Abstract
This randomized controlled trial (NCT03889821) examined Mindfulness Based Stress Reduction (MBSR) in conjunction with the Parent-implemented Early Start Denver Model (P-ESDM). A previous report described improved metrics of parental distress (Weitlauf et al., 2020). This manuscript examines child outcomes. Sixty-three children with ASD (< 36 months) and their parents received 12 P-ESDM sessions. Half of parents also received MBSR. Longitudinal examination of whole sample means revealed modest improvements in autism severity, cognitive, and adaptive skills. There was not a significant time × group interaction for children whose parents received MBSR. Future work should examine more proximal markers of child or dyadic change to enhance understanding of the impact of providing direct treatment for parents as part of early intervention initiatives.
Keywords: P-ESDM, mindfulness, young children, autism spectrum disorder
Although low-intensity parent-mediated interventions for young children with or at-risk of Autism Spectrum Disorder (ASD) have gained momentum over the past decade, (Rogers et al., 2019; Stahmer et al., 2020; Wetherby et al., 2018), evidence of their impact on child developmental outcomes such as cognitive skills, adaptive skills, and autism symptom severity remains unclear (Oono, Honey, & McConachie, 2013; Weitlauf, McPheeters, et al., 2014). Parent-mediated intervention protocols can give parents the skills to support their children during naturalistic, everyday interactions (Estes, Swain, & Macduffie, 2019; Rogers et al., 2012; Rogers et al., 2019; Stahmer et al., 2020; Wetherby et al., 2018), buffering parents against increased stress (Estes et al., 2014; Rollins, John, Jones, & De Froy, 2019) and potentially reducing the need for intensive one-on-one care in the face of provider shortages (Zhang & Cummings, 2020). In the midst of this emphasis on parent training, a well-established literature documents that parents of children with ASD are at increased risk of heightened psychological and parenting distress. However, few studies have paired parent-mediated early intervention with targeted support for parents’ own wellbeing, rather than parental motivation or skill in intervention implementation. Little is known about whether directly treating parental distress as part of an early intervention protocol has positive impacts on young children with ASD.
Broadly, evidence for low-intensity early childhood parent training programs for ASD supports their potential for teaching parents new skills and, potentially, reducing or protecting against stress (Estes et al., 2019; Rogers et al., 2019; Rollins et al., 2019; Stahmer et al., 2020; Tarver et al., 2019; Vibert et al., 2020; Weitlauf et al., 2020). However, data remain inconclusive regarding impact on child outcomes, including which outcomes are most likely to be affected and how to predict parent and child response to treatment (Bearss et al., 2015; Schreibman et al., 2015; Weitlauf, McPheeters, et al., 2014). For example, a recent small study within a state early intervention system compared Project imPACT for Toddlers versus usual care for 12- to 30-month-old children at-risk of ASD. Parents who received Project imPACT showed significantly more positive parent-child interactions, while gains on child variables such as social-communication skills were promising but non-significant (Stahmer et al., 2020). Another commonly used and well-researched parent-mediated early intervention paradigm for ASD is the Parent-implemented Early Start Denver Model (Rogers et al., 2012). Early work comparing P-ESDM to treatment-as-usual for 14- to 24-month-old children found that, after 12-weeks, parents receiving P-ESDM report stronger therapeutic alliances with therapists, but children across both groups made comparable developmental gains. In a recent examination of an intervention offering12-weeks of clinic-based P-ESDM alone versus clinic-based P-ESDM enhanced with parental motivational interviewing as well as a home visit, Rogers et al. found immediate post-treatment differences regarding parental ability to implement aspects of the intervention, but did not find group differences in child developmental outcomes such as level of ASD symptoms, cognitive skills, or adaptive skills for these 12- to 30-month-old participants (Rogers et al., 2019).
In addition to the strengths and improvements described above, numerous studies have documented higher levels of parental distress in ASD relative to the parents of children with other developmental disabilities (Dykens, Fisher, Taylor, Lambert, & Miodrag, 2014; Estes et al., 2013; Seymour, Giallo, & Wood, 2017; Taylor & Warren, 2012; Warren, Vehorn, Dohrmann, Newsom, & Taylor, 2013). This stress may be heightened related to receiving an ASD diagnosis (Bohadana, Morrissey, & Paynter, 2020; Weitlauf, Vehorn, Taylor, & Warren, 2014) and be influenced by degree of self-reported resolution with the diagnostic outcome (Reed & Osborne, 2019). Parent stress is likely to have subsequent impacts on self-perceptions of relationships with children, physical health, and ability to navigate systems of care (Bohadana et al., 2020; Nicholas, Macculloch, Roberts, Zwaigenbaum, & McKeever, 2020). Amidst these experiences, parents may be asked to implement an intervention protocol that requires them to learn and then implement strategies within the home (Bearss et al., 2015; Gunning, Holloway, & Grealish, 2020; Pellecchia et al., 2020; Schaefer & Andzik, 2020). Therefore, it is important to understand whether directly supporting parental wellbeing within the context of parent-mediated early intervention for ASD makes a differential impact on children’s developmental gains.
One method of promoting parental wellbeing is through the teaching of Mindfulness Based Stress Reduction (MBSR) (Kabat-Zinn & Chapman-Waldrop, 1988; Kabat-Zinn et al., 1992). In healthy adults as well as adults diagnosed with anxiety or mood disorders, MBSR has been shown to reduce anxiety, stress, distress, and depressive symptoms (Goldin et al., 2016; Hoge et al., 2013; Khoury, Sharma, Rush, & Fournier, 2015). Additional work has examined MBSR for adults that experience chronic pain, stress, or burnout due to chronic illness, job type, or intense caregiving roles such as those experienced by parents of children with ASD. For example, MBSR has been shown to reduce stress or burnout for healthcare providers and learners (Kriakous, Elliott, Lamers, & Owen, 2020; Lamothe, Rondeau, Malboeuf-Hurtubise, Duval, & Sultan, 2016; Lebares et al., 2018; Song & Lindquist, 2015), educators (Miller, Fletcher, & Kabat-Zinn, 1995; Todd, Cooksey, Davies, McRobbie, & Brophy, 2019), caregivers of people with dementia (K. W. Brown, Coogle, & Wegelin, 2016), and individuals with chronic pain (Cash et al., 2015; Khoo et al., 2019; Smith & Langen, 2020). Given the negative impacts of parental distress and mental health diagnoses on child wellbeing in the general population (Goodman et al., 2011; Hattangadi et al., 2020; Kamis, 2021; Uddin et al., 2020), it follows that offering stress tolerance and reduction strategies for children with ASD may also yield positive downstream impacts by improving aspects of parental wellbeing.
In an earlier publication (Weitlauf et al., 2020), we presented parent data from a randomized controlled trial of P-ESDM with and without Mindfulness Based Stress Reduction (MBSR) for parents. Relative to parents who participated in P-ESDM only, parents who also received MBSR reported reduced parental distress and increased mindfulness. Main effects across combined groups emerged, with some child variables impacting parent functioning: high parental distress at baseline related to younger child age, with high baseline depression related to parent-reported levels of child challenging behavior. In the current work, a companion to the original publication that is derived from the same study protocol and sample, we present results of planned analyses examining changes in key markers of child development. Specifically, we examined 1) between-group differences in child adaptive skills, cognitive skills, and autism symptoms over time and 2) overall group impacts of P-ESDM on longitudinal outcomes.
