Abstract
Problem: COVID-19 has impacted United States workers and workplaces in multiple ways including workplace violence events (WVEs). This analysis scanned online media sources to identify and describe the characteristics of WVEs related to COVID-19 occurring in the United States during the early phases of the pandemic. Method: Publicly available online media reports were searched for COVID-19-related WVEs during March 1–October 31, 2020. A list of 41 keywords was used to scan four search engines using Natural Language Processing (NLP). Authors manually reviewed media reports for inclusion using the study definition and to code variables of interest. Descriptive statistics were calculated across three types of violence: non-physical, physical, and events with both physical and non-physical violence. Results: The search of media reports found 400 WVEs related to COVID-19 during March 1–October 31, 2020. Of the WVEs, 27% (n = 108) involved non-physical violence, 27% (n = 109) physical violence, and 41% (n = 164) both physical and non-physical violence. Nineteen WVEs could not be assigned to a specific type of violence (5%). Most occurred in retail and dining establishments (n = 192, 48%; n = 74, 19%, respectively). Most WVEs related to COVID-19 were perpetrated by a customer or client (n = 298, 75%), but some were perpetrated by a worker (n = 61, 15%). Most perpetrators were males (n = 234, 59%) and acted alone (n = 313, 79%). The majority of WVEs were related to mask disputes (n = 286, 72%). In 22% of the WVEs, the perpetrator coughed or spit on a worker while threatening infection from SARS-CoV-2, the virus that causes COVID-19. Discussion: This analysis demonstrated that media scraping may be useful for workplace violence surveillance. The pandemic resulted in unique violent events, including those perpetrated by workers. Typical workplace violence prevention strategies may not be effective in reducing COVID-19-related violence. More research on workplace training for workers during public health crises is needed.
Keywords: Nonfatal injuries, Workplace violence, Occupational safety and health, COVID-19, Workplace mask policies
1. Problem
The COVID-19 pandemic has resulted in over 43 million reported cases and over 698,000 deaths in the United States as of October 2021 (CDC, 2021, CDC, 2021, CDC, 2021). The impact of COVID-19 on U.S. workplaces, employers, and employees has been unprecedented. Some workers have lost jobs and dealt with financial instability, others adjusted to the challenges of working from home, while essential workers on the frontlines faced fears of the risk of infection (Fan-Yun et al., 2021, Lund et al., 2021). Regardless of occupation, most U.S. workers faced, and continue to face, extraordinary stress and uncertainty during the pandemic. One study found that 70% of U.S. workers felt more stressed during COVID-19 than at any other point in their professional career (Ginger, 2020). In addition to these challenges, numerous media reports of workers being verbally and physically assaulted during the COVID-19 pandemic raised concerns about the potential for an increase in workplace violence events (WVEs) (McGuire et al., 2021, Rodríguez-Bolaños et al., 2020).
Early in the pandemic, media reported on retail workers being verbally assaulted, spit on, and physically attacked while enforcing COVID-19 mitigation practices such as mask wearing or physical distancing. Several of these episodes resulted in worker fatalities (Hanbury, 2020, MacFarquhar, 2020, Rogers, 2020). More recently, international studies have examined violence among healthcare professionals during the pandemic. While many of these studies could not compare violence during COVID-19 with that of pre-COVID levels, all studies found a high prevalence of violence among healthcare workers that significantly impacted their quality of life (Bhatti et al., 2021, Bitencourt et al., 2021, Ghareeb et al., 2021). In mid-2021, as new COVID-19 variants such as Delta emerged, the Centers for Disease Control and Prevention (CDC) updated public health guidance to re-recommend mask wearing, regardless of vaccination status (CDC, 2021, CDC, 2021, Centers for Disease Control and Prevention (CDC), 2020). Because of this changing guidance, some cities imposed new restrictions. For example, in mid-2021, New York City started requiring workers and customers of indoor workplaces such as gyms, restaurants, and theaters to provide proof of vaccination (Weixel, 2021). How employers and employees monitor, enforce, and comply with these policies and impact on future episodes of violence is unknown.
As long as the need for employers to implement and enforce COVID-19 mitigation policies remains, so does the potential for WVEs related to these COVID-19 policies. More information is needed on the occupations, industries, situations, and locations of WVEs to better understand these events and develop effective recommendations for prevention. Unfortunately, to the best of our knowledge, no analysis of U.S. WVEs related to the COVID-19 pandemic has been published. This may be due to the significant time-lag from event to data delivery using traditional surveillance sources. Collecting timely data on WVEs on a national scale may not be feasible during a public health emergency. Media reports can be used to augment traditional surveillance methods to provide more timely information (Brownstein et al., 2009, Chretien et al., 2009). During the COVID-19 pandemic, digital disease detection methods have been used to increase our knowledge of COVID-19′s impact on several industries and occupations (Kelly-Reif et al., 2021, Tomasi et al., 2021). The current study used similar methods to collect timely data from diverse web-based sources on COVID-19-related WVEs occurring in the early phases of the pandemic in the United States. This paper enumerates and characterizes WVEs by industry and type of violence.
2. Method
2.1. Data sources
This study searched publicly available online media reports to collect data on WVEs related to COVID-19 that occurred in U.S workplaces during the early phases of the COVID-19 pandemic. Four major search engines were searched from March 1–October 31, 2020, using keywords. Two search strategies were used. One strategy searched for present day news articles across local, regional, and national news outlets using a combination of four search engines: news.Google.com, news.yahoo.com, bing.com/news, and duckduckgo.com. Multiple search engines were used to improve coverage and reduce bias from using a single search site. Since search engines only return media reports from the previous 30 days, a second strategy was used to search data archives for older news reports. Data archives from Buzzsumo.com were searched because it is one of the largest and most comprehensive vendors of historical news archives. Searches were performed between May and October of 2020.
2.2. Search process and keywords
The authors developed an initial list of 41 keywords 1 relevant to workplace violence and COVID-19 to search the online media sites. After the first search, the list of keywords was refined using Natural Language Processing (NLP). The NLP analysis identified word trends, additional relevant keywords, and removed keywords that did not result in WVEs. For example, the NLP analysis found that verbs like “spit,” “shot,” and “assault” were often accompanied with the noun “mask” in relevant media reports. And the keywords “assault employee” identified numerous irrelevant media reports; therefore, search terms were altered to improve the search outcomes. Four search engines were explored using the final list of keywords and all possible combinations for a total of 188 unique web searches. A custom and asynchronous algorithm using the Python programming language was developed to perform the searches concurrently.
2.3. Inclusion and exclusion criteria
All discovered media reports were filtered by the computer using pre-developed inclusion and exclusion criteria. Media reports were included if they were: (1) written in English; (2) published during March 1–October 31, 2020; and (3) originated from a domain of.com,.us,.io,.org,.net,.media,.gov, or.edu. Next, filtering steps were developed to label media reports that met specific exclusion criteria. Media articles were excluded if they: (a) were published outside the specified dates; (b) occurred outside of the United States; (c) were reported in a video or audio format; or (d) were not related to COVID-19.
