Abstract
The objective
this study aims to investigate the relationship between folic acid and colorectal cancer (CRC).
Methods
google scholar, Pubmed, Pubmed central were searched from 1994 to 2022 for articles on the association between folic acid and CRC using the combinations: folic acid and colorectal cancer risk, folic acid and colorectal cancer survival, folic acid and colorectal cancer recurrence.
Main message
to describe and discuss the effect that folic acid might play on colorectal cancer (CRC) risk, recurrence and survivals, taking into account the possible differences between the men and women.
Conclusion
Our article supports the idea that says: vit-B9 has a dual-modulator effect on CRC carcinogenesis. However, its role in preventing recurrence and improving survival rates remains unresolved with a possible potential role of folate metabolism genotype variations. Therefore, more evidence from clinical studies is needed.
Keywords: Folic acid, Colorectal cancer, Recurrence, Survival, Risk
Highlights
-
•
Colorectal cancer is one of the most life-threatening tumors.
-
•
Folic acid plays important role in multiple pathologies.
-
•
Folic acid has a dual-modulator effect on the colorectal cancer tumorgenesis.
-
•
The role of folate in preventing recurrence and improving survival rates remains unresolved.
1. Introduction
CRC is one of the most threatening tumors, comprising 10.2% of all diagnosed tumors and 9.2% of cancer-related mortality worldwide [1]. In 2018, it was ranked the third malignancy in incidence, and the second malignancy in mortality related to cancer [2]. The CRC rates are expected to increase [2] despite the screening programs [3].
Vit-B9 (folic acid; FA) is a water-soluble vitamin that plays a significant role in de novo synthesis of purines and thymidine as well as its essential role in preventing several disorders such as megaloblastic anemia, atherosclerosis, neural tube defects and cancer [4]. Herein, we aim to clarify the relationship between folic acid and CRC.
2. Methods
Google scholar, Pubmed, Pubmed central were searched from 1994 to 2022 for articles on the association between folic acid and CRC using the combinations: folic acid and colorectal cancer risk, folic acid and colorectal cancer survival, folic acid and colorectal cancer recurrence.
3. Discussion
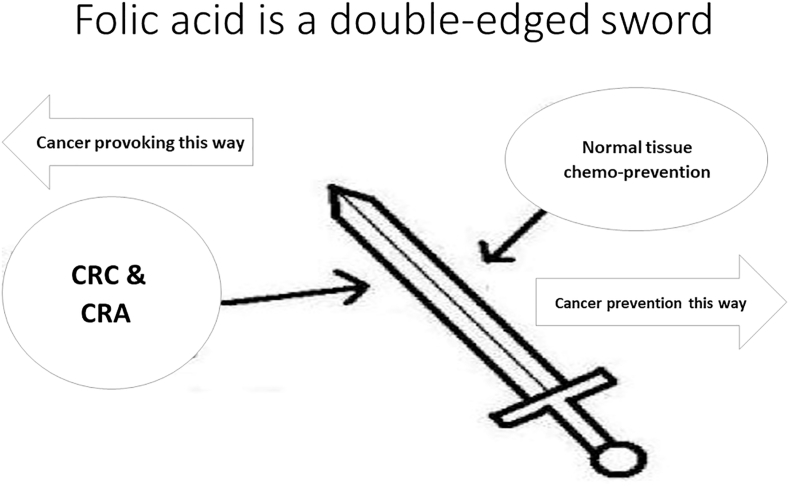
3.1. Folate & CRC risk: folic acid is a double-edged sword
The relationship between folate and cancer seems to be contradictory [4]. In malignant cells and other rapidly dividing ones, antifolate agents slower the tumor growth as they cause ineffective DNA synthesis [4]. However, folate deficiency predisposes normal tissues to malignant transformations; which explains the protective role of folate in preventing carcinogenesis [4]. However, Hubner, R A et al [5] study found a similar results, suggesting a dual-modulator effect (Fig. 1) of folate on the CRC tumorgenesis; in which folate has a preventive role in the absence of malignant foci and a provoking effect in the presence of such foci (Table 1).
Fig. 1.
Vit-B9 has a dual-modulator effect on CRC carcinogenesis.
