Abstract
Background/Objective
Obsessive compulsive disorder is a disorder of special relevance in mental health, however, not all patients respond adequately to traditional intervention systems. The present work aims to study the usefulness of mindfulness-based interventions in patients with obsessive compulsive disorder.
Method
An exhaustive search of the literature between 1996 and 2021 allowed us to locate 11 published articles. The effect size was the pretest-posttest standardized mean change calculated for obsession-compulsion, as well as depression symptoms and conscious coping.
Results
he results showed mean effect sizes for mindfulness in the reduction of obsessive-compulsive symptoms (d + = 0.648) and, to a lesser extent, depression (d + = 0.417) and the improvement in Mindfull coping (d + = 0.509). There was no significant decrease in effect size when mindfulness was applied in patients with residual symptoms from previous treatments.
Conclusions
These results are promising regarding the usefulness of the application of intervention programs based on mindfulness in people with obsessive compulsive disorder, both as an alternative option and as a complementary treatment to more traditional intervention formats.
Keywords: Obsessive-compulsive disorder, Mindfulness, Meta-analysis, Psychological therapy
Obsessive compulsive disorder (OCD) is characterized by obsessive intrusive thoughts and compulsive behaviors that increase and become chronic over time, with an estimated prevalence between 2% and 3% (Fawcett, Power, & Fawcett, 2020). This brings significant loss of quality of life and progressive levels of clinically relevant discomfort.
Although Cognitive behavioral therapy (CBT) has been shown to be highly effective in treatment of this disorder (Hamatani et al., 2020; Law & Boisseau; Rosa-Alcázar et al., 2019, 2021), it has also been consistently noted that around a third of patients do not respond adequately to this treatment (Fisher, Cherry, Stuart, Rigby, & Temple, 2020). Along with this limitation, an added difficulty is the high dropout rate, as the very nature of the technique can be excessively aversive as it involves eliciting high levels of anxiety (Johnco, McGuire, Roper, & Storch, 2020; Keleher, Jassi, & Krebs, 2020). Finally, relapse rate following this type of intervention is around 20% (Hansen, Kvale, Hagen, Havnen, & Öst, 2019).
Given the limitations of an exclusively behavioral approach, the study of the efficacy of other types of alternatives, separately or together with ERP, has become a line of research progressively gaining more interest.
From a theoretical point of view, it has been suggested that mindfulness-based treatment programs (MBT) could be useful in OCD treatment (Fairfax, 2008; Hawley et al., 2017; Afshari, 2020; Cludius et al., 2020; Didonna, 2020).
Strauss et al. (2018) have pointed out different mechanisms that could indicate the usefulness of this intervention in these patients. Among these, the absence of judgment, the distancing of thought, the loss of the power of thought over action, or from a moral point of view, the distinction of the subject between them and their thoughts have been highlighted. (Pérez-Aranda et al., 2021), however there is little research on this topic. In addition, most studies suffer from certain methodological weaknesses, or present single case studies.
The purpose of this meta-analysis was to examine the global effectiveness of mindfulness for OCD patients to improve obsessive-compulsive symptoms.
With this in mind, the current study had three goals: 1) to analyze the global effectiveness of mindfulness for OCD including obsessive-compulsive, depression and coping mindfulness outcomes; 2) to compare mindfulness to other types of treatment; 3) to study whether there are differences in effectiveness of mindfulness between studies that have previously received CBT and those that have not; 4) to examine the presence of possible moderator variables related to participants, interventions and methodologies used in the studies. Exclusion criteria included comorbidity with bipolar disorder, schizophrenia spectrum disorders, psychotic disorders, personality disorders, anorexia, bulimia, substance abuse disorders, and neurocognitive disorders.
Method
This systematic review and meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines (Page et al., 2021). This research study is based on the ethical principles and recommendations of the “Declaration of Helsinki” (World Medical Association, 2013). The authors have not pre-registered the protocol.
Selection criteria
For inclusion in this research, studies had to fulfill the following criteria based on PICOS statement (Page et al., 2021): (a) to examine the efficacy of mindfulness for OCD in adult and pediatric patients diagnosed by standardized criteria (e.g. any version of the Diagnostic and Statistical Manual, DSM, or International Classification of Diseases, ICD); (b) to include at least one treatment group with pretest and posttest measures and, optionally, follow-up measures; (c) the sample size in the posttest should be greater than four participants; therefore, single-case designs were excluded; (d) the study was required to include the obsessive and compulsive symptoms as dependent variable; (e) statistical data reported in the study had to allow us to compute effect sizes, and (f) to be written in English or Spanish.
Search strategy
Firstly, several electronic databases were consulted: Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE, CINAHL, and PsycINFO. The following keywords were combined, in English and Spanish, in the electronic searches: ([obsessive compulsive disorder] or [OCD]), and ([mindfulness] or [mindfulness based intervention] or [MBI] or [mindfulness based stress reduction]) which should be in the title or the abstract. Secondly, localized studies references were reexamined. Finally, e-mails were sent to ten experts who frequently published in the area to locate unpublished studies. experts who frequently published on treatments for obsessional disorder.