A second step in the computer search process determined the work-relatedness of the media report. Machine learning was employed to determine if a worker or employee was mentioned in the media report. First, two ‘seed’ terms (worker and employee) were used to train the NLP algorithm to build a library of word patterns to identify worker synonyms. From here, the NLP algorithm was used to identify media reports involving workers found within the narrative text. The final machine learning algorithm sample included 21,201 media reports of potential WVEs related to COVID-19 occurring during March 1, 2020, through October 31, 2020. The authors manually reviewed these media reports to establish the final dataset used for analysis.
2.4. Case selection
The study definition of a case involving WVE and COVID-19 was a violent event occurring in a workplace and related to COVID-19 mitigation measures such as masking and physical distancing. The violence could be physical (hitting, kicking) or non-physical (threatening, yelling, or verbal abuse). Non-physical violence was defined as ‘using words, gestures, or actions with the intent of intimidating or frightening an individual such as yelling, swearing, or using words to hurt an individual’ (Gerberich et al., 2011, NIOSH, 1996). Physical violence was defined as ‘hitting, slapping, kicking, pushing, choking, grabbing, or any action that leads to physical contact with the intention of injuring or causing harm’ (Gerberich et al., 2011, NIOSH, 1996). For this study, the WVE definition may also include threatening to infect someone with SARS-CoV-2 while spitting or coughing. It could also involve individuals damaging property such as store displays in an attempt to threaten a worker or coughing on products (categorized as a non-physical event). Finally, for the purposes of this study, cases where the violence was perpetrated by a worker were also included to fully capture instances of violence in U.S. workplaces.
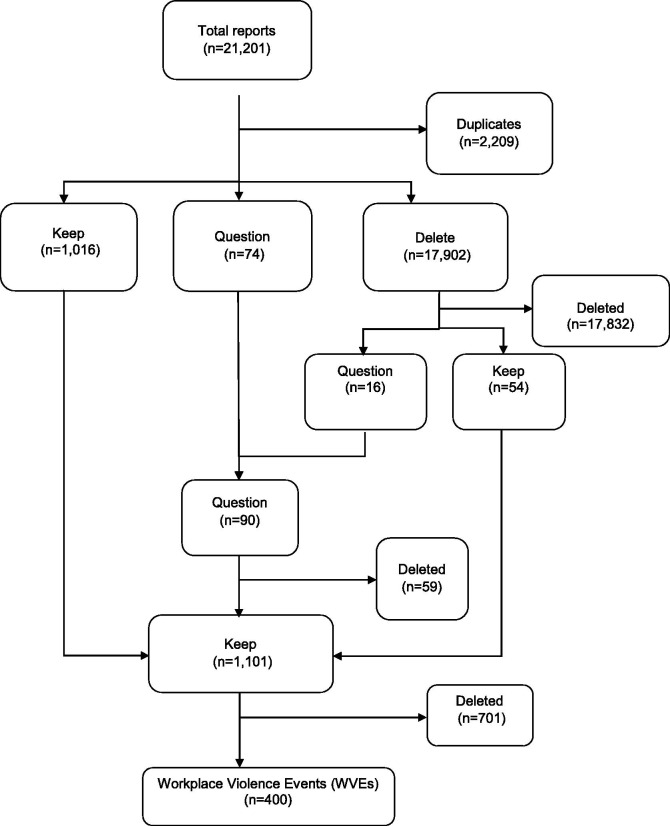
Although many layers of review at the computer level were used, the 21,201 media reports required manual review to confirm they met the study definition. Thus, the media reports were divided among three authors for manual review (Fig. 1 ). During this manual review, each media report was labeled “keep,” “delete,” “duplicate,” or “question.” Reports were labeled “keep” if the event met the study definition and “delete” if the event met any of the exclusion criteria, did not occur at a workplace, was not related to COVID-19, or occurred outside the United States. If the report was a re-reporting of another previously identified report, it was labeled “duplicate.” If information was lacking in the report on exclusion or inclusion criteria, it was labeled “question” for group discussion. After the first round of manual review, 1,016 reports were labeled ‘keep,’ 74 were labeled ‘question,’ 2,209 were labeled ‘duplicate,’ and 17,902 were labeled ‘delete.’ The high number of deletes was likely due to the inability of the computer algorithm to properly identify duplicates and fully verify the relevance of the media reports.
Fig. 1.
Flowchart of Search Process and Case Selection between March 1 and October 31, 2020.
The authors reviewed the 17,902 reports labeled ‘delete’ as a quality control measure. As a result, 54 reports were re-labeled ‘keep’, 16 re-labeled ‘question,’ and the remaining 17,832 reports were finally deleted. The 90 reports labeled as ‘question’ (74 + 16) were reviewed and discussed by all authors and 31 reports were moved into the ‘keep’ category. In the final round of manual review, 1,101 reports labeled as “keep” (1,016 + 54 + 31) were divided among all the authors. The final sample included 400 reports that were labeled WVE cases. The high number of cases that were deleted from the original media reports were due to duplicates not previously identified and reports not fully meeting the study definition. The search and case selection processes are summarized in Fig. 1.
2.5. Variables
All authors manually reviewed the final WVE cases to code the following variables: city, state, company, month, industry (healthcare, public safety, retail, dining, other, unknown), the perpetrator of the event, the victim of the event, number of perpetrators, gender of perpetrator, whether the event was associated with a mask dispute, whether the event was associated with a physical distancing dispute, whether a perpetrator coughed or spit on a worker, whether a perpetrator coughed or spit on a customer, law enforcement involvement, and type of violence (physical, non-physical, or both). States were grouped into regions based on the U.S. Census Bureau groupings (U.S. Department of Commerce, 1994). Industry was not coded using pre-determined codes or classification systems. A perpetrator was defined as a person or persons who initiated the WVE. For the purposes of this study, events involving spitting or coughing were considered physical WVEs.
2.6. Statistical analysis
Descriptive statistics were calculated and compared across three types of violence: nonphysical events, physical events, and events with both physical and non-physical elements using Pearson chi-square tests and Fisher’s exact test for categorical variables. If > 20% of the expected cell counts were less than 5, then the Fisher's exact test p-value was used (Kim, 2017). This was noted in all tables. Because of the number of comparisons that were made, all p-values were adjusted using the Bonferroni correction and adjustment procedure (Bland & Altman, 1995). The Bonferroni method is preferred when carrying out multiple tests without preplanned hypotheses (Perneger, 1998). All analyses were performed using SAS 9.4 (SAS Institute, Cary, NC, USA). Table 1 ′s adjusted p-value was p = 0.01 and Table 2 ′s adjusted p-value was p = 0.0038. Table 1, Table 2′s p-value tests for significant differences across the type of violence.
