and regions were observed. Thus, this review provides a valid summary of the existing evidence on acceptability of and attitudes towards HPV vaccine in China. We recognise that there was no common definition of the term ‘effectiveness’ in the included studies; we list the wording used (in English and Chinese) in Table S9. Finally, studies since 2017 were not included in the systematic review, but we have compared findings in contemporary literature published since 2017 with our findings.
5. CONCLUSIONS AND IMPLICATIONS
To our knowledge, this is the first and most comprehensive systematic review to explore regional and demographic variations in acceptability of HPV vaccine in China and our review highlights important differences in willingness and barriers to accept the HPV vaccine between different populations and regions of China. Our findings indicate that barriers affecting the willingness to take HPV vaccine are complex, involving multiple factors. Overall, for rural women, particularly in western regions, low perceived risk of cervical cancer and the high vaccine price were the most prominent barriers, while for undergraduates and parents of teenagers in urban areas, particularly in the eastern region, the major concerns were the safety and effectiveness of the HPV vaccine.
Our review highlights potential strategies for policy makers. It is currently government policy (Cao, 2020; Y. Xue, 2019) that individuals can pay for the HPV vaccine out of pocket or through private or employer insurance (Cao, 2020; Y. Xue, 2019). Subsidising vaccines, particularly for rural western regions, should be considered. Moreover, high rates of HPV vaccination coverage are necessary to achieve global targets for elimination (four or fewer cases per 100,000 women‐years). Elimination rates will be much lower if only screening and treatment are used without vaccination (Brisson et al., 2020; Canfell et al., 2020). Our findings may help inform policy in other regions and populations that have not yet been included in academic studies, although we recommend that research in these provinces and communities is carried out.
FUNDING INFORMATION
This work was carried out in part during Du Wang's PhD studies at the University of Edinburgh, supported by a University of Edinburgh Global Research Scholarship.
CONFLICT OF INTEREST
All authors declared no conflicts of interests. The funder of the study had no role in the study design, data collection, data analysis, data interpretation or writing of the report. The corresponding authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Supporting information
Table S1. Search strategies for English‐ and Chinese‐ language databases
Table S2. Quality assessment tool (items and scores)
Table S3. Quality assessment of included studies
Tables S4. Rationale for undertaking narrative synthesis instead of meta‐analysis
Table S5. Socio‐demographic characteristics in Eastern, Central and Western China
Table S6. Characteristics of included studies
Table S7. Findings of studies reporting acceptability of the HPV vaccine for personal use in mainland China
Table S8. Findings of studies reporting parental acceptability of HPV vaccine for a daughter/son in mainland China
Table S9. Studies reporting barriers affecting the acceptability of HPV vaccine (for personal use).
Table S10. Findings of studies reporting the reasons for not accepting the HPV vaccine for personal use in mainland China
Table S11. Findings of studies reporting parental reasons for accepting the HPV vaccine for their daughter or son in mainland China
Table S12. Findings of studies reporting willingness to pay for HPV vaccine by price ranges in mainland China
ACKNOWLEDGMENT
We would like to thank Yufei Jia for preparing the map.
Wang, D. , Wu, J. , Du, J. , Ong, H. , Tang, B. , Dozier, M. , Weller, D. , & Campbell, C. (2022). Acceptability of and barriers to human papillomavirus vaccination in China: A systematic review of the Chinese and English scientific literature. European Journal of Cancer Care, 31(3), e13566. 10.1111/ecc.13566
Funding information University of Edinburgh Global Research Scholarship, Grant/Award Number: NA
Contributor Information
Du Wang, Email: duwang84@163.com.