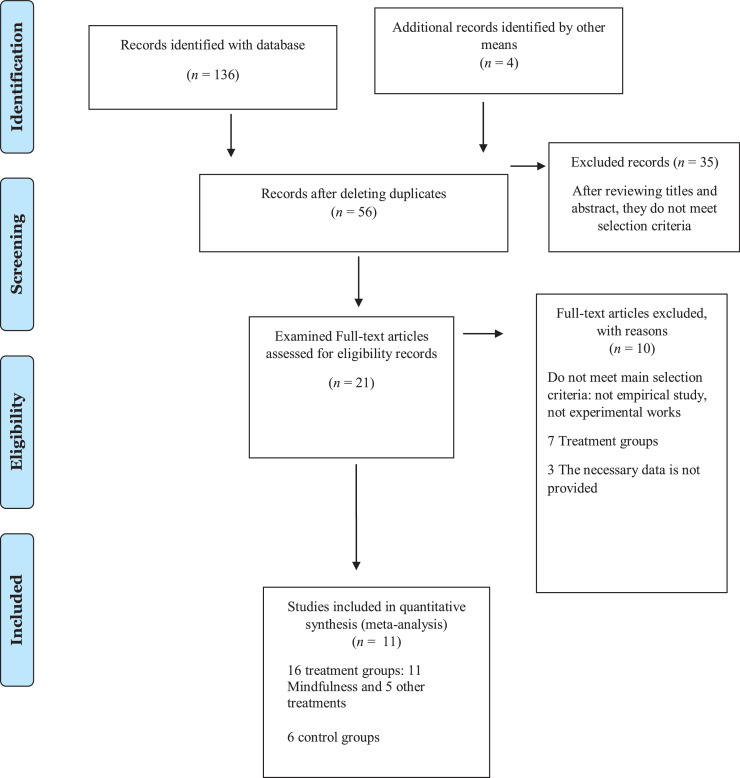
The search strategy produced a total of 140 references. (136 from the different databases and 4 extracted by other means). Figure 1 presents a flowchart summarizing the screening and selection process of studies. From all studies revised, 11 articles fulfilled selection criteria, all written in English and published between 1996 and February 2021.
Figure 1.
Flow diagram of screening and selection process of studies.
The 11 articles produced a total of 11 groups that applied mindfulness, two relaxation groups, one exposition prevention relapse group (EPR), one cognitive restructuration group, one EPR+mindfulness group and six control groups. The total sample included 550 participants in the posttest measurements, with a median sample size of 25 participants. The studies came from Germany (27.5%), Canada (27.5%), USA (9%), Iran (9%), United Kingdom (9%), Scandinavian countries (9%), and Italy (9%). Although we endeavored to locate unpublished studies, all those included in the meta-analysis were published papers.
Coding of moderator variables
In order to examine the potential influence of study characteristics on effect sizes, potential moderator variables were coded. The treatment variables coded were: (a) techniques applied to the OCD participants (mindfulness, CBT, relaxation); (b) type mindfulness (mindfulness-based stress and anxiety reduction MBSR, mindfulness-based cognitive therapy, MBCT, other); (c) CBT prior to mindfulness (yes, non); (d) treatment duration (number of weeks); (e) treatment intensity (number of weekly hours); (f) treatment magnitude (total number of intervention hours per participant); (g) mode of intervention (individual versus group).
Several participant characteristics were also coded: (a) mean age of sample (in years); (b) gender distribution (percentage of males).
The methodological variables coded were: (a) attrition from pretest to posttest, and follow-up, (b) type control group (active, inactive); and (c) methodological quality of study (on a scale of 0–6 points).1
The coding process was carried out in a standardized and systematic way since a codebook and a protocol for registering the variables2 had previously been produced. Studies were coded independently by two separate coders specialized in the field of OCD treatment. To assess reliability of the coding process, 25% of studies were randomly selected and subjected to a double coding process by two previously trained coders. Inconsistencies between the coders were resolved by consensus. Results showed very satisfactory inter-coder reliability, with kappa coefficients ranging from 0.80 to 1 for the categorical variables, and intra-class correlations between 0.95 and 1 for continuous varaibles.
Computation of effect sizes
In this meta‐analysis, the analysis unit was the group, not the study, and the effect‐size index was the standardized mean change index, defined as the difference between pretest and posttest means divided by the pretest standard deviation: , with c(m) being a correction factor for small sample sizes (Morris, 2000). A d index was calculated for each of the 16 treatment group (11 mindfulness, 5 other treatment) as well as for each of the 6 control groups included in selected studies. Positive values for d indicated a favorable change in the group from the pretest to the posttest.
Separate effect sizes (d indices) were calculated for obsessive-compulsive symptoms, depression symptoms and mindfulness coping. For reliability assessment of effect size calculations, the same random sample of studies used in the coding reliability study was subjected to a double process of effect size calculations, obtaining excellent inter-coder reliability, with intra-class correlations over 0.90. Inconsistencies between the coders were resolved by consensus. To assess the clinical significance of the average effect sizes, we rely on a systematic review of 50 meta-analyses was carried out on the effectiveness of clinical psychology treatments (Rubio-Aparicio, Sanchez-Meca, Marin-Martinez, & y Lopez-Lopez, 2019). In particular, d values around 0.64, 0.98, and 1.26 were interpreted as reflecting low, moderate, and large clinical relevance, respectively.
Statistical analysis
Separate meta-analyses were carried out with the effect sizes for each outcome measure: obsessive-compulsive, depression and mindfulness coping outcomes.
To assess heterogeneity of effect sizes, the Q statistic and I2 index were calculated. I2 indices around 25%, 50%, and 75% were interpreted as reflecting low, moderate, and large heterogeneity, respectively (Higgins, Tompson, Deeks, & Altman, 2003). For each outcome measure, a forest plot was constructed, and a weighted mean effect size with a 95% confidence interval (CI) was calculated with the improved method proposed by Sinha, Hartung, and Knapp (2011)). The first analysis consisted of comparing the mean effect size of treatment groups to control groups using the F statistic developed by Knapp and Hartung (2003). This comparison was done separately for each outcome measure and for the pretest‐posttest effect sizes. Furthermore, an adjusted average effect size was calculated for each outcome measure as dadj = dT − dC, dT, and dC were the pooled standardized pretest‐posttest mean changes in the treated group and control groups, respectively.
