Abstract
Purpose
We report a case of lipid keratopathy in a radial keratotomy incision that was successfully managed with radiofrequency diathermy of the neovascular pedicle responsible for the lipid deposition.
Observations
No perioperative or postoperative complications were noted. Following the procedure, the lesion showed significant decrease in lipid deposits and opacification along with disappearance of the neovascular pedicle.
Conclusions and importance
Radiofrequency diathermy of neovascular pedicle may represent an effective and safe alternative treatment option for treating lipid keratopathy. This is a first ever report of lipid keratopathy inside a radial keratotomy incision that was successfully managed by radiofrequency diathermy.
Keywords: Radiofrequency diathermy, Radial keratotomy, Lipid keratopathy, Corneal opacification
Highlights
-
•
We report a case of lipid keratopathy in a radial keratotomy incision.
-
•
We successfully managed the case with radiofrequency diathermy of the neovascular pedicle.
-
•
After treatment, the lesion showed regression of the opacification along with disappearance of the neovascular pedicle.
-
•
Radiofrequency diathermy may represent an effective and safe alternative treatment option for treating lipid keratopathy.
1. Introduction
Lipid keratopathy is a corneal degeneration that is commonly identified in eyes with a history of ocular trauma or ocular pathology associated with cornea neovascularization. It was first described by Cogan et al., in 1958.1 Its identifying features include cholesterol and phospholipid deposition in the corneal stroma, corneal thinning along with corneal neovascularization. Abnormal neovascularization of the cornea disturbs the immune privilege of the cornea by facilitating the migration of innate immune cells to the regional lymph nodes via the afferent vessels and migration of activated lymphocytes towards the cornea via the efferent vessels.
Two forms of the disease have been described in the literature. Primary lipid keratopathy, a form that is fairly uncommon, is usually bilateral and the patient doesn't present any signs of corneal pathology. This form of the disease usually occurs without prior vascularization or inflammation of the affected cornea. No pathophysiological mechanism has been described but there has been a connection to excess lipid production and a failure to metabolize fat encountered with systemic dyslipoproteinemias including Tangier disease (Familial high density lipoprotein deficiency) and LCAT (lecithin cholesterol acyltransferase) deficiency.2
The other form of the disease is secondary lipid keratopathy that has a frequent association with ocular trauma and ocular pathology. The mechanism of this form involves a disturbance of the balance between angiogenic and antiangiogenic factors, an upregulation of angiogenic factors that favors corneal neovascularization leading to an increased possibility of lipid deposition as larger quantities of lipoproteins reach the cornea. The clinical presentation is usually unilateral with cream colored opacification or fan-like cholesterol crystals being deposited adjacent to the primary neovascular pedicle.2
2. Case report
A 71-year-old female patient was referred by her ophthalmologist to the cornea service of our hospital for the diagnosis and management of a symptomatic lesion in the cornea of her left eye. The patient complained of a sensation of discomfort and vision fluctuation in the affected eye. The patient had a history of radial keratotomy (RK) performed in both eyes 25 years prior to presentation, bilateral phacoemulsification procedure performed two years prior, a peripheral iridotomy in the right eye and a history of treatment with Xalatan (Sandoz Pharmaceuticals AG, Switzerland) that was suspended two months prior to presentation.
At initial consultation the manifest visual acuity (VA) was 0.8 in the right eye and 1.0 in the left eye.
Slit lamp examination showed bilateral peripheral radial keratotomy incisions. In the left eye, some perilimbal superficial vessels were noted between the keratotomy incisions at the 12, 2 and 5 o'clock positions. A prominent neovascular pedicle was identified at the 2 o' clock position, adjacent to an old phacoemulsification side port incision, extending 3mm towards the center of the cornea inside a radial keratotomy incision with notable fat deposits along its course. The lesion stained slightly with fluorescein (Fig. 1A–D).
Fig. 1.
Pre-intervention images. A prominent neovascular pedicle at the 2 o' clock position that extended 3mm towards the center of the cornea inside a radial keratotomy incision with notable fat deposits along its course. A: The lesion stained slightly with fluorescein. B–D: Slit lamp images of the lesion. Fig. 1D The arrow demonstrates the neovascular pedicle of the lesion, E: An anterior segment optical coherence tomography (AS-OCT) of the lesion showed the RK incision with notable corneal stromal thinning up to 50% of the stromal thickness, along with compensatory epithelial hyperplasia.
The anterior chamber was deep and quiet. A well-placed posterior chamber intraocular lens implant and a capsulotomy were noted. The right eye presented with radial keratotomy incisions, superficial perilimbal vessels between 9, 10 and 6, 7 o' clock positions between the incisions. Peripheral iridectomy was noted at 1 o'clock location along with a posterior chamber intraocular lens implant. The posterior segment had no abnormalities in both eyes.