Christine Campbell, Email: Christine.Campbell@ed.ac.uk.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Brisson, M. , Kim, J. J. , Canfell, K. , Drolet, M. , Gingras, G. , Burger, E. A. , Martin, D. , Simms, K. T. , Bénard, É. , Boily, M. C. , Sy, S. , Regan, C. , Keane, A. , Caruana, M. , Nguyen, D. T. N. , Smith, M. A. , Laprise, J. F. , Jit, M. , Alary, M. , … Hutubessy, R. (2020). Impact of HPV vaccination and cervical screening on cervical cancer elimination: A comparative modelling analysis in 78 low‐income and lower‐middle‐income countries. Lancet, 395Placeholder Text, 575–590. 10.1016/S0140-6736(20)30068-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruni, L. A. G. , Serrano, B. , Mena, M. , Gómez, D. , Muñoz, J. , Bosch, F. X. , & de Sanjosé, S. (2018). Human papillomavirus and related diseases in China. Retrieved from https://hpvcentre.net/statistics/reports/XWX.pdf
- Bruni, L. A. G. , Serrano, B. , Mena, M. , Gómez, D. , Muñoz, J. , Bosch, F. X. , & de Sanjosé, S. (2019). Human papillomavirus and related diseases in the world. Retrieved from https://hpvcentre.net/statistics/reports/XWX.pdf
- Canfell, K. , Kim, J. J. , Brisson, M. , Keane, A. , Simms, K. T. , Caruana, M. , Burger, E. A. , Martin, D. , Nguyen, D. T. N. , Bénard, É. , Sy, S. , Regan, C. , Drolet, M. , Gingras, G. , Laprise, J. F. , Torode, J. , Smith, M. A. , Fidarova, E. , Trapani, D. , … Hutubessy, R. (2020). Mortality impact of achieving WHO cervical cancer elimination targets: A comparative modelling analysis in 78 low‐income and lower‐middle‐income countries. Lancet, 395Placeholder Text, 591–603. 10.1016/S0140-6736(20)30157-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao, K. (2020). The first domestic HPV vaccine has been produced. Retrieved from http://society.people.com.cn/n1/2020/0103/c1008-31534395.html?scene=2&clicktime=1578120587&enterid=1578120587&from=timeline&isappinstalled=0
- Chang, I. J. , Huang, R. , He, W. , Zhang, S. K. , Wang, S. M. , Zhao, F. H. , Smith, J. S. , & Qiao, Y. L. (2013). Effect of an educational intervention on HPV knowledge and vaccine attitudes among urban employed women and female undergraduate students in China: A cross‐sectional study. BMC Public Health, 13, 916–923. 10.1186/1471-2458-13-916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, W. , Zheng, R. , Baade, P. D. , Zhang, S. , Zeng, H. , Bray, F. , Jemal, A. , Yu, X. Q. , & He, J. (2016). Cancer statistics in China, 2015. CA: A Cancer Journal for Clinicians, 66Placeholder Text, 115–132. 10.3322/caac.21338 [DOI] [PubMed] [Google Scholar]
- Cheng, Y. , Qi, B. , Wu, X. X. , & Pan, M. Z. (2017). Prevalence, subtype distribution of human papillomavirus infection, and vaccination willingness among women in Wuyuan County. Shanghai Journal of Preventive Medicine, 29Placeholder Text, 872‐875, 879. [Google Scholar]
- Cui, B. (2010). The analysis of the awareness of human papillomavirus (HPV) and HPV vaccine and the willingness of vaccination among urban and rural women. (Master Thesis). Dalian Medical University. [Google Scholar]
- Fan, B. J. (2009). Investigation on cervical cancer screening, HPV infection and vaccine awareness among outpatients. (Master Thesis). Liaoning University of Chinese Medicine. [Google Scholar]
- Fatima, M. (2014). Cross‐sectional study on Uyghur cervical cancer in Hotan Karkax County, Xinjiang. (Doctor Thesis). XinJiang Medical University. [Google Scholar]
- Fen, S. W. (2010). Women's knowledge of human papilloma‐virous (HPV) and their attitudes toward HPV vaccine. (Master Thesis). Zhejiang University. [Google Scholar]
- Feng, S. , Xu, X. , Jin, Y. , & Yao, X. (2012). Women's knowledge of human papillomavirus (HPV) and their attitudes toward HPV vaccine: Preparing for HPV vaccination in China. Asia‐Pacific Journal of Public Health, 24Placeholder Text, 522–531. 10.1177/1010539511415838 [DOI] [PubMed] [Google Scholar]
