Abstract
Objective
To explore the transitions of different blood pressure states based on a multistate Markov model among the Chinese elderly population.
Setting
A community health centre in Xiamen, China.
Participants
1833 elderly Chinese people.
Methods
A multistate Markov model was built based on 5001 blood pressure measurements from 2015 to 2020. Research was conducted to explore the process of hypertension progression, providing information on the transition probability, HR and the mean sojourn time in three blood pressure states, namely normal state, elevated state and hypertensive state.
Results
Probabilities of moving from the normal state to the hypertensive state in the first year were 16.97% (female) and 21.73% (male); they increased dramatically to 47.31% (female) and 51.70% (male) within a 3-year follow-up period. The sojourn time in the normal state was 1.5±0.08 years. Elderly women in the normal state had a 16.97%, 33.30% and 47.31% chance of progressing to hypertension within 1, 2 and 3 years, respectively. The corresponding probabilities for elderly men were 21.73%, 38.56% and 51.70%, respectively. For elderly women starting in the elevated state, the probabilities of developing hypertension were 25.07%, 43.03% and 56.32% in the next 1, 2 and 3 years, respectively; while the corresponding changes for elderly men were 20.96%, 37.65% and 50.86%. Increasing age, body mass index (BMI) and glucose were associated with the probability of developing hypertension from the normal state or elevated state.
Conclusions
Preventive actions against progression to hypertension should be conducted at an early stage. More awareness should be paid to elderly women with elevated state and elderly men with normal state. Increasing age, BMI and glucose were critical risk factors for developing hypertension. The derived transition probabilities and sojourn time can serve as a significant reference for making targeted interventions for hypertension progression among the Chinese elderly population.
Keywords: hypertension, epidemiology, public health
Strengths and limitations of this study.
A multistate Markov model was used to explore the state transition dynamics of three blood pressure states, and to investigate the risk factors affecting the progression of hypertension in the Chinese elderly population.
The derived transition probabilities and sojourn time can serve as a significant reference for the development of proactive and targeted interventions for hypertension progression among the Chinese elderly population.
Owing to time and financial limitations, the research only focused on the cohort population over 5 years in one city.
The hypertensive state was regarded as an absorbing state, meaning that the reverse transition from the hypertensive state to the normal or elevated state was not considered.
Some significant covariates such as various life habits of diet, smoking, exercise and psychological status were not covered, but are worthy of investigation in further research.
Introduction
Hypertension is defined by Chinese and European guidelines as an office systolic blood pressure (SBP) of ≥140 mm Hg and/or diastolic blood pressure (DBP) of ≥90 mm Hg without any antihypertensive medication.1 2 As a significantly increasing global health issue, hypertension is the leading cause of cardiovascular and cerebrovascular diseases, chronic kidney disease and cognitive dysfunction.3–8 It is likewise regarded as the most frequent modifiable risk factor for cardiovascular-related mortality, morbidity, disability and health expense in the global population.9–14 During the last decade, the prevalence of hypertension has rapidly increased.15 16 At present, approximately 1.13 billion people worldwide live with hypertension, and the number is predicted to increase by 15%–20% by 2025.17 In China, hypertension is emerging as a major public health problem and influences more than 270 million people18 19; its incidence increases with age, affecting more than 60% of people older than 60 years.20
Sound evidence has identified various risk factors for hypertension, including genetic, environmental and socialdemographic perspectives, such as family history, diet, stress, obesity, age, gender and hypercholesterolaemia.21–24 However, the methods commonly used to discover these risk factors in previous research, namely, logistic regression and Cox proportional models, do not provide adequate information about the dynamitic process of blood pressure evolution.24–27 Indeed, the natural process of hypertension involves dynamic evolution, and hypertensive individuals experience different stages along its progression trajectory with the passage of time.28 According to the hypertension prevention guidelines in China, blood pressure can be divided into three categories: the normal state, elevated state and hypertensive state.1 29 The elevated state is the blood pressure range of prehypertension, with a value of 120–139 mm Hg for SBP and 80–89 mm Hg for DBP without antihypertensive medication; it represents the transition from a normal state to hypertension in clinical diagnosis.1 In addition to the hypertensive state, the elevated state is also related to a higher risk of fatal cardiovascular disease. Therefore, it is imperative to investigate the transition patterns among different levels of blood pressure for early detection and prevention.30
Multistate Markov modelling has been widely used in healthcare research to analyse the progression of various chronic diseases, such as hepatitis,31 diabetes,32 chronic kidney disease33 and Alzheimer’s disease.34 It likewise can be used to analyse the transition from a normal (non-disease) state, through a mild state to a severe and/or death state.35 As an effective method for dealing with repeated measurement data, multistate Markov modelling can provide information on interstate transitions, transition probability, HR and the mean sojourn time of the transition in the cohort population.28 29 There have been two studies exploring transition of the blood pressure states based on multistate Markov models. One study focused on the US working population aged 18–54 years28; the other study focused on the Chinese population with a mean age of 37.54±13.80 years. Compared with the young working population, elderly people have a higher incidence of hypertension, and are worthy of more attention and investigation.29
Therefore, our research contributed to exploring the state transition dynamics of three blood pressure states via multistate Markov modelling and investigating the risk factors associated with the progression of hypertension among the Chinese elderly population, which have not been explored in the existing literature. Furthermore, our study estimated, for this group of elderly persons, the sojourn time in each blood pressure state and the transition probabilities from one state to other states, to provide initial statistical foundations for early hypertension prevention, timely targeted interventions and effective geriatric nursing.