Table 1.
Workplace Violence Events in the U.S. by Type and Industry: March – October, 2020.*
| Non-Physical Violence Only N (%) |
Physical Violence Only N (%) |
Both Physical & Non-Physical N (%) |
P-value** | Total | |
|---|---|---|---|---|---|
| Industry | |||||
| Healthcare | 2 (2%) | 5 (5%) | 8 (5%) | 0.50*** | 15 (4%) |
| Public Safety | 2 (2%) | 9 (8%) | 26 (16%) | 0.0006*** | 37 (9%) |
| Retail | 52 (48%) | 59 (54%) | 81 (49%) | 0.64 | 192 (48%) |
| Dining | 29 (27%) | 17 (16%) | 28 (17%) | 0.07 | 74 (19%) |
| Other | 21 (19%) | 18 (17%) | 20 (12%) | 0.25 | 59 (15%) |
| Missing | 2 (2%) | 1 (1%) | 1 (1%) | N/A | 4 (4%) |
| Total | 108 (27%) | 109 (27%) | 164 (41%) | 400 (100%) | |
Columns do not add to Total due to the exclusion of the 19 cases that either could not be categorized into type of violence or involved only property damage.
Adjusted level of statistical significance is 0.01; p-values test for statistical differences across type of violence.
P-value from the Fisher’s Exact Test.
Table 2.
Characteristics of Perpertrators and Victims of Workplace Violence Events by Type in the U.S.: March – October, 2020*.
| Non-Physical Violence Only N (%) |
Physical Violence Only N (%) |
Both Physical & Non-Physical N (%) |
P-value** | Total | |
|---|---|---|---|---|---|
| Perpetrator of Event | 0.005 | ||||
| Worker | 21 (19%) | 25 (23%) | 15 (9%) | 61 (15%) | |
| Customer, Client, Non-Worker | 82 (76%) | 79 (73%) | 137 (84%) | 298 (75%) | |
| Victim of Event | |||||
| Only a Worker | 59 (55%) | 53 (49%) | 97 (59%) | 0.23 | 209 (52%) |
| Only a Customer, Client, Non-Worker | 33 (31%) | 50 (46%) | 48 (29%) | 0.011 | 131 (33%) |
| Both a Worker and Customer, Client, Non-Worker | 8 (7%) | 4 (4%) | 11 (7%) | 0.46*** | 23 (6%) |
| Did the Perpetrator Cough/Spit on a Worker? | <0.0001 | ||||
| Cough, Spit, or Both | 10 (10%) | 16 (14%) | 60 (37%) | 86 (22%) | |
| No Cough or Spit | 98 (91%) | 92 (84%) | 104 (63%) | 294 (74%) | |
| Did the Perpetrator Cough/Spit on a Customer? | 0.23 | ||||
| Cough, Spit, or Both | 6 (6%) | 11 (11%) | 18 (12%) | 35 (10%) | |
| No Cough or Spit | 101 (94%) | 98 (90%) | 143 (87%) | 342 (86%) | |
| Number of Perpetrators | 0.95 | ||||
| Single | 88 (82%) | 91 (84%) | 135 (82%) | 314 (79%) | |
| Multiple | 18 (17%) | 17 (16%) | 28 (17%) | 63 (16%) | |
| Gender of Perpetrators | |||||
| Male | 51 (48%) | 74 (68%) | 109 (67%) | 0.0016 | 234 (59%) |
| Female | 37 (34%) | 25 (23%) | 32 (20%) | 0.0196 | 94 (24%) |
| Both | 11 (10%) | 5 (5%) | 16 (10%) | 0.23*** | 32 (8%) |
| Was the Event Associated with a Mask Dispute? | <0.0001 | ||||
| Yes | 98 (90%) | 87 (80%) | 101 (62%) | 286 (72%) | |
| No | 9 (8%) | 19 (17%) | 55 (34%) | 83 (21%) | |
| Was the Event Associated with a Physical Distancing Dispute? | 0.0314*** | ||||
| Yes | 4 (4%) | 8 (7%) | 22 (13%) | 34 (9%) | |
| No | 103 (95%) | 98 (90%) | 136 (83%) | 337 (84%) | |
| Was Law Enforcement Involved? | <0.0001 | ||||
| Yes | 39 (36%) | 71 (65%) | 118 (72%) | 228 (57%) | |
| No | 55 (51%) | 7 (6%) | 13 (8%) | 75 (19%) | |
| Total | 108 (27%) | 109 (27%) | 164 (41%) | 400 (100%) |
Columns do not add to the Total due to unknowns within each category and the exclusion of the 19 cases that either could not be categorized into type of violence or involved only property damage.
Adjusted level of statistical significance is 0.0038; p-values test for statistical differences across type of violence.
P-value from the Fisher’s Exact Test.
3. Results
3.1. WVEs related to COVID-19 in U.S. Workplaces
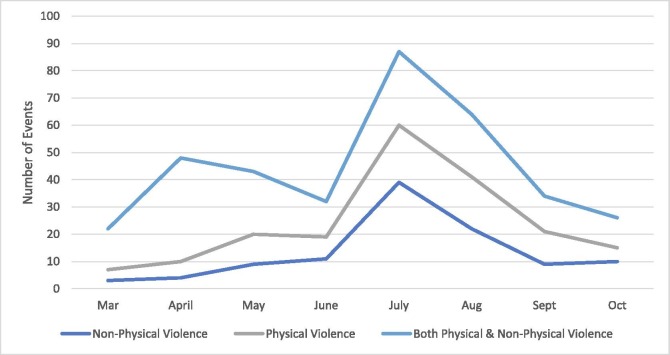
The search and validation of media reports captured 400 WVEs related to COVID-19 in the United States during the 8-month period between March 1, 2020, and October 31, 2020. Twenty-seven percent of the identified reports involved only non-physical violence (n = 108), 27% involved only physical violence (n = 109), and 41% involved both physical and non-physical violence (n = 164) (Table 1). Nineteen WVEs (5%) related to COVID-19 involved only property damage or could not be assigned to a specific type of violence from the media reports. All types of WVEs peaked in July (Fig. 2 ). Non-physical violence events also peaked in April in addition to July.
Fig. 2.
Workplace Violence Events in the U.S. by Type and Month: March – October, 2020*. *Non-physical violence = using words, gestures, or actions with the intent of intimidating or frightening an individual such as yelling, swearing, or using words to hurt an individual (Gerberich et al., 2011, NIOSH, 1996). Physical violence = hitting, slapping, kicking, pushing, choking, grabbing, or any action that leads to physical contact with the intention of injuring or causing harm. Also includes coughing or spitting for the purposes of this study (Gerberich et al., 2011, NIOSH, 1996).