Given that our meta-analysis did not include unpublished papers, an analysis of publication bias was performed by constructing funnel plots with the trim-and-fill method for imputing missing effect sizes and applying the Egger test (Rothstein, Sutton, & Borenstein, 2006) The influence of moderator variables on effect sizes was carried out by assuming a mixed-effects model. ANOVAs and meta-regressions were applied for categorical and continuous moderator variables, respectively (Borenstein, Hedges, Higgins, & Rothstein, 2009). In particular, the improved t- and F- statistic developed by Knapp and Hartung (2003) were applied to assess statistical association of each moderator with obsessive-compulsive symptoms effect sizes only with those studies which applied mindfulness and control group. QW and QE statistics were computed to assess model misspecification in ANOVAs and meta-regressions, respectively. Additionally, an estimate of the proportion of variance accounted for by the moderator variable was calculated. Statistical analyses were carried out with the statistical package Comprehensive meta-analysis 3.0, CMA 3.3 (Borenstein et al., 2020).
Results
Distribution of effect sizes and heterogeneity
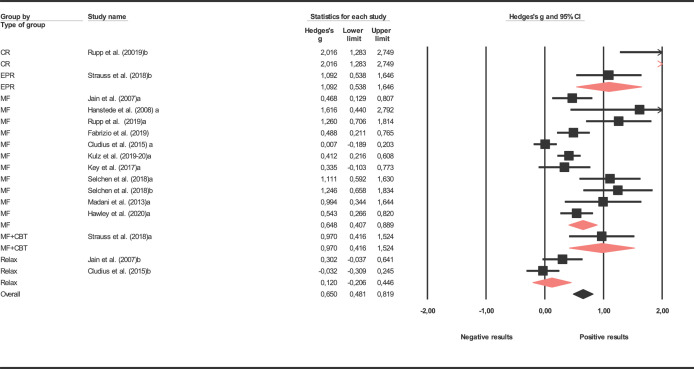
Effect sizes and characteristics for each individual study included in the meta-analysis are shown in Table 1 presents results obtained for treatment and control groups in obsessive-compulsive symptoms in posttest. Results are also presented in depression and mindfulness coping in posttest. Results in follow-up were not presented as they only reported 6 studies. The average effect size for obsessive-compulsive symptoms was statistically significant for the 11 mindfulness treatment groups reaching a medium magnitude according to Cohen (1988) in posttest (d+ = 0.666), 1 mindfulness+CBT study (d+ = 0.970) and 1 EPR study (d+ = 1.092) reaching statistical significance in postest. The mean effect size by 2 relaxation groups was low (d+ = 0.120) while the cognitive restructuring group achieved highest results (d+ =2.016). The different interventions show significant differences. However, this data must be viewed with caution as treatment categories had 1 or 2 studies, except for mindfulness. The mean effect size yielded by the six control groups in posttest was negative (d+ = -0.047). Forest plot for obsessive-compulsive symptoms are presented in Figure 2. A weighted ANOVA applied to compare the mean effects of the treatment and control groups showed statistically significant differences in favor of the treatment group (QB(1) = 138.58, p <0.001). The effect size obtained on depression was non statistically significant for the nine treatment groups which reported it, reaching a low magnitude in posttest (d+ = 0.389). The effect size in the control group was null (d+ = 0.059). The coping mindfulness effect size obtained was statistically significant between the treatment group (d+ =0.568) and control group (d+ =0.158).
Table 1.
Some characteristics and effects sizes for individual studies included in the meta-analysis.
| Study | N | Mean age | % Gender | Treatment | Mode Intervention | Duration treatment | Quality | G´s Hedges |
|---|---|---|---|---|---|---|---|---|
| Jain et al. (2007)a | 27 | 25.00 | 17.60 | Mindfulness | Group | 4 | 4.50 | 0.468 |
| Jain et al. (2007)b | 24 | 25.00 | 17.60 | Relaxation | Group | 4 | 4.50 | 0.302 |
| Jain et al. (2007)c | 30 | 25.00 | 17.60 | Control | 4.50 | -0.365 | ||
| Hanstede et al. (2008))a | 8 | 25.00 | 29.40 | Mindfulness | Group | 8 | 3.50 | 1.616 |
| Hanstede et al. (2008))b | 9 | 25.00 | 29.40 | Control | 3.50 | 0.081 | ||
| Rupp et al. (2019)a | 21 | 30.81 | 28.57 | Mindfulness | Group | 2 | 5,45 | 1.260 |
| Rupp et al. (2019)b | 22 | 31.23 | 54.54 | Cognitive Restructuring | Group | 2 | 5.50 | 2.016 |
| Rupp et al. (2019)c | 21 | 30.43 | 42.86 | Control | 4.46 | 0.087 | ||
| Didonna et al., 2019 | 35 | 37.20 | 57.00 | Mindfulness | Group | 11 | 3.50 | 0.488 |
| Cludius et al. (2015)a | 49 | 39.88 | 38.77 | Mindfulness | Individual | 6 | 2.54 | 0.007 |
| Cludius et al. (2015)b | 38 | 41.37 | 26.31 | Relajación | Individual | 6 | 2.61 | -0.032 |
| Külz et al. (2019)-20)a | 61 | 37.61 | 34.40 | Mindfulness | Group | 8 | 3.82 | 0.412 |
| Külz et al. (2019)-20)b | 64 | 39.59 | 42.20 | Control | 3.83 | 0.263 | ||
| Key et al. (2017)a | 18 | 40.53 | 50.00 | Mindfulness | Group | 8 | 2.73 | 0.335 |
| Key et al. (2017)b | 18 | 46.06 | 55.60 | Control | 3.34 | -0.193 | ||
| Selchen et al. (2018)a | 19 | 40.68 | 36.80 | Mindfulness | Group | 8 | 4.00 | 1.111 |
| Selchen et al. (2018)b | 18 | 43.61 | 44.40 | Mindfulness | Group | 8 | 4.00 | 1.246 |
| Strauss et al. (2018)a | 19 | 33.00 | 21.00 | Mindfulness+ CBT | Group | 10 | 4.64 | 0.970 |
| Strauss et al. (2018)b | 18 | 27.00 | 50.00 | Exposición | Group | 10 | 4.67 | 1.092 |
| Madani et al. (2013)a | 15 | 0.00 | Mindfulness | Group | 4 | 2.80 | 0.994 | |
| Madani et al. (2013)b | 15 | 0.00 | Control | 2.80 | -0.221 | |||
| Hawley et al. (2020) | 36 | 26.00 | Mindfulness | Individual | 8 | 5.45 | 0.543 |
N: sample size in posttest for each group, Treatment duration (number of), G´s Hedges: effect size for obsessive-compulsive symptoms pre-postest outcome.