Methods
Full study details are described in an earlier publication (Weitlauf et al., 2020). All parents and children participated in 12 sessions of P-ESDM. Parents randomized to the MBSR condition received six sessions of MBSR based upon work by Dykens et al. (2014) and modified for the parents of young children with new diagnoses of ASD. These sessions, which involved only the parent (no children present), lasted for one hour per week and began approximately two weeks after P-ESDM initiation. Select information regarding child participants and the P-ESDM protocol are presented below.
Participants
Participants were recruited from an outpatient tertiary care ASD diagnostic clinic between 2015–2017. Eligibility criteria included being less than 36 months of age at time of consent and meeting criteria for a diagnosis of ASD based on comprehensive developmental evaluation (described below). Additional eligibility criteria included parental English proficiency. Exclusion criteria included severe child sensorimotor impairment (e.g., not walking, significant trouble with vision or hearing) that could not be corrected and would impact ability to participate in intervention tasks or assessment activities. All procedures were approved by the medical center Institutional Review Board. No adverse events were reported.
Of 103 eligible families, 63 consented to participate (see Weitlauf et al., 2020 for CONSORT chart) and provided usable child data. Half of participants were placed in each group based upon parental treatment condition (P-ESDM only; P-ESDM + MBSR). Randomization was accomplished prior to recruitment using an online random number generator. A unique computer file was created for each possible participant number that contained group assignment. A blinded member of the study staff only opened that file and informed the participant of group assignment after consent was obtained. One parent withdrew from the study prior to providing any data. Our final child sample included 62 participants (P-ESDM = 32, P-ESDM + MBSR = 30) who were included in analyses. Of these, 7 families withdrew before completing their third P-ESDM session, and an additional 8 families were lost to 6- month follow-up. Attrition rates did not differ by parent intervention group or demographic variables.
Mean child age at time of enrollment was 2.28 years (sd = .45 years). The majority of participants were male (n = 49). The sample was predominantly White (n = 52) as well as Asian (n = 4), Black or African-American (n = 2), and Native American (n = 2). Mean annual household income was approximately $65,000 per year (sd = $32,000).
We examined the mean number of hours of outside intervention (developmental childcare center or preschool; speech therapy; occupational therapy, or applied behavior analytic services) that participants received across groups and over time (see Table 1). Although some variability emerged in number of participants in treatment, differences were generally small, with high standard deviations reflecting variability across individuals within this relatively small sample.
Table 1.
Number of participants (n) enrolled in outside therapies and average hours per month, over time and by group.
| T1 | T2 | T3 | |
|---|---|---|---|
|
| |||
| ADOS-2 Calibrated Severity Score | |||
|
| |||
| P-ESDM | 8.34 (1.49) | 7.45 (1.70) | 7.58 (1.91) |
| P-ESDM + MBSR | 7.93 (1.76) | 7.10 (2.06) | 7.08 (2.00) |
| Total Sample | 8.15 (1.63) | 7.33 (1.86) | 7.33 (1.95) |
|
| |||
| MSEL Early Learning Composite - T-Score Mean (sd) | |||
|
| |||
| P-ESDM | 55.75 (13.32) | 55.76 (11.59) | 55.84 (12.06) |
| P-ESDM + MBSR | 60.07 (10.18) | 61.15 (16.24) | 68.13 (20.15) |
| Total Sample | 57.73 (12.08) | 58.31 (14.11) | 61.86 (17.49) |
|
| |||
| MSEL Expressive Language - Raw Score Mean (sd) | |||
|
| |||
| P-ESDM | 11.53 (5.05) | 14.97 (6.42) | 17.68 (9.03) |
| P-ESDM + MBSR | 11.75 (5.20) | 17.62 (8.28) | 22.05 (9.05) |
| Total Sample | 11.63 (5.08) | 16.22 (7.41) | 19.82 (9.21) |
|
| |||
| MSEL Receptive Language - Raw Score Mean (sd) | |||
|
| |||
| P-ESDM | 10.41 (5.45) | 15.62 (6.07) | 17.08 (8.97) |
| P-ESDM + MBSR | 12.29 (7.50) | 19.04 (7.41) | 23.12 (9.82) |
| Total Sample | 11.28 (6.50) | 17.35 (6.89) | 20.04 (9.79) |
|
| |||
| MSEL Fine Motor - Raw Score Mean (sd) | |||
|
| |||
| P-ESDM | 20.44 (2.79) | 21.76 (3.41) | 24.64 (5.51) |
| P-ESDM + MBSR | 20.45 (4.04) | 23.23 (2.17) | 25.38 (4.95) |
| Total Sample | 20.44 (3.41) | 22.45 (3.35) | 25.00 (5.20) |
|
| |||
| MSEL Visual Reception - Raw Score Mean (sd) | |||
|
| |||
| P-ESDM | 20.44 (2.79) | 21.76 (3.50) | 24.95 (7.47) |
| P-ESDM + MBSR | 20.89 (4.31) | 24.77 (4.59) | 28.08 (5.90) |
| Total Sample | 20.52 (4.56) | 23.38 (4.35) | 26.49 (6.86) |
|
| |||
| VABS-II Interpersonal Skills – Raw Score Mean (sd) | |||
|
| |||
| P-ESDM | 21.41 (4.02) | 24.31 (6.14) | 26.00 (6.61) |
| P-ESDM + MBSR | 21.04 (5.31) | 25.35 (4.77) | 27.50 (6.47) |
| Total Sample | 21.23 (4.63) | 24.80 (5.51) | 26.73 (6.52) |
|
| |||
| VABS-II Play Skills – Raw Score Mean (sd) | |||
|
| |||
| P-ESDM | 8.53 (2.97) | 11.79 (6.05) | 12.92 (7.07) |
| P-ESDM + MBSR | 9.21 (2.70) | 11.58 (5.79) | 16.04 (7.60) |
| Total Sample | 8.85 (2.85) | 11.69 (5.88) | 14.45 (7.43) |
|
| |||
| VABS-II Receptive Language – Raw Score Mean (sd) | |||
|
| |||
| P-ESDM | 12.22 (7.28) | 17.76 (7.15) | 18.56 (7.50) |
| P-ESDM + MBSR | 13.29 (8.07) | 19.81 (7.80) | 22.46 (7.02) |
| Total Sample | 12.72 (7.61) | 18.73 (7.47) | 20.47 (7.46) |
|
| |||
| VABS-II Expressive Language – Raw Score Mean (sd) | |||
|
| |||
| P-ESDM | 20.75 (14.37) | 28.86 (16.78) | 33.40 (18.93) |
| P-ESDM + MBSR | 18.32 (9.10) | 31.08 (16.65) | 41.79 (21.71) |
| Total Sample | 19.62 (12.16) | 29.91 (16.14) | 37.61 (20.56) |
Note. All between-group T1-T2 and T2-T3 comparisons non-significant (ps > .05).
ADOS-2 = Autism Diagnostic Observation Schedule, Second Edition. MSEL = Mullen Scales of Early Learning. VABS-II = Vineland Adaptive Behavior Scales, Second Edition.
Measures
Autism symptoms.
The Autism Diagnostic Observation Schedule – Second Edition (ADOS-2) is a standardized clinical observation system for use with people with developmental ages of 12 months and older.(C. Lord et al., 2000) Each module yields Calibrated Severity Scores (CSS; range: 1–10) based on age group and language level, which were used in these analyses. Higher scores reflect higher levels of autism symptoms. Although many children transitioned between ADOS-2 modules based upon their ages over the course of the study, the utilization of the standardized severity score should minimize any impact (Esler et al., 2015).
Cognitive Assessment.
