Abstract
Background and Aim
Although postpartum acute kidney injury (PPAKI) is declining in developing countries, it is still a leading cause of maternal and fetal morbidity and mortality. The study aimed to determine the causes, risk factors, and the outcomes of patients with postpartum acute kidney injury managed at Mogadishu Somali Turkey Training and Research Hospital, in Mogadishu, Somalia over a two years period.
Methods
This study was conducted retrospectively at Mogadishu Somali-Turkey Training and Research Hospital, Somalia’s largest teaching and referral hospital. During a two-year period (January 2020 to December 2021), we evaluated women who had acute kidney injury during the postpartum period and were hospitalized in our hospital. The data was also evaluated for postpartum admission day and hospital stay. The requirement for dialysis and the results were documented. Maternal outcomes are categorized as follows: Complete recovery after discharge/follow-up, chronic dependence on hemodialysis and death during admission.
Results
We studied 79 postpartum AKI patients. The mean age of the participants was 28.67 ± 6.14. Most patients (51%) were aged 20–30, followed by 30–40 (29%). According to self-reported comorbidities, most individuals had no history of chronic diseases, 8 (10.1%) had hypertension and 3 (3.8%) had heart failure, and DM and HTN 2(2.5%). The most common causes of PPAKI were eclampsia (24.1%), hemorrhagic shock, intrauterine mortality (16.5%), placenta abruptio and uterine rupture (8.9%). Hemorrhage (5.1%) and placenta previa (2.5%). The patient’s outcome was associated with age (p=0.04), platelet (p=0.024), and hospital stay (p=0.009).
Conclusion
Postpartum acute kidney injury is very common in underdeveloped nations. Preeclampsia/Eclampsia, obstetric bleeding, and intrauterine death are the leading causes of postpartum acute kidney injury in Somalia. This tragic scenario may be avoided by providing appropriate antenatal care and raising awareness among Somali women about the benefits of antenatal care provided by public institutions.
Keywords: postpartum AKI, pregnancy-related acute kidney injury, Somalia, eclampsia
Introduction
Acute kidney injury (AKI) is a sudden loss of kidney function that causes urea and other nitrogenous waste products to be retained, as well as extracellular volume and electrolyte imbalance.1 AKI diagnosed between the time of childbirth and six weeks after delivery was referred to as postpartum AKI.2 Postpartum acute kidney injury (PPAKI) is a common cause of obstetric AKI. Over the second half of the 20th century,3 the incidence of PRAKI has decreased dramatically, with a low incidence of 1.5–2.8% in developed countries4 and a higher prevalence of 15–20% in developing countries.5 Even though, pregnancy-related acute kidney injury (PRAKI) is becoming less common in developing countries, it is still a major cause of maternal and fetal morbidity and mortality.6
The maternal mortality rate (MMR) in Somalia is high and reported to be 692 per 100,000 live births, as per the Somalia Health Demographic Survey report, 2020. The MMR in Somalia has decreased from 732 in 2015 to 692 in 2020, according to the Maternal Mortality Estimation Inter-Agency Group for Somalia. Even though there is a decrease, it is still high when compared to neighboring nations like Kenya (362 per 100,000), Ethiopia (412 per 100,000), and Uganda (412 per 100,000).7 Maternal conditions are the leading cause of death in women between the ages of 15 and 49 in Somalia.8 High fertility rates, poor contraceptive uptake, low skilled birth attendance rate, inadequate access to maternal health services, inadequate access to emergency obstetric care, and the usage of female circumcision are all factors that contribute to Somalia’s high maternal mortality rate. In the five years preceding the Somalia Health Demographic Survey report, 68% of women did not have any antenatal care (ANC) visit during their most recent pregnancy. At least once, 31% of those who went to get ANC obtained it from qualified persons (doctors/clinical officers or nurses/midwives/auxiliary midwives). A doctor or clinical officer provided ANC to 12% of women, while a midwife, nurse, or auxiliary midwife provided care to 19%.7
Place of delivery also plays an important role in determining the outcome and the complication of the pregnancy. According to the Somalia Health Demographic Survey report, 2020, only 32% of Somalia births are attended by a competent health professional, such as a doctor/clinical officer or a nurse/midwife/auxiliary midwife. According the data, one out of every five births (21%) occurred in a health facility in the five years before the survey, with the vast majority of births (79%) delivered at home. The survey shows that 2% of mothers deliver their babies through caesarian section.