Methods
Aim and design
A quantitative longitudinal study was conducted to explore the transitions of different blood pressure states based on a multistate Markov model among the Chinese elderly population.
Participants
This research included individuals who volunteered to have a community-organised free annual physical examination in a community health centre of a hospital funded by the Chinese Government from 2015 to 2020. The inclusion criteria were participants aged 60 years or above, who attended at least two checkups, including at least one for baseline data and one for follow-up data. The exclusion criteria were individuals who had hypertension at baseline, or whose record had missing data on age, gender, blood pressure, body mass index (BMI) or blood glucose. After preprocessing, a total of 1833 individuals were included in the study. The maximum follow-up time was 5.7 years, and the mean follow-up was approximately 2.5 years.
Patient and public involvement
Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research. Patients or the public were not invited to contribute to the writing or editing of this article for readability or accuracy.
Data collection
This study used data from the annual physical examination. During each annual check-up, the individual’s height, weight, abdominal circumference, blood pressure and ECG were assessed, and a blood test was taken to measure their blood glucose. Sociodemographic data such as age, gender and marital status were collected by health professionals.
Blood pressure was measured by professional medical staff using an Omron electronic sphygmomanometer with appropriately sized cuffs, measuring SBP and DBP in the resting, sitting position on the right and left upper arm, respectively.36 37 All participants gave at least two mandatory blood pressure measurements, with an interval of 10 min,38 and the average of two measurements was used as the result. If the numerical difference of the SBP or DBP readings between the two mandatory measurements was more than 10 mm Hg, a third blood pressure measurement was conducted to avoid error. In order to improve the accuracy of measurement, participants were asked to relax for >5 min, and avoid caffeine, exercise and smoking for at least 30 min before measurement. Neither the participant nor the observer was allowed to talk during the rest period or during the measurement.
In the research, three blood pressure states were categorised according to the Chinese Hypertension Prevention Guide 2010 Third Edition1: (1) normal state: SBP less than 120 mm Hg, DBP less than 80 mm Hg, and not taking any antihypertensive medicine; (2) elevated state: SBP 120–139 mm Hg (DBP <90 mmHg) or DBP 80–89 mm Hg (SBP <140 mm Hg), and not taking any antihypertensive medicine and (3) hypertensive state: SBP at least 140 mm Hg or DBP at least 90 mmHg or taking any antihypertensive medicine.
The BMI is the ratio of a person’s weight (in kilograms) to the square of their height (in metres). In this study, four BMI categories were defined by the Chinese Center for Disease Control and Prevention: (1) underweight: BMI less than 18.5 kg/m2; (2) normal: BMI ranging from 18.5 to 24.0 kg/m2; (3) overweight: BMI ranging from 24.0 kg/m2 to 28.0 kg/m2 and (4) obese: BMI higher than 28.0 kg/m2.
Statistical analysis
Descriptive analysis was used to describe the socialdemographic and clinical data. For continuous data, the mean and SD were used, and for categorical data, frequencies and percentages were used. HRs and corresponding 95% CIs were used in the statistical analysis. The multistate Markov model was built using the ‘msm’ package of R software.39 The χ2 test was used to compare differences in baseline characteristics between the male and female participants. All the statistical analyses were conducted using R software (R Foundation, Vienna, Austria). A p<0.05 was considered statistically significant.
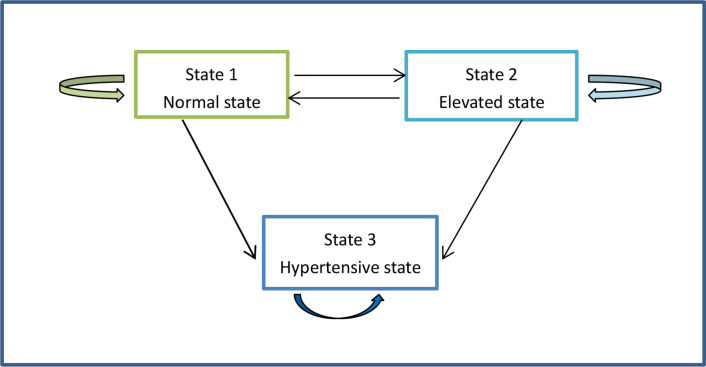
In the Markov model of this study, there are three blood pressure states of interest: state 1 (normal state), state 2 (elevated state) and state 3 (hypertensive state). A state change is regarded as a transition. If a state can continue to transition to another, it is classified as a transient state; otherwise, it is an absorbing state, meaning a lifelong health condition.39 In the research, both the normal state and the elevated state were transient states as the model assumed that the two states could transition to each other as well as to the hypertensive state. By contrast, once an individual transitioned to the hypertension state, he or she could not return to the normal state or elevated state because the transitions from hypertension to the other states were not natural processes.28
Six possible transitions among the three states are illustrated in figure 1. For example, the blood pressure of an individual can stay in the current state or transition to any of the other states, such as normal → normal, normal →elevated, normal →hypertensive, elevated →elevated, elevated →normal, elevated →hypertensive. The sojourn time means the average length of time the blood pressure remained in a transient state before transitioning to a new state.
