Abstract
Purpose
Integration of smartphones has overcome barriers in traditional education; this trial aimed at exploring this ubiquitous platform in oral health education. A smartphone application promoting preschooler’s oral health was designed and its effectiveness was compared with that of common oral health education delivered in paediatric dental settings.
Methods
This controlled clinical trial was performed on preschooler–mother dyads referring to the clinic of Tehran School of Dentistry in 2019–2020. Initially, the dyads were randomly partitioned to application intervention or common training groups. The mothers answered an interviewer-administered questionnaire on paediatric dentistry knowledge, attitude and practice regarding children’s oral health; modified plaque index (m-PI) and modified gingival index (m-GI) of children were measured. Subsequently, the smartphone application was installed for application intervention group and an educational pamphlet and verbal explanations were given to common training group. In 1-month and 3-month follow-ups, the questionnaires and clinical measurement were re-done. A generalized estimating equation (GEE) was used to investigate the effect of training methods.
Results
Among the participants 51 dyad attended baseline and follow-up assessments. The preschoolers mean age was 4.6 ± 1.2 years and 54.4% were girls. Both trainings improved mothers’ knowledge and practice regarding children’s oral health and reduced children’s m-PI and m-GI (p < 0.050). The 3-month follow-up revealed a better m-GI in application intervention group (p < 0.001).
Conclusions
Considering the greater improvement of paediatric gingival status in the application intervention group, it appears that smartphone applications may provide a promising tool for more prolonged impacts in children oral health care.
Trial registration
IRCT, IRCT20131102015238N3. Registered 28 July 2019 https://en.irct.ir/trial/40933
Supplementary Information
The online version contains supplementary material available at 10.1007/s40368-022-00731-9.
Keywords: Smartphone, Application, Mother, Oral health, Preschooler
Introduction
Mobile health (mHealth) apps promote healthy lifestyles by enabling people to better manage their healthcare and well-being, and to access relevant information at any time and place (Baheti and Toshniwal 2014; Underwood et al. 2015). These apps are being developed as a tool in prevention, diagnosis, data collection, monitoring treatment adherence and disease monitoring, especially in patient-centred care (Iribarren et al. 2016; Estai et al. 2017). They have been successful in providing health promotion interventions to patients with chronic diseases and conditions, such as diabetes, asthma, pain and in-patient education and awareness (Underwood et al. 2015; Tiffany et al. 2018), as well as in medication adherence (Elangovan and Arulchelvan 2013).
Mobile phones can help overcome limitations, such as geographical constraints and privacy loss, in traditional interventions (Elangovan and Arulchelvan 2013). Considering their popularity and development, mobile phones are also an appropriate platform for improving health outcomes (Iribarren et al. 2016). Specially the recent wider use of smartphones and high-speed Internet access help patients monitor their health status by themselves or by remote contact with healthcare providers (Kumar et al. 2016).
Over the past few years, the number of available health-related applications has increased by more than twice. Approximately, 40,000 mHealth apps were identified in 2013, reaching 165,000 apps in 2015 (Iribarren et al. 2016) and 325,000 apps in 2017, while about 29% of those have downloaded an application report downloading a health-related app (Tiffany et al. 2018).
Similar to other health fields, smartphones have sparked new opportunities in development of oral health interventions (Scheerman et al. 2018), and previously recognised principal limitations of mHealth in dentistry, such as poor quality of phone cameras, limited storage space and data transfer failure (Estai et al. 2017), are gradually getting resolved in new generations of smartphones. Electronic interventions are an alternative to traditional methods of disseminating oral health information to child caregivers (Albert et al. 2014). Results of a systematic review in 2018 showed that mHealth, as an adjunct, can be effective in improving daily oral hygiene (Toniazzo et al. 2019).
Early childhood caries (ECC) is the most common chronic disease in early childhood and is considered a principal problem in both developing and developed countries. Its prevalence is about 70% in less developed countries and in disadvantaged populations in developed countries, and even to more than 80% in some areas of the United Arab Emirates and villages in China (Anil and Anand 2017). The prevalence of ECC is more than 87% in Iranian preschoolers ranging from 5 to 6 years old (Khoshnevisan et al. 2018). The existence of dental plaque indicates poor oral hygiene and is a major risk factor for caries (Premaraj et al. 2020) and ECC.
Preschoolers are unable to take care of themselves and depend on their parents for oral healthcare purposes (Abduljalil and Abuaffan 2016). Mothers are main role models for children's behaviours; since early oral health habits are one of the main elements of maintaining oral health in adulthood, mothers need to teach health skills, proper eating habits and health practices to their children (Abduljalil and Abuaffan 2016).
Nowadays, there are many oral health apps; however, according to a study conducted in the United States (Tiffany et al. 2018) the most used apps have generally poor qualities; this suggests that developing evidence-based oral health applications with appropriate content and right motivating design principles is needed.
Furthermore, the above-mentioned study states that software developers had the highest contribution in designing the majority (58%) of applications, instead of oral health specialists. Also, theoretical foundations were not used for content, or experimental validation in several applications (Tiffany et al. 2018). By Parker et al. (2019), most of the applications are not validated by any dental authority and official organisations or their effectiveness had not been evaluated properly. In a recent study (Alqarni et al. 2018), an application was designed to increase mothers’ knowledge of children's health, but again no clinical evaluation was performed.
In Iran common training methods, such as pamphlets and verbal examination, are mostly used to educate mothers about children’s oral health. To the best of author’s knowledge, there are no trials on the long-term effect of mHealth apps to improve oral health of preschoolers of 6 years old or younger, especially trials that evaluate this effect clinically and compare it to common teaching methods.