- Fu, C. J. , Pan, X. F. , Zhao, Z. M. , Saheb‐Kashaf, M. , Chen, F. , Wen, Y. Zhong, X. N. (2014). Knowledge, perceptions and acceptability of HPV vaccination among medical students in Chongqing, China, Asian Pac J Cancer Prev, 15Placeholder Text, 6187–6193. 10.7314/APJCP.2014.15.15.6187 [DOI] [PubMed] [Google Scholar]
- Gao, J. , Zhen, Q. , & Liu, L. (2017a). Status of community nurses'cognition on human papillomavirus vaccine. Nursing Research of China, 35, 4558–4559. [Google Scholar]
- Gao, Y. , Zhou, H. , Singh, N. S. , Powell‐Jackson, T. , Nash, S. , Yang, M. , Guo, S. , Fang, H. , Alvarez, M. M. , Liu, X. , Pan, J. , Wang, Y. , & Ronsmans, C. (2017b). Progress and challenges in maternal health in western China: A countdown to 2015 national case study. The Lancet Global Health, 5Placeholder Text, e523‐e536. 10.1016/S2214-109X(17)30100-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong, F. Q. (2014). Cross‐sectional study on the awareness of the HPV and HPV vaccination among non‐medical major university students (master thesis). Dalian Medicine University. [Google Scholar]
- Gu, C. , Niccolai, L. M. , Yang, S. , Wang, X. , & Tao, L. (2015). Human papillomavirus vaccine acceptability among female undergraduate students in China: The role of knowledge and psychosocial factors. Journal of Clinical Nursing, 24Placeholder Text, 2765–2778. 10.1111/jocn.12871 [DOI] [PubMed] [Google Scholar]
- He, X. , Liang, S. C. , Cui, M. C. , Wang, X. L. , & Liu, H. T. (2010). Investigation on consciousness about human papilloma virus and cervical Cancer in college students. Modern Preventive Medicine, 21, 4097–4098. [Google Scholar]
- He, M. , Zhao, F. H. , Hong, Y. , Den, J. H. , & Li, L. Y. (2011). Survey on awareness and attitude towards HPV and HPV vaccination for cervical Cancer prevention among urban women and medical professionals. China Cancer, 20Placeholder Text, 483–488. [Google Scholar]
- Hong, Y. , Zhang, C. , Li, X. , Lin, D. , & Liu, Y. (2013). HPV and cervical cancer related knowledge, awareness and testing behaviors in a community sample of female sex workers in China. BMC Public Health, 13, 696–703. 10.1186/1471-2458-13-696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu, S. Y. , Hong, Y. , Zhao, F. H. , Lewkowitz, A. K. , Chen, F. , Zhang, W. H. , & Qiao, Y. L. (2011). Prevalence of HPV infection and cervical intraepithelial neoplasia and attitudes towards HPV vaccination among Chinese women aged 18‐25 in Jiangsu Province. Chinese Journal of Cancer Research, 23Placeholder Text, 25–32. 10.1007/s11670-011-0025-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu, H. S. L. W. X. , Ren, Z. F. , Zeng, X. M. , Zhao, F. H. , & Qiao, Y. L. (2014a). Investigation on acceptance of HPV vaccination and its determinants among the parents of junior high school students in Guangzhou City. Chinese Journal of Disease Control & Prevention, 07, 659–662. [Google Scholar]
- Hu, S. Y. , Zheng, R. S. , Zhao, F. H. , & Zhang, S. W. (2014b). Trend analysis of cervical cancer incidence and mortality rates in Chinese women during 1989‐2008. Acta Acad Med Sin, 36Placeholder Text, 119–125. [DOI] [PubMed] [Google Scholar]
- Hu, D. , Martin, C. , Dredze, M. , & Broniatowski, D. A. (2020). Chinese social media suggest decreased vaccine acceptance in China: An observational study on Weibo following the 2018 Changchun Changsheng vaccine incident. Vaccine, 38Placeholder Text, 2764–2770. 10.1016/j.vaccine.2020.02.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, G. F. (2011). Analysis of results of 196 cases of cervical human papillomavirus. Maternal and Child Health Care of China, 17, 2598–2599. [Google Scholar]
