Abstract
Objective:
Social isolation and loneliness have been linked to numerous determinants of health and well-b eing. However, the effects of social isolation and loneliness on oral health remain unclear. The purpose of this study was to examine the effects of social isolation and loneliness on the number of remaining teeth and the rate of tooth loss over time among Chinese older adults.
Methods:
We used three waves of data (2011/2012, 2014 and 2018) from the Chinese Longitudinal Healthy Longevity Survey with 4268 older adults aged 65 and older who were interviewed in at least two waves. The number of remaining teeth was first evaluated at baseline and then subsequently at follow- up visits. Mixed- effects Poisson regression was used to examine the associations between social isolation, loneliness, and both the number of remaining teeth and the rate of tooth loss.
Results:
Social isolation was associated with fewer remaining teeth (β = −.06, 95% CI = −0.13 to 0.00, p < .05) and accelerated tooth loss (β = −.02, 95% CI = −0.02 to −0.01, p < .01) after adjusting for sociodemographic covariates, lifestyle and oral hygiene behaviours, physical and cognitive health, and loneliness. Loneliness was neither associated with the number of remaining teeth (β = .15, 95% CI = −0.01 to 0.30, p = .06) nor with the rate of tooth loss (β = −.01, 95% CI = −0.02 to 0.00, p = .16) after adjusting for all other factors.
Conclusions:
This study provides strong evidence that social isolation was associated with fewer remaining teeth and accelerated tooth loss among Chinese older adults. These findings expand our knowledge about the impact of social disconnection on tooth loss. More future studies are needed to further examine the associations between social connections and oral conditions using longitudinal cohort studies and intervention studies.
Keywords: China, elderly, oral health, social connection, social relationship
1 |. INTRODUCTION
Tooth loss reflects individuals’ history of oral diseases and the quality of dental care services obtained over the life course. In 2010, approximately 158 million people (2.3% world population) were edentulous.1 Older adults are more affected by tooth loss. They have insufficient access to dental care than their younger counterparts.2 Data from the 4th National Oral Health Epidemiological Survey of China (conducted in 2015/2016) showed that 4.5% of Chinese older adults aged 65– 74 were edentulous and only 2.7% utilized dental services in the past 12 months.3 Tooth loss is associated with diminished physical function,4 cognitive decline5 and chronic conditions.6 The relationships between tooth loss and adverse health outcomes highlighted the critical need for more research to identify modifiable factors associated with tooth loss, particularly among older adults.
Social isolation and loneliness are global public health concerns. Approximately 24% of community-dwelling older adults aged 65 and above are considered to be socially isolated in the United States,7 while 29.8% of older adults in China report feeling lonely.8 Social isolation, the structural aspect of social disconnection, is defined as the objective state of having few social relationships and/or infrequent social contact with others.7 On the contrary, loneliness has been conceptualized as the functional indicator of social disconnection caused by the discrepancy between actual and desired social relationships.7 Growing literature suggested that social isolation and loneliness are adverse for health in late life and serve as predictors for psychological disorders,9 cognitive decline10 and overall mortality.11,12 However, one key limitation in the literature is that only a few studies have examined the associations between social disconnection and oral health.13–15
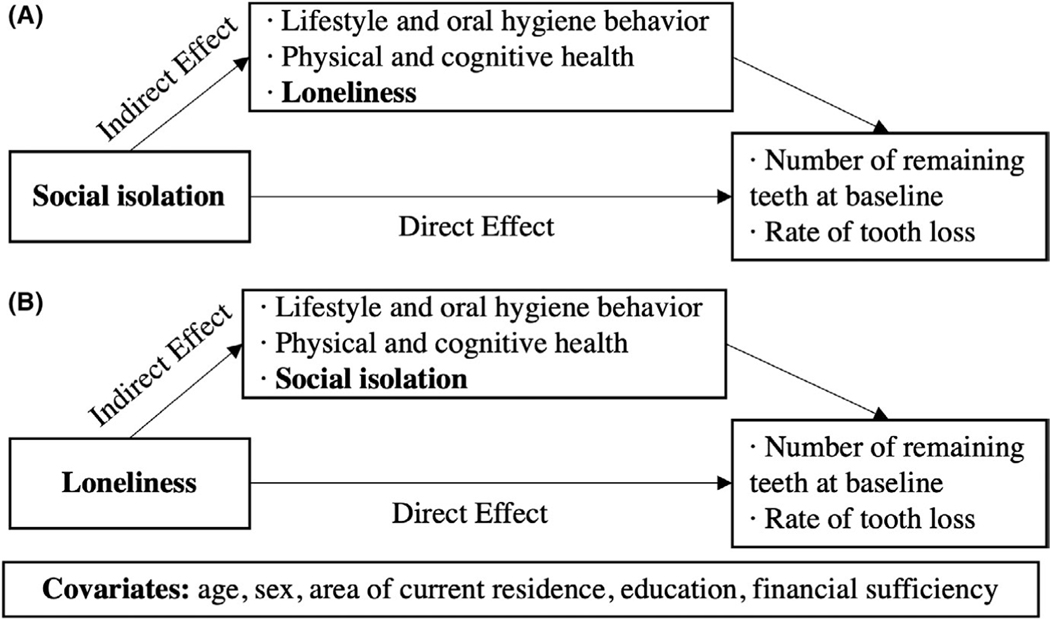
Several pathways may link social disconnection and health outcomes, including lifestyle, health- risk behaviours and physiological dysregulation.16,17 For example, people who feel lonely are more likely to smoke,17 and people who lack social support have infrequent tooth brushing and less dental attendance.18 These behaviours are implicated in tooth loss. In the physiological dysregulation pathway, social disconnection has been associated with risk factors that deteriorate oral health, including cognitive impairment, functional disability and comorbidities.7 As such, theoretical models of social disconnection and health are applicable to oral health.19 As stated earlier, social isolation and loneliness are distinct concepts of social disconnection and have independent associations with different health outcomes.20 A previous study revealed that social isolation and loneliness were only moderately correlated.21 Thus, analysing both objective and subjective aspects of social disconnection in one study can allow us to better understand how these two social constructs affect oral health.20,22 In this study, we proposed a conceptual model (Figure 1) to examine the effects of social isolation and loneliness on tooth loss.
