Abstract
Objectives
This study introduced a three-dimensional (3D) surface-to-surface matching technique to evaluate the mandibular symmetry of teenagers and adults with unilateral second molar scissor bite.
Methods
The targets came from 73 cone-beam computed tomography (CBCT) images with unilateral second molar scissor bite, including teenagers (n = 30) and adults (n = 43). 73 images without scissor bite and matched in sex and age were selected as controls. The scans were developed into 3D mandible models and seven mandibular functional unit models, including condylar process (Co), coronoid process (Cr), mandibular ramus (Ra), mandibular angle (Ma), alveolar process (Ap), mandibular body (Mb) and chin process (Ch). The surface-to-surface matching technique was introduced. 3D deviation analysis and matching percentages calculation were performed and compared to evaluate the symmetry of the mandible.
Results
Comparisons were made between the study samples and control samples. For teenagers, the matching percentages of the entire mandible (55.31 ± 7.24%), Mb (69.04 ± 9.22%) and Co (65.19 ± 10.67%) in the study group were lower than that of the entire mandible (60.87 ± 6.38%) (P <0.01), Mb (75.0 ± 8.71%) (P <0.05) and Co (70.25 ± 8.20%) (P <0.05) in the control group. While Ap, Ra, Ch, Cr and Ma showed no statistically significant differences (P >0.05). For adults, the matching percentages of the entire mandible (48.88 ± 9.77%), Ap (65.83 ± 11.21%), Mb (64.43 ± 12.03%), Ch (79.17 ± 10.29%), Ra (64.11 ± 9.84%) and Co (61.08 ± 11.64%) in the study group were lower than the entire mandible (59.28 ± 5.49%) (P <0.01), Ap (73.65 ± 9.10%) (P <0.01), Mb (71.66 ± 8.40%) (P <0.01), Ch (83.86 ± 5.59%) (P <0.05), Ra (68.54 ± 7.87%) (P <0.05) and Co (66.20 ± 10.62%) (P <0.05) of the control group. Only Cr and Ma showed no statistically significant differences (P >0.05).
Conclusion
Mandibular asymmetry was observed in both teenagers and adults with unilateral second molar scissor bite. Moreover, compared with teenagers, more mandibular units of adult patients were affected.
Clinical significance
Based on the surface-to-surface matching technique, the symmetric and morphological information of the mandible can be converted into visual color maps and quantitative descriptions. This method can bring convenience to the study of the growth of mandible, orthodontic treatment and orthognathic surgery design.
Keywords: Cone-beam computed tomography, Three-dimensional imaging, Second molar, Scissor bite
Highlights
-
•
The surface-to-surface matching technique was introduced to evaluate mandibular symmetry.
-
•
The 3D colored-map can quickly perform visual analysis and objective quantification.
-
•
Seven functional mandibular units were examined to locate asymmetrical anatomical regions.
-
•
Teenagers and adults were analyzed to discuss age differences.
-
•
This method can be applied in various fields like orthodontics, orthognathic, and orthopedics.
Cone-beam computed tomography; Three-Dimensional imaging; Second molar; Scissor bite.
1. Introduction
The morphology and growth of the mandible are very important in the oral and maxillofacial fields. The symmetry of the mandible affects the masticatory function and aesthetics [1]. Therefore, the diagnosis of asymmetries is very vital for orthodontic treatment and orthognathic surgery design. Although two-dimensional (2D) radiography such as lateral cephalograms, posteroanterior cephalograms, and panoramic radiographs have been commonly used in clinical, the magnification errors and disproportional enlargement indeed severely affected the analysis [2]. In practice, the proper diagnosis before treatment is necessary for therapeutic options. Therefore, measurements based on two dimensions which merely measure the point, liner, and angle have limitations in accurate measurement, analysis, and treatment planning [3].
Technologies are encouraged to obtain information and analyze data from three dimensions, to evaluate the tooth, soft tissue, and hard tissue [4, 5, 6]. For example, by means of a 3-dimensional finite element model (3D FEM), the characteristics of tooth movement can be studied [7]. The development of 3D facial image systems has enabled researchers to evaluate aesthetics and proportions of facial soft tissues [8]. As for hard tissue, cone-beam computed tomography (CBCT) has come into wide use in recent years. Exploring scientific methods to accurately assess mandibular symmetries and morphological characteristics in 3D view is in great demand. Unlike 2D radiography, the reconstruction model derived from CBCT allows multiple 3D views to be observed in space instead of a single sagittal view [9, 10]. Moreover, based on the software, the segmentation of the mandible from CBCT can be built into a personalized 3D digital mandible model, which will benefit further evaluation [11]. Admitted that more and more studies applied CBCT and 3D digital models on measurement and diagnosis, lots of them were still based on an old 2D fashion to evaluate “point-to-point” distances rather than “surface-to-surface”, without following the mandibular contour [12].