- Huang, H. , Zhao, F. H. , Xie, Y. , Wang, S. M. , & Pan, X. F. (2013). Knowledge and attitude toward HPV and prophylactic HPV vaccine among college students in Chengdu. Modern Preventive Medicine, 16, 3071–3073+3080. [Google Scholar]
- Huang, Y. H. , Zhen, G. P. , Xiang, Y. , Jiang, Y. H. , & Liu, D. Y. (2014). A research about awareness and acceptance of HPV vaccines degrees in Shenzhen Luohu community. Modern Hospital, 05, 144–146. [Google Scholar]
- Lei, J. H. , & Zhong, K. (2015). Investigation and analysis of the cognition and demand of human papillomavirus vaccine in physical examination population. Chinese General Practice Nursing, 16, 1562–1563. [Google Scholar]
- Levin, C. E. , Sharma, M. , Olson, Z. , Verguet, S. , Shi, J. F. , Wang, S. M. , Qiao, Y. L. , Jamison, D. T. , & Kim, J. J. (2015). An extended cost‐effectiveness analysis of publicly financed HPV vaccination to prevent cervical cancer in China. Vaccine, 33Placeholder Text, 2830–2841. 10.1016/j.vaccine.2015.02.052 [DOI] [PubMed] [Google Scholar]
- Li, J. (2011). The analysis of the awareness of human papillomavirus (HPV) and HPV vaccine among doctors and government officials. (Master Thesis). Dalian Medical University. [Google Scholar]
- Li, J. , Tu, Z. , Zhao, C. , Song, D. , & Wang, H. (2008). An investigation of HPV prevalence among women living in Beijing and their cognition and attitude toward HPV and HPV vaccine. Chinese Cancer, 03, 168–172. [Google Scholar]
- Li, J. , Li, L. K. , Ma, J. F. , Wei, L. H. , Niyazi, M. , Li, C. Q. , Xu, A. D. , Wang, J. B. , Liang, H. , Belinson, J. , & Qiao, Y. L. (2009). Knowledge and attitudes about human papillomavirus (HPV) and HPV vaccines among women living in metropolitan and rural regions of China. Vaccine, 27Placeholder Text, 1210–1215. 10.1016/j.vaccine.2008.12.020 [DOI] [PubMed] [Google Scholar]
- Li, M. , Ju, L. R. , Li, B. L. , Liu, F. , Zhou, J. Y. , & Qi, Q. (2013). Survey of the cognition on human papillomavirus and it's preventive vaccine of junior schoolstudents' parents and university students in Beijing. Chinese Journal of Woman and Child Health Research, 1, 14–17. [Google Scholar]
- Li, J. , Kang, L. N. , Li, B. , Pang, Y. , Huang, R. , & Qiao, Y. L. (2015). Effect of a group educational intervention on rural Chinese women's knowledge and attitudes about human papillomavirus (HPV) and HPV vaccines. BMC Cancer, 15, 691–701. 10.1186/s12885-015-1682-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, Y. , Lin, Z. , He, F. , Hu, Z. , Zimet, G. D. , Alias, H. , & Wong, L. P. (2019). Factors influencing intention to obtain the HPV vaccine and acceptability of 2‐, 4‐ and 9‐valent HPV vaccines: A study of undergraduate female health sciences students in Fujian, China, Vaccine, 37Placeholder Text, 6714–6723. 10.1016/j.vaccine.2019.09.026 [DOI] [PubMed] [Google Scholar]
- Liu, Q. , Xiao, D. L. , Xie, W. L. , & Wan, Y. P. (2015). Investigation on the knowledge of papillomavirus infection in 590 students in vocational colleges and universities. Today Nurse, 05, 158–160. [Google Scholar]
- Liu, X. W. , Zhao, X. Y. , Chen, X. , & Liu, L. (2016). Investigation on cognition and vaccination intention of human papillomavirus vaccine in women with cervical cancer screening. Chinese Journal of Biologicals, 08, 893–896. [Google Scholar]
- Liu, R. J. , Lu, Q. R. , Xia, Y. Y. , & Zhang, J. (2017). Investigation on cognition and attitude of college students to human papillomavirus vaccine in Ningbo. Modern Practical Medicine, 01, 92–94. [Google Scholar]
- Lu, J. , Mou, W. , Zhou, W. Y. , & Jiang, M. B. (2016). Survey of awareness and attitudes of human papilloma virus vaccine among college students, governmental officials and medical staff in Shanghai. Chinese Journal of Vaccines and Immunization, 01, 70–75. [Google Scholar]