In many parts of the world, the primary cause of PRAKI is hypertensive diseases of pregnancy, such as pre-eclampsia and eclampsia; hemolysis, elevated liver enzymes, low platelets (HELLP) syndrome, which account for nearly 75% of all cases.9,10
Postpartum acute kidney injury burdens the already strained health care system in Somalia, where the number of noncommunicable diseases has recently increased, as one study in Mogadishu reported that around 45% of hospital admissions were related to kidney diseases.11
The study aimed to determine the causes, risk factors and the outcomes in patients with postpartum acute kidney injury managed at Mogadishu Somali Turkey Training and Research Hospital, in Mogadishu, Somalia over a two years period.
Materials and Methods
This retrospective cross-sectional design study was carried out at Mogadishu Somali-Turkey Training and Research Hospital in Mogadishu, the capital of Somalia, which is the largest teaching and referral hospital in the country.
Ethical approval was obtained prior to data collection from the Institutional Review Board (IRB) of Mogadishu Somali Turkey Training and Research Hospital, and patient consent was waived due to the retrospective design of our study. Patients’ data were obtained from the medical record system and anonymously analyzed to protect patient privacy. This study complies with the Declaration of Helsinki.
Inclusion Criteria
All postpartum patients who were previously healthy and developed acute kidney injury and fulfilled the diagnostic definition of acute kidney within the guidelines of Kidney Disease Improving Global Outcome (KDIGO).
Exclusion Criteria
Patients with evidence of kidney disease before pregnancy, have a history of kidney stone disease, have small kidney sizes, and elevated serum creatinine before gestation have been excluded from the study.
History, clinical observations, hemogram, renal function tests, electrolytes, liver functions, and ultrasonography were collected and studied for women who presented with acute kidney injury in the postpartum period and were admitted to our hospital for two years (January 2020 to December 2021). The data were also examined from the day of postpartum admission and the length of stay in the hospital. The need for dialysis was also documented, as was the outcome. Maternal outcome has been classified as follows: • Complete recovery at discharge/follow-up. • Chronic hemodialysis dependent: Patients who required continuous hemodialysis at the time of discharge and for more than 3 months after discharge. • Death- those who died during the admission.
Acute kidney injury is defined according to Kidney Disease Improving Global Outcome (KDIGO) Guidelines as any of the following: a) Increase in serum creatinine (SCr) by X0.3 mg/dl (X26.5 lmol/l) within 48 hours; b) an increase in SCr to X1.5 times baseline, which is known or presumed to have occurred within the previous 7 days; c) urinary volume of 0.5 mL/kg/h for 6 hours.12
Pre-eclampsia was defined by three signs: hypertension [systolic blood pressure (SBP) 140 mm Hg and/or diastolic blood pressure (DBP) 90 mm Hg]; edema; and proteinuria after 20 weeks of pregnancy.
Eclampsia was defined by the presence of generalized convulsions and/or loss of consciousness during pregnancy or postpartum.
Sepsis was defined as per surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2021 definition of life-threatening organ dysfunction caused by a dysregulated host response to infection.13
IBM’s SPSS software version 22.0 was used to analyze the data. The median standard deviation was used to represent the results. Fisher’s exact and Chi-square tests were utilized.
Results
We analyzed a total of 79 postpartum patients with acute kidney injury. The mean age of the study participants was 28.67±6.14. Most of the patients 41 (52%), were between 20–30 years old, followed by 30–40 years, which constitutes 29(36.7%) whereas less than 20 years and more than 40 years reposted 8.9%, and 2.5% respectively (Table 1).
