Abstract
In recent years digital technologies have become a major means for providing health-related services and this trend was strongly reinforced by the current Coronavirus disease 2019 (COVID-19) pandemic. As it is well-known that regular physical activity has positive effects on individual physical and mental health and thus is an important prerequisite for healthy aging, digital technologies are also increasingly used to promote unstructured and structured forms of physical activity. However, in the course of this development, several terms (e.g., Digital Health, Electronic Health, Mobile Health, Telehealth, Telemedicine, and Telerehabilitation) have been introduced to refer to the application of digital technologies to provide health-related services such as physical interventions. Unfortunately, the above-mentioned terms are often used in several different ways, but also relatively interchangeably. Given that ambiguous terminology is a major source of difficulty in scientific communication which can impede the progress of theoretical and empirical research, this article aims to make the reader aware of the subtle differences between the relevant terms which are applied at the intersection of physical activity and Digital Health and to provide state-of-art definitions for them.
Keywords: Digital Health, Electronic Health, Mobile Health, Telehealth, Telemedicine, Physical activity, Physical training, Aging
Introduction
There is a substantial and still growing amount of evidence showing that regular physical activity (e.g., in the form of physical exercise and/or physical training – see Table 1 for definitions) is, among other lifestyle factors such as diet and sleep, an important factor to preserve or restore physical and mental health during the whole lifespan [14–18]. Although the above-mentioned evidence suggests that an adequate level of regular physical activity is a mandatory prerequisite to ensure overall health, worldwide more than two-thirds of adolescents [19] and almost one-third of adults [20–22] do not reach the recommended level of regular physical activity. From a public health perspective, the latter findings - indicating that a large amount of the world population has to be classified as physically inactive - are rather alarming [23]. In this context, there is also evidence that the level of physical inactivity increases as a function of age [22, 24, 25] and that older adults spend a relatively large amount of their wakening hours sedentary [26–29], whereby for the latter even an increase has been observed in the last years [28]. The fact that a considerable amount of the worldwide population does not reach the recommended level of physical activity [1, 2] has been significantly exacerbated because of the Coronavirus disease 2019 (COVID-19)-related public health actions (e.g., home confinement). Unfortunately, the latter has led in the general [30–36] and in the aging population [30, 33, 34, 37, 38] to a further increase in sedentary behavior and a decrease in the level of regular physical activity. Given that higher levels of physical inactivity and sedentary behavior are associated with detrimental health consequences [23, 39–43], the above-presented evidence suggests that, especially in the aging population, appropriate countermeasures such as interventions to promote regular and structured forms of physical activity - defined as physical exercise and/or physical training (see Table 1) - should be initiated. The latter idea is strongly reinforced by mounting evidence showing that regular and structured forms of physical activity are a crucial element of healthy aging [44–51].
Table 1.
Overview of the definitions of physical activity, physical exercise, physical inactivity, physical intervention, physical training, and sedentary behavior. The definitions are based on the following literature [1–13]
| Term | Definition |
|---|---|
| Physical activity | “...is defined as all muscle-induced bodily movements (e.g., in occupational or leisure time) leading to an increase in the energy expenditure above ∼1.0/1.5 MET (metabolic equivalent of the task; 1 MET = 1 kcal (4.184 kJ) • kg− 1 • h− 1).” |
| Physical exercise | “…is defined as a specific form of physical activity that is planned, structured, repetitive, and purposive to maintain or improve increasing or, at least, maintaining the performance in one or more fitness dimensions. Physical exercise can be differentiated based on temporal characteristics in acute (single bout/session of) physical exercise and chronic (multiple bouts/sessions of) physical exercise.” |
| Physical inactivity | “…is defined as an insufficient level of physical activity to meet specific recommendations (e.g., provided by the World Health Organization).” |
| Physical intervention | "...is an umbrella term that encompasses both physical exercise and physical training." |
| Physical training | “…is defined as chronic physical exercises being conducted regularly in a planned, structured, and purposive manner with the objective of increasing or, at least, maintaining the performance in one or more fitness dimensions.” |
| Sedentary behavior | “…is defined as behavior any waking behavior characterized by an energy expenditure of 1.5 METs or lower while sitting, reclining or lying.” |
Definition and delineation of the relevant terms
In recent years the utilization of digital technologies to promote regular and structured forms of physical activity has become a very popular field for both research and practical application, especially in the aging population [52, 53]. Indeed, there is some evidence that Electronic Health interventions [54] and Mobile Health interventions [55–57] (see next section for a definition and differentiation of the terms) can increase the regular level of physical activity in older adults.
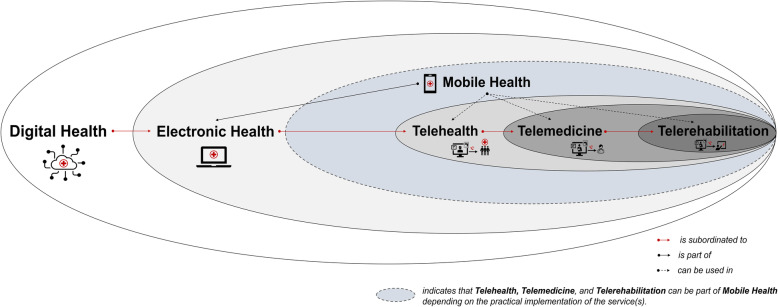
Several terms are commonly used when references are made to the application of digital technologies in different health care settings such as in the prevention and rehabilitation of (age-related) diseases. For instance, the terms (i) Digital Health, (ii) Electronic Health, (iii) Mobile Health, (iv) Telehealth, (v) Telemedicine, (vi) and Telerehabilitation are commonly used relatively interchangeably for the above-mentioned purpose as no generally accepted definition of these terms has yet been reached [58–79], which is probably caused by a distinct overlap in their meanings. As ambiguous terminology is a major source of difficulty in scientific communication which can impede progress in both theoretical and empirical research, we will at first provide definitions for (i) Digital Health, (ii) Electronic Health, (iii) Mobile Health, (iv) Telehealth, (v) Telemedicine, and (vi) Telerehabilitation (see also Fig. 1). Second, we discuss the implications of these definitions with regard to the promotion of physical activity.