- Ma, D. , Qiu, H. , Wang, H. Q. , & Liang, T. M. (2012). Investigation on the cognition and acceptability of medical personnel to human papillomavirus and its vaccine in a hospital of Tangshan city. Maternal and Child Health Care of China., 03, 397–400. [Google Scholar]
- Ma, D. , Wei, Y. , Li, O. , & Wang, W. C. (2013a). Study on medical student knowledge and attitudes regarding HPV and its vaccine. Maternal and Child Health Care of China, 28, 4699–4702. [Google Scholar]
- Ma, X. J. , Meng, X. J. , Dong, J. Y. , Zhang, L. G. , & Zhang, J. (2013b). A study on the cognition and influencing factors of HPV in adult women. Progress in Obstetrics and Gynecology, 06, 491–493. [Google Scholar]
- Meng, L. P. , Li, J. M. , Jia, Y. H. , Liu, Y. W. , & He, X. (2015). Analysis of women's cognition to HPV and HPV vaccine in Bao'an district, Shenzhen City. Journal of Public Health and Preventive Medicine, 05, 54–57. [Google Scholar]
- Moher, D. , Liberati, A. , Tetzlaff, J. , Altman, D. G. , & Group, P . (2009). Preferred reporting items for systematic reviews and meta‐analyses: The PRISMA statement. BMJ, 339, b2535. 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan, X. F. , Zhao, Z. M. , Sun, J. , Chen, F. , Wen, Q. L. , Liu, K. , Song, G. Q. , Zhang, J. J. , Wen, Y. , Fu, C. J. , & Yang, C. X. (2014). Acceptability and correlates of primary and secondary prevention of cervical cancer among medical students in Southwest China: Implications for cancer education. PLoS ONE, 9Placeholder Text, e110353. 10.1371/journal.pone.0110353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan, X. F. , Li, R. , Pan, A. , & Larson, H. (2016). Human papillomavirus vaccine approval in China: A major step forward but challenges ahead. The Lancet Infectious Diseases, 16Placeholder Text, 1322–1323. 10.1016/S1473-3099(16)30450-9 [DOI] [PubMed] [Google Scholar]
- Ran, L. M. , Wang, Y. , Mo, L. , Wu, C. W. , & Zhan, J. (2014). Survey of knowledge awareness on cervical cancer prevention among check‐up women in Guiyang City. Chinese Journal of Health Education, 06, 552–554. [Google Scholar]
- Ren, C. L. , Hou, S. M. , Zhang, S. P. , Hou, Y. H. , & Zhang, S. X. (2011). Knowledge popularization status on cancer in cervix in Han, Hui and Uygur Chinese females in Malan area. Medical Journal of General Equipment Headquarters, 04, 224–226. [Google Scholar]
- Ren, J. , Wagner, A. L. , Zheng, A. , Sun, X. , Boulton, M. L. , Huang, Z. , & Zikmund‐Fisher, B. J. (2018). The demographics of vaccine hesitancy in Shanghai, China, PLoS One, 13Placeholder Text, e0209117. 10.1371/journal.pone.0209117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan, R. , & Cochrane Consumers and Communication Review Group . (2020). Cochrane Consumers and Communication Review Group: data synthesis and analysis. Retrieved from http://cccrg.cochrane.org
- Santhanes, D. , Yong, C. P. , Yap, Y. Y. , Saw, P. S. , Chaiyakunapruk, N. , & Khan, T. M. (2018). Factors influencing intention to obtain the HPV vaccine in south east Asian and Western Pacific regions: A systematic review and meta‐analysis. Scientific Reports, 8Placeholder Text, 3640–3650. 10.1038/s41598-018-21912-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shao, S. J. , Yue, T. F. , & Zhang, L. Q. (2013). HPV infection in female and the cognition about HPV and HPV vaccine. Journal of Tianjin Medical University, 02, 127–130. [Google Scholar]
- Song, D. (2007). Investigation and analysis of (HPV) infection rate and population cognition of HPV vaccine among women in Shanxi Province. (Master Thesis). Dalian Medical University. [Google Scholar]
- Su, Q. , Yang, J. , Cheng, Y. M. , & Xu, L. J. (2016). Knowledge about HPV and HPV vaccine among outpatients in Xi'an city. Chinese Journal of Reproductive Health, 0Placeholder Text, 311–314. [Google Scholar]
