Abstract
Objective
To determine the associations between Adverse Childhood Experiences (ACEs), adolescent screen time, and physical activity during the early COVID-19 pandemic.
Methods
Data (2016–2020) from the Adolescent Brain Cognitive Development (ABCD) study were analyzed. Linear regression analyses estimated associations between ACE score and screen time and physical activity in May 2020, adjusting for potential confounders.
Results
Of the 6749 adolescent respondents primarily aged 12–13, 81.6% reported a history of one ACE or more. In adjusted models, a higher ACE score was significantly associated with greater hours per day of screen time, with youth with ≥4 ACEs associated with 2.3 more hours of screen time per day compared to youth with 0 ACEs. In addition, the adjusted models found that a higher ACE score was associated with lower physical activity; youth with ≥4 ACEs averaged 0.8 fewer hours per week of physical activity and 0.5 fewer days per week of 60 minutes of physical activity compared to youth with 0 ACEs. Gender and race were also significantly associated with changes in screen time and physical activity.
Conclusions
ACEs are associated with higher adolescent sedentary behaviors, particularly greater screen time, during the early COVID-19 pandemic (May 2020). Clinicians caring for youth exposed to trauma in the postpandemic environment should explore screen time and physical activity behaviors.
Keywords: Adverse Childhood Experiences, adolescence, COVID-19, physical activity, screen time
What's New.
In a national sample of 6749 early adolescents surveyed during the COVID-19 pandemic (May 2020), a higher ACE score was associated with significantly greater hours per day of screen time and fewer hours per week of physical activity.
Alt-text: Unlabelled box
During the COVID-19 pandemic, school closures and social distancing policies resulted in dramatic changes in adolescent behavior; adolescent recreational screen time more than doubled from 3.8 hours per day to 7.7 hours per day, not including screen time for schoolwork.1 In contrast physical activity nearly halved. The percentage of the adolescents meeting Health and Human Services’ (HHS) moderate-to-vigorous physical activity (MVPA) guidelines, defined as 60 minutes of moderate to strenuous physical activity, decreased from 16.1% (prepandemic) to 8.9% (during the pandemic–May 2020).2 , 3 Given that excessive screen time and low physical activity are associated with poor adolescent physical health outcomes such as obesity and negative mental health outcomes such as higher rates of depression and anxiety, understanding correlates for elevated sedentary behaviors is critical to designing effective screenings and interventions.1 , 3, 4, 5, 6 In addition, given that the biggest rise in obesity prevalence is seen in late childhood to early adolescence, it is vital to examine screen time and physical activity potential risk factors in this age group.7
Recent research has demonstrated that Adverse Childhood Experiences (ACEs) are associated with sedentary behaviors including elevated screen time and low physical activity in youth.8 While the majority of these studies have assessed ACEs and adult health behaviors,8 , 9 there have been a few notable pediatric studies. A national cohort study by Jackson, et al., found that an ACE score of 4 or more compared to children or adolescents who have experienced no ACEs is associated with a three-fold higher relative risk of heavy digital media use.10 A study by Harada, et al., found that ACE exposure in children is associated with lower healthy weight behaviors including elevated screen time and lower rates of physical activity.11 However, neither of these studies explored the relationship between ACEs and the dramatic changes in adolescent lifestyle behaviors during the pandemic, a time of significant increased family stressors (financial insecurity, social isolation, and health risks). Further, neither of these studies focused on early adolescence, a critical period of development and growth. This study aims to determine the associations between ACEs, screen time, and physical activity of early adolescents during May 2020. We hypothesize that, after adjusting for confounders, elevated ACE scores among adolescents will be associated with higher rates of sedentary behaviors including higher screen time and lower physical activity.
Methods
Study Population
This study used data from the Adolescent Brain Cognitive Development (ABCD) Study, a large, diverse, prospective cohort study of brain development and health across adolescents from 21 recruitment sites across the United States. (see Appendix further details). We used data from the from the 3.0 data release which included baseline (2016–2018) one-year follow-up (2017–2019), the first half of 2-year follow-up (2018–2019), and the COVID Rapid Response Research (RRR) Survey 1 (May 2020). We omitted study participants who were missing data for sociodemographic variables or did not complete the COVID RRR Survey 1. After omitting these participants, the sample consisted of 6749 adolescents predominately aged 12–13 (range 10–14) that reflect demographic and socio-economic diversity of the United States. Written informed consent and assent were obtained from a parent/guardian and the child, respectively, to participate in the ABCD study.