Figure 1.
The three blood pressure state transitions in the Markov model.
Results
Baseline characteristics of participants
In this study, 1833 participants were included, with 5001 measurement records. At the baseline check-up, 443 (25.17%) participants were in the normal state and 1390 (75.83%) participants were in the elevated state. However, at the final check-up, 247 (13.48%) individuals were in the normal state, 447 (24.39%) individuals were in the elevated state, and 1139 (62.14%) individuals were in the hypertensive state (table 1).
Table 1.
The statistic of blood pressure state transition
| Blood pressure state | Baseline check-up N (%) | Final check-up N (%) |
| Normal state | 443 (24.17) | 247 (13.48) |
| Elevated state | 1390 (75.83) | 447 (24.39) |
| Hypertensive state | 0 (0) | 1139 (62.14) |
| Total | 1833 (100.00) | 1833 (100.00) |
Among these participants, the mean age was 65.5 (6.04) years, and 967 (52.76%) were female. The baseline characteristics of these participants, and their discrepancies between male and female participants, are summarised in table 2.
Table 2.
Baseline characteristics of participants
| Variable | Overall, N=1833* | Male, N=866 | Female, N=967 | P value† |
| Age mean (SD) | 65.5 (6.04) | 65.7 (5.85) | 65.4 (6.20) | 0.031 |
| Married | 1605/1830 (88%) | 817/865 (94%) | 788/965 (82%) | <0.001 |
| Blood pressure | 0.002 | |||
| Normal state | 443/1833 (24%) | 181/866 (21%) | 262/967 (27%) | |
| Elevated state | 1390/1833 (76%) | 685/866 (79%) | 705/967 (73%) | |
| Glucose mean (SD) | 5.6 (1.67) | 5.5 (1.38) | 5.8 (1.88) | <0.001 |
| Diabetes | 119/1833 (6.5%) | 51/866 (5.9%) | 68/967 (7.0%) | 0.300 |
| BMI | <0.001 | |||
| Normal | 1160/1833 (63%) | 579/866 (67%) | 581/967 (60%) | |
| Obese | 78/1833 (4.3%) | 28/866 (3.2%) | 50/967 (5.2%) | |
| Overweight | 421/1833 (23%) | 170/866 (20%) | 251/967 (26%) | |
| Underweight | 174/1833 (9.5%) | 89/866 (10%) | 85/967 (8.8%) | |
| Abnormal ECG | 466/1662 (28%) | 248/779 (32%) | 218/883 (25%) | 0.001 |
*Mean (SD), n/N (%)
†Wilcoxon rank sum test; Pearson’s χ2 test.
BMI, body mass index.;
Transition frequency from one check-up to the following check-up
Among 5001 blood pressure measurements in 1833 elderly people over the period 2015–2020, 1833 measurements were conducted at the baseline check-up and 3168 measurements were conducted at follow-up checkups. The numbers of transitions from one check-up (given by the row state) to the next one (given by the column state) are shown in table 3.
Table 3.
Observed number of transitions from one check-up to the next check-up
| From\to | Normal | Elevated | Hypertensive | Total |
| Normal | 430 (47.25%) | 242 (26.59%) | 238 (26.15%) | 910 (100.00%) |
| Elevated | 284 (12.58%) | 1073 (47.52%) | 901 (39.90%) | 2258 (100.00%) |
Of the 3168 transitions, 26.59% showed deterioration from the normal state to the elevated state at the next check-up, 26.15% from the normal state to the hypertensive state, and 47.25% with the normal state showed no change. Similarly, there were 1073 occurrences where participants remained in the elevated state, 901 (39.90%) cases where participants progressed from the elevated state to hypertension, while 284 (12.25%) cases showed alleviation from the elevated state to the normal state at the following visit.