Table 1.
Folate & CRC risk.
| Study (first author) | size | Duration | Study design | Effect on crc risk |
|---|---|---|---|---|
| VAN GUELPEN, B ET AL 2006 (7) | 663 | 4.2 years | Prospective study based on the Northern Sweden Health and Disease Study (NSHDS) | Low folate status is associated with decreased CRC risk |
| COLE, BERNARD F ET AL 2007 (12) | 1021 | 10 years | Randomized-control trial (RCT) | No effect |
| GAO, QIN-YAN ET AL 2013 (13) | 800 | 3 years | RCT | Folate supplementation is associated with decreased CRC risk |
| GYLLING, BJÖRN ET AL 2014 (8) | 993 | 10.8 years | Nested case-control study within NSHDS, included subjects from Västerbotten Intervention Program (VIP) & Mammography Screening Project (MSP) populations | Low folate status is associated with decreased CRC risk |
| QIN, TINGTING ET AL 2015 (10) | – | – | Meta-analysis | No effect |
| DING, HUI ET AL 2016 (29) | 1310 | participants without CRA was 2.1 years compared with 1.8 years for patients with CRA. | Prospective study | High folate status is associated with decreased CRC risk & recurrence |
| MOAZZEN, SARA ET AL 2018 (9) | – | – | Meta-analysis | No effect |
| MOAZZEN, SARA ET AL 2020 (11) | 405 | 10 years | Case-control | No effect |
The association between folate intake and CRC risk seems to be complicated as it depends on multiple factors such as gender, age, alcohol consumption, and smoking [6]. However, some studies found that low plasma folate was associated with lower CRC risk [7,8]. Whereas, other studies found no effect of folate on CRC risk at all [[9], [10], [11]]. In 2007, a randomized-control trail (RCT) was performed by Cole, Bernard F et al [12], found that 1 mg/dl intake of folic acid had no effect on reducing CRC risk, in contrast with Gao, Qin-Yan et al [13], which revealed a significant reduction in colorectal adenoma especially left-sided ones. Furthermore, in Larsson, Susanna C et al [14] cohort study, caffeine and smoking were tested for their effect on the relationship between vit B9 and CRC. Interestingly, caffeine has not modified the relation, in contrast with smoking, which suggests that smokers may take advantage from high vit B9 intake. In 2013, a prospective study found that folate fortification may decrease the cancerous effect of alcohol on colorectal mucosa [15].
In 2011, a study performed by Sie KK, Medline A et al [16]determined that maternal folic acid supplementation recommended to women at child-bearing-age was associated with lower colorectal cancer risk in the offspring. However, in 2020, a case-control study found an opposite result [10]. Interestingly, the association between folate and CRC risk may differ between genders. This result was observed in a cohort study performed by Brink, Mirian et al [17]; which stated that no association was found between Dietary folate intake and colon cancer risk in both sexes, regardless of the presence of k-Ras mutations. However, this situation was different for rectal cancer, as an inverse association was found between folate intake and rectal cancer risk in men especially with K-Ras mutated tumors, whereas an increased association was found in women.
3.2. Folate & CRC survival
Several researches were concerned about the effect of folic acid on CRC survival rate with mixed results ranging from supporting to opposing its use in CRC patients. According to Ting PC, Lee WR [18] study; patients who take folic acid had a significant improve in CRC survival, that was attributed to its role in inhibiting colorectal cancer cell proliferation and migration. However, a different result was observed in Focus consortium [19] study as folic acid levels and its derivatives were not associated with neither CRC survival nor CRC recurrence. In 2003, a cohort study found that CRC patients who took both 5FU and folinic acid had less survival rate than those who took 5FU alone [20]. However, this result was opposed in 2015 by Mayer, Benjamin et al [21] study, which showed for the first time, that the addition of folinic acid to adjuvant chemotherapy regiments had given a better outcome among colon cancer (CC) patients, especially among the elderly.