Fig. 1.
Schematic illustration of the relationships between Digital Health, Electronic Health (eHealth), Mobile Health (mHealth), Telehealth, Telemedicine, and Telerehabilitation
Digital Health is an umbrella term that covers the application of digital technologies in the context of health and, as shown in Fig. 1, is a subordinate construct that comprises both Electronic Health and Mobile Health [52]. According to the World Health Organization, Digital Health is rooted in Electronic Health, but also encompasses other related areas such as “big data”, genomics, and artificial intelligence [52].
Electronic Health (eHealth) is, according to the World Health Organization, characterized by “the use of information and communications technology (ICT) in support of health and health-related fields” [52]. As a branch of Electronic Health, Mobile Health (mHealth) refers to “the use of mobile wireless technologies for public health” [52].
Both Telehealth and Telemedicine encompass the utilization of electronic communications and information technologies to remotely provide health care services (e.g., when participants are at different locations) [80–82]. In particular, the term Telehealth compromises services of all health care professionals and thus also includes non-clinical services [80, 81]. In contrast, the term Telemedicine, in a narrow sense, refers specifically to clinical services [80, 82, 83]. As shown in Fig. 1, Telehealth and Telemedicine are both branches of Electronic Health [73, 79] and thus also a part of Digital Health [84].
Telerehabilitation is a branch of Telemedicine and can be defined as the remote provision of rehabilitation services via telecommunication technologies [85–87]. As shown in Fig. 1, Telerehabilitation is a subordinate part of Telehealth, Electronic Health, and Digital Health.
Please note that Telemedicine and Telerehabilitation can be further subdivided [70, 88, 89], but discussing these subordinated branches is beyond the scope and aim of this article.
Implications with regard to physical activity
From a conceptual view, interventions aiming to promote physical activity through digital technologies fall within the scope of the definitions of Digital Health, Electronic Health, and Telehealth but do not necessarily fulfil the criteria of Mobile Health and Telemedicine. Since not all physical interventions that utilize digital technologies fall within the scope of Mobile Health and Telemedicine, the criteria used to characterize these theoretical constructs may constitute a valuable starting point for finding the appropriate wording.
With respect to Mobile Health, interventions aiming to promote physical activity through digital technologies are covered by the definition of Mobile Health when mobile and wireless technologies such as wearables and/or smartphones are used. Thus, when looking for an appropriate wording, the following questions should be answered: Which digital technology has been used to deliver/receive the health-related intervention?
Given the opinion that Telemedicine does refer specifically to remote clinical services [80, 82, 83], interventions aiming to promote, for instance, structured forms of physical activity such as physical exercise and/or physical training by utilizing digital technologies are, in a strict sense, only part of Telemedicine, when they are part of a clinical service. However, the latter interpretation strongly depends on the definition of Telemedicine. Based on the above-discussed aspects, answering the following question will help to identify the appropriate wording: In which context has the health-related intervention been prescribed?
Practical examples - the devil is in the details
In this section, we will provide three examples to illustrate challenges in the attempt to derive an appropriate wording which in our view should be as narrow as possible and as broad as necessary.
The examples are based on the application of mobile apps that are delivered/received via smart devices such as smartphones and tablets, and videoconference software. Both applications have become popular tools to promote and deliver structured forms of physical activity [90, 91].
First example
There is an increasing number of mobile apps that are used to provide physical interventions in a non-clinical context to counteract the age-related decline of physical and cognitive capabilities [92–95]).
With reference to the first question of our proposed approach (Which digital technology has been used to deliver/receive the health-related intervention?) and based on the fact that the physical interventions in the first example rely on mobile apps (i.e., delivered/received via smartphone or tablet), these interventions fulfill the criteria of Digital Health, Electronic Health, Mobile Health, and Telehealth. However, as the apps are used in a non-clinical context (e.g., physical interventions to prevent the age-related decline of physical and cognitive capabilities [92–95]), they do not fall within the definitions of Telemedicine and Telerehabilitation. Thus, these interventions should be referred to as Telehealth and/or Mobile Health applications.
Second example
Comparable to the increase of mobile apps in the non-clinical context, there is also an increase of mobile apps for the use in clinical settings. For example, the Kaia app which is typically delivered/received via a mobile device (e.g., a smartphone) provides physical exercises for the therapy of (older) individuals suffering from back pain [96–98].
With respect to our proposed approach aiming to derive an appropriate wording, the answer to the first question (Which digital technology has been used to deliver/receive the health-related intervention?) is that smartphone apps fall within the definitions of Digital Health, Electronic Health, Mobile Health, and Telehealth, whereas they only meet the criteria for Telemedicine and Telerehabilitation when they are part of a clinical service (e.g., as a Digital Health application [DiGA]). The latter point is related to the second question (In which context has the health-related intervention been prescribed?). In this context, this mobile app can be referred to as a Telemedicine application, or in a narrower sense as a Telerehabilitation application because this mobile app is used to prescribe physical exercises in a clinical context (e.g., as therapy against back pain [96–98]).