An anterior segment optical coherence tomography (AS-OCT) of the lesion showed the RK incision with notable corneal stroma thinning up to 50% of the stromal thickness, along with compensatory epithelial hyperplasia. The lipid deposits of the lesion were hyperreflective (Fig. 1E).
A treatment with a steroid containing antibiotic (Tobradex) (Alcon Switzerland SA, Switzerland) was initially prescribed 4 times a day for a week followed by a tapering schedule of 1 drop per week for a treatment duration of 4 weeks in combination with artificial tears.
Upon reevaluation, there was no improvement of the lipid deposits and minimal effect on the corneal vessels along with no symptomatic improvement. After discussion with the patient, an informed consent was obtained for treatment of the lesion with radiofrequency diathermy.
In the operating room, the procedure was performed under topical anesthesia.
Using the diathermy tip, thermal ablation of the neovascular pedicle for duration of 2 seconds was performed 1mm from the limbus. The Klöti device was set to the diathermy mode at 4–6 W. No intraoperative complications were observed.
In the subsequent follow-up visits a progressive improvement of the lesion and the symptoms were noted. A month after the procedure a partial resolution of the neovascular pedicle was obvious (Fig. 2). Five months later, a substantial improvement of the clinical image was noted along with decrease of the opacification at the lesion site (Fig. 3). Eleven months later, the lesion showed almost complete regression of the lipid deposits and the opacification along with disappearance of the neovascular pedicle. The patient described a near absence of discomfort and a significant improvement of vision fluctuations (Fig. 4).
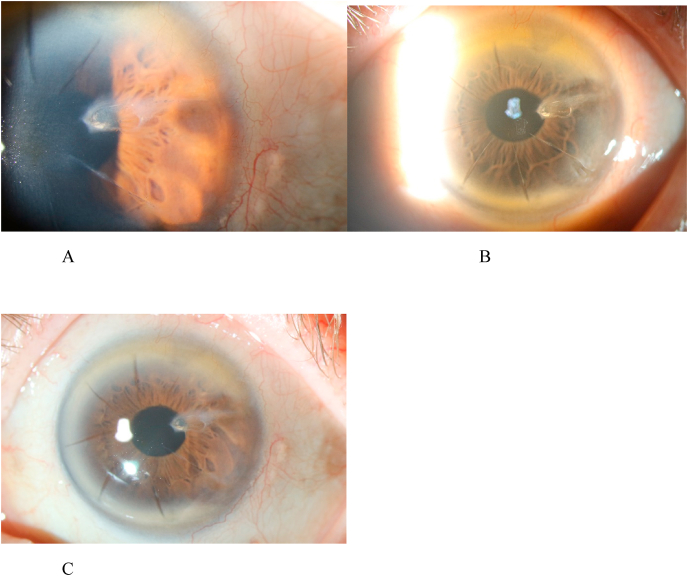
Fig. 2.
Slit lamp images of the lesion 1-month post intervention (A–C) with partial regression of the neovascular pedicle shown in Fig. 2C. (arrow).
Fig. 3.
Slit lamp images of the lesion 5-months post intervention. Substantial improvement is visible in comparison to the pre-op and 1-month post-op images.
Fig. 4.
Slit lamp images of the lesion 11-months post intervention. Almost complete resolution is visible in comparison to pre-op images and 1-month, 5-months post-op images.
3. Discussion
The management of lipid keratopathy is based on two directives. The first should be to identify the underlying cause or disease that has led to the insult. By identifying the cause some preventive steps can be taken in order to decrease the risk of progression or reemergence of the disease on the same or on a different site. The second directive is to eliminate the corneal neovascular pedicle that sustains the lesion and as a result to induce absorption of lipids. By occluding a neovascular pedicle, the continuous deposition of lipoproteins is arrested thus favoring lipid clearance. In addition, the amount of circulating leucocytes in the corneal tissue is reduced, thereby impeding the perpetuation of the inflammatory response.
In this case, as the location of the neovascular pedicle corresponded to the area where the phacoemulsification side port incision crossed the radial keratotomy incision, it was considered as the most likely precipitating event of the inflammatory process that led to the pathology.
Today, standard therapy begins with a corticosteroid regimen usually coadministered with topical antibiotics. Corticosteroids have the ability to decrease inflammation by inhibiting inflammatory mediators. This approach is potentially helpful in patients in which the cause of neovascularization is inflammatory. Well known side effects connected to ocular topical use include infection, cataract progression and intraocular pressure elevation.