Table 1.
Demographics and Clinical Characteristics of the Study Population
| Factors | Frequency/Mean | Died | Survived | χ2 | P-value |
|---|---|---|---|---|---|
| Age Group (Years) | |||||
| <20 | 7(8.9%) | 2(28.6%) | 5(71.4%) | 9.052 | 0.029* |
| 20–30 | 41(52%) | 7(17.1%) | 34(82.9%) | ||
| 31–40 | 29(36.7%) | 0(0.0%) | 29(100.0%) | ||
| >40 | 2(2.5%) | 1(50.0%) | 1(50.0%) | ||
| Comorbidities | |||||
| No Comorbid | 65(82.3%) | 10(15.4%) | 55(84.6%) | 2.466 | 0.651 |
| Hypertension | 8(10.1%) | 0(0.0%) | 8(100.0%) | ||
| Heart Failure | 3(3.8%) | 0(0.0%) | 3(100.0%) | ||
| Diabetes with HTN | 2(2.5%) | 0(0.0%) | 1(100.0%) | ||
| Hypothyroidism | 1(1.3%) | 0(0.0%) | 2(100.0%) | ||
| Cause of Postpartum AKI | |||||
| Eclampsia | 19(24.1%) | 1(5.3%) | 18(94.7%) | 19.350 | 0.152 |
| Sepsis | 4(5.1%) | 2(50%) | 2(50%) | ||
| Uterine rupture | 7(8.9%) | 0(0.0%) | 7(100.0%) | ||
| Placenta previa | 2(2.5%) | 0(0.0%) | 2(100%) | ||
| PPH | 4(5.1%) | 1(25.0%) | 3(75.0%) | ||
| Intrauterine death | 13(16.5%) | 1(7.7%) | 12(92.3%) | ||
| Hemorrhagic Shock | 13(16.5%) | 3(23.1%) | 10(76.9%) | ||
| Placenta abruptio | 7(8.9%) | 0(0.0%) | 7(100.0%) | ||
| Eclampsia and Sepsis | 1(1.3%) | 0(0.0%) | 1(100.0%) | ||
| Uterine rupture Plus Hemorrhagic Shock | 2(2.5%) | 0(0.0%) | 2(100.0%) | ||
| Eclampsia Plus Placenta previa Plus Hemorrhagic Shock | 1(1.3%) | 0 (0.0%) | 1(100.0%) | ||
| Placenta previa Plus Intrauterine death | 1(1.3%) | 0 (0.0%) | 1(100.0%) | ||
| Eclampsia Plus Uterine rupture | 3(3.8%) | 1(33.3%) | 2(66.7%) | ||
| Eclampsia Plus Hemorrhagic Shock | 1(1.3%) | 0(0.0%) | 1(100.0%) | ||
| Sepsis Plus Hemorrhagic Shock | 1(1.3%) | 1(100.0%) | 0(0.0%) | ||
| Urine Output | |||||
| Anuric | 57(72.15%) | 7(25.9) | 20(74.1) | 2.1 | 0.67 |
| Oliguric | 24(27.84%) | 3(5.8) | 49(94.2) | ||
| Duration of stay | |||||
| 5 days | 7(30.43) | 16(69.56) | 9.5 | 0.009* | |
| 5–10 days | 11.48±11.02 | 2(7.69) | 24(92.30) | ||
| >10 days | 1(3.33) | 29(96.66) | |||
| USG | |||||
| Not done | 8(10.1%) | 2(25.0%) | 6(75.0%) | 4.424 | 0.219 |
| Normal Abdominal | 17(21.5%) | 4(23.5%) | 13(76.5%) | ||
| Renal Parenchymal Disease | 51(64.6%) | 4(7.8%) | 47(92.2%) | ||
| Unilateral/Bilateral Renal Atrophy | 3(3.8%) | 0(0.0%) | 3(100.0%) | ||
Note: *p values <0.05 are statistically significant.