Third example
There is a growing number of studies that use videoconference software in a non-clinical context to remotely deliver physical exercise sessions (i.e., online classes) to foster healthy aging [99–102].
As in the current example, the physical exercise sessions are delivered in a non-clinical context, these interventions do not fulfil the criteria of Telemedicine or Telerehabilitation (second question - In which context has the health-related intervention been prescribed?). Concerning the first question (Which digital technology has been used to deliver/receive the health-related intervention?) an explicit answer is rather difficult as it depends on the technological devices that are used to deliver/receive the content. In particular, when the online physical exercise sessions are solely delivered/received via stationary devices such as a television screen or a stationary computer, the definitions of Digital Health, Electronic Health, and Telehealth are met, but the criteria for Mobile Health are not fulfilled. In this case, Electronic Health and Telehealth can be used to refer to this intervention. However, when the same online content is solely delivered/received via a smartphone or a tablet, it fulfills the criteria of Digital Health, Electronic Health, Telehealth, and Mobile Health. In the latter case, we recommend, based on our approach, to refer to this intervention as a Mobile Health application. If both stationary (e.g., television screen) and mobile devices (e.g., smartphone) are used to receive the online physical exercise sessions, we suggest to refer to these interventions as Electronic Health or Telehealth applications since the criteria of Mobile Health are not met by each participant (e.g., only those who use a mobile device such as a smartphone to receive the intervention).
Based on the above-presented examples, it becomes apparent that an appropriate differentiation between Digital Health, Electronic Health, Mobile Health, Telehealth, Telemedicine, and Telerehabilitation can be very challenging as the definitions of these terms overlap to some extent. Moreover, although the approach proposed in this publication can serve as a guide to use an appropriate wording, it needs to be noted that a universal recommendation cannot be provided as the appropriate wording strongly depends on the particular case. In order to avoid misunderstandings, researchers should pay close attention to the subtle conceptual difference when they use the terms (i) Digital Health, (ii) Electronic Health, (iii) Mobile Health, (iv) Telehealth, (v) Telemedicine, and (vi) Telerehabilitation instead of using them relatively interchangeable. In addition, official bodies (e.g., World Health Organization) should make efforts to reach generally accepted definitions of the terms which are relevant in the field of physical activity and Digital Health.
Conclusions
In recent years, digital technologies have become a popular tool for the promotion of physical activity (e.g., wearables, delivery of physical exercise sessions via online classes or smartphone apps) both in scientific research and in practical application [90, 91]. As terminological ambiguity can be a major source of difficulty impeding communication and thus progress in both theoretical and empirical research, here, we aimed to make the reader aware of the subtle differences between the relevant terms and provide state-of-the-art definitions for them. To that end, we hope that this article could provide the reader with a more nuanced view on relevant terms in the field of physical activity and Digital Health which, in turn, might foster further progress in this impactful research field.
Acknowledgments
The authors would like to acknowledge the financial support for the Article Processing Charges provided by the University of Potsdam and Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) - grant number 491466077.
Authors’ contributions
F.H.: conceptualization, writing – original draft, visualization P.T.: visualization, writing – review & editing; T.G.: conceptualization, writing – review & editing, supervision; M.A.R.: writing - review and editing; N.G.M.: writing – review & editing, resources, supervision. The author(s) read and approved the final manuscript.
Funding
The authors received no specific funding for this work.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors gave final approval of the submitted version.
Competing interests
The authors declare no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–1462. doi: 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . WHO guidelines on physical activity and sedentary behaviour. Geneva: World Health Organization; 2020. [PubMed] [Google Scholar]
- 3.Budde H, Schwarz R, Velasques B, Ribeiro P, Holzweg M, Machado S, Brazaitis M, Staack F, Wegner M. The need for differentiating between exercise, physical activity, and training. Autoimmun Rev. 2016;15(1):110–111. doi: 10.1016/j.autrev.2015.09.004. [DOI] [PubMed] [Google Scholar]
- 4.Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100(2):126–131. [PMC free article] [PubMed] [Google Scholar]
