Summary
Background
Movement towards Universal Health Coverage (UHC) can improve health services, risk factor management, and inequality in non-communicable diseases (NCD); conversely, prioritizing and monitoring NCD management can support pathways to UHC in resource-limited settings. We aimed to estimate trends in NCD management indicators in Vietnam from 2010, and projections to 2030 at national and sub-national levels; compute the probability of reaching UHC targets; and measure inequalities in NCD management indicators at demographic, geographic, and socio-economic levels.
Methods
We included data of 37,595 households from four nationally representative surveys from 2010. We selected and estimated the coverage of NCD health service and risk management indicators nationally and by six sub-national groups. Using Bayesian models, we provided trends and projections and calculated the probability of reaching UHC targets of 80% coverage by 2030. We estimated multiple inequality indices including the relative index of inequality, slope index of inequality, and concentration index of inequality, and provided an assessment of improvement in inequalities over the study period.
Findings
Nationally, all indicators showed a low probability of achieving 2030 targets except sufficient use of fruit and vegetables (SUFV) and non-use of tobacco (NUT). We observed declining trends in national coverage of non-harmful use of alcohol (NHUA), sufficient physical activity (SPA), non-overweight (NOW), and treatment of diabetes (TOD). Except for SPA, no indicator showed the likelihood of achieving 2030 targets at any regional level. Our model suggested a non-achievement of 2030 targets for all indicators in any wealth quintile and educational level, except for SUFV and NUT. There were diversities in tendency and magnitude of inequalities with widening gaps between genders (SPA, TOD), ethnic groups (SUFV), urban-rural areas (TOH), wealth quintiles, and educational levels (TOD, NUT, NHUA).
Interpretation
Our study suggested slow progress in NCD management at the national level and among key sub-populations in Vietnam, together with existing and increasing inequalities between genders, ethnicities, geographic areas, and socioeconomic groups. We emphasised the necessity of continuously improving the healthcare system and facilities, distributing resources between geographic areas, and simultaneously integrating economic, education, and gender intervention and programs.
Funding
None.
Keywords: Tobacco smoking, Use of alcohol, Use of fruit and vegetables, Physical activity, Overweight, Diabetes, High cholesterol, Cervical cancer
Research in context.
Evidence before this study
We performed a systematic search in PubMed for literature and studies related to evaluating non-communicable disease (NCD) management and progress toward Universal Health Coverage (UHC) in Vietnam in English and Vietnamese before June 1st, 2022. We found no study accessed the trends in, projections of NCD management indicators in Vietnam at national and sub-national levels. None estimated the probability of achieving the 2030 targets at national and sub-national levels. Also, none presented the comprehensive inequality analyses in NCD management indicators in Vietnam with estimations, patterns, and trends of inequalities between demographic, geographic, and socioeconomic groups.
Added value of this study
This study provided to the best of our knowledge the first comprehensive picture of NCD management indicators and progress toward UHC in Vietnam at national and sub-national levels based on nationally-representative data. In addition, it applied Bayesian statistics to estimate the probabilities of accomplishing the UHC targets by 2030. Furthermore, our comprehensive inequality analyses with estimations, patterns, and trends in demographic, geographic, and socioeconomic inequalities could thoroughly support the government and policymakers in revising and updating future equity-oriented interventions and programs. Although we observed significant improvements in some prevention and treatment indicators from 2010–2015, our data suggested no achievement of 2030 targets for the majority of NCD indicators at either national or sub-national levels. Our inequality analysis showed existing and, in some cases, widening demographic, geographic, and socioeconomic inequalities in numerous NCD indicators with different patterns and trends, which in turn may restrict the chances of UHC achievement in Vietnam.
Implications of all the available evidence
Our study suggested slow progress in NCD management at the national level and among key sub-populations in Vietnam, together with existing and increasing inequalities between genders, ethnicities, geographic areas, and socioeconomic groups. We emphasized the necessity of continuously improving the healthcare system and facilities and further research in the area.
Alt-text: Unlabelled box
Introduction
Non-communicable diseases (NCDs), also known as chronic diseases, accounted for the largest portion of the global burden of disease with 41·1 million deaths (73·4%) and 874,500 (53·0%) years of life lost (YLL) in 2017, a 22·7% increase in deaths and 13·6% increase in YLLs from 2007.1 Four common modifiable behavioral risk factors – tobacco use, unhealthy diet, low physical activity, and harmful use of alcohol – contributed to 67% of NCDs-attributable deaths and disability-adjusted life-years (DALY).2 Thus, lessening these four modifiable risk factors is the key goal of the “best-buys” interventions of the World Health Organization (WHO),3 a set of cost-effective and highly feasible interventions that would reduce the economic losses due to NCDs in low- and middle-income countries (LMICs) by an average of US$ 25 billion per country annually.4 Since the 2000s, WHO has developed many other global strategies and action plans which comprehensively contributed to the prevention and control of NCDs,5, 6, 7, 8 toward the ultimate goal of health for all.9 In parallel, global initiatives to establish equity-oriented health information systems are increasing. Universal Health Coverage (UHC), which aims to ensure healthcare services in LMICs are available to all people in need without financial hardship, is a core part of these plans. Specifically, UHC targets that by 2030 at least 80% of the population can access quality healthcare services regardless of socioeconomic status or geographic area.10 Although many NCDs historically were known as “diseases of the rich”, the burden of NCDs has been chiefly concentrated in LMICs with 31.4 million deaths (76% global NCD-caused deaths).1 Thus, progressing toward UHC can improve health services, risk factor management, and inequality in NCDs; conversely, prioritizing and monitoring NCD managements can support pathways to UHC among those resource-limited settings.11 Hence, monitoring the progress towards these targets and trends in NCD-related risk management is critical for supporting those governments and policymakers in improving health policies and programs.
As a lower middle-income country, Vietnam has been suffering the accelerating burden of NCDs due to rapid urbanization, economic development, and population ageing.12 In particular, there were 318,425 deaths, 6·7 million YLLs, and 14 million DALYs related to NCDs, accounting for 72%, 56%, and 66% of total deaths, YLLs, and DALYs in 2010 in Vietnam, respectively.13 This country has shown increasing trends in NCD-related hospital admissions (from 38% to 66%) and deaths (from 42% to 73%) in the period 1986–2015.14 The Vietnamese government has early recognized the massive impact of NCDs on population health by implementing two phases of the National Program on NCD Prevention & Control (2002–2010 and 2010–2015). The updated National Strategy on Prevention and Control of NCDs predominantly centralized prevention activities (behavior change communication, screening, and early detection), treatment management, and capacity enhancement.15 However, recent studies showed the lack of accessibility to NCD treatment services,16 inadequate coverage of preventive services (to control risk factors),17 and the insufficient quality and quantity of human resources for health may hamper NCD management progress.18 Additionally, there are existing inequalities in readiness, availability, and utilization of NCD services in primary healthcare facilities.19
The rapid demographic and social transitions also pose difficulties in achieving UHC and health equity in Vietnam.20 World Bank reported that impoverished people are the most disadvantaged groups with higher disease risk but a lower chance of receiving healthcare services.21 In addition, Vietnam is generally categorized into 6 regions with diverse ethnic (54 ethnic groups), demographic, geographic, and socioeconomic characteristics. Thus, this country is threatened by multiple dimensions of inequalities in health.22 Our previous work showed the slow progress toward UHC in Vietnam with rising inequalities in some maternal, newborn, and child health indicators.23 As Vietnam enters the epidemiological transition, monitoring the trends in coverage of NCD services and risk factor managements, and measuring the inequalities between sub-national levels should be prioritized to ensure the achievement of UHC in this developing country. However, no previous study has provided this critical evidence-based information from a nationally-representative design.
In the present study, we aimed to estimate trends in NCD management indicators in Vietnam from 2010 and projections up to 2030 at national and sub-national levels and compute the probability of accomplishing UHC targets by 2030. We presented a comprehensive measure of inequality in NCD management in Vietnam with estimations and trends for demographic, geographic, and socioeconomic inequalities in NCD management indicators.
Methods
This is a secondary data analysis using data from the Vietnam STEPwise Approach to NCD Risk Factor Surveillance (VSTEPS) and Vietnam Global Adult Tobacco Survey (VGATS). Detailed descriptions of sampling method and participant recruitment are presented elsewhere,24,25 while information of included surveys is in Supplementary Table S1. In brief, these surveys are nationally representative household surveys using a two-stage cluster sampling method targeted to men and women who are aged 15 and above and mainly reside in Vietnam, and did not include those who resided in military-based or other institutions (e.g., hospitals, prisons, nursing homes, etc.). In the present analysis, we included 37,595 households from four datasets from 2010 to 2015.
