Abstract
Pulmonary arterial hypertension (PAH) is a progressively life‐threatening disease that causes right heart failure (RHF). Renal dysfunction frequently complicates PAH with RHF and is associated with a worse prognosis. Renal replacement therapy (RRT) may be a therapeutic option, although its efficacy and safety are unclear. We describe a 30‐year‐old male with severe PAH who developed renal insufficiency and diuretic‐refractory volume overload complicated with RHF but was successfully managed with intermittent RRT via a subcutaneously fixed superficial artery for 4 years. RRT led to haemodynamic stability, which enabled us to carefully de‐titrate parenteral PAH drugs without worsening RHF. This case highlights that RRT may be a potential alternative for haemodynamic and volume control of refractory fluid retention complicated with RHF in severe PAH cases. Further studies are warranted to gain more insight into patient selection and the optimal timing of RRT in PAH patients with deteriorating RHF.
Keywords: Pulmonary arterial hypertension, Right heart failure, Volume overload, Acute kidney injury, Renal replacement therapy
Introduction
Pulmonary arterial hypertension (PAH) is a progressive, life‐threatening disease affecting small pulmonary arteries with proliferations of vascular endothelial and smooth muscle cells, leading to elevated pulmonary arterial resistance and right heart failure (RHF). 1 Acute kidney injury (AKI) is a frequent complication of PAH with RHF and is associated with a worse prognosis. 2 Proposed mechanisms of AKI include venous congestion, decreased cardiac output and subsequent regional blood flow, and neurohormonal modifications. 3 Moreover, even subtle renal deterioration can result in worse haemodynamics and an increased risk of mortality. 4 Renal replacement therapy (RRT) may be a considerable therapeutic option for diuretic‐refractory volume overload complicating AKI and RHF; however, only a few reports support this strategy for PAH patients. 5 , 6 Here, we report a patient with severe PAH who developed AKI and subsequent fluid retention associated with RHF but was successfully managed with intermittent RRT (IRRT) via a subcutaneously fixed superficial artery for 4 years.
Case report
A 30‐year‐old male was diagnosed with idiopathic PAH in 2005 and referred to our institution for consideration for lung transplantation (LT) in 2015. Before the referral, intravenous epoprostenol (IV Epo; via a Hickman catheter) was started 5 years after initiating oral PAH drugs due to uncontrollable haemodynamics. At that era, because higher dose IV Epo was considered one of the few effective PAH drugs, the IV Epo was up‐titrated to a higher dose over time and improved his haemodynamics. He suffered from recurrent catheter infections accompanied by RHF and transient renal dysfunction, but the IV Epo was continued for over 10 years while adjusting oral drug doses.
On referral to our institution, he was classified as World Health Organization functional class III and intermediate risk according to the ESC/ERS guidelines under IV Epo (213 ng/kg/min), riociguat (Rio) 7.5 mg, macitentan (Mac) 10 mg, and diuretics (furosemide 80 mg and trichlormethiazide 1 mg). His blood pressure was 104/58 mmHg. Laboratory data showed a plasma brain natriuretic peptide (BNP) level of 173 pg/mL and serum creatinine (Cre) level of 0.89 mg/dL [estimated glomerular filtration rate (eGFR) = 105 mL/min/1.73 m2]. Transthoracic echocardiography showed a normal left ventricular ejection fraction and mild tricuspid regurgitation with tricuspid annular plane systolic excursion of 22 mm. Right heart catheterization (RHC) showed a mean pulmonary arterial pressure (mPAP) of 34 mmHg, right atrial pressure (RAP) of 9 mmHg, pulmonary artery pulsatility index (PAPi: calculated by systolic PAP–diastolic PAP/RAP) of 3.6, cardiac index obtained by thermodilution method (CI) of 8.0 L/min/m2, cardiac power index (CPI; calculated as the mean arterial pressure × CO/451/body surface area) of 1.27, pulmonary arterial wedge pressure (PAWP) of 11 mmHg, and pulmonary vascular resistance (PVR) of 170 dynes/s/cm5, suggesting pre‐capillary pulmonary hypertension with chronic RHF and a hyperdynamic state.