The Mullen Scales of Early Learning (MSEL) is a standardized developmental test for children up to age five years (Mullen, 1995). It provides four domain scores (Visual Reception, Fine Motor, Receptive Language, Expressive Language) and yields an overall ability index (Early Learning Composite, ELC; M=100, SD=15). Higher scores reflect higher ability levels. Although widely used in research for young children with ASD (Girault et al., 2020; Masi et al., 2021; McClure et al., 2021), standard scores for children with significant communication and developmental concerns may suffer from a floor effect that muffles the ability to detect small change in skill. As such, in this work, we examined the overall ELC as well as the raw domain scores.
Adaptive Functioning.
The Vineland Adaptive Behavior Scales – Second Edition (VABS-II), Interview Form is a semi-structured parent interview (Sparrow & Cicchetti, 1985). It yields four domain standard scores: Communication, Daily Living Skills, Socialization, and Motor Skills (M = 100, SD = 15), and an overall Adaptive Behavior Composite (M = 100, SD = 15). Higher scores reflect better-developed adaptive behavior skills. In this work, we examined the impact on overall ABC scores as well as the subdomains of Socialization and Communication, both of which are primary emphases of the P-ESDM curriculum. Similar to the MSEL, we present the overall ABC as well as raw subscale scores.
Intervention
P-ESDM.
As described in Weitlauf et al. (2020), all children received P-ESDM. The P-ESDM intervention consisted of 12 consecutive weekly clinic-based sessions, each of which lasted approximately one hour and included the child, one parent, and a therapist. P-ESDM began approximately 1.35 months after diagnosis (sd = 1.45 weeks) and took an average of 15.87 weeks (sd = 3.33 weeks) to complete due to accommodating families’ schedules. P-ESDM therapists included six licensed Board Certified Behavior Analysts trained to fidelity by ESDM-certified trainers. P-ESDM is a manualized intervention with a detailed parent-training curriculum and a specific coaching intervention method (Rogers et al., 2012). Therapists introduce skills through written and verbal descriptions, modeling, guided practice, and feedback, with embedded emphasis on skill generalization. Based upon application of the P-ESDM Fidelity Checklist, therapists covered 94% of intended content across sessions, with no significant differences between groups (p > .10). Regarding parent implementation of session strategies, an independent samples t-test of therapist ratings of parent performance indicated that parents implemented strategies within sessions at equal levels across groups (t(51) = −.20, p > .10). There were no differences in parent implementation across treatment groups.
P-ESDM + MBSR.
The 30 parents randomized to P-ESDM + MBSR attended six additional one-hour individual sessions, without their children present. Sessions focused on teaching, reviewing, and practicing targeted stress reduction strategies chosen for their potential realistic applicability to the parents of very young children with developmental concerns. Fidelity of the MBSR intervention was tracked using fidelity checklists that therapists completed at the end of each visit. Fidelity of covering required topics across all completed sessions was 97.9%. The four MBSR therapists were clinicians with at least a Master’s degree and expertise in behavioral intervention and ASD. MBSR therapists were, supervised by a licensed clinical psychologist with formal MBSR training. The MBSR protocol was based upon the work of Dykens et al. (2014) and modified for individual administration for parents of young children with ASD (Weitlauf et al., 2020).
Analytic Plan
We analyzed change across two periods of time: from baseline (T1) to end of treatment (T2), a span of 3 months; and from end of treatment (T2) to end of study (T3), a span of 6 months. This allowed us to assess the impact of treatment during active treatment itself, and, then, during the post-treatment window to better understand immediate effects as well as the maintenance of effects over time. Mean changes over time by treatment group were estimated using separate linear mixed effects models for each outcome. Fixed effects were time, treatment, and the time by treatment interactions, and random intercepts were included to account for repeated measures correlation. The linear mixed effects model assumes that missing values at any given time point are missing at random, so we are able to use all collected data for a subject even if missing one or two time points. Likelihood ratio tests (3 d.f.) were used to determine if there was any effect of treatment at any of the three time points.
Results
Change over time by treatment group.
We did not find significant differences across treatment groups. As seen in Table 2, children whose parents did or did not receive MBSR performed similarly at all timepoints (ps > .05). Although the T3 scores on the VABS-II Communication domain appear different, this did not reach significance (p = .056).
Table 2.
Child developmental assessment scores.
| T1 (Start of Treatment) | T2 (Post-Treatment) | T3 (6-month Follow-Up) | ||||
|---|---|---|---|---|---|---|
| P-ESDM | P-ESDM+MBSR | P-ESDM | P-ESDM+MBSR | P-ESDM | P-ESDM+MBSR | |
| Developmental childcare or preschool | n = 7 | n = 5 | n = 8 | n = 6 | n = 10 | n = 9 |
| Hours/month (mean, sd) | 8.23 (21.35) | 5.44 (16.82) | 18.10 (31.41) | 12.38 (22.84) | 41.47 (52.56) | 41.71 (44.36) |
| Speech therapy | n = 10 | n = 12 | n = 10 | n = 10 | n = 10 | n = 10 |
| Hours/month (mean, sd) | 1.47 (2.24) | 2.57 (3.58) | 1.77 (2.63) | 2.00 (2.71) | 3.63 (4.56) | 2.63 (2.82) |
| Occupational therapy | n = 15 | n = 17 | n = 14 | n = 13 | n = 11 | n = 10 |
| Hours/month (mean, sd) | 2.16 (2.44) | 2.70 (2.67) | 2.00 (2.07) | 2.57 (2.52) | 3.70 (4.26) | 3.28 (2.72) |
| ABA therapy | n = 7 | n = 3 | n = 10 | n = 9 | n = 9 | n = 5 |
| Hours/month (mean, sd) | 2.00 (4.41) | 0.64 (1.97) | 5.46 (10.89) | 4.13 (8.31) | 6.64 (7.82) | 4.13 (8.31) |
Change over time across groups.
Next, we combined the sample to investigate the impact of P-ESDM on child outcomes during and after treatment (see Table 1). Severity scores on the ADOS-2 decreased from T1 to T2 (−.82 points; p < .01) but did not change from T2 to T3 (.05 points; p > .10, see Fig. 1).
Figure 1.