Measurement of NCD prevention and control
We selected NCD health service and risk management indicators from within WHO's global monitoring frameworks and indicators (“best-buys”,3 NCD framework,26 UHC framework,27 and global health indicator28) and based on available data in Vietnam. We finally collected four prevention indicators including non-use of tobacco (NUT), non-harmful use of alcohol (NHUA), sufficient physical activity (SPA), and sufficient use of fruit and vegetables (SUFV); and five treatment indicators including non-overweight (NOW), screening for cervical cancer (SCC), treatment of diabetes (TOD), treatment of hypertension (TOH) and treatment of high cholesterol (TOHC). We estimated the coverage of these indicators for each survey and year nationally and stratified by gender (men and women), ethnicity (Kinh ethnic and other minorities), living area (urban and rural), region (Northern mountainous, Red river delta, Central Coast, Central Highlands, Southeast, and Mekong river delta), wealth quintile (richest, richer, middle, poorer, poorest) and educational level (lower than primary school, primary school, secondary school, high school, university and higher). Details of estimated indicators with definition, denominator, numerator and data source are described in Supplementary Table S2. To make adequate statistical inferences for the Vietnamese population, we adjusted all the estimated coverages for complex survey design including sampling weights, clustering, and stratification using the survey package.29 Several composite indices of service coverage have been developed for tracking the progress toward Universal Health Coverage by aggregating, arithmetic averaging, or geometric averaging of weighted individual indicators.30, 31, 32 In this study, we derived composite indicators of prevention (i.e., coverage of controlling four main risk factors), treatment (i.e., coverage of controlling overweight, diabetes, and hypertension), and management (all indicators) using random-effect meta-analysis, similar to a previous study in reproductive, maternal, newborn and child health.23
Measurement of inequalities
To provide a comprehensive analysis of inequality in NCD management, we used multiple indices of inequality including the relative index of inequality (RII), slope index of inequality (SII), and the concentration index of inequality (CnI). The RII and SII indicate the relative ratio and absolute difference in percentage points of coverages between the most advantaged and disadvantaged sub-groups, while the CnI presents the magnitude or extent of inequality.23 We examined multiple dimensions of inequality including participant's gender, ethnic group (Kinh vs. other minorities), living area (urban vs. rural), regional level (highest coverage vs. lowest coverage regions), household wealth (richest vs. poorest), and educational level (university and higher vs. lower than primary). Additionally, we evaluated the improvement in relative, absolute, and extent inequalities in the period by calculating the differences in RII, SII, and CnI between two time points (the years 2010 and 2015). We estimated the 95% Confidence Intervals (CIs) and p-values for significance assessment of improvement in inequalities over the period.
Principal component analysis
We measured wealth inequalities using the household income status or asset-based wealth index, which were created by ranking the household income or wealth score into quintiles. Because the VGATS datasets did not contain household income information, we estimated asset-based wealth index by applying principal component analysis (PCA) to available variables of housing assets and services,33 which is regularly performed in Demographic and Health Surveys (DHS) and Multiple Indicator Cluster Surveys (MICS).34 Specifically, we performed PCA on different sets of household assets and services for rural and urban areas, then applied a regression-based method to estimate the national wealth score from urban- and rural-specific scores, which allows adjustments for contextual variation between urban and rural areas.34 Details of the Stata commands and results are in the Supplementary file.
Multiple imputation approach
The VSTEPS datasets encompassing household income information have high proportions of missing values (15·7% in our data – not shown). Additionally, the missing income patterns cannot be assumed as missing completely at random as it can depend on other variables' values.35 Thus, the conventional practice of “listwise deletion”, which eliminates missing values in any analysing variables, can cause bias and should not be used. The multiple imputation approach has been commonly used for handling missing income data in national health surveys using the widely accepted assumption of missing at random in previous works.35,36 In this study, we applied multiple imputation using the fully conditional specification (FCS) basis and predictive mean matching (PMM) algorithm for reducing bias in estimating trends and inequalities.37
Statistical analysis
Bayesian models were applied to produce the posterior predictive distributions of the indicators for calculating the probability of reaching UHC targets by 2030. The use of Bayesian modeling allowed for the calculation of specific probabilities of meeting targets and crossing specific thresholds, which is impossible with non-Bayesian models since classical confidence intervals do not allow the estimation of specific probabilities of predictions within specific ranges.38 In national models, we applied Bayesian linear regression with logit transformed values of all coverage indicators as the dependent variables and survey year as an independent variable. In models that were stratified by subgroups (wealth quintile, educational level, urban-rural area, gender, and ethnic group), we included and tested the interaction terms between these variables and survey year using the leave-one-out cross-validation method.39 Particularly, for models of regional level, we applied the Bayesian mixed-effect models and tested the significance of random slope to assess the variations between regions over time.40 Details of covariate selections are in Supplementary Tables S3-S8. We fitted a series of 240 models using a Markov Chain Monte Carlo (MCMC) algorithm with 5000 samples, 1000 for burn-in, two chains, and thinning two times. We used the potential scale reduction factor and trace plots for model diagnosis.38 We calculated the probability of achieving UHC targets (as of 80% coverage) for NCD health service indicators and the average annual percentage of change over study periods. Rubin's rules were applied to pool parameter estimates from Bayesian models and to derive confidence intervals of inequality indices of imputed wealth quintile.38,41,42 All statistical analyses (except PCA) were performed in R (version 4.1.1).
Sensitivity analysis
We performed a sensitivity analysis of composite indices by applying two other aggregate methods of arithmetic and geometric average of equally-weighted individual indicators to produce national and sub-national estimations. We then included them in Bayesian models for trend and projection analysis and compared their results with those of random-effect meta-analysis.
Ethical statement: The present study did not require ethical approval because it is based on de-identified publicly available data.
Role of the funding source
The authors did not receive any funds for conducting this study. PN, SG, HVN, MH, and BT had access to the raw data. PN had full access to all the data and had final responsibility for the decision to submit for publication.
Results
Trends in and projections of NCD management coverage and probability of achieving targets by 2030
Table 1 describes the national coverage of NCD indicators in Vietnam from 2010 to 2030, with estimations from observed data (2010 and 2015) and projections from Bayesian models (2020 and 2030). All indicators showed a very low probability (0%) of achieving 2030 targets except sufficient use of fruit and vegetables (SUFV) and non-use of tobacco (NUT). We observed negative average annual percentage change (AAPC) in non-harmful use of alcohol (NHUA), sufficient physical activity (SPA), non-overweight (NOW), and treatment of diabetes (TOD), which indicated declining trends in coverage of those indicators in 2010–2030. Supplementary Table S9 shows the AAPC of all NCD health service and management indicators in 2010–2015, 2015–2020, and 2020–2030.
Table 1.
National coverage of Non-Communicable Disease management indicators.
| Indicators | Estimated coverage (95% CI) |
Predicted coverage (95% CrI) |
AAPC from 2010–2030 (95% CrI) | Probability reach target (%)† | ||
|---|---|---|---|---|---|---|
| Year 2010 | Year 2015 | Year 2020 | Year 2030 | |||
| Non-use of tobacco | 74·2 (73·4 to 75·0) | 77·5 (76·2 to 78·7) | 80·4 (78·9 to 82·0) | 85·5 (82·7 to 88·0) | 0·6 (0·4 to 0·7) | 100·0 |
| Non-harmful use of alcohol | 80·1 (79·1 to 81·0) | 76·2 (74·1 to 78·1) | 71·8 (68·6 to 74·8) | 61·8 (53·9 to 68·9) | -0·9 (-1·3 to -0·5) | 0·0 |
| Sufficient physical activity | 69·2 (68·0 to 70·4) | 71·2 (68·9 to 73·3) | 73·0 (69·9 to 75·7) | 76·6 (70·4 to 81·5) | 0·4 (0·0 to 0·6) | 9·2 |
| Sufficient use of fruit and vegetables | 18·3 (17·2 to 19·5) | 42·9 (40·2 to 45·5) | 71·5 (68·7 to 74·2) | 96·5 (95·5 to 97·4) | 3·9 (3·8 to 4·0) | 100·0 |
| Non-overweight | 88·0 (87·2 to 88·9) | 84·5 (82·7 to 86·1) | 80·0 (76·7 to 83·1) | 68·6 (59·1 to 76·9) | -1·0 (-1·5 to -0·5) | 0·4 |
| Treatment of diabetes | 50·9 (45·5 to 56·3) | 38·8 (32·2 to 46·0) | 27·9 (16·7 to 42·0) | 12·6 (3·5 to 35·5) | -1·9 (-2·6 to -0·6) | 0·0 |
| Treatment of hypertension | 25·4 (24·0 to 26·9) | 29·1 (26·3 to 32·1) | 32·9 (26·9 to 39·5) | 41·4 (28·1 to 56·2) | 0·8 (0·1 to 1·6) | 0·0 |
| Composite NCD Prevention | 60·6 (59·8 to 61·4) | 67·5 (65·9 to 68·9) | 73·6 (70·8 to 76·2) | 83·4 (79·0 to 87·0) | 1·1 (0·9 to 1·3) | 93·2 |
| Composite NCD Treatment | 56·1 (50·7 to 61·3) | 51·6 (44·5 to 58·6) | 47·2 (32·4 to 61·5) | 38·2 (14·1 to 68·6) | -0·9 (-2·2 to 0·8) | 0·2 |
| Composite NCD Service Coverage | 58·8 (53·4 to 64·0) | 61·2 (54·0 to 67·8) | 63·6 (48·4 to 76·2) | 68·3 (35·9 to 88·8) | 0·5 (-1·3 to 1·7) | 18·1 |
Notes:
WHO's targets of at least 80% health service coverage for the entire population by 2030 for Universal Health Coverage; 95% CI = 95% Confidence Interval; 95% CrI = 95% Credible Interval; AAPC=Average annual percentage change; The observed coverages during 2010–2015 were calculated based on the original datasets; NCD: Non-communicable disease.