Scissor bite is a malocclusion characterized by the buccal inclination of the maxillary posterior tooth and/or lingual inclination of the mandibular posterior tooth without occlusal contact. Scissor bite is mainly found in the second molar. Unilateral scissors bite was likely to be related to many oral craniofacial problems [13]. In clinical, patients with unilateral scissor bite always choose to use the unaffected side. And unilateral scissor bite was reported to be associated with disordered chewing patterns and occlusal interference. The decayed tooth, tooth elongation, and bad periodontal condition can be observed in the scissor bite side [14]. In addition, the scissor bite can cause a long-term blockage of the bite, which hinders the growth of the mandible. Elongated tooth tips may also cause ulcers and mucosal lesions [15]. Therefore, learning more about unilateral scissor bite does make sense in clinics. However, there were relatively fewer reports about the association between unilateral second molar scissor bite and mandibular symmetry. In addition, few reports compared the difference between teenagers and adults.
The purpose of this study was to introduce the 3D surface-to-surface matching technique to evaluate the mandibular symmetry of patients with unilateral second molar scissor bite. Furthermore, following this methodology, the present study also aimed to compare the morphological characteristics of the mandibles in teenagers and adults.
2. Material and methods
2.1. Study population
This retrospective study was carried out on pretreatment CBCTs. The operating parameters in CBCT (Newtom Vgi, Italy) scanning were set to 90.0 kV and 9 mA, the scanning time was 24 s, and the voxel size was 0.3mm. The subjects were consecutively collected from patients who attended the Hospital of Stomatology, Guanghua School of Stomatology, Sun Yat-sen University between 2014 to 2021. The study was conducted according to ethical standards defined by the Helsinki Declaration of 1964, including subsequent amendments or comparable ethical standards. And the ethical approval was obtained from the ethics committee of the Affiliated Stomatology Hospital of Sun Yat-sen University, Guangzhou, China (Approval No. KQEC-2021-41-02). All patients provided written informed consent to participate. All subjects selected in this experiment have been de-identified to protect patient privacy.
A power analysis was carried out to evaluate the sample size for this research [10]. According to a preliminary pilot study, a mean difference of 5.9% and standard deviation of 7.9% were used as outcomes to perform the power analysis calculation. The analysis indicated that a simple size of 28 patients was required to get a power of 80% for a two-side significance level of 5%.
According to the following inclusion criteria and exclusion criteria, the CBCT of study group consisted of 30 teenagers and 43 adults with unilateral second molar scissor bite. Age and gender matched-paired samples were served as teenager control group (n = 30) and adult control group (n = 43). Characteristics of the samples are shown in Table 1. The inclusion criteria are listed as follows: (1) Unilateral second molar scissor bite; (2) No distortion or artifacts in CBCT images. The exclusion criteria were: (1) Systemic disease; (2) Oral and maxillofacial trauma; (3) Oral and maxillofacial anomalies; (4) Previous oral and maxillofacial surgery; (5) Crossbite: mandibular teeth occluded buccally to their antagonists; (6) Dentition defect. The overall process of the study is shown in Figure 1. All measurements were taken by the same specialized operator (YX).
Table 1.
Characteristics of the samples.
| teenagers (n = 30) |
adults (n = 43) |
|||
|---|---|---|---|---|
| study group | control group | study group | control group | |
| N | 30 | 30 | 43 | 43 |
| Gender (Male/Female) | 14/16 | 14/16 | 16/27 | 16/27 |
| Age (year) | 13.57 ± 1.33 | 13.27 ± 1.64 | 25.53 ± 5.35 | 25.70 ± 4.92 |
Figure 1.
The flow chart of the research.
2.2. Original mandible model and mirrored mandible model
The obtained CBCT data was converted into Digital Imaging and Communications in Medicine (DICOM) format (Figure 2a). Then the CBCT data were imported into Mimics version 20.0 (Materialize NV, Liege, Belgium) to develop the initial segmentation mask (Figure 2b). The Edit Mask tool was used to develop the mandible region (Figure 2c). After enhancement of boundaries by erasing unnecessary information and adjusting the visualization of the segmentation mask, the original mandible part was calculated (Figure 2d). Then the original mandible model was mirrored, to obtain the mirrored mandible model (Figure 2e). After that, the two models were exported (.stl).
Figure 2.
(a) CBCT data was imported to the Mimics software. (b) The initial segmentation mask. (c) The mandible part was calculated. (d) The original mandible model was developed. (e) The mirrored mandible model was developed. (f) Best Fit Alignment.
2.3. Alignment
The models obtained from last step were imported to Geomagic Control X software (version 2018.1.1, 3D Systems, Santa Clara, CA 95054, USA). In this software, the original mandible model was set as the reference data and the mirrored mandible model was set as the test data. Then the “Initial Alignment” tool was used for the initial overlay. After that, the “Best Fit Alignment” function was used for the final superimposition (Figure 2f). The registration accuracy was set to at least 0.1 mm, and the surface registration percentage was set to a maximum of 100% [16].