- 5.Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(Supplement):S498–S504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 6.Herold F, Törpel A, Hamacher D, Budde H, Gronwald T. A discussion on different approaches for prescribing physical interventions - four roads Lead to Rome, but which one should we choose? J Pers Med. 2020;10(3):55. doi: 10.3390/jpm10030055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Herold F, Törpel A, Hamacher D, Budde H, Zou L, Strobach T, et al. Causes and consequences of Interindividual response variability: a call to apply a more rigorous research design in acute exercise-cognition studies. Front Physiol. 2021;12. 10.3389/fphys.2021.682891. [DOI] [PMC free article] [PubMed]
- 8.Herold F, Müller P, Gronwald T, Müller NG. Dose-response matters! - a perspective on the exercise prescription in exercise-cognition research. Front Psychol. 2019;10:2338. doi: 10.3389/fpsyg.2019.02338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Herold F, Hamacher D, Schega L, Müller NG. Thinking while moving or moving while thinking - concepts of motor-cognitive training for cognitive performance enhancement. Front Ag Neurosci. 2018;10:228. doi: 10.3389/fnagi.2018.00228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Falck RS, Davis JC, Khan KM, Handy TC, Liu-Ambrose T. A wrinkle in measuring time use for cognitive health: how should we measure physical activity, sedentary behaviour and sleep? Am J Lifestyle Med. 2021;155982762110314:155982762110314. doi: 10.1177/15598276211031495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pate RR, O'Neill JR, Lobelo F. The evolving definition of “sedentary”. Exerc Sport Sci Rev. 2008;36(4):173–178. doi: 10.1097/JES.0b013e3181877d1a. [DOI] [PubMed] [Google Scholar]
- 12.Tremblay MS, Aubert S, Barnes JD, Saunders TJ, Carson V, Latimer-Cheung AE, et al. Sedentary behavior research Network (SBRN) - terminology consensus project process and outcome. Int J Behav Nutr Phys Act. 2017;14(1):75. doi: 10.1186/s12966-017-0525-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sedentary Behaviour Research Network Letter to the editor: standardized use of the terms “sedentary” and “sedentary behaviours”. Appl Physiol Nutr Metab. 2012;37(3):540–542. doi: 10.1139/h2012-024. [DOI] [PubMed] [Google Scholar]
- 14.Pedersen BK, Saltin B. Evidence for prescribing exercise as therapy in chronic disease. Scand J Med Sci Sports. 2006;16(Suppl 1):3–63. doi: 10.1111/j.1600-0838.2006.00520.x. [DOI] [PubMed] [Google Scholar]
- 15.Pedersen BK, Saltin B. Exercise as medicine - evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports. 2015;25:1–72. doi: 10.1111/sms.12581. [DOI] [PubMed] [Google Scholar]
- 16.Kivipelto M, Mangialasche F, Ngandu T. Lifestyle interventions to prevent cognitive impairment, dementia and Alzheimer disease. Nat Rev Neurol. 2018;14(11):653–666. doi: 10.1038/s41582-018-0070-3. [DOI] [PubMed] [Google Scholar]
- 17.Luan X, Tian X, Zhang H, Huang R, Li N, Chen P, Wang R. Exercise as a prescription for patients with various diseases. J Sport Health Sci. 2019;8(5):422–441. doi: 10.1016/j.jshs.2019.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stubbs B, Vancampfort D, Hallgren M, Firth J, Veronese N, Solmi M, Brand S, Cordes J, Malchow B, Gerber M, Schmitt A, Correll CU, de Hert M, Gaughran F, Schneider F, Kinnafick F, Falkai P, Möller HJ, Kahl KG. EPA guidance on physical activity as a treatment for severe mental illness: a meta-review of the evidence and position statement from the European psychiatric association (EPA), supported by the International Organization of Physical Therapists in mental health (IOPTMH) Eur Psychiatry. 2018;54:124–144. doi: 10.1016/j.eurpsy.2018.07.004. [DOI] [PubMed] [Google Scholar]
- 19.Guthold R, Stevens GA, Riley LM, Bull FC. Global trends in insufficient physical activity among adolescents: a pooled analysis of 298 population-based surveys with 1·6 million participants. Lancet Child Adolescent Health. 2020;4(1):23–35. doi: 10.1016/S2352-4642(19)30323-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kohl HW, Craig CL, Lambert EV, Inoue S, Alkandari JR, Leetongin G, Kahlmeier S. The pandemic of physical inactivity: global action for public health. Lancet. 2012;380(9838):294–305. doi: 10.1016/S0140-6736(12)60898-8. [DOI] [PubMed] [Google Scholar]
- 21.Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob Health. 2018;6(10):e1077–e1086. doi: 10.1016/S2214-109X(18)30357-7. [DOI] [PubMed] [Google Scholar]
- 22.Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380(9838):247–257. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- 23.Blair SN. Physical inactivity: the biggest public health problem of the 21st century. Br J Sports Med. 2009;43(1):1–2. [PubMed] [Google Scholar]
- 24.Guthold R, Ono T, Strong KL, Chatterji S, Morabia A. Worldwide variability in physical inactivity a 51-country survey. Am J Prev Med. 2008;34(6):486–494. doi: 10.1016/j.amepre.2008.02.013. [DOI] [PubMed] [Google Scholar]
