Abstract
In prediabetes, blood glucose levels are higher than normal; however, they remain below the diabetes threshold. Studies conducted on biomarkers for this disease result in controlling diabetes mellitus (DM) or reducing the risk of developing complications. Lipid profile parameters are considered important predictors of DM. Therefore, this study was conducted on three groups of normoglycemic (n=30), pre-diabetics (n=125), and diabetics (n=30) to recognize the predictive role of lipid parameters in the transition from pre-diabetes to diabetes. In this experiment, in addition to total cholesterol and triglycerides, very-low-density lipoprotein (VLDL), low-density lipoprotein (LDL), high-density lipoprotein (HDL), triglyceride/HDL ratio, and fasting triglyceride-fasting blood glucose (FBG) index were measured. Based on the results, medians for total cholesterol, LDL, HDL, LDL/HDL ratio, cholesterol/HDL ratio, and LDL/HDL ratio did not differ significantly across the groups of normoglycemia, prediabetes, and diabetes. For triglyceride, the medians were significantly higher in pre-diabetes and also diabetes, compared to normoglycemia (i.e., 127.9 and 129.1 vs. 94.5 mg/dL, respectively [P<0.001]). Moreover, the same results were observed in the case of VLDL (i.e., 25.6 and 30.9 vs. 18.9 mg/dL, respectively). The triglyceride/HDL ratio significantly increased pre-diabetics and diabetics, compared to normoglycemic (2.72 and 2.67 vs. 2.18, respectively). Moreover, the median of the triglyceride-FBG index significantly had an increase in pre-diabetics and diabetics, compared to normoglycemic (8.89 and 9.38 vs. 8.22, respectively). The importance of triglyceride, VLDL, triglyceride/HDL ratio, and triglyceride-FBG index in distinguishing between pre-diabetes and normoglycemia was verified by a receiver operating characteristic curve analysis of the results. Logistic regression analysis confirmed the risk effects of the four parameters on pre-diabetes and diabetes. Therefore, triglyceride, VLDL, triglyceride-FBG index, and triglyceride/HDL ratio are considered promising biomarkers used to predict pre-diabetes and DM in the general population.
Keywords: Pre-diabetes; Diabetes; Normoglycemia, Lipid profile; Triglyceride-glucose index; Triglyceride/high-density lipoprotein ratio
1. Introduction
Type 2 diabetes mellitus (T2DM) is recognized as a public health concern with a major impact on the overall quality of life and human health. The overall economic development and urbanization in lifestyle increase the burden of disease in various parts of the world, such as Iraq ( 1 , 2 ). The problem is further complicated by comorbidities of the cardiovascular system as T2DM patients are more susceptible to coronary artery disease, linked to increased mortality rates among these patients ( 3 , 4 ). In this context, two major modifiable risk factors of T2DM are investigated which include dyslipidemia and hypertension with both factors accounting for two-thirds of the disability among T2DM patients worldwide ( 5 ). Diabetic dyslipidemia, defined by the American Diabetes Association, is used to describe dysregulated levels of lipids in patients with type 2 diabetes (T2DM), including total cholesterol, triglyceride, very-low-density lipoprotein (VLDL), low-density lipoprotein (LDL), and high-density lipoprotein (HDL) ( 6 ). Abnormal levels of these lipid parameters increase the particular concern due to their complex clinical implications in T2DM patients ( 7 ). In the case of pre-diabetes, a transition metabolic state from normoglycemia to T2DM leads to an increased risk of cardiovascular disease ( 8 ), and the patients have abnormalities in the lipid profile. However, the correlation among pre-diabetes, T2DM, and lipids may be subjected to ethnic differences, depending on the patient's nutritional status, environment, and lifestyle ( 9 ). Furthermore, some studies revealed the predictive significance of lipid parameters in the outcome of pre-diabetes ( 10 , 11 ). A fasting triglyceride-fasting blood glucose (FBG) index was investigated to help predict insulin resistance and cardiovascular illness in people with type 2 diabetes ( 4 ). Therefore, this study was conducted on three groups of Iraqi individuals, including normoglycemic, pre-diabetics, and diabetics (T2DM) to understand the predictive role of lipid parameters in the transition from pre-diabetes to diabetes.