Measures
Exposure Variables
ACE score was determined through parent and adolescent responses in the baseline (2016–2018), 1-year follow-up (2017–2019), and first half of 2-year follow-up (2018–2019) surveys. The ABCD study assesses nine of ten ACEs reflecting the items in the original CDC-Kaiser ACE study12; emotional abuse was not included as it was not evaluated in the ABCD study.13 A yes response to any of the following nine ACEs at any timepoint was counted as one-point; physical abuse, sexual abuse, household violence, household mental illness, substance abuse in the household, divorce/separation, criminal household member, emotional neglect, and physical neglect (Supplemental Table 1).
Outcome Variables
Screen time was determined using adolescents’ COVID RRR Survey 1 (May 2020) responses. Adolescents self-reported hours of use on a typical day of the following 7 modalities: multiple-player gaming, single-player gaming, texting, social media, video chatting, browsing the internet, and watching or streaming movies, videos, or television shows, excluding schoolwork.14 Total screen time was calculated by summing average screen time of these seven modalities.
Physical activity was determined using adolescents’ COVID RRR Survey 1 (May 2020) responses, which used questionnaires adapted from the International Physical Activity Questionnaire (IPAQ) Short-form.15 Adolescents were asked to report the daily duration (hours and minutes) and frequency (days per week) of daily duration of ≥60 minutes spent in moderate to vigorous physical activities (MVPA), which henceforth we will refer to as physical activity.
Covariates
Parents reported participants’ sex (male or female), country of birth (US or outside US), and race/ethnicity (White, Black, Native American, Latino/Hispanic, Asian, or Other), highest parent education (high school or lower vs college or higher), and household income (less than $75,000 or $75,000 or more, based on the U.S. median household income) at baseline.16
COVID-19 related variables were assessed in the COVID RRR Survey 1 (May 2020) and included school closure (yes or no), child diagnosed with COVID-19 (yes or likely vs no), and loss of household income due to COVID-19 (yes or no).
Statistical Analyses
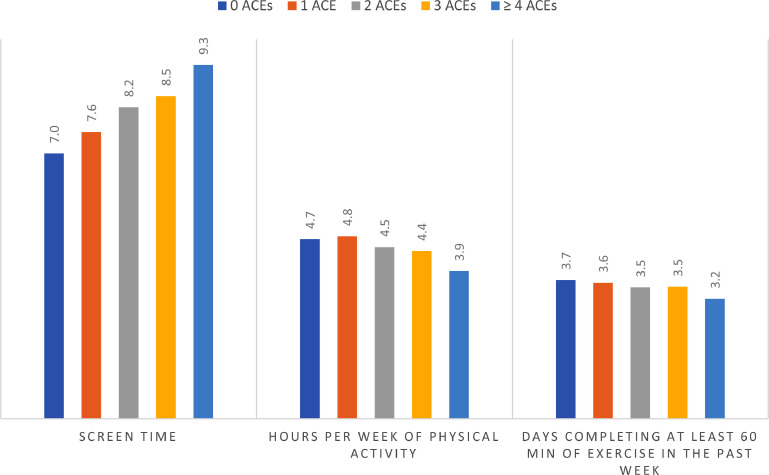
Linear regression analyses estimated associations between reported ACE score (0–9, continuous) and May 2020 screen time and physical activity. Analyses were adjusted for sociodemographic characteristics and COVID-19 related variables listed above. Figure 1 shows mean screen time and physical activity by ACE score, categorized as 0 through ≥4. In this figure, we used ≥4 as a cutoff because prior research has found a cumulative ACE score of 4 or more to be “a de facto threshold for identifying elevated risk for a wide range of negative medical, mental health, and social outcomes.”17
Figure 1.
ACEs and lifestyle behaviors in early adolescents during the COVID-19 pandemic (May 2020). ABCD propensity weights were applied based on the American Community Survey from the 2018 US Census.
Data were weighted using propensity weights from the ABCD study to approximate the 2018 American Community Survey by the US Census.18 All analyses were conducted using Stata 17.0.
Results
Table 1 presents descriptive characteristics of the 6,749 participants aged primarily 12-13 years old. The analytic sample was racially and ethnically diverse (17.4% Latino, 12.1% Black, 6.4% Asian, 2.7% Native American, and 1.3% Other). Four in 5 participants reported a history of one ACE or more at baseline, and 8.7% reported four or more ACEs. Adolescents reported 7.9 hours of daily screen time and 4.6 hours per week of physical activity in the past week.