After LT registration, the IV Epo was down‐titrated to suppress his high output cardiac state, and tolvaptan was started to reduce volume excess. However, he was readmitted for RHF deterioration triggered by a catheter infection. His blood pressure was 88/46 mmHg, while the heart rate was 76 b.p.m., and the plasma BNP level was 273 pg/mL. Transthoracic echocardiography showed severe tricuspid regurgitation with tricuspid annular plane systolic excursion of 12 mm. After hospitalization, increased diuretics and the addition of intravenous inotropes with dobutamine and dopamine did not improve his haemodynamics or volume overload, resulting in AKI (presumably due to renal congestion). The serum Cre level increased from 0.67 to 2.41 mg/dL (eGFR 26 mL/min/m2) over a few days, and he developed anuria, which exacerbated the excess fluid. RHC showed a RAP of 16 mmHg, mPAP of 39 mmHg, PAPi of 1.8, PAWP of 18 mmHg, CI of 8.2 L/min/m2, CPI of 0.98, and PVR of 128 dynes/s/cm5. Because of the high PAWP and RAP with anuria, continuous RRT (CRRT) was started for volume control. Fluid removal rate of CRRT was initiated with 30 mL/h and gradually elevated to 80 mL/h over a few days. After CRRT for 3 weeks with concomitant medical treatment including inotropic agents with dobutamine, dopamine, and noradrenaline, the mPAP decreased to 29 mmHg, and the PAWP (8 mmHg) and RAP (10 mmHg) also decreased without haemodynamic collapse. However, despite the decreased serum Cre level (to 0.47 mg/dL; eGFR 133 mL/min/m2), he needed regular RRT for volume control, suggesting that he was at the irreversible renal insufficiency stage due to RHF. Three months after, we decided to start IRRT via a subcutaneously fixed superficial artery instead of an arteriovenous shunt. This proved effective; there were no adverse events and the optimal volume control for RHF enabled us to switch from parenteral prostanoids to oral selexipag (Sel). He was discharged without an intravenous catheter 6 months after the IRRT was started. Although he was removed from the LT patient register because of IRRT dependence, RHC after 1 year revealed well‐controlled haemodynamics (mPAP = 29 mmHg, RAP = 16 mmHg, PAPi = 1.4, PAWP = 10 mmHg, PVR = 195 dynes/s/cm5, CI = 4.0 L/min/m2, CPI = 0.83) on treatment with oral Sel, Mac, Rio, and IRRT (Figure 1 ). He did not deteriorate or require readmission following discharge, but died of sepsis complicated with pancreatitis 4 years after initiating IRRT, without marked RHF deterioration.
Figure 1.
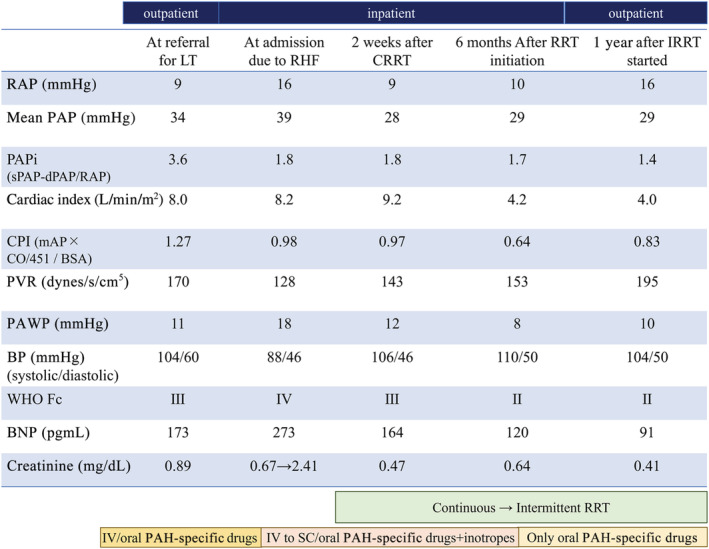
Clinical course of biological and haemodynamic variables of the patient. BNP, plasma brain natriuretic peptide; BP, blood pressure; BSA, body surface area; CPI, cardiac power index; CRRT, continuous renal replacement therapy; CO, cardiac output; dPAP, diastolic pulmonary arterial pressure; Fc, functional class; IRRT, intermittent renal replacement therapy; IV, intravenous; LT, lung transplantation; mAP, mean arterial pressure; PAP, pulmonary arterial pressure; PAWP, pulmonary arterial wedge pressure; PVR, pulmonary vascular resistance; RAP, right atrial pressure; RHF, right heart failure; SC, subcutaneous; sPAP, systolic pulmonary arterial pressure; WHO, World Health Organization.