2. Materials and Methods
2.1. Populations Studied
This prospective study was conducted on three different groups of people including 30 apparently healthy individuals, normoglycemia, (42.5±12.9 years; 50% males), 125 pre-diabetics (47.2±11.1 years; 53.6% males), and 30 T2DM patients (49.8±13.1 years; 50% males) from December 2020 to May 2021. The normoglycemia, pre-diabetes, and diabetes were defined according to the American Diabetes Association criteria, based on assessing FBG less than 100, between 100 and 125, and ≥ 126 mg/dL, respectively, as well as glycated hemoglobin (HbA1c: less than 5.7, between 5.7 and 6.4, and ≥ 6.5%, respectively) ( 12 ). Only people who met these criteria were included in this study; in addition to pregnant women with gestational diabetes, smokers, alcoholics, and patients with cardiovascular and kidney diseases and hepatic failure were excluded from the study.
2.2. Laboratory Methods
Blood samples were collected by a vein puncture after 10-12 h of fasting, and the blood sample (5 mL) was split into two aliquots for further testing and analysis. The first aliquot (2 mL) was dispensed into a tube containing ethylene-diamine tetra-acetic acid (EDTA), removed from the tube (EDTA), and then processed in less than three hours and utilized for HbAlc measurement in the same manner as stated earlier. The second aliquot (remaining blood [3 mL]) was transferred to a plain tube, and after clotting, the tube was centrifuged (3000 rpm for 15 min) to gather serum and assess for FBG, total cholesterol, triglyceride, VLDL, LDL, and HDL using Cobas c 311 analyzer (Cobas-Roche, Germany) preloaded with the respective reagent kits. In addition, two related indices were assessed, including triglyceride-FBG index and triglyceride/HDL ratio. The former index is computed using the following equation: ln [fasting triglycerides (mg/dl) FBG (mg/dl)/2] ( 13 ).
2.3. Statistical Analysis
All non-parametric variables (including skewed variables) were represented as the median and interquartile range (IQR: 25%-75%) and a significant difference between medians was determined using the Kruskal-Wallis test, followed by the Mann-Whitney U test, respectively. The prognostic relevance of total cholesterol, triglyceride, VLDL, LDL, and HDL in prediabetes and diabetes was determined using receiver operating characteristic (ROC) curve analysis. The area under the curve (AUC), 95% confidence interval (CI), cut-off value, sensitivity, and specificity were all used to assess the significance. To estimate the odds ratio (OR) and 95% CI, the participants were distributed into two groups according to the median of total cholesterol, triglyceride, VLDL, LDL, and HDL (> and ≤ median), and then logistic regression analysis was conducted. A P-value of ≤0.05 was considered statistically significant. The statistical analysis was conducted using the IBM SPSS software (version 25; Armonk, NY: IBM Corp).
3. Results
3.1. Fasting Blood Glucose and Glycated Hemoglobin
Medians of FBG and Hb1Ac were significantly elevated in pre-diabetes (106.6 [IQR:103.7%-112.5%] mg/dL and 5.90 [IQR: 5.80%-6.20%], respectively; P<0.001) and diabetes (157.14 [IQR: 133.0%-181.2%] mg/dL and 7.05 [IQR: 6.70%-8.11%], respectively; P<0.001), compared to normoglycemia (80.2 [IQR: 77.1%-86.1%] mg/dL and 4.50 [4.10%-4.70%], respectively). Both medians were also significantly increased in diabetes, compared to prediabetes (P<0.001) (Figure 1).
Figure 1.