Abbreviations: IUD, Intrauterine death; USG, ultrasound AKI acute kidney injury; PPH, postpartum hemorrhage.
For self-reported comorbidities, most of the patients reported that they had no history of chronic diseases 65(82.3%) while 8 (10.1%) and 3(3.8%) have hypertension and heart failure; the remaining 1 (1.3%), 2(2.5%) had a hypothyroidism, DM and HTN, respectively (Table 1).
The common causes of PRAKI were eclampsia 19 (24.1%), hemorrhagic shock, intrauterine death (16.5%), placenta abruptio and uterine rapture in 8.9%, followed by sepsis, postpartum hemorrhage 5.1%, and placenta previa 2.5% (Table 1).
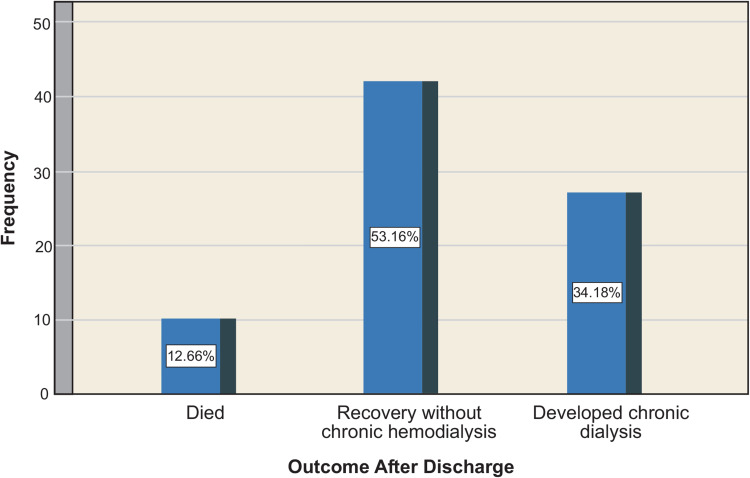
The mean of laboratory test results reported that Aspartate Aminotransferase, Alanine Transaminase, white blood cell count, hemoglobin, serum creatinine urea, sodium, potassium uric acid and albumin were 216.9±445.3, 146.3±268.8, 16.6±9.17, 7.58±2.36, 15.7±79.00, 136.4±85.95, 129.6±13.34, 10.2±47.40, 9.5±3.08, 2.86±2.42, respectively (Table 2). The mean hospital stays were 11.48 ± 11.02 days. 27 (34.2%) patients became dialysis-dependent, while 42 (53.2%) had a full renal recovery, 10 deaths were recorded, giving a maternal mortality rate of 12.7% (Figure 1).
Table 2.
Laboratory and Clinical Characteristics of the Study Population
| Laboratory and Clinical Characteristics | Frequency/Mean | Died | Survived | χ2 | P-value |
|---|---|---|---|---|---|
| Glucose | |||||
| Hypoglycemia | 109.67±53.73 | 2(28.6%) | 5(71.4%) | 2.010 | 0.366 |
| Normal | 6(12.5%) | 42(87.5%) | |||
| Hyperglycemia | 2(8.3%) | 22(91.7%) | |||
| AST | 0.461 | 0.395 | |||
| Normal | 216.91±445.3 | 2(8.7%) | 21(91.3%) | ||
| Abnormal | 8(14.3%) | 48(85.7%) | |||
| ALT | 1.950 | 0.145 | |||
| Normal | 146.29±268.77 | 3(7.5%) | 37(92.5%) | ||
| Abnormal | 7(17.9%) | 32(82.1%) | |||
| Urea (mg/dL) | 0.611 | 0.575 | |||
| Normal | 136.37±85.95 | 0(0.0%) | 4(100.0%) | ||