3.3. Folate & CRC/A recurrence
Several studies also discussed the relationship between folate supplementation and CRC recurrence, yielding different results as many of them found no protective role against colorectal adenoma (CRA) and carcinoma (CRC) [[22], [23], [24], [25]]. The ukCAP [26] & Greece [27] trials found that folate supplementation with 0.5–1 mg/day had no effect on CRA recurrence. However, the Detroit VA trial [28]; in which individuals with resected adenoma were supplied with 5 mg/day of vit-B9 for 3 years, reported a significant decrease in CRA recurrence. In Nurses' Health Study/Health Professionals Follow-Up Study (NHS-HPFS) [22], although 1 mg/day supplementation of vit-B9 within 3 years was fond to decrease the CRA risk in those with low baseline plasma folate concentration(≤7.5 ng/ml), the overall effect didn't affect CRA recurrence. Moreover, the Aspirin/Folate Polyp Prevention study (AFPPS) [12]stated that 1 mg/day supplementation of folate for 6years was associated with 67% increased risk of CRA recurrence. In Ding, Hui et al. study, higher plasma folate concentrations were associated with decreased CRA occurrence and recurrence [29].In 2011, a combined analysis of the AFPPS, NHS-HPFS, & ukCAP studies was performed and determined no effect of folate supplementation on CRA recurrence [30]. In 2013, a meta-analysis of the mentioned studies found a borderline increased risk of CRA recurrence [31].This can be explained by the presence of pre-existing undiagnosed neoplastic foci [32] or can be attributed to genotype variations of folate metabolism as a significant decrease in CRC recurrence was found among patients heterozygous for MTRR A66G and MTHFR A1298C polymorphisms. Moreover, a significant reduction in recurrence was also seen in MTRR A66G heterozygotes who received folate supplementation but not in those who didn't receive it. However, MTHFR C677T and MTR A2756G polymorphism had no significant reduction, in addition to the TSER, TSER 3R G > C and TS14de16 variants that had no effect on recurrence at all [33]. These findings suggest that genotype variations of folate metabolism may affect the development of CRA [33] (Table 2).
Table 2.
Folate & CRC/A recurrence.
| Study | Sample size (N) | Dose (MG/DAY) | Duration | Effect on CRA recurrence |
|---|---|---|---|---|
| Greece (1994) (26) | 60 | 1 | 2 years (YR) | No effect |
| AFPPS (2007) (12) | 1021 | 1 | 6 YR | 67% increased risk |
| Detroit VA (2008) (28) | 94 | 5 | 3 YR | 46% decreased risk |
| (UKCAP) (2008) (27) | 853 | 0.5 | 3 YR | No effect |
| (NHS-HPFS) (2009) (22) | 672 | 1 | 3 YR | No effect |
| Ibrahim, Ezzeldin M, and Jamal M Zekri Meta-analysis (2010) (25) | 1580 | 1 | 1-3 YR | No effect |
| Combined Analysis of AFPPS, NHS-HPFS, & UKCAP (2011) (30) | 2632 | 0.5–1 | 6–42 months | No effect |
| Meta-Analysis of AFPPS, NHS-HPFS, & UKCAP (2013) (31) | 2632 | 0.5–1 | 3-6 YR | Increased risk |
| Focus CONSORTIUM (2020) (19) | 2024 | – | a | No effect |
-
-The COLON [34](n = 1094) and EnCoRe [35](n = 297) studies are ongoing prospective cohort studies that recruit newly diagnosed colorectal cancer patients since 2010 and 2012, respectively. (from eleven hospitals in the Netherlands for the COLON study and from three hospitals in the Netherlands for the EnCoRe study).
-
-CORSA [36](n = 209) is an ongoing study since 2003, recruiting colorectal cancer patients in cooperation with the province-wide screening project “Burgenland Prevention Trial of Colorectal Disease with Immunological Testing” (B-PREDICT) using fecal occult blood testing (FOBT).
-
-ColoCare [36] is an ongoing, international, prospective cohort study. Patients were recruited since 2010 at the University Hospital of Heidelberg and the National Center for Tumor Diseases in Heidelberg, Germany(n = 260) (ColoCare HD). ColoCare patients were also recruited since 2015 at Huntsman Cancer Institute(n = 46) (Salt Lake City, U.S.) (ColoCare HCI) and since 2007 at Fred Hutchinson Cancer Research Center(n = 118) (Seattle, U.S.) (ColoCare FHCRC).