3.2. Describing WVEs related to COVID-19 in the U.S.
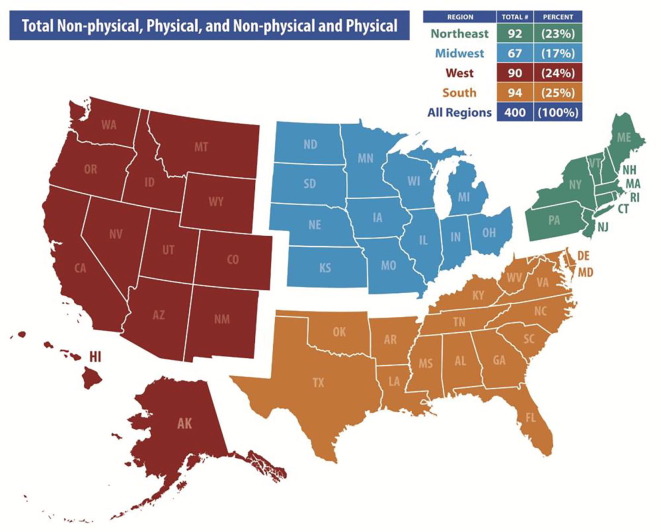
Overall, nearly 50% of the identified WVEs related to COVID-19 occurred in retail establishments (n = 192, 48%), 19% in dining establishments (n = 74), 9% among public safety workers (n = 37), and 4% in healthcare settings (n = 15) (Table 1). Fifteen percent of WVEs related to COVID-19 occurred in other types of establishments such as fitness centers, transportation services, and hair salons (n = 59). WVEs occurring in the public safety industry were significantly more likely to involve both physical and non-physical violence (p = 0.0006). WVEs related to COVID-19 were reported on throughout the U.S. regions equally. Twenty-five percent occurred in the South (n = 94), 24% in the West (n = 90), 23% in the Northeast (n = 92), and 17% in the Midwest (n = 67; Fig. 3 ). The largest number of non-physical WVEs were reported in the West (n = 34, 32%), the largest number of physical WVEs were reported in the South (n = 33, 30%), and the largest number of WVEs with both physical and non-physical violence were reported in the Northeast (n = 47, 29%), though these differences were not statistically significant (adjusted p = 0.0125).
Fig. 3.
Workplace Violence Events in the U.S. by State: March – October 2020*. *Numbers in regions do not add to 400 due to the exclusion of 57 cases where state could not be properly coded.
3.3. Characteristics of perpetrators and victims of WVEs related to COVID-19 in the U.S.
Most reported WVEs related to COVID-19 were perpetrated by a customer, client, or non-worker (n = 298, 75%), but 15% were perpetrated by a worker (n = 61) (Table 2). The worker was the sole victim of the WVE in 52% of the reported events (n = 209), a customer or client was the sole victim in 33% events (n = 131), and both the worker and a customer or client were considered the victims in 6% of the WVEs (n = 23). When a customer or client was the sole victim of the WVE, it was more likely to involve only physical violence, though this difference was not statistically significant (p = 0.011). Most perpetrators were males (n = 234, 59%) and most acted alone (n = 314, 79%). Males were significantly more likely to be the perpetrator of physical WVE related to COVID-19 (67% physical violence; 48% non-physical violence) (p = 0.0016).
The majority of identified WVEs related to COVID-19 were due to a mask dispute (n = 286, 72%). Nine percent of WVEs were due to a physical distancing dispute (n = 34, 9%). Non-physical WVEs were significantly more likely to be due to a mask dispute (p < 0.0001). In 22% of the WVEs, the perpetrator coughed or spit on a worker while threatening them with infections from SARS-CoV-2 (n = 86). Law enforcement was involved with 57% of the WVEs (n = 228) and were significantly more likely to be involved with increasing severity of violence (non-physical only 36%, physical only 65%, both physical and non-physical 72%; p < 0.0001).
3.4. WVEs related to COVID-19 in the U.S. by industry
There were differences in the identified WVEs related to COVID-19 across industries (Table 3 ). Customers and clients were more likely to be the perpetrator of the WVE related to COVID-19 in retail and dining establishments (82% and 81%, respectively). Coughing or spitting on a worker was more common in healthcare and public safety (67% and 81%, respectively). Perpetrators acting alone were most common in the healthcare and public safety sectors (93% and 100%, respectively). WVEs caused by a mask dispute were more common in retail and dining establishments (83% and 82%, respectively). Law enforcement was more commonly involved with WVEs related to COVID-19 that occurred in healthcare or retail establishments (60% and 63%, respectively).
Table 3.
Characteristics of Workplace Violence Events in the U.S. by Industry: March – October, 2020*.
| Healthcare N (%) |
Public Safety N (%) |
Retail N (%) |
Dining N (%) |
Other N(%) |
Total N (%) |
|
|---|---|---|---|---|---|---|
| Perpetrator of Event | ||||||
| Worker | 3 (20%) | 5 (14%) | 29 (15%) | 13 (17%) | 12 (19%) | 62 (16%) |
| Customer, Client, Non-Worker | 11 (73%) | 27 (73%) | 164 (82%) | 63 (81%) | 45 (69%) | 310 (79%) |
| Victim of Event | ||||||
| Only a Worker | 12 (80%) | 32 (87%) | 87 (44%) | 43 (55%) | 41 (63%) | 215 (54%) |
| Only a Customer, Client, Non-Worker | 2 (13%) | 4 (11%) | 81 (41%) | 28 (36%) | 17 (26%) | 132 (33%) |
| Both a Worker & Customer, Client, Non-Worker | 0 (0%) | 0 (0%) | 16 (8%) | 5 (6%) | 3 (5%) | 24 (6%) |
| Neither | 1 (7%) | 0 (0%) | 10 (5%) | 2 (3%) | 3 (5%) | 16 (4%) |
| Did the Perpetrator Cough/Spit on a Worker? | ||||||
| Cough, Spit, Both | 10 (67%) | 30 (81%) | 31 (17%) | 11 (13%) | 6 (9%) | 88 (22%) |
| No | 5 (33%) | 7 (19%) | 167 (84%) | 67 (86%) | 58 (89%) | 304 (77%) |
| Did the Perpetrator Cough/Spit on a Customer? | ||||||
| Cough, Spit, Both | 1 (7%) | N/A | 24 (13%) | 8 (10%) | 3 (5%) | 36 (10%) |
| No | 14 (93%) | N/A | 171 (86%) | 70 (90%) | 61 (94%) | 316 (80%) |
| Number of Perpetrators | ||||||
| Single | 14 (93%) | 37 (100%) | 165 (83%) | 56 (72%) | 53 (82%) | 325 (82%) |
| Multiple | 1 (7%) | 0 (0%) | 33 (17%) | 20 (26%) | 11 (17%) | 65 (17%) |
| Sex of Perpetrators | ||||||
| Male | 10 (67%) | 25 (68%) | 132 (66%) | 38 (49%) | 34 (52%) | 239 (61%) |
| Female | 3 (20%) | 12 (32%) | 45 (23%) | 24 (31%) | 16 (25%) | 100 (25%) |
| Both | 0 (0%) | 0 (0%) | 17 (9%) | 8 (10%) | 8 (12%) | 33 (8%) |
| Event Associated with a Mask Dispute? | ||||||
| Yes | 5 (33%) | 5 (14%) | 166 (83%) | 64 (82%) | 57 (88%) | 297 (75%) |
| No | 8 (53%) | 32 (87%) | 28 (14%) | 12 (15%) | 6 (9%) | 86 (22%) |
| Event Associated with a Physical Distancing Dispute? | ||||||
| Yes | 2 (13%) | 1 (3%) | 20 (10%) | 8 (10%) | 5 (8%) | 36 (9%) |
| No | 11 (73%) | 35 (95%) | 175 (88%) | 70 (90%) | 58 (89%) | 349 (88%) |
| Was Law Enforcement Involved? | ||||||
| Yes | 9 (60%) | N/A | 125 (63%) | 33 (42%) | 29 (45%) | 196 (50%) |
| No | 1 (7%) | N/A | 30 (15%) | 27 (35%) | 22 (34%) | 80 (20%) |
| Total | 15 | 37 | 200 | 78 | 65 | 400 (100%) |
Columns do not add to the Total due to unknowns within each category and the exclusion of the 19 cases that either could not be categorized into type of violence or involved only property damage.