The aim of the present trial was to design a health promotion application with reminders and compare its effectiveness with common oral health education delivered in paediatric dental settings. In this trail, it was hypothesised that application-based and common oral health training methods have similar effect on knowledge, attitude and practice of mothers, and oral health of their preschoolers.
Material and methods
General setting and method of the trial
This is a single-blind, parallel, randomised controlled trial with the allocation ratio of 1: 1. The CONSORT statement is used as a guide to write this article; see Additional file 1.
In order to compare the effectiveness of a newly developed smartphone application intervention with common training method, this trial was performed on preschooler–mother dyads who were referred to the clinic of School of Dentistry, Tehran University of Medical Sciences during August 2019 to January 2020.
Inclusion criteria: Due to cultural reasons (for instance, mothers are routinely more involved in children's oral appointments), this trial has been carried out on dyads composed of mothers, condition to owning a smartphone and their preschoolers ranging from 2 to 6 years old.
Exclusion criteria: Exclusion criteria included unwillingness to assist the trial or children with systemic diseases and health conditions.
Prior to data collection, the second author who is specialist in paediatric dentistry was considered the gold standard during the calibration process. Subsequently, a calibration between the examiner dentist, the first author and the specialist was performed by examining 10 two- to six-year-old children, who were not participants of this trial. The examination was re-done one hour later to assess intra-examiner reliability (K = 0.83–0.96).
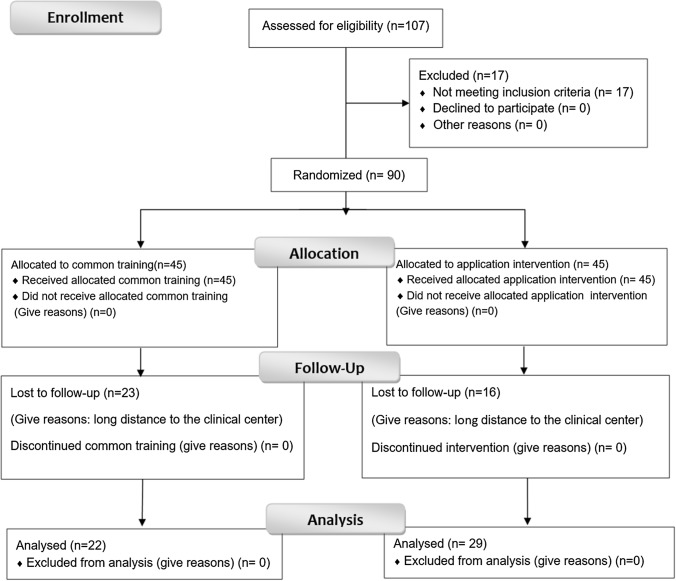
The preschooler–mother dyads were randomly allocated into two equal groups (Fig. 1) using a simple randomisation method by a computer software (Microsoft Excel). Random allocation sequences were performed by the third author, participants were enrolled and interventions were assigned by the fourth author, and as mentioned above all examinations were performed by the first author.
Fig. 1.
CONSORT flow diagram of the randomised controlled trial
Initially, the mothers responded to an interviewer-administered questionnaire; see Additional file 2. Right after that modified dental plaque index (m-PI) of children as a short-term clinical consequence and their modified gingival index (m-GI) as a long-term clinical consequence were measured. Next, the application was installed on the mothers’ smartphones in application group. The mothers were informed about a phone number given in the application, offering support and help in application-related questions and problems. In contrast, an educational pamphlet (see Pamphlet Design Subsection) was given to mothers in common training group, and while distributing the pamphlets, topics, such as brushing technique, the use of fluoride toothpaste, healthy eating and regular dental visits, were verbally explained. After one month, mothers were invited to bring along their child to receive a free toothpaste and toothbrush. At this visit, the questionnaires were re-administered by interviewing mothers and children’s oral status (i.e., m-PI and m-GI) was re-examined. After three months, the mothers were re-contacted and asked to bring along their children for a free fluoride therapy. At that visit, the interviewer-administered questionnaires were filled out for the last time, and the m-PI and m-GI of children were re-examined.
Sample size
The following formula is used to calculate the sample size of two groups:
The computation gave a size of 29 persons for each group. This result is obtained by taking into account the standard deviation of 2 for m-PI (modified Plaque Index), study power of 80%, alpha = 5% and detection of 1.5 score difference between the two groups. Considering 30% attrition, the sample size of each group was increased to 45 persons for baseline.
The questionnaire of the trial
The interviewer-administered questionnaire consists of four following sections: mothers’ knowledge about children’s oral health (18 questions), mothers’ attitudes (5 questions), mothers’ self-reported practice towards children’s health (5 questions) and demographic information (see Table 1 for a summary and Additional file 2 for more details). The latter includes questions on child’s age, sex, mother’s age, education of parents (non-academic/academic), and self-reported economic status of the family (excellent, good, moderate, poor). In addition, a form about child’s oral health status was inserted at the end of questionnaire.
Table 1.