Table 1.
Descriptive Characteristics of Participants in the Adolescent Brain Cognitive Development (ABCD) Study, May 2020, (n = 6,749)
| Mean (SD) or % (n)* | |
|---|---|
| Demographic characteristics | |
| Age | 12.5 (0.9) |
| Sex | |
| Female | 48.8% (3,247) |
| Male | 51.2% (3,502) |
| Race and ethnicity | |
| White | 59.9% (4,013) |
| Latino / Hispanic | 17.4% (1,018) |
| Black | 12.1% (976) |
| Asian | 6.4% (484) |
| Native American | 2.7% (200) |
| Other | 1.3% (58) |
| Household income | |
| Less than $75,000 | 48.4% (2,028) |
| $75,000 and greater | 51.6% (4,4082) |
| Parents’ highest education | |
| High school education or less | 13.4% (752) |
| College education or more | 86.6% (5,986) |
| COVID-19 related variables | |
| School closure | |
| Yes physically closed | 97.4% (6,481) |
| No | 2.6% (139) |
| Child diagnosed with COVID-19 | |
| Yes | 0.6% (46) |
| No | 99.4% (6,695) |
| Loss of household income due to COVID-19 | |
| Yes | 49.2% (3,199) |
| No | 50.8% (3,504) |
| Self-reported ACE score | |
| 0 | 18.4% (1,291) |
| 1 | 32.4% (2,320) |
| 2 | 26.4% (1,789) |
| 3 | 14.1% (895) |
| ≥ 4 | 8.7% (454) |
| Lifestyle Behaviors | |
| Screen time | 7.9 (6.6) |
| Hours per week of physical activity | 4.6 (6.5) |
| Days completing at least 60 min of exercise in the past week | 3.5 (2.3) |
Propensity weights from the Adolescent Brain Cognitive Development Study were applied based on the 2018 American Community Survey from the US Census
Reported n's do not correspond with % because propensity weights were applied, and each participant has a sample weighting
Unadjusted and adjusted linear regressions examining the associations between ACE score and lifestyle behaviors (screen time and physical activity) are presented in Table 2 . In adjusted models, ACEs were associated with higher screen time, fewer hours per week of physical activity, and fewer days per week completing at least 60 minutes of physical activity. Figure 1 demonstrates that, compared to adolescents with 0 ACEs, youth with ≥4 ACEs averaged 2.3 additional hours of screen time per day, 0.8 fewer hours of physical activity per week, and 0.5 fewer days of 60 minutes of exercise per week.
Table 2.
Associations Among Self-reported ACE Score and Lifestyle Behaviors (Screen Time, Exercise) During the COVID-19 Pandemic, May 2020, (ACEs 0:4), Adjusting for Sociodemographic Characteristics and COVID-19 Related Variables
| Hours per Day of Screen Time |
Hours per Week of Physical Activity |
Days Completing at Least 60 Min of Exercise in the Past Week |
||||
|---|---|---|---|---|---|---|
| B (95% CI) | P | B (95% CI) | P | B (95% CI) | p | |
| Unadjusted model | ||||||
| ACEs | 0.54 (0.36, 0.71) | <.001 | −0.19 (−0.35, −0.03) | .022 | −0.10 (−0.15, −0.05) | <0.001 |
| Adjusted Model* | ||||||
| ACEs | 0.44 (0.26, 0.62) | <.001 | −0.17 (−0.34, 0.00) | .048 | −0.09 (−0.14, −0.03) | 0.001 |
| Sociodemographic characteristics | ||||||
| Age | 0.83 (0.60, 1.06) | <.001 | −0.47 (−0.70, −0.23) | <.001 | 0.19 (0.12, 0.27) | <0.001 |
| Sex | ||||||
| Female | Reference | Reference | Reference | |||
| Male | 1.03 (0.63, 1.43) | <.001 | 0.51 (0.13, 0.90) | .008 | 0.22 (0.10, 0.35) | <0.001 |
| Race and ethnicity | ||||||
| White | Reference | Reference | Reference | |||
| Latino / Hispanic | 1.17 (0.48, 1.86) | .001 | −0.55 (−1.23, 0.13) | .115 | −0.56 (−0.77, −0.36) | <0.001 |
| Black | 2.46 (1.68, 3.23) | <.001 | 0.24 (−0.43, 0.92) | .476 | −0.39 (−0.61, −0.170.21) | <0.001 |
| Asian | −0.34 (−1.11, 0.43) | .389 | −0.55 (−1.47, 0.37) | .244 | −0.29 (−0.57, −0.01) | 0.041 |
| Native American | 2.51 (0.73, 4.29) | .006 | −0.60 (−1.63, 0.43) | .254 | −0.38 (−0.82, 0.05) | 0.082 |
| Other | 2.26 (−0.04, 4.56) | .055 | −0.82 (−2.41, 0.78) | .316 | 0.11 (−0.72, 0.94) | 0.796 |
| Household income | ||||||
| $75,000 and greater | Reference | Reference | Reference | |||
| Less than $75,000 | 0.34 (−0.14, 0.81) | .166 | −0.72 (−1.20, −0.23) | .004 | −0.15 (−0.31, 0.00) | 0.050 |
| Parents' highest education | ||||||
| College education or more | Reference | Reference | Reference | |||