4. Discussion
Our study described WVEs related to COVID-19 reported by the media during the early stages of the pandemic in the United States during March 1 and October 31, 2020. Media reports can be used to supplement traditional surveillance systems to identify at risk workers and situations when other data sources are not yet available. As an example, the most common data source for fatal WVEs is the Bureau of Labor Statistics’ (BLS) Census of Fatal Occupational Injury (CFOI). Every December, the BLS updates the CFOI using data from the prior year. Thus, CFOI data normally has a two-year lag.
Using media reports, this study found that nearly half of identified WVEs occurred in retail settings. Most identified WVEs related to COVID-19 were due to a mask dispute and were perpetrated by a customer, but some events were perpetrated by a worker. Nearly a quarter of the WVEs involved a customer voluntarily coughing or spitting on a worker while threatening infection from SARS-CoV-2. Media reports have previously been used to surveil for COVID-19 fatalities among various occupations, but the current study suggests these methods may also be useful for other occupational safety and health outcomes, such as workplace violence (Kelly-Reif et al., 2021, Tomasi et al., 2021). In addition, the Kelly-Reif et al. study found the sensitivity of media scans to detect first responder COVID-19 fatalities was high at 88% (Kelly-Reif et al., 2021).
Our results showed that reported WVEs related to COVID-19 peaked in April and July, 2020. One explanation for the peak in July is pandemic fatigue. Pandemic fatigue is defined by the World Health Organization (WHO) as “demotivation to follow recommended protective behaviors, emerging gradually over time…’ (World Health Organization, 2020). In the context of our findings, pandemic fatigue is possibly higher when cases are fewer and people no longer believe that following protective behaviors are needed. As new variants of the virus emerge and outbreaks continue to occur, pandemic fatigue may continue to further increase tensions as people tire of the continued perceived restrictions to “normal” life. WVEs may continue to impact workers as prevention policies continue or are reinstated in many industries including retail and food service.
One of the most common COVID-19 mitigation recommendations is the wearing of a mask. Masks provide source control and help protect wearers and others by filtering potentially infectious respiratory droplets (CDC, 2021, CDC, 2021, Centers for Disease Control and Prevention (CDC), 2020). The majority of identified COVID-19 related WVEs were associated with mask disputes. Between April and July 2020, 33 state governors ordered businesses to require their customers and employees to wear face masks (Jacobs & Ohinmaa, 2020). Of these 33 states, over 80% (n = 27) relied on businesses for enforcement of this policy (Jacobs & Ohinmaa, 2020). In the early phases of the pandemic, it is possible that mask disputes were caused by rising tensions from COVID-19 that disrupted work and the economy, among other aspects of daily life. These disruptions may make individuals feel that they have lost control over parts of their lives when told what to do in retail and dining establishments – wear a mask and physically distance from others (Brehm, 1966). It is also possible that individuals came to believe misinformation about the effectiveness of COVID-19 mitigation measures (CDC, 2021, CDC, 2021, Centers for Disease Control and Prevention (CDC), 2020, Roozenbeek et al., 2020). These disruptions in daily life, paired with misinformation about mitigation measures, may have played a role in customers, clients, and workers perpetrating violence in U.S. workplaces (CDC, 2021, CDC, 2021, Centers for Disease Control and Prevention (CDC), 2020, Roozenbeek et al., 2020).
The COVID-19 pandemic continues to raise several potential stressors among U.S. workers, particularly those in the retail and food service industries. One potential stressor for these workers may be performing job tasks, such as policy enforcement, without proper training and organizational resources. The accumulation of stressors may result in problematic levels of job stress and anxiety (Havermans et al., 2018, Morgantini et al., 2020). The National Institute for Occupational Safety and Health (NIOSH) defines job stress as the harmful physical and emotional responses that occur when job demands do not match the capabilities, resources, or needs of employees (NIOSH, 1999). This study suggests that workplace violence may be another stressor faced by retail and food service workers. Additional stressors of lower wages among retail and food service workers paired with fear of occupational exposure to COVID-19 may disproportionally impact these workers (Anderson, 2021, Ceryes et al., 2021, Giorgi et al., 2020, U.S. Bureau of Labor Statistics, 2021). While several reports highlight the impacts of the pandemic on workers’ mental health, most of these articles focused on healthcare workers (Abdoli et al., 2021, Aguglia et al., 2021, Carmassi et al., 2020, Evanoff et al., 2020, Giorgi et al., 2020). More research is needed on the pandemic’s mental health impact and prevention resources for non-healthcare frontline workers.
Another important finding from this study was that the identified WVEs related to COVID-19 had unique features. Workplace violence is traditionally defined as ‘any act or threat of physical violence, harassment, intimidation, or other threatening disruptive behavior that occurs at the work site. It ranges from threats and verbal abuse to physical assaults and even homicide. It can affect and involve employees, clients, customers and visitors’ (OSHA, n.d.). While the definition states workplace violence can affect and involve both employees and customers, historically, the focus of workplace violence has been violence directed at workers (Bureau of Justice Statistics (BJS), 2001, University of Iowa, 2001). However, this study highlights that workers can also perpetrate COVID-19 related violence in the workplace. As mentioned above, employees face many COVID-19 stressors including short-staffed worksites, childcare/school difficulties, and everyday worries about the pandemic. In the WHO manual for occupational safety and health during public health emergencies, the WHO explains how stress during a public health emergency can cause a person to feel overwhelmed and can reduce their ability to cope (World Health Organization (WHO), 2018). Employers could engage their employees to identify and mitigate psychosocial and work organization factors (e.g., workload, scheduling, availability of resources, work-life balance, ability to take sick leave) believed to contribute to job stress. Employees experiencing mental health symptoms that are impacting their functioning should be supported in seeking care from a qualified mental health professional.