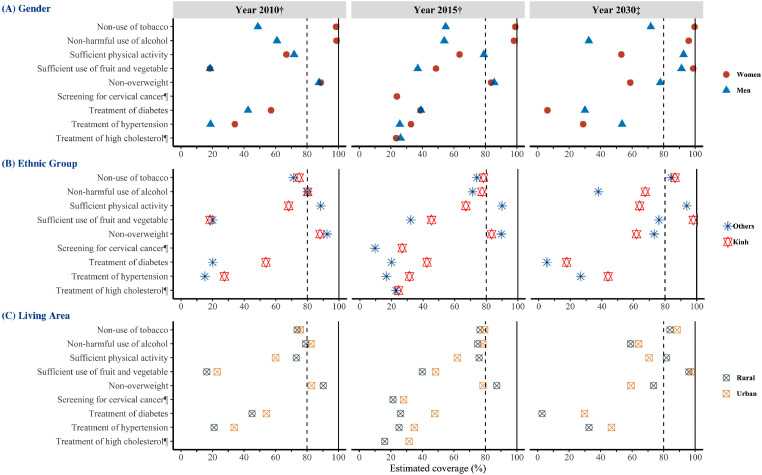
Figure 1 shows the estimates of all NCD indicators stratified by gender (A), ethnic group (B), and living area (C) in the years 2010, 2015, and projections to 2030. We observed discrepancies in NCD management coverages between men and women. While women would achieve the 2030 targets in NUT and NHUA, men were lagging in those indicators and had no chance of reaching 80% coverage by 2030. In contrast, women were left behind in SPA, NOW, and TOH. In the latest available survey (2015), we observed that minority ethnic and those living in rural areas were left behind in most of the NCD indicators, compared to Kinh (majority ethnic) and those living in urban, except for SPA and NOW. We predicted no achievement of 2030 targets for all indicators in any ethnic groups or living areas, except for SUFV and NUT. The results of the stratified analyses by gender, ethnic group, and living area are provided in Supplementary Tables S10–S12.
Figure 1.
Observations and projections of Non-communicable disease management indicators in Vietnam by (A) Gender; (B) Ethnic group; and (C) Living area. Notes: † Estimation from observed data in 2010 and 2015; ‡ Projections from Bayesian models; ¶ Only data in 2015 is available; The colored shapes are the estimated and projected values for wealth quintile levels; the horizontal axis shows coverage scales from 0–100%; the horizontal dotted lines present the UHC targets of 80% coverage.
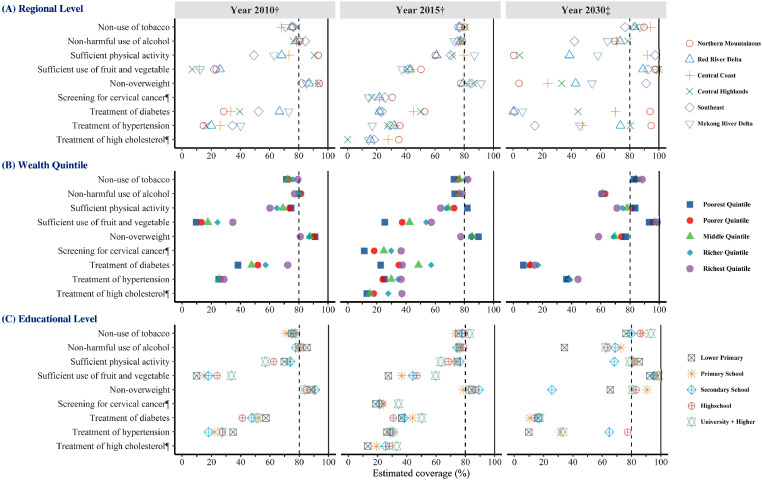
Figure 2 presents the estimates of all NCD indicators by regional level (A), wealth quintile (B), and educational level (C) in the year 2010, 2015 and projections to 2030. Regarding the regional level, except for SUFV, no indicators showed the likelihood of achieving 2030 targets in any region. Additionally, we observed diversities in coverages of NCD indicators between regions. While the Southeast and Central coast regions would reach the 2030 targets for some prevention indicators (NOW, NUT), they would be left behind in treatment indicators. In contrast, the Northern mountainous and Central highland regions would reach the targets for treatment indicators (TOD and TOH), but they would be left behind in some prevention indicators. Regarding wealth quintiles, the most impoverished people would be left behind in most of the indicators, except, for NOW, NHUA, and SPA. However, we predicted no achievement of 2030 targets for all indicators in any wealth quintile, except for SUFV and NUT. Regarding educational levels, the lowest educational levels would be left behind in most indicators, except for SPA. Similar to wealth quintiles, we predicted no achievement of 2030 targets for all indicators in any educational levels except for SUFV and NUT. The results of the stratified analyses by regional level, wealth quintile (completed and imputed data), and educational level, are included in Supplementary Tables S13–S16. The national and sub-national results for the NCD composite indicators (overall, prevention, and treatment) are shown in Supplementary Figures S1–S3. Our sensitivity analysis showed comparable outcomes between random-effect meta-analysis and alternative methods (geometric average and arithmetic average) by gender, ethnic group, living area, regional level, wealth quintile, and educational level (Supplementary Tables S17–S22). Supplementary Figures S4–S10 present the trends in and projections of all NCD indicators at stratified groups.
Figure 2.
Observations and projections of Non-communicable disease management indicators in Vietnam by (A) Regional level; (B) Wealth quitile; and (C) Educational level. † Estimation from observed data in 2010 and 2015; ‡ Projections from Bayesian models; ¶ Only data in 2015 is available; The colored shapes are the estimated and projected values for wealth quintile levels; the horizontal axis shows coverage scales from 0–100%; the horizontal dotted lines present the UHC target of 80% coverage;
Estimations and trends in inequalities in NCD management indicators
Table 2 presents the relative, slope, and concentration indices of inequality in all NCD indicators in 2015 by gender, ethnic group, urban-rural setting, region, wealth quintile, and educational level. Although there were statistically significant inequalities in NCD indicators across all indices (RII, SII, and CnI), we observed diversities in the tendency and magnitude of inequalities between inequality sites (stratified variables). Most NCD indicators had a higher concentration of coverage among women than among men, except SPA and treatment of high cholesterol (TOHC). Gender inequality showed the most significant gap in NUT and NHUA with RII of 0·18 and 0·29, SII of -92·80 and -90·88, and CnI of -0·15 and -0·14, respectively. Ethnic inequality also existed, with minority groups lagging behind in all NCD management indicators, excluding SPA, and the highest gap was observed in screening for cervical cancer (SCC) with RII=5·89 (95% CI: 5·15 to 6·72), SII=32·52 (30·79 to 34·26), and CnI=0·09 (0·08 to 0·10). Both geographic inequalities (rural-urban and regional inequalities) had the highest gap in TOH and TOHC. Socioeconomic inequalities (wealth and education inequalities) showed the most significant gap in SCC, TOHC, and SUFV, with no statistically significant inequalities in NHUA and TOH. The inequality analyses of the year 2010 are shown in Supplementary Table S23. The sub-analyses of wealth inequalities stratified by gender, ethnic group, and living area is in Supplementary Table S24–26.
Table 2.