2.4. 3D deviation analysis of the mandible
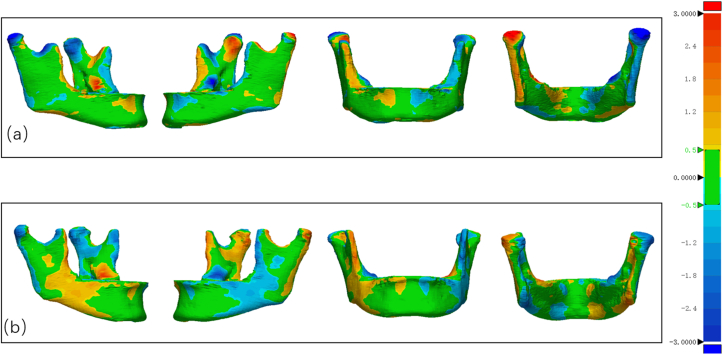
The distances between the original mandible model and the corresponding mirrored mandible model area were displayed in the form of color-coded maps, as shown in Figure 3. 3D Comparison” tool was used for the 3D deviation analysis. The color green was defined as within tolerance (set to ±0.50 mm). When the distance difference was greater than +0.5mm, the color changed from yellow to red. When the distance difference was less than -0.5mm, the color changed from light blue to dark blue. Darker color represented further distance between the corresponding areas of the two models [16, 17]. The percentage of the distance between the two models within the tolerance range was defined as the matching percentage (%). The lower matching percentage represented a more significant asymmetry of the mandible.
Figure 3.
3D Surface deviation analysis of mandibles. (a) teenager study group. (b) adult study group.
2.5. 3D deviation analysis of mandibular functional units
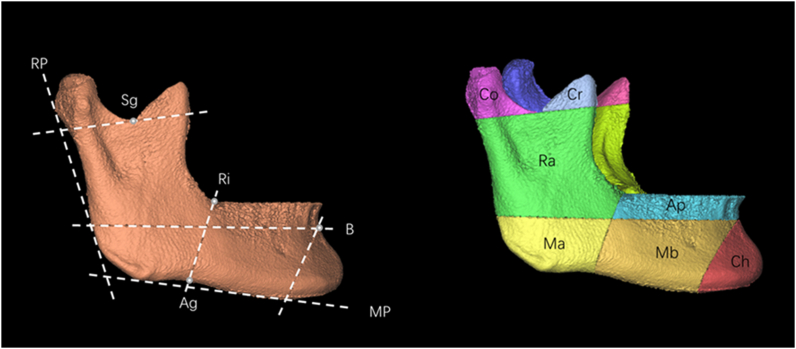
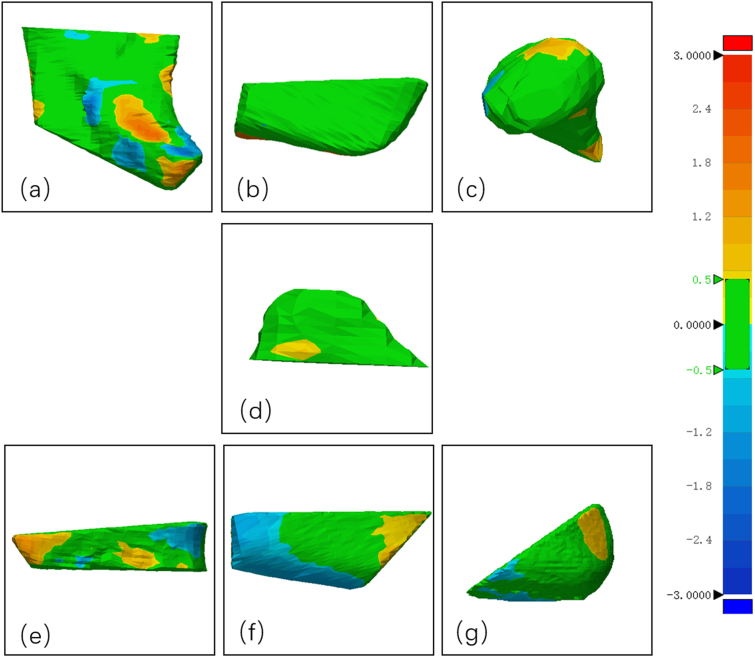
As the functional matrix theory revealed, mandible development was associated with the independent growth of mandibular functional units. According to the landmarks (Table 2), the mandible was constructed to the mandibular functional units (alveolar process, mandibular body, condylar process, chin, coronoid process, mandibular ramus, and mandibular angle) (Figure 4). The mandibular units models were mirrored to obtain the mirrored models. After that, initial alignment and best-fit alignment were used. Same to the above method, the tolerance range of the deviation analysis was set to 0.50 mm, and the color changed with the distance. When the distance difference was within ±0.50 mm, the color was green. When the distance was greater than +0.5mm, the color changed from yellow to red. When the distance difference was less than -0.5mm, the color changed from light blue to dark blue (Figure 5). After that, the matching percentages of each mandibular unit were calculated.
Table 2.
The landmarks to delimitate the mandible.
| Landmark | Definition |
|---|---|
| Sg | Deepest point on the sigmoid notch |
| B | Supramental, the most concave point on mandibular symphysis |
| Ri | Ramus inflexion, the transition between the front edge of mandibular ramus and the mandibular body |
| Ag | Antegonion, the most concave point of the anterior notch of the mandibular angle |
| MP | Mandibular plane, tangent to the lower edge of the mandible |
| RP | Ramal plane, tangent to the condylar process and mandibular ramus |
Figure 4.