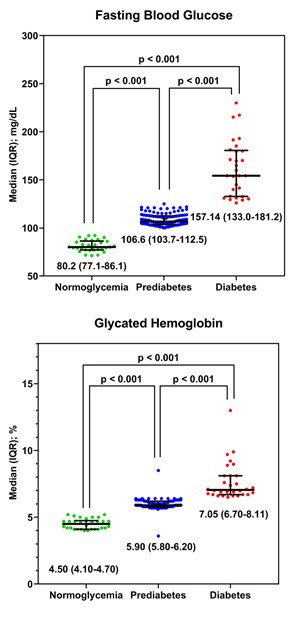
Median levels of fasting blood glucose and glycated hemoglobin in normoglycemic, prediabetics, and diabetics
3.2. Serum Profile of Lipids
As indicated in table 1, no significant change was in total cholesterol, LDL, HDL, LDL/HDL, and cholesterol/HDL ratio among the groups of normoglycemia, pre-diabetes, and diabetes. For triglyceride, the medians were significantly higher in pre-diabetes and diabetes than normoglycemia (i.e., 127.9 [IQR: 104.4%-190.9%] and 129.1 [IQR: 95.5%-192.7%] vs. 94.5 [IQR: 76.5%-100.5%] mg/dL, respectively; P<0.001). A similar observation was also made in the case of VLDL (25.6 [IQR: 20.9%-36.8%] and 30.9 [IQR: 22.7%-42.1%] vs. 18.9 [IQR: 15.2%-20.1%] mg/dL, respectively; P<0.001). Moreover, the triglyceride/HDL ratio was significantly increased in pre-diabetics (2.72 [IQR: 2.16%-4.03%]) and diabetics (2.67 [IQR: 1.73%-4.14%]), compared to normoglycemic (2.18 [IQR: 1.63%-2.55%]; P=0.003), while no considerable difference was between pre-diabetics and diabetics. In addition, a significantly increased median of the triglyceride-FBG index was in pre-diabetics (8.89 [IQR: 8.65%-9.20%]) and diabetics (9.38 [IQR: 9.05%-9.57%]), compared to normoglycemic (8.22 [8.03%-8.31%]; P<0.001), and this increase was more obvious in diabetics with a significant difference, compared to pre-diabetics (Table 1).
Table 1.
Lipid profile parameters in normoglycemic, pre-diabetics, and diabetics
| Variable | Median (IQR: 25%-75%) | P-value | ||
|---|---|---|---|---|
| Normoglycemia (n=30) | Pre-diabetes (n=125) | Diabetes (n=30) | ||
| Total cholesterol (mg/dL) | 176.6 (166.5-188.7)A | 182.1 (160.9-221.5)A | 182.9 (164.0-227.7)A | 0.262 |
| Triglyceride (mg/dL) | 94.5 (76.5-100.5)A | 127.9 (104.4-190.9)B | 129.1 (95.5-192.7)B | < 0.001 |
| VLDL (mg/dL) | 18.9 (15.2-20.1)A | 25.6 (20.9-36.8)B | 30.9 (22.7-42.1)B | < 0.001 |
| LDL (mg/dL) | 111.4 (102.2-120.3)A | 112.0 (83.1-133.9)A | 107.9 (74.9-151.9)A | 0.956 |
| HDL (mg/dL) | 40.1 (38.8-55.2)A | 46.3 (39.5-56.4)A | 51.7 (43.8-57.9)A | 0.162 |
| LDL/HDL ratio | 2.8 (1.9-2.9)A | 2.3 (1.7-3.1)A | 2.1 (1.6-3.3)A | 0.714 |
| Cholesterol/HDL ratio | 4.2 (3.1-4.5)A | 3.9 (3.2-4.7)A | 3.9 (3.1-5.0)A | 0.991 |
| Triglyceride/HDL ratio | 2.18 (1.63-2.55)A | 2.72 (2.16-4.03)B | 2.67(1.73-4.14)B | 0.003 |
| Triglycerides-FBG index | 8.22 (8.03-8.31)A | 8.89 (8.65-9.20)B | 9.38 (9.05-9.57)C | < 0.001 |
Similar letters indicate no significant difference among medians in rows (P-value>0.05).
Different letters indicate a significant difference among medians in rows (P-value≤0.05).
3.3. ROC Curve Analysis
ROC curve analysis demonstrated the significance of triglyceride, VLDL, triglyceride/HDL ratio and triglyceride-FBG index among normoglycemia and prediabetes or diabetes. In the case of triglyceride, the calculated AUCs were 0.822 (95% CI: 0.756-0.888; P<0.001; cut-off value=100.1 mg/dL; sensitivity=76.7%; specificity=76.7%) and 0.783 (95% CI: 0.656-0.911; P<0.001; cut-off value=100.1 mg/dL; sensitivity=73.3%; specificity=73.3%) in pre-diabetes and diabetes, respectively. Higher AUCs with better sensitivity and specificity were associated with VLDL. In pre-diabetes vs. normoglycemia, the AUC was 0.823 (95% CI: 0.756-0.889; P<0.001; cut-off value=20.3 mg/dL; sensitivity=78.4%; specificity=76.7%) and in diabetes vs. normoglycemia was 0.824 (95% CI: 0.704-0.945; P<0.001; cut-off value=20.7 mg/dL; sensitivity=80.0%; specificity=80.0%). However, significantly better AUC values were recorded for the triglyceride-FBG index, which were 0.924 and 0.978 in pre-diabetes and diabetes, respectively, with the sensitivity and specificity improved and exceeded 86% (Tables 2 and 3; Figures 2 and 3).
