Abstract
Background:
Helicobacter pylori eradication is associated with reduced gastric cancer and peptic ulcer disease incidence and mortality. Factors influencing patients’ experiences surrounding H. pylori diagnosis and management are not well-described. Current patient perceptions can influence adherence to treatment, and also their anxieties related to this potentially carcinogenic condition. The objective of this study was to understand the patient experience surrounding H. pylori management and to qualitatively construct a contextual framework to inform and guide providers who manage patients with H. pylori infection
Methods:
We conducted a qualitative analysis using a focus group and one-on-one telephone interviews. An iterative inductive/deductive approach was applied to recorded transcripts to identify and hierarchically order themes. Patient experience was defined according to major themes within a structured health behavior framework.
Results:
Theme saturation was achieved with thirteen participants (mean age 50.4 years; 62% female; 38% non-Hispanic white). Qualitative analysis yielded a total of 987 codes that resulted in five major themes related to the patient H. pylori experience: context of decision making; health beliefs; barriers experienced; cues to action; and impact of new knowledge. These themes aligned with the Health Behavior Model framework. Participants were motivated to treat H. pylori. However, the experience was more often perceived negatively versus positively. The perceived patient-provider interaction contributed most prominently to the negative experience compared to other patient experiences, including treatment-related side effects. Internal cues, including symptoms and fear of cancer, modified participants’ perceptions and motivation to accept treatment.
Conclusions:
Patient experiences related to H. pylori management are predominantly negative. Increasing providers’ awareness about patients’ values, beliefs, anxieties, and expectations surrounding H. pylori diagnosis/treatment may improve provider-patient communication and, ideally, related outcomes.
Keywords: Helicobacter pylori, Qualitative, Quality improvement, Patient experience, Compliance (Mesh Terms: Adult and Treatment)
BACKGROUND
Helicobacter pylori (H. pylori) is a World Health Organization-designated class I carcinogenic agent that infects approximately 50% of the global population.1 H. pylori is the strongest known risk factor for gastric cancer and is a leading cause of peptic ulcer disease.2 Eradication of H. pylori reduces gastric cancer and peptic ulcer disease incidence and related mortality.3,4 Accordingly, eradication treatment is recommended for all individuals diagnosed with H. pylori. In the United States (US), approved first-line regimens include 2–3 antibiotics and high-dose acid suppression dosed two-three times per day for 14 days.5
However, failure to eradicate H. pylori with current treatments is common. Patient nonadherence to treatment is one leading contributor to eradication failure. Healthcare providers may not have sufficient understanding of the patient experience surrounding H. pylori diagnosis and management, or the information which patients value most when discussing treatment. This, in turn, might have downstream consequences, such as undermining treatment adherence. For example, if patients place a high value on avoiding side effects, they might be less inclined to accept 14 days of treatment if they are minimally symptomatic or asymptomatic. However, if patients place a high value on cancer prevention interventions, they may be more motivated to commit to the full treatment course despite bothersome, but nonserious side effects.
The primary objective of this study was to qualitatively describe the patient experience surrounding H. pylori treatment and construct a contextual framework to facilitate and positively affect this experience.
METHODS
We conducted a qualitative study to describe the H. pylori experience using a combination of a focus group (FG) and one-on-one interviews. This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Vanderbilt University Medical Center Institutional Review Board. Participants granted verbal informed consent and received a $25 gift-card as compensation.
Inclusion criteria and participant recruitment
Individuals ≥18 years old who had tested positive for H. pylori and completed at least one course of approved eradication treatment5 within 6 months of the session were eligible; 6 months was the designated cut-off to increase patient recall for the experience. A study coordinator contacted eligible individuals with information about the study and re-confirmed eligibility. Additional data collection elements are provided in the Supplementary Material. Study enrollment ended once theme saturation was reached. In qualitative research, thematic saturation is deemed to be achieved when conducting additional focus groups or interviews no longer provides novel information. Thematic saturation is a judgement that occurs after discussion among the interviewers, coders, and investigators.