Figure 2.
Forest plot of effect sizes for obsessive-compulsive symptoms and grouped as a function of type of treatment.
Note. d index = standardized pretest-posttest mean change. CR: Cognitive restructuration; EPR: Exposition prevention relapse; MF: Mindfulness; MF+CBT: Mindfulness+ Cognitive Behavioral Therapy; Relax = relaxation.
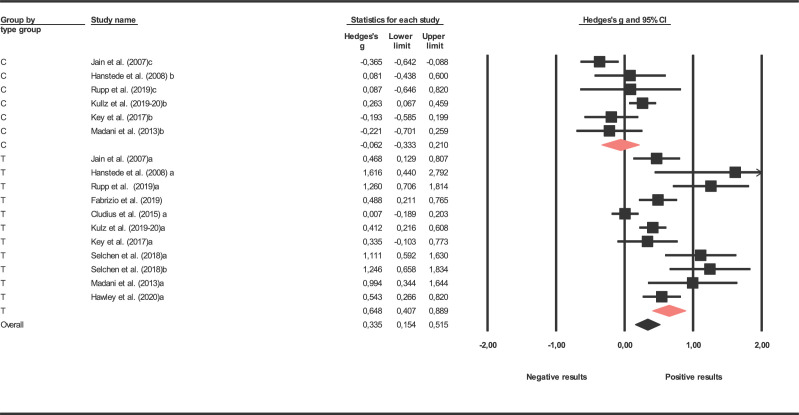
As the main interest of the study was focused on mindfulness techniques, we compare mindfulness with the control groups. Significant differences were found only in the obsessive-compulsive variable (p = .003, R2 = 0.51) (Table 2). Forest plots for obsessive-compulsive symptoms are presented in Figure 3.
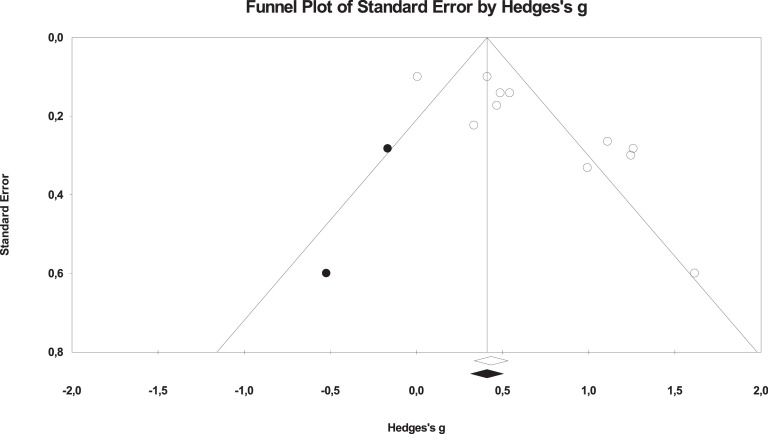
Figure 4.
Funnel plot of 11 d indices for Mindfulness treatment groups when applying standard error.
Table 2.
Results for effect sizes as a function of the outcome measure for treatment and control groups.
| All treatment groups (k = 16) | Control groups (k = 6) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome Measure | k | d+ | 95% CI LL UL | Q I2 | k | d+ | 95% CI LL UL | Q I2 | ||||
| Obsessive-compulsive | 16 | 0.732 | 0.487 | 0.986 | 122.964*** | 87.801 | 6 | -0.047 | -0.291 | 0.198 | 15.615* | 67.980 |
| Depression | 9 | 0.389 | 0.217 | 0.561 | 17.667* | 54.717 | 2 | 0.059 | -0.337 | 0.455 | 3.378 | 70.400 |
| Mindfulness coping | 8 | 0.568 | 0.242 | 0.893 | 44.785*** | 84.370 | 2 | 0.158 | -0.017 | 0.334 | 0.874 | 0.000 |
| Mindfulness groups (k = 11) | Control Groups (k = 6) | |||||||||||
| Obsessive-compulsive | 11 | 0.648 | 0.407 | 0.889 | 48.389*** | 83.670 | 6 | -0.062 | -0.333 | 0.210 | 15.463* | 67.665 |
| Depression | 6 | 0.417 | 0.190 | 0.644 | 14.362* | 65.186 | 2 | 0.059 | -0.337 | 0.455 | 3.378 | 70.400 |
| Mindfulness coping | 6 | 0.509 | 0.126 | 0.891 | 38.866*** | 87.135 | 2 | 0.158 | -0.017 | 0.334 | 0.874 | 0.000 |
* p < .05. ** p < .01. *** p < .001. 95% C.I.: 95% confidence interval. k = number of studies. Q = heterogeneity statistic. I2 = heterogeneity index (%). d+ = mean effect size. dl and du = lower and upper confidence limits.
Figure 3.
Forest plot of the effect sizes for the obsessive-compulsive symptoms and grouped as a function of Mindfulness treatment and control group.
Note. d index = standardized pretest-posttest mean change. C = Control. T = treatment.