- Tian, T. (2017). Investigation on cognition and infection of human papillomavirus in male and male sex population. (Master Thesis). Xinjiang Medical University. [Google Scholar]
- Wagner, A. L. , Masters, N. B. , Domek, G. J. , Mathew, J. L. , Sun, X. , Asturias, E. J. , Boulton, M. L. (2019). Comparisons of vaccine hesitancy across five low‐ and middle‐income countries. Vaccines (Basel), 7Placeholder Text, 155–165. 10.3390/vaccines7040155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, X. M. , Feng, X. X. , Zhai, Y. L. , Wei, C. L. , & Qiao, Y. L. (2012). Cervical cancer screening and acceptance of HPV vaccine in women of Shanxi province. Chinese Journal of Public Health, 05, 650–651. [Google Scholar]
- Wang, S. M. , Zhang, S. K. , Pan, X. F. , Ren, Z. F. , Yang, C. X. , Wang, Z. Z. , Gao, X. H. , Li, M. , Zheng, Q. Q. , Ma, W. , Zhao, F. H. , Qiao, Y. L. , & Sivasubramaniam, P. (2014a). Human papillomavirus vaccine awareness, acceptability, and decision‐making factors among Chinese college students. Asian Pacific Journal of Cancer Prevention, 15Placeholder Text, 3239–3245. 10.7314/APJCP.2014.15.7.3239 [DOI] [PubMed] [Google Scholar]
- Wang, X. , Lei, S. Y. , Zhu, G. H. , Ma, M. , & Zhao, L. L. (2014b). Analysis on cognition and attitude of patients with cervical cancer toward human papilloma virus (HPV)and HPV vaccine. Chinese Nursing Research, 13, 1589–1591. [Google Scholar]
- Wang, L. , Ouyang, Y. Q. , & Wang, X. H. (2015a). Analysis of cognitive status of human papillomavirus and vaccine in 125 nursing students with cervical cancer. Journal of Nursing (China), 17, 47–50. [Google Scholar]
- Wang, W. , Ma, Y. , Wang, X. , Zou, H. , Zhao, F. , Wang, S. , Zhang, S. , Zhao, Y. , Marley, G. , & Ma, W. (2015b). Acceptability of human papillomavirus vaccine among parents of junior middle school students in Jinan, China, VACCINE, 33Placeholder Text, 2570–2576. 10.1016/j.vaccine.2015.04.010 [DOI] [PubMed] [Google Scholar]
- Wang, Z. , Wang, J. , Fang, Y. , Gross, D. L. , Wong, M. C. S. , Wong, E. L. Y. , & Lau, J. T. F. (2018). Parental acceptability of HPV vaccination for boys and girls aged 9‐13years in China—A population‐based study. Vaccine, 36Placeholder Text, 2657–2665. 10.1016/j.vaccine.2018.03.057 [DOI] [PubMed] [Google Scholar]
- Wu, Y. (2011). An investigation of the cognition and reception towards HPV vaccine among women living in Hangzhou. Chinese Preventive Medicine, 04, 321–323. [Google Scholar]
- Xiao, W. , & Bian, M. L. (2009). Women's knowledge, attitudes, and intentional concerning cervical cancer greening and human papillomavirus vaccine. Journal of China‐Japan Friendship Hosptal (02), 79–82. [Google Scholar]
- Xie, W. L. , Zhao, B. X. , Jiang, P. P. , Wang, R. , & Wan, Y. P. (2015). Analysis of cognition and attitude of inpatients on HPV vaccine related knowledge in three grade A hospital in Hengyang city. Chinese Nursing Research, 11, 1373–1375. [Google Scholar]
- Xu, J. , & Li, Y. Q. (2014). The cognition and attitude analysis of human papillomavirus and HPV vaccine in college students. Journal of Youjiang Medical University for Nationalities, 01, 72–73. [Google Scholar]
- Xue, Y . (2019). Knowledge: HPV vaccine. Retrieved from http://www.gov.cn/fuwu/2019-07/17/content_5410452.htm
- Xue, L. , Hu, W. , Zhang, H. , Xie, Z. , Zhang, X. , Zhao, F. , Qiao, Y. , Gao, L. , & Ma, W. (2018). Awareness of and willingness to be vaccinated by human papillomavirus vaccine among junior middle school students in Jinan, China, Hum Vaccin Immunother, 14Placeholder Text, 404–411. 10.1080/21645515.2017.1393132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan, X. L. (2016). Analysis on the development strategy of pharmaceutical cold chain logistics in China from the perspective of “Shandong vaccine incident”.