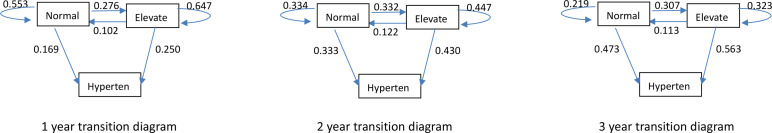
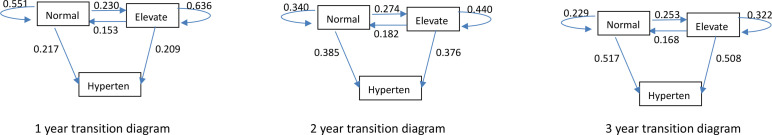
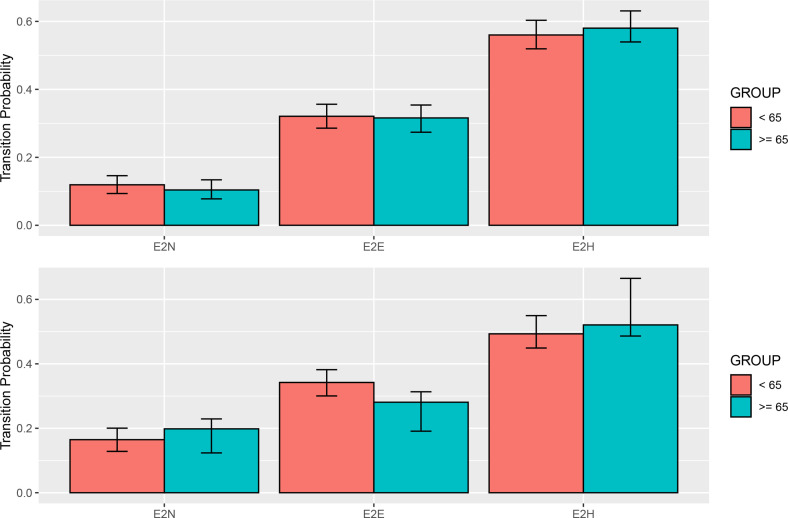
The six possible blood pressure state transitions with the corresponding probabilities over 1-year, 2-year and 3-year periods, stratified by gender, are illustrated in figures 2 and 3. Compared with male participants, female participants have lower probabilities of transitioning from the normal state to the hypertensive state, but have higher probabilities of moving from the elevated state to the hypertensive state over any period of time. For instance, elderly women in the normal state had a 16.97%, 33.30% and 47.31% chance of progressing to hypertension if the next check-up was performed after an interval of 1 year, 2 years and 3 years, respectively. By contrast, the chances of elderly men moving from the normal state to the hypertensive state were 21.73%, 38.56% and 51.70% within 1, 2 and 3 years, respectively. For elderly women starting in the elevated state, the probabilities of developing hypertension were 25.07%, 43.03% and 56.32% in the next 1, 2 and 3 years, respectively; while the corresponding probabilities for elderly men transitioning between the two states were 20.96%, 37.65% and 50.86%. As time went by, both female and male participants had a higher probability of developing hypertension. For example, the probabilities of changing from the normal state to the hypertensive state over a 1-year follow-up period were 16.97% (female) and 21.73% (male), which increased dramatically to 47.31% (female) and 51.70% (male) within the 3-year follow-up period.
Figure 2.
State transition diagrams for female participants.
Figure 3.
State transition diagrams for male participants.
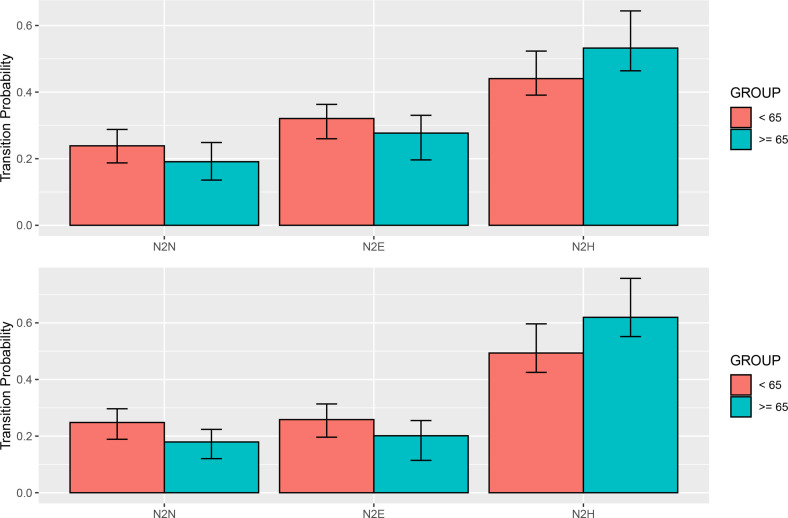
We further stratified the study individuals by gender and age group, and the transition probabilities in the third year originating from the normal state or the elevated state at baseline are illustrated in figure 4 and figure 5, respectively. The detailed corresponding numerical values are described in online supplemental table S1. As shown, both female and male participants with age ≧65 years were more likely to progress to hypertension whether starting from the normal state or the elevated state within the next 3 years, in comparison with the corresponding participants who were <65 years old.
Figure 4.
Transition probabilities from the normal state in the third year, stratified by gender and age group.
Figure 5.
Transition probabilities from the elevated state in the third year, stratified by gender and age group.
bmjopen-2021-059805supp001.pdf (36.2KB, pdf)
The sojourn time for the normal state in the study cohort was 1.5±0.08 years, and the duration of the elevated state was 2.0±0.07 years.