Publication bias
All studies included in this meta-analysis were published papers. To assess the existence of publication bias the Egger test was applied to the d indices obtained from the treatment groups. Finding a non-statistically significant result for the intercept can be interpreted as evidence against publication bias. In our case, this result was obtained with the Egger test: T = 4.117, p =0.001. Finally, publication bias was also assessed by constructing a funnel plot and applying the Duval and Tweedie's (2000) ‘trim-and-fill’ method. Figure 3 presents the funnel plot obtained with the 11 original d indices for the mindfulness treatment groups. The trim-and-fill method imputed two values to achieve symmetry in the funnel plot. When a mean effect (and its 95% CI) was calculated with the 11 d indices plus the two imputed values, we obtained d+ = 0.409 (95% CI: 0.313 and 0.505).
Predictor/Moderator of obsessive-compulsive effect sizes
Analysis of moderating variables was carried out on the 11 studies which used the mindfulness treatment. As Table 2 shows, the 11 effect sizes for the mindfulness treatment groups exhibited large heterogeneity in obsessive-compulsive symptoms (I2 = 83.670%). Consequently, analyses were performed of the characteristics of studies that could affect effect size variability.
Tables 3 and 4 present the results of the simple meta-regressions and ANOVAs for the continuous and categorical moderators, respectively. Regarding simple meta-regressions, one of them revealed statistically significant relationship with the obsessive-compulsive symptoms: the sample size (p = .022; R2 = 0.52).
Table 3.
Results of ANOVAs for the influence of qualitative variables on effect sizes for obsessive-compulsive symptoms.
| Moderator variable | k | d+ | 95%C.I.dl du | ANOVA results |
|---|---|---|---|---|
|
Type mindfulness MBCT MBSR DM Others |
5 1 1 4 |
0.522 0.468 1.260 0.256 |
0.382 0.662 0.129 0.807 0.706 1.814 |0.102 0.410 |
F(3, 7) = 0.53, p = .667 R2 = 0.0 QW(10) = 48.389, p = .000 |
|
Mode of intervention: Individual Group |
9 2 |
0.580 0.186 |
0.457 0.704 0.026 0.346 |
F(1,9) = 2,90, p =0.123 R2 = 0.20 QW(10) = 43.389, p > .000 |
| Previous treatment Yes No |
3 8 |
0.599 0.690 |
0.162 1.036 0.365 1.014 |
F(1,9) =0.06, p =0.810 R2 = 0.0 QW(9) = 48.389, p = .000 |
| Management intervention With therapist No therapist |
9 2 |
0.746 0.266 |
0.499 0.993 -0.259 0.791 |
F(1,9) =2,90, p =0.123 R2 = 0.20 QW(9) = 27.508, p = .001 |
Note. k = number of studies. d+ = mean effect size for each category. 95% C.I. = 95% confidence interval for d+. dl and du = lower and upper confidence limits around d+. QW: within-categories statistic. F = Knapp-Hartung's statistic. R2 = proportion of variance explained. MBCT: Mindfulness Based Cognitive Therapy; MBRS: Mindfulness based reduction stress; DM: Deteached Mindfulness.
Table 4.
Results of simple meta-regressions of continuous variables on effect sizes for obsessive-compulsive measures.
| Cluster/moderator variable | k | bj | t | p | R2 |
|---|---|---|---|---|---|
| Treatment duration | 11 | -0.035 | -0.60 | .566 | .00 |
| Treatment intensity | 10 | 0.035 | 0.23 | .882 | .00 |
| Treatment magnitude | 10 | -0.012 | -0.67 | .519 | .00 |
| Mean age | 10 | -0.001 | -0.31 | .310 | .00 |
| Gender | 10 | -0.008 | -0.78 | .459 | .00 |
| Attrition postest | 11 | -0.613 | -0.37 | .721 | .00 |
| Sample size | 11 | -0.019 | -2.76 | .022 | .52 |
| Methodological quality | 11 | 0.171 | 1.26 | .238 | .15 |
Note. ** p < .001. k = number of studies. bj = regression coefficient. t = statistic for testing significance of each predictor. p = probability level for the t statistic. R2 = proportion of variance accounted for by the predictors.
Discussion
The aims of this work were to verify whether intervention through mindfulness is an effective treatment in obsessive compulsive disorder, both in a general way and in comparison with other treatments or used as complementary therapy for treatment of residual symptoms following cognitive behavioral therapy. Likewise, in this study the modulating role that other variables might play in the efficacy of this form of intervention has been assessed.
The effect size was statistically significant in obsessive-compulsive symptoms for the 11 groups of FM treatment, with a mean magnitude according to Cohen (1988) in post-test (d+ = 0.648). However, some studies presented low effect sizes (Cludius et al., 2015; Key, Rowa, Bieling, McCabe, & Pawluk, 2017; Külz et al., 2019). Cludius et al. (2015) used self-administered mindfulness sessions through audio recordings. Rosa-Alcázar, Sánchez-Meca, Gómez-Conesa, and Marín-Martínez (2008) observed the importance of the therapist, since the therapist-guided exposure therapies were better than self-exposure therapies. Key et al. (2017), Külz et al. (2019) and Landmann, Cludius, Tuschen-Caffier, Moritz, and Külz (2020) used participants who had previously received behavioral therapy based on exposure and response prevention, maintaining residual symptoms in the former and with refractory patients in the latter, in other words patients resistant to treatment. Thus, we can report that mindfulness treatment is effective in reducing obsessive-compulsive symptoms following treatment.
As regards other benefits related to the application of mindfulness in patients with obsessive compulsive disorder, the size of the depression effect was medium-low magnitude (d+ = 0.417), while the magnitude of the effect on coping skills was medium (d+ = 0.509). Therefore, this intervention not only improves obsessive-compulsive symptoms but also reduces depressive responses. In line with that found in some previous research, as depression is often comorbid with OCD, improvements in obsessive-compulsive symptoms also lead to improvements in depression, but to a lesser degree.