Inequality analyses of Non-Communicable Disease management in Vietnam in year 2015.
| Indicators | Index | Gender inequality | Ethnic inequality | Urban-Rural Inequality | Regional Inequality | Wealth Inequality | Educational Inequality |
|---|---|---|---|---|---|---|---|
| Non-use of tobacco | RII | 0·28 (0·28 to 0·28)*** | 1·15 (1·13 to 1·17)*** | 1·08 (1·07 to 1·09)*** | 1·09 (1·08 to 1·10)*** | 1·15 (1·11 to 1·20)*** | 1·11 (1·10 to 1·12)*** |
| SII | -92·80 (-93·49 to -92·11)*** | 10·52 (9·39 to 11·65)*** | 6·24 (5·49 to 6·98)*** | 6·97 (6·30 to 7·63)*** | 11·07 (8·07 to 14·06)*** | 8·26 (7·60 to 8·92)*** | |
| CnI | -0·15 (-0·15 to -0·15)*** | 0·01 (0·01 to 0·01)*** | 0·01 (0·01 to 0·01)*** | 0·01 (0·01 to 0·02)*** | 0·02 (0·02 to 0·03)*** | 0·02 (0·01 to 0·02)*** | |
| Non-harmful use of alcohol | RII | 0·29 (0·28 to 0·29)*** | 1·09 (1·07 to 1·11)*** | 1·10 (1·08 to 1·11)*** | 1·11 (1·09 to 1·12)*** | 1·02 (0·96 to 1·08) | 0·98 (0·97 to 0·99)** |
| SII | -90·88 (-91·96 to -89·81)*** | 6·70 (5·11 to 8·30)*** | 7·25 (6·09 to 8·41)*** | 7·93 (6·90 to 8·96)*** | 1·38 (-3·32 to 6·08) | -1·52 (-2·55 to -0·49)** | |
| CnI | -0·14 (-0·15 to -0·14)*** | 0·01 (0·00 to 0·01)*** | 0·01 (0·01 to 0·01)*** | 0·02 (0·01 to 0·02)*** | 0·00 (-0·01 to 0·01) | -0·00 (-0·01 to -0·00)** | |
| Sufficient physical activity | RII | 1·34 (1·31 to 1·36)*** | 0·63 (0·62 to 0·64)*** | 0·72 (0·70 to 0·73)*** | 1·58 (1·56 to 1·61)*** | 0·76 (0·71 to 0·82)*** | 0·86 (0·85 to 0·87)*** |
| SII | 20·84 (19·59 to 22·08)*** | -35·71 (-37·08 to -34·34)*** | -23·81 (-25·07 to -22·56)*** | 32·38 (31·32 to 33·44)*** | -19·24 (-24·27 to -14·20)*** | -11·12 (-12·23 to -10·01)*** | |
| CnI | 0·04 (0·03 to 0·04)*** | -0·04 (-0·04 to -0·03)*** | -0·04 (-0·04 to -0·04)*** | 0·07 (0·07 to 0·07)*** | -0·04 (-0·05 to -0·03)*** | -0·03 (-0·03 to -0·02)*** | |
| Sufficient use of fruit and vegetables | RII | 0·60 (0·58 to 0·62)*** | 2·06 (1·96 to 2·18)*** | 1·47 (1·42 to 1·52)*** | 1·51 (1·46 to 1·55)*** | 2·68 (2·35 to 3·05)*** | 2·29 (2·22 to 2·35)*** |
| SII | -21·61 (-22·99 to -20·23)*** | 27·58 (25·82 to 29·34)*** | 16·53 (15·15 to 17·91)*** | 17·32 (16·09 to 18·54)*** | 43·14 (37·82 to 48·46)*** | 35·38 (34·19 to 36·56)*** | |
| CnI | -0·06 (-0·07 to -0·06)*** | 0·04 (0·04 to 0·05)*** | 0·05 (0·04 to 0·05)*** | 0·06 (0·06 to 0·07)*** | 0·16 (0·14 to 0·18)*** | 0·13 (0·13 to 0·14)*** | |
| Non-overweight | RII | 1·07 (1·05 to 1·08)*** | 0·87 (0·85 to 0·88)*** | 0·83 (0·82 to 0·84)*** | 1·22 (1·21 to 1·24)*** | 0·85 (0·80 to 0·90)*** | 1·05 (1·04 to 1·06)*** |
| SII | 5·41 (4·24 to 6·58)*** | -12·09 (-13·45 to -10·73)*** | -15·28 (-16·46 to -14·09)*** | 16·69 (15·69 to 17·70)*** | -13·25 (-18·02 to -8·49)*** | 4·08 (3·05 to 5·11)*** | |
| CnI | 0·01 (0·01 to 0·01)*** | -0·01 (-0·01 to -0·01)*** | -0·02 (-0·02 to -0·02)*** | 0·03 (0·03 to 0·03)*** | -0·02 (-0·03 to -0·02)*** | 0·01 (0·01 to 0·01)*** | |
| Screening for cervical cancer | RII | NA | 5·89 (5·15 to 6·72)*** | 1·93 (1·81 to 2·06)*** | 2·27 (2·14 to 2·41)*** | 4·40 (3·34 to 5·80)*** | 2·01 (1·90 to 2·13)*** |
| SII | NA | 32·52 (30·79 to 34·26)*** | 16·32 (14·70 to 17·94)*** | 19·94 (18·53 to 21·35)*** | 35·74 (29·64 to 41·83)*** | 16·69 (15·27 to 18·10)*** | |
| CnI | NA | 0·09 (0·08 to 0·10)*** | 0·08 (0·07 to 0·09)*** | 0·13 (0·12 to 0·14)*** | 0·23 (0·19 to 0·27)*** | 0·11 (0·10 to 0·12)*** | |
| Treatment of diabetes | RII | 0·59 (0·55 to 0·65)*** | 3·14 (2·68 to 3·67)*** | 2·12 (1·95 to 2·30)*** | 2·18 (2·02 to 2·35)*** | 1·87 (1·33 to 2·63)*** | 1·28 (1·19 to 1·38)*** |
| SII | -16·26 (-18·85 to -13·67)*** | 29·07 (25·88 to 32·26)*** | 23·31 (20·73 to 25·90)*** | 26·19 (23·94 to 28·44)*** | 19·14 (8·73 to 29·55)*** | 7·84 (5·54 to 10·13)*** | |
| CnI | -0·07 (-0·08 to -0·05)*** | 0·06 (0·05 to 0·07)*** | 0·09 (0·08 to 0·10)*** | 0·13 (0·11 to 0·14)*** | 0·10 (0·05 to 0·15)*** | 0·04 (0·03 to 0·05)*** | |
| Treatment of hypertension | RII | 0·63 (0·53 to 0·73)*** | 4·48 (3·15 to 6·36)*** | 3·38 (2·80 to 4·08)*** | 3·30 (2·84 to 3·84)*** | 1·62 (0·86 to 3·06) | 1·01 (0·88 to 1·16) |
| SII | -18·16 (-24·23 to -12·10)*** | 44·66 (37·06 to 52·26)*** | 43·60 (37·67 to 49·53)*** | 44·93 (39·79 to 50·06)*** | 20·99 (-3·40 to 45·39) | 0·32 (-5·07 to 5·71) | |
| CnI | -0·06 (-0·08 to -0·04)*** | 0·07 (0·05 to 0·08)*** | 0·13 (0·11 to 0·15)*** | 0·18 (0·16 to 0·20)*** | 0·08 (-0·02 to 0·18) | 0·00 (-0·02 to 0·02) | |
| Treatment of high cholesterol | RII | 1·31 (1·13 to 1·52)*** | 1·59 (1·22 to 2·07)** | 3·19 (2·72 to 3·74)*** | 3·57 (3·10 to 4·11)*** | 3·45 (1·85 to 6·44)*** | 2·30 (2·02 to 2·62)*** |
| SII | 6·99 (3·08 to 10·90)*** | 10·60 (5·04 to 16·16)*** | 27·77 (24·19 to 31·35)*** | 28·68 (25·57 to 31·78)*** | 28·14 (13·98 to 42·30)*** | 20·91 (17·74 to 24·07)*** | |
| CnI | 0·03 (0·01 to 0·05)*** | 0·02 (0·01 to 0·03)*** | 0·14 (0·12 to 0·15)*** | 0·18 (0·16 to 0·20)*** | 0·19 (0·09 to 0·28)*** | 0·13 (0·11 to 0·15)*** |
Notes: RII=Relative Index of Inequality; SII=Slope Index of Inequality; CnI=Concentrate Index of Inequality; ***, **, * Statistically significant results with p < 0·001, p < 0·01, and p < 0·05, respectively; CI=Confidence Interval; The inequality analyses of NCD indicators in 2010 are in the Supplementary.
RII shows the ratio of health service coverage in comparison groups (i.e., gender, ethnic group, living area, regional level, wealth quintile, educational level) between the top and bottom categories (e.g., men/women, majority/minorities, urban/rural, richest/poorest, etc.). Interpretation: RII=1 (p-value>0·05) suggests insufficient evidence of inequality in health service coverage, RII<1 (p-value<0·05) suggests pro-bottom inequality (higher coverage in bottom category than in top category), RII>1 suggests pro-top inequality (higher coverage in top category than in bottom category);
Similarly, SII presents the difference in percentage points of health service coverage between the top and bottom categories of comparison groups (gender, ethnic group, living area, regional level, wealth quintile, educational level). Interpretation: SII=0 (p-value>0·05) suggests insufficient evidence of inequality in health service coverage, SII<0 (p-value<0·05) suggests pro-bottom inequality (higher coverage in bottom category than in top category), SII>0 suggests pro-top inequality (higher coverage in top category than in bottom category);
CnI ranges from -1 to 1 and indicates the magnitude or extent of inequality in health service coverage. Interpretation: CnI=0 (p-value>0·05) suggests insufficient evidence of inequality in health service coverage, CnI<0 (p-value>0·05) suggests pro-bottom inequality (higher concentration of health service coverage in bottom category than in top category), CnI>0 suggests pro-top inequality (higher concentration of health service coverage in top category than in bottom category).