Procedures
The moderator guide (instrument) was designed as semi-structured prompts with built-in cues to guide open discussion with participants. The content and organization of the FG and telephone interviews were the same, and were developed by a gastroenterologist with H. pylori expertise (SCS) (Supplementary Material). The instruments were pilot-tested among providers (primary care and gastroenterology) with iterative modifications made prior to the participant sessions. All materials were at a 9th grade or lower reading level.6 A trained moderator (KB) conducted and recorded all sessions. The FG and telephone interviews were conducted at Vanderbilt University Medical Center between November 1, 2019 through February 20, 2020, with the single FG occurring in November 2019.
FG/Interview Content
The instrument included questions related to: 1) general knowledge of H. pylori and clinical implications (pre- versus post-diagnosis) and source of this knowledge (e.g. internet, healthcare provider); 2) experience surrounding receipt of H. pylori diagnosis, education, and the provider interaction; 3) experience and education received regarding H. pylori treatment, treatment barriers and side effects (both perceived and actual); 4) treatment expectations including symptom improvement; 5) factors that, in general, influence participants’ decision to engage in health behaviors. (Supplementary Material)
Statistical approach: Qualitative coding and analyses
Data coding and analysis were managed by the Vanderbilt University Qualitative Research Core (Microsoft Excel 2016 and SPSS version 26.0), led by a PhD-level psychologist, and conducted in accord with the Standards for Reporting Qualitative Research.7
A hierarchical coding system was developed and refined. Major categories were divided into subcategories, with additional hierarchical division as appropriate. A rubric of definitions and rules were developed for each category. (Supplementary Table 1)
Two experienced qualitative data coders (KB and RS) independently coded and then compared transcripts to establish inter-coder consensus and resolve any discrepancies. This process was iteratively performed until consensus was consistently achieved. Each statement was treated as a separate quote and each quote could be assigned multiple codes. An iterative inductive/deductive approach was used to identify higher-order themes.8–10 Inductively, coded quotes were sorted by category to identify themes and inter-theme relationships. Deductively, the themes aligned with the Health Belief Model (HBM), a well-established psychosocial theory of health behaviors and decision-making11,12, which guided the analysis.
RESULTS
Participant characteristics
Of 22 eligible individuals, we enrolled 14 participants. Five individuals participated in the FG and 9 in individual telephone interviews. One participant was excluded due to hearing impairment resulting in 13 participants. A total of 605 unique participant quotes were coded. After applying the hierarchical coding system in which participant quotes could be assigned more than one code, there were 987 codes used to identify higher-order themes. Saturation of theme consistency was noted at 10 participants. The information obtained from the remaining 3 interviews did not substantially change the findings nor contribute novel information, further confirming theme saturation. Accordingly, because theme saturation was achieved, we did not enroll additional patients.
Participant and H. pylori-related characteristics are detailed in Table 1. Participants’ mean age was 50.4 years (standard deviation, SD: 10.5) and 62% (8/13) were female. Five self-identified as non-Hispanic white, 5 as non-Hispanic African-American, two as ‘other’, and 1 preferred not to answer. All participants reported at least a high school degree or higher, with 9/13 (69%) reporting at least some college or technical training. The majority of participants (10/13, 77%) reported clinical symptoms related to H. pylori infection.