As for the usefulness of mindfulness-based therapies as an effective procedure compared to other forms of treatment, we observed that techniques based on EPR and cognitive-restructuring reached highest effect sizes but were not representative due to the small number of included studies in each type of treatment. Specifically, Strauss et al. (2018) used two treatment groups, one based on ERP and the other on ERP based on mindfulness. Analysis of effect sizes showed that both groups improved in obsessive-compulsive symptoms after treatment and six months of follow-up. They also compared two interventions, cognitive restructuring and mindfulness, observing a significant improvement in both groups; that based on CBT being greater (Rosa-Alcázar et al., 2008). However, a greater number of studies by type of treatment is required to reach definitive conclusions.
Another of our proposed aims was to study whether mindfulness-based interventions could be an appropriate option as complementary therapy followng the use of other intervention procedures, specifically CBT. Results did not show significant differences with respect to its application as an initial form of treatment (p = .81). Nevertheless, these results should again be taken with caution, since there were only three studies where another therapeutic option was developed prior to mindfulness-based therapy. Specifically, in the study carried out by Selchen, Hawley, Regev, Richter, and Rector (2018), two mindfulness-based therapy groups were developed, one after the 14-week CBT treatment, without statistically significant differences between the two groups. Külz et al. (2019) used 125 patients with OCD and residual symptoms after cognitive behavioral therapy was used. Finally, Key et al. (2017) used a treatment based on the MBCT program tested in patients refractory to CBT, results showing a significant improvement when comparing treatment group with control group. This leads us to conclude that mindfulness, both as an initial treatment for OCD and as a complementary treatment, is effective, showing a medium effect size.
A further aim was to analyze the moderating role of some characteristics of studies. Of all variables analyzed, only the number of participants per group reached statistical significance, explaining 52% variance. Specifically, it was observed that the larger the sample size, the smaller the effect sizes. This is in line with other studies and reports the need to be able to work with groups where the therapist can meet participants and adapt the treatment to their characteristics (Leeuwerik, Cavanagh, & Strauss, 2019). We must indicate that perhaps the low number of included studies prevented us from reaching more relevant conclusions regarding the implication of moderating variables in results.
Results obtained in this work have important clinical implications. Firstly, they appear promising regarding the usefulness of the application of intervention programs based on mindfulness in people with obsessive-compulsive disorder, improving both obsessive-compulsive and depressive responses, although to a lesser extent in the latter. On the other hand, comparison between mindfulness intervention groups developed on patients with or without previous CBT interventions did not yield significant differences. This seems to support the usefulness of mindfulness in residual symptoms and / or in patients refractory to the intervention procedures of choice in this disorder. However, only one study compared normal ERP and mindfulness-based ERP (Strauss et al., 2018).
This research is not without limitations. Firstly, the scarcity of randomized clinical trials comparing the efficacy of mindfulness-based treatment groups and other types of treatment in patients with obsessive compulsive disorder. Secondly, we were unable to carry out an optimal account of results maintenance since only 6 studies reported follow-up data. Nonetheless, results obtained in analyzed studies seem to support theoretic proposals drawn by different authors such as Landmann et al. (2020)), or Rupp et al. (2019)) who indicate that psychological intervention based on mindfulness may be a valid option in patients who do not respond adequately to more traditional psychological treatments.
Another important aspect to highlight is that, as it is known, mindfulness-based treatment is a form of intervention that is not explicitly focused on the symptomatic treatment of specific psychological disorders (Bravo, Lindsay, & Pearson, 2022). In this sense, there is considerable heterogeneity in the intervention programs applied in the different studies with which we have worked. Thus, while some studies applied adaptations of the mindfulness program for stress and anxiety reduction (MBRS) (Hanstede, Gidron, & Nyklíček, 2008; Jain et al., 2007), other studies used adaptations of mindfulness-based cognitive therapy for the treatment of depression (MBCT) (Selchen et al., 2018; Strauss et al., 2018) and other works developed specific packages on mindfulness training (Hanstede et al., 2008; Madani, Kananifar, Atashpour, & Habil, 2013).
Footnotes
The items comprising the methodological quality scale were: (1) random versus non-random assignment of participants to the groups; (2) the internal validity of the design (active control group, non-active control group or no control group); (3) the sample size in the postest; (4) attrition in the treatment group; (5) the use of intent-to-treat analysis, and (6) the use of blinded assessors in measuring the outcomes. Each one was rated from 0 to 1.
Both documents can be obtained from the corresponding author upon request.