Table 2.
Receiver operating characteristic curve analysis of triglyceride and VLDL in pre-diabetes
| Variable | AUC | 95% CI | P-value | Cut-off value | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|---|---|
| Triglyceride | 0.822 | 0.756-0.888 | < 0.001 | 100.1 mg/dL | 76.7 | 76.7 |
| VLDL | 0.823 | 0.756-0.889 | < 0.001 | 20.3 mg/dL | 78.4 | 76.7 |
| Triglyceride/HDL ratio | 0.708 | 0.624-0.791 | < 0.001 | 2.40 | 63.2 | 63.3 |
| Triglyceride-FBG index | 0.924 | 0.883-0.966 | < 0.001 | 8.39 | 88.8 | 86.7 |
Table 3.
Receiver operating characteristic curve analysis of triglycerides and VLDL in diabetes
| Variable | AUC | 95% CI | P-value | Cut-off value | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|---|---|
| Triglyceride | 0.783 | 0.656-0.911 | < 0.001 | 100.1 mg/dL | 73.3 | 73.3 |
| VLDL | 0.824 | 0.704-0.945 | < 0.001 | 20.7 mg/dL | 80.0 | 80.0 |
| Triglyceride/HDL ratio | 0.637 | 0.487-0.786 | 0.069 | 2.30 | 53.3 | 53.3 |
| Triglyceride-FBG index | 0.978 | 0.946-1.000 | < 0.001 | 8.47 | 90.0 | 90.0 |
Figure 2.
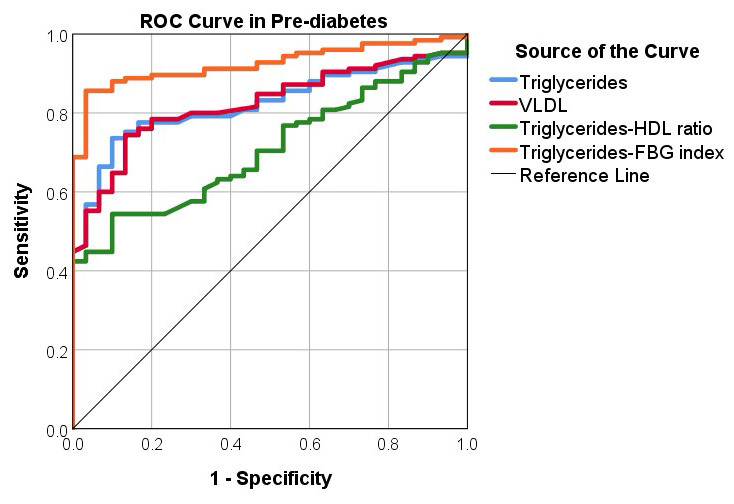
Receiver operating characteristic curve analysis of triglyceride, VLDL, triglyceride/HDL ratio, and triglyceride-FBG index in pre-diabetes (Data from Table 2)
Figure 3.

Receiver operating characteristic curve analysis of triglyceride, VLDL, triglyceride/HDL ratio, and triglyceride-FBG index in diabetes (Data from Table 3)
3.4. Logistic Regression Analysis
Triglyceride and VLDL were linked to an increased chance of developing pre-diabetes or diabetes, according to a logistic regression study (Tables 4 and 5). The interest of the current study was the association of pre-diabetes, increased levels of triglycerides, and VLDL with ORs of 19.02 (95% CI: 4.44-81.41; P<0.001) and 17.82 (95% CI: 4.16-76.24; P<0.001), respectively. However, considering the triglyceride-FBG index leading to an increased risk of pre-diabetes and diabetes development, the estimated ORs were 32.44 (95% CI:4.43-237.54; P<0.001) and 188.50 (95% CI: 20.55-1729.43; P< 0.001), respectively.
Table 4.