FIGURE 1.
Conceptual models. Note. Model A for Hypothesis 1 on examining the effect of social isolation on tooth loss; Model B for Hypothesis 2 on examining the effect of loneliness on tooth loss
To our knowledge, no previous study has used a nationally representative sample to investigate the effects of social isolation and loneliness on tooth loss among Chinese older adults. Relevant studies have been conducted in other countries, including the United Kingdom (UK) and India.13– 15 However, China’s unique social, economic, cultural and political contexts may influence its older population’s tooth loss and related behaviours.3 Thereby, we used data from the Chinese Longitudinal Healthy Longevity Survey (CLHLS) to test the two hypotheses among Chinese older adults: (1) social isolation is associated with fewer teeth and accelerated tooth loss; (2) loneliness is associated with fewer teeth and accelerated tooth loss.
2 |. MATERIALS AND METHODS
2.1 |. Data and study population
CLHLS is a nationally representative longitudinal survey of Chinese older adults aged 65 and older with an oversampling of individuals over 80 years old. The survey was first conducted in 1998, and the participants were followed every 2– 4 years. The CLHLS used a multistage, stratified cluster sampling method. Participants were recruited from 22 out of 31 provinces in China, with residents in those provinces representing 85% of the total population. Given that the information on oral hygiene behaviour has only been available since 2011, we used the latest three waves of the data. Detailed information about the CLHLS was reported elsewhere.23
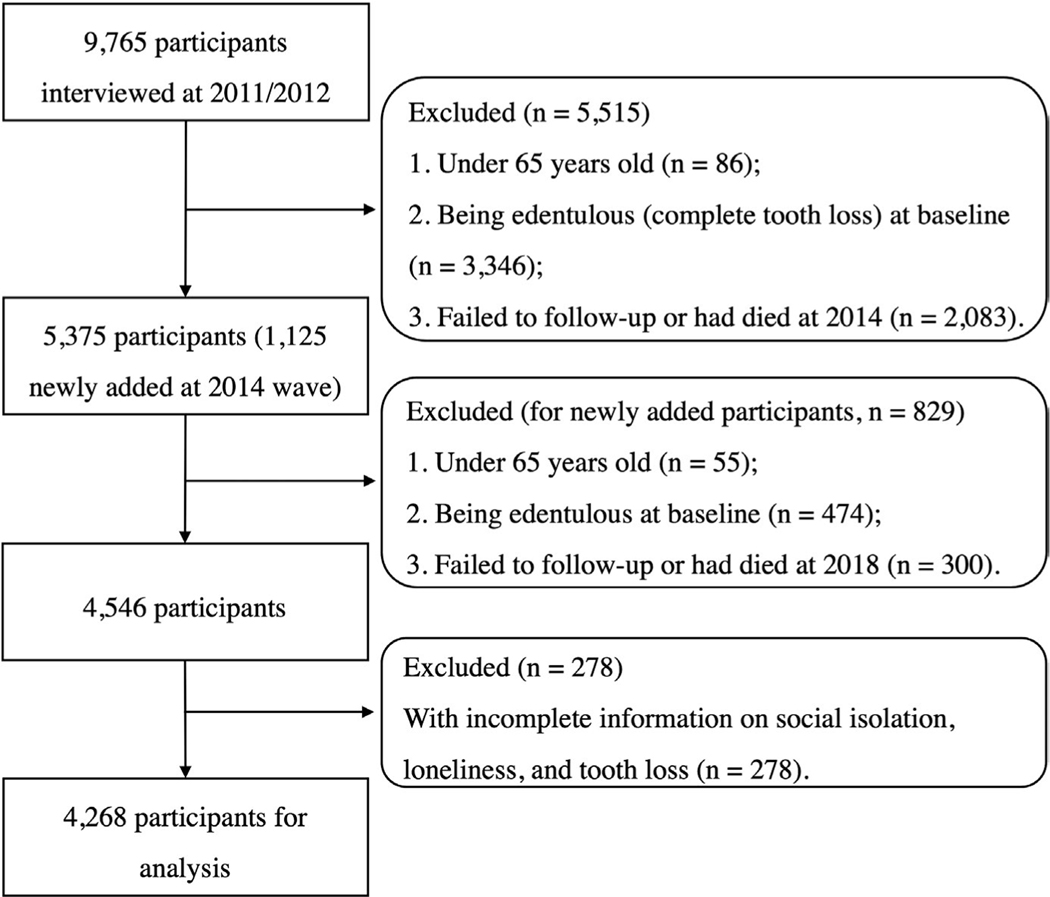
This study included data collected in 2011/2012, 2014 and 2018 and participants who completed at least two waves of the interviews. A total of 9765 participants were first surveyed in 2011/2012, and 1125 participants were newly added in 2014. We excluded the following participants: those under 65 years of age (n = 141); were edentulous at baseline (n = 3820); failed to follow- up or had died before the next wave following the baseline interview (n = 2383); or had incomplete information on social isolation, loneliness and tooth loss at baseline (n = 278). Therefore, the analytic sample consisted of 4268 participants who contributed 10 479 observations over the study period (Figure 2).