Knowledge, attitude and practice questions’ bodies
| Knowledge | 1.Time of first primary tooth eruption | 2. Transmission of bacteria from mother to child | 3. Fluoridated toothpastes for younger than 3 years old is inadvisable | 4. The first signs of caries in children | 5. Start time for cleaning and tooth brushing primary tooth |
| 6. Fluoridated toothpastes prevent dental caries | 7. Children should not use fluoride | 8. Frequency of intake of sugar more harmful than its used total amount | 9. Irrigation of teeth with copious water after tooth brushing prevent caries | 10. Consumption of xylitol decrease dental caries | |
| 11. Acidity of mouth returns to normal 5 min after a meal | 12. Bottle feeding can cause early childhood caries | 13. Carious primary teeth need restoration | 14–18 Candy, fruit juice, cola, cheese and tea cause dental caries | ||
| Attitude | 1. Is it important that parents clean their child’s teeth? | 2. Primary teeth do not need much care as they eventually fall out anyway | 3. I believe that dental problems can lead to children’s general health problems | 4. Early childhood caries is preventable | 5. Regular dental visits are important for preventing oral diseases |
| Practice | 1. Who brushes your child’s teeth? | 2. How often does your child brush his/her teeth? | 3. Does your child rinse his/her mouth after eating sugary foods? | 4. How often does your child have a sweet snack or drink? | 5. Do you use fluoridated toothpaste for your child? |
The questionnaire was designed based on previous valid questionnaires (Mohebbi et al. 2018; Jain et al. 2014) and a number of new questions designed by the authors. The content and face validity of the questionnaire were assessed by a group of 7 experts of community oral health and paediatric dentistry. Necessary modifications were performed to reach agreement on controversial items. Grammar, wording, proper item allocation and scaling were examined by experts (Content Validity Index (CVI) > 0.83 for all questions). For reliability assessment, the questionnaires were given to 10 mothers, who were not participants of this trial. They were asked to answer the questions twice with a 2-week interval. For all questions, the coefficient of agreement was at least 0.85.
Clinical oral examinations
After interviewing mothers, clinical oral examination was performed on children; see Clinical Examination form in the additional file 2. Dental plaque and gingival status were measured based on, respectively, Löe-Silness modified dental plaque index and modified gingival index (Carranza and Newman 1996) using a disposable dental explorer and a dental mirror:
m-PI: Scores of 0, 1 and 2, respectively, indicated absence of dental plaque, presence of plaque in gingival margin and plaque extending beyond the gingival margin. The mean plaque of all teeth for each child was computed as well (ranging over rational numbers between 0 and 2).
m-GI: Scores 0 and 1, respectively, indicated absence and presence of gingival inflammation. The mean gingival status of all teeth for each child was computed (ranging over rational numbers between 0 and 1).
Below, the word modified might be dropped from modified dental plaque and modified gingival indices when understood.
Blinding
The examiner was blind to the participants’ groups.
Ethical considerations
This trial is considered voluntary participation. Each participant had to sign an informed consent form before entering the trial and were informed of its objectives and protocol. Participants had the right to withdraw from the trial at any stage. This trial ensured information confidentiality and privacy. This trial had no risk or harm to participants.
This trial was approved by the Ethics Committee of the University of Tehran with the code IR.TUMS.DENTISTRY.REC.1397.196 and is registered in the Iranian Registry of Clinical Trials with the code IRCT20131102015238N3.
Application design
To design the application, first educational materials based on American Academy for Pediatric Dentistry (AAPD) guidelines (‘Policy on Early Childhood Caries (ECC): Classifications, Consequences, and Preventive Strategies’; ‘Policy on the Use of Xylitol’; ‘Policy on Use of Fluoride’) were collected. Then contents and user interfaces of all applications on the Android platform, available on Google Play and Bazaar (the most used Iranian app market), were investigated. Oral health as the keyword for the above-mentioned search, both in English and Persian, was used. At the time of designing the author’s app, no scientifically certificated Persian app was found. Finally, an application was designed to improve mothers’ knowledge about children’s oral health based on the best evidence and guidelines, and the educational design principles. This application was designed for Android operating system with JAVA programming language in Android Studio version 3.1.4. The SQLite website was used to design and install the database, and DB Browser and SQLite version 3.10.1 were used to transfer data to the database.
The application provided the following paediatric oral health information to mothers: proper nutrition, use of fluoride toothpaste, regular dental visits, and information about children’s oral health, such as a video presenting the scrub brushing technique and amount of toothpaste for different ages. In order to foster oral health promotion behaviours, every night at 9:00 p.m. a notification popped up (and rang) on the mother’s smartphone reminding them to brush their preschooler’s teeth. The application was evaluated by a group of oral health professionals, paediatric dentists, e-learning and programming specialists. A pilot study was performed by installing the app for three mothers; no misunderstanding about the content was found. This, however, resulted in updating the user interface of final design.
Pamphlet design
As a common practice in oral health trainings, pamphlets along with verbal explanations were provided. The pamphlet had the same educational content as the application. They also include colour images and a visual explanation of the scrub brushing technique. The educational content was also explained verbally to mothers.
Statistical analysis
Data analysis was carried out using SPSS software version 24. Standard deviation and mean were calculated for quantitative variables, while percentage and frequency were reported for qualitative variables. The correct answers to questions on mothers' knowledge about children’s oral health were scored one, and scored zero otherwise (including ‘I do not know the answer’). The knowledge score of each dyad was computed as a total sum of scores from all above-mentioned questions. The answers to the questions on mothers’ attitude were scored based on a five-point Likert scale, ranging from zero (worst attitude) to four (best attitude). The total attitude score of each dyad was computed as a total sum of all score from questions on the attitudes of mothers. The range of scores for each question on mothers’ practice varied, and the total score for each dyad was the sum of all scores. Finally, a generalized estimating equation (GEE) with exchangeable correlation structure was used to investigate the effect of methods on the outcomes of knowledge, attitude and mothers’ practice regarding children’s oral health, dental plaque and gingivitis status over time, after adjusting the two groups in terms of demographic variables. Little’s test was used to determine whether loss to follow-up was missing completely at random (MCAR). The significance level was set at 0.05.