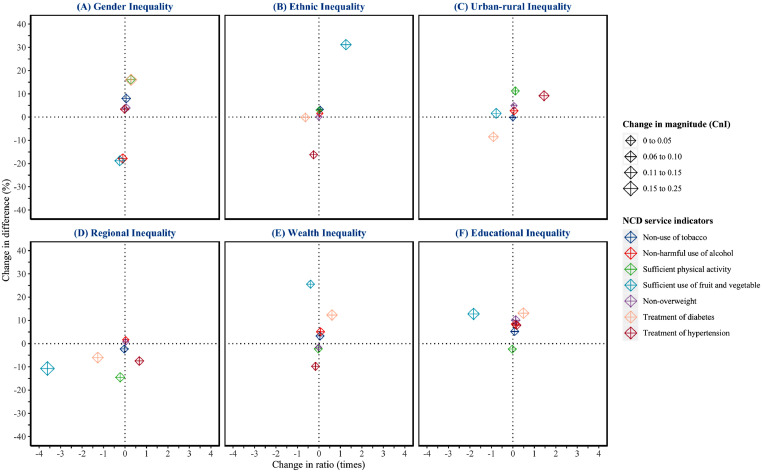
Figure 3 shows the NCD indicators with statistically significant changes in all inequality indices (RII, SII, and CnI) from 2010−2015. In each figure, the bottom-left quadrant shows the indicators with significant improvements in all three dimensions of inequality (relative, absolute, and magnitude terms) for gender inequality (SUVF, NHUA), ethnic inequality (TOH), urban-rural inequality (TOD), regional inequality (SUFV, NOW, SPA), wealth inequality (TOH, SPA) and educational inequality (SPA). In contrast, attention should be paid to those indicators with increasing trends in inequality (top-right corner) with widening gaps between genders (SPA, TOD), ethnic groups (SUFV), urban-rural areas (TOH), wealth quintiles, and educational levels (TOD, NUT, NHUA). Detailed estimates of changes in inequalities for all NCD management indicators from 2010−2015 with 95% CIs and p-values are in Supplementary Table S27. Supplementary Table S28–S30 describes the changes in socioeconomic inequalities stratified by gender, ethnic group, and urban-rural area.
Figure 3.
Changes in inequalities in Non-Communicable disease management in Vietnam from 2010–2015 (A) Gender inequality; (B) Ethnic inequality; (C) Urban-rural inequality; (D) Regional inequality; (E) Wealth inequality; and (F) Educational inequality. NCD indicators are expressed as colored diamond shapes, The horizontal axis shows changes in ratio = changes in relative index of inequality (RII) between two time points, the vertical axis shows changes in difference = changes in slope index of inequality (SII) between two time points; the size of the shapes indicates the change in magnitude = absolute changes in concentration index of inequality (CnI); Positive values suggest an increasing trend in inequality, and negative values express a decreasing trend in inequality.
Discussion
This study provides the first comprehensive picture of NCD management indicators and progress toward UHC in Vietnam at national and sub-national levels. Although we observed significant improvements in some prevention and treatment indicators from 2010–2015, most NCD indicators will not achieve the global targets by 2030 at either national or sub-national levels. Our inequality analysis showed existing and, in some cases, widening gender, ethnic, rural-urban, regional, socioeconomic, and educational inequalities in numerous NCD indicators with different patterns and trends, restricting the chances of UHC achievement in Vietnam.
For managing NCD risk factors and controlling NCD burdens in LMICs, WHO's best-buys are the most cost-effective interventions with a cost less than US$100 per DALY averted.3 They targeted improving physical activity, healthy diet, and reducing tobacco use and harmful use of alcohol in LMICs, with every single US$ invested in implementing these interventions estimated to return at least US$ 7 by 2030.43 Since Vietnam joined the WHO Framework Convention on Tobacco Control (WHO FCTC) in 2005,44 the country has made remarkable improvements in all components of MPOWER, a tobacco-free initiative with practical, affordable, and achievable interventions for effective tobacco control.45 In this study, however, we observed slow progress in non-use of tobacco in the study period and projected a limited chance of reaching the 2030 targets among men, which is consistent with previous research,25 and suggests only modest effectiveness of tobacco control programs in Vietnam. Concerns have been raised about the appropriateness and effectiveness of Vietnam's smoke-free regulations in preventing secondhand smoke in public places.46 Additionally, the WHO's report on the global tobacco epidemic 2021 showed that smoking cigarettes has become more affordable in Vietnam since 2010 as cigarette price per capita GDP decreased at an annual rate of over 1·45%.45 Although the inequality in NUT showed improvements since 2010, we still observed that men, those living in rural areas, those of minority ethnicity, the poor, and those of low educational levels were being left behind by tobacco control efforts. A particular tobacco consumption pattern in Vietnam is the prevalent use of traditional water pipes (thuốc lào) in rural areas, which remain affordable because they are not taxed, and are more acceptable than cigarettes among Vietnamese people due to misperceptions of lower health risks.17 Thus, further investigation of the health impact of smoking thuốc lào is needed, as well as tailor-made and well-designed interventions targeting vulnerable groups in rural settings should be initiated.
In the present study, we observed a declining trend in NHUA with no improvement in the study period and narrowed chance of achieving the 2030 targets. Vietnam has consistently reported a high level of alcohol consumption, with 8·3 litres per capita consumed in 2016 compared to a global average of 6·4 litres. This is a large increase on the 4·7 litres consumed in 2010 and is forecast to rise to 11·4 litres in 2025.47 To better prevent harmful use of alcohol and reduce alcohol-related harms in LMICs, in addition to the Global Strategy,7 WHO has launched the SAFER initiative with five high-impact strategies,48 and recommended best-buys and other highly cost-effectiveness interventions.3 Prior to 2016, Vietnam promoted several policies for controlling alcohol-related harm, including national policy, national action plan, excise taxes, restrictions in minimum age and specific locations for off-premise and on-premise sales, laws in drink driving, regulations on alcohol advertising and sponsorship. However, previous research identified poor implementation and compliance with those policies and regulations due to various factors, including the lack of strict monitoring systems and control policies,17 government's vested interests in alcohol manufacturing,49 and interference of the alcohol industry in policy processes (e.g., lobbying to nullify the key articles of laws and regulations).50 Our findings showed no significant inequality between wealth quintiles, suggesting that the current excise tax on alcoholic beverages may be insufficient in reducing alcohol use among poor people, as it is still quite low compared to other countries.49 Additionally, traditional alcohol production (home brewing) drinking cultures could be another challenge to alcohol-beverage taxations,51,52 as poor people may switch to these cheap, unregulated, homemade products once the alcohol price is unaffordable.53 Belatedly, the newly promulgated Law on prevention and control of alcohol-related harms, the first comprehensive alcohol law, has been in effect since Jan 1, 2020, and is expected to contribute to reductions in harmful use of alcohol and alcohol-related harm.54 However, as alcohol consumption is associated with particular lifestyles and cultures, the strict and transparent implementation and comprehensive support of the government, and the involvement of all communities and stakeholders with various initiatives are critical to ensure the feasibility and effectiveness of controlling harmful use of alcohol.
Together with reducing tobacco use and harmful use of alcohol, improving physical activity and healthy diet are four modifiable risk factors targeted by WHO's global monitoring framework and action plan for NCD prevention and control. Although our study found slightly higher physical activity levels than the global average among Vietnamese of both genders,55 SPA showed a decreasing trend with no chance of reaching the 2030 targets of the global action plan on physical activity 2018–2030.55 Additionally, our inequality analyses showed that women, people of Kinh ethnicity, those living in urban areas, wealthier people, and those of high educational level had lower physical activity levels. This could be due to rapid urbanization in Vietnam, which changed the occupation distributions and increased proportions of white-collar workers with sedentary behaviors, in addition to the universal use of motorbikes for private transport. Thus, we argue that future physical activity programs should promote workplace-based, daily-activity integrated, and women-focused interventions. Lessons should be learned from some developed countries in the availability and accessibility of public transport to boost daily physical activity by walking.56 As a global response, WHO has provided a technical package for increasing global physical activity levels named ACTIVE with four key policy areas (societies, environments, people, and systems).57 Despite the existing difficulties in measuring physical activity levels,58 Vietnam has implemented several nationally-representative surveys for accessing physical activity among the population.17 However, currently no report or study is evaluating the implementation of WHO's ACTIVE program in Vietnam, which warrants further development of comprehensive monitoring and evaluating systems.