- Yan, J. , Wang, X. L. , & Wang, X. H. (2013). Survey on cognition of HPV vaccine among women living in high prevalence area of cervical cancer in Gansu Province. Chinese Journal of Health Education, 10, 913–916. [Google Scholar]
- Yang, G. Q. , Wu, Q. X. , Chang, H. O. , Wen, M. Z. , & Lai, X. J. (2013). Study on cognition of women to human papillomavirus infection of genital tract and cervical cancer and the related factors. Maternal & Child Health Care of China, 33, 5515–5516. [Google Scholar]
- Yang, R. T. , Li, G. Q. , & Chen, W. (2014). Investigation and analysis on the influence of Kangtai hepatitis B vaccine incident in Shenzhen on the vaccination behavior of children's parents in Linze County. Bulletin of Disease Control and Prevention, 29 Placeholder Text, 10–12. [Google Scholar]
- Yang, J. , Xu, L. J. , Xu, L. , Yu, M. , Cheng, Y. M. , & Nie, N. (2016). Awareness of HPV and HPV vaccine among non‐medical specialty female college students in Xi'an City. Chinese Journal of Woman and Child Health Research, 08, 923–925. [Google Scholar]
- Ye, J. R. (2011). Investigation and analysis on the knowledge of cervical cancer prevention and treatment among married women in Daling Mountain town of Dongguan City and its countermeasures. Chinese and Foreign Women Health, 09, 350–351. [Google Scholar]
- Yin, Y. (2017). HPV vaccination in China needs to be more cost‐effective. Lancet, 390Placeholder Text, 1735–1736. 10.1016/S0140-6736(17)32606-5 [DOI] [PubMed] [Google Scholar]
- You, D. , Han, L. , Li, L. , Hu, J. , Zimet, G. D. , Alias, H. , Danaee, M. , Cai, L. , Zeng, F. , & Wong, L. P. (2020). Human papillomavirus (HPV) vaccine uptake and the willingness to receive the HPV vaccination among female college students in China: A multicenter study. Vaccines (Basel), 8Placeholder Text, 31–50. 10.3390/vaccines8010031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu, J. , Yang, H. Y. , Yan, Z. L. , & Tan, X. J. (2013). The survey on female sexuality and HPV awareness in Linxiang district of Yunnan province. Chongqing Medicine, 29, 3532–3533+3561. [Google Scholar]
- Yu, Y. , Xu, M. , Sun, J. , Li, R. , Li, M. , Wang, J. , Zhang, D. , & Xu, A. (2016). Human Papillomavirus Infection and Vaccination: Awareness and Knowledge of HPV and Acceptability of HPV Vaccine among Mothers of Teenage Daughters in Weihai, Shandong, China, PLoS 1, 11Placeholder Text, e0146741. 10.1371/journal.pone.0146741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaza, S. , Wright‐De Aguero, L. K. , Briss, P. A. , Truman, B. I. , Hopkins, D. P. , Hennessy, M. H. , & Pappaioanou, M. (2000). Data collection instrument and procedure for systematic reviews in the guide to community preventive services. Task force on community preventive services. American Journal of Preventive Medicine, 18Placeholder Text, 44–74. 10.1016/S0749-3797(99)00122-1 [DOI] [PubMed] [Google Scholar]
- Zeng, X. , Ren, Z. F. , Wei, X. , Lin, W. , & Qiao, Y. (2015). Knowledge and attitude of the students in Sun Yat‐sen University regarding human papillomavirus and its vaccine. Modern Preventive Medicine, 10, 1822–1825. [Google Scholar]
- Zhang, Y. Y. (2016). Study on preventive behavior of cervical cancer based on health belief model. (Master Thesis), Xiamen University. Retrieved from http://d.g.wanfangdata.com.cn/Thesis_Y3026200.aspx
- Zhang, H. , Yu, D. X. , Liu, C. X. , Wang, S. M. , Xiao, Y. , Peng, Y. H. , & Wang, Z. Z. (2014a). Parental acceptance of junior high school students for human papillomavirus vaccination: A survey at one school in Wuhan. Journal of Public Health and Preventive Medicine, 01, 49–52. [Google Scholar]
- Zhang, S. K. , Huang, R. , Wang, S. M. , Zhao, F. H. , & Qiao, Y. L. (2014b). Investigation of knowledge and acceptability of human papillomavirus vaccine and assessment of health education among employed urban women in China. Cancer Research and Clinic, 2, 114–117. [Google Scholar]
- Zhang, X. X. , Zhao, C. , Cui, S. H. , Zhao, Y. , Bi, X. Q. , Zhao, L. J. , & Wei, L. H. (2014c). An investigation of HPV prevalence among women living in Fengning of Hebei Province and their awareness toward knowledge of HPV and HPV vaccine. Chinese Journal of Clinical Obstetrics and Gynecology, 04, 318–321. [Google Scholar]
- Zhang, S. K. , Pan, X. F. , Wang, S. M. , Yang, C. X. , Gao, X. H. , Wang, Z. Z. , Li, M. , Ren, Z. F. , Zheng, Q. Q. , Ma, W. , Zhao, F. H. , & Qiao, Y. L. (2015). Knowledge of human papillomavirus vaccination and related factors among parents of young adolescents: A nationwide survey in China. Annals of Epidemiology, 25Placeholder Text, 231–235. 10.1016/j.annepidem.2014.12.009 [DOI] [PubMed] [Google Scholar]