Table 1:
Study participant characteristics
| Participant ID | Age Range*, Sex | Race | Hispanic ethnicity | Highest educational level achieved | Clinical symptoms of H. pylori | H. pylori testing modality | First course of H. pylori therapy | Family history gastric cancer | Side effects experienced? | Participant felt adequately counseled by healthcare provider | Would accept repeated course of therapy if indicated? |
|---|---|---|---|---|---|---|---|---|---|---|---|
| One-on-one Telephone Interview Participants | |||||||||||
| 1 | 50–55, Female | Other | No | College | Yes | Serology | Yes | No | No | No | Yes |
| 2 | 50–55, Female | Other | No | Trade school | Yes | Breath test | No | Yes | No | Yes | Yes |
| 3 | 65+, Male | White | No | College | Yes | Histology | Yes | No | No | No | Yes |
| 4 | 56–59, Male | AA | No | High school | Yes | Serology | No | No | Yes | No | Yes |
| 5 | 40–49, Female | White | No | College | No | Histology | Yes | No | Yes | No | No |
| 6 | 30–39, Female | White | No | Associates | No | Histology | Yes | No | No | No | No |
| 7 | 50–55, Male | AA | No | College | Yes | Stool test | Yes | No | Unable to recall | No | Yes |
| 9* | 60–65, Female | Declined to answer | Declined to answer | Masters | Yes | Histology and Serology | No | No | Yes | No | No |
| Focus Group Participants | |||||||||||
| 10 | 40–49, Female | AA | No | College | No | Breath test | No | No | Yes | No | No |
| 11 | 50–55, Male | AA | No | High school | Yes | Breath test | Yes | No | Yes | No | Unsure |
| 12 | 50–55, Female | AA | No | High school | Yes | Serology | No | No | Yes | No | Yes |
| 13 | 50–55, Male | White | No | High school | Yes | Histology | Yes | No | Yes | No | Yes |
| 14 | 30–39, Female | White | No | Masters | Yes | Stool test | Yes | Yes | Yes | No | Yes |
Note: Age range is provided to protect anonymity. Participant #8 removed due to hearing impairment and inability to complete interview
Abbreviations: AA, African-American
In general, participants were motivated to accept treatment for H. pylori, and this was driven largely by internal and external cues, detailed below.
Themes and Contextual Framework
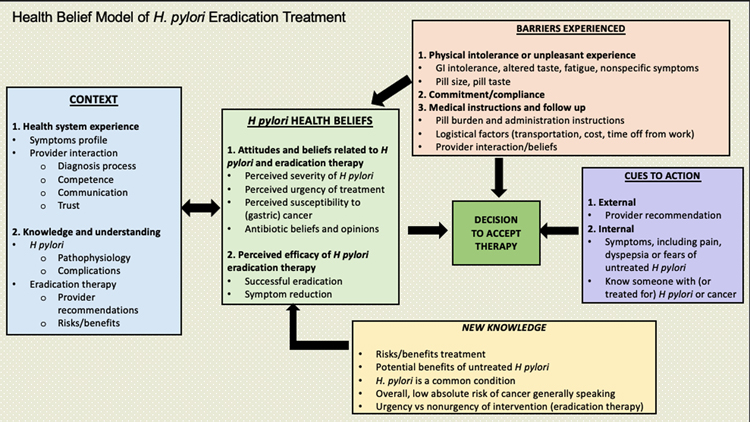
Five major themes related to participants’ experience with H. pylori treatment emerged: context of decision making; health beliefs; barriers experienced; cues to action; and impact of new knowledge (Figure 1). These themes were consistent among participants irrespective of mode of participation (FG or interview). Additional details regarding the synthesis of this tiered model are provided, along with representative quotes (Supplementary Tables 1, 2).
Figure 1. Health Belief Model of H. pylori Eradication Treatment.
The left panel in the framework represents context (blue box), which includes the existing knowledge and experiences that an individual draws upon to make a decision regarding whether to accept H. pylori eradication treatment. Participants’ experience with the healthcare system and their existing knowledge and understanding of H. pylori and eradication treatment comprised the major contextual themes for decision-making. The central panel (green box) of the framework includes the current attitudes and beliefs that the patient holds about H. pylori including perceived severity of H. pylori, perceived susceptibility to cancer, antibiotic beliefs, and perceived treatment efficacy. New knowledge (yellow box) includes the categories of information typically conveyed by providers, ideally as the foundation of shared decision-making. The decision regarding therapy is additionally influenced by internal and external cues to action for treating H. pylori. Experienced barriers (tan box) may function as a modifier of health beliefs, or may directly influence the decision to seek treatment. Beliefs, new knowledge, barriers, and cues to action all interact to influence H. pylori treatment decisions.
Theme 1: Context
The context of decision making includes the existing knowledge and experiences that participants use to make decisions. With respect to existing knowledge about H. pylori, nearly all participants (12/13) reported that they had never heard of the condition, the implications, or the treatment prior to their diagnosis. One participant reported limited knowledge because she knew someone “…who had it [H. pylori]. I knew what it was but I didn’t have the real details.” Most participants researched H. pylori on their own using the internet.