Results
At first 107 preschooler–mother dyads were evaluated for inclusion criteria, of whom 90 dyads met the inclusion criteria. Dyads were randomly and equally divided into common training and application group. In the first follow-up, 23 people in common training group and 16 people in application group dropped out of this trial and there was no further drop out in the two groups (see CONSORT diagram in Fig. 1).
The percentage of girls (54.4%) in total was higher than that of boys. Among children, less than 50% had regular dental visits of every 6 months to a year, that is, 33.3% in common training group and 44.4% in application group (see below Table 2). In general, as self-reported by mothers in both groups, the socioeconomic status of most families was moderate and good. The mean age of mothers was 35.6 ± 5.0 years (age range 24–47 years) and the mean age of the preschoolers was 4.6 ± 1.2 years (age range 2–6 years).
Table 2.
Demographic information of mothers and children in common training method and application groups
| Variable | Category | Common training groups | App groups | ||||
|---|---|---|---|---|---|---|---|
| At baseline (total) | Follow-up | Loss to follow-up | At baseline (total) | Follow-up | Loss to follow-up | ||
| n = 45 | n = 22 | n = 23 | n = 45 | n = 29 | n = 16 | ||
| Gender of the child | Boy | 22 (48.9%) | 9 (40.9%) | 13 (56%) | 19 (42.2%) | 12 (41.4%) | 7 (43.8%) |
| Girl | 23 (51.1%) | 13 (59.1%) | 10 (43.5%) | 26 (57.8%) | 17 (58.6%) | 9 (56.3%) | |
| Child dental visit | Problem | 23 (51.1%) | 10 (45.5%) | 13 (56.5%) | 5 (11.1%) | 3 (10.3%) | 2 (12.5%) |
| Every 6 months to 1 year | 15 (33.3%) | 9 (40.9%) | 6 (26.1%) | 20 (44.4%) | 14 (48.3%) | 6 (37.5%) | |
| Irregular | 6 (13.3%) | 2 (9.1%) | 4 (17.4%) | 7 (15.6%) | 5 (17.2%) | 2 (12.5%) | |
| Etc | 1 (2.2) | 1 (4.5%) | 0 (0%) | 13 (28.9%) | 7 (24.1%) | 6 (37.5%) | |
| Level of education of mother | Non-academic | 20 (44.4%) | 5 (22.7%) | 15 (65.2%) | 3 (6.7%) | 2 (6.9%) | 1 (6.3%) |
| Academic | 25 (55.6%) | 17 (77.3%) | 8 (34.8%) | 42 (93.3%) | 27 (93.1%) | 15 (93.8%) | |
| Level of education of father | Non-academic | 26 (57.8%) | 9 (40.9%) | 17 (73.9%) | 3 (6.7%) | 1 (3.4%) | 2 (12.5%) |
| Academic | 19 (42.2%) | 13 (59.1%) | 6 (26.1%) | 42 (93.3%) | 28 (96.6%) | 14 (87.5%) | |
| Socioeconomic status of the family | Excellent | 0 (0%) | 0 (0%) | 0 (0%) | 1 (2.2%) | 1 (3.4%) | 0 (0%) |
| Good | 12 (26.7%) | 7 (31.8%) | 5 (21.7%) | 23 (51.1%) | 16 (55.2%) | 7 (43.8%) | |
| Moderate | 26 (57.8%) | 12 (54.5%) | 14 (60.9%) | 21 (46.7%) | 12 (41.4%) | 9 (56.3%) | |
| Poor | 7 (15.6%) | 3 (13.6%) | 4 (17.4%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Age of mother | Average | 34.8 | 36.4 | 33.2 | 36.4 | 36.5 | 36.3 |
| SD | 5.3 | 4.6 | 5.6 | 4.5 | 4.9 | 3.9 | |
| Age of child | Average | 4.7 | 4.5 | 4.8 | 4.6 | 4.7 | 4.4 |
| SD | 1.2 | 1.1 | 1.2 | 1.2 | 1.3 | 1.2 | |
Table 3 shows mean, standard deviation, the maximum and minimum obtained score of mothers’ attributes regarding children’s oral health, plaque and gingival indices at baseline, and 1-month and 3-month follow-ups. The mean total knowledge score of mothers in common training group at baseline was 11.1 ± 2.0 (where the total score ranges over 0–18), and this mean increased to 14.0 ± 2.0 and 14.5 ± 1.9 in the first and second follow-ups, respectively. In application group, the mothers' knowledge score was initially 10.9 ± 2.3, which increased to 13.1 ± 1.6 and 13.5 ± 1.8 in the first and second follow-ups, respectively.
Table 3.