Another important feature of workplace violence in this study was customers and clients threatening to infect employees with SARS-CoV-2. Based on the WVEs related to COVID-19 identified in this study, saliva was ‘weaponized’ just like a gun or knife. In fact, the federal government now considers saliva as a biological agent and can result in the perpetrator being charged with a federal crime (Cheema & Deeks, 2020). This may require employers to reconsider how they train and protect employees from violent events in the workplace.
To address the threat that workers face, CDC published guidance on limiting workplace violence associated with COVID-19 prevention policies in retail and services businesses (CDC, 2020). Recommended practices include clearly communicating the policies related to adherence to public health guidance such as masking, physical distancing, and occupancy limits at the entrance of and throughout the establishment. Second, establishing standard operating procedures when a potential threat is identified at work. This may include training employees on recognizing warning signs of violence, de-escalation tactics, how to remove oneself from a violent situation, where to seek a safe space, when to notify a supervisor, and when to call law enforcement. Finally, employers could consider installing security systems (e.g., alarms, panic buttons) to disrupt violent events and improve response time for law enforcement.
In addition to retail and food service workers, law enforcement officers also face risks of exposure to SARS-CoV-2 during the performance of their job duties that involve close contact with members of the public (Jennings & Perez, 2020). This not only includes responding to various disturbances such as domestic violence, but also responding to calls of WVE due to COVID-19 when perpetrators may resist arrest and become violent. Our data suggest that law enforcement was involved with 57% of the WVEs related to COVID-19 reported in the media. Law enforcement was significantly more likely to be involved with increasing severity of violence (non-physical only 36%, physical only 65%, both physical and non-physical 72%; p < 0.0001). Despite having the statutory authority to issue citations, fines, or jail sentences, most law enforcement entities have been reluctant to issue penalties for violations of mask mandates (Carlton, 2020, Goodland, 2020). The reluctance could be due to several factors: police department resource constraints, belief that the enforcement of mitigation measures is the responsibility of the public health community, discouraging arrests for low-level offenses to avoid introducing new people to crowded jail cells, and the fact that enforcement could expose officers to the virus and possible infection (Department of Homeland Security, 2020, Jennings and Perez, 2020). While our data suggest that over half of the COVID-19 WVEs involved law enforcement, this may overrepresent law enforcement involvement due to the media’s use of police scanners to cover and report stories (Kirby et al., 2021, Studley, 2020).
Although this study provided important data on the occurrence and characteristics of WVEs related to COVID-19 in the United States, it is not without limitations and the data should be interpreted with caution. First, the identified WVEs most likely underestimate the actual number of events. Undoubtably many WVEs are not picked-up by media. Second, some media reports may have included incorrect or incomplete information on the examined variables, including industry and type of violence. Third, the location of the WVE may be biased because media reporting varies by region and audience. Also, while the research team aimed for consistency in the interpretation of media reports and coding of variables, it should be noted that this was a subjective task. Another limitation is the differential results by industry. Since media reports are created based on news that may attract the most readers, some WVEs that are common, may not be equally covered in media reports. For example, WVEs occurring in healthcare may be more commonplace and be less likely to result in a media report. Because of this, the data presented here do not represent a census or a representative sample. Finally, these findings may not be generalizable nor comparable to different phases of the pandemic-especially since this study was conducted prior to vaccine availability.
This study demonstrated that media scraping may be useful for identifying occupational safety and health outcomes outside of fatality counts (Kelly-Reif et al., 2021, Tomasi et al., 2021). Using a combination of multiple search engines, case identification was maximized and represented a strength of the study. While data from traditional surveillance systems are still needed to provide representative and high-quality data, media reports can be used to augment these traditional systems to identify areas of concern quickly and provide situational awareness. Given the rapid and changing nature of the COVID-19 pandemic, using media reports to characterize workplace violence allows workplaces to develop improved preventive policies and training to reduce the risk of violence. The COVID-19 pandemic resulted in unique situations for workplaces and in turn, unique instances of violence. Typical workplace violence strategies may not be effective in reducing COVID-19 related episodes of violence. These findings are important as employers will continue to ask employees to enforce COVID-19 mitigation policies.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The research team thanks Mr. Herman Chu from Advanced Technologies and Laboratories. Mr. Chu’s work toward the media scraping methodology is greatly appreciated. This work was supported by the National Institute for Occupational Safety and Health (NIOSH). The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the National Institute for Occupational Safety and Health or the Centers for Disease Control and Prevention.
Biographies
Hope M. Tiesman, MSPH, PhD is a research epidemiologist at the National Institute for Occupational Safety and Health (NIOSH). Dr. Tiesman received a PhD in epidemiology from the University of Iowa in 2007. Her research interests include the occupational safety and health of police officers, the mental health of workers, and the scientific evaluation of workplace programs.
Suzanne Marsh received her B.S. degree in Statistics from Virginia Tech in 1989 and her M.P.A. from West Virginia University in 2006. She is a research statistician and team lead in the Division of Safety Research in the National Institute for Occupational Safety and Health. Her current research interests include first responder occupational injuries and workplace violence.
Srinivas Konda, MPH, is currently an Epidemiologist in the Division of Safety Research at NIOSH within the CDC. His breadth of interest includes work-related traumatic brain injury, workplace violence, motor vehicle injuries, and drug-related injuries that spans all occupations and some focus areas such as law enforcement officers, teachers, taxi drivers, tow truck drivers, and EMS workers.
Dr. Suzanne Tomasi received her DVM from The Ohio State University in 2005. In 2015 she completed an MPH at The Ohio State University. After graduate school and Veterinary Public Health residency, she was accepted into the CDC’s Epidemic Intelligence Service (EIS) program. She currently works as an epidemiologist at NIOSH with a focus on occupational respiratory diseases. Other NIOSH works include working with the American Veterinary Medical Association on several veterinary occupational projects such as an assessment of suicide among veterinarians.
Dr. Douglas Wiegand received a master’s degree in social psychology from Claremont Graduate University (2000) and a PhD in clinical psychology from Virginia Tech (2006). He currently works in the health hazard evaluation program at the National Institute for Occupational Safety and Health, where he assesses and makes recommendations for reducing job stress and associated health outcomes.
Dr. Tom Hales received his B.A. degree in Human Biology from Stanford University in 1979. He received his M.D. degrees from Case Western Reserve University in 1983. He received is M.P.H. degree in epidemiology from University of California Berkeley in 1997. He is a senior medical epidemiologist with NIOSH as a Medical Officer with the Fire Fighter Fatality Investigation and Prevention Program. His research interests include the study of fire fighters and other public safety officials
Sydney Webb, PhD served as a lead health communication specialist at NIOSH. She received her PhD in Communication Studies in 2012. She has over a decade of professional experience in health communication. While at NIOSH, she led the development of several communication products and campaigns on a wide range of topics. She is currently a Research Communications Analyst with RTI International in the Center for Communication Science.