References
- Afshari B. In: What to know about mindfulness. Carvalho T.A., editor. Hauppauge, NY: Nova Science Publishers; 2020. Psychology of mindfulness: Revisiting past and present researches, prospects ahead, and move toward future directions; pp. 47–97. [Google Scholar]
- Borenstein M., Hedges L.V., Higgins J.P.T., Rothstein H.R. John Wiley & Sons; Chichester, UK: 2009. Introduction to meta-analysis. [Google Scholar]
- Borenstein M., Cooper H., Hedges L., Valentine J. Effect sizes for continuous data. he handbook of research synthesis and meta-analysis. 2009;2:221–235. [Google Scholar]
- Bravo A.J., Lindsay E.K., Pearson M.R. Handbook of assessment in mindfulness research. Springer International Publishing; New York: 2022. Nature, Assessment, and Mechanisms of Mindfulness; pp. 1–12. [Google Scholar]
- Cludius B., Hottenrott B., Alsleben H., Peter U., Schröder J., Moritz S. ¿Mindfulness para el TOC? No hay evidencia de un efecto directo de un enfoque de tratamiento de autoayuda. Journal of Obsessive-Compulsive and Related Disorders. 2015;6:59–65. doi: 10.1016/j.jocrd.2015.05.003. * [DOI] [Google Scholar]
- Cludius B., Landmann S., Rose N., Heidenreich T., Hottenrott B., Schröder J., et al. Long-term effects of mindfulness-based cognitive therapy in patients with obsessive-compulsive disorder and residual symptoms after cognitive behavioral therapy: Twelve-month follow-up of a randomized controlled trial. Psychiatry Research. 2020;291:113–119. doi: 10.1016/j.psychres.2020.113119. [DOI] [PubMed] [Google Scholar]
- Cohen J. 2ª ed. New York: Erlbaum; 1988. Statistical power analisys for the behavior. [Google Scholar]
- Didonna F. The Guilford Press; New York: 2020. Mindfulness-based cognitive therapy for OCD: A treatment manual. [Google Scholar]
- Didonna F., Lanfredi M., Xodo E., Ferrari C., Rossi R., Pedrini L. Mindfulness-based cognitive therapy for obsessive-compulsive disorder: A pilot study. Journal of Psychiatric Practice. 2019;25:156–170. doi: 10.1097/PRA.0000000000000377. * [DOI] [PubMed] [Google Scholar]
- Duval S., Tweedie R. Trim and fill: A simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–463. doi: 10.1111/j.0006-341X.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- Fairfax H. The use of mindfulness in obsessive compulsive disorder: Suggestions for its application and integration in existing treatment. Clinical Psychology & Psychotherapy: An International Journal of Theory & Practice. 2008;15:53–59. doi: 10.1002/cpp.557. * [DOI] [PubMed] [Google Scholar]
- Fawcett E.J., Power H., Fawcett J.M. Women Are at Greater Risk of OCD Than Men: A Meta-Analytic Review of OCD Prevalence Worldwide. The Journal of Clinical Psychiatry. 2020;81:19r13085. doi: 10.4088/JCP.19r13085. [DOI] [PubMed] [Google Scholar]
- Fisher P.L., Cherry M.G., Stuart T., Rigby J.W., Temple J. People with obsessive-compulsive disorder often remain symptomatic following psychological treatment: A clinical significance analysis of manualised psychological interventions. Journal of Affective Disorders. 2020;275:94–108. doi: 10.1016/j.jad.2020.06.019. [DOI] [PubMed] [Google Scholar]
- Hamatani S., Tsuchiyagaito A., Nihei M., Hayashi Y., Yoshida T., Takahashi J., Hirano Y., et al. Predictors of response to exposure and response prevention-based cognitive behavioral therapy for obsessive-compulsive disorder. Bmc Psychiatry [Electronic Resource] 2020;20(433) doi: 10.1186/s12888-020-02841-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen B., Kvale G., Hagen K., Havnen A., Öst L.-G. The Bergen 4-day treatment for OCD: Four years follow-up of concentrated ERP in a clinical mental health setting. Cognitive Behaviour Therapy. 2019;48:89–105. doi: 10.1080/16506073.2018.1478447. [DOI] [PubMed] [Google Scholar]
- Hanstede M., Gidron Y., Nyklíček I. Los efectos de una intervención de atención plena sobre los síntomas obsesivo-compulsivos en una población estudiantil no clínica. The Journal of Nervous and Mental Disease. 2008;196:776–779. doi: 10.1097/NMD.0b013e31818786b8. * [DOI] [PubMed] [Google Scholar]
- Hawley L.L., Rogojanski J., Vorstenbosch V., Quilty L.C., Laposa J.M., Rector N.A. The structure, correlates, and treatment related changes of mindfulness facets across the anxiety disorders and obsessive compulsive disorder. Journal of Anxiety Disorders. 2017;49:65–75. doi: 10.1016/j.janxdis.2017.03.003. * [DOI] [PubMed] [Google Scholar]
- * Hawley, L. L., Rector, N. A., Da Silva, A., Laposa, J. M., & Richter, M. A. (2020). Technology Supported Mindfulness for Obse ssive Compulsive Disorder: Self-Reported Mindfulness and EEG Correlates of Mind Wandering. Behaviour Research and Therapy, Preprints. E-Journals. https://search.ebscohost.com/login.aspx?direct=true&db=eoah&AN=54447641&lang=es&site=ehost-live&scope=site. [DOI] [PubMed]
- Higgins J., Tompson S., Deeks J., Altman D. A meta-analysis on the effectiveness of smart-learning. Bmj. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain S., Shapiro S.L., Swanick S., Roesch S.C., Mills P.J., Bell I., Schwartz G.E.R., et al. A randomized controlled trial of mindfulness meditation versus relaxation training: Effects on distress, positive states of mind, rumination, and distraction. Annals of Behavioral Medicine. 2007;33:11–21. doi: 10.1207/s15324796abm3301_2. * [DOI] [PubMed] [Google Scholar]
- Johnco C., McGuire J.F., Roper T., Storch E.A. A meta-analysis of dropout rates from exposure with response prevention and pharmacological treatment for youth with obsessive compulsive disorder. Depression and Anxiety. 2020;37:407–417. doi: 10.1002/da.22978. [DOI] [PubMed] [Google Scholar]
- Keleher J., Jassi A., Krebs G. Clinician-reported barriers to using exposure with response prevention in the treatment of paediatric obsessive-compulsive disorder. Journal of Obsessive-Compulsive and Related Disorders. 2020;24 doi: 10.1016/j.jocrd.2019.100498. * [DOI] [PMC free article] [PubMed] [Google Scholar]