Other therapeutic options target to eliminate the corneal neovascular vessels. These include anti-VEGF antibodies, needle point cautery, photodynamic therapy (PDT) and argon laser coagulation.3
Anti-VEGF antibodies, which are commonly used in choroidal neovascularization, while successful in management of corneal neovascularization, can be complicated by the appearance of epithelial defects, neurotrophic keratopathy and corneal stromal thinning4,5 In addition, they are not effective in the treatment of mature neovascular vessels and have the potential for life threatening side effects in patients with thromboembolic risk factors.2,6
Needle point cautery is a fairly successful option in treating neovascular corneal vessels. When this method is used, the needle of a 10-0 monofilament nylon suture is inserted inside the lumen of the neovascular pedicle and an alternating current produced from a monopolar diathermy machine set to 0.5–1 mA is applied for the duration of 2–3 seconds. Because of the uncertainty of the depth of the needle insertion, this method may be associated with increased risk of corneal microperforation and corneal intrastromal hemorrhages.7,8 The advantages of this method include its low cost, its wide availability and its decreased need to retreat these patients (57.1% of the patients demonstrated regression of all vessels during the first follow-up and did not require retreatment).8
Photodynamic therapy (PDT) is a cancer cell treatment option also used in ophthalmology in the treatment of choroidal neovascularization encountered in age related macular degeneration (AMD). In PDT, a light sensitive substance (verteporfin/dihematoporhyn) is injected intravenously followed by tissue irradiation with a low power laser directed towards the tissues of interest. The resulting free radical generation causes endothelial damage that causes a microvascular thrombosis that leads to occlusion of the blood vessel in the targeted area without any effect in the surrounding tissues. The main disadvantage of this method is the limited availability that is restricted only to big centers and the relatively higher cost compared to the other options.9
Argon laser photocoagulation of the desired vessel while effective in obliteration of mature and superficial vessels is not as potent in managing extensive or deep corneal neovascularization and due to its high energy levels it has been associated with a number of complications including injury to the corneal endothelium, the lens and iris atrophy.10
Klöti et al., in 1984, originally described the method of using a miniaturized bipolar diathermy for anterior lens capsulotomy during an infantile cataract surgery. The technique involves the use of a radiofrequency of 500 KHz to heat a platinum tip of 500 μm to a temperature of 160 °C. The blunt tip with its curved surface ensures a maximum depth of 500 μm and thus decreases the risk of corneal microperforation in comparison to fine needle diathermy.11,12 However, this may also mean that by treating more superficial vessels additional sessions for complete regression of a neovascular pedicle are necessary (Fig. 5).
Fig. 5.
The Kloti device (Klöti, Oertli ®, Switzerland) used in the procedure comprising of the A. Bipolar diathermy control unit and B. the miniaturized bipolar diathermy tip that through the use of a radiofrequency signal of 500 KHz heats the platinum tip of the diathermy to a temperature of 160 °C.
Kymionis et al.13 described the successful use of the technique in 2 patients with lipid keratopathy secondary to post keratitis neovascularization. The first case required 3 treatment sessions for a complete regression of the neovascular pedicle, while the second case required 2 treatment sessions for vessel regression. After a 12-month follow-up of these patients no intraoperative or postoperative complications were observed along with regression of the lipid deposits and neovascularization. In addition, a subjective symptomatic improvement along with visual acuity increase in 1 of these patients was observed. This technique has been described as safe, precise, easy to perform under topical anesthesia, effective for deeper corneal vessels, well tolerated by the patients and very easily accessible with a relatively low cost.
Substance P neuropeptide (SP) as a drug target seems to be an interesting topic of research. Substance P, a member of the tachykinin family, is secreted from nerve endings and immune cells in inflammation and binds to neurokinin receptors (NK1R) which triggers epithelial proliferation as well as angiogenesis. Barbariga et al., in 201814 in their original publication used murine animal models and targeted three different substance P precursor Tac-1 knockout genes. They induced corneal neovascularization in the three groups using three methods, namely de-epithelization, alkali burn or a corneal intrastromal suture and in each group they compared the wild type mice with the knockout ones. Substance P tear level measurements correlated positively with the corneal neovascularization levels in all three groups and the Tac-1 knockout groups showed less corneal neovascularization.
4. Conclusions
Radiofrequency diathermy may represent an effective and safe alternative treatment option for treating lipid keratopathy. To the best of our knowledge, this is a first ever report of successful resolution of lipid keratopathy in a radial keratotomy incision. Further studies should take place in order to investigate the safety and efficacy of this technique, as well as the need for retreatment in a larger number of cases over longer periods of follow-up.
Patient consent
Consent to publish this case report has been obtained from the patient in writing.