The two main contributors to participants’ healthcare system experience were their symptom profiles and their provider interaction. Therefore, participants who reported being asymptomatic relied predominantly on provider communication. Four main components comprised provider interaction: sharing the diagnosis, provider competence, provider communication, and participants’ trust of their provider (Figure 1). Of the participants, 3/13 (23.1%) felt that their provider attempted to explain their diagnosis, while none (0%) reported that their provider explained treatment side effects.
In general, participants more often perceived the context of H. pylori therapy negatively versus positively. Participants’ perception of the patient-provider interaction was the most prominent contributor to the overall negative experience. For example, one participant recalled the interaction as “Oh, by the way you have H. pylori…this is what we suggest you do and whatever…and I was like “okay” and that was it” (Participant #3) There was sometimes blame and disbelief towards the provider for not diagnosing H. pylori infection earlier “I had been going to my doctor all these years, all this time, and she never found it” (Participant #1); and even anger “[I] was very, very shocked and upset when I just got a letter from Dr. X and nobody called me to say “Hi, you have this”” (Participant #5).
Theme 2: Health Beliefs
No participants reported adequate shared decision-making between providers and patients regarding H. pylori treatment. The “decision” to accept therapy was influenced most by participants’ 1) attitudes and beliefs related to H. pylori and antibiotics; and 2) their perception of the efficacy of H. pylori treatment with respect to likelihood of successful eradication, and symptom improvement/resolution (Figure 1).
The severity of the clinical symptoms that participants attributed to H. pylori, as well as their perceived individual susceptibility to gastric cancer were the themes that consistently influenced initial acceptance of treatment and, if indicated, re-treatment. Among participants, there was variability in the perceived urgency for H. pylori treatment. For example, one participant felt anxiety over the diagnosis and the need for urgent eradication: “I thought that I had to have it [eradication treatment]… like the infection would spread or something worse would happen if I didn’t treat it [H. pylori] immediately.” Others felt less anxiety and urgency, instead expressing a desire to “just get rid of it [H. pylori]” (Participant #6). Participants with a family history of cancer were particularly concerned, as were participants who experienced nonspecific symptoms that could be consistent with gastric cancer.
Participants’ prior experiences and opinions about antibiotic therapy also influenced their health beliefs. Some perceived antibiotics as routine, whereas others preferred to avoid antibiotics unless absolutely necessary. Participants’ interpretations of providers’ perceptions might have also influenced their own individual health beliefs: “As a matter of fact, it was a nonevent for me…She [Dr. X] was just kind of, ‘Oh by the way, you have this H. pylori. It’s pretty common. Here’s a round of antibiotics.’ I was like, ‘Okay, no problem.’ (Participant #3)
Perceived treatment efficacy was the second major subcategory that influenced participants’ health beliefs about H. pylori (Figure 1). Of the 13 participants, 100% believed that the first treatment would eradicate H. pylori. No participants reported that their healthcare provider had counseled them that the first round of eradication therapy might not be effective. Of the 10 (77%) participants who were symptomatic, all believed that H. pylori treatment would resolve their symptoms completely.
Theme 3: Barriers experienced
Participants reported that, prior to H. pylori treatment, they were unaware of the barriers and side effects they actually experienced. These barriers and side-effects also influenced decision-making indirectly by modifying health beliefs/attitudes (Figure 1).
The three main, non-mutually exclusive subcategories of barriers were: 1) physical intolerance or adverse experience with treatment; 2) difficulties with treatment adherence, including regimen complexity; and 3) difficulties with acquiring treatment (e.g. cost) and follow-up. Participants who discussed the treatment course with their providers had less perceived barriers compared to participants who did not.
Over 60% (8/13) reported treatment side effects (Table 1), most often GI-related, with all except one participant reporting these as mild. The participant who reported more severe side effects developed C. difficile infection, recalling that it was “…worse than the symptoms that you have with H. pylori. …I thought I had food poisoning.” Participants reported multiple barriers to medication adherence, including large pill sizes, unpleasant pill taste, pill burden, complicated regimen, and forgetfulness. Participants also reported health system barriers including uncertainty regarding the timing and necessity of repeat testing to confirm H. pylori eradication. Except for the participant who developed C. difficile, all other participants reported that any side effects or barriers experienced were inconvenient, but they were not so strong as to change their desire for treatment.