Covariate effects on blood pressure state transitions
The covariates included in the research were age, gender, marriage, BMI, glucose and ECG. The effects of the covariates on blood pressure state transition with statistical significance are summarised in table 4. Gender, BMI, age and glucose had some significant associations with possible transitions. For example, increasing age, BMI and glucose were risk factors for developing hypertension from the normal state or elevated state (HR 1.04–1.12). Female participants and participants with higher glucose levels were less likely to return from the elevated state to the normal state than their male counterparts (HR 0.61–0.83).
Table 4.
Covariate effects on blood pressure state transitions
| Covariate | Normal–Elevated HR (95% CI) |
Normal-Hypertensive HR (95% CI) |
Elevated–Normal HR (95% CI) |
Elevated –Hypertensive HR (95% CI) |
| Gender | 1.131 (0.807 to 1.586) | 0.544 (0.288 to 1.028) | 0.606 (0.412 to 0.891) | 1.461 (0.999 to 2.136) |
| BMI | 1.038 (0.992 to 1.086) | 1.124 (1.058 to 1.195) | 1.017 (0.963 to 1.074) | 1.019 (0.983 to 1.057) |
| Age | 1.016 (0.980 to 1.054) | 1.042 (1.010 to 1.075) | 1.018 (0.990 to 1.047) | 1.017 (0.997 to 1.037) |
| Glucose | 1.013 (0.947 to 1.083) | 0.876 (0.697 to 1.102) | 0.827 (0.715 to 0.956) | 1.054 (1.012 to 1.097) |
| Marriage | 0.989 (0.574 to 1.702) | 0.961 (0.347 to 2.665) | 1.073 (0.607 to 1.897) | 0.866 (0.630 to 1.189) |
| Abnormal ECG | 0.737 (0.516 to 1.052) | 0.920 (0.479 to 1.767) | 0.794 (0.545 to 1.155) | 1.026 (0.825 to 1.275) |
Reference categories of covariates: gender, ref=male; marriage, ref=single/divorced/widowed; abnormal ECG, ref=normal.
BMI, body mass index.
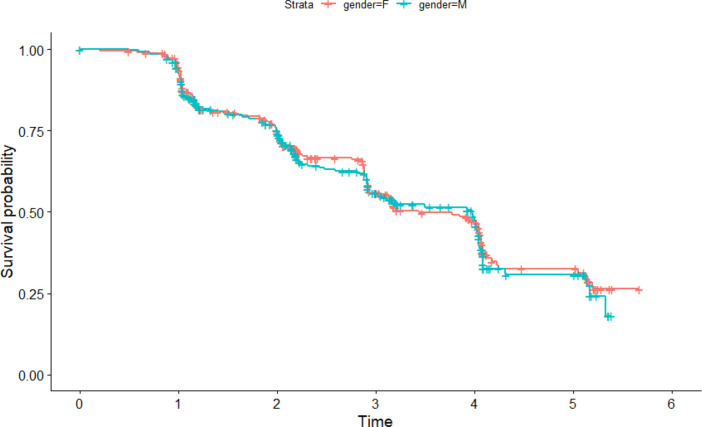
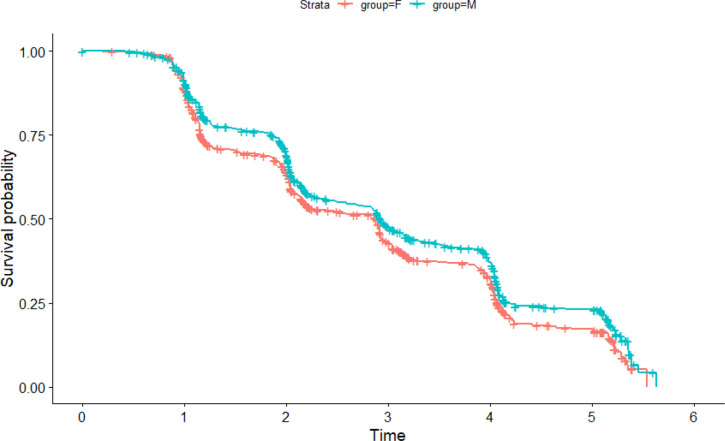
Survival probability based on the multistate Markov model
The multistate Markov model can be used to infer the survival probability for each subgroup in the future, which may provide insightful information for individuals. In this study, the survival probability represents the probability of not transitioning into the hypertensive state. Survival probability curves over 5 years for all subgroups stratified by female and male categories are given in figures 6 and 7. The survival probability decreased significantly with increased time among all subgroups. As shown in figure 6, the survival probability for female participants originating from the normal state was similar to the probability for male participants (no difference, p=0.70). Figure 7 illustrates that male participants starting from the elevated state had a higher survival probability over 5 years than female participants (p=0.01).
Figure 6.
Survival distribution starting from the normal state.
Figure 7.
Survival distribution starting from the elevated state.
Discussion
Sound evidence has verified that, when compared with the young population, elderly people have a higher incidence of hypertension, which is worthy of more attention and investigation.29 In 2020, there were 254 million people aged ≥60 years in China, accounting for 18.1% of the population.40 Therefore, in this study, we explored the state transition dynamics of three blood pressure states via multi-state Markov models and investigated the risk factors associated with the progression of hypertension in the elderly population in China, which has not been explored in the existing literature.