Overweight and obesity have been rising,59 despite the fact that global strategies have been implemented with a focus on improving physical activity and healthy diets.6,55 In the present study, we observed the decreasing trends with negative annual percentage changes in NOW with no chance of achieving the 2030 targets at the national level, which concurred with the global trends and previous studies that recognized overweight and obesity as emerging health problems in Vietnam.60,61 In addition, we projected decreasing sufficient physical activity among women from 60·2% (55·6 to 64·3) in 2020 to 53·0% (43·5 to 62·1) in 2030 (Supplementary Table S10), which is comparable with the estimate among women in 28 European countries of 61·8% (60·3 to 63·3) in 2017.62 These findings were similar to the global declined trends in physical activity from 2001 to 2016 with lower physical activity levels among women, among older people, and in higher-income countries.63 As Vietnam has accelerated economic development with rapid urbanization and population aging, it is understandable that physical activity levels could be decreasing if no effective interventions were implemented, especially for women. In this study, we observed similar patterns of inequalities in NOW and SPA as women, Kinh ethnic groups, those living in urban areas, wealthy people, and those with high education levels are falling behind in those indicators. It also confirmed the association between physical activity and overweight/obesity and accorded with research from the Asian Development Bank Institute that Asian people are “wealthy but unhealthy” in overweight and obesity.64 Several cost-effective interventions have been identified exclusively for Asian countries such as sugar-sweetened beverage taxation, food labelling, marketing restrictions on unhealthy food, and other school-based interventions involving homes and communities.64 While some interventions have been adopted in Vietnam,65 some (e.g., sugar-sweetened beverage taxation) still need further investigation and cautious implementation.66 Additionally, lessons should be learned from Japan, one of the developed countries with the lowest prevalence of overweight and obesity. The Japanese government comprehensively implemented workplace-based interventions and school-based nutrition education to control obesity and improve the health of current and future generations.67
As an agricultural country, Vietnamese traditional meals normally contain large amounts of plant-based foods (e.g., fruits, vegetables, rice, cereals), however, the coverage of SUFV in 2010 was quite low. The present study showed the tremendous improvement of SUFV in 2015 and projected the country will achieve the 2030 target at the national level and in most sub-populations. Several dietary guidelines were introduced by the Vietnamese Ministry of Health and the National Institute of Nutrition to encourage the daily consumption of vegetables and fruit. However, we predicted a low probability of achieving the 2030 targets among ethnic minorities and observed substantial gaps between socioeconomic groups and geographic areas. In addition, men are less likely to eat fruit and vegetables but more likely to smoke tobacco and drink alcohol, which may suggest potential barriers for improving SUFV rather than socioeconomic and geographic factors. The absence of recommendations on exact daily uptake amounts and subsidies for enhancing fruit and vegetable consumption could be potential obstacles to the long-term and sustainable achievement of Vietnam's healthy diet.65,68
Cervical cancer, one of four most common cancers among women with more than 340,000 deaths in 2020, has been recognized as a global public health priority.69 In 2020, WHO released a global strategy for cervical cancer elimination, focusing on primary prevention (HPV vaccination for girls aged 9-14 years; tobacco and sexuality education for girls and boys), secondary prevention (screening for women aged 30-49 years; and treatment as quick as possible), and tertiary prevention (treatment of invasive cancer at any age), with specific targets of 90%-70%-90% by 2030.70 As of 2021, Vietnam has improved the availability of secondary prevention and treatment services,71 but our study showed low coverage of cervical cancer screening (23·8%) in 2015 in Vietnam, with inequalities between ethnicities, socioeconomic levels, and geographic areas. Additionally, there is no HPV (Human papillomavirus) vaccination in the national program and no social health insurance support for cervical cancer screening in Vietnam. These are crucial obstacles to achieving global targets for cervical cancer elimination in Vietnam.
Diabetes is one of four priority NCDs targeted for control worldwide with rapid rises in both the number of cases (from 108 million in 2008 to 422 million people in 2014) and prevalence (from 4·7% to 8·5%).72 In our study, we observed a decrease in treatment of diabetes, and low coverage of treatments of hypertension and high cholesterol, which suggests slow progress in the management of diabetes and other NCDs in Vietnam. The inequality analyses showed that ethnic minorities, those living in rural areas, those of low income, and those of low educational levels were lagging behind in treatment of diabetes, hypertension, and high cholesterol. Although there is still no global strategy and action plan for controlling diabetes, several initiatives and technical packages have been progressively developed including SHAKE for reducing salt consumption,73 REPLACE for eliminating industrially-produced trans-fatty acids,74 and HEARTS for cardiovascular disease management in primary healthcare.75 While the implementation of these initiative packages has not been reported in Vietnam, the government has made efforts to improve diabetes, high blood pressure, and cholesterol management services for vulnerable people. Specifically, the costs of testing and treatment for diabetes and hypertension have been covered by social health insurance, thus ensuring the affordability of these NCD management services for all people. In addition to increasing social health insurance coverage, the Vietnamese Government also focused on implementing treatment and management of diabetes and hypertension at primary healthcare facilities and strengthening the capacity of grassroots healthcare workers to improve the availability, accessibility, and acceptability of NCD management services.76 We expected these implementations could significantly alter our projections by sufficiently enhancing the coverage of NCD management services in Vietnam. Unfortunately, these components of financial risk protection and healthcare costs (including intangible social costs) were not available in the investigated data and thus were not incorporated in statistical models. Therefore, future nationally-representative household surveys should be re-designed to integrate health finance components, which may be meaningful for evaluating the effectiveness of national health programs and interventions.
Our study provides the first comprehensive estimates of NCD management indicators in Vietnam at national and sub-national levels based on nationally-representative data. In addition, it applied Bayesian statistics to estimate the probabilities of accomplishing the UHC targets by 2030. Furthermore, our comprehensive inequality analyses with estimations, patterns, and trends in demographic, geographic, and socioeconomic inequalities could thoroughly support the government and policymakers in revising and updating future equity-oriented interventions and programs. Nevertheless, the present study contains some limitations. Although we tried to include all the available population-based household data from 2010, the unavailability of post-2015 data and too few data points widened the uncertainty estimates and potentially impacted the accuracy of long-term trends and projections. While Bayesian models can be used to adjust data limitation in longitudinal analysis with appropriate informative priors, it requires in-depth prior knowledge and comprehensive sensitivity analyses in choosing hyperparameters of the prior distribution.77 Since we applied non-informative priors to simplify the modeling process of 240 models, our projections might have diminished precision and thus require interpretation with caution.78 Additionally, as our projections were based on the widely-accepted assumption that the last trends (2010–2015) remained constant with unchanged future policies, they may not be able to reflect the newly-implemented or revised policies after the study period. Although our inequality analyses were less likely to be altered by the few data points, they still were impacted by limitation in secondary data analysis, and constrained within the available NCD indicators of WHO's STEPS and GATS. This limitation also restricted our variable selection for statistical models to predominantly be based on those collected as part of the design of STEPS and GATS surveys. Although these surveys applied well-known, simple, standardized methods for monitoring and evaluating key NCD risk factors within and between countries, recently-reported issues in some STEPS indicators may require further investigation with validation and sensitivity analysis of different indicator definitions.24 Additionally, self-report designs in some questions (i.e., whether respondents are using medication for treating/controlling NCDs) might introduce measurement errors that may randomly or systematically alter our presented statistics. Composite indices have the advantage of summarizing a broad spectrum of information and supporting within-country, between-country, and cross-time comparisons. However, the interpretations of those composite indices should be made with caution as some further validation work may be needed. Finally, the present study warrants further investigations in providing more up-to-date and comprehensive trends and projections of NCD management coverage in Vietnam by using the national routine health management information system, upcoming Vietnam Global Adult Tobacco Survey 2021, or even meta-analysis from recently published studies.
In conclusion, our study revealed the slow progress in NCD management at the national level and among key sub-populations in Vietnam, together with existing and increasing inequalities between genders, ethnicities, geographic areas, and socioeconomic groups. Despite these challenges, with recent government support and facilitation and newly implemented national policies and programs, we believe Vietnam still has the possibility of achieving UHC targets and other global targets on NCD prevention and control. Nonetheless, we emphasize the necessity of continuously improving the healthcare system and facilities, appropriately re-distributing resources between geographic areas, simultaneously integrating economic, education, and gender intervention and programs. Additionally, it is critical to develop the monitoring and evaluation system at national and sub-national levels and provide publicly available data, which in turn would provide evidence-based information and enable the government's rapid response and decision making.
Contributors
Literature search: P.N., P.L.
Study conceptualization: P.N., S.G.
Methodology: P.N., S.G.
Data collection: H.V.N., B.T., M.H.
Data analysis and interpretation: P.N., S.G., H.V.N., M.H.
Writing - Original Draft: P.N., P.L., S.G.