FIGURE 2.
Flow diagram of included and excluded participants
2.2 |. Measurements
2.2.1 |. Tooth Loss
The self- reported number of remaining teeth was measured at each wave using the following question: ‘how many natural teeth do you still have?’. The number of remaining teeth ranged from 0 to 32.
2.2.2 |. Social isolation
Participants were considered to be socially isolated based on the following criteria: living alone, were not/no longer married, lacked social support and did not participate in social activities.11,20 According to previous studies conducted in China,24,25 information on social isolation consists of six variables: (1) living alone, (2) divorced/widowed/ never married, (3) unavailability of help when required, (4) unavailability of confidant when needed, (5) unavailability of care provided by family members when sick and (6) not participating in social activities. The social isolation index was a continuous variable constructed by a sum of these variables,10,11 with a higher score indicating greater social isolation (ranges 0 to 6). For illustrative purposes, we followed the procedure proposed by Steptoe and colleagues11 for classifying social isolation. Participants were categorized into two groups by the top quartile (≥2 = isolated vs. <2 points = not isolated).
2.2.3 |. Loneliness
Loneliness was measured by one question: ‘do you often feel lonely?’, with the response options being ‘never’, ‘seldom’, ‘sometimes’, ‘often’ and ‘always’. This single- item measure has been widely used and has been proved to be highly associated with multi- item loneliness scales.26 Given that loneliness is more likely to be underreported in survey design due to its perceived undesirable nature,26 we dichotomized loneliness into two categories (0 = never/seldom lonely, 1 = always/often/sometimes lonely).
2.2.4 |. Lifestyle, oral hygiene behaviour, physical and cognitive health
Lifestyle was measured by participants’ smoking and drinking status. Oral hygiene behaviour was measured by their toothbrushing frequency. Activities of daily living (ADLs) and chronic conditions were used to measure physical health.23 We used education- adjusted mini- mental state examination (MMSE cut- off points to define cognitive impairment: participants with no formal education (score <18); participants with 1– 6 years of schooling (score < 21); and participants with more than 6 years of schooling (score < 25). 23 The reliability and validity of these measures on Chinese older adults were demonstrated elsewhere. All variables were measured at each wave and regarded as time- varying variables (see Table A1 for details).
2.2.5 |. Covariates
Participants’ sociodemographic characteristics were treated as time- invariant covariates, which included age (years), sex (men/women), area of current residence (rural/urban), education (years of schooling = 0 years, 1– 6 years, >6 years) and financial sufficiency (financial support received was sufficient to pay for daily expenses, yes/no).
2.3 |. Statistical analyses
We first assessed the frequencies, mean (M) and standard deviations (SDs) of baseline characteristics. Mixed- effects regression modelling was employed to analyse the number of remaining teeth because this model could account for modelling variance between and within each individual and unevenly timed points across individuals. Additionally, the number of remaining teeth was considered count data and had a fixed upper limit value. Therefore, mixed- effects Poisson regression was adopted for the analysis.27
To test the first hypothesis, we specified a series of models with covariates nested within individuals. Model 1 included only the fixed effect of social isolation. Model 2 introduced a random effect for time to estimate individual variability in slope estimates. Models 3– 5 were built on Model 2 to examine the effects of lifestyle and oral hygiene behaviour, physical and cognitive health, and loneliness, followed by a full model (Model 6) that included a time by social isolation interaction to determine whether the rate of tooth loss varied by social isolation. Sociodemographic characteristics (age, sex, area of current residence, education and financial sufficiency) were added as covariates in all models. Six identical models were fitted for the effect of loneliness on tooth loss.
Formal mediation analyses using the Karlson- Holm- Breen (KHB) method were conducted to examine whether lifestyle, oral hygiene behaviour, and physical and cognitive health mediated the associations between social disconnection and tooth loss. The KHB method decomposed the total effects of social disconnection on tooth loss into direct and indirect effects in both linear and nonlinear probability models.28
Sensitivity analyses were also conducted to examine whether a potential bias was introduced by including participants who failed to follow- up or had died. All statistical analyses were performed using Stata 15.1 (StataCorp; College Station, TX: StataCorp LLC.), and a p- value below .05 was regarded as significant.
3 |. RESULTS
3.1 |. Characteristics of the study population
The characteristics of the 4268 participants at baseline are shown in Table 1. More than a quarter (27.5%) of the participants were categorized as socially isolated, and 26.5% were categorized as feeling lonely. Social isolation and loneliness were positively correlated (r = 0.204, p < .001). The number of remaining teeth for participants at baseline was 14.5 (SD = 9.6).
TABLE 1.