| Abnormal | 10(13.3%) | 65(86.7%) | |||
| Sodium (mmol/L) | 3.387 | 0.184 | |||
| Low Sodium | 129.56±13.34 | 8(13.6%) | 51(86.4%) | ||
| Normal | 1(5.6%) | 17(94.4%) | |||
| High Sodium | 1(50.0%) | 1(50.0%) | |||
| Potassium (mmol/L) | 3.016 | 0.221 | |||
| Low Potassium | 10.15±47.40 | 1(14.3%) | 6(85.7%) | ||
| Normal | 4(8.0%) | 46(92.0%) | |||
| High Potassium | 5(22.7%) | 17(77.3%) | |||
| Uric Acid | 7.626 | 0.022* | |||
| Low Uric acid | 9.51±3.08 | 1(100.0%) | 0(0.0%) | ||
| Normal | 2(7.4%) | 25(92.6%) | |||
| High Uric Acid | 7(13.7%) | 44(86.3%) | |||
| Albumin | 0.774 | 0.679 | |||
| Low Albumin | 2.86±2.42 | 10(13.5%) | 64(86.5%) | ||
| Normal | 0(0.0%) | 2(100.0%) | |||
| High Albumin | 0(0.0%) | 3(100.0%) | |||
| CPR | 1.113 | 0.372 | |||
| Normal | 76.46±56.79 | 0(0.0%) | 7(100.0%) | ||
| Abnormal | 10(13.9%) | 62(86.1%) | |||
| Platelet | 8.725 | 0.013* | |||
| Low Platelet | 4(12.9%) | 27(87.1%) | |||
| Normal | 3(7.1%) | 39(92.9%) | |||
| High platelet | 3(50.0%) | 3(50.0%) | |||
Note: *P-values < 0.05 are statistically significant.
Abbreviations: SD, standard deviation; ALT, Alanine transaminase; AST, Aspartate transaminase; CRP, C-reactive protein.
Figure 1.
Outcomes of the study population.
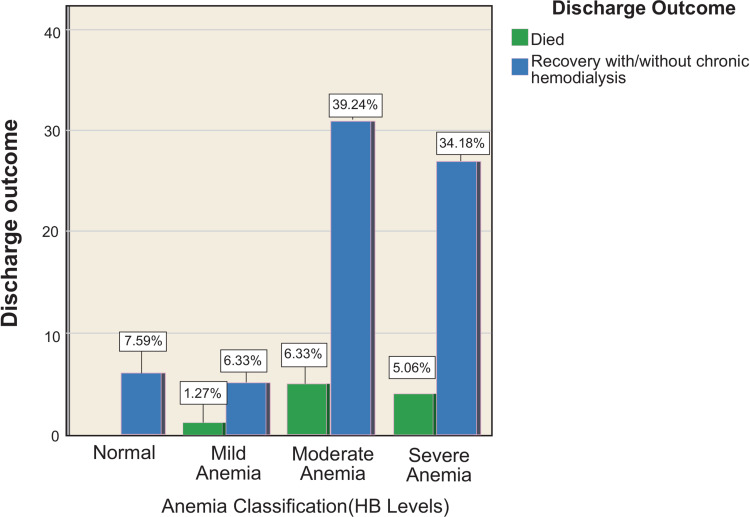
About 34% of postpartum patients had severe anemia during their presentation. Although it was not statistically significant, the probability of postpartum death was higher in mothers with severe and moderate anemia and fewer in mothers with mild anemia. On the contrary, surviving mothers were common in mothers without anemia (Figure 2).
Figure 2.
Classification of anemia according to WHO anemia classification.
There was a significant association between age (χ2=4.11, p<0.04), platelet (χ2=8.19, p=0.024), and duration of stay (χ2=9.5, p=0.009, uric acid levels (p<0.022) and the outcome of the patient (died and survived) (Table 2).