Writing - Review & Editing: P.N., S.G., P.L., H.L.N., A.D., B.T., M.H., H.V.N.
Visualization: P.N.
Supervision: S.G.
Project administration: P.L.
The work reported in the paper has been performed by the authors unless clearly specified in the text.
Data sharing statement
The data that support the findings of this study are available from the corresponding author upon request.
Declaration of interests
We declare no conflict of interest.
Acknowledgment
We would like to express our sincere appreciation for critical review and comments from Dr. Kota Katanoda, Division of Surveillance and Policy Evaluation, National Cancer Center Institute for Cancer Control, Tokyo, Japan.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2022.101550.
Appendix. Supplementary materials
References
- 1.GBD 2017 Causes of Death Collaborators Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1736–1788. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD. Risk Factor Collaborators Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1923–1994. doi: 10.1016/S0140-6736(18)32225-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization . World Health Organization; Geneva, Switzerland: 2017. Tackling NCDs: ‘Best Buys' and Other Recommended Interventions for the Prevention and Control of Noncommunicable Diseases. CC BY-NC-SA 3.0 IGO. [Google Scholar]
- 4.Chisholm D, Llopis E, Prettner K, Stein A, Feigl A. World Economic Forum; Geneva, Switzerland: 2011. From Burden to “Best Buys”: Reducing the Economic Impact of Non-Communicable Disease in Low-and Middle-Income Countries: Program on the Global Demography of Aging. [Google Scholar]
- 5.World Health Organization . World Health Organization; Geneva, Switzerland: 2000. Global Strategy for the Prevention and Control of Noncommunicable Diseases. [Google Scholar]
- 6.World Health Organization Global Strategy on Diet, Physical Activity and Health. 2004 [Google Scholar]
- 7.World Health Organization . World Health Organization; Geneva, Switzerland: 2010. Global Strategy to Reduce the Harmful Use of Alcohol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization . World Health Organization; Geneva, Switzerland: 2013. Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013-2020. [Google Scholar]
- 9.Gilmour S, Mai PL, Nguyen P, Dhungel B, Tomizawa M, Nguyen H. Progress towards health for all: time to end discrimination and marginalization. Int J Environ Res Public Health. 2020;17(5):1696. doi: 10.3390/ijerph17051696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization, World Bank . World Health Organization; Geneva, Switzerland: 2014. Monitoring Progress Towards Universal Health Coverage at Country and Global Level: Framework, Measures and Targets. [Google Scholar]
- 11.Vázquez TR, Ghebreyesus TA. Beating NCDs can help deliver universal health coverage. Lancet. 2017;390(10101):1473–1474. doi: 10.1016/S0140-6736(17)32470-4. [DOI] [PubMed] [Google Scholar]
- 12.Vietnam Ministry of Health, Health Partnership Group . Ministry of Health; Hanoi, Vietnam: 2014. Joined Annual Health Review: Strengthening Prevention and Control of Non-Communicable Disease. [Google Scholar]
- 13.Institute for Health Metrics and Evaluation . Institute for Health Metrics and Evaluation; Seattle, WA: 2013. Vietnam Global Burden of Disease Study 2010 Results 1990–2010. [Google Scholar]
- 14.Vietnam Ministry of Health . Medical Publishing House; Hanoi, Vietnam: 2017. Health Statistics Yearbook 2015. [Google Scholar]
- 15.Vietnam Ministry of Health . Vietnam Ministry of Health; Hanoi, Vietnam: 2015. National Strategy for the Prevention and Control of Noncommunicable Disease Period 2015-2025. [Google Scholar]
- 16.Nguyen TT, Hoang MV. Non-communicable diseases, food and nutrition in Vietnam from 1975 to 2015: the burden and national response. Asia Pac J Clin Nutr. 2018;27(1):19–28. doi: 10.6133/apjcn.032017.13. [DOI] [PubMed] [Google Scholar]
- 17.Thuy Duyen N, Van Minh H, Van Huy N, et al. Patterns of behavioral risk factors for non-communicable diseases in Vietnam: A narrative scoping review. Health Psychol Open. 2020;7(2) doi: 10.1177/2055102920967248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nguyen PT, Nguyen VH, Phan HTT, Cao CTH. Situation of human resources and staff training of four provincial HIV/AIDS control centers in Northern Vietnam and some related factors in 2013. Vietnam J Prevent Med. 2015;25(7(167)):75–82. [Google Scholar]
- 19.Duong DB, Minh HV, Ngo LH, Ellner AL. Readiness, availability and utilization of rural Vietnamese health facilities for community based primary care of non-communicable diseases: a crosssectional survey of 3 provinces in northern Vietnam. Int J Health Policy Manag. 2019;8(3):150–157. doi: 10.15171/ijhpm.2018.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Bank Group . World Bank Group; Washington, DC: 2017. Moving Toward UHC: Vietnam - National Initiatives, Key Challenges, and the Role of Collaborative Activities. [Google Scholar]
- 21.Bredenkamp C, Buisman LR, Prencipe LM, Wagstaff A. World Bank Group; Washington, DC: 2012. Vietnam - Health Equity and Financial Protection Report; pp. 1–45. [Google Scholar]
- 22.Vietnam Partnership for Action in Health Equity . Institute For Social Development Studies; Hanoi, Vietnam: 2014. Health System in Vietnam: Towards Target with Equity. [Google Scholar]
- 23.Nguyen PT, Rahman MS, Le PM, et al. Trends in, projections of, and inequalities in reproductive, maternal, newborn and child health service coverage in Vietnam 2000-2030: a Bayesian analysis at national and sub-national levels. Lancet Reg Health West Pac. 2021;15 doi: 10.1016/j.lanwpc.2021.100230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bui TV, Blizzard CL, Luong KN, et al. National survey of risk factors for non-communicable disease in Vietnam: prevalence estimates and an assessment of their validity. BMC Public Health. 2016;16(1):498. doi: 10.1186/s12889-016-3160-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Van Minh H, Giang KB, Ngoc NB, et al. Prevalence of tobacco smoking in Vietnam: findings from the Global Adult Tobacco Survey 2015. Int J Public Health. 2017;62(Suppl 1):121–129. doi: 10.1007/s00038-017-0955-8. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization . World Health Organization; Geneva, Switzerland: 2014. Noncommunicable Diseases Global Monitoring Framework: Indicator Definitions and Specifications. [Google Scholar]
- 27.World Health Organization, Bank W . World Health Organization; Geneva, Switzerland: 2015. Tracking Universal Health Coverage: First Global Monitoring Report. [Google Scholar]
- 28.World Health Organization . World Health Organization; Geneva, Switzerland: 2018. Global Reference List of 100 Core Health Indicators (Plus Health-Related SDGs) [Google Scholar]
- 29.Lumley T. Wiley; Hoboken, N.J: 2010. Complex Surveys: A Guide to Analysis Using R. [Google Scholar]
- 30.Boerma JT, Bryce J, Kinfu Y, et al. Mind the gap: equity and trends in coverage of maternal, newborn, and child health services in 54 Countdown countries. Lancet. 2008;371(9620):1259–1267. doi: 10.1016/S0140-6736(08)60560-7. [DOI] [PubMed] [Google Scholar]
- 31.Hogan DR, Stevens GA, Hosseinpoor AR, Boerma T. Monitoring universal health coverage within the Sustainable Development Goals: development and baseline data for an index of essential health services. Lancet Glob Health. 2018;6(2):e152–e168. doi: 10.1016/S2214-109X(17)30472-2. [DOI] [PubMed] [Google Scholar]
- 32.Wagstaff A, Neelsen S. A comprehensive assessment of universal health coverage in 111 countries: a retrospective observational study. Lancet Glob Health. 2020;8(1):e39–e49. doi: 10.1016/S2214-109X(19)30463-2. [DOI] [PubMed] [Google Scholar]
- 33.Filmer D, Pritchett LH. Estimating wealth effects without expenditure data–or tears: an application to educational enrollments in states of India. Demography. 2001;38(1):115–132. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- 34.Rutstein SO. Macro International; Calverton, Maryland, USA: 2008. The DHS Wealth Index: Approaches for Rural and Urban Areas. [Google Scholar]
- 35.Schenker N, Raghunathan TE, Chiu P-L, Makuc DM, Zhang G, Cohen AJ. Multiple imputation of missing income data in the national health interview survey. J Am Stat Assoc. 2006;101(475):924–933. [Google Scholar]
- 36.National Center for Health Statistics . National Center for Health Statistics; Hyattsville, Maryland: 2019. Multiple Imputation of Family Income and Personal Earnings in the National Health Interview Survey: Methods and Examples. [Google Scholar]