Mean, standard deviation, the maximum and minimum obtained score of mothers’ attributes regarding children’s oral health, plaque and gingival indices
| Common training group | App group | |||||
|---|---|---|---|---|---|---|
| Baseline (n = 45) |
1-month follow-up (n = 22) | 3-month follow-up (n = 22) | Baseline (n = 45) |
1-month follow-up (n = 29) | 3-month follow-up (n = 29) | |
| Knowledge | ||||||
| Mean | 11.1 | 14.0 | 14.5 | 10.9 | 13.1 | 13.5 |
| SD | 2.0 | 2.0 | 1.9 | 2.3 | 1.6 | 1.8 |
| Attitude | ||||||
| Mean | 18.7 | 19.7 | 19.4 | 18.6 | 19.4 | 19.5 |
| SD | 1.7 | 0.7 | 1.7 | 1.6 | 0.8 | 1.0 |
| Practice | ||||||
| Mean | 4.9 | 8.2 | 7.7 | 4.8 | 8.5 | 8.5 |
| SD | 2.2 | 1.6 | 2.0 | 2.3 | 1.8 | 2.0 |
| Mean plaque | ||||||
| Mean | 1.0 | 0.7 | 0.5 | 0.7 | 0.5 | 0.4 |
| SD | 0.4 | 0.3 | 0.3 | 0.3 | 0.3 | 0.3 |
| Mean gingival | ||||||
| Mean | 0.3 | 0.2 | 0.4 | 0.3 | 0.2 | 0.1 |
| SD | 0.2 | 0.1 | 0.1 | 0.2 | 0.1 | 0.1 |
The mean total attitude score in two groups increased with a relatively similar trend. The mean total practice score of mothers regarding child’s oral health in common training group at baseline was 4.9 ± 2.2 (where the total practice score ranges over 0–14); this mean increased to 8.2 ± 1.6 and reached to 7.7 ± 2.0 in the first and second follow-ups, respectively. In application group, the practice score of mothers regarding child’s oral health was initially 4.8 ± 2.3, which reached to 8.5 in both first (± 1.8) and second (± 2.0) follow-ups.
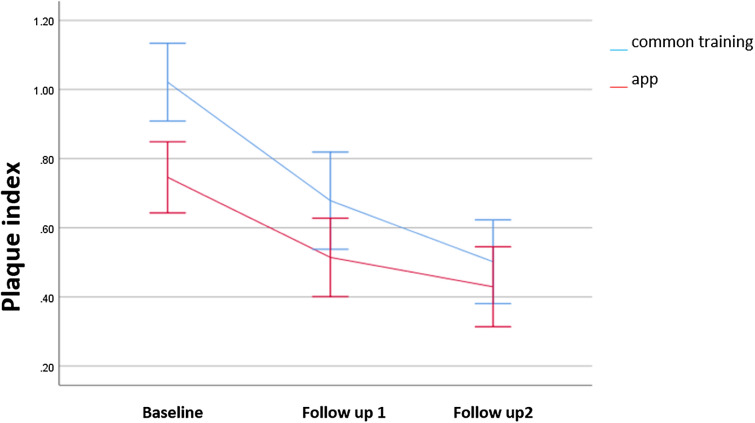
The mean dental plaque score in common training group was initially 1.0 ± 0.4 (where the m-PI for each individual is a rational number between 0 and 2); this mean decreased to 0.7 ± 0.3 and 0.5 ± 0.3 in 1- and 3-month follow-ups, respectively. Furthermore, in application group, it was 0.7 ± 0.3 at baseline, which decreased to 0.5 ± 0.3 and 0.4 ± 0.3 in 1- and 3-month follow-ups, respectively.
The mean gingival index score in common training group decreased from 0.3 ± 0.2 (where the m-GI for each individual is a rational number between 0 and 1) in baseline to 0.2 ± 0.1 in the first follow-up, and increased to 0.4 ± 0.1 in 3-month follow-up. In application group, the gingival index score was 0.3 ± 0.2 at the baseline and reached 0.2 ± 0.1 and 0.1 ± 0.1 in the first and second follow-ups, respectively.
In common training group, comparison of both follow-ups to baseline (before intervention) illustrates a significant improvement in mothers’ knowledge and practice regarding children’s oral health (p < 0.001). Mothers’ attitudes only improved in 1-month follow-up respect to baseline (p < 0.001). The mean dental plaque dropped down in both follow-ups (p < 0.001) compared to baseline, and also in 3-month follow-up compared to 1-month one (p = 0.022). In addition, the gingival condition revealed an improvement of 10 percent in the first follow-up compared to baseline (p < 0.001), and a worsening in 3-month follow-up compared to both baseline (p = 0.009) and 1-month follow-up (p < 0.001). The reported worsening in these comparisons is 10 and 20 percent, respectively.
In application group, Mothers’ knowledge, attitude and practice regarding children’s oral health improved when comparing between both follow-ups to baseline (p < 0.001 for all of them). Compared to baseline, the mean dental plaque improved in both 1-month (p = 0.001) and 3-month follow-ups (p < 0.001). There are improvements in gingival conditions between all comparison points: 1-month follow-up to baseline (p < 0.001), 3-month follow-up both to baseline (p < 0.001) and 1-month follow-up (p = 0.002). The reported improvements in these comparisons are 20 and 10 percent, respectively.
Table 4 shows a comparison between two above-mentioned methods. There was no significant difference between two methods regarding knowledge, attitude and practice of mothers and mean modified dental plaque of child. Figure 2 illustrates the mean score of dental plaque in the two groups at the time of examinations, which follow a relatively similar decreasing trend.
Table 4.