Mandibular functional units construction. Co, condylar process; Cr, coronoid process; Ra, mandibular ramus; Ma, mandibular angle; Ap, alveolar process; Mb, mandibular body; Ch, chin process.
Figure 5.
3D Surface deviation analysis of mandibular functional units. Co, condylar process; Cr, coronoid process; Ra, mandibular ramus; Ma, mandibular angle; Ap, alveolar process; Mb, mandibular body; Ch, chin process.
2.6. Statistical analysis
The data from study groups and control groups were conducted the descriptive statistical analysis. Microsoft Excel (2016, Microsoft, Redmond, Wash) was used to record the measurement results. SPSS (version 25.0; IBM, Armon, NY) was used for statistical analysis. The whole mandible and mandibular functional units (alveolar process, mandibular body, condylar process, chin, coronoid process, mandibular ramus, and mandibular angle) were compared between the study and control groups. In this study, Shapiro–Wilk test was used to test the normality of the data. The data of mandible, condylar process, alveolar process and mandibular body were normally distributed; so, the independent t-test was conducted for them. The data of mandibular ramus, mandibular angle, coronoid process and chin were not normally distributed; therefore, the Mann-Whitney U test was used for them. In order to assess the methodological error, measurements were repeated for ten randomly selected CBCT images 8 weeks after the first examination by the same specialized operator. The intraclass correlation coefficient (ICC) was used to assess the consistency and reproducibility. The magnitude of the random error was assessed using the Dahlberg formula [18, 19] (D = , where di is the difference between the first and the second measurement, and N is the sample size which was re-measured). The measurements were considered highly reliable. The intraclass correlation coefficient value was 0.945 (95% CI, 0.915–0.964). The random error ranged from 0.9% to 4.2%. P values less than 0.05 were considered statistically significant.
3. Results
The matching percentages of the mandibles were recorded in Table 3. Firstly, study groups and control groups were compared. As for teenagers, the mandible matching percentage of the study group (55.31 ± 7.24%) was lower than that of the control group (60.87 ± 6.38%) (P <0.01). For adults, the matching percentage of the study group (48.88 ± 9.77%) was also lower than that of the control group (59.28 ± 5.49%) (P <0.01). What is more, compared with that of the teenager study group, lower matching percentages of the adult study group were found (P < 0.05). However, there was no difference between the teenager control group and the adult control group (P >0.05).
Table 3.
Mandible matching percentage of the study group and control group.
| Total | Matching percentages (mean; %) | SD | Significance | ||
|---|---|---|---|---|---|
| Teenagers | study group | 30 | 55.31 | 7.24 | ∗∗ |
| control group | 30 | 60.87 | 6.38 | ||
| Adults | study group | 43 | 48.88 | 9.77 | ∗∗ |
| control group | 43 | 59.28 | 5.49 | ||
The results were normally distributed. P values were based on the independent t-test. The level of significance was set at 0.05. ∗∗ = p <0.01.
According to the 3D color maps, it was revealed that some mandibular anatomic areas appeared more remarkable asymmetrical morphology. The mandible was divided into seven mandibular functional units, including the alveolar process, mandibular body, condylar process, chin, coronoid process, mandibular ramus, and mandibular angle. Matching percentages of the mandibular functional units were calculated and compared (Figure 6). For the teenagers, the matching percentages of the mandibular body (69.04 ± 9.22%) (P<0.05) and condylar process (65.19 ± 10.67%) (P <0.05) of the study group were lower than the control samples. No statistically significant difference was found at other units, including the alveolar process, chin, coronoid process, mandibular ramus, and mandibular angle (P >0.05). However, in the adult study group, the results highlighted that more areas were suffered, and more significant mismatches mainly localized at the alveolar process (65.83 ± 11.21%), mandibular body (64.43 ± 12.03%), chin units (79.17 ± 10.29%), mandibular ramus (64.11 ± 9.84%) and condylar process (61.08 ± 11.64%) (P <0.05). No significance was found in the coronoid process and mandibular angle (P >0.05).
Figure 6.
Matching percentages of the mandibular functional units. The level of significance was set at 0.05. ∗ = p <0.05; ∗∗ = p <0.01.
4. Discussion
In our study, the surface-to-surface matching technique was introduced to evaluate the symmetry and morphology of the mandible with unilateral second molar scissor bite. According to the results, unilateral second molar scissors bite was found associated with mandibular asymmetry. Moreover, both teenagers and adults can be affected. In particular, asymmetry was more frequently observed in adults, especially at the alveolar process, mandibular body, chin units, mandibular ramus, and condylar process. However, teenagers with unilateral second molar scissor bite appeared to affect less asymmetric mandibular units than adults. Only the mandibular body unit and condylar process were affected.
Nowadays, the emerging sophisticated engineering software provides new opportunities to comprehensively evaluate craniofacial anatomical characteristics and morphological changes. The “surface-to-surface” mapping method is used to evaluate the distances between the two model surfaces [20]. The distance length is displayed in different colors and formed in a 3D color map to analyze the morphological difference visually [16]. What is more, the mirroring method provides an important method for analyzing craniofacial asymmetry. Via comparing the original model and mirrored model, the difference between the left and right can be evaluated [21]. Quantitative analysis can be performed by best fit alignment and calculating the matching percentage [22]. The information obtained via this new measurement method can facilitate comprehensive diagnosis and treatment planning.