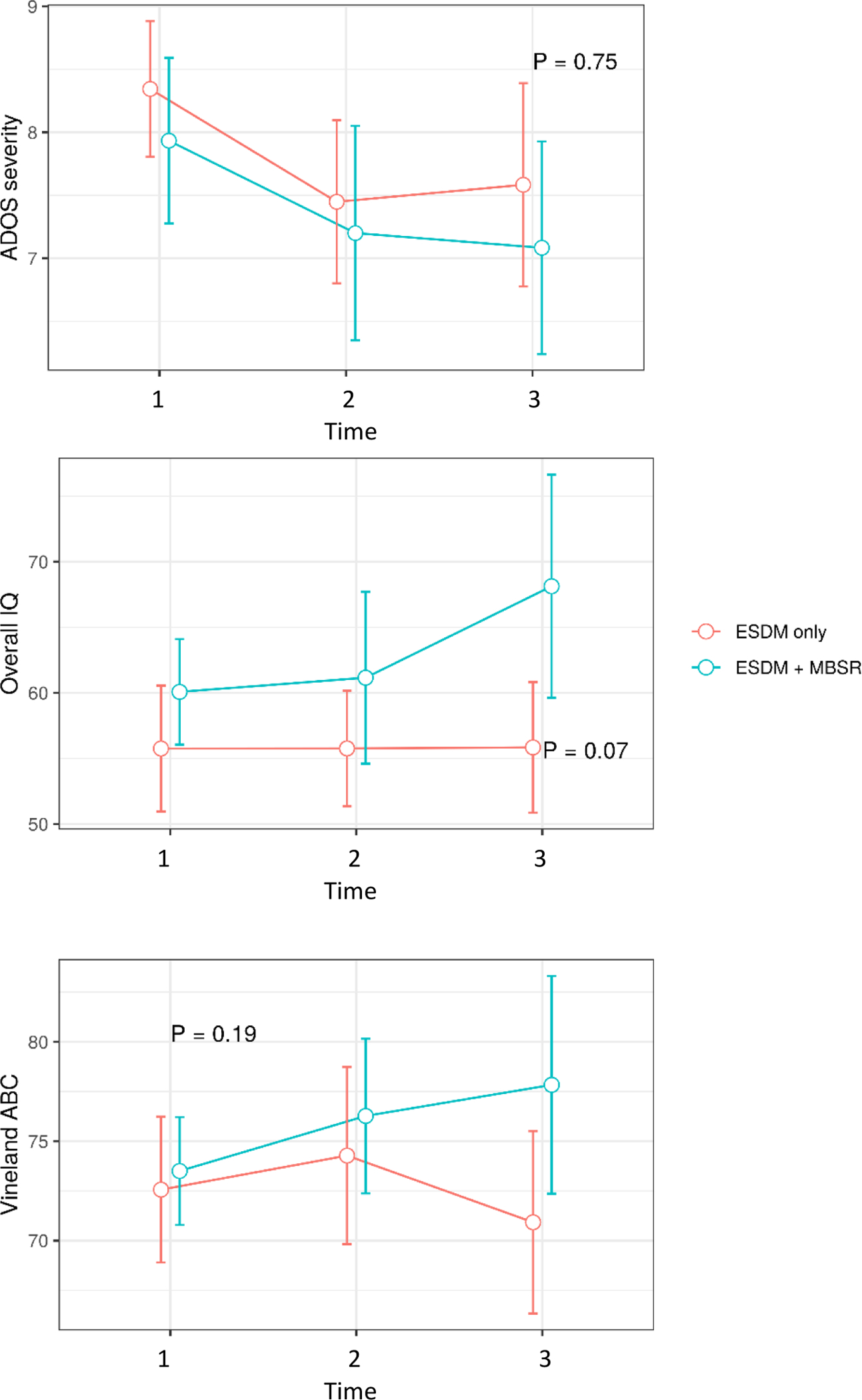
Group comparison for ADOS Severity Score, Overall IQ score, and Vineland ABC.
Regarding MSEL developmental scales, overall Early Learning Composite scores did not change from T1 to T2 (.51 points, p > .10) but significantly increased from T2 to T3 (3.94 points, p < .01). The standardized subscale scores did not change over time. Raw scores increased for Visual Reception (T1-T2, 3.12 points, p < .001; T2- T3, 1.6 points, p < .001), Receptive Language (T1- T2, 6.00 points, p < .001; T2 to T3, 2.39 points, p < .01), Expressive Language (T1 to T2, 4.41 points, p < .001; T2 to T3, 3.5 points, p < .001), and Fine Motor (T1-T2, 2.09 points, p < .001; T2-T3, 2.49 points, p < .001).
Regarding adaptive scales, no significant change occurred in the overall Adaptive Behavior Composite (T1-T2, 2.02 points, p = .052; T2-T3, −.40 points, p > .10). The standardized subscale scores did not change over time. Improvements in subscale raw scores were observed that were likely commensurate with maturation, including: Receptive Language (T1-T2, 5.56 points, p < .001; T2-T3, 1.99 points; p < .05), Expressive Language (T1-T2, 9.22 points, p < .001; T2-T3, 8.14 points, p <.001), Interpersonal (T1-T2, 3.63 points, p < .001; T2-T3, 2.06 points, p < .05), and Play Skills (T1-T2, 2.81 points, p < .001; T2-T3, 2.67 points, p < .05).
Changes based on age or sex.
We also examined whether age group or gender modified outcomes. We divided participants into four categories: Younger than 24 months, 24–29 months, 30–35 months, and 36 months and above. We found that some outcomes (particularly the raw scores of the MSEL subscales) improved with age, consistent with maturation of the child. However, there was no evidence that age group was correlated with change in outcomes from month 1 to month 3, month 3 to month 6, or month 1 to month 6 (all correlations nonsignificant, with ps > .10). There was also no evidence that changes in outcomes were associated with gender (all correlations nonsignificant, with ps > .10). Finally, there was no evidence that the intervention effect was modified by age or gender for any outcome. We note that our sample was primarily male, making gender effects more difficult to estimate.
Discussion
Although the positive impact of early developmental and behavioral intervention on young children with ASD is well-documented (Reichow, Hume, Barton, & Boyd, 2018; Weitlauf, McPheeters, et al., 2014), the same parents who commonly self-report high levels of psychological distress (Falk, Norris, & Quinn, 2014; Scherer, Verhey, & Kuper, 2019) are also the targets of parent-mediated intervention strategies (Ingersoll, Wainer, Berger, & Walton, 2017; Kasari, Gulsrud, Paparella, Hellemann, & Berry, 2015; Nevill, Lecavalier, & Stratis, 2018; Oono et al., 2013; Watson et al., 2017). Less is known about how directly supporting parents during this critical window of intervention onset and developmental monitoring may impact parents and families (Da Paz & Wallander, 2017; Wainer, Hepburn, & McMahon Griffith, 2017). In a previous publication, initial findings from this RCT supported the utility of MBSR for reducing aspects of parental distress and improving parental mindfulness (Weitlauf et al., 2020). In the additional analyses described in the present paper, we examined whether parental MBSR training resulted in differential child developmental outcomes commonly utilized within the literature: autism symptom severity scores, developmental skills, and adaptive behavior, both overall as well as related to language, social, and play domains.
We did not find between group differences in child outcomes based upon parental MBSR participation. Across parental treatment groups, mean child functioning showed similar developmental trajectories within treatment and after the treatment period. As seen within the standard deviations in Table 1, and consistent with the well-documented heterogeneity of the autism spectrum (Lord et al., 2020), there was a tremendous amount of variability between children within groups and at the same timepoints in spite of the narrow age band of our targeted recruitment sample. A larger sample size would likely have allowed for more fine-tuned understanding of trajectories across groups as well as individual phenotypic or parental characteristics predictive of change, beyond parental treatment group. Indeed, assessment and quantification of changes in dyadic interaction and parental responsivity (Green et al., 2010) represent a crucial next step in future work, particularly given recent findings (Zaidman-Zait, 2020) linking aspects of maternal attention, inhibition, and coping strategies to positive affect in interactions between mothers and their children with ASD.
When examining trajectories across the entire sample, three key findings emerged. First, overall autism symptom severity decreased during treatment but remained relatively stable in the post-treatment period. Importantly, ADOS-2 severity scores are not necessarily indicators of other aspects of well-being or functioning within the family unit (McStay, Dissanayake, Scheeren, Koot, & Begeer, 2014; van Heijst & Geurts, 2015), and it is very well known and accepted that autism symptoms are not a function of parent behavior or emotional state (Bennett, Webster, Goodall, & Rowland, 2018). However, describing symptom change in response to differential parent ability to engage fully with aspects of parent-mediated treatment is an important empirical question worthy of ongoing investigation. As noted in the recent comprehensive review by Trembath et al. (2019), a multitude of parent, child, system, and socio-cultural factors could impact outcomes when examining parent-mediated interventions for children with ASD. Additionally, individual variability likely exists in the intervention techniques most used or preferred by parents and the impact of those techniques on child outcomes, all of which in turn is likely influenced by children themselves (Waddington, van der Meer, Sigafoos, & Whitehouse, 2020).