- 25.Gomes M, Figueiredo D, Teixeira L, Poveda V, Paúl C, Santos-Silva A, Costa E. Physical inactivity among older adults across Europe based on the SHARE database. Age Ageing. 2017;46(1):71–77. doi: 10.1093/ageing/afw165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harvey JA, Chastin SFM, Skelton DA. Prevalence of sedentary behavior in older adults: a systematic review. Int J Environ Res Public Health. 2013;10(12):6645–6661. doi: 10.3390/ijerph10126645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hamrik Z, Sigmundová D, Kalman M, Pavelka J, Sigmund E. Physical activity and sedentary behaviour in Czech adults: results from the GPAQ study. Eur J Sport Sci. 2014;14(2):193–198. doi: 10.1080/17461391.2013.822565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Du Y, Liu B, Sun Y, Snetselaar LG, Wallace RB, Bao W. Trends in adherence to the physical activity guidelines for Americans for aerobic activity and time spent on sedentary behavior among US adults, 2007 to 2016. JAMA Netw Open. 2019;2(7):e197597. doi: 10.1001/jamanetworkopen.2019.7597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harvey JA, Chastin SFM, Skelton DA. How sedentary are older people? A systematic review of the amount of sedentary behavior. J Aging Phys Act. 2015;23(3):471–487. doi: 10.1123/japa.2014-0164. [DOI] [PubMed] [Google Scholar]
- 30.Wilke J, Mohr L, Tenforde AS, Edouard P, Fossati C, González-Gross M, et al. A pandemic within the pandemic? Physical activity levels substantially decreased in countries affected by COVID-19. Int J Environ Res Public Health. 2021;18(5). 10.3390/ijerph18052235. [DOI] [PMC free article] [PubMed]
- 31.Wunsch K, Kienberger K, Niessner C. Changes in physical activity patterns due to the Covid-19 pandemic: a systematic review and Meta-analysis. Int J Environ Res Public Health. 2022;19(4). 10.3390/ijerph19042250. [DOI] [PMC free article] [PubMed]
- 32.Stockwell S, Trott M, Tully M, Shin J, Barnett Y, Butler L, McDermott D, Schuch F, Smith L. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review. BMJ Open Sport Exerc Med. 2021;7(1):e000960. doi: 10.1136/bmjsem-2020-000960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Runacres A, Mackintosh KA, Knight RL, Sheeran L, Thatcher R, Shelley J, et al. Impact of the COVID-19 pandemic on sedentary time and behaviour in children and adults: a systematic review and Meta-analysis. Int J Environ Res Public Health. 2021;18(21). 10.3390/ijerph182111286. [DOI] [PMC free article] [PubMed]
- 34.Elvén M, Kerstis B, Stier J, Hellström C, von Heideken Wågert P, Dahlen M, et al. Changes in physical activity and sedentary behavior before and during the COVID-19 pandemic: a Swedish population study. Int J Environ Res Public Health. 2022;19(5). 10.3390/ijerph19052558. [DOI] [PMC free article] [PubMed]
- 35.Christensen A, Bond S, McKenna J. The COVID-19 conundrum: keeping safe while becoming inactive. A rapid review of physical activity, sedentary behaviour, and exercise in adults by gender and age. PLoS One. 2022;17(1):e0263053. doi: 10.1371/journal.pone.0263053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Trabelsi K, Ammar A, Masmoudi L, Boukhris O, Chtourou H, Bouaziz B, Brach M, Bentlage E, How D, Ahmed M, Mueller P, Mueller N, Hsouna H, Romdhani M, Hammouda O, Paineiras-Domingos L, Braakman-jansen A, Wrede C, Bastoni S, Pernambuco C, Mataruna-Dos-Santos L, Taheri M, Irandoust K, Khacharem A, Bragazzi N, Strahler J, Washif J, Andreeva A, Bailey S, Acton J, Mitchell E, Bott N, Gargouri F, Chaari L, Batatia H, khoshnami S, Samara E, Zisi V, Sankar P, Ahmed W, Ali G, Abdelkarim O, Jarraya M, Abed K, Moalla W, Souissi N, Aloui A, Souissi N, Gemert-Pijnen L, Riemann B, Riemann L, Delhey J, Gómez-Raja J, Epstein M, Sanderman R, Schulz S, Jerg A, al-Horani R, Mansi T, Dergaa I, Jmail M, Barbosa F, Ferreira-Santos F, Šimunič B, Pišot R, Pišot S, Gaggioli A, Steinacker J, Zmijewski P, Clark CCT, Apfelbacher C, Glenn J, Saad H, Chamari K, Driss T, Hoekelmann A. Globally altered sleep patterns and physical activity levels by confinement in 5056 individuals: ECLB COVID-19 international online survey. Biol Sport. 2021;38(4):495–506. doi: 10.5114/biolsport.2021.101605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Browne RAV, Macêdo GAD, Cabral LLP, Oliveira GTA, Vivas A, Fontes EB, Elsangedy HM, Costa EC. Initial impact of the COVID-19 pandemic on physical activity and sedentary behavior in hypertensive older adults: an accelerometer-based analysis. Exp Gerontol. 2020;142:111121. doi: 10.1016/j.exger.2020.111121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yamada M, Kimura Y, Ishiyama D, Otobe Y, Suzuki M, Koyama S, Kikuchi T, Kusumi H, Arai H. Effect of the COVID-19 epidemic on physical activity in community-dwelling older adults in Japan: a cross-sectional online survey. J Nutr Health Aging. 2020;24(9):948–950. doi: 10.1007/s12603-020-1424-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Saunders TJ, McIsaac T, Douillette K, Gaulton N, Hunter S, Rhodes RE, Prince SA, Carson V, Chaput JP, Chastin S, Giangregorio L, Janssen I, Katzmarzyk PT, Kho ME, Poitras VJ, Powell KE, Ross R, Ross-White A, Tremblay MS, Healy GN. Sedentary behaviour and health in adults: an overview of systematic reviews. Appl Physiol Nutr Metab. 2020;45(10 (Suppl. 2)):S197–S217. doi: 10.1139/apnm-2020-0272. [DOI] [PubMed] [Google Scholar]