Theme 4: Cues to action
According to the HBM, cues to action impact individuals’ decisions to engage in a health behavior.11,12 In line, participants’ motivation to accept H. pylori treatment and their commitment to therapy were influenced most by cues to action. We identified two major within-theme subcategories, which were categorized as ‘internal’ or ‘external’. (Figure 1) The strongest internal cues were participants’ self-reported symptoms, their fears related to untreated H. pylori infection, and whether or not they knew someone with complications of H. pylori infection or cancer. Internal cues strongly influenced participants’ perception of their own individual gastric cancer risk (i.e. Theme 2: health beliefs).
The dominant external cue was healthcare providers’ recommendations, including their ability to express the rationale for treatment. “So [providers should] take the time to explain [to patients] what’s expected daily and how important it is to stick to it. … ‘You [patient] have to stick with this regimen. These are the consequences if you [patient] don’t.’” (Focus group participant #2)
Theme 5: Impact of new knowledge
After participation in this study, 100% reported that they learned new information about H. pylori and treatment, which they neither received from their respective patient-provider interaction nor via other sources at the time of their H. pylori diagnosis/treatment. This information influenced participants’ perception of treatment as a “health-promoting behavior”, which was more prominent in asymptomatic compared to symptomatic participants. New information had the least impact on participants with severe symptoms and on participants whose treatment was effective. For example, one participant reported his symptoms were so severe that he would have “given his left leg” to not have H. pylori.
Participants were also asked to quantify the level of cancer risk below which they would forego H. pylori treatment. For most, this individual cancer risk threshold varied between 1% to 5%. Generally, participants acknowledged that even though a 5% risk was still small, most stated that they would need reassurance from their providers that foregoing eradication therapy was safe. One participant was uncomfortable with <1% risk of gastric cancer and would still elect treatment: “I would still have to say I would have to take it. […] less than 1% is not that much […] But just to fight it off, to make sure, that I won’t get it, yes, I would pick the treatment…Just because. To be honest, it’s scary.”
Summary of participant experiences
When asked how their experiences related to their H. pylori treatment and management could have been improved, participants unanimously expressed that they would have appreciated better provider communication and anticipatory guidance related to potential side effects or barriers. Participants also desired more education about H. pylori and its consequences.
At the end of the session, participants were asked to consider their perceived 1) experience related to H. pylori 2) risks of untreated H. pylori infection and 3) treatment risks and benefits. Nearly 40% (5/13) reported that they would decline anti-H. pylori therapy if provided with the option now (N=4), or were unsure (N=1). Notably, three of the four who reported they would decline therapy were asymptomatic (indication for H. pylori testing: pre-bariatric surgery evaluation in 2, unknown in 1).
DISCUSSION
To our knowledge, this is the first study to delineate patient experiences surrounding H. pylori management, and contextualize these experiences using a well-accepted framework. We identified that participants were motivated to undergo treatment for H. pylori, primarily because of their own internal cues (i.e. symptoms) as well as external cues from their providers. However, participants most often perceived the overall H. pylori experience as predominantly negative. Suboptimal patient-provider interaction, insufficient education and guidance, and insufficient assessment of patients’ expectations of the therapeutic outcome were key themes contributing to the negative experience. Instituting appropriate corrective measures to address the 5 major themes we identified, with particular attention to patient-provider interaction, may improve the patient experience and, ideally, facilitate adherence to H. pylori treatment.