Discussion
In developing countries, postpartum acute kidney injury is still quite common, and it has devastating consequences for both maternal and fetal survival. We could not find any previous papers on the prevalence of pregnancy-related AKI in Somalia, therefore, we cannot comment on any changes in the local prevalence of postpartum AKI in Somalia, but studies from neighboring countries showed a high prevalence of pregnancy-related acute kidney injury when compared to developed countries, with 13% from Ethiopia14 and 3.2% from Kenya.15
To the best of our knowledge, this was the first study to determine the demographic characteristics and risk factors of postpartum AKI in Somalia.
The mean age of our study participants was 28.67±6.14 which is comparable to reports from other studies.5,14,16 The study population consisted of young women whose peak age was between 20 to 30 years, which was younger than those reported in Nigeria.17 This difference could be explained by the religious and cultural differences between the population. Our study population’s young age could explain why 82.3% had no premorbid medical conditions.
Pre-eclampsia-eclampsia was the most common cause of postpartum acute kidney injury in our study, similar to previous studies in Kenya and Ethiopia.14,15 Pre-eclampsia/eclampsia or HELLP syndrome, is the most common cause of AKI in pregnant women around the world.18 In Goplani’s5 study, puerperal sepsis was the primary cause of AKI, however Khalil et al19 observed that hemorrhage was the main cause of AKI in their study.
Over 75% of the patients had anemia, clearly demonstrating that the overall antenatal care of these patients was poor. In a study conducted in one of Mogadishu’s internally displaced camps, the prevalence of anemia in pregnant patients was 44.4% and more than 50% of these participants never visited antenatal care.20
In our study, the maternal mortality rate was 12.7%, which is similar to a previous study conducted in Ethiopia14 and almost another report from Pakistan that observed a maternal mortality rate of 15%.19
Using ANC package on a timely and frequent basis allows the delivery of essential services such as identification and management obstetric complications such as preeclampsia, tetanus toxoid immunization, intermittent preventive treatment for malaria during pregnancy (IPTp), and identification and management of infections such as HIV, syphilis, and other sexually transmitted infections (STIs). ANC also provides a chance for competent birth attendance to encourage healthy behaviors such as breastfeeding, early postnatal care, and planning of pregnancy spacing.21
Limitations
This study has some limitations. First, we could not find any prior studies about the postpartum acute kidney injury from Somalia, to compare and contrast with our study results. Second, in the retrospective nature of our study, there may be some unmeasured confounders. Third, the sample size may be small, but this can be a foundation for similar studies with more sample sizes.
Conclusion
Obstetrical complications like postpartum acute kidney injury are still common in developing countries. Preeclampsia/Eclampsia, obstetrical hemorrhages, and intrauterine death are the leading causes of postpartum acute kidney injury in Somalia. This disastrous scenario can be prevented only by providing adequate antenatal care, the provision of health facilities, and raising awareness among Somali women about the benefits of antenatal care provided by public hospitals.
Disclosure
The authors declare no conflicts of interest in relation to this work.
References
- 1.Mehta RL, Kellum JA, Shah SV, et al. Acute kidney injury network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11(2):1–8. doi: 10.1186/cc5713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eswarappa M, Madhyastha PR, Puri S, Varma V, Bhandari A, Chennabassappa G. Postpartum acute kidney injury: a review of 99 cases. Ren Fail. 2016;38(6):889–893. doi: 10.3109/0886022X.2016.1164015 [DOI] [PubMed] [Google Scholar]
- 3.Saraswathi RS. Acute kidney injury in obstetrics- a case report. J Med Dent Sci. 2017;16(8):97–98. [Google Scholar]
- 4.Siva Rama Krishna G, Vani D. Pregnancy related acute renal failure in a tertiary care hospital. IOSR J Dent Med Sci. 2019;18(4):27–30. [Google Scholar]
- 5.Goplani KR, Shah PR, Gera DN, et al. Pregnancy-related acute renal failure: a single-center experience. Indian J Nephrol. 2008;18(1):17–21. doi: 10.4103/0971-4065.41283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jim B, Garovic VD. Acute kidney injury in pregnancy. Semin Nephrol. 2017;37(4):378–385. doi: 10.1016/j.semnephrol.2017.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DNS Government of Somalia. The Somali health and demographic survey 2020; 2020.