Comparison of the impact of the application with common training group by GEE analysis
| B | 95% confidence L | Interval U | Std. error | p value | |
|---|---|---|---|---|---|
| Knowledge | |||||
| 1-month follow-up vs. baseline | − 0.3 | − 1.4 | 0.8 | 0.6 | 0.607 |
| 3-month follow-up vs. baseline | − 0.3 | − 1.5 | 0.9 | 0.6 | 0.578 |
| 3-month vs 1-month follow-up | 0.0 | − 1.1 | 1.0 | 0.5 | 0.939 |
| Attitude | |||||
| 1-month follow-up vs. baseline | 0.0 | − 0.7 | 0.7 | 0.3 | 0.957 |
| 3-month follow-up vs. baseline | 0.4 | − 0.6 | 1.4 | 0.5 | 0.452 |
| 3-month vs 1-month follow-up | 0.4 | − 0.4 | 1.3 | 0.4 | 0.347 |
| Practice | |||||
| 1-month follow-up vs. baseline | 0.6 | − 0.5 | 1.8 | 0.6 | 0.259 |
| 3-month follow-up vs. baseline | 1.1 | − 0.1 | 2.3 | 0.6 | 0.065 |
| 3-month vs 1-month follow-up | 0.4 | − 0.7 | 1.6 | 0.6 | 0.432 |
| Mean plaque | |||||
| 1-month follow-up vs. baseline | 0.1 | − 0.1 | 0.3 | 0.1 | 0.220 |
| 3-month follow-up vs. baseline | 0.2 | 0.0 | 0.4 | 0.1 | 0.068 |
| 3-month vs 1-month follow-up | 0.1 | − 0.1 | 0.3 | 0.1 | 0.322 |
| Mean gingival | |||||
| 1-month follow-up vs. baseline | 0.0 | − 0.1 | 0.0 | 0.0 | 0.375 |
| 3-month follow-up vs. baseline | − 0.3 | − 0.3 | − 0.2 | 0.0 | < 0.001 |
| 3-month vs 1-month follow-up | − 0.2 | − 0.3 | − 0.2 | 0.0 | < 0.001 |
Fig. 2.
The measured PI in both training method groups in the baseline, 1-month and 3-month follow-up
In Table 4, in comparison of application group with common training group, some notable improvements of gingival condition were seen in 3-month follow-up respective to both baseline (p < 0.001) and 1-month follow-up (p < 0.001). Figure 3 shows the gingival status in which the application group seemingly had more improvement than in common training group in 3-month follow-up.
Fig. 3.
The measured GI in both training method groups in the baseline, 1-month and 3-month follow-up
Discussion
The obtained results showed that both training methods have improved mothers’ knowledge and practice and reduced children’s dental plaque. A notable finding of this trial is that the gingival status in application group had improved over time, in contrast to common training group. This finding confirms the effectiveness of the designed smartphone application in changing mothers’ behaviour in the longer term.
Smartphones have affected almost every aspect of human life in the twenty-first century (Kumar et al. 2016), such as providing an opportunity for parental interaction for promoting oral health (Scheerman et al. 2018). The 2015 surveys showed that an average of 43% of residents in 40 countries have a mobile device (Tiffany et al. 2018). In fact, approximately 1.57 billion people had smartphones in 2014, reaching 2.23 billion people in 2017 (Lee et al. 2018). In 2018, approximately 77% of US residents had a mobile phone (Tiffany et al. 2018). Surveys have also shown that the use of smartphones among Iranian people has increased from 2 million people in 2013 to 27 million people in 2015 (approximately, 2.5 and 33.75%, respectively). Furthermore, due to the virtualisation of many activities during the COVID-19 period, such as school education, this figure is increasing; in a recent report this number has reached 45.4 million, and this growing trend continues (Kermani 2017; ‘How many smartphones are in the world?’).
Prior to this trial, among participants less than 50% had regular dental visits of every six months to a year. This indicates a need to create a culture of regular children’s dental visit for parents. Also, in situations where face-to-face visits are impossible (such as COVID pandemic), virtual methods, such as communication applications and tele-visits, are helpful (Machado et al. 2020).
The scores of mothers’ knowledge and their practice in both groups had improved in both follow-ups compared to baseline. In application group, in addition to the images and content of the application, the improvement might be due to accessibility of the application anytime and anywhere. The results of this trial are consistent with a study in the UK, in which an application to motivate and improve people’s oral health practice was studied (Underwood et al. 2015). Another similar study (Alqarni et al. 2018) indicated improvement in mothers’ knowledge; however, this latter study lacks clinical data and the study period was only 2 weeks. Due to the longer period in this current trial and the presence of clinical data, the effect of application on knowledge and practice change is more clearly observed. The improvement observed in the children oral hygiene in each group in both follow-ups compared to baseline is noteworthy. However, comparing the two groups to each other, there was no significant difference between the oral hygiene of the children in any phases. This result is consistent with a study conducted in China, where WeChat application was used to send educational messages (Li et al. 2016). In contrast, a study conducted in Italy on children aged 4–7 years old revealed a significant decrease in dental plaque in application group (Zotti et al. 2019). In another study (Alkadhi et al. 2017), the plaque index in the application group decreased as in this current. However, contrary to this trial, the application method was more efficient than the verbal method in plaque reduction in people subjected to orthodontic treatment. This might be due to the fact that, in addition to verbal explanation, in this trial explanatory pamphlets were provided to common training group.
Although reduction of dental plaque is important as a clinical measure, such a reduction might be the effect of a last-minute teeth brushing, done for various reasons such as a mother’s social desirability in the dental setting as one of responsible adults for her child’s oral health. To better measure the continuity and regularity of tooth brushing, the current paper considers long-term indicators, such as gingival index. In this trial, improvement in gingival health was observed for both methods of education at 1-month follow-up compared to baseline. Despite this initial improvement, the gingival status in common training group not only did not improve at 3-month follow-up but also significantly worsened, compared to both baseline and 1-month follow-up. In contrast, in application group, the gingival status improved significantly at 3-month follow-up compared to both baseline and 1-month follow-up. These remarkable results show that application method had more lasting effects in long term than common training method.