Studies have shown the association between mandibular muscle contraction and malocclusion. Masticatory muscle strength was necessary for the growth and development of the mandible [23, 24]. A scissor bite in the area of the second molars is often a therapy-resistant problem in everyday clinical practice [25]. The position of the second molar is very close to the attachment area of the masticatory muscles. As a result, its buccal and lingual structures seem to be influenced by masticatory. A previous study found that patients with unilateral scissor bite preferred to use the normal side to exercise their chewing function. This experiment then evaluated the mandibular movement, masseter, and temporal muscle activities during mastication. The abnormal mandibular movement mode was exhibited during the mastication process. The mastication pattern on the scissor bite side was narrower, the closing time was longer, the closing speed was slower, and the masseter and temporal muscle activity were lower [26]. The change in muscle function is an essential factor influencing the growth and development of craniofacial bones remodeling. Moss [27] proposed the theory of functional units. The mandible can be divided into different units, and each unit will be affected by the surrounding functional matrix. The development of the entire mandible resulted from the joint growth and development of these functional units. Moreover, these skeletal units were affected by the surrounding tissues and muscular structures attached to them [28]. The muscle fibers and the force generated during muscle movement can be transmitted to the bones [24]. A better understanding of the relationship between craniofacial deformities and muscles will help clinical diagnosis and treatment [23]. One study has found that unilateral atrophy of the masseter muscle affected the local morphology of the bones. In the experiment, botulinum toxin A (BTXA) was injected into a specific site to induce muscle function decline, and bone changes were observed, thereby discovering the interaction between masticatory muscles and craniofacial bones [29]. Mandibular remodeling was a complex process. Many of the mechanisms have not yet been fully elucidated. But what can be observed was that the biomechanical response of the “functional matrix” of surrounding tissues can indeed affect bones. In addition, changes in bone remodeling during development were also manifestations of adaptive functional activities [27, 30].
Although scissor bite adversely affects facial symmetry, mastication, and mandible growth, it is usually unnoticed by patients [31]. As mentioned above, various factors can lead to scissor bite malocclusion. And in turn, malocclusion can also have a series of effects on the mandible growth, masticatory system, and joints. Unilateral scissor bite is not self-correcting, and according to an investigation about the worldwide prevalence of dental malocclusion, scissor bite increase from primary to permanent dentition [32]. Besides, mandibular asymmetry correlated to mandibular body length and mandibular rotation [33]. The continuous periosteal ossification with bone resorption led to bone remodeling [34]. Therefore, it was supposed that if the unilateral second molar scissor bite remains untreated for years, the mandible's asymmetry will worsen as time goes on. When the scissor bite persists, the posterior teeth of the lower jaw will be subjected to the force of the lingual tilt, and the posterior teeth of the upper jaw will elongate in the vertical direction. If this situation continues in this way, the alveolar bone may be severely affected, resulting in skeletal compensation, and leading to inclined occlusal surfaces and asymmetric mandibular growth [15]. Muscles express different sarcomeric proteins that determine different contractile properties. These may vary with age and activity patterns. Muscle plasticity impacts pathology and physiology [35]. Therefore, correcting the scissor bite at a young age makes sense.
The challenges of correcting a scissor bite include the buccal tilt of the maxillary molars and the lingual tilt of the mandibular molars. For the early treatment of young patients, when the inclination of the dentition mainly manifests the scissor bite side, and there is no apparent vertical growth of the maxillary alveolar bone, fixed and detachable appliances can be selected for treatment. Nojima et al. reported a case concerning correcting a patient with a scissor bite. The patient was a child with mixed dentition. By bonding and shrinking the quad-helix appliance on the upper jaw, the bite was opened, and the width of the upper jaw arch was reduced, independent of the child's cooperation [36]. Shyagali used TAS appliance (T-Tarulatha, A-Akashdeep, and S-Shyagali) for the correction of expanded maxillary arch and the scissor bite [37].
For adult patients with scissor bite, the main challenges lie in protecting the anchorage during the treatment of tilted dentition and alveolar bone deformities. Micro-screws have been widely used in the field of orthodontics in recent years. They play an important role by being implanted in the bones as anchors [38]. Wang et al. used micro-screws combined with traditional sliding MBT™ straight wire technology to achieve vertical control. Wang et al. treated a patient with high-angle bone type II malocclusion with a scissor bite. Micro-screws were placed in the anterior and posterior segments of the upper jaw. This method reduced deep overbite, corrected the scissor bite, and helped the mandibular plane's counterclockwise rotation, thereby improving facial profile [39]. For severe scissor bite, multiple teeth are involved. Especially in older patients, the vertical growth of the upper alveolar bone collapsed mandibular arch, and a significant degree of overlap of the upper and lower teeth are more likely to appear. Simply using orthodontic appliances or anchored micro-implants will be challenging to correct severe scissor bite. For such severe cases of bone asymmetry, a combination of orthodontics and orthognathic surgery can be a better treatment option [40, 41].