- 8.World Health Oraganization. Global health estimates: leading causes of death [Internet]; 2019. Available from: https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/ghe-leading-causes-of-death. Accessed July 7, 2022.
- 9.Hildebrand AM, Liu K, Shariff SZ, et al. Characteristics and outcomes of AKI treated with dialysis during pregnancy and the postpartum period. J Am Soc Nephrol. 2015;26(12):3085–3091. doi: 10.1681/ASN.2014100954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prevalence SA, El-taher SM, Fouad NA, Fouad MA, Mahedy AW. Outcome assessment of pregnancy-related acute kidney injury in morocco: a National Prospective Study. Saudi J Kidney Dis Tran. 2015;26(6):1215–1222. [DOI] [PubMed] [Google Scholar]
- 11.Öznur S, Bashir AM. A retrospective evaluation of patients hospitalized in the internal medicine department at the Turkey Recep Tayyip Erdogan Somalia Mogadishu Training and Research Hospital. Turkish J Intern Med. 2021;3(4):177–187. [Google Scholar]
- 12.Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Inter. 2012; 2(Suppl 1):1–138. [Google Scholar]
- 13.Evans L, Zhang Y, Rong Z, et al. Surviving Sepsis Campaign: international guidelines for management of sepsis and septic shock 2021. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2021;33(10):1159–1164. doi: 10.3760/cma.j.cn121430-20211009-01442 [DOI] [PubMed] [Google Scholar]
- 14.Bekele D, Ahmed M, Ibrahim A, Seman Kedir GC, Chan G. Profile and outcomes of women with pregnancy-related acute kidney injury requiring dialysis at a center in Ethiopia. Int J Gynaecol Obstet. 2017;138(2):138–141. doi: 10.1002/ijgo.12201 [DOI] [PubMed] [Google Scholar]
- 15.Kivai JM, Kayima JK, Were AO, Zahida Q. Impact of pregnancy related acute kidney injury on foetal survival: a single centre experience in Kenya st udy of efficacy of various surgical techniques in use for cont rolling bleeding from placent al bed. IOSR J Dent Med Sci. 2019;18:13–17. [Google Scholar]
- 16.Najar M, Shah A, Wani I, et al. Pregnancy related acute kidney injury: a single center experience from the Kashmir Valley. Indian J Nephrol. 2008;18(4):159. doi: 10.4103/0971-4065.45291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Adejumo OA, Akinbodewa AA, Enikuomehin OC, Lawal OM, Abolarin OS, Alli OE. Pregnancy-related acute kidney injury: etiologies and short-term outcomes in a tertiary hospital in Southwest Nigeria. Saudi J Kidney Dis Transpl. 2019;30(6):1423–1430. doi: 10.4103/1319-2442.275487 [DOI] [PubMed] [Google Scholar]
- 18.Siribamrungwong M, Chinudomwong P. Relation between acute kidney injury and pregnancy-related factors. J Acute Dis. 2016;5(1):22–28. doi: 10.1016/j.joad.2015.08.002 [DOI] [Google Scholar]
- 19.Khalil MAM, Azhar A, Anwar N, Aminullah N-U-D, Wali R. Aetiology, maternal and foetal outcome in 60 cases of obstetrical acute renal failure. J Ayub Med Coll Abbottabad. 2009;21(4):46–49. [PubMed] [Google Scholar]
- 20.Ahmed RH, Yussuf AA, Ali AA, et al. Anemia among pregnant women in internally displaced camps in Mogadishu, Somalia: a cross-sectional study on prevalence, severity and associated risk factors. BMC Pregnancy Childbirth. 2021;21(1):1–9. doi: 10.1186/s12884-021-04269-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization. Standards for improving quality of maternal and newborn care in health facilities. World Health Organization; 2016:84. [Google Scholar]