| High school education or less | 0.71 (−0.15, 1.57) | .106 | 0.04 (−0.57, 0.66) | .892 | −0.46 (−0.67, −0.24) | <0.001 |
| COVID−19 related variables | ||||||
| School closure | ||||||
| No | Reference | Reference | Reference | |||
| Yes, physically closed | 0.41 (−1.04, 1.85) | .582 | −0.28 (−1.94, 1.39) | .744 | 0.01 (−0.45, 0.47) | 0.968 |
| Child diagnosed with COVID−19 | ||||||
| No | Reference | Reference | Reference | |||
| Yes | 0.30 (−1.49, 2.10) | .739 | −1.42 (−3.23, 0.39) | .125 | −0.01 (−0.80, 0.77) | 0.970 |
| Loss of household income due to COVID− 19 | ||||||
| No | Reference | Reference | Reference | |||
| Yes | 0.16 (−0.25, 0.58) | .444 | 0.14 (−0.26, 0.53) | .492 | −0.03 (−0.15, 0.10) | 0.685 |
Bold indicates P < .05. ABCD propensity weights were applied based on the American Community Survey from the US Census.
All adjusted models include sociodemographic characteristics (age, sex, race/ethnicity, household income, parent education, site) and COVID-19 related variables (school closure, child diagnosed with COVID-19, and loss of household income due to COVID-19).
Relative to White respondents, Latino/Hispanic and Black racial/ethnic groups were significantly associated with higher screen time and fewer days completing 60 minutes of exercise in the past week. Male gender was associated with higher screen time and higher physical activity.
Discussion
This large, racially diverse, national study of young adolescents found that self-reported ACEs were significantly associated with sedentary behaviors during the early pandemic (May 2020). Similar to prior studies, we found that adolescents had high levels of recreational screen time with an average of 7.9 hours1 and low levels of physical activity, averaging 4.6 hours a week of physical activity, which is far less than the recommend 7 hours per week1 , 3; compared to youth with 0 ACEs, adolescents with ≥4 ACEs averaged 2.3 additional hours of screen time per day, 0.8 fewer hours of physical activity per week, and 0.5 fewer days of 60 minutes of exercise per week.
This study builds upon prepandemic research that has demonstrated significant relationships between ACEs and greater digital media use10 , 11 and lower physical activity11 by showing that ACEs associated with adolescent sedentary behaviors during the early pandemic. The increase by 2.3 hours increase in screen time is less notable than the 3-fold higher difference observed by Jackson et al. This more marginal increase may be partially explained by the global increase in screen time and decrease in physical activity of nearly all youth during the early weeks of the pandemic when nearly all schools were closed. Nevertheless, despite being a smaller association than previously observed, we believe that 2 additional hours of screen represents a meaningful difference in behavior. Further, an ACE score of ≥4 was associated with 0.8 hours fewer hours of physical activity per week and 0.5 days fewer days completed 60 minutes of physical activity, which rounded is one day fewer per week of meeting HHS physical activity guidelines. This decrease in physical activity among youth who have experienced childhood adversity is notable because physical activity, particularly participation in sports teams, has been found to protect against ACE-associated toxic stress; specifically, it has been associated with lower rates of the future development depression and anxiety, thus, pointing to a pressing need to develop interventions to increase physical activity for youth with a history of ACEs post-COVID.19
Our study further adds to the literature by examining sedentary behavioral patterns of early adolescents. The developmental trajectory from childhood to emerging adulthood is a particularly critical period, which is vulnerable to the establishment of health-related behavioral risk factors.20 Thus, understanding the correlates of excessive screen time and lower physical activity is important to inform potential intervention strategies that break patterns of poor health behaviors that emerge in early adolescence.