Discussion
We described a PAH patient complicated with renal insufficiency and volume overload due to RHF, who underwent RRT effectively and safely for 4 years, with simultaneous clinical improvement of the PAH.
Right heart failure often causes cardiorenal syndrome, including AKI, by causing venous congestion and reduced renal perfusion pressure, 3 which is a challenging and potentially fatal complication. In RHF with PAH, the large increase in the transpulmonary gradient due to fixed resistance in the pulmonary vasculature complicates treatment regimens. 7 One of the treatment goals in RHF is to manage the right ventricular preload appropriately and reduce systemic congestion. Decongestion improves right ventricular decompression, ventricular interdependence, left ventricular filling, and cardiac output. 6 Thus, fluid volume management in PAH patients is crucial for preventing and managing RHF. Diuretics are the main medication and effectively reduce right ventricular wall stress; however, diuretic‐refractory cases require RRT. 6 Sztrymf et al. reported that RRT is feasible for AKI complicated with RHF in PAH patients, although it is associated with a poor prognosis. Moreover, the introduction of RRT in unstable PAH patients may be hazardous due to complications such as hypotension. Their policy is to delay RRT in the absence of anuria, uremic complications, or intractable severe acidosis or hyperkalemia. 5
Our patient developed anuria and had volume overload with elevated RAP, PAWP, and mPAP. Therefore, RRT was considered unavoidable. However, no adverse events occurred with careful management, including inotropes and pulmonary vasodilators. Furthermore, improvement of right ventricular decompression and ventricular interdependence by decongestion with RRT might contribute to avoiding haemodynamic deterioration. Although the serum Cre level improved, diuretics could not control fluid retention. This suggests that his renal insufficiency was relatively irreversible and continuing RRT was necessary to control the volume overload with RHF. In addition, high‐dose IV Epo can cause symptomatic high cardiac output failure and fluid retention, 8 which plays a role for worsening RHF and renal hypoperfusion. 9 Reducing IV Epo to the optimal dose is one way to solve this problem, although no criteria have been established for de‐escalation of IV Epo. Hence, it is often difficult to start reducing IV Epo, especially in severe PAH with RHF. In our case, it highlights that volume management with RRT could maintain the fluid balance, which helped us to down‐titrate the IV Epo carefully, ultimately to oral Sel without haemodynamic worsening.
Conclusions
In conclusion, RRT may be a potential alternative for fluid and haemodynamic control of AKI, and subsequent relative renal insufficiency and volume expansion complicated with RHF, in severe PAH cases. Further study is warranted to gain more insight into patient selection and the optimal timing of RRT in PAH patients with deteriorating RHF.