- Zhang, Y. , Wang, Y. , Liu, L. , Fan, Y. , Liu, Z. , Wang, Y. , & Nie, S. (2016). Awareness and knowledge about human papillomavirus vaccination and its acceptance in China: A meta‐analysis of 58 observational studies. BMC Public Health, 16, 216–230. 10.1186/s12889-016-2873-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao, F. , & Qiao, Y. (2019). Cervical cancer prevention in China: A key to cancer control. Lancet, 393Placeholder Text, 969–970. 10.1016/S0140-6736(18)32849-6 [DOI] [PubMed] [Google Scholar]
- Zhao, D. J. , Gong, X. Z. , Hu, Z. G. , Ding, Y. , & Hong, Q. Y. (2010). Investigation on cognitive level of cervical human papillomavirus and its vaccine among community women in Shanghai. Chinese Journal of Biologicals, 05, 558–560. [Google Scholar]
- Zhao, F. H. , Tiggelaar, S. M. , Hu, S. Y. , Zhao, N. , Hong, Y. , Niyazi, M. , Qiao, Y. L. (2012). A multi‐center survey of HPV knowledge and attitudes toward HPV vaccination among women, government officials, and medical personnel in China. Asian Pacific Journal of Cancer Prevention, 13Placeholder Text, 2369–2378. 10.7314/APJCP.2012.13.5.2369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, Y. , Liu, Y. H. , Liu, Z. H. , Wang, R. , Chen, Y. L. , & Wan, Y. P. (2012). Study on university students' awareness and knowledge of human papillomavirus infections. Modern Preventive Medicine, 17, 4453–4454+4459. [Google Scholar]
- Zhou, Y. Q. , Fan, A. F. , Yang, Z. J. , & Liu, Z. H. (2016a). Cognition of acceptance of HPV vaccine in female doctors and influence factors analysis. Journal of Clinical Nursing, 02, 2–4. [Google Scholar]
- Zhou, Y. Q. , Yang, J. , & Wu, R. F. (2016b). Questionnaires survey on the cognition of prevention and treatment for cervical lesions among females from Shenzhen communities. Chinese Journal of Modern Nursing, 0Placeholder Text, 3578–3581. [Google Scholar]
- Zhu, Q. Y. , Wang, C. C. , Xu, Y. P. , & Cai, Y. Y. (2015). Analysis of incidence of cervical cancer and cognitive status of cervical cancer and HPV in women. Chinese Journal of Public Health Management, 05, 768–769. [Google Scholar]
- Zhu, J. H. , Zhou, X. H. , Xi, S. J. , Huang, W. , & Lv, X. (2016). The cognitive study on human papillomavirus and human papillomavirus vaccine among MSM in Xiacheng district of Hangzhou. China Preventive Medicine, 03, 212–216. [Google Scholar]
- Zhu, Y. R. , Hu, X. L. , & Sheng, C. H. (2017). A survey of college students' cognition and attitude towards HPV vaccine. Today Nurse, 11, 25–27. [Google Scholar]
- Zou, H. , Meng, X. , Jia, T. , Zhu, C. , Chen, X. , Li, X. , Xu, J. , Ma, W. , & Zhang, X. (2016a). Awareness and acceptance of human papillomavirus (HPV) vaccination among males attending a major sexual health clinic in Wuxi, China: A cross‐sectional study. Human Vaccines & Immunotherapeutics, 12Placeholder Text, 1551–1559. 10.1080/21645515.2015.1099771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou, H. , Wang, W. , Ma, Y. , Wang, Y. , Zhao, F. , Wang, S. , Zhang, S. , & Ma, W. (2016b). How university students view human papillomavirus (HPV) vaccination: A cross‐sectional study in Jinan, China, Hum Vaccin Immunother, 12Placeholder Text, 39–46. 10.1080/21645515.2015.1072667 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Search strategies for English‐ and Chinese‐ language databases
Table S2. Quality assessment tool (items and scores)
Table S3. Quality assessment of included studies
Tables S4. Rationale for undertaking narrative synthesis instead of meta‐analysis
Table S5. Socio‐demographic characteristics in Eastern, Central and Western China
Table S6. Characteristics of included studies
Table S7. Findings of studies reporting acceptability of the HPV vaccine for personal use in mainland China
Table S8. Findings of studies reporting parental acceptability of HPV vaccine for a daughter/son in mainland China
Table S9. Studies reporting barriers affecting the acceptability of HPV vaccine (for personal use).
Table S10. Findings of studies reporting the reasons for not accepting the HPV vaccine for personal use in mainland China
Table S11. Findings of studies reporting parental reasons for accepting the HPV vaccine for their daughter or son in mainland China
Table S12. Findings of studies reporting willingness to pay for HPV vaccine by price ranges in mainland China
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