- 37.Nguyen PT, Katanoda K, Saito E, Hori M, Nakayama T, Matsuda T. Trends in lung cancer incidence by gender, histological type and stage at diagnosis in Japan, 1993-2015: a multiple imputation approach. Int J Cancer. 2022;151(1):20–32. doi: 10.1002/ijc.33962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gelman A, Carlin JB, Stern HS, Dunson DB, Vehtari A, Rubin DB. 3rd ed. Chapman and Hall/CRC; London, UK: 2013. Bayesian Data Analysis. [Google Scholar]
- 39.Vehtari A, Gelman A, Gabry J. Practical Bayesian model evaluation using leave-one-out cross-validation and WAIC. Stat Comput. 2017;27:1413–1432. [Google Scholar]
- 40.Nguyen PT, Gilmour S, Le PM, Onishi K, Kato K, Nguyen HV. Progress toward HIV elimination goals: trends in and projections of annual HIV testing and condom use in Africa. AIDS. 2021;35(8):1253–1262. doi: 10.1097/QAD.0000000000002870. [DOI] [PubMed] [Google Scholar]
- 41.Van Buuren S, Brand JPL, Groothuis-Oudshoorn CGM, DB Rubin. Fully conditional specification in multivariate imputation. J Stat Comput Simulat. 2006;76(12):1049–1064. [Google Scholar]
- 42.Little RJA, Rubin DB. 3rd ed. Wiley; Hoboken, NJ: 2020. Statistical Analysis with Missing Data. Wiley series in probability and statistics; p. 1. Online resource. [Google Scholar]
- 43.World Health Organization . World Health Organization; Geneva, Switzerland: 2018. Saving Lives, Spending Less: A Strategic Response to Noncommunicable Diseases. [Google Scholar]
- 44.Minh HV, Ngan TT, Mai VQ, et al. Tobacco Control Policies in Vietnam: review on MPOWER Implementation Progress and Challenges. Asian Pac J Cancer Prev. 2016;17(S1):1–9. doi: 10.7314/apjcp.2016.17.s1.1. [DOI] [PubMed] [Google Scholar]
- 45.World Health Organization . World Health Organization; Geneva, Switzerland: 2021. WHO Report on the Global Tobacco Epidemic 2021: Addressing New and Emerging Products. [Google Scholar]
- 46.Nguyen VH, Do DA, Do TTH, et al. Smoke-free environment policy in Vietnam: what did people see and how did they react when they visited various public places? J Prev Med Hyg. 2019;60(1):E36–E42. doi: 10.15167/2421-4248/jpmh2019.60.1.942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.World Health Organization . World Health Organization; Geneva, Switzerland: 2018. Global Status Report on Alcohol and Health 2018. [Google Scholar]
- 48.World Health Organization . World Health Organization; Geneva, Switzerland: 2018. SAFER: Preventing and Reducing Alcohol-related Harms. [Google Scholar]
- 49.Tam NM, Doran CM, Hill PS, Dunne MP. Alcohol reform in Viet Nam: confronting rising consumption, injury and harm. Appl Health Econ Health Policy. 2012;10(5):285–287. doi: 10.1007/BF03261861. [DOI] [PubMed] [Google Scholar]
- 50.Park K. New law on prevention and control of alcohol related harms in Vietnam. J Glob Health Sci. 2019;1 [Google Scholar]
- 51.Lincoln M. Alcohol and drinking cultures in Vietnam: a review. Drug Alcohol Depend. 2016;159:1–8. doi: 10.1016/j.drugalcdep.2015.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Luu BN, Nguyen TT, Newman IM. Traditional alcohol production and use in three provinces in Vietnam: an ethnographic exploration of health benefits and risks. BMC Public Health. 2014;14(1):731. doi: 10.1186/1471-2458-14-731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lachenmeier D, Pham HA, Popova S, Rehm J. The quality of alcohol products in Vietnam and its implications for public health. Int J Environ Res Public Health. 2009;6:2090–2101. doi: 10.3390/ijerph6082090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.National Assembly of the Socialist Republic of Vietnam . National Assembly; Hanoi, Vietnam: 2019. Law No. 44/2019/QH14 dated June 14, 2019 of the National Assembly on Prevention and Control of Harms of Liquor and Beer Abuse. [Google Scholar]
- 55.World Health Organization . World Health Organization; Geneva, Switzerland: 2018. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World. [Google Scholar]
- 56.Rissel C, Curac N, Greenaway M, Bauman A. Physical activity associated with public transport use–a review and modelling of potential benefits. Int J Environ Res Public Health. 2012;9(7):2454–2478. doi: 10.3390/ijerph9072454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.World Health Organization . World Health Organization; Geneva, Switzerland: 2018. ACTIVE: A Technical Package for Increasing Physical Activity. [Google Scholar]
- 58.Bui TV, Blizzard CL, Luong KN, et al. Physical activity in Vietnam: estimates and measurement issues. PloS One. 2015;10(10) doi: 10.1371/journal.pone.0140941. e0140941-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Blüher M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. 2019;15(5):288–298. doi: 10.1038/s41574-019-0176-8. [DOI] [PubMed] [Google Scholar]
- 60.Cuong TQ, Dibley MJ, Bowe S, Hanh TTM, Loan TTH. Obesity in adults: an emerging problem in urban areas of Ho Chi Minh City, Vietnam. Eur J Clinic Nutr. 2007;61(5):673–681. doi: 10.1038/sj.ejcn.1602563. [DOI] [PubMed] [Google Scholar]
- 61.Walls HL, Peeters A, Son PT, et al. Prevalence of underweight, overweight and obesity in urban Hanoi, Vietnam. Asia Pac J Clin Nutr. 2009;18(2):234–239. [PubMed] [Google Scholar]
- 62.Nikitara K, Odani S, Demenagas N, Rachiotis G, Symvoulakis E, Vardavas C. Prevalence and correlates of physical inactivity in adults across 28 European countries. Eur J Public Health. 2021;31(4):840–845. doi: 10.1093/eurpub/ckab067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob Health. 2018;6(10):e1077–e1086. doi: 10.1016/S2214-109X(18)30357-7. [DOI] [PubMed] [Google Scholar]
- 64.Helble M, Sato A. Asian Development Bank Institute; Toyko, Japan: 2018. Wealthy But Unhealthy: Overweight and Obesity in Asia and the Pacific: Trends, Costs, and Policies for Better Health. [Google Scholar]
- 65.Buse K, Aftab W, Akhter S, et al. The state of diet-related NCD policies in Afghanistan, Bangladesh, Nepal, Pakistan, Tunisia and Vietnam: a comparative assessment that introduces a “policy cube” approach. Health Policy Plan. 2020;35(5):503–521. doi: 10.1093/heapol/czz175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Luong L, Vu LH. Impacts of excise taxation on non-alcoholic beverage consumption in Vietnam. Sustainability. 2020;12(3):1092. [Google Scholar]
- 67.Miyoshi M, Tsuboyama-Kasaoka N, Nishi N. School-based "Shokuiku" program in Japan: application to nutrition education in Asian countries. Asia Pac J Clin Nutr. 2012;21(1):159–162. [PubMed] [Google Scholar]
- 68.Hop le T, Van TK, Thanh HK. Food based dietary guidelines in Vietnam: progress and lessons learned. Asia Pac J Clin Nutr. 2011;20(3):495–499. [PubMed] [Google Scholar]
- 69.Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021 doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 70.World Health Organization . World Health Organization; Geneva, Switzerland: 2020. Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem. [Google Scholar]
- 71.World Health Organization . World Health Organization; Geneva, Switzerland: 2021. Cervical Cancer Country Profiles. [Google Scholar]
- 72.World Health Organization . World Health Organization; Geneva, Switzerland: 2016. Global Report on Diabetes. [Google Scholar]
- 73.World Health Organization . World Health Organization; Geneva, Switzerland: 2016. The SHAKE Technical Package for Salt Reduction. [Google Scholar]
- 74.World Health Organization . World Health Organization; Geneva, Switzerland: 2021. REPLACE Trans Fat: An Action Package to Eliminate Industrially Produced Trans-Fatty Acids. [Google Scholar]
- 75.World Health Organization . World Health Organization; Geneva, Switzerland: 2016. Hearts: Technical Package for Cardiovascular Disease Management in Primary Health Care. [Google Scholar]
- 76.Vietnam Ministry of Health . Vietnam Ministry of Health; Hanoi, Vietnam: 2018. Decision No.2559/QD-BYT on Promulgate Plan to Strengthen the Implementation of Treatment and Management of Hypertension and Diabetes Following Family Medicine Principles at Commune/Ward/Township Health Stations 2018-2020. [Google Scholar]
- 77.Rolfe M. Queensland University of Technology; Queensland, Australia: 2010. Bayesian Models for Longitudinal Data. [Google Scholar]
- 78.Lambert PC, Sutton AJ, Burton PR, Abrams KR, Jones DR. How vague is vague? A simulation study of the impact of the use of vague prior distributions in MCMC using WinBUGS. Stat Med. 2005;24(15):2401–2428. doi: 10.1002/sim.2112. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.