4. Conclusion
Our article supports the protective role of folic acid in the absence of tumor foci and its cancerous effect in the presence of such foci; which may explain the different results of folate effect on CRC risk and support the role of anti-folate agents as chemotherapy drugs. However, the role of folate in preventing recurrence and improving survival rates remains unresolved and requires further evidence from clinical trials, with a possible potential role of folate metabolism genotype variations.
Ethical approval
Not applicable. It is a review.
Sources of funding
This article did not receive any funding.
Author contributions
HK: is the mentor, drafted the manuscript.
RD, TS, YS, ZA & JE: collected the data and participated in revising the article.
ZA: is the guarantor and supervisor & critically revised the article.
MG: is the oncologist & participated in revising the article.
Registration of research studies
Not applicable. It's a review.
Guarantor
Dr Zuheir Alshehabi.
Consent
NA.
Declaration of competing interest
No conflict of interest.
Acknowledgement
Not applicable.
Abbreviations
- CRC
Colorectal cancer
- CRA
Colorectal adenoma
- FA
Folic acid
- RCT
Randomized control trial
- 5FU
5-Fluorouracil
References
- 1.Yuan Zhong, Zhu Yan, Li Quanpeng, Wang Fei, Ge Xianxiu, Zhou Guangxin, Lin Miao. Association between Mediterranean diet adherence and colorectal cancer: a dose-response meta-analysis. Am. J. Clin. Nutr. June 2020;111(6):1214–1225. doi: 10.1093/ajcn/nqaa083. [DOI] [PubMed] [Google Scholar]
- 2.Schwingshackl Lukas, et al. Adherence to mediterranean diet and risk of cancer: an updated systematic review and meta-analysis. Nutrients. 2017;9(10):1063. doi: 10.3390/nu9101063. (Crossref. Web) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shaukat Aasma, et al. Role of supplemental calcium in the recurrence of colorectal adenomas: a metaanalysis of randomized controlled trials. Am. J. Gastroenterol. 2005;100(2):390–394. doi: 10.1111/j.1572-0241.2005.41220.x. [DOI] [PubMed] [Google Scholar]
- 4.Kim Y.-I. Folate: a magic bullet or a double edged sword for colorectal cancer prevention? Gut. 2006;55(10):1387–1389. doi: 10.1136/gut.2006.095463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hubner R.A., Houlston R.S. Folate and colorectal cancer prevention. Br. J. Cancer. 2009;100(2):233–239. doi: 10.1038/sj.bjc.6604823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Du Wan, et al. Folate and fiber in the prevention of colorectal cancer: between shadows and the light. World J. Gastroenterol. 2010;16(8):921–926. doi: 10.3748/wjg.v16.i8.921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Van Guelpen B., et al. Low folate levels may protect against colorectal cancer. Gut. 2006;55(10):1461–1466. doi: 10.1136/gut.2005.085480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gylling Björn, et al. Vol. 23. 2014. Low folate levels are associated with reduced risk of colorectal cancer in a population with low folate status; pp. 2136–2144. (Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology). 10. [DOI] [PubMed] [Google Scholar]
- 9.Moazzen Sara, et al. Folic acid intake and folate status and colorectal cancer risk: a systematic review and meta-analysis. Clin. Nutr. 2018;37(6 Pt A):1926–1934. doi: 10.1016/j.clnu.2017.10.010. [DOI] [PubMed] [Google Scholar]
- 10.Qin Tingting, et al. Folic acid supplements and colorectal cancer risk: meta-analysis of randomized controlled trials. Sci. Rep. 1 Jul. 2015;5(12044) doi: 10.1038/srep12044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moazzen Sara, et al. Folic acid supplement intake and risk of colorectal cancer in women; A case control study. Annal Global Health. 27 Feb. 2020;86(1 23) doi: 10.5334/aogh.2664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cole Bernard F., et al. Folic acid for the prevention of colorectal adenomas: a randomized clinical trial. JAMA. 2007;297(21):2351–2359. doi: 10.1001/jama.297.21.2351. [DOI] [PubMed] [Google Scholar]