There are some significant findings in the research. First, our study found that, of the 3168 transitions, 26.15% of participants showed deterioration from the normal state to the hypertensive state at the next check-up, much higher than the corresponding 16.98% and 9.18% reported in previous studies of the working population.28 29 This further confirmed that older people should be given much more attention in hypertension prevention and research. Second, we found that both female and male participants in the normal state had a low probability of developing hypertension in the first year; however, this probability increased substantially in the following 3 years, which is consistent with the prior research on young people.28 29 In this study, the percentage changes from the normal state to the hypertensive state in the first year were 16.97% (female) and 21.73% (male), which increased dramatically to 47.31% (female) and 51.70% (male) within the 3-year follow-up period. Furthermore, the sojourn time in the normal state was 1.5±0.08 years in the study cohort. These results indicate that preventive actions and effective intervention on hypertension progression should be conducted at an early stage, and at least 1 yearly check-up is strongly recommended for the elderly population. Third, male participants were found to have high probabilities of transitioning from the normal state to hypertension, in comparison with female participants. For example, elderly women in the normal state have a 16.97%, 33.30% and 47.31% chance of progressing to hypertension within 1, 2 and 3 years, respectively. By contrast, the corresponding probabilities for elderly men were 21.73%, 38.56% and 51.70%, respectively. The findings align with those of a prior study that indicated that more attention should be paid to elderly men with normotension.28 41 42
However, we also found that elderly female participants had higher probabilities of developing from the elevated state to the hypertensive state than male participants. For instance, for elderly women starting in the elevated state, the probabilities of developing hypertension were 25.07%, 43.03% and 56.32% in the next 1, 2 and 3 years, respectively; the corresponding probabilities for elderly men were 20.96%, 37.65% and 50.86%, respectively. Female participants were less likely to return from the elevated state to the normal state than their male counterparts in the study (HR 0.61, 95% CI 0.41 to 0.89). Our survival probability pilot also illustrated that male participants starting from the elevated state had a higher survival probability over 5 years than female participants (p=0.01). The above findings show that more attention should be paid to the progression from the elevated state to hypertension in elderly women. In this study, if an elderly individual was diagnosed with elevated blood pressure, health professionals in the community health centre provided a face-to-face health education session and sent text messages to the patient describing how to prevent hypertension through diet, exercise, daily blood pressure testing, etc.
In addition to age and gender, as discussed above, higher BMI (HR 1.12, 95% CI 1.06 to 1.20) and blood glucose levels (HR 1.05, 95% CI 1.01 to 1.10) were identified to be risk factors for developing hypertension from the normal state or elevated state. Previous research has also found that the HR for transitioning from the normal state to the hypertensive state increases with higher BMI values28 29 43 and higher glucose levels.44
In summary, the research has made key contributions. First, a multistate Markov model was used to explore the state transition dynamics of three blood pressure states, and to investigate how several important covariates affected the progression or alleviation of hypertension in the Chinese elderly population. Furthermore, through the developed model, the sojourn time in each blood pressure state and the transition probabilities from one state to another state were estimated, thereby supplying statistical foundations for preventive actions and effective intervention in the progression of hypertension for elderly people.
Limitations
The limitations of the study can be summarised as follows: (1) Owing to time and financial limitations, we only focused on a cohort population for 5 years in one city; thus the study findings may not be representative and fit for extrapolation; (2) In this study, the hypertensive state was regarded as an absorbing state, meaning that the reverse transition from a hypertensive state to a normal or elevated state was not considered and (3) Some significant covariates, such as various lifestyle habits of diet, smoking, exercise, other medical conditions and psychological status, were not covered in the current study, and are worthy of investigation in further research.
Conclusions
The findings regarding the three blood pressure state transition probabilities should increase awareness of the timely prevention for elderly women with elevated blood pressure and elderly men with normal blood pressure. Preventive actions and effective intervention on hypertension progression should be conducted at an early stage, and at least 1 yearly check-up is strongly recommended for elderly people. Increasing age, BMI and blood glucose were risk factors for developing hypertension from the normal state or elevated state. The derived transition probabilities and sojourn time can serve as a significant reference for health professionals when developing proactive and targeted interventions for hypertension progression among the Chinese elderly population.
Supplementary Material
Acknowledgments
We would like to thank all participants who voluntarily participated in this study.
Footnotes
XZ and JX contributed equally.
Contributors: XZ and JX performed the statistical analysis and interpretation and wrote the manuscript. YZ, LX and LZ contributed to the conceptualisation of the research process and critically reviewed the manuscript. BZ and YW were responsible for the overall content as guarantors. All authors read and approved the final manuscript. Other author footnotes: XZ and JX made equal contributions to this manuscript.
Funding: YW was supported by grants from the Fujian Province Planning Project of Science and Technology (2019D015). JX was supported by the Medical Science and Technology Research Fund Project of Guangdong Province (grant no. A2020405).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s)
Ethics approval
This study was approved by the review committee of the No. 2 Affiliated Hospital of Xiamen Medical College (2018005). Participants gave informed consent to participate in the study before taking part.