Logistic regression analysis of triglyceride and VLDL in prediabetes vs. normoglycemia
| Variable | Normoglycemia (n=30) | Pre-diabetes (n=125) | OR (95% CI) | P-value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| > Median | ≤ Median | > Median | ≤ Median | |||||||
| N | % | N | % | N | % | N | % | |||
| Triglyceride | 2 | 6.7 | 28 | 93.3 | 72 | 57.6 | 53 | 42.4 | 19.02 (4.44-81.41) | < 0.001 |
| VLDL | 2 | 6.7 | 28 | 93.3 | 70 | 56.0 | 55 | 44.0 | 17.82 (4.16-76.24) | < 0.001 |
| Triglyceride/HDL ratio | 7 | 23.3 | 23 | 76.7 | 68 | 54.4 | 57 | 45.6 | 3.92 (1.59-9.67) | 0.002 |
| Triglyceride-FBG index | 1 | 3.3 | 29 | 96.7 | 66 | 52.8 | 59 | 47.2 | 32.44 (4.43-237.54) | < 0.001 |
Table 5.
Logistic regression analysis of triglyceride and VLDL in diabetes vs. normoglycemia
| Variable | Normoglycemia (n=30) | Diabetes (n=30) | OR (95% CI) | P-value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| > Median | ≤ Median | > Median | ≤ Median | |||||||
| N | % | N | % | N | % | N | % | |||
| Triglyceride | 2 | 6.7 | 28 | 93.3 | 17 | 56.7 | 13 | 43.3 | 18.31 (3.77-88.80) | < 0.001 |
| VLDL | 2 | 6.7 | 28 | 93.3 | 20 | 66.7 | 10 | 33.3 | 28.00 (5.68-138.09) | < 0.001 |
| Triglyceride/HDL ratio | 7 | 23.3 | 23 | 76.7 | 15 | 50.0 | 15 | 50.0 | 3.29 (1.11-9.77) | 0.060 |
| Triglyceride-FBG index | 1 | 3.3 | 29 | 96.7 | 26 | 86.7 | 4 | 13.3 | 188.50 (20.55-1729.43) | < 0.001 |
3.5. Correlation Analysis
The correlation between triglyceride-FBG index and triglyceride/HDL ratio was analyzed in normoglycemic, pre-diabetics, and diabetics using Spearman's rank correlation test, showing a significant positive correlation between the two parameters in the three groups, while the correlation coefficient (rs) showed different values. The highest rs was recorded in pre-diabetics (rs=0.882; P<0.001), followed by normoglycemic (rs=0.768; P<0.001) and diabetics (rs=0.162; P<0.001) (Figure 4).
Figure 4.

Spearman's rank correlation analysis between the triglyceride-FBG index and triglyceride/HDL ratio
4. Discussion
Based on the results, triglyceride and VLDL are two key lipid markers, which can identify pre-diabetes using ROC curve analysis, and are also linked to an increased risk of diabetes using logistic regression analysis. Pre-diabetics and diabetics had considerably higher levels of both measures in their blood. Furthermore, triglyceride in the triglyceride-FBG index leads to a predictive significance in distinguishing pre-diabetes and normoglycemia that recorded an AUC of 0.924, associated with a 32.44-folds raised risk of progressing pre-diabetes with the higher risk among diabetic patients (OR=188.50). Therefore, triglyceride, alone or incorporated in the triglyceride-FBG index, is considered a significant predictor of prediabetes and diabetes. In line with these findings, previous studies also revealed that triglyceride had elevated levels in prediabetics and T2DM patients, and their positive association with the risk of developing cardiovascular diseases was markedly recognized ( 14 - 16 ). Additionally, a link between high serum levels of triglyceride and over-secretion of insulin in apparently healthy individuals has been reported ( 17 , 18 ). Hypertriglyceridemia may have a causal relationship with insulin resistance, and reducing levels of triglyceride serum in the individuals with hypertriglyceridemia was associated with a decline in the levels of serum insulin and low incidence of T2DM ( 19 , 20 ). Therefore, changes in the levels of triglyceride were paralleled by changes in T2DM incidence, and a 4% elevated risk may accompany every 10 mg/dL increase in the triglyceride ( 21 ). Furthermore, hypertriglyceridemia was linked to increased mortality rates in T2DM patients due to cardiovascular diseases ( 22 ).