- 13.Gao Qin-Yan, et al. Folic acid prevents the initial occurrence of sporadic colorectal adenoma in Chinese older than 50 years of age: a randomized clinical trial. Cancer Prev. Res. 2013;6(7):744–752. doi: 10.1158/1940-6207.CAPR-13-0013. [DOI] [PubMed] [Google Scholar]
- 14.Larsson Susanna C., et al. Vol. 14. 2005. A prospective study of dietary folate intake and risk of colorectal cancer: modification by caffeine intake and cigarette smoking; pp. 740–743. (Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology). 3. [DOI] [PubMed] [Google Scholar]
- 15.Nan Hongmei, et al. Prospective study of alcohol consumption and the risk of colorectal cancer before and after folic acid fortification in the United States. Ann. Epidemiol. 2013;23(9):558–563. doi: 10.1016/j.annepidem.2013.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sie Karen K.Y., et al. Effect of maternal and postweaning folic acid supplementation on colorectal cancer risk in the offspring. Gut. 2011;60(12):1687–1694. doi: 10.1136/gut.2011.238782. [DOI] [PubMed] [Google Scholar]
- 17.Brink Mirian, et al. Dietary folate intake and k-ras mutations in sporadic colon and rectal cancer in The Netherlands Cohort Study. Int. J. Cancer. 2005;114(5):824–830. doi: 10.1002/ijc.20775. [DOI] [PubMed] [Google Scholar]
- 18.Ting P.C., Lee W.R., Huo Y.N., Hsu S.P., Lee W.S. Folic acid inhibits colorectal cancer cell migration. J. Nutr. Biochem. 2019 Jan;63:157–164. doi: 10.1016/j.jnutbio.2018.09.020. Epub 2018 Oct 6. PMID: 30393128. [DOI] [PubMed] [Google Scholar]
- 19.Geijsen A.J.M.R., Ulvik A., Gigic B., Kok D.E., van Duijnhoven F.J.B., Holowatyj A.N., Brezina S., van Roekel E.H., Baierl A., Bergmann M.M., Böhm J., Bours M.J.L., Brenner H., Breukink S.O., Bronner M.P., Chang-Claude J., de Wilt J.H.W., Grady W.M., Grünberger T., Gumpenberger T., Herpel E., Hoffmeister M., Huang L.C., Jedrzkiewicz J.D., Keulen E.T.P., Kiblawi R., Kölsch T., Koole J.L., Kosma K., Kouwenhoven E.A., Kruyt F.M., Kvalheim G., Li C.I., Lin T., Ose J., Pickron T.B., Scaife C.L., Schirmacher P., Schneider M.A., Schrotz-King P., Singer M.C., Swanson E.R., van Duijvendijk P., van Halteren H.K., van Zutphen M., Vickers K., Vogelaar F.J., Wesselink E., Habermann N., Ulrich A.B., Ueland P.M., Weijenberg M.P., Gsur A., Ulrich C.M., Kampman E. Circulating folate and folic acid concentrations: associations with colorectal cancer recurrence and survival. JNCI Cancer Spectr. 2020 Jul 7;4(5) doi: 10.1093/jncics/pkaa051. PMID: 33134831; PMCID: PMC7583160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moehler Markus, et al. Comparison of a 48-hour infusion of 5-fluorouracil without folinic acid with 24-hour folinic acid/5-fluorouracil in patients with metastatic colorectal cancer refractory to bolus folinic acid/5-fluorouracil. A prospective cohort study. Chemotherapy. 2003;49(1–2):85. doi: 10.1159/000069778. 9. [DOI] [PubMed] [Google Scholar]
- 21.Mayer Benjamin, et al. Stratified survival analysis after adjuvant chemotherapy of colon cancer reveals a benefit for older patients. Anticancer Res. 2015;35(10):5587–5593. [PubMed] [Google Scholar]
- 22.Wu K., Platz E.A., Willett W.C., Fuchs C.S., Selhub J., Rosner B.A., Hunter D.J., Giovannucci E. A randomized trial on folic acid supplementation and risk of recurrent colorectal adenoma. Am. J. Clin. Nutr. 2009;90(6):1623–1631. doi: 10.3945/ajcn.2009.28319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van Dijk M., Pot G.K. The effects of nutritional interventions on recurrence in survivors of colorectal adenomas and cancer: a systematic review of randomised controlled trials. Eur. J. Clin. Nutr. 2016 May;70(5):566–573. doi: 10.1038/ejcn.2015.210.Epub.2016.Jan.13. PMID: 26757838. [DOI] [PubMed] [Google Scholar]