Compliance with ethics guidelines
Informed consent in written and oral form was obtained from the patient prior to publication.
Human and animal rights
Not applicable.
Data availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Authorship
VB and CH wrote the first draft of the case report. KH provided specialist advice, revised the draft, was the main care provider for the patient and performed the procedure.
Declaration of competing interest
All the authors declare no conflict of interest, financial or otherwise.
Acknowledgements
We would like to acknowledge the help of the photography service of Jules Gonin Eye Hospital for preparing the manuscript images.
Contributor Information
Vasilios Batis, Email: vasileios.batis@fa2.ch.
Céline Häller, Email: celine.haller@fa2.ch.
Kattayoon Kate Hashemi, Email: kattayoon.hashemi@fa2.ch.
References
- 1.Cogan D.G., Kuwabara T. Lipid keratopathy and atheroma. Circulation. 1958 Oct;18(4 Part 1):519–525. [PubMed] [Google Scholar]
- 2.Hall M.N., Moshirfar M., Amin-Javaheri A., Ouano D.P., Ronquillo Y., Hoopes P.C. Lipid keratopathy: a review of pathophysiology, differential diagnosis, and management. Ophthalmol Ther. 2020;9(4):833–852. doi: 10.1007/s40123-020-00309-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gupta D., Illingworth C. Treatments for corneal neovascularization: a review. Cornea. 2011;30(8):927–938. doi: 10.1097/ICO.0b013e318201405a. [DOI] [PubMed] [Google Scholar]
- 4.Kim S.W., Ha B.J., Kim E.K., Tchah H., Kim T.I. The effect of topical bevacizumab on corneal neovascularization. Ophthalmology. 2008 Jun;115(6):e33–e38. doi: 10.1016/j.ophtha.2008.02.013. [DOI] [PubMed] [Google Scholar]
- 5.Rosenstein J.M., Krum J.M. New roles for VEGF in nervous tissue--beyond blood vessels. Exp Neurol. 2004 Jun;187(2):246–253. doi: 10.1016/j.expneurol.2004.01.022. [DOI] [PubMed] [Google Scholar]
- 6.Ferrari G., Dastjerdi M., Okanobo A., et al. Topical ranibizumab as a treatment of corneal neovascularization. Cornea. 2013;32(7):992–997. doi: 10.1097/ICO.0b013e3182775f8d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Faraj L.A., Elalfy M.S., Said D.G., Dua H.S. Fine needle diathermy occlusion of corneal vessels. Br J Ophthalmol. 2014 Sep;98(9):1287–1290. doi: 10.1136/bjophthalmol-2014-304891. [DOI] [PubMed] [Google Scholar]
- 8.Pillai C.T., Dua H.S., Hossain P. Fine needle diathermy occlusion of corneal vessels. Investig Ophthalmol Vis Sci. 2000 Jul;41(8):2148–2153. [PubMed] [Google Scholar]
- 9.Bucher F., Bi Y., Gehlsen U., Hos D., Cursiefen C., Bock F. Regression of mature lymphatic vessels in the cornea by photodynamic therapy. Br J Ophthalmol. 2014;98(3):391–395. doi: 10.1136/bjophthalmol-2013-303887. [DOI] [PubMed] [Google Scholar]
- 10.Baer J.C., Foster C.S. Corneal laser photocoagulation for treatment of neovascularization. Efficacy of 577 nm yellow dye laser. Ophthalmology. 1992;99(2):173–179. [PubMed] [Google Scholar]
- 11.Klöti R. Bipolar wet-field diathermy in microsurgery. Klin Monatsblätter Augenheilkd. 1984;184(5):442–444. doi: 10.1055/s-2008-1054517. [DOI] [PubMed] [Google Scholar]
- 12.Gassmann F., Schimmelpfennig B., Klöti R. Anterior capsulotomy by means of bipolar radio-frequency endodiathermy. J Cataract Refract Surg. 1988;14(6):673–676. doi: 10.1016/s0886-3350(88)80040-3. [DOI] [PubMed] [Google Scholar]
- 13.Kymionis G., Voulgari N., Grentzelos M., Aliferis K., Hashemi K., Mikropoulos D. Use of radiofrequency diathermy for the treatment of chronic corneal neovascularization with lipid keratopathy. Open Ophthalmol J. 2019;13(1):65–67. [Google Scholar]
- 14.Barbariga M., Fonteyne P., Ostadreza M., Bignami F., Rama P., Ferrari G. Substance P modulation of human and murine corneal neovascularization. Investigative Opthalmology & Visual Science. 2018;59(3):1305. doi: 10.1167/iovs.17-23198. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.