The HBM is a framework commonly used to understand and evaluate behaviors related to health promotion and disease prevention interventions11,12, of which H. pylori treatment qualifies. According to the HBM, individuals’ perception that the behavior is a “health-promoting” behavior is fundamental to their engagement. So-called “modifying factors”, including demographics, educational status, health knowledge, and internal/external cues, might impact this perception. In the HBM, the perceived susceptibility to disease, the severity of disease/symptoms, the perceived benefits of preventative action, and the perceived barriers are the major drivers of an individual’s likelihood to engage in a health behavior.11,12 Our findings align with the HBM paradigm, particularly among symptomatic individuals. Moreover, our study identified that among asymptomatic individuals, in whom perceived susceptibility to and severity of disease are dampened or nonexistent, instead framing H. pylori eradication as a health-promoting and cancer prevention behavior was effective for enhancing commitment to therapy.
One main finding of this study is that the patient experience surrounding H. pylori therapy is influenced most significantly by the patient-provider interaction and by patients’ own internal cues—namely, the severity of symptoms and fear of (gastric) cancer. Based on our findings, the shared decision-making process should include provider verbal communication with patients regarding the H. pylori diagnosis, the expected risks and benefit of treatment, the therapy-related side effects and barriers, along with a lay explanation of the consequences of untreated infection in the context of each patient’s individual risk. We postulate that this discussion might positively impact patients’ experiences.
The shared decision-making process should also include a better understanding of patients’ outcome expectancy related to treatment.13 All participants expected that eradication treatment would be successful with the first attempt. Furthermore, symptomatic patients expected that their symptoms would fully resolve. Even despite adequate adherence to the medication regimen, failure to eradicate H. pylori is common; and, successful eradication might not fully resolve symptoms. This mismatch in patients’ actual versus expected outcome is problematic, particularly when patients are fully adherent to therapy, as it may elicit a feeling of failure and contribute to patients’ negative experience with H. pylori therapy. Plausibly, improving effective patient-provider communication may better direct patient expectations.
Lastly, there was a near universal lack of pre-diagnosis knowledge regarding H. pylori, which is consistent with prior literature.14 This contributed to participants’ anxiety and fear about the consequences of untreated H. pylori infection. This observation further emphasizes the pivotal, but largely unmet, role of providers in shaping the patient experience related to the management of H. pylori.
One primary strength of this study is that we were able to achieve theme saturation relatively quickly. This reflects the consistency of the themes and experiences reported by participants, as well as the effectiveness of the survey instrument and its implementation. Notwithstanding, there are a few limitations. Although we had gender and racial diversity, this group was recruited from a single academic medical center and consisted primarily of non-Hispanic African-American and white participants who were relatively well-educated, and within the 30–65-year-old age range. Therefore, we recommend caution when generalizing these findings to other populations. We restricted eligibility to individuals who had received H. pylori treatment within 6 months of the FG/interview date, as well as offered a small participation incentive in order to mitigate the impact of recall and participant bias15, respectively, although these may continue to be present.
CONCLUSION
In conclusion, we conducted a qualitative analysis of the patient experience surrounding H. pylori management and identified major themes which were inter-related and align with the HBM. Our data demonstrate that patients are motivated to accept and comply with H. pylori treatment, but that their overall experience is predominantly negative. The quality and depth of the shared decision-making process, especially patients’ interactions with the diagnosing/treating healthcare providers, is fundamental to their perception of the experience.
Supplementary Material
Acknowledgements
Funders: SCS and this work was supported by the Agency for Healthcare Research (AHRQ) and Quality and Patient-Centered Outcomes Research Institute (PCORI) K12 HS026395, American Gastroenterological Association Research Scholar Award, and Veterans Affairs Career Development Award ICX002027A. Additional funding support for co-authors include DK R0158587, CA R01 77955, CA P01 116087 (RP). The content is solely the responsibility of the listed authors and does not necessarily represent the official views of the funding agencies.
Funding/Grant Support.
SCS and this work was supported by the Agency for Healthcare Research (AHRQ) and Quality and Patient-Centered Outcomes Research Institute (PCORI) K12 HS026395, American Gastroenterological Association Research Scholar Award, and Veterans Affairs Career Development Award ICX002027A-01. Additional funding support for co-authors include DK R0158587, CA R01 77955, CA P01 116087 (RP). The content is solely the responsibility of the listed authors and does not necessarily represent the official views of the funding agencies.
Footnotes
Disclosures/competing interests statement. The authors have no potential conflicts (financial, professional, nor personal) that are relevant to this manuscript.