- 24.Sharma N., Trope B., Lipman T.O. Vitamin supplementation: what the gastroenterologist needs to know. J. Clin. Gastroenterol. 2004 Nov-Dec;38(10):844–854. doi: 10.1097/00004836-200411000-00003. PMID: 15492599. [DOI] [PubMed] [Google Scholar]
- 25.Ibrahim Ezzeldin M., Jamal M Zekri. Folic acid supplementation for the prevention of recurrence of colorectal adenomas: metaanalysis of interventional trials. Med. Oncol. 2010;27(3):915–918. doi: 10.1007/s12032-009-9306-9. [DOI] [PubMed] [Google Scholar]
- 26.Logan Richard F.A., et al. Aspirin and folic acid for the prevention of recurrent colorectal adenomas. Gastroenterology. 2008;134(1):29–38. doi: 10.1053/j.gastro.2007.10.014. [DOI] [PubMed] [Google Scholar]
- 27.Paspatis G.A., Karamanolis D.G. Folate supplementation and adenomatous colonic polyps. Dis. Colon Rectum. 1994;37(12):1340–1341. doi: 10.1007/BF02257810. [DOI] [PubMed] [Google Scholar]
- 28.Jaszewski Richard, et al. Folic acid supplementation inhibits recurrence of colorectal adenomas: a randomized chemoprevention trial. World J. Gastroenterol. 2008;14(28):4492–4498. doi: 10.3748/wjg.14.4492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ding H., Gao Q.Y., Chen H.M., Fang J.Y. People with low serum folate levels have higher risk of colorectal adenoma/advanced colorectal adenoma occurrence and recurrence in China. J. Int. Med. Res. 2016 Aug;44(4):767–778. doi: 10.1177/0300060516650075.Epub.2016.Jun.29. PMID: 27358263; PMCID: PMC5536616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Figueiredo Jane C., et al. Folic acid and prevention of colorectal adenomas: a combined analysis of randomized clinical trials. Int. J. Cancer. 2011;129(1):192–203. doi: 10.1002/ijc.25872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vollset Stein Emil, et al. Effects of folic acid supplementation on overall and site-specific cancer incidence during the randomised trials: meta-analyses of data on 50,000 individuals. Lancet (London, England) 2013;381(9871):1029–1036. doi: 10.1016/S0140-6736(12)62001-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim Y.I. Current status of folic acid supplementation on colorectal cancer prevention. Curr Pharmacol Rep. 2016;2:21–33. doi: 10.1007/s40495-016-0046-1. [DOI] [Google Scholar]
- 33.Hubner Richard A., et al. Vol. 15. 2006. Folate metabolism polymorphisms influence risk of colorectal adenoma recurrence; pp. 1607–1613. (Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology). 9. [DOI] [PubMed] [Google Scholar]
- 34.Winkels, Renate M., et al. The COLON study: colorectal cancer: longitudinal, Observational study on Nutritional and lifestyle factors that may influence colorectal tumour recurrence, survival and quality of life. BMC Cancer. 27 May. 2014;14(374) doi: 10.1186/1471-2407-14-374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.van Roekel, Eline H., et al. Vol. 23. 2014. The applicability of the international classification of functioning, disability, and health to study lifestyle and quality of life of colorectal cancer survivors; pp. 1394–1405. (Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology). 7. [DOI] [PubMed] [Google Scholar]
- 36.Ulrich Cornelia M., et al. Vol. 28. 2019. The ColoCare study: a paradigm of transdisciplinary science in colorectal cancer outcomes; pp. 591–601. (Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology). 3. [DOI] [PMC free article] [PubMed] [Google Scholar]