We also found that identifying as Latino/Hispanic or Black was significantly associated with higher screen time and fewer days completing 60 minutes of physical activity relative to White respondents. This is consistent with prepandemic findings,10 which are thought to be secondary to structural racism–driven factors including differences in built environment. For example, historic redlining has led to higher rates of families of racial minorities living in socially disadvantaged, high-crime neighborhoods, with fewer green spaces,21 which may create safety risks that limit families’ ability to engage in outdoor physical activities. Further, these factors were likely exacerbated by the disproportional effects of COVID-19 pandemic on racial groups. Studies have shown that during the pandemic, people from marginalized racial groups experienced higher rates of food insecurity, COVID-19 related morbidity and mortality, and had a likelihood of being an essential worker.22 This may have prevented caregivers from providing meaningful supervision and decreased adolescent ability to engage in physical activity.
As greater screen time and lower physical activity have been associated with adolescent depression, anxiety, and obesity,1 , 3 these findings are critical to future screening and treatment practices as the pandemic continues to evolve. This study further highlights the importance of screening for ACEs. Once identified, clinicians and future programming caring for ACE-exposed adolescents and their families can provide education about 1) the potential harms of heavy digital use and 2) the biological and psychosocial benefits of physical activity to reduce stress and stress effects. Using a trauma-informed lens, they can next help identify family strengths and context-appropriate strategies to limit digital media use and increase physical activity.
Limitations to this study include the use of self-report data and potential for retrospective recall bias. Second, adolescents often multitask on screens; thus, the computed total could be an overestimate. Third, one ACE from the original Kaiser study, emotional abuse, was not assessed, so we cannot estimate its effects. Nonetheless, these findings provide support for the importance of exploring screen time and physical activity among adolescents who have experienced childhood adversity, educating families about potential mental health consequences, and collaborating on treatment options. Future studies should explore resiliency factors that mitigate the relationship between childhood adversity and lifestyle behaviors as the pandemic progresses.
Funding
J.M.N. was funded by the American Heart Association Career Development Award (CDA34760281) and the National Heart, Lung, and Blood Institute (K08HL159350).
Role of the Funder/Sponsor
The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Financial Disclosure
The ABCD Study was supported by the National Institutes of Health and additional federal partners under award numbers U01DA041022, U01DA041025, U01DA041028, U01DA041048, U01DA041089, U01DA041093, U01DA041106, U01DA041117, U01DA041120, U01DA041134, U01DA041148, U01DA041156, U01DA041174, U24DA041123, and U24DA041147. A full list of supporters is available at https://abcdstudy.org/nihcollaborators. A listing of participating sites and a complete listing of the study investigators can be found at https://abcdstudy.org/principal-investigators.html. ABCD consortium investigators designed and implemented the study and/or provided data but did not necessarily participate in the analysis or writing of this report
Footnotes
Conflicts of interest statement: The authors have no conflict to declare.
Supplementary data related to this article can be found online at https://doi.org/10.1016/j.acap.2022.07.007.