Baseline characteristics of the 4268 participants
| Variables | % | M ± SD | Range |
|---|---|---|---|
| Age (years old) | 80.4 ± 9.7 | 65– 112 | |
| Sex | |||
| Women | 50.4 | ||
| Men | 49.6 | ||
| Current residence | |||
| Rural areas | 80.5 | ||
| Urban areas | 19.5 | ||
| Education level (year of schooling) | |||
| 0 year | 51.0 | ||
| 1–6 years | 35.2 | ||
| ≥ 6 years | 13.8 | ||
| Financial sufficiency (enough for daily expenses) | |||
| Yes | 80.5 | ||
| No | 19.5 | ||
| Smoking | |||
| Never | 63.1 | ||
| Former | 15.6 | ||
| Current | 21.3 | ||
| Drinking | |||
| Never | 65.7 | ||
| Former | 14.2 | ||
| Current | 20.1 | ||
| Toothbrushing frequency | |||
| Never | 22.0 | ||
| Less than once a day | 14.7 | ||
| Once a day | 46.1 | ||
| More than once a day | 17.2 | ||
| Impaired activities of daily living | 10.8 | ||
| One or more chronic conditions | |||
| With | 46.0 | ||
| Without | 54.0 | ||
| Cognitive impairment (MMSE) | 9.3 | ||
| Loneliness | |||
| Yes (always/often/sometimes feel lonely) | 26.5 | ||
| No (seldom/not feel lonely) | 73.5 | ||
| Social isolation | |||
| Yes (≥2) | 27.5 | ||
| No (<2) | 72.5 | ||
| Number of remaining teeth | 14.5 ± 9.6 | 1–32 |
Abbreviations: M, mean; MMSE, mini- mental state examination; SD, standard deviation.
3.2 |. Longitudinal association between social isolation/loneliness and tooth loss
Table 2 presents the results from the mixed- effects Poisson regressions. As shown in Model 1, social isolation was significantly associated with fewer teeth (β = −.05, 95% CI = −0.11 to −0.00, p < .05). As expected, older adults lost teeth over time (β = −.06, 95% CI = −0.06 to −0.05, p < .001, Model 2). After accounting for the effects of lifestyle and oral hygiene behaviour, physical and cognitive health, and loneliness in Models 3– 5, the coefficient estimates of the associations between social isolation with the number of remaining teeth remained substantively unchanged. In the final Model 6 that included the interaction between social isolation and time, we found that socially isolated participants had a higher rate of decline in the number of teeth over time (βinteraction = −.02, 95% CI = −0.02 to −0.01, p < .01). In contrast, findings in Table 3 show that the coefficient of loneliness with number of remaining teeth was not significant (β = −.01, 95% CI = −0.05 to 0.04, p = .83, Model 1). The insignificant associations remained after accounting for the effects of other factors in Models 3– 5. In the full Model 6, feeling lonely was neither related to the number of remaining teeth (β = .15, 95% CI = −0.01 to 0.30, p = .06), nor related to the rate of tooth loss (βinteraction = −.01, 95% CI = −0.02 to −0.00, p = .16).
TABLE 2.
Association of social isolation with the number of remaining teeth and rate of tooth loss over the 7-year follow-up (n = 4268)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |
|---|---|---|---|---|---|---|
| Parameter | β-coefficients (95% Cl) | |||||
| Social isolation (ref. No) | ||||||
| Yes | −.05 (−0.11, −0.00)* | −.06 (−0.11, −0.00)* | −.06 (−0.11, −0.01)* | −.06 (−0.11, 0.00)* | −.06 (−0.12, −0.01)* | −.06 (−0.13, −0.00)* |
| Time (in years) | −.06 (−0.06, −0.05)*** | −.06 (−0.06, −0.05)*** | −.05 (−0.06, −0.05)*** | −.05 (−0.06, −0.04)*** | −.05 (−0.05, −0.04)*** | |
| Smoking (ref. Never) | ||||||
| Former | −.01 (−0.06, 0.05) | −.03 (−0.12, 0.05) | −.03 (−0.12, 0.05) | −.03 (−0.11, 0.05) | ||
| Current | −.01 (−0.07, 0.05) | −.03 (−0.13, 0.07) | −.03 (−0.13, 0.07) | −.03 (−0.13, 0.07) | ||
| Drinking (ref. Never) | ||||||
| Former | −.02 (−0.07, 0.03) | −.00 (−0.09, 0.08) | −.00 (−0.09, 0.08) | −.01 (−0.09, 0.07) | ||
| Current | −.01 (−0.06, 0.04) | −.03 (−0.05, 0.11) | −.03 (−0.05, 0.11) | −.03 (−0.05, 0.11) | ||
| Toothbrushing frequency (ref. Never) | ||||||
| Less than once a day | .12 (0.06, 0.18)*** | .08 (0.02, 0.14)*** | .08 (0.02, 0.14)*** | .08 (0.02, 0.14)*** | ||
| Once a day | .16 (0.10,0.21)*** | .11 (0.02, 0.21)*** | .11 (0.02, 0.21)*** | .11 (0.02, 0.20)*** | ||
| More than once a day | .17 (0.10, 0.24)*** | .12 (0.01, 0.24)*** | .12 (0.01, 0.24)*** | .12 (0.01, 0.23)*** | ||
| Impaired activities of daily living (ref. No) | ||||||
| Yes | −.18 (−0.26, −0.09)** | −.18 (−0.26, −0.09)** | −.18 (−0.26, −0.09)** | |||
| Cognitive impairment (ref. No) | ||||||
| Yes | −.09 (−0.16, −0.02)*** | −.09 (−0.16, −0.02)*** | −.09 (−0.16, −0.02)*** | |||
| With one or more chronic conditions (ref. Without) | ||||||
| Yes | .01 (−0.06, 0.08) | .01 (−0.06, 0.08) | .01 (−0.06, 0.08) | |||
| Loneliness (ref. No) | ||||||
| Yes | .03 (−0.02, 0.09) | .03 (−0.02, 0.09) | ||||
| Social isolation ×Time | −.02 (−0.02, −0.01)** | |||||
| Covariates | ||||||
| Age | −.03 (−0.03, −0.03)*** | −.03 (−0.04, −0.03)*** | −.03 (−0.03, −0.03)*** | −.03 (−0.03, −0.02)*** | −.03 (−0.03, −0.02)*** | −.03 (−0.03, −0.02)*** |