References
- 1.Liu LS. Chinese guidelines for the management of hypertension. Zhonghua Xin Xue Guan Bing Magazine 2010;2011:579–615. [PubMed] [Google Scholar]
- 2.Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J 2018;39:3021–104. 10.1093/eurheartj/ehy339 [DOI] [PubMed] [Google Scholar]
- 3.Herman WW, Konzelman JL, Prisant LM, Joint national committee on prevention, detection, evaluation, and treatment of high blood pressure . The seventh report of the joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Bethesda (MD: National heart, lung, and blood institute (US), 2004. [PubMed] [Google Scholar]
- 4.Lawes CMM, Vander Hoorn S, Rodgers A, et al. Global burden of blood-pressure-related disease, 2001. Lancet 2008;371:1513–8. 10.1016/S0140-6736(08)60655-8 [DOI] [PubMed] [Google Scholar]
- 5.Kokubo Y, Matsumoto C. Hypertension is a risk factor for several types of heart disease: review of prospective studies. Adv Exp Med Biol 2017;956:419–26. 10.1007/5584_2016_99 [DOI] [PubMed] [Google Scholar]
- 6.Oparil S, Acelajado MC, Bakris GL, et al. Hypertension. Nat Rev Dis Primers 2018;4:1–21. 10.1038/nrdp.2018.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tackling G, Borhade MB, Tackling G. Hypertensive heart disease. In: StatPearls. Treasure Island (FL): StatPearls Publishing, 2020. https://www.ncbi.nlm.nih.gov/books/NBK539800/ [PubMed] [Google Scholar]
- 8.Jan Y-T, Tsai P-S, Longenecker CT, et al. Thoracic aortic calcification and pre-clinical hypertension by new 2017 ACC/AHA hypertension guidelines. Diagnostics 2021;11:1027. 10.3390/diagnostics11061027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 2016;387:957–67. 10.1016/S0140-6736(15)01225-8 [DOI] [PubMed] [Google Scholar]
- 10.Khaja SU, Mathias KC, Bode ED, et al. Hypertension in the United States fire service. Int J Environ Res Public Health 2021;18:5432. 10.3390/ijerph18105432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.GBD 2015 Risk Factors Collaborators . Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the global burden of disease study 2015. Lancet 2016;388:1659–724. 10.1016/S0140-6736(16)31679-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Di Palo KE, Barone NJ. Hypertension and heart failure: prevention, targets, and treatment. Heart Fail Clin 2020;16:99–106. 10.1016/j.hfc.2019.09.001 [DOI] [PubMed] [Google Scholar]
- 13.Dominguez LJ, Veronese N, Barbagallo M. Magnesium and hypertension in old age. Nutrients 2021;13:139. 10.3390/nu13010139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ye X, Yi Q, Shao J, et al. Trends in prevalence of hypertension and hypertension phenotypes among Chinese children and adolescents over two decades (1991-2015). Front Cardiovasc Med 2021;8:627741. 10.3389/fcvm.2021.627741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kearney PM, Whelton M, Reynolds K, et al. Global burden of hypertension: analysis of worldwide data. Lancet 2005;365:217–23. 10.1016/S0140-6736(05)17741-1 [DOI] [PubMed] [Google Scholar]
- 16.Forouzanfar MH, Liu P, Roth GA, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990-2015. JAMA 2017;317:165–82. 10.1001/jama.2016.19043 [DOI] [PubMed] [Google Scholar]
- 17.WHO . Hypertension, 2019. Available: https://www.who.int/newsroom/factsheets/detail/hypertension [Accessed 2 Oct 2020].