- 40.Rojer AGM, Ramsey KA, Amaral Gomes ES, D'Andrea L, Chen C, Szoeke C, et al. Objectively assessed physical activity and sedentary behavior and global cognitive function in older adults: a systematic review. Mech Ageing Dev. 2021;198:111524. doi: 10.1016/j.mad.2021.111524. [DOI] [PubMed] [Google Scholar]
- 41.Ramsey KA, Rojer AGM, D'Andrea L, Otten RHJ, Heymans MW, Trappenburg MC, et al. The association of objectively measured physical activity and sedentary behavior with skeletal muscle strength and muscle power in older adults: a systematic review and meta-analysis. Ageing Res Rev. 2021;67:101266. doi: 10.1016/j.arr.2021.101266. [DOI] [PubMed] [Google Scholar]
- 42.Falck RS, Davis JC, Liu-Ambrose T. What is the association between sedentary behaviour and cognitive function? A systematic review. Br J Sports Med. 2017;51(10):800–811. doi: 10.1136/bjsports-2015-095551. [DOI] [PubMed] [Google Scholar]
- 43.Ekelund U, Tarp J, Steene-Johannessen J, Hansen BH, Jefferis B, Fagerland MW, Whincup P, Diaz KM, Hooker SP, Chernofsky A, Larson MG, Spartano N, Vasan RS, Dohrn IM, Hagströmer M, Edwardson C, Yates T, Shiroma E, Anderssen SA, Lee IM. Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: systematic review and harmonised meta-analysis. BMJ. 2019;366:l4570. doi: 10.1136/bmj.l4570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Erickson KI, Donofry SD, Sewell KR, Brown BM, Stillman CM. Cognitive aging and the promise of physical activity. Annu Rev Clin Psychol. 2022;18(1):417–442. doi: 10.1146/annurev-clinpsy-072720-014213. [DOI] [PubMed] [Google Scholar]
- 45.García-Hermoso A, Ramirez-Vélez R, Sáez de Asteasu ML, Martínez-Velilla N, Zambom-Ferraresi F, Valenzuela PL, et al. Safety and Effectiveness of Long-Term Exercise Interventions in Older Adults: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Sports Med. 2020;311(6):2387–1106. doi: 10.1007/s40279-020-01259-y. [DOI] [PubMed] [Google Scholar]
- 46.Cartee GD, Hepple RT, Bamman MM, Zierath JR. Exercise promotes healthy aging of skeletal muscle. Cell Metab. 2016;23(6):1034–1047. doi: 10.1016/j.cmet.2016.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liu-Ambrose T, Barha C, Falck RS. Active body, healthy brain: exercise for healthy cognitive aging. Int Rev Neurobiol. 2019;147:95–120. doi: 10.1016/bs.irn.2019.07.004. [DOI] [PubMed] [Google Scholar]
- 48.Cunningham C, O’Sullivan R, Caserotti P, Tully MA. Consequences of physical inactivity in older adults: A systematic review of reviews and meta-analyses. Scand J Med Sci Sports. 2020;30(5):816–827. doi: 10.1111/sms.13616. [DOI] [PubMed] [Google Scholar]
- 49.Dipietro L, Campbell WW, Buchner DM, Erickson KI, Powell KE, Bloodgood B, Hughes T, Day KR, Piercy KL, Vaux-Bjerke A, Olson RD, 2018 Physical Activity Guidelines Advisory Committee* Physical activity, injurious falls, and physical function in aging: an umbrella review. Med Sci Sports Exerc. 2019;51(6):1303–1313. doi: 10.1249/MSS.0000000000001942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rebelo-Marques A, de Sousa Lages A, Andrade R, Ribeiro CF, Mota-Pinto A, Carrilho F, Espregueira-Mendes J. Aging Hallmarks: The Benefits of Physical Exercise. Front Endocrinol (Lausanne) 2018;9:258. doi: 10.3389/fendo.2018.00258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chodzko-Zajko W, Schwingel A, Park CH. Successful aging: the role of physical activity. Am J Lifestyle Med. 2009;3(1):20–28. doi: 10.1177/1559827608325456. [DOI] [Google Scholar]
- 52.World Health Organization . WHO guideline: recommendations on digital interventions for health system strengthening. Geneva: World Health Organization; 2019. [PubMed] [Google Scholar]
- 53.World Health Organization . BE MOBILE BE HE@LTHY: A handbook on how to implement mHealth. 2018. [Google Scholar]
- 54.Muellmann S, Forberger S, Möllers T, Bröring E, Zeeb H, Pischke CR. Effectiveness of eHealth interventions for the promotion of physical activity in older adults: a systematic review. Prev Med. 2018;108:93–110. doi: 10.1016/j.ypmed.2017.12.026. [DOI] [PubMed] [Google Scholar]
- 55.Elavsky S, Knapova L, Klocek A, Smahel D. Mobile health interventions for physical activity, sedentary behavior, and sleep in adults aged 50 years and older: a systematic literature review. J Aging Phys Act. 2019;27(4):565–593. doi: 10.1123/japa.2017-0410. [DOI] [PubMed] [Google Scholar]
- 56.Eckerstorfer LV, Tanzer NK, Vogrincic-Haselbacher C, Kedia G, Brohmer H, Dinslaken I, Corcoran K. Key elements of mHealth interventions to successfully increase physical activity: Meta-regression. JMIR Mhealth Uhealth. 2018;6(11):e10076. doi: 10.2196/10076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mönninghoff A, Kramer JN, Hess AJ, Ismailova K, Teepe GW, Tudor Car L, Müller-Riemenschneider F, Kowatsch T. Long-term effectiveness of mHealth physical activity interventions: systematic review and Meta-analysis of randomized controlled trials. J Med Internet Res. 2021;23(4):e26699. doi: 10.2196/26699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cunningham SG, Wake DJ, Waller A, Morris AD. Definitions of eHealth. In: Gaddi A, Capello F, Manca M, editors. eHealth, care and quality of life. Milano: Springer Milan; 2014. pp. 15–30. [Google Scholar]