| Women (ref. Men) | −.07 (−0.12, −0.03)** | −.07 (−0.12, −0.02)** | −.09 (−0.14, −0.03)** | −.06 (−0.12, −0.00)* | −.06 (−0.12, −0.00)* | −.06 (−0.12, −0.01)* |
| Current residence (ref. Urban areas) | ||||||
| Rural areas | −.02 (−0.09, 0.05) | −.01 (−0.08, 0.06) | .01 (−0.06, 0.08) | .01 (−0.06, 0.09) | .01 (−0.06, 0.09) | .01 (−0.06, 0.09) |
| Education level (ref. 0 year of schooling) | ||||||
| 1–6 years | .10 (0.04,0.15)*** | .10 (0.05, 0.15)*** | .08 (0.02, 0.13)** | .07 (0.02, 0.13)** | .08 (0.02, 0.13)** | .08 (0.02, .13)** |
| ≥6 years | .21 (0.14, 0.27)*** | .21 (0.14, 0.27)*** | .18 (0.12, 0.24)*** | .18 (0.11, 0.24)*** | .18 (0.11, 0.25)*** | .18 (0.11, 0.25)*** |
| Financial sufficiency (ref. Not enough) | ||||||
| Enough | −.03 (−0.09, 0.02) | −.03 (−0.08, 0.03) | −.02 (−0.08, 0.03) | −.01 (−0.07, 0.05) | −.02 (−0.07, 0.04) | −.02 (−0.07, 0.04) |
| Log-pseudolikelihood | −33623 | −33469 | −32823 | −31782 | −30918 | −30123 |
Note: CI, confidence interval; ref, reference group; β-coefficients are standardized regression coefficient derived from mixed-effects Poisson models.
Model 1 included only the effect of social isolation.
Model 2 introduce a random effect for time (in years) to estimate individual variability in slope estimates.
Models 3–5 added the effects of lifestyle and oral hygiene behaviour, physical and cognitive health, and loneliness.
Model 6 added a time by social isolation interaction to determine whether the rate of tooth loss varied by social isolation.
All models include sociodemographic characteristics as covariates (age, sex, area of current residence, education and financial sufficiency)
p < .05
p < .01
p < .001.
TABLE 3.
Association of loneliness with the number of remaining teeth and rate of tooth loss over the 7-year follow-up (n = 4268)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |
|---|---|---|---|---|---|---|
| Parameter | β-coefficients (95% Cl) | |||||
| Loneliness (ref. No) | ||||||
| Yes | −.01 (−0.05, −0.04) | −.00 (−0.05, 0.05) | .01 (−0.03, 0.06) | .01 (−0.04, 0.06) | .03 (−0.02, 0.09) | .15 (−0.01, 0.30) |
| Time (in years) | −.06 (−0.06, −0.05)*** | −.06 (−0.06, −0.05)*** | −.05 (−0.06, −0.05)*** | −.05 (−0.06, −0.05)*** | −.05 (−0.06, −0.04)*** | |
| Smoking (ref. Never) | ||||||
| Former | −.00 (−0.06, 0.05) | −.04 (−0.12, 0.04) | −.03 (−0.12, 0.05) | −.03 (−0.12, 0.05) | ||
| Current | −.00 (−0.06, 0.06) | −.01 (−0.11, 0.08) | −.03 (−0.13, 0.07) | −.03 (−0.13, 0.07) | ||
| Drinking (ref. Never) | ||||||
| Former | −.01 (−0.06, 0.04) | −.01 (−0.08, 0.07) | −.00 (−0.09, 0.08) | −.01 (−0.09, 0.08) | ||
| Current | −.01 (−0.04, 0.05) | .02 (−0.06, 0.10) | .03 (−0.05, 0.11) | .03 (−0.05, 0.11) | ||
| Toothbrushing frequency (ref. Never) | ||||||
| Less than once a day | .13 (0.07, 0.18)*** | .07 (0.01, 0.13)* | .07 (0.01, 0.13)* | .07 (0.01, 0.13)* | ||
| Once a day | .17 (0.12,0.22)*** | .14 (0.05, 0.23)** | .11 (0.02, 0.21)* | .11 (0.02, 0.21)* | ||
| More than once a day | .18 (0.11, 0.25)*** | .15 (0.04, 0.25)** | .12 (0.01, 0.24)* | .12 (0.01, 0.23)* | ||
| Impaired activities of daily living (ref. No) | ||||||
| Yes | −.18 (−0.26, −0.09)** | −.18 (−0.26, −0.09)** | −.18 (−0.26, −0.09)** | |||
| Cognitive impairment (ref. No) | ||||||
| Yes | −.09 (−0.16, −0.02)*** | −.09 (−0.16, −0.02)*** | −.09 (−0.16, −0.02)*** | |||
| With one or more chronic conditions (ref. Without) | ||||||
| Yes | .02 (−0.02, 0.06) | .02 (−0.02, 0.07) | .02 (−0.02, 0.07) | |||
| Social isolation (ref. No) | ||||||
| Yes | .06 (−0.11, −0.01)* | .06 (−0.11, −0.01)* | ||||
| Loneliness × Time | −.01 (−0.02, 0.00) | |||||
| Covariates | ||||||
| Age | −.03 (−0.03, −0.03)*** | −.03 (−0.04, −0.03)*** | −.03 (−0.03, −0.03)*** | −.03 (−0.03, −0.02)*** | −.03 (−0.03, −0.02)*** | −.03 (−0.03, −0.02)*** |
| Women (ref. Men) | −.09 (−0.13, −0.04)** | −.09 (−0.13, −0.04)** | −.09 (−0.15, −0.04)** | −.07 (−0.12, −0.02)* | −.06 (−0.12, −0.00)* | −.06 (−0.12, −0.01)* |
| Current residence (ref. Urban areas) | ||||||
| Rural areas | −.02 (−0.09, 0.05) | −.01 (−0.08, 0.06) | .01 (−0.06, 0.08) | .01 (−0.06, 0.09) | .01 (−0.06, 0.09) | .01 (−0.06, 0.09) |
| Education level (ref. 0 year of schooling) | ||||||
| 1–6 years | .11 (0.06, 0.16)*** | .11 (0.06, 0.16)*** | .09 (0.04, 0.14)** | .08 (0.03, 0.13)** | .08 (0.02, 0.13)** | .08 (0.02, .13)** |
| ≥6 years | .22 (0.16, 0.28)*** | .21 (0.15, 0.28)*** | .19 (0.13, 0.25)*** | .18 (0.12, 0.25)*** | .18 (0.11, 0.25)*** | .18 (0.11, 0.25)*** |
| Financial sufficiency (ref. Not enough) | ||||||
| Enough | −.03 (−0.08, 0.03) | −.03 (−0.09, 0.02) | −.03 (−0.08, 0.02) | −.01 (−0.07, 0.04) | −.02 (−0.07, 0.04) | −.02 (−0.07, 0.04) |
| Log-pseudolikelihood | −35726 | −35092 | −30756 | −29715 | −28187 | −26822 |
Note: See Table 2.