- 18.Griffin G. Antiplatelet therapy and anticoagulation in patients with hypertension. Am Fam Physician 2005;71:897–9. [PubMed] [Google Scholar]
- 19.Xiong X, Yang X, Liu Y, et al. Chinese herbal formulas for treating hypertension in traditional Chinese medicine: perspective of modern science. Hypertens Res 2013;36:570–9. 10.1038/hr.2013.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chow CK, Teo KK, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA 2013;310:959–68. 10.1001/jama.2013.184182 [DOI] [PubMed] [Google Scholar]
- 21.Patel RS, Masi S, Taddei S. Understanding the role of genetics in hypertension. Eur Heart J 2017;38:2309–12. 10.1093/eurheartj/ehx273 [DOI] [PubMed] [Google Scholar]
- 22.Li C, Sun D, Liu J, et al. A prediction model of essential hypertension based on genetic and environmental risk factors in northern Han Chinese. Int J Med Sci 2019;16:793–9. 10.7150/ijms.33967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bigazzi R, Zagato L, Lanzani C, et al. Hypertension in high school students: genetic and environmental factors: the HYGEF study. Hypertension 2020;75:71–8. 10.1161/HYPERTENSIONAHA.119.13818 [DOI] [PubMed] [Google Scholar]
- 24.Zhang Y, Yang H, Ren M, et al. Distribution of risk factors of hypertension patients in different age groups in Tianjin. BMC Public Health 2021;21:247. 10.1186/s12889-021-10250-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shihab HM, Meoni LA, Chu AY, et al. Body mass index and risk of incident hypertension over the life course: the Johns Hopkins precursors study. Circulation 2012;126:2983–9. 10.1161/CIRCULATIONAHA.112.117333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tohidi M, Hatami M, Hadaegh F, et al. Triglycerides and triglycerides to high-density lipoprotein cholesterol ratio are strong predictors of incident hypertension in middle Eastern women. J Hum Hypertens 2012;26:525–32. 10.1038/jhh.2011.70 [DOI] [PubMed] [Google Scholar]
- 27.Zhang W, Wang L, Chen Y, et al. Identification of hypertension predictors and application to hypertension prediction in an urban Han Chinese population: a longitudinal study, 2005-2010. Prev Chronic Dis 2015;12:E184. 10.5888/pcd12.150192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang J, Liu F, Wang B, et al. Blood pressure states transition inference based on multi-state Markov model. IEEE J Biomed Health Inform 2021;25:237–46. 10.1109/JBHI.2020.3006217 [DOI] [PubMed] [Google Scholar]
- 29.Wang Y, Ma Z, Xu C, et al. Prediction of transfer among multiple states of blood pressure based on Markov model: an 18-year cohort study. J Hypertens 2018;36:1506–13. 10.1097/HJH.0000000000001722 [DOI] [PubMed] [Google Scholar]
- 30.Mills KT, Obst KM, Shen W, et al. Comparative effectiveness of implementation strategies for blood pressure control in hypertensive patients: a systematic review and meta-analysis. Ann Intern Med 2018;168:110–20. 10.7326/M17-1805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tada T, Kumada T, Toyoda H, et al. Long-Term natural history of liver disease in patients with chronic hepatitis B virus infection: an analysis using the Markov chain model. J Gastroenterol 2018;53:1196–205. 10.1007/s00535-018-1467-x [DOI] [PubMed] [Google Scholar]
- 32.Wong LY, Toh MPHS, Tham LWC. Projection of prediabetes and diabetes population size in Singapore using a dynamic Markov model. J Diabetes 2017;9:65–75. 10.1111/1753-0407.12384 [DOI] [PubMed] [Google Scholar]
- 33.Grover G, Sabharwal A, Kumar S, et al. A multi-state Markov model for the progression of chronic kidney disease. Turkiye Klinikleri J Biostat 2019;11:1–14. 10.5336/biostatic.2018-62156 [DOI] [Google Scholar]
- 34.Brookmeyer R, Abdalla N. Multistate models and lifetime risk estimation: Application to Alzheimer’s disease. Stat Med 2019;38:1558–65. 10.1002/sim.8056 [DOI] [PubMed] [Google Scholar]
- 35.Srikanth P. Using Markov chains to predict the natural progression of diabetic retinopathy. Int J Ophthalmol 2015;8:383 132–7. 10.3980/j.issn.2222-3959.2015.01.25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Attard SM, Herring AH, Zhang B, et al. Associations between age, cohort, and urbanization with SBP and DBP in China: a population-based study across 18 years. J Hypertens 2015;33:948–56. 10.1097/HJH.0000000000000522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guo J, Zhu Y-C, Chen Y-P, et al. The dynamics of hypertension prevalence, awareness, treatment, control and associated factors in Chinese adults: results from CHNS 1991-2011. J Hypertens 2015;33:1688–96. 10.1097/HJH.0000000000000594 [DOI] [PubMed] [Google Scholar]
- 38.Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 2003;42:1206–52. 10.1161/01.HYP.0000107251.49515.c2 [DOI] [PubMed] [Google Scholar]
- 39.Jackson CH. Multi-state models for panel data: the msm package for R. J Stat Softw 2011;38:1–28. 10.18637/jss.v038.i08 [DOI] [Google Scholar]
- 40.China development research foundation . China development report-aging population in 2020: development trend and policy options, 2020. Available: http://www.199it.com/archives/1068230.html
- 41.Singh S, Shankar R, Singh GP. Prevalence and associated risk factors of hypertension: a cross-sectional study in urban Varanasi. Int J Hypertens 2017;2017:1–10. 10.1155/2017/5491838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Faulkner JL, Belin de Chantemèle EJ. Sex differences in mechanisms of hypertension associated with obesity. Hypertension 2018;71:15–21. 10.1161/HYPERTENSIONAHA.117.09980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Davis J, Juarez D, Hodges K. Relationship of ethnicity and body mass index with the development of hypertension and hyperlipidemia. Ethn Dis 2013;23:65–70. [PMC free article] [PubMed] [Google Scholar]
- 44.Huang Z, Wang G, Jonas JB, et al. Blood pressure control and progression of arteriosclerosis in hypertension. J Hypertens 2021;39:1221–9. 10.1097/HJH.0000000000002758 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-059805supp001.pdf (36.2KB, pdf)
Data Availability Statement
Data are available on reasonable request.