Second, changes noted in raw scores of receptive and expressive communication skills (MSEL, VABS-II) are of unclear clinical significance. It is similarly difficult to draw conclusions regarding the overall improvements across groups on the MSEL Early Learning Composite in the post-treatment period relative to active treatment. Given the relatively short treatment window as compared to the post-treatment follow-up period, as well as the reliance of these instruments on parent report or brief windows of assessment, these changes may be artifacts of time and maturation within this very young participant sample. Future work would benefit from more intensive direct observation and assessment of communication and problem-solving skills using instruments designed to detect fine-grained changes within this age group.
Finally, it is important not to interpret the lack of differential child functioning according to group as evidence that support for parents is ineffective. Mounting evidence supports the positive impact of MBSR on a variety of health-related outcomes (Alsubaie et al., 2017; Khoury et al., 2015). Parents in this work self-reported improvements in parental stress levels as well as mindfulness skills (Weitlauf et al., 2020), and it is unknown how those changes impacted other aspects of family functioning or evolved over time. Cartwright and Mount (2021) recently provided brief (15-minute) non-specific support to parents prior to implementing a manualized parent-mediated intervention, which allowed parents to express stressors, questions, and concerns that might have interfered with the integrity of session activities. Ultimately, understanding family-level outcome variables continues to be an important avenue of work (Wainer et al., 2017) to define outcomes of meaning, such as those related to quality of life, beyond a standardized assessment battery (Lord et al., 2020).
To capture variability on those factors that are most important to parents, future studies may wish to more directly assess changes in variables such as parental perceptions of family connectedness, functionality, or identity. That is, in keeping with increasing recognition of promoting hope, positivity, and identity as part of the early diagnostic and treatment process (H. M. Brown, Stahmer, Dwyer, & Rivera, 2021), it is possible that measuring pre-post treatment change in variables such as parental attitudes about autism, parental self-efficacy to meet their children’s needs or effectively engage in treatment, parental knowledge about ways to support their children, and hope for their children’s futures may offer salient targets for intervention (Manohar, Kandasamy, Chandrasekaran, & Rajkumar, 2020; Russell & Ingersoll, 2021; Schertz, Lester, Erden, Safran, & Githens, 2020). This may be especially important given the tremendous phenotypic heterogeneity not only of the autism spectrum (Lombardo, Lai, & Baron-Cohen, 2019; Lord et al., 2020), but also of which outcomes are actually the most meaningful and predictive of wellbeing for the parents that also participate in treatment.
This work has several important limitations. First, future investigations must include a treatment-as-usual control group to better understand the specific impact of P-ESDM versus maturation on outcomes. Additionally, although we tracked fidelity to P-ESDM procedures, it is possible that the quality of intervention varied across therapists, and tracking such will be important in ongoing work. Exploring changes in parent-child dyadic interaction that could be related to mindfulness practice or reduced stress, such as parental responsivity or affect, represents an important avenue of meaningful future investigation. Another limitation is attrition and its impact on our decreasing sample size. Although our longitudinal study experienced high rates of attrition over its 9-month time period (Weitlauf et al., 2020), much of which was due to family relocation, this impacted our ability to directly assess outcomes for a substantial minority of participants. Significant variability occurred across participants in this work, with some children showing trajectories of steady improvement, others steady decline, and still others uneven profiles. Such variability in post-diagnostic symptom and skill trajectories has been documented across several studies (Gotham, Pickles, & Lord, 2012; Solomon et al., 2018). A more robust treatment design that controls for potential effects of maturation would strengthen future investigations.
Finally, and importantly, the majority of our sample included White families of moderate to high socioeconomic status. Families from diverse racial, ethnic, linguistic, geographic, and socioeconomic backgrounds face significant barriers to equitable access to care and are often excluded from the research that impacts that care (Antezana, Scarpa, Valdespino, Albright, & Richey, 2017; Dababnah, Shaia, Campion, & Nichols, 2018; Hine et al., 2020; Liptak et al., 2008; Shaia, Nichols, Dababnah, Campion, & Garbarino, 2020; Zuckerman, Chavez, Regalado Murillo, Lindly, & Reeder, 2018). It will be important for future work not only to deliberately recruit diverse families, but to also seek their input and utilize that input when designing intervention paradigms.
Although complex, understanding and describing the ways in which reducing parental stress impacts children with ASD in the post-diagnostic period and beyond represents an important direction of future work, particularly for those intervention programs that emphasize parental involvement.
Funding:
All phases of this study were supported by the Health Resources & Services Administration Maternal & Child Health Bureau, R40MC27706. Study design and implementation received core support from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (U54 HD08321) and the Vanderbilt Institute for Clinical and Translational Research (VICTR), which is funded by the National Center for Advancing Translational Sciences (NCATS) Clinical Translational Science Award (CTSA) Program, Award Number 5UL1TR002243-03.
Footnotes
Declarations
Conflict of Interest: The authors have no financial relationships or conflicts of interest relevant to this article to disclose.
Compliance with Ethical Standards: This trial has been registered at www.clinicaltrials.gov (identifier NCT03889821). All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. All procedures were approved and overseen by the Vanderbilt University Medical Center Institutional Review Board.
References
- Alsubaie M, Abbott R, Dunn B, Dickens C, Keil TF, Henley W, & Kuyken W (2017). Mechanisms of action in mindfulness-based cognitive therapy (MBCT) and mindfulness-based stress reduction (MBSR) in people with physical and/or psychological conditions: A systematic review. Clinical Psychology Review, 55, 74–91. doi: 10.1016/j.cpr.2017.04.008 [DOI] [PubMed] [Google Scholar]
- Antezana L, Scarpa A, Valdespino A, Albright J, & Richey JA (2017). Rural Trends in Diagnosis and Services for Autism Spectrum Disorder. Front Psychol, 8, 590. doi: 10.3389/fpsyg.2017.00590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bearss K, Johnson C, Smith T, Lecavalier L, Swiezy N, Aman M, … Scahill L (2015). Effect of Parent Training vs Parent Education on Behavioral Problems in Children With Autism Spectrum Disorder. Journal of the American Medical Association, 313(15), 1524. doi: 10.1001/jama.2015.3150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett M, Webster AA, Goodall E, & Rowland S (2018). Establishing Contexts for Support: Undoing the Legacy of the “Refrigerator Mother” Myth. In Life on the Autism Spectrum: Translating Myths and Misconceptions into Positive Futures (pp. 61–80). Singapore: Springer Singapore. [Google Scholar]