Formal mediation tests were conducted for lifestyle, oral hygiene behaviour, and physical and cognitive health using the KHB method. The results are presented in the Table A2. These analyses indicated mediating effects of smoking, drinking, toothbrushing frequency, impaired ADL and cognitive impairment on the association between social isolation and tooth loss (all p < .05). In comparison, the mediating effects of chronic conditions were not significant.
3.3 |. Sensitivity analyses
Sensitivity analyses were conducted to test potential biases by repeating the analysis when including participants who failed to follow- up or who had died. The coefficients for social isolation and loneliness were comparable with those in the main analysis (social isolation: β = −.06, 95% CI = −0.12 to −0.01, p < .05; loneliness: β = .12, 95% CI = −0.02 to 0.26, p = .06).
4 |. DISCUSSION
The purpose of this study was to examine the effects of social isolation and loneliness on the number of remaining teeth and the rate of tooth loss over a 7- year follow- up among Chinese older adults. The findings supported the first hypothesis, which stated that social isolation was associated with fewer teeth and accelerated tooth loss among Chinese older adults. On the contrary, the second hypothesis was not supported. Loneliness was neither associated with fewer teeth nor with the changes in the number of remaining teeth.
Previous studies conducted in the UK indicated that social isolation was associated with fewer teeth and poor self- rated oral health.13,14 Existing literature has provided several reasons to account for these associations. For example, compromised oral health is due to lower socioeconomic status induced by lack of access to and quality of dental care services, as well as isolation- related health- risk behaviour (eg smoking, drinking and infrequent toothbrushing).7,18,29 These behavioural pathways were also supported in the present study. An alternative explanation is that socially isolated Chinese older adults are less engaged in social activities and health- promoting activities (eg physical activity, spiritual growth and stress management),30 which could negatively affect oral health.19 In this study, we found that functional health was a major pathway linking social isolation and tooth loss. Socially isolated older adults were more vulnerable to functional disability, which may lead to infrequent oral hygiene behaviour, as well as greater risk of systemic inflammation.31,32 These behavioural and physiological changes have likewise been implicated in the aetiology of periodontitis,33 which might result in tooth loss.
In alignment with the social determinants of oral health framework,19 findings in this study indicated that social isolation, along with other risk factors such as smoking, drinking, infrequent toothbrushing, impaired physical function, cognitive impairment and lower education level, were regarded as risk factors for a higher number of teeth lost. However, further analyses showed that chronic conditions did not mediate the association between social isolation and tooth loss, suggesting that these factors are a part of the pathways, but not the only one, that leads to greater tooth loss. Although measured confounders were adjusted for, there may be residual confounding due to unmeasured covariates or imprecisely measured confounders. Finally, while statistical mediation implies mechanism, we were not able to trace the mechanisms using the current methods of statistical mediation34 and the available data. In this respect, given that chronic conditions are unlikely to be causally associated with poor oral health, these variables may serve as proxies for other unmeasured mediators (eg inflammation, oxidative stress).
In the present study, there was not an association between loneliness and tooth loss. This finding is inconsistent with a previous cross-sectional study that found loneliness was associated with decayed, missing and filled tooth index scores, periodontal disease and edentulousness.15 These discrepancies might be due to several reasons: different sample sizes, research designs, oral health measures and instruments for measuring loneliness. One distinct characteristic of the participants in this study is that the average age was 80.4, and centenarians (age ≥ 100 years) comprised 5.5% of our total participants. Previous research indicated that loneliness was less common with centenarians,35 and the robust oldest- old (age ≥ 85 years) adults have a greater capacity to buffer loneliness than youngest- or middle- old adults.36 Further studies with diverse populations at different age groups are warranted to clarify this issue.