The surface-to-surface matching technique was considered as a user-friendly tool. Via this methodology, the symmetry and morphology information can be converted into maps with different colors. This method may be applied in daily practice, bringing convenience to the clinical diagnosis and treatment. This study mainly focused on the characteristics of the mandible with unilateral second molar scissor bite before treatment. The after-treatment cases have not been evaluated. If these patients can be followed up for further longitudinal researches in the future, it will be helpful to study the effect of orthodontic interventions. In addition, surface-to-surface matching techniques are expected to find wider application in other medical fields, such as computer-aided orthognathic surgery design and orthopedics.
5. Conclusion
Unilateral second molar scissors bite was associated with mandibular asymmetry, and both teenagers and adults can be affected. However, adults with unilateral second molar scissor bite appeared to affect more asymmetric mandibular units than teenagers. Adults presented more asymmetric alveolar, mandibular body, condylar process, mandibular ramus, and chin units. The coronoid process and mandibular angle showed no significance compared with the adult control group. Teenagers with unilateral second molar scissor bite showed much less asymmetry. The mandibular body and condylar process played a more dominant role in the asymmetry of the mandible than the alveolar process, chin units, mandibular ramus, coronoid process, and mandibular angle.
Declarations
Author contribution statement
Yajuan Xie: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
Runling Zeng: Performed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Jiayin Yan: Conceived and designed the experiments; Performed the experiments; Wrote the paper.
Tong Yan: Analyzed and interpreted the data; Wrote the paper.
Jiali Tan: Conceived and designed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
This work was supported by the Guangdong Basic and Applied Basic Research Foundation (2022A1515011094), Guangdong Financial Fund for High-Caliber Hospital Construction (174-2018-XMZC-0001-03-0125/C-05), Science and Technology Planning Project of Guangdong Province, China (2020A0505100034), and Undergraduate Education Quality Program of Sun Yat-Sen University (Academic Affairs [2022] No. 20).
Data availability statement
Data will be made available on request.
Declaration of interest’s statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper
Acknowledgements
We appreciate the support from the participants. In addition, we are grateful to Professor Yu Han for reviewing and editing our paper.
References
- 1.Lipowicz A., Wolanski W., Kawlewska E., Zwolska P., Kulesa-Mrowiecka M., Dowgierd K., Linek P., Mysliwiec A. Evaluation of mandibular growth and symmetry in child with congenital zygomatic-coronoid ankylosis. Symmetry (Basel). 2021;13 [Google Scholar]
- 2.You K.-H., Kim K.-H., Lee K.-J., Baik H.-S. Three-dimensional computed tomography analysis of mandibular morphology in patients with facial asymmetry and mandibular retrognathism. Am. J. Orthod. Dentofacial Orthop. 2018;153:685–691. doi: 10.1016/j.ajodo.2017.08.024. [DOI] [PubMed] [Google Scholar]
- 3.Fan W., Gao D., Wang Y., Chen Y., Li Y., Lu S., Wang Z. Three-dimensional measurement and analysis of mandibular characteristics in subjects with impacted mandibular second molars. Orthod. Craniofac. Res. 2020;23:332–341. doi: 10.1111/ocr.12375. [DOI] [PubMed] [Google Scholar]
- 4.Kazemipoor M., Valizadeh F., Jambarsang S. Three-dimensional pattern of inflammatory periapical lesion extension in the premolar's region: an application of K-means clustering. Curr Med Imaging. 2021;17:1151–1158. doi: 10.2174/1573405617666210225090213. [DOI] [PubMed] [Google Scholar]
- 5.Li C., Lin L., Zheng Z., Chung C.-H. A user-friendly protocol for mandibular segmentation of CBCT images for superimposition and internal structure analysis. J. Clin. Med. 2021;10:127. doi: 10.3390/jcm10010127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.d’Apuzzo F., Minervini G., Grassia V., Rotolo R.P., Perillo L., Nucci L. Mandibular coronoid process hypertrophy: diagnosis and 20-year follow-up with CBCT, MRI and EMG evaluations. Appl. Sci. 2021;11:4504. [Google Scholar]
- 7.Cozzani M., Sadri D., Nucci L., Jamilian P., Pirhadirad A.P., Jamilian A. The effect of Alexander, Gianelly, Roth, and MBT bracket systems on anterior retraction: a 3-dimensional finite element study. Clin. Oral Invest. 2020;24:1351–1357. doi: 10.1007/s00784-019-03016-6. [DOI] [PubMed] [Google Scholar]