The above could be due to the presence and possibility of rewatching the instructional videos on tooth brushing, or by regularly sent notifications reminding mothers to brush their children’s teeth. Both of these would lead mothers adhering tooth brushing, that is, the important component in maintaining children’s oral health. Also in Alkadhi et al. (2017) using mobile application as an active reminder led to reduction in gingival index. In contrast, in Li et al. (2016), after using WeChat application, no significant difference in gingival index between common training and application groups was seen. Finally, a study in Italy showed that in a longer period, i.e., 6-, 9- and 12-month follow-ups, the gingival status was significantly better in application group, which as in this trial could confirm effectiveness of applications in long term (Zotti et al. 2016).
Due to the importance of maintaining proper oral health behaviour over a long period of time, and since developing a habit takes an average of 66 days (Scheerman et al. 2018), it seems that the 3-month period of exposure to the designed application of this trial is long enough to guarantee a fairly long-term behaviour change. Overall, the use of the application as a modern tool and a new approach is likely to give mothers more incentive to care for their children’s oral health (Underwood et al. 2015).
In this trial there was loss to follow-up, where the individuals became lost for reasons not related to the method and outcome of the trial. Little’s test was used to determine whether loss to follow-up were missing completely at random (MCAR), and the analysis strengthened the obtained results by showing that these individuals had no effect on the final result.
As a limitation of this trial, note that in some new generations of smartphones, the notifications were reported to be blocked by the security system of the phone. In such cases the technical support of the team helped the mothers fix the problem and unblock notifications. In addition, (1) only those with smartphones could participate and (2) preschoolers could not be educated along with their mothers. In order to overcome this latter limitation and as a future study, an addition of cartoons or children’s games related to oral health as features could be considered. Furthermore, effects of cultural adaptation and regular updates on application’s educational contents could be investigated.
Conclusion
Considering any limitations of the present 3-month randomised controlled trial, the following conclusion can be made:
There was no significant difference between common training and application methods regarding knowledge, attitude and practice of mothers and mean modified dental plaque of child.
A noteworthy point in this trial is the improvement of paediatric gingival status as a long-term consequence in application group.
This trial shows that training with both methods led to promoting mothers' knowledge and practice about children’s health as well as reducing children's dental plaque.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors wish to thank all involved preschooler and mothers for the valuable participation and co-operation in the study. This study was implemented as part of a post graduate doctoral thesis (No. 1034t) and supported by Tehran University of Medical Sciences (TUMS); Grant no. 41979.
Abbreviations
- App
Application
- m-PI
Modified plaque index
- m-GI
Modified gingival index
- GEE
Generalized estimating equation
- SD
Standard deviation
Author contributions
Mina Shirmohammadi conducted the search and review of retrieved documents. Mina Shirmohammadi, Simin Z. Mohebbi conceived and designed the study. Samaneh Razeghi, Simin Z. Mohebbi and Mina Shirmohammadi collected the data. Mina Shirmohammadi, Ahamad Reza Shamshiri and Simin Z. Mohebbi performed the data analysis and prepared the first draft of the manuscript. All authors (Mina Shirmohammadi, Samaneh Razeghi, Ahamad Reza Shamshiri, Simin Z. Mohebbi) performed the interpretation, contributed to drafting the manuscript, provided input into versions of the manuscript, read, and approved the final manuscript.
Data availability
The datasets used and analysed during the current trial are available from the corresponding author on reasonable request.
Declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval and consent to participate
See Ethical Consideration Subsection.
Consent for publication
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
M. Shirmohammadi, Email: shmina77@gmail.com
S. Razeghi, Email: s-razeghi@tums.ac.ir
A. R. Shamshiri, Email: arshamshiri@tums.ac.ir
S. Z. Mohebbi, Email: smohebbi@tums.ac.ir
References
- Abduljalil HS, Abuaffan AH. 'Knowledge and practice of mothers in relation to dental health of pre-school children. Adv Genet Eng. 2016;5:1–7. doi: 10.4172/2169-0111.1000153. [DOI] [Google Scholar]
- Albert D, Barracks SZ, Bruzelius E, Ward A. 'Impact of a web-based intervention on maternal caries transmission and prevention knowledge, and oral health attitudes. Matern Child Health J. 2014;18:1765–71. doi: 10.1007/s10995-013-1421-8. [DOI] [PubMed] [Google Scholar]
- Alkadhi OH, Mohammed NZ, Read SA, Husam KA, Turki HA, Nancy MA. The effect of using mobile applications for improving oral hygiene in patients with orthodontic fixed appliances: a randomised controlled trial. J Orthod. 2017;44:157–63. doi: 10.1080/14653125.2017.1346746. [DOI] [PubMed] [Google Scholar]
- Alqarni AA, Alfaifi HM, Aseeri NA, Gadah T, Togoo RA. Efficacy of a self-designed mobile application to improve child dental health knowledge among parents. J Int Soc Prev Commun Dent. 2018;8:424. doi: 10.4103/jispcd.jispcd_195_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anil S, Anand PS. Early childhood caries: prevalence, risk factors, and prevention. Front Pediatr. 2017;5:157. doi: 10.3389/fped.2017.00157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baheti MJ, Toshniwal N. Orthodontic apps at fingertips. Progress Orthod. 2014;15:1–5. doi: 10.1186/s40510-014-0036-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carranza FA, Newman MG. Clinical periodontology. 8. Philadelphia: W. B Saunders Company; 1996. [Google Scholar]