Declarations
Ethics approval and consent to participate: All participants included in this study provided both verbal and written voluntary consent and were allowed to withdraw their participation at any time. This study was approved by the Vanderbilt University Medical Center Institutional Review Board.
Consent for publication: Not applicable.
Availability of data and materials: The data generated and analyzed during the current study are not publicly available due to some personal provider information being verbalized within transcript documents. The de-identified data are available in included in this published article and supplementary material.
Writing assistance. No additional writing assistance was used for this manuscript
Prior presentations: This work has not been previously presented
Publisher's Disclaimer: This AM is a PDF file of the manuscript accepted for publication after peer review, when applicable, but does not reflect postacceptance improvements, or any corrections. Use of this AM is subject to the publisher’s embargo period and AM terms of use. Under no circumstances may this AM be shared or distributed under a Creative Commons or other form of open access license, nor may it be reformatted or enhanced, whether by the Author or third parties. See here for Springer Nature’s terms of use for AM versions of subscription articles: https://www.springernature.com/gp/open-research/policies/accepted-manuscript-terms
References
- 1.Hooi JKY, Lai WY, Ng WK, et al. Global Prevalence of Helicobacter pylori Infection: Systematic Review and Meta-Analysis. Gastroenterology 2017; 153: 420–9. [DOI] [PubMed] [Google Scholar]
- 2.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018; 68: 394–424. [DOI] [PubMed] [Google Scholar]
- 3.Sonnenberg A, Turner KO, Genta RM. Low Prevalence of Helicobacter pylori-Positive Peptic Ulcers in Private Outpatient Endoscopy Centers in the United States. Am J Gastroenterol 2020; 115: 244–50. [DOI] [PubMed] [Google Scholar]
- 4.Sonnenberg A, Wasserman IH. Associations of peptic ulcer and gastric cancer with other diseases in US veterans. Am J Public Health 1995; 85: 1252–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chey WD, Leontiadis GI, Howden CW, Moss SF. ACG Clinical Guideline: Treatment of Helicobacter pylori Infection. Am J Gastroenterol 2017; 112: 212–39. [DOI] [PubMed] [Google Scholar]
- 6.Readability Test Results. https://www.webfx.com/tools/read-able/check.php (accessed Aug 17, 2020).
- 7.O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med 2014; 89: 1245–51. [DOI] [PubMed] [Google Scholar]
- 8.Azungah T Qualitative research: deductive and inductive approaches to data analysis. Qualitative Research Journal 2018; 18: 383–400. [Google Scholar]
- 9.Tjora A Qualitative Research as Stepwise-Deductive Induction. Abingdon, Oxon; New York, NY: : Routledge, 2018. | Series: Routledge advances in research methods; 26: Routledge, 2018 DOI: 10.4324/9780203730072. [DOI] [Google Scholar]
- 10.Fereday J, Muir-Cochrane E. Demonstrating rigor using thematic analysis: A hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods 2006; 5: 80–92. [Google Scholar]
- 11.Jones CL, Jensen JD, Scherr CL, Brown NR, Christy K, Weaver J. The Health Belief Model as an explanatory framework in communication research: exploring parallel, serial, and moderated mediation. Health Commun 2015; 30: 566–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Glanz K, Rimer BK, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice, 4th edn. John Wiley & Sons, 2008. [Google Scholar]
- 13.Reesor L, Vaughan EM, Hernandez DC, Johnston CA. Addressing outcomes expectancies in behavior change. Am J Lifestyle Med 2017; 11: 430–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shah SC, Nunez H, Chiu S, et al. Low baseline awareness of gastric cancer risk factors amongst at-risk multiracial/ethnic populations in New York City: results of a targeted, culturally sensitive pilot gastric cancer community outreach program. Ethn Health 2020; 25: 189–205. [DOI] [PubMed] [Google Scholar]
- 15.Lee M, Kemp JA, Canning A, Egan C, Tataronis G, Farraye FA. A randomized controlled trial of an enhanced patient compliance program for Helicobacter pylori therapy. Arch Intern Med 1999; 159: 2312–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.