- 8.Celebi A.A., Kau C.H., Femiano F., Bucci L., Perillo L. A three-dimensional anthropometric evaluation of facial morphology. J. Craniofac. Surg. 2018;29 doi: 10.1097/SCS.0000000000004110. [DOI] [PubMed] [Google Scholar]
- 9.Srinivasan S., Tee B.C., Wang A., Gohel A., Kim D.-G., Deguchi T., Sun Z. Reliability and accuracy of assessing temporary anchorage device-tooth root contact with cone-beam computed tomography. Am. J. Orthod. Dentofacial Orthop. 2021;159:271–280. doi: 10.1016/j.ajodo.2020.01.020. [DOI] [PubMed] [Google Scholar]
- 10.Dekel E., Nucci L., Weill T., Flores-Mir C., Becker A., Perillo L., Chaushu S. Impaction of maxillary canines and its effect on the position of adjacent teeth and canine development: a cone-beam computed tomography study. Am. J. Orthod. Dentofacial Orthop. 2021;159:e135–e147. doi: 10.1016/j.ajodo.2020.10.015. [DOI] [PubMed] [Google Scholar]
- 11.Qiu B., van der Wel H., Kraeima J., Glas H.H., Guo J., Borra R.J.H., Witjes M.J.H., van Ooijen P.M.A. Mandible segmentation of dental CBCT scans affected by metal artifacts using coarse-to-fine learning model. J. Personalized Med. 2021;11 doi: 10.3390/jpm11060560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Evangelista K., Valladares-Neto J., Garcia Silva M.A., Soares Cevidanes L.H., de Oliveira Ruellas A.C. Three-dimensional assessment of mandibular asymmetry in skeletal Class I and unilateral crossbite malocclusion in 3 different age groups. Am. J. Orthod. Dentofacial Orthop. 2020;158:209–220. doi: 10.1016/j.ajodo.2019.08.010. [DOI] [PubMed] [Google Scholar]
- 13.Baik U.-B., Kim Y., Sugawara J., Hong C., Park J.H. Correcting severe scissor bite in an adult. Am. J. Orthod. Dentofacial Orthop. 2019;156:113–124. doi: 10.1016/j.ajodo.2017.11.047. [DOI] [PubMed] [Google Scholar]
- 14.Shimazaki K., Otsubo K., Yonemitsu I., Kimizuka S., Omura S., Ono T. Severe unilateral scissor bite and bimaxillary protrusion treated by horseshoe Le Fort I osteotomy combined with mid-alveolar osteotomy. Angle Orthod. 2014;84:374–379. doi: 10.2319/050513-344.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deffrennes G., Deffrennes D. Management of Brodie bite: note on surgical treatment. Int. Orthod. 2017;15:640–676. doi: 10.1016/j.ortho.2017.09.023. [DOI] [PubMed] [Google Scholar]
- 16.Leonardi R., Lo Giudice A., Rugeri M., Muraglie S., Cordasco G., Barbato E. Three-dimensional evaluation on digital casts of maxillary palatal size and morphology in patients with functional posterior crossbite. Eur. J. Orthod. 2018;40:556–562. doi: 10.1093/ejo/cjx103. [DOI] [PubMed] [Google Scholar]
- 17.Méndez-Manjón I., Guijarro-Martínez R., Valls-Ontañón A., Hernández-Alfaro F. Early changes in condylar position after mandibular advancement: a three-dimensional analysis. Int. J. Oral Maxillofac. Surg. 2016;45:787–792. doi: 10.1016/j.ijom.2016.01.002. [DOI] [PubMed] [Google Scholar]
- 18.Galvão M., Sato J., Coelho E. Dahlberg formula: a novel approach for its evaluation. Dental Press Journal of Orthodontics. 2012;17:115–124. [Google Scholar]
- 19.Leonardi R., Muraglie S., Crimi S., Pirroni M., Musumeci G., Perrotta R. Morphology of palatally displaced canines and adjacent teeth, a 3-D evaluation from cone-beam computed tomographic images. BMC Oral Health. 2018;18:156. doi: 10.1186/s12903-018-0617-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lo Giudice A., Ronsivalle V., Grippaudo C., Lucchese A., Muraglie S., Lagravère M.O., Isola G. One step before 3D printing-evaluation of imaging software accuracy for 3-dimensional analysis of the mandible: a comparative study using a surface-to-surface matching technique. Materials. 2020;13:2798. doi: 10.3390/ma13122798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Muraglie S., Leonardi R., Aboulazm K., Stumpo C., Loreto C., Grippaudo C. Evaluation of structural skeletal asymmetry of the glenoid fossa in adult patients with unilateral posterior crossbite using surface-to-surface matching on CBCT images. Angle Orthod. 2020;90:376–382. doi: 10.2319/061819-415.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gkantidis N., Schauseil M., Pazera P., Zorkun B., Katsaros C., Ludwig B. Evaluation of 3-dimensional superimposition techniques on various skeletal structures of the head using surface models. PLoS One. 2015;10 doi: 10.1371/journal.pone.0118810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Raoul G., Rowlerson A., Sciote J., Codaccioni E., Stevens L., Maurage C.A., Duhamel A., Ferri J. Masseter myosin heavy chain composition varies with mandibular asymmetry. J. Craniofac. Surg. 2011;22:1093–1098. doi: 10.1097/SCS.0b013e3182107766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sciote J.J., Raoul G., Ferri J., Close J., Horton M.J., Rowlerson A. Masseter function and skeletal malocclusion. Rev Stomatol Chir Maxillofac Chir Orale. 2013;114:79–85. doi: 10.1016/j.revsto.2013.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bertl M.H., Astl E. Digital workflow for manufacturing a modified transpalatal arch for scissor bite correction. Informationen Aus Orthodontie Und Kieferorthopaedie. 2021;53:285–290. [Google Scholar]