The present study found a discrepancy in the associations of social isolation and loneliness with tooth loss. Based on a recently developed conceptual framework on ageing and oral health,37 health behaviours are the key to oral health. Previous studies suggest that social isolation may result in a lack of instrumental or emotional support that could affect health behaviours,11,17 and thus leads to compromised oral health.19 For older adults who feel lonely, social networks are still in place, and which can help them keep healthy behaviours.17 In fact, previous studies have found similar discrepancies for other health outcomes in Chinese older adults. For example, a 4- year cohort study found that social isolation, rather than loneliness, was associated with cognitive decline in Chinese older adults.10 Another longitudinal study indicated that socially isolated Chinese older adults with cardiovascular disease had an increased risk of mortality and that the association was independent of loneliness.12 Our results highlight the need to further examine the mechanisms between social isolation and oral health status.
To the best of our knowledge, this is the first study to examine the effect of social disconnection on oral health using data from a nationally representative cohort. Our study suggests that maintaining and improving social connections may benefit oral health among Chinese older adults. It is critical to developing interventions and programmes that promote intergenerational support within families and improve older adults’ peer and social connections within local communities. More research is needed to further examine the associations between social connections and oral conditions using longitudinal cohort and intervention studies.
This study has a few limitations. First, excluding individuals who failed to follow- up or had died may potentially lead to a selection bias. A sensitivity analysis was conducted by including individuals who failed to follow- up or who had died, and the results were similar to the primary findings. Second, both health status and the number of remaining teeth of participants were self-reported. Although self-reported data may be affected by recall bias and measurement error, evidence suggests that self-reported oral health indicators are valid and are strongly associated with objective clinical measures.38 Third, social isolation and loneliness may decrease the frequency of dental visits, especially among older adults. However, the measure on dental visits was not included in CLHLS. Although dental care utilization is relatively low among Chinese older adults, especially for the oldest old,3 future studies need to control for this variable. Forth, older adults’ oral health status (eg periodontal disease, dental caries) affects the number of teeth and the rate of tooth loss over time; however, these oral health measures were not included in CLHLS. Finally, lifestyle, oral hygiene behaviour and loneliness were all measured by only one single item. These measures may be less valid and reliable than composite scales.
5 |. CONCLUSIONS
This longitudinal study of community-d welling older adults aged ≥ 65 provides evidence of the effect of social isolation on tooth loss, with the association seemingly independent of loneliness, sociodemographic characteristics, lifestyle and oral hygiene behaviour, and health status. These findings expand our knowledge about the impact of social disconnection on tooth loss in Chinese older adults.
Supplementary Material
ACKNOWLEDGEMENT
This study is partially supported by the National Institutes of Health (R56AG067619 and U01DE027512).
Funding information
National Institute on Aging, Grant/Award Number: 1R56AG067619; National Institute of Dental and Craniofacial Research, Grant/Award Number: U01DE027512
Footnotes
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of the article at the publisher’s website.
CONFLICT OF INTEREST
Nothing to disclose.
DATA AVAILABILITY STATEMENT
The CLHLS datasets are publicly available at the National Archive of Computerized Data on Aging (ICPSR 36179). Researchers may obtain the datasets after sending a data user agreement to the CLHLS team. http://www.icpsr.umich.edu/icpsrweb/NACDA/studies/36179
REFERENCES
- 1.Peres MA, Macpherson LMD, Weyant RJ, et al. Oral diseases: a global public health challenge. The Lancet. 2019;394(10194):249–260. [DOI] [PubMed] [Google Scholar]
- 2.Dye BA, Tan S, Smith V, et al. Trends in oral health status: United States, 1988– 1994 and 1999– 2004. Vital Health Stat 11. 2007;(248):1–92. https://stacks.cdc.gov/view/cdc/6834 [PubMed] [Google Scholar]
- 3.Xu M, Cheng M, Gao X, et al. Factors associated with oral health service utilization among adults and older adults in China, 2015–2016. Community Dent Oral Epidemiol. 2020;48(1):32–41. [DOI] [PubMed] [Google Scholar]
- 4.Komiyama T, Ohi T, Tomata Y, et al. Dental status is associated with incident functional disability in community- dwelling older japanese: a prospective cohort study using propensity score matching. J Epidemiol. 2020;30(2):84–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kang J, Wu B, Bunce D, et al. Bidirectional relations between cognitive function and oral health in ageing persons: a longitudinal cohort study. Age Ageing. 2020;49(5):793–799. [DOI] [PubMed] [Google Scholar]
- 6.Cheng F, Zhang M, Wang Q, et al. Tooth loss and risk of cardiovascular disease and stroke: a dose- response meta analysis of prospective cohort studies. PLoS One. 2018;13(3):e0194563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Academies of Sciences, Engineering, and Medicine, ed. Social Isolation and Loneliness in Older Adults: Opportunitiies for the Health Care System. The National Academies Press. 2020. [PubMed] [Google Scholar]
- 8.Yang K, Victor CR. The prevalence of and risk factors for loneliness among older people in China. Ageing Soc. 2008;28(3):305–327. [Google Scholar]