- Bohadana G, Morrissey S, & Paynter J (2020). Self-Compassion in Mothers of Children with Autism Spectrum Disorder: A Qualitative Analysis. Journal of Autism and Developmental Disorders. doi: 10.1007/s10803-020-04612-2 [DOI] [PubMed] [Google Scholar]
- Brown HM, Stahmer AC, Dwyer P, & Rivera S (2021). Changing the story: How diagnosticians can support a neurodiversity perspective from the start. Autism, 25(5), 1171–1174. doi: 10.1177/13623613211001012 [DOI] [PubMed] [Google Scholar]
- Brown KW, Coogle CL, & Wegelin J (2016). A pilot randomized controlled trial of mindfulness-based stress reduction for caregivers of family members with dementia. Aging Ment Health, 20(11), 1157–1166. doi: 10.1080/13607863.2015.1065790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cartwright JE, & Mount KB (2021). Adjunctive Parental Support Within Manualized Parent Training for Children with Autism Spectrum Disorder. Child Psychiatry & Human Development. doi: 10.1007/s10578-021-01210-w [DOI] [PubMed] [Google Scholar]
- Cash E, Salmon P, Weissbecker I, Rebholz WN, Bayley-Veloso R, Zimmaro LA, … Sephton SE (2015). Mindfulness meditation alleviates fibromyalgia symptoms in women: results of a randomized clinical trial. Ann Behav Med, 49(3), 319–330. doi: 10.1007/s12160-014-9665-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Da Paz NS, & Wallander JL (2017). Interventions that target improvements in mental health for parents of children with autism spectrum disorders: A narrative review. Clinical Psychology Review, 51, 1–14. doi: 10.1016/j.cpr.2016.10.006 [DOI] [PubMed] [Google Scholar]
- Dababnah S, Shaia WE, Campion K, & Nichols HM (2018). “We Had to Keep Pushing”: Caregivers’ Perspectives on Autism Screening and Referral Practices of Black Children in Primary Care. Intellect Dev Disabil, 56(5), 321–336. doi: 10.1352/1934-9556-56.5.321 [DOI] [PubMed] [Google Scholar]
- Dykens EM, Fisher MH, Taylor JL, Lambert W, & Miodrag N (2014). Reducing distress in mothers of children with autism and other disabilities: a randomized trial. Pediatrics, 134(2), e454–463. doi: 10.1542/peds.2013-3164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esler AN, Bal VH, Guthrie W, Wetherby A, Ellis Weismer S, & Lord C (2015). The Autism Diagnostic Observation Schedule, Toddler Module: Standardized Severity Scores. Journal of Autism and Developmental Disorders, 45(9), 2704–2720. doi: 10.1007/s10803-015-2432-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estes A, Olson E, Sullivan K, Greenson J, Winter J, Dawson G, & Munson J (2013). Parenting-related stress and psychological distress in mothers of toddlers with autism spectrum disorders. Brain Development, 35(2), 133–138. doi: 10.1016/j.braindev.2012.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estes A, Swain DM, & Macduffie KE (2019). The effects of early autism intervention on parents and family adaptive functioning. Pediatric Medicine, 2, 21–21. doi: 10.21037/pm.2019.05.05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estes A, Vismara L, Mercado C, Fitzpatrick A, Elder L, Greenson J, … Rogers S (2014). The impact of parent-delivered intervention on parents of very young children with autism. Journal of Autism and Developmental Disorders, 44(2), 353–365. doi: 10.1007/s10803-013-1874-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falk NH, Norris K, & Quinn MG (2014). The factors predicting stress, anxiety and depression in the parents of children with autism. Journal of Autism and Developmental Disorders, 44(12), 3185–3203. doi: 10.1007/s10803-014-2189-4 [DOI] [PubMed] [Google Scholar]
- Girault JB, Swanson MR, Meera SS, Grzadzinski RL, Shen MD, Burrows CA, … Piven J (2020). Quantitative trait variation in ASD probands and toddler sibling outcomes at 24 months. J Neurodev Disord, 12(1), 5. doi: 10.1186/s11689-020-9308-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Morrison A, Jazaieri H, Brozovich F, Heimberg R, & Gross JJ (2016). Group CBT versus MBSR for social anxiety disorder: A randomized controlled trial. J Consult Clin Psychol, 84(5), 427–437. doi: 10.1037/ccp0000092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, & Heyward D (2011). Maternal depression and child psychopathology: a meta-analytic review. Clin Child Fam Psychol Rev, 14(1), 1–27. doi: 10.1007/s10567-010-0080-1 [DOI] [PubMed] [Google Scholar]
- Gotham K, Pickles A, & Lord C (2012). Trajectories of autism severity in children using standardized ADOS scores. Pediatrics, 130(5), e1278–e1284. doi: 10.1542/peds.2011-3668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green J, Charman T, McConachie H, Aldred C, Slonims V, Howlin P, … Pickles A (2010). Parent-mediated communication-focused treatment in children with autism (PACT): a randomised controlled trial. Lancet, 375(9732), 2152–2160. doi: 10.1016/s0140-6736(10)60587-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunning C, Holloway J, & Grealish L (2020). An evaluation of parents as behavior change agents in the Preschool Life Skills program. Journal of Applied Behavior Analysis, 53(2), 889–917. doi: 10.1002/jaba.660 [DOI] [PubMed] [Google Scholar]
- Hattangadi N, Cost KT, Birken CS, Borkhoff CM, Maguire JL, Szatmari P, & Charach A (2020). Parenting stress during infancy is a risk factor for mental health problems in 3-year-old children. BMC Public Health, 20(1), 1726. doi: 10.1186/s12889-020-09861-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hine JF, Allin J, Allman A, Black M, Browning B, Ramsey B, … Allen, W. (2020). Increasing Access to Autism Spectrum Disorder Diagnostic Consultation in Rural and Underserved Communities: Streamlined Evaluation Within Primary Care. J Dev Behav Pediatr, 41(1), 16–22. doi: 10.1097/dbp.0000000000000727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge EA, Bui E, Marques L, Metcalf CA, Morris LK, Robinaugh DJ, … Simon NM (2013). Randomized controlled trial of mindfulness meditation for generalized anxiety disorder: effects on anxiety and stress reactivity. J Clin Psychiatry, 74(8), 786–792. doi: 10.4088/JCP.12m08083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingersoll BR, Wainer AL, Berger NI, & Walton KM (2017). Efficacy of low intensity, therapist-implemented Project ImPACT for increasing social communication skills in young children with ASD. Developmental Neurorehabilitation, 20(8), 502–510. doi: 10.1080/17518423.2016.1278054 [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J, & Chapman-Waldrop A (1988). Compliance with an outpatient stress reduction program: rates and predictors of program completion. J Behav Med, 11(4), 333–352. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J, Massion AO, Kristeller J, Peterson LG, Fletcher KE, Pbert L, … Santorelli SF (1992). Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatry, 149(7), 936–943. doi: 10.1176/ajp.149.7.936 [DOI] [PubMed] [Google Scholar]
- Kamis C (2021). The Long-Term Impact of Parental Mental Health on Children’s Distress Trajectories in Adulthood. Soc Ment Health, 11(1), 54–68. doi: 10.1177/2156869320912520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasari C, Gulsrud A, Paparella T, Hellemann G, & Berry K (2015). Randomized comparative efficacy study of parent-mediated interventions for toddlers with autism. Journal of Consulting and Clinical Psychology, 83(3), 554–563. doi: 10.1037/a0039080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoo EL, Small R, Cheng W, Hatchard T, Glynn B, Rice DB, … Poulin PA (2019). Comparative evaluation of group-based mindfulness-based stress reduction and cognitive behavioural therapy for the treatment and management of chronic pain: A systematic review and network meta-analysis. Evid Based Ment Health, 22(1), 26–35. doi: 10.1136/ebmental-2018-300062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoury B, Sharma M, Rush SE, & Fournier C (2015). Mindfulness-based stress reduction for healthy individuals: A meta-analysis. Journal of Psychosomatic Research, 78(6), 519–528. doi: 10.1016/j.jpsychores.2015.03.009 [DOI] [PubMed] [Google Scholar]