Appendix. Supplementary Data
References
- 1.Nagata JM, Cortez CA, Cattle CJ, et al. Screen time use among us adolescents during the COVID-19 pandemic: findings from the Adolescent Brain Cognitive Development (ABCD) Study. JAMA Pediatr. 2021;176:94–96. doi: 10.1001/jamapediatrics.2021.4334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The role of the pediatrician in primary prevention of obesity | Pediatrics | American Academy of Pediatrics. Accessed February 14, 2022. https://publications.aap.org/pediatrics/article/136/1/e275/29301/The-Role-of-the-Pediatrician-in-Primary-Prevention
- 3.Nagata JM, Cortez CA, Dooley EE, et al. Moderate-to-vigorous intensity physical activity among adolescents in the USA during the COVID-19 pandemic. Prev Med Rep. 2022;25 doi: 10.1016/j.pmedr.2021.101685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paulich KN, Ross JM, Lessem JM, et al. Screen time and early adolescent mental health, academic, and social outcomes in 9- and 10- year old children: utilizing the Adolescent Brain Cognitive Development SM (ABCD) Study. PLoS ONE. 2021;16 doi: 10.1371/journal.pone.0256591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rodriguez-Ayllon M, Cadenas-Sánchez C, Estévez-López F, et al. Role of physical activity and sedentary behavior in the mental health of preschoolers, children and adolescents: a systematic review and meta-analysis. Sports Med Auckl NZ. 2019;49:1383–1410. doi: 10.1007/s40279-019-01099-5. [DOI] [PubMed] [Google Scholar]
- 6.Nagata JM, Iyer P, Chu J, et al. Contemporary screen time usage among children 9-10-years-old is associated with higher body mass index percentile at 1-year follow-up: a prospective cohort study. Pediatr Obes. 2021;16:e12827. doi: 10.1111/ijpo.12827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity among adults and youth: United States, 2015-2016. NCHS Data Brief. 2017:1–8. [PubMed] [Google Scholar]
- 8.Nurius PS, Green S, Logan-Greene P, et al. Life course pathways of adverse childhood experiences toward adult psychological well-being: a stress process analysis. Child Abuse Negl. 2015;45:143–153. doi: 10.1016/j.chiabu.2015.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stults-Kolehmainen MA, Sinha R. The effects of stress on physical activity and exercise. Sports Med Auckl NZ. 2014;44:81–121. doi: 10.1007/s40279-013-0090-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jackson DB, Testa A, Fox B. Adverse childhood experiences and digital media use among U.S. Children. Am J Prev Med. 2021;60:462–470. doi: 10.1016/j.amepre.2020.09.018. [DOI] [PubMed] [Google Scholar]
- 11.Harada M, Guerrero A, Iyer S, et al. The relationship between adverse childhood experiences and weight-related health behaviors in a national sample of children. Acad Pediatr. 2021;21:1372–1379. doi: 10.1016/j.acap.2021.05.024. [DOI] [PubMed] [Google Scholar]
- 12.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) study. Am J Prev Med. 1998;14:245–258. doi: 10.1016/S0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 13.Hoffman EA, Clark DB, Orendain N, et al. Stress exposures, neurodevelopment and health measures in the ABCD study. Neurobiol Stress. 2019;10 doi: 10.1016/j.ynstr.2019.100157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bagot KS, Matthews SA, Mason M, et al. Current, future and potential use of mobile and wearable technologies and social media data in the ABCD study to increase understanding of contributors to child health. Dev Cogn Neurosci. 2018;32:121–129. doi: 10.1016/j.dcn.2018.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee PH, Macfarlane DJ, Lam T, et al. Validity of the international physical activity questionnaire short form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act. 2011;8:115. doi: 10.1186/1479-5868-8-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bureau UC. Income and poverty in the United States: 2018. Census.gov. Accessed February 14, 2022. https://www.census.gov/library/publications/2019/demo/p60-266.html
- 17.Briggs EC, Amaya-Jackson L, Putnam KT, et al. All adverse childhood experiences are not equal: the contribution of synergy to adverse childhood experience scores. Am Psychol. 2021;76:243–252. doi: 10.1037/amp0000768. [DOI] [PubMed] [Google Scholar]
- 18.Heeringa SG, Berglund PA.A guide for population-based analysis of the Adolescent Brain Cognitive Development (ABCD) study baseline data.; 2020:2020.02.10.942011. doi:10.1101/2020.02.10.942011
- 19.Easterlin MC, Chung PJ, Leng M, et al. Association of team sports participation with long-term mental health outcomes among individuals exposed to adverse childhood experiences. JAMA Pediatr. 2019;173:681–688. doi: 10.1001/jamapediatrics.2019.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dahl RE, Allen NB, Wilbrecht L, et al. Importance of investing in adolescence from a developmental science perspective. Nature. 2018;554:441–450. doi: 10.1038/nature25770. [DOI] [PubMed] [Google Scholar]
- 21.Boeck MA, Wei W, Robles AJ, et al. The structural violence trap: disparities in homicide, chronic disease death, and social factors across San Francisco neighborhoods. J Am Coll Surg. 2022;234:32–46. doi: 10.1016/j.jamcollsurg.2021.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lopez L III, Hart LH, III, Katz MH. Racial and ethnic health disparities related to COVID-19. JAMA. 2021;325:719–720. doi: 10.1001/jama.2020.26443. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.