- 59.Della MV. What is e-health (2): the death of telemedicine? J Med Internet Res. 2001;3(2):E22. doi: 10.2196/jmir.3.2.e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Boogerd EA, Arts T, Engelen LJ, van de Belt TH. “What is eHealth”: time for an update? JMIR Res Protoc. 2015;4(1):e29. doi: 10.2196/resprot.4065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Eysenbach G. What is e-health? J Med Internet Res. 2001;3(2):E20. doi: 10.2196/jmir.3.2.e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hallberg D, Salimi N. Qualitative and quantitative analysis of definitions of e-health and m-health. Healthc Inform Res. 2020;26(2):119–128. doi: 10.4258/hir.2020.26.2.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Istepanian RS, AlAnzi T. Biomedical Information Technology. Elsevier; 2020. Mobile health (m-health) pp. 717–733. [Google Scholar]
- 64.Malvey D, Slovensky DJ. From telemedicine to telehealth to eHealth: where does mHealth fit? In: Malvey D, Slovensky DJ, editors. mHealth. Boston: Springer US; 2014. pp. 19–43. [Google Scholar]
- 65.Meier CA, Fitzgerald MC, Smith JM. eHealth: extending, enhancing, and evolving health care. Annu Rev Biomed Eng. 2013;15(1):359–382. doi: 10.1146/annurev-bioeng-071812-152350. [DOI] [PubMed] [Google Scholar]
- 66.Morrison C. Defining digital health. 2006. [Google Scholar]
- 67.Scott RE, Mars M. Here we go again – ‘digital health’. J Int Soc Telemed Ehealth. 2019;7:1–2. doi: 10.29086/JISfTeH.7.e1. [DOI] [Google Scholar]
- 68.Oh H, Rizo C, Enkin M, Jadad A. What is eHealth?: a systematic review of published definitions. World Hospitals and Health Services. 2005;41(1):32–29. doi: 10.2196/jmir.7.1.e1. [DOI] [PubMed] [Google Scholar]
- 69.Pagliari C, Sloan D, Gregor P, Sullivan F, Detmer D, Kahan JP, Oortwijn W, MacGillivray S. What is eHealth (4): a scoping exercise to map the field. J Med Internet Res. 2005;7(1):e9. doi: 10.2196/jmir.7.1.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pinciroli F. A manifesto on telehealth and telemedicine. J Am Med Inform Assoc. 2001;8(4):349–350. doi: 10.1136/jamia.2001.0080349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shaw T, McGregor D, Brunner M, Keep M, Janssen A, Barnet S. What is eHealth (6)? Development of a Conceptual Model for eHealth: Qualitative Study with Key Informants. J Med Internet Res. 2017;19(10):e324. doi: 10.2196/jmir.8106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Showell C, Nøhr C. How should we define eHealth, and does the definition matter? Stud Health Technol Inform. 2012;180:881–884. [PubMed] [Google Scholar]
- 73.Sood S, Mbarika V, Jugoo S, Dookhy R, Doarn CR, Prakash N, Merrell RC. What is telemedicine? A collection of 104 peer-reviewed perspectives and theoretical underpinnings. Telemed J E Health. 2007;13(5):573–590. doi: 10.1089/tmj.2006.0073. [DOI] [PubMed] [Google Scholar]
- 74.Stowe S, Harding S. Telecare, telehealth and telemedicine. Eur Geriatr Med. 2010;1(3):193–197. doi: 10.1016/j.eurger.2010.04.002. [DOI] [Google Scholar]
- 75.Tuckson RV, Edmunds M, Hodgkins ML. Telehealth. N Engl J Med. 2017;377(16):1585–1592. doi: 10.1056/NEJMsr1503323. [DOI] [PubMed] [Google Scholar]
- 76.Williatte-Pellitteri L. New technologies, telemedicine, eHealth, data…what are you talking about? The Lawyer’s point of view. In: André A, editor. Digital Medicine. Cham: Springer International Publishing; 2019. pp. 93–102. [Google Scholar]
- 77.Gogia S. Fundamentals of Telemedicine and Telehealth. Elsevier; 2020. Rationale, history, and basics of telehealth; pp. 11–34. [Google Scholar]
- 78.Vollmar HC, Kramer U, Müller H, Griemmert M, Noelle G, Schrappe M. Digitale Gesundheitsanwendungen – Rahmenbedingungen zur Nutzung in Versorgung, Strukturentwicklung und Wissenschaft – Positionspapier der AG Digital Health des DNVF. [Position Paper of The AG Digital Health DNVF on Digital Health Applications: Framework Conditions For Use in Health Care, Structural Development and Science] Gesundheitswesen. 2017;79(12):1080–1092. doi: 10.1055/s-0043-122233. [DOI] [PubMed] [Google Scholar]
- 79.Otto L, Harst L, Schlieter H, Wollschlaeger B, Richter P, Timpel P. Proceedings of the 11th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2018) 2018. Towards a Unified Understanding of eHealth and Related Terms – Proposal of a Consolidated Terminological Basis; pp. 533–539. [Google Scholar]
- 80.The American Telemedicine Association . Telemedicine, Telehealth, and Health Information Technology: An ATA Issue Paper. 2006. pp. 1–13. [Google Scholar]
- 81.World Health Organization . Telemedicine: opportunities and developments in member states report on the second global survey on eHealth. Geneva Switzerland: World Health Organization; 2010. [Google Scholar]
- 82.What is telehealth? How is telehealth different from telemedicine? 2021. https://www.healthit.gov/faq/what-telehealth-how-telehealth-different-telemedicine.