- Kriakous SA, Elliott KA, Lamers C, & Owen R (2020). The Effectiveness of Mindfulness-Based Stress Reduction on the Psychological Functioning of Healthcare Professionals: a Systematic Review. Mindfulness (N Y), 1–28. doi: 10.1007/s12671-020-01500-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamothe M, Rondeau É, Malboeuf-Hurtubise C, Duval M, & Sultan S (2016). Outcomes of MBSR or MBSR-based interventions in health care providers: A systematic review with a focus on empathy and emotional competencies. Complement Ther Med, 24, 19–28. doi: 10.1016/j.ctim.2015.11.001 [DOI] [PubMed] [Google Scholar]
- Lebares CC, Hershberger AO, Guvva EV, Desai A, Mitchell J, Shen W, … Harris HW (2018). Feasibility of Formal Mindfulness-Based Stress-Resilience Training Among Surgery Interns: A Randomized Clinical Trial. JAMA Surg, 153(10), e182734. doi: 10.1001/jamasurg.2018.2734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liptak GS, Benzoni LB, Mruzek DW, Nolan KW, Thingvoll MA, Wade CM, & Fryer GE (2008). Disparities in diagnosis and access to health services for children with autism: data from the National Survey of Children’s Health. J Dev Behav Pediatr, 29(3), 152–160. doi: 10.1097/DBP.0b013e318165c7a0 [DOI] [PubMed] [Google Scholar]
- Lombardo MV, Lai MC, & Baron-Cohen S (2019). Big data approaches to decomposing heterogeneity across the autism spectrum. Mol Psychiatry, 24(10), 1435–1450. doi: 10.1038/s41380-018-0321-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord, Brugha TS, Charman T, Cusack J, Dumas G, Frazier T, … Veenstra-Vanderweele J (2020). Autism spectrum disorder. Nature Reviews Disease Primers, 6(1). doi: 10.1038/s41572-019-0138-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C, Risi S, Lambrecht L, Cook EH, Leventhal BL, DiLavore PC, … Rutter M (2000). The Autism Diagnostic Observation Schedule-Generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders, 30(3), 205–223. doi:Doi 10.1023/A:1005592401947 [DOI] [PubMed] [Google Scholar]
- Manohar H, Kandasamy P, Chandrasekaran V, & Rajkumar RP (2020). Can RCTs capture it all?-Need for qualitative studies on parent-mediated interventions for children with Autism Spectrum Disorder. Asian J Psychiatr, 48, 101915. doi: 10.1016/j.ajp.2019.101915 [DOI] [PubMed] [Google Scholar]
- Masi A, Dissanayake C, Alach T, Cameron K, Fordyce K, Frost G, … Eapen V (2021). Clinical outcomes and associated predictors of early intervention in autism spectrum disorder: a study protocol. BMJ Open, 11(8), e047290. doi: 10.1136/bmjopen-2020-047290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClure LA, Lee NL, Sand K, Vivanti G, Fein D, Stahmer A, & Robins DL (2021). Connecting the Dots: a cluster-randomized clinical trial integrating standardized autism spectrum disorders screening, high-quality treatment, and long-term outcomes. Trials, 22(1), 319. doi: 10.1186/s13063-021-05286-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McStay RL, Dissanayake C, Scheeren A, Koot HM, & Begeer S (2014). Parenting stress and autism: the role of age, autism severity, quality of life and problem behaviour of children and adolescents with autism. Autism, 18(5), 502–510. doi: 10.1177/1362361313485163 [DOI] [PubMed] [Google Scholar]
- Miller JJ, Fletcher K, & Kabat-Zinn J (1995). Three-year follow-up and clinical implications of a mindfulness meditation-based stress reduction intervention in the treatment of anxiety disorders. Gen Hosp Psychiatry, 17(3), 192–200. [DOI] [PubMed] [Google Scholar]
- Mullen EL (1995). Mullen Scales of Early Learning. Circle Pines, MN: American Guidance Service. [Google Scholar]
- Nevill RE, Lecavalier L, & Stratis EA (2018). Meta-analysis of parent-mediated interventions for young children with autism spectrum disorder. Autism, 22(2), 84–98. doi: 10.1177/1362361316677838 [DOI] [PubMed] [Google Scholar]
- Nicholas DB, Macculloch R, Roberts W, Zwaigenbaum L, & McKeever P (2020). Tensions in Maternal Care for Children, Youth, and Adults With Autism Spectrum Disorder. Global Qualitative Nursing Research, 7, 233339362090758. doi: 10.1177/2333393620907588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oono IP, Honey EJ, & McConachie H (2013). Parent-mediated early intervention for young children with autism spectrum disorders (ASD). Cochrane Database of Systematic Reviews. doi: 10.1002/14651858.cd009774.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellecchia M, Beidas RS, Mandell DS, Cannuscio CC, Dunst CJ, & Stahmer AC (2020). Parent empowerment and coaching in early intervention: study protocol for a feasibility study. Pilot and Feasibility Studies, 6(1). doi: 10.1186/s40814-020-00568-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed P, & Osborne LA (2019). Reaction to diagnosis and subsequent health in mothers of children with autism spectrum disorder. Autism, 23(6), 1442–1448. doi: 10.1177/1362361318815641 [DOI] [PubMed] [Google Scholar]
- Reichow B, Hume K, Barton EE, & Boyd BA (2018). Early intensive behavioral intervention (EIBI) for young children with autism spectrum disorders (ASD). Cochrane Database of Systematic Reviews. doi: 10.1002/14651858.cd009260.pub3 [DOI] [Google Scholar]
- Rogers S, Estes A, Lord C, Vismara L, Winter J, Fitzpatrick A, … Dawson G (2012). Effects of a brief Early Start Denver model (ESDM)-based parent intervention on toddlers at risk for autism spectrum disorders: a randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 51(10), 1052–1065. doi: 10.1016/j.jaac.2012.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers S, Estes A, Vismara L, Munson J, Zierhut C, Greenson J, … Talbott M (2019). Enhancing Low-Intensity Coaching in Parent Implemented Early Start Denver Model Intervention for Early Autism: A Randomized Comparison Treatment Trial. Journal of Autism and Developmental Disorders, 49(2), 632–646. doi: 10.1007/s10803-018-3740-5 [DOI] [PubMed] [Google Scholar]
- Rollins PR, John S, Jones A, & De Froy A (2019). Pathways Early ASD Intervention as a Moderator of Parenting Stress on Parenting Behaviors: A Randomized Control Trial. Journal of Autism and Developmental Disorders, 49(10), 4280–4293. doi: 10.1007/s10803-019-04144-4 [DOI] [PubMed] [Google Scholar]
- Russell KM, & Ingersoll B (2021). Factors related to parental therapeutic self-efficacy in a parent-mediated intervention for children with autism spectrum disorder: A mixed methods study. Autism, 25(4), 971–981. doi: 10.1177/1362361320974233 [DOI] [PubMed] [Google Scholar]
- Schaefer JM, & Andzik NR (2020). Evaluating Behavioral Skills Training as an Evidence-Based Practice When Training Parents to Intervene with Their Children. Behavior Modification, 0145445520923996. doi: 10.1177/0145445520923996 [DOI] [PubMed] [Google Scholar]
- Scherer N, Verhey I, & Kuper H (2019). Depression and anxiety in parents of children with intellectual and developmental disabilities: A systematic review and meta-analysis. PLoS One, 14(7), e0219888. doi: 10.1371/journal.pone.0219888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schertz HH, Lester JN, Erden E, Safran S, & Githens P (2020). Challenges and contributors to self-efficacy for caregivers of toddlers with autism. Autism, 24(5), 1260–1272. doi: 10.1177/1362361319899761 [DOI] [PubMed] [Google Scholar]