Footnotes
Abuse, argument, assault, attack, battery, beating up, bullying, compliance, Coronavirus, coughed, covid, COVID-19, employee, enforcing masks, face coverings, fight, firearm, gun, harass, harassment, intimidation, killed, mask(s), murder, pandemic, physical assault, physical violence, PPE, punching, shot (shooting), spit, stab (stabbing), threat, threatening, verbal abuse, victimization, violence, weapon, worker(s), workplace, workplace violence.
References
- Abdoli N., Farnia V., Jahangiri S., Radmehr F., Alikhani M., et al. Sources of Sleep Disturbances and Psychological Strain for Hospital Staff Working during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2021;18(12):6289. doi: 10.3390/ijerph18126289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aguglia A., Amerio A., Costanza A., Parodi N., Copello F., Serafini G., et al. Hopelessness and post-traumatic stress symptoms among healthcare workers during the COVID-19 pandemic: Any role for mediating variables? International Journal of Environmental Research and Public Health. 2021;18(12):6579. doi: 10.3390/ijerph18126579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson, D. A. (2021). Retail jobs among the most common occupations. https://www.census.gov/library/stories/2020/09/profile-of-the-retail-workforce.html#:~:text=1%20Retail%20workers%20are%20younger.%20Over%20half%20of,workers%20were%20more%20likely%20to%20have%20Medicaid.%20. (accessed August 3, 2021).
- Bhatti O.A., Rauf H., Aziz N., Martins R.S., Khan J.A. Violence against healthcare workers during the COVID-19 pandemic: A review of incidents from a lower-middle-income country. Annuals of Global Health. 2021;87(1):41. doi: 10.5334/aogh.3203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bitencourt M.R., Alarcão A.C.J., Silva L.L., Dutra A.C., Caruzzo N.M., Roszkowski I., et al. Predictors of violence against health professionals during the COVID-19 pandemic in Brazil: A cross-sectional study. PLoS One. 2021;16(6):e0253398. doi: 10.1371/journal.pone.0253398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bland J.M., Altman D.G. Multiple significance tests: The Bonferroni method. BMJ. 1995;310:170. doi: 10.1136/bmj.310.6973.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brehm J.W. Academic Press; 1966. A theory of psychological reactance. [Google Scholar]
- Brownstein J.S., Freifeld C.C., Madoff L.C. Digital disease detection: Harnessing the web for public health surveillance. New England Journal of Medicine. 2009;360(21):2153–2157. doi: 10.1056/NEJMp0900702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of Justice Statistics (BJS) (2001). Violence in the Workplace, 1993–1999. https://bjs.ojp.gov/content/pub/pdf/vw99.pdf. (accessed August 18, 2021).
- Carlton J. Mandatory mask laws aren’t enforced as coronavirus continues to spread. Wall Street Journal. 2020 (accessed August 14, 2021) [Google Scholar]
- Carmassi C., Foghi C., Dell’Oste V., Cordone A., Bertelloni C.A., Bui E., et al. PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: What can we expect after the COVID-19 pandemic. Psychiatry Research. 2020;292:113312. doi: 10.1016/j.psychres.2020.113312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. COVID Data Tracker. https://covid.cdc.gov/covid-data-tracker/#datatracker-home. (accessed on October 3, 2021).
- Centers for Disease Control and Prevention. Interim public health recommendations for fully vaccinated people. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/fully-vaccinated-guidance.html. (accessed August 17, 2021).
- Centers for Disease Control and Prevention (2021). Science brief: Community use of cloth masks to control the spread of SARS-CoV-2. https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/masking-science-sars-cov2.htm. (accessed August 14, 2021). [PubMed]
- Centers for Disease Control and Prevention (CDC) (2020). Limiting workplace violence associated with COVID-19 prevention policies in retail and services businesses. Atlanta, GA: U.S. Department of Health and Human Services, CDC, National Center for Immunization and Respiratory Diseases. https://www.cdc.gov/coronavirus/2019-ncov/community/organizations/business-employers/limit-workplace-violence.html.
- Ceryes C., Robinson J., Biehl E., Wirtz A.L., Barnett D.J., Neff R. Frequency of workplace controls and associations with safety perceptions among a national sample of US Food Retail Workers During the COVID-19 pandemic. Journal of Occupational Environmental Medicine. 2021;63(7):557–564. doi: 10.1097/JOM.0000000000002218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheema, M., and Deeks A. (2020). Prosecuting purposeful coronavirus exposure as terrorism. Available at: https://www.lawfareblog.com/prosecuting-purposeful-coronavirus-exposure-terrorism. (accessed August 8, 2021).
- Chretien J.P., Tomich N.E., Gaydos J.C., Kelley P.W. Real-time public health surveillance for emergency preparedness. American Journal of Public Health. 2009;99(8):1360–1363. doi: 10.2105/AJPH.2008.133926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Homeland Security (2020). COVID-19 exposure and risk mitigation best practices for law enforcement. Department of Homeland Security. Available at: https://www.theiacp.org/sites/default/files/COVID-10%20LE%20Risk%20Mitigation%20and%20Exposure%20Best%20Practices%20_Final.pdf. (accessed August 14, 2021).
- Evanoff B.A., Strickland J.R., Dale A.M., Hayibor L., Page E., Duncan J.G., et al. Work-related and personal factors associated with mental well-being during the COVID-19 response: Survey of health care and other workers. Journal of Medical Internet Research. 2020;22(8):e21366. doi: 10.2196/21366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan-Yun L., Suharlim C., Kales S.N., Yang J. Association between SARS-CoV-2 infection, exposure risk and mental health among a cohort of essential retail workers in the USA. Occupational and Environmental Medicine. 2021;78(4):237–243. doi: 10.1136/oemed-2020-106774. [DOI] [PubMed] [Google Scholar]
- Gerberich S.G., Nachreiner N.N., Ryan A.D., Church T.R., McGovern P.M., Geisser M.S., et al. Violence against educators: A population-based study. Journal of Occupational and Environmental Medicine. 2011;53(3):294–302. doi: 10.1097/JOM.0b013e31820c3fa1. [DOI] [PubMed] [Google Scholar]
- Ghareeb N.S., El-Shafei D.A., Eladl A.M. Workplace violence among healthcare workers during COVID-19 pandemic in a Jordanian governmental hospital: the tip of the iceberg. Environmental Science and Pollution Research International. 2021:1–9. doi: 10.1007/s11356-021-15112-w. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginger (2020). Workforce attitudes towards mental health. Available at: https://f.hubspotusercontent40.net/hubfs/5327495/2020%20Workforce%20Attitudes%20Toward%20Mental%20Health.pdf.