The current study also indicated that assessing the triglyceride-FBG index may be more important in predicting pre-diabetes and diabetes than triglyceride alone since this index is closely related to diabetes to recognize early insulin resistance without measuring insulin ( 23 ). Insulin resistance is considered a condition with an impaired biological response to insulin stimulation, resulting in reducing the disposal of glucose and hyperinsulinemia ( 24 ). Hyperglycemia, visceral adiposity hypertension, dyslipidemia, and up-regulated levels of inflammatory markers are all metabolic repercussions of insulin resistance, linked to an elevated risk of T2DM and cardiovascular disease ( 25 , 26 ). Impaired fasting glucose and/or glucose tolerance are observed in pre-diabetics, and lifestyle changes can lower the progression of prediabetes to diabetes by around 58% in three years ( 27 ). Moreover, insulin resistance can also drive some pathological events related to lipid deposition within insulin-responsive tissues (i.e. liver, viscera, and skeletal muscles) of prediabetics, leading to the low-grade type of inflammation and T2DM ( 28 ), and insulin resistance is also linked to high levels of VLDL ( 5 , 29 ). According to the results, VLDL levels were significantly elevated in pre-diabetics and diabetics, particularly in diabetics. A further study also confirmed that the VLDL was more up-regulated in the serum of diabetics than pre-diabetics; however, the levels were significantly higher in both groups than controls ( 30 ). Therefore, the lipid profile as a significant risk factor is highlighted in all T2DM follow-up programs virtually.
However, the triglyceride-FBG index and the triglyceride/HDL ratio were elevated in the serum of pre-diabetics and diabetics, compared to normoglycemia, the difference was only significant in pre-diabetics. This ratio is also known as the atherogenic index that is one of the most important risk factors for cardiovascular disease ( 31 ). A higher ratio of triglyceride/HDL is associated with endothelial dysfunction, proposed as a good marker of predicting insulin resistance ( 32 , 33 ). Regarding the results, this ratio can also be useful in monitoring glycemic control and identifying the risk of cardiovascular diseases in asymptomatic T2DM subjects ( 34 ). In Chinese cohort research, the triglyceride/HDL ratio substantially correlates with incident T2DM ( 35 ).
Therefore, triglyceride, VLDL, triglyceride-FBG index, and triglyceride/HDL ratio are considered promising biomarkers used to predict pre-diabetes and T2DM generally.
Authors' Contribution
Study concept and design: O. H. J. and M. M. M.
Ad’hiah, A. H
Acquisition of data: M. M. M.
Analysis and interpretation of data: O. H. J.
Drafting of the manuscript: A. H. A.
Critical revision of the manuscript for important intellectual content: O. H. J. and M. M. M.
Statistical analysis: O. H. J. and M. M. M.
Administrative, technical, and material support: O. H. J. and M. M. M.
Ethics
All studies were performed in compliance with the rules of humane treatment of Mustansiriyah University, Baghdad, Iraq.
Conflict of Interest
The authors declare that they have no conflict of interest.
Acknowledgment
The authors would like to thank the Biology Department, College of Science, Al-Mustansiriyah University (www.uomustansiriyah.edu.Iq) Baghdad, Iraq, and the University of Baghdad Baghdad, Iraq.
References
- 1.Abusaib M, Ahmed M, Nwayyir HA, Alidrisi HA, Al-Abbood M, Al-Bayati A, et al. Iraqi Experts Consensus on the Management of Type 2 Diabetes/Prediabetes in Adults. Clin Med Insights Endocrinol Diabetes. 2020;13:1179551420942232. doi: 10.1177/1179551420942232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Onyango EM, Onyango BM. The Rise of Noncommunicable Diseases in Kenya: An Examination of the Time Trends and Contribution of the Changes in Diet and Physical Inactivity. J Epidemiol Glob Health. 2018;8(1-2):1–7. doi: 10.2991/j.jegh.2017.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cui J, Liu Y, Li Y, Xu F, Liu Y. Type 2 Diabetes and Myocardial Infarction: Recent Clinical Evidence and Perspective. Front Cardiovasc Med. 2021;8:644189. doi: 10.3389/fcvm.2021.644189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sarría-Santamera A, Orazumbekova B, Maulenkul T, Salustri A, Glushkova N, Makashev D, et al. Macrovascular Complications in Patients with Diabetes Mellitus: Incidence and Impact on Survival in Kazakhstan. Res Sq. 2021 [Google Scholar]