- 83.Montes J, Eichinger KJ, Pasternak A, Yochai C, Krosschell KJ. A post pandemic roadmap toward remote assessment for neuromuscular disorders: limitations and opportunities. Orphanet J Rare Dis. 2022;17(1):5. doi: 10.1186/s13023-021-02165-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lowery C. What is digital health and what do I need to know about it? Obstet Gynecol Clin N Am. 2020;47(2):215–225. doi: 10.1016/j.ogc.2020.02.011. [DOI] [PubMed] [Google Scholar]
- 85.Peretti A, Amenta F, Tayebati SK, Nittari G, Mahdi SS. Telerehabilitation: review of the state-of-the-art and areas of application. JMIR Rehabil Assist Technol. 2017;4(2):e7. doi: 10.2196/rehab.7511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Russell TG. Physical rehabilitation using telemedicine. J Telemed Telecare. 2007;13(5):217–220. doi: 10.1258/135763307781458886. [DOI] [PubMed] [Google Scholar]
- 87.Russell TG. Telerehabilitation: a coming of age. Australian J Physiother. 2009;55(1):5–6. doi: 10.1016/S0004-9514(09)70054-6. [DOI] [PubMed] [Google Scholar]
- 88.Winters JM. Telerehabilitation research: emerging opportunities. Annu Rev Biomed Eng. 2002;4(1):287–320. doi: 10.1146/annurev.bioeng.4.112801.121923. [DOI] [PubMed] [Google Scholar]
- 89.Brienza DM, McCue M. Introduction to Telerehabilitation. In: Kumar S, Cohn ER, editors. Telerehabilitation. London: Springer London; 2013. pp. 1–11. [Google Scholar]
- 90.Thompson WR. Worldwide survey of fitness trends for 2021. ACSM’s Health Fitness J. 2021;25(1):10–19. doi: 10.1249/FIT.0000000000000631. [DOI] [Google Scholar]
- 91.Thompson WR. Worldwide survey of fitness trends for 2022. ACSMs Health Fit J. 2022;26(1):11–20. doi: 10.1249/FIT.0000000000000732. [DOI] [Google Scholar]
- 92.Netz Y, Yekutieli Z, Arnon M, Argov E, Tchelet K, Benmoha E, Jacobs JM. Personalized exercise programs based upon remote assessment of motor fitness: a pilot study among healthy people aged 65 years and older. Gerontology. 2021;68(4):1–15. doi: 10.1159/000517918. [DOI] [PubMed] [Google Scholar]
- 93.Netz Y, Argov E, Yekutieli Z, Ayalon M, Tchelet K, Ben-Sira D, Amar Y, Jacobs JM. Personalized multicomponent exercise programs using smartphone technology among older people: protocol for a randomized controlled trial. BMC Geriatr. 2021;21(1):605. doi: 10.1186/s12877-021-02559-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Jungreitmayr S, Kranzinger C, Venek V, Ring-Dimitriou S. Effects of an app-based physical exercise program on selected parameters of physical fitness of females in retirement: a randomized controlled trial. Front Physiol. 2022;13. 10.3389/fphys.2022.821773. [DOI] [PMC free article] [PubMed]
- 95.Jungreitmayr S, Ring-Dimitriou S, Trukeschitz B, Eisenberg S, Schneider C. Effects of an information and communication technology-based fitness program on strength and balance in female home care service users. Int J Environ Res Public Health. 2021;18(15). 10.3390/ijerph18157955. [DOI] [PMC free article] [PubMed]
- 96.Priebe JA, Haas KK, Moreno Sanchez LF, Schoefmann K, Utpadel-Fischler DA, Stockert P, Thoma R, Schiessl C, Kerkemeyer L, Amelung V, Jedamzik S, Reichmann J, Marschall U, Toelle TR. Digital treatment of Back pain versus standard of care: the cluster-randomized controlled trial, Rise-uP. J Pain Res. 2020;13:1823–1838. doi: 10.2147/JPR.S260761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Priebe JA, Utpadel-Fischler D, Toelle TR. Less pain, better sleep? The effect of a multidisciplinary Back pain app on sleep quality in individuals suffering from Back pain - a secondary analysis of app user data. J Pain Res. 2020;13:1121–1128. doi: 10.2147/JPR.S232792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Toelle TR, Utpadel-Fischler DA, Haas K-K, Priebe JA. App-based multidisciplinary back pain treatment versus combined physiotherapy plus online education: a randomized controlled trial. NPJ Digit Med. 2019;2(1):34. doi: 10.1038/s41746-019-0109-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Chang S-H, Wang L-T, Chueh T-Y, Hsueh M-C, Hung T-M, Wang Y-W. Effectiveness of Facebook remote live-streaming-guided exercise for improving the functional fitness of community-dwelling older adults. Front Med. 2021;8. 10.3389/fmed.2021.734812. [DOI] [PMC free article] [PubMed]
- 100.Li F, Harmer P, Fitzgerald K, Winters-Stone K. A cognitively enhanced online tai Ji Quan training intervention for community-dwelling older adults with mild cognitive impairment: a feasibility trial. BMC Geriatr. 2022;22(1):76. doi: 10.1186/s12877-021-02747-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Li F, Harmer P, Voit J, Chou L-S. Implementing an online virtual falls prevention intervention during a public health pandemic for older adults with mild cognitive impairment: a feasibility trial. Clin Interv Aging. 2021;16:973–983. doi: 10.2147/CIA.S306431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Kuldavletova O, Pasquier F, Bigot L, Langeard A, Gauthier A, Quarck G. Videoconference-based adapted physical exercise training is a good and safe option for seniors. IJERPH. 2021;18(18):9439. doi: 10.3390/ijerph18189439. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.