Conflict of interest
M.S. belongs to the Department, endowed by HIMEDIC Inc. and Siemens Healthcare K.K.; however, the status is irrelevant to the contents of the paper. E.A. belongs to the Department, endowed by NIPRO‐Corp, Terumo‐Corp., Senko‐Medical‐Instrument‐Mfg., Century‐Medical, Inc., ONO‐pharmaceutical‐Co., Ltd. Medtronic‐JAPAN Co., Ltd, Nippon‐Shinyaku Co., Ltd, Abiomed‐Inc, AQuA‐Inc, Fukuda‐Denshi Co., Ltd, Mochida‐Pharmaceutical‐Co.; Boehringer‐Ingelheim‐Pharmaceuticals Inc., and Sun‐Medical‐Technology‐Research Corp. The other authors have no conflicts of interest to disclose. There are no patents, products in development, or marketed products to declare.
Funding
This work was supported by the Ministry of Education, Culture, Sports, Science and Technology of Japan through Grant‐in‐Aid 21K16050.
Shimbo, M. , Hatano, M. , Ishii, S. , Saito, A. , Yagi, H. , Minatsuki, S. , Maki, H. , Amiya, E. , Takeda, N. , and Komuro, I. (2022) Renal replacement therapy as a therapeutic option for right heart failure in severe pulmonary arterial hypertension. ESC Heart Failure, 9: 2728–2731. 10.1002/ehf2.13945.
References
- 1. Chin KM, Rubin LJ. Pulmonary arterial hypertension. J Am Coll Cardiol. 2008; 51: 1527–1538. [DOI] [PubMed] [Google Scholar]
- 2. Haddad F, Fuh E, Peterson T, Skhiri M, Kudelko KT, de Jesus Perez V, Winkelmayer WC, Doyle RL, Chertow GM, Zamanian RT. Incidence, correlates, and consequences of acute kidney injury in patients with pulmonary arterial hypertension hospitalized with acute right‐side heart failure. J Card Fail. 2011; 17: 533–539. [DOI] [PubMed] [Google Scholar]
- 3. Jentzer JC, Bihorac A, Brusca SB, del Rio‐Pertuz G, Kashani K, Kazory A, Kellum JA, Mao M, Moriyama B, Morrow DA, Patel HN, Rali AS, van Diepen S, Solomon MA. Contemporary management of severe acute kidney injury and refractory cardiorenal syndrome. J Am Coll Cardiol. 2020; 76: 1084–1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Shah SJ, Thenappan T, Rich S, Tian L, Archer SL, Gomberg‐Maitland M. Association of serum creatinine with abnormal hemodynamics and mortality in pulmonary arterial hypertension. Circulation. 2008; 117: 2475–2483. [DOI] [PubMed] [Google Scholar]
- 5. Sztrymf B, Prat D, Jacobs FM, Brivet FG, O'Callaghan DS, Price LC, Jais X, Sitbon O, Simonneau G, Humbert M. Renal replacement therapy in patients with severe precapillary pulmonary hypertension with acute right heart failure. Respiration. 2013; 85: 464–470. [DOI] [PubMed] [Google Scholar]
- 6. Hansen L, Burks M, Kingman M, Stewart T. Volume management in pulmonary arterial hypertension patients: an expert pulmonary hypertension clinician perspective. Pulm Ther. 2018; 4: 13–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sztrymf B, Souza R, Bertoletti L, Jais X, Sitbon O, Price LC, Simonneau G, Humbert M. Prognostic factors of acute heart failure in patients with pulmonary arterial hypertension. Eur Respir J. 2010; 35: 1286–1293. [DOI] [PubMed] [Google Scholar]
- 8. Kataoka M, Yanagisawa R, Yoshino H, Satoh T. Massive ascites in pulmonary arterial hypertension: caution with epoprostenol. Ann Am Thorac Soc. 2013; 10: 726–727. [DOI] [PubMed] [Google Scholar]
- 9. Reddy YNV, Melenovsky V, Redfield MM, Nishimura RA, Borlaug BA. High‐output heart failure: a 15‐year experience. J Am Coll Cardiol. 2016; 68: 473–482. [DOI] [PubMed] [Google Scholar]