- 5.Hirano T. Pathophysiology of Diabetic Dyslipidemia. J Atheroscler Thromb. 2018;25(9):771–82. doi: 10.5551/jat.RV17023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu L, Parhofer KG. Diabetic dyslipidemia. Metab Clin Exp. 2014;63(12):1469–79. doi: 10.1016/j.metabol.2014.08.010. [DOI] [PubMed] [Google Scholar]
- 7.Bhowmik B, Siddiquee T, Mujumder A, Afsana F, Ahmed T, Mdala IA, et al. Serum Lipid Profile and Its Association with Diabetes and Prediabetes in a Rural Bangladeshi Population. Int J Environ Res Public Health. 2018;15(9) doi: 10.3390/ijerph15091944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rijkelijkhuizen JM, Nijpels G, Heine RJ, Bouter LM, Stehouwer CD, Dekker JM. High risk of cardiovascular mortality in individuals with impaired fasting glucose is explained by conversion to diabetes: the Hoorn study. Diabetes Care. 2007;30(2):332–6. doi: 10.2337/dc06-1238. [DOI] [PubMed] [Google Scholar]
- 9.Mooradian AD. Dyslipidemia in type 2 diabetes mellitus. Nat Clin Pract Endocrinol Metab. 2009;5(3):150–9. doi: 10.1038/ncpendmet1066. [DOI] [PubMed] [Google Scholar]
- 10.Santos-Gallego CG, Rosenson RS. Role of HDL in those with diabetes. Curr Cardiol Rep. 2014;16(8) doi: 10.1007/s11886-014-0512-5. [DOI] [PubMed] [Google Scholar]
- 11.Wang L, Cong HL, Zhang JX, Hu YC, Wei A, Zhang YY, et al. Triglyceride-glucose index predicts adverse cardiovascular events in patients with diabetes and acute coronary syndrome. Cardiovasc Diabetol. 2020;19(1):80. doi: 10.1186/s12933-020-01054-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Association AD. Standards of Medical Care in Diabetes-2016: Summary of Revisions. Diabetes Care. 2016;39 (1):S4–5. doi: 10.2337/dc16-S003. [DOI] [PubMed] [Google Scholar]
- 13.Guerrero-Romero F, Simental-Mendia LE, Gonzalez-Ortiz M, Martinez-Abundis E, Ramos-Zavala MG, Hernandez-Gonzalez SO, et al. The product of triglycerides and glucose, a simple measure of insulin sensitivity. Comparison with the euglycemic-hyperinsulinemic clamp. J Clin Endocrinol Metab. 2010;95(7):3347–51. doi: 10.1210/jc.2010-0288. [DOI] [PubMed] [Google Scholar]
- 14.Alexopoulos AS, Qamar A, Hutchins K, Crowley MJ, Batch BC, Guyton JR. Triglycerides: Emerging Targets in Diabetes Care? Review of Moderate Hypertriglyceridemia in Diabetes. Curr Diab Rep. 2019;19(4):13. doi: 10.1007/s11892-019-1136-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nichols GA, Philip S, Reynolds K, Granowitz CB, Fazio S. Increased Cardiovascular Risk in Hypertriglyceridemic Patients With Statin-Controlled LDL Cholesterol. J Clin Endocrinol Metab. 2018;103(8):3019–27. doi: 10.1210/jc.2018-00470. [DOI] [PubMed] [Google Scholar]
- 16.Upadhyay RK. Emerging risk biomarkers in cardiovascular diseases and disorders. J Lipids. 2015;2015:971453. doi: 10.1155/2015/971453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aarsland A, Chinkes D, Wolfe RR. Contributions of de novo synthesis of fatty acids to total VLDL-triglyceride secretion during prolonged hyperglycemia/hyperinsulinemia in normal man. J Clin Invest. 1996;98(9):2008–17. doi: 10.1172/JCI119005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McLaughlin T, Abbasi F, Lamendola C, Yeni-Komshian H, Reaven G. Carbohydrate-induced hypertriglyceridemia: an insight into the link between plasma insulin and triglyceride concentrations. J Clin Endocrinol Metab. 2000;85(9):3085–8. doi: 10.1210/jcem.85.9.6838. [DOI] [PubMed] [Google Scholar]
- 19.Cheal KL, Abbasi F, Lamendola C, McLaughlin T, Reaven GM, Ford ES. Relationship to insulin resistance of the adult treatment panel III diagnostic criteria for identification of the metabolic syndrome. Diabetes. 2004;53(5):1195–200. doi: 10.2337/diabetes.53.5.1195. [DOI] [PubMed] [Google Scholar]