- 9.Donovan NJ, Wu Q, Rentz DM, Sperling RA, Marshall GA, Loneliness GMM. depression and cognitive function in older U.S. adults: Loneliness, depression and cognition. Int J Geriatr Psychiatry. 2017;32(5):564–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yu B, Steptoe A, Chen Y, Jia X. Social isolation, rather than loneliness, is associated with cognitive decline in older adults: the China Health and Retirement Longitudinal Study. Psychol Med. 2021;2020:1–8. [DOI] [PubMed] [Google Scholar]
- 11.Steptoe A, Shankar A, Demakakos P, Wardle J. Social isolation, loneliness, and all- cause mortality in older men and women. Proc Natl Acad Sci. 2013;110(15):5797–5801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yu B, Steptoe A, Chen LJ, Chen YH, Lin CH, Ku PW. Social isolation, loneliness, and all- cause mortality in patients with cardiovascular disease: a 10- year follow- up study. Psychosom Med. 2020;82(2):208–214. [DOI] [PubMed] [Google Scholar]
- 13.Aminu AQ. Adult Dental Health Survey 2009: association between oral health outcomes and living arrangements of older adults in the UK. Br Dent J. 2019;227(2):115–120. [DOI] [PubMed] [Google Scholar]
- 14.McGrath C, Bedi R. Influences of social support on the oral health of older people in Britain. J Oral Rehabil. 2002;29(10):918–922. [DOI] [PubMed] [Google Scholar]
- 15.Singh A, Purohit BM, Taneja S. Loneliness and disability as predictors of oral diseases among 2 groups of older adults in central India. J Am Dent Assoc. 2020;151(6):427–437. [DOI] [PubMed] [Google Scholar]
- 16.Cacioppo JT, Cacioppo S. Social relationships and health: the toxic effects of perceived social isolation: social relationships and health. Soc Personal Psychol Compass. 2014;8(2):58–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kobayashi LC, Steptoe A. Social isolation, loneliness, and health behaviors at older ages: longitudinal cohort study. Ann Behav Med. 2018;52(7):582–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mathur MR, Tsakos G, Parmar P, Millett CJ, Watt RG. Socioeconomic inequalities and determinants of oral hygiene status among Urban Indian adolescents. Community Dent Oral Epidemiol. 2016;44(3):248–254. [DOI] [PubMed] [Google Scholar]
- 19.Watt RG, Sheiham A. Integrating the common risk factor approach into a social determinants framework. Community Dent Oral Epidemiol. 2012;40(4):289–296. [DOI] [PubMed] [Google Scholar]
- 20.Holt- Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta- analytic review. Perspect Psychol Sci. 2015;10(2):227–237. [DOI] [PubMed] [Google Scholar]
- 21.McHugh J, Kenny R, Lawlor B, Steptoe A, Kee F. The discrepancy between social isolation and loneliness as a clinically meaningful metric: findings from the Irish and English longitudinal studies of ageing (TILDA and ELSA): social asymmetry and cognitive function. Int J Geriatr Psychiatry. 2017;32(6):664–674. [DOI] [PubMed] [Google Scholar]
- 22.Cornwell EY, Waite LJ. Social disconnectedness, perceived isolation, and health among older adults. J Health Soc Behav. 2009;50(1):31–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zeng Y, Poston DL, Ashbaugh Vlosky D, Gu D, eds. Healthy Longevity in China: Demographic, Socioeconomic, and Psychological Dimensions. Springer; 2008. [Google Scholar]
- 24.Zhou Z, Wang P, Fang Y. Loneliness and the risk of dementia among older Chinese adults: gender differences. Aging Ment Health. 2018;22(4):519–525. [DOI] [PubMed] [Google Scholar]
- 25.Chen L, Zhou R. Does self- reported hearing difficulty decrease older adults’ cognitive and physical functioning? The mediating role of social isolation. Maturitas. 2020;141:53–58. [DOI] [PubMed] [Google Scholar]
- 26.Luo Y, Waite LJ. Loneliness and mortality among older adults in China. J Gerontol B Psychol Sci Soc Sci. 2014;69(4):633–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wu L. Mixed Effects Models for Complex Data. Chapman & Hall/CRC Press; 2010. [Google Scholar]
- 28.Karlson KB, Holm A. Decomposing primary and secondary effects: a new decomposition method. Res Soc Stratif Mobil. 2011;29(2):221–237. [Google Scholar]
- 29.Dyal SR, Valente TW. A systematic review of loneliness and smoking: small effects, Big Implications. Subst Use Misuse. 2015;50(13):1697–1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wu F, Sheng Y. Social isolation and health- promoting behaviors among older adults living with different health statuses: a cross- sectional study. Int J Nurs Sci. 2021;8(3):304–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cacioppo JT, Cacioppo S, Capitanio JP, Cole SW. The neuroendocrinology of social isolation. Annu Rev Psychol. 2015;66(1):733–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yang YC, McClintock MK, Kozloski M, Li T. Social isolation and adult mortality: the role of chronic inflammation and sex differences. J Health Soc Behav. 2013;54(2):183–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rosania AE, Low KG, McCormick CM, Rosania DA. Stress, depression, cortisol, and periodontal disease. J Periodontol. 2009;80(2):260–266. [DOI] [PubMed] [Google Scholar]
- 34.VanderWeele TJ. Mediation and mechanism. Eur J Epidemiol. 2009;24(5):217–224. [DOI] [PubMed] [Google Scholar]
- 35.Leitch S, Glue P, Gray AR, Greco P, Barak Y. Comparison of psychosocial variables associated with loneliness in centenarian vs elderly populations in New Zealand. JAMA Netw Open. 2018;1(6):e183880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ukraintseva S, Yashin AI, Arbeev KG. Resilience versus robustness in aging. J Gerontol A Biol Sci Med Sci. 2016;71(11):1533–1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wu B, Mao W, Qi X, Pei Y. Immigration and oral health in older adults: an integrative approach. J Dent Res. 2021;100(7):686–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Matsui D, Yamamoto T, Nishigaki M, et al. Validity of self- reported number of teeth and oral health variables. BMC Oral Health. 2017;17(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The CLHLS datasets are publicly available at the National Archive of Computerized Data on Aging (ICPSR 36179). Researchers may obtain the datasets after sending a data user agreement to the CLHLS team. http://www.icpsr.umich.edu/icpsrweb/NACDA/studies/36179