- Schreibman L, Dawson G, Stahmer AC, Landa R, Rogers SJ, McGee GG, … Halladay A (2015). Naturalistic Developmental Behavioral Interventions: Empirically Validated Treatments for Autism Spectrum Disorder. Journal of Autism and Developmental Disorders, 45(8), 2411–2428. doi: 10.1007/s10803-015-2407-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seymour M, Giallo R, & Wood CE (2017). The psychological and physical health of fathers of children with Autism Spectrum Disorder compared to fathers of children with long-term disabilities and fathers of children without disabilities. Research in Developmental Disabilities, 69, 8–17. doi: 10.1016/j.ridd.2017.07.018 [DOI] [PubMed] [Google Scholar]
- Shaia WE, Nichols HM, Dababnah S, Campion K, & Garbarino N (2020). Brief Report: Participation of Black and African-American Families in Autism Research. J Autism Dev Disord, 50(5), 1841–1846. doi: 10.1007/s10803-019-03926-0 [DOI] [PubMed] [Google Scholar]
- Smith SL, & Langen WH (2020). A Systematic Review of Mindfulness Practices for Improving Outcomes in Chronic Low Back Pain. Int J Yoga, 13(3), 177–182. doi: 10.4103/ijoy.IJOY_4_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon M, Iosif AM, Reinhardt VP, Libero LE, Nordahl CW, Ozonoff S, … Amaral DG (2018). What will my child’s future hold? phenotypes of intellectual development in 2–8-year-olds with autism spectrum disorder. Autism Research, 11(1), 121–132. doi: 10.1002/aur.1884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song Y, & Lindquist R (2015). Effects of mindfulness-based stress reduction on depression, anxiety, stress and mindfulness in Korean nursing students. Nurse Educ Today, 35(1), 86–90. doi: 10.1016/j.nedt.2014.06.010 [DOI] [PubMed] [Google Scholar]
- Sparrow SS, & Cicchetti DV (1985). Diagnostic uses of the Vineland Adaptive Behavior Scales. Journal of Pediatric Psychology, 10(2), 215–225. [DOI] [PubMed] [Google Scholar]
- Stahmer AC, Rieth SR, Dickson KS, Feder J, Burgeson M, Searcy K, & Brookman-Frazee L (2020). Project ImPACT for Toddlers: Pilot outcomes of a community adaptation of an intervention for autism risk. Autism, 24(3), 617–632. doi: 10.1177/1362361319878080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarver J, Palmer M, Webb S, Scott S, Slonims V, Simonoff E, & Charman T (2019). Child and parent outcomes following parent interventions for child emotional and behavioral problems in autism spectrum disorders: A systematic review and meta-analysis. Autism, 1362361319830042. doi: 10.1177/1362361319830042 [DOI] [PubMed] [Google Scholar]
- Taylor JL, & Warren ZE (2012). Maternal depressive symptoms following autism spectrum diagnosis. Journal of Autism and Developmental Disorders, 42(7), 1411–1418. doi: 10.1007/s10803-011-1375-x [DOI] [PubMed] [Google Scholar]
- Todd C, Cooksey R, Davies H, McRobbie C, & Brophy S (2019). Mixed-methods evaluation comparing the impact of two different mindfulness approaches on stress, anxiety and depression in school teachers. BMJ Open, 9(7), e025686. doi: 10.1136/bmjopen-2018-025686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trembath D, Gurm M, Scheerer NE, Trevisan DA, Paynter J, Bohadana G, … Iarocci G (2019). Systematic review of factors that may influence the outcomes and generalizability of parent-mediated interventions for young children with autism spectrum disorder. Autism Res, 12(9), 1304–1321. doi: 10.1002/aur.2168 [DOI] [PubMed] [Google Scholar]
- Uddin J, Alharbi N, Uddin H, Hossain MB, Hatipoğlu SS, Long DL, & Carson AP (2020). Parenting stress and family resilience affect the association of adverse childhood experiences with children’s mental health and attention-deficit/hyperactivity disorder. J Affect Disord, 272, 104–109. doi: 10.1016/j.jad.2020.03.132 [DOI] [PubMed] [Google Scholar]
- van Heijst BF, & Geurts HM (2015). Quality of life in autism across the lifespan: a meta-analysis. Autism, 19(2), 158–167. doi: 10.1177/1362361313517053 [DOI] [PubMed] [Google Scholar]
- Vibert BA, Dufek S, Klein CB, Choi YB, Winter J, Lord C, & Kim SH (2020). Quantifying Caregiver Change Across Early Autism Interventions Using the Measure of NDBI Strategy Implementation: Caregiver Change (MONSI-CC). Journal of Autism and Developmental Disorders, 50(4), 1364–1379. doi: 10.1007/s10803-019-04342-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waddington H, van der Meer L, Sigafoos J, & Whitehouse A (2020). Examining parent use of specific intervention techniques during a 12-week training program based on the Early Start Denver Model. Autism, 24(2), 484–498. doi: 10.1177/1362361319876495 [DOI] [PubMed] [Google Scholar]
- Wainer AL, Hepburn S, & McMahon Griffith E (2017). Remembering parents in parent-mediated early intervention: An approach to examining impact on parents and families. Autism, 21(1), 5–17. doi: 10.1177/1362361315622411 [DOI] [PubMed] [Google Scholar]
- Warren Z, Vehorn A, Dohrmann E, Newsom C, & Taylor JL (2013). Brief report: Service implementation and maternal distress surrounding evaluation recommendations for young children diagnosed with autism. Autism, 17(6), 693–700. doi: 10.1177/1362361312453881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson LR, Crais ER, Baranek GT, Turner-Brown L, Sideris J, Wakeford L, … Nowell SW (2017). Parent-Mediated Intervention for One-Year-Olds Screened as At-Risk for Autism Spectrum Disorder: A Randomized Controlled Trial. Journal of Autism and Developmental Disorders, 47(11), 3520–3540. doi: 10.1007/s10803-017-3268-0 [DOI] [PubMed] [Google Scholar]
- Weitlauf AS, Broderick N, Stainbrook JA, Taylor JL, Herrington CG, Nicholson AG, … Warren ZE (2020). Mindfulness-Based Stress Reduction for Parents Implementing Early Intervention for Autism: An RCT. Pediatrics, 145(Supplement 1), S81–S92. doi: 10.1542/peds.2019-1895k [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitlauf AS, McPheeters ML, Peters B, Sathe N, Travis R, Aiello R, … Warren Z (2014). In Therapies for Children With Autism Spectrum Disorder: Behavioral Interventions Update. Rockville (MD). [PubMed] [Google Scholar]
- Weitlauf AS, Vehorn AC, Taylor JL, & Warren ZE (2014). Relationship satisfaction, parenting stress, and depression in mothers of children with autism. Autism, 18(2), 194–198. doi: 10.1177/1362361312458039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wetherby AM, Woods J, Guthrie W, Delehanty A, Brown JA, Morgan L, … Lord C (2018). Changing Developmental Trajectories of Toddlers With Autism Spectrum Disorder: Strategies for Bridging Research to Community Practice. Journal of Speech Language and Hearing Research, 61(11), 2615–2628. doi: 10.1044/2018_JSLHR-L-RSAUT-18-0028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaidman-Zait A (2020). The contribution of maternal executive functions and active coping to dyadic affective dynamics: Children with autism spectrum disorder and their mothers. Autism, 24(3), 645–657. doi: 10.1177/1362361319854653 [DOI] [PubMed] [Google Scholar]
- Zhang YX, & Cummings JR (2020). Supply of Certified Applied Behavior Analysts in the United States: Implications for Service Delivery for Children With Autism. Psychiatric Services, 71(4), 385–388. doi: 10.1176/appi.ps.201900058 [DOI] [PubMed] [Google Scholar]
- Zuckerman KE, Chavez AE, Regalado Murillo C, Lindly OJ, & Reeder JA (2018). Disparities in Familiarity With Developmental Disabilities Among Low-Income Parents. Acad Pediatr, 18(8), 944–951. doi: 10.1016/j.acap.2018.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]