- 20.Lee SJ, Moye LA, Campos H, Williams GH, Sacks FM. Hypertriglyceridemia but not diabetes status is associated with VLDL containing apolipoprotein CIII in patients with coronary heart disease. Atherosclerosis. 2003;167(2):293–302. doi: 10.1016/s0021-9150(03)00007-8. [DOI] [PubMed] [Google Scholar]
- 21.Tirosh A, Shai I, Bitzur R, Kochba I, Tekes-Manova D, Israeli E, et al. Changes in triglyceride levels over time and risk of type 2 diabetes in young men. Diabetes Care. 2008;31(10):2032–7. doi: 10.2337/dc08-0825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Emerging Risk Factors C, Di Angelantonio E, Sarwar N, Perry P, Kaptoge S, Ray KK, et al. Major lipids, apolipoproteins, and risk of vascular disease. JAMA. 2009;302(18):1993–2000. doi: 10.1001/jama.2009.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lim J, Kim J, Koo SH, Kwon GC. Comparison of triglyceride glucose index, and related parameters to predict insulin resistance in Korean adults: An analysis of the 2007-2010 Korean National Health and Nutrition Examination Survey. PLoS One. 2019;14(3):0212963. doi: 10.1371/journal.pone.0212963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cerf ME. Beta cell dysfunction and insulin resistance. Front Endocrinol (Lausanne) 2013;4:37. doi: 10.3389/fendo.2013.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gast KB, Tjeerdema N, Stijnen T, Smit JW, Dekkers OM. Insulin resistance and risk of incident cardiovascular events in adults without diabetes: meta-analysis. PLoS One. 2012;7(12):e52036. doi: 10.1371/journal.pone.0052036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xia C, Li R, Zhang S, Gong L, Ren W, Wang Z, et al. Lipid accumulation product is a powerful index for recognizing insulin resistance in non-diabetic individuals. Eur J Clin Nutr. 2012;66(9):1035–8. doi: 10.1038/ejcn.2012.83. [DOI] [PubMed] [Google Scholar]
- 27.Tuso P. Prediabetes and lifestyle modification: time to prevent a preventable disease. Perm J. 2014;18(3):88–93. doi: 10.7812/TPP/14-002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reaven G. The metabolic syndrome or the insulin resistance syndrome? Different names, different concepts, and different goals. Endocrinol Metab Clin North Am. 2004;33(2):283–303. doi: 10.1016/j.ecl.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 29.Pihlajamaki J, Gylling H, Miettinen TA, Laakso M. Insulin resistance is associated with increased cholesterol synthesis and decreased cholesterol absorption in normoglycemic men. J Lipid Res. 2004;45(3):507–12. doi: 10.1194/jlr.M300368-JLR200. [DOI] [PubMed] [Google Scholar]
- 30.Kansal S, Kamble TK. Lipid Profile in Prediabetes. J Assoc Physicians India. 2016;64(3):18–21. [PubMed] [Google Scholar]
- 31.Dobiás̆ová M, Frohlich J. The plasma parameter log (TG/HDL-C) as an atherogenic index: correlation with lipoprotein particle size and esterification rate inapob-lipoprotein-depleted plasma (FERHDL) Clin Biochem. 2001;34(7):583–8. doi: 10.1016/s0009-9120(01)00263-6. [DOI] [PubMed] [Google Scholar]
- 32.González-Chávez A, Simental-Mendía LE, Elizondo-Argueta S. Elevated triglycerides/HDL-cholesterol ratio associated with insulin resistance. Cir Cir. 2011;79(2):126–31. [PubMed] [Google Scholar]
- 33.Keles N, Aksu F, Aciksari G, Yilmaz Y, Demircioglu K, Kostek O, et al. Is triglyceride/HDL ratio a reliable screening test for assessment of atherosclerotic risk in patients with chronic inflammatory disease? . North Clin Istanb. 2016;3(1):39–45. doi: 10.14744/nci.2016.52824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Babic N, Valjevac A, Zaciragic A, Avdagic N, Zukic S, Hasic S. The Triglyceride/HDL Ratio and Triglyceride Glucose Index as Predictors of Glycemic Control in Patients with Diabetes Mellitus Type 2. Med Arch. 2019;73(3):163–8. doi: 10.5455/medarh.2019.73.163-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen Z, Hu H, Chen M, Luo X, Yao W, Liang Q, et al. Association of Triglyceride to high-density lipoprotein cholesterol ratio and incident of diabetes mellitus: a secondary retrospective analysis based on a Chinese cohort study. Lipids Health Dis. 2020;19(1):33. doi: 10.1186/s12944-020-01213-x. [DOI] [PMC free article] [PubMed] [Google Scholar]