- Key B.L., Rowa K., Bieling P., McCabe R., Pawluk E.J. Mindfulness-based cognitive therapy as an augmentation treatment for obsessive–compulsive disorder. Clinical Psychology & Psychotherapy. 2017;24:1109–1120. doi: 10.1002/da.22978. [DOI] [PubMed] [Google Scholar]
- Knapp G., Hartung J. Improved tests for a random effects meta-regression with a single covariate. Statistics in Medicine. 2003;22:2693–2710. doi: 10.1002/sim.1482. [DOI] [PubMed] [Google Scholar]
- Külz A.K., Landmann S., Cludius B., Rose N., Heidenreich T., Jelinek L., Moritz S., et al. Mindfulness-based cognitive therapy (MBCT) in patients with obsessive–compulsive disorder (OCD) and residual symptoms after cognitive behavioral therapy (CBT): A randomized controlled trial. European Archives of Psychiatry and Clinical Neuroscience. 2019;269:223–233. doi: 10.1007/s00406-018-0957-4. * [DOI] [PubMed] [Google Scholar]
- Landmann S., Cludius B., Tuschen-Caffier B., Moritz S., Külz A.K. Changes in the daily life experience of patients with obsessive-compulsive disorder following mindfulness-based cognitive therapy: Looking beyond symptom reduction using ecological momentary assessment. Psychiatry Research. 2020;286 doi: 10.1016/j.psychres.2020.112842. [DOI] [PubMed] [Google Scholar]
- Law C., Boisseau C.L. Exposure and Response Prevention in the Treatment of Obsessive-Compulsive Disorder: Current Perspectives. Psychology Research and Behavior Management. 2019;12:1167–1174. doi: 10.2147/PRBM.S211117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeuwerik T., Cavanagh K., Strauss C. The association of trait mindfulness and self-compassion with obsessive-compulsive disorder symptoms: Results from a large survey with treatment-seeking adults. Cognitive Therapy and Research. 2019;44:120–135. doi: 10.1007/s10608-019-10049-4. [DOI] [Google Scholar]
- Madani N.A.M., Kananifar N., Atashpour S.H., Habil M. The effects of mindfulness group training on the rate of obsessive-compulsive disorder symptoms on the women in Isfahan City (Iran) International Medical Journal. 2013;20:13–17. http://prof.khuisf.ac.ir/images/Uploaded_files/1[8219592].PDF * [Google Scholar]
- Morris S.B. Distribution of the standardized mean change effect size for meta-analysis on repeated measures. British Journal of Mathematical and Statistical Psychology. 2000;53:17–29. doi: 10.1348/000711000159150. [DOI] [PubMed] [Google Scholar]
- Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Bmj. 2021;372 doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Aranda A., García-Campayo J., Gude F., Luciano J.V., Feliu-Soler A., González-Quintela A., Montero-Marinh J., et al. Impact of mindfulness and self-compassion on anxiety and depression: The mediating role of resilience. International Journal of Clinical and Health Psychology. 2021;21(2) doi: 10.1016/j.ijchp.2021.100229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosa-Alcázar Á., García-Hernández M.D., Parada-Navas J.L., Olivares-Olivares P.J., Martínez-Murillo S., Rosa-Alcázar A.I. Coping strategies in obsessive-compulsive patients during Covid-19 lockdown. International Journal of Clinical and Health Psychology. 2021;21(2):100223. doi: 10.1016/j.ijchp.2021.100223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosa-Alcázar Á., Rosa-Alcázar A.I., Olivares-Olivares P.J., Parada-Navas J.L., Rosa-Alcázar E., Sánchez-Meca J. Family involvement and treatment for young children with Obsessive-Compulsive Disorder: Randomized control study. International Journal of Clinical and Health Psychology. 2019;19:218–227. doi: 10.1016/j.ijchp.2019.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosa-Alcázar A.I., Sánchez-Meca J., Gómez-Conesa A., Marín-Martínez F. Psychological treatment of obsesive-compulsive disorder: A meta-analysis. Clinical Psychology Review. 2008;28:1310–1325. doi: 10.1016/j.cpr.2008.07.001. [DOI] [PubMed] [Google Scholar]
- Rothstein H.R., Sutton A.J., Borenstein M. West Sussex: John Wiley & Sons; 2006. Publication bias in meta-analysis: Prevention, assessment and adjustments. [Google Scholar]
- Rubio-Aparicio M., Sanchez-Meca J., Marin-Martinez F., y Lopez-Lopez J.A. Directrices para la presentación de informes de revisiones sistemáticas y metanálisis. [Guidelines for reporting systematic reviews and meta-analyses.] Anales De Psicología /Annals of Psychology. 2019;34:412–420. doi: 10.6018/analesps.34.2.320131. [DOI] [Google Scholar]
- Rupp C., Falke C., Gühne D., Doebler P., Andor F., Buhlmann U. A study on treatment sensitivity of ecological momentary assessment in obsessive–compulsive disorder. Clinical Psychology & Psychotherapy. 2019;26:695–706. doi: 10.1002/cpp.2392. * [DOI] [PubMed] [Google Scholar]
- Selchen S., Hawley L.L., Regev R., Richter P., Rector N.A. Mindfulness-based cognitive therapy for OCD: Stand-alone and post-CBT augmentation approaches. International Journal of Cognitive Therapy. 2018;11:58–79. doi: 10.1007/s41811-018-0003-3. * [DOI] [Google Scholar]
- Sinha B.K., Hartung J., Knapp G. Hoboken, NJ: John Wiley & Sons; 2011. Statistical meta-analysis with applications. [Google Scholar]
- Strauss C., Lea L., Hayward M., Forrester E., Leeuwerik T., Jones A.M., Rosten C., et al. Mindfulness-based exposure and response prevention for obsessive compulsive disorder: Findings from a pilot randomised controlled trial. Journal of Anxiety Disorders. 2018;57:39–47. doi: 10.1016/j.janxdis.2018.04.007. * [DOI] [PubMed] [Google Scholar]
- World Medical Association World Medical Association Declaration of HelsinkiEthical Principles for Medical Research Involving Human Subjects. Jama. 2013;310:2191–2194. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]