- Giorgi G., Lecca L.I., Alessio F., Finstad G.L., Bondanini G., Lulli L.G., et al. COVID-19-Related Mental Health Effects in the Workplace: A Narrative Review. International Journal of Environmental Research and Public Health. 2020;17(21):7857. doi: 10.3390/ijerph17217857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodland, M. (2020). Enforcement of the mask mandate: who's doing it, who isn't. Colorado Politics. Available at: https://www.coloradopolitics.com/news/enforcement-of-the-mask-mandate-whos-doing-it-who-isnt/article_c92144e8-cc52-11ea-95c8-abf3c540f622.html. (accessed August 14, 2021).
- Hanbury, M. (2020). A family dollar security guard was killed after he refused to let a customer into the store because they weren't wearing a mask. Available at: https://www.businessinsider.com/retail-workers-face-violence-from-shoppers-over-new-pandemic-rules-2020-5.
- Havermans B.M., Brouwers E.P.M., Hoek R.J.A., van der Anema J., Beek A.J., Boot C.R.L. Work stress prevention needs of employees and supervisors. BMC Public Health. 2018;18(642):1–11. doi: 10.1186/s12889-018-5535-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs, P., and Ohinmaa, A.P. (2020). The enforcement of statewide mask wearing mandates to prevent COVID-19 in the US: an overview, Vol. 9, pp. 1100. [DOI] [PMC free article] [PubMed]
- Jennings W.G., Perez N.M. The Immediate impact of COVID-19 on law enforcement in the United States. American Journal of Criminal Justice. 2020;June 2020:1–12. doi: 10.1007/s12103-020-09536-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly-Reif K., Rinsky J.L., Chiu S.K., Burrer S., de Perio M.A., Trotter A.G., et al. Media reports as a tool for timely monitoring of COVID-19-related deaths among first responders-United States, April 2020. Public Health Reports. 2021;136(3):315–319. doi: 10.1177/0033354921999171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H.Y. Statistical notes for clinical researchers: Chi-squared test and Fisher's exact test. Restorative dentistry & endodontics. 2017;42(2):152–155. doi: 10.5395/rde.2017.42.2.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby, K. A, Meltzer, A. S,, Rein, W. (2021). Guidelines for use of information from police scanners. Radio Television Digital News Association (RTDNA). Available at: https://www.rtdna.org/content/scanner. (accessed August 14, 2021).
- Lund, S., Madgavkar, A., Manyika, J., Smit, S., Ellingrud, K., Robinson, O. (2021). The future of work after COVID-19. Available at: https://www.mckinsey.com/featured-insights/future-of-work/the-future-of-work-after-covid-19#.
- MacFarquhar, N. (2020). Who’s enforcing mask rules? Often retail workers and they’re getting hurt. Available at: https://www.nytimes.com/2020/05/15/us/coronavirus-masks-violence.html.
- McGuire S.S., Gazley B., Majerus A.C., Mullan A.F., Clements C.M. Impact of the COVID-19 pandemic on workplace violence at an academic emergency department. Annals of Emergency Medicine. 2021;78(2):S33–S34. doi: 10.1016/j.ajem.2021.09.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgantini L.A., Naha U., Wang H., Francavilla S., Acar Ö., Flores J.M., et al. Factors contributing to healthcare professional burnout during the COVID-19 pandemic: A rapid turnaround global survey. PLoS ONE. 2020;15(9):e0238217. doi: 10.1371/journal.pone.0238217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIOSH (1996). Current intelligence bulletin 57: Violence in the workplace; risk factors and prevention strategies. Cincinnati, OH: U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. 96–100.
- NIOSH (1999). Stress…at work. Cincinnati, OH: Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, publication number 99–101. https://www.cdc.gov/niosh/docs/99-101/pdfs/99-101.pdf.
- Perneger T.V. What’s wrong with Bonferroni’s adjustment. BMJ. 1998;316:1236–1238. doi: 10.1136/bmj.316.7139.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Bolaños R., Cartujano-Barrera F., Cartujano B., Flores Y.N., Cupertino A.P., Gallegos-Carrillo K. The urgent need to address violence against health workers during the COVID-19 pandemic. Med Care. 2020;58(7):663. doi: 10.1097/MLR.0000000000001365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers, J. (2020). Retail workers finding new stresses in the age of COVID-19: ‘It’s insane’. Available at: https://www.boston.com/news/coronavirus/2020/06/07/retail-covid-19-stress.
- Roozenbeek J., Schneider C.R., Dryhurst S., Keyy J., Freeman A.L.J., Recchia G., et al. Susceptibility to misinformation about COVID-19 around the world. Royal Society of Open Science. 2020;7(10):1–15. doi: 10.1098/rsos.201199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Occupational Safety and Health Administration (OSHA). (N.D). Workplace Violence. https://www.osha.gov/workplace-violence. (accessed August 18, 2021).
- Studley, L. (2020). Bill may increase media, public access to police communication. Rocky Mountain Collegian. Available at: https://collegian.com/2020/02/category-news-bill-may-increase-media-public-access-to-police-communication. (accessed August 14, 2021).
- Tomasi S.E., Ramirez-Cardenas A., These M.S., Rinsky J.L., Chiu S.K., Luckhaupt S., et al. COVID-19 mortality among Amalgamated Transit Union (ATU) and Transport Workers Union (TWU) workers-March-July 2020, New York City metro area. American Journal of Industrial Medicine. 2021;64(9):723–730. doi: 10.1002/ajim.23281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Bureau of Labor Statistics (2021). Food services and drinking places: NAICS 722. https://www.bls.gov/iag/tgs/iag722.htm. (accessed August 3, 2021).
- U.S. Department of Commerce (1994). Geographic Areas Reference Manual. https://www2.census.gov/geo/pdfs/reference/GARM/GARMcont.pdf. (accessed August 5, 2021).
- University of Iowa (2001). Workplace violence: A report to the nation. Available at: https://iprc.public-health.uiowa.edu/wp-content/uploads/2015/09/workplace-violence-report-1.pdf.
- Weixel, N. (2021). New York City to require vaccination for indoor activities, restaurants, gyms. Available at: https://thehill.com/policy/healthcare/566073-new-york-city-to-require-vaccination-for-indoor-activities-restaurants-gyms.
- World Health Organization (WHO) (2018). Occupational safety and health in public health emergencies: A manual for protecting health workers and responders. Available at: https://apps.who.int/iris/bitstream/handle/10665/275385/9789241514347-eng.pdf. (accessed August 3, 2021).
- World Health Organization (2020). Pandemic fatigue – Reinvigorating the public to prevent COVID-19. Policy framework for supporting pandemic prevention and management. Copenhagen: WHO Regional Office for Europe; 2020. License: CC BY-NC-SA 3.0 IGO.