- Elangovan R, Arulchelvan Sriram. A study on the role of mobile phone communication in tuberculosis DOTS treatment. Indian J Commun Med: Off Publ Indian Assoc Prev Soc Med. 2013;38:229. doi: 10.4103/0970-0218.120158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estai M, Bunt SM, Kruger Esther, Tennant Marc. The use of mobile health applications in school dental screening. Aust Dent J. 2017;62:394–96. doi: 10.1111/adj.12527. [DOI] [PubMed] [Google Scholar]
- How many smartphones are in the world?. https://www.bankmycell.com/blog/how-many-phones-are-in-the-world. Accessed 5 June 2021
- Iribarren SJ, Schnall R, Stone PW, Carballo-Diéguez A. Smartphone applications to support tuberculosis prevention and treatment: review and evaluation. JMIR mHealth uHealth. 2016;4:e25. doi: 10.2196/mhealth.5022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain R, Oswal KC, Chitguppi R. Knowledge, attitude and practices of mothers toward their children’s oral health: a questionnaire survey among subpopulation in Mumbai (India) J Dent Res Sci Dev. 2014;1:40–5. doi: 10.4103/2348-3407.135073. [DOI] [Google Scholar]
- Kermani H. Smartphone practice and lifestyle: the case of urban in Iran. Sociol Studies Youth. 2017;8:61–78. [Google Scholar]
- Khoshnevisan MH, Ghasemianpour M, Samadzadeh H. Oral health status and healthcare system in IR Iran. J Contemp Med Sci. 2018;4:107–118. [Google Scholar]
- Kumar PD, Madan AA, Mohandoss TW, Rooban T, Vernon LT. Using smartphone video “selfies” to monitor change in toothbrushing behavior after a brief intervention: a pilot study. Indian J Dent Res: Off Publ Indian Soc Dent Res. 2016;27:268. doi: 10.4103/0970-9290.186241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J-A, Choi M, Lee SA, Jiang N. Effective behavioral intervention strategies using mobile health applications for chronic disease management: a systematic review. BMC Med Inform Decis Mak. 2018;18:1–18. doi: 10.1186/s12911-018-0591-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X, Zhen-Rui X, Tang N, Ye C, Zhu X-L, Zhou T, Zhao Z-H. Effect of intervention using a messaging app on compliance and duration of treatment in orthodontic patients. Clin Oral Investig. 2016;20:1849–59. doi: 10.1007/s00784-015-1662-6. [DOI] [PubMed] [Google Scholar]
- Machado RA, Lins N, de Souza R, Oliveira M, Júnior HM, Bonan PRF. Social media and telemedicine for oral diagnosis and counselling in the COVID-19 era. Oral Oncol. 2020 doi: 10.1016/j.oraloncology.2020.104685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohebbi SZ, Rabiei S, Yazdani R, Nieminen P, Virtanen JI. Evaluation of an educational intervention in oral health for primary care physicians: a cluster randomized controlled study. BMC Oral Health. 2018;18:1–7. doi: 10.1186/s12903-018-0676-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker K, Bharmal RV, Sharif MO. The availability and characteristics of patient-focused oral hygiene apps. Br Dent J. 2019;226:600–04. doi: 10.1038/s41415-019-0197-7. [DOI] [PubMed] [Google Scholar]
- Policy on early childhood caries (ECC): classifications, consequences, and preventive strategies. https://www.aapd.org/research/oral-health-policies-recommendations/early-childhood-caries-classifications-consequences-and-preventive-strategies/. Accessed 29 May 2021
- Policy on the use of xylitol. https://www.aapd.org/research/oral-health-policies-recommendations/use-of-xylitol/ Accessed 29 May 2021
- Policy on use of fluoride. https://www.aapd.org/research/oral-health-policies-recommendations/use-of-fluoride/ Accessed 29 May 2021
- Premaraj TS, Vella R, Chung J, Lin Q, Hunter P, Underwood K, Premaraj S, Zhou Y. Ethnic variation of oral microbiota in children. Sci Rep. 2020;10:1–10. doi: 10.1038/s41598-020-71422-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheerman JFM, Van Meijel B, Van Empelen P, Kramer GJC, Verrips GHW, Pakpour AH, Van den Braak MCT, Van Loveren C. Study protocol of a randomized controlled trial to test the effect of a smartphone application on oral-health behavior and oral hygiene in adolescents with fixed orthodontic appliances. BMC Oral Health. 2018;18:1–10. doi: 10.1186/s12903-018-0475-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiffany B, Blasi P, Catz SL, McClure JB. Mobile apps for oral health promotion: content review and heuristic usability analysis. JMIR mHealth uHealth. 2018;6:e11432. doi: 10.2196/11432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toniazzo MP, Nodari D, Muniz FWMG, Weidlich P. Effect of mHealth in improving oral hygiene: a systematic review with meta-analysis. J Clin Periodontol. 2019;46:297–309. doi: 10.1111/jcpe.13083. [DOI] [PubMed] [Google Scholar]
- Underwood B, Birdsall J, Kay E. The use of a mobile app to motivate evidence-based oral hygiene behaviour. Br Dent J. 2015;219:E2–E2. doi: 10.1038/sj.bdj.2015.660. [DOI] [PubMed] [Google Scholar]
- Zotti F, Dalessandri D, Salgarello S, Piancino M, Bonetti S, Visconti L, Paganelli C. Usefulness of an app in improving oral hygiene compliance in adolescent orthodontic patients. Angle Orthod. 2016;86:101–07. doi: 10.2319/010915-19.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zotti F, Pietrobelli A, Malchiodi L, Nocini P-F, Albanese M. Apps for oral hygiene in children 4–7 years: fun and effectiveness. J Clin Expl Dent. 2019;11:e795. doi: 10.4317/jced.55686. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and analysed during the current trial are available from the corresponding author on reasonable request.