- 26.Tomonari H., Kubota T., Yagi T., Kuninori T., Kitashima F., Uehara S., Miyawaki S. Posterior scissors-bite: masticatory jaw movement and muscle activity. J. Oral Rehabil. 2014;41:257–265. doi: 10.1111/joor.12148. [DOI] [PubMed] [Google Scholar]
- 27.Moss M.L., Rankow R.M. The role of the functional matrix in mandibular growth. Angle Orthod. 1968;38:95–103. doi: 10.1043/0003-3219(1968)038<0095:TROTFM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 28.Kim B.C., Bertin H., Kim H.J., Kang S.H., Mercier J., Perrin J.P., Corre P., Lee S.H. Structural comparison of hemifacial microsomia mandible in different age groups by three-dimensional skeletal unit analysis. J. Cranio-Maxillo-Fac. Surg. 2018;46:1875–1882. doi: 10.1016/j.jcms.2018.08.009. [DOI] [PubMed] [Google Scholar]
- 29.Kwon T.G., Park H.S., Lee S.H., Park I.S., An C.H. Influence of unilateral masseter muscle atrophy on craniofacial morphology in growing rabbits. J. Oral Maxillofac. Surg. 2007;65:1530–1537. doi: 10.1016/j.joms.2006.10.059. [DOI] [PubMed] [Google Scholar]
- 30.Smartt J.M., Jr., Low D.W., Bartlett S.P. The pediatric mandible: I. A primer on growth and development. Plast. Reconstr. Surg. 2005;116:14e–23e. doi: 10.1097/01.prs.0000169940.69315.9c. [DOI] [PubMed] [Google Scholar]
- 31.Baik U.B., Kim Y., Sugawara J., Hong C., Park J.H. Correcting severe scissor bite in an adult. Am. J. Orthod. Dentofacial Orthop. 2019;156:113–124. doi: 10.1016/j.ajodo.2017.11.047. [DOI] [PubMed] [Google Scholar]
- 32.Lombardo G., Vena F., Negri P., Pagano S., Barilotti C., Paglia L., Colombo S., Orso M., Cianetti S. Worldwide prevalence of malocclusion in the different stages of dentition: a systematic review and meta-analysis. Eur. J. Paediatr. Dent. 2020;21:115–122. doi: 10.23804/ejpd.2020.21.02.05. [DOI] [PubMed] [Google Scholar]
- 33.Evangelista K., Valladares-Neto J., Garcia Silva M.A., Soares Cevidanes L.H., de Oliveira Ruellas A.C. Three-dimensional assessment of mandibular asymmetry in skeletal Class I and unilateral crossbite malocclusion in 3 different age groups. Am. J. Orthod. Dentofacial Orthop. 2020;158:209–220. doi: 10.1016/j.ajodo.2019.08.010. [DOI] [PubMed] [Google Scholar]
- 34.Maspero C., Farronato M., Bellincioni F., Cavagnetto D., Abate A. Assessing mandibular body changes in growing subjects: a comparison of CBCT and reconstructed lateral cephalogram measurements. Sci. Rep. 2020;10 doi: 10.1038/s41598-020-68562-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gries K.J., Zysik V.S., Jobe T.K., Griffin N., Leeds B.P., Lowery J.W. Muscle-derived factors influencing bone metabolism. Semin. Cell Dev. Biol. 2022;123:57–63. doi: 10.1016/j.semcdb.2021.10.009. [DOI] [PubMed] [Google Scholar]
- 36.Nojima K., Takaku S., Murase C., Nishii Y., Sueishi K. A case report of bilateral brodie bite in early mixed dentition using bonded constriction quad-helix appliance. Bull. Tokyo Dent. Coll. 2011;52:39–46. doi: 10.2209/tdcpublication.52.39. [DOI] [PubMed] [Google Scholar]
- 37.Shyagali T.R., Bal A.S. A Novel appliance for the correction of scissor bite. International Journal of Orthodontic Rehabilitation. 2020;11:199–202. [Google Scholar]
- 38.Nakamura M., Kawanabe N., Adachi R., Yamashiro T., Kamioka H. Nonsurgical orthodontic treatment of a hypodivergent adult patient with bilateral posterior scissors bite and excessive overjet. Angle Orthod. 2019;89:333–349. doi: 10.2319/111617-791.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang X.D., Zhang J.N., Liu D.W., Lei F.F., Zhou Y.H. Nonsurgical correction of a severe anterior deep overbite accompanied by a gummy smile and posterior scissor bite using a miniscrew-assisted straight-wire technique in an adult high-angle case. Korean J Orthod. 2016;46:253–265. doi: 10.4041/kjod.2016.46.4.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim K.A., Yu J.J., Chen Y., Kim S.J., Kim S.H., Nelson G. Surgery versus nonsurgery option for scissors bite treatment. J. Craniofac. Surg. 2015;26:e726–729. doi: 10.1097/SCS.0000000000002227. [DOI] [PubMed] [Google Scholar]
- 41.Ratna P., Srinivasan B., Devaki Vijayalakshmi R., Ravanth Kumar C. Surgical correction of brodie bite in adults: a novel surgical splint. J Maxillofac Oral Surg. 2017;16:263–266. doi: 10.1007/s12663-016-0969-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.