Abstract
Background
Rifaximin, a rifamycin antibiotic, is widely used to treat infectious diarrhea but not commonly used in H. pylori eradication. With its potential advantages of the agent, some studies were conducted on this topic. The aim of this study is to assess effectiveness and safety of rifaximin-containing regimens and to evaluate whether they are alternative choices for H. pylori eradication.
Methods
Scientific databases including PubMed, EMbase and Cochrane Library were used to identify clinical trials on rifaximin-containing regimens published from January 2000 to October 2021. Review Manager 5.4 and STATA12 were adopted for the systematic review.
Results
In this study, totally 1025 patients were included from 3 randomized controlled and 9 single-arm studies. It showed that the differences in effectiveness and safety between rifaximin-containing and first-line regimens were not statistically significant in randomized controlled trials. However, the results of the single-arm trials indicated that the eradication and adverse drug reaction rate varied suggesting data instability (r=38.1%-85.4%, rADR 0.00–67.5% by ITT analysis). Among them, the eradication rate of pediatric patients (r=85.4% by ITT analysis) was higher than that of adult patients (r=38.1–74.5% by ITT analysis). Meanwhile, in all adult subgroups (triple or quadruple, with or without amoxicillin, different duration and rifaximin dose), the results did not show sufficient effectiveness as all the eradication rates did not meet the minimum ideal or ideal target.
Conclusion
Taken together, rifaximin-containing regimens should not be recommended for H. pylori eradication as they cannot achieve the eradication rate desired.
Keywords: rifaximin, Helicobacter pylori, effectiveness and safety, systematic review
Plain Language Summary
Rifaximin is a distinctive antibacterial drug with many advantages. However, fewer attentions have been paid to its antibacterial effect on H. pylori than those of the other antibiotics and the present conclusions are not consistent. In this manuscript, we have demonstrated whether rifaximin-containing regimens can meet satisfactory effectiveness and stable safety profile in H. pylori eradication treatment via systematic review. The main results are unsatisfactory due to the unstable and low eradication rate. The well safety profile has not been proven either. We speculate that the rifaximin-containing regimens are not suitable for naïve patients and rescue therapy from the current studies. Therefore, it is emphasized that the regimens containing rifaximin should not be used routinely for H. pylori eradication unless further research would prove that it is effective and safe enough.
Introduction
Helicobacter pylori (H. pylori), affecting about 44.3% of the world’s population,1 has become a major global public health problem threatened people globally, since it can pose a risk of peptic ulcers, gastric cancer, dyspepsia and other digestive diseases.2 In recent decades, international guidelines and clinical practices have agreed on the active treatment of H. pylori and achieving desired eradication rate as an effective way to cure these diseases and preventing them from progressing to gastric cancer.3 However, H. pylori has also become a global health priority since its resistance to commonly used antibacterial agents, such as clarithromycin, metronidazole and levofloxacin (multidrug resistance), has been on the rise in recent years. Meanwhile, the use of broad-spectrum antibiotics and antibiotic abuse may also contribute to the increase and treatment failure, which is significantly higher than before.4
Rifaximin, a rifamycin antibiotic, is a structural analog of rifampicin that inhibits RNA synthesis in bacteria by binding to the β-subunit of DNA-dependent RNA polymerase.5,6 It can achieve intestinal concentrations that are 250–500 times higher than its minimal inhibitory concentration (MIC90),7 with a strong intraluminal antibacterial effect. It may also reduce virulence factors and the morphology of bacteria, inhibit bacterial attachment, and decrease the mucosal inflammatory response.7,8 Based on these features, it is widely used in the treatment of local infections such as diarrhea and cirrhosis now, rather than systematic infection or infections from other sites but gastrointestinal tract. The less-frequent applications of rifaximin may reduce the resistance rate to H. pylori. Meanwhile, as a non-absorption agent, rifaximin has little interaction with other drugs and with tiny impact on normal flora outside the gastrointestinal tract.
Thus, in order to improve H. pylori eradication rate and decrease treatment failure, it is critical to provide some new paths for treatment. Rifaximin appears to be a suitable alternative. However, there are no systematic reviews on this topic in the past 20 years. This study included the clinical trials (both randomized controlled and single-arm trials) that met the inclusion criteria to investigate the efficacy and safety of rifaximin for H. pylori eradication on a systematic and scientific basis.
Data and Methods
Literature Inclusion and Exclusion Criteria
The inclusion criteria were as follows: (1) randomized controlled trials (RCTs) and single-arm trials (SATs) of rifaximin-containing regimens for H. pylori eradication in humans, in any language; (2) trials in which H. pylori infection were confirmed by either urea breath test, or upper gastrointestinal (GI) tract endoscopic biopsies; (3) trials with outcomes including the H. pylori eradication rates and adverse drug reactions. The H. pylori eradication rates were calculated by intention-to-treat analysis (ITTA) and per-protocol analysis (PPA) (if available).
The exclusion criteria were as follows: (1) duplicate publications; (2) animal studies, basic research studies, systematic reviews, meta-analyses, retrospective studies, case reports, or conference presentations; (3) abstract-only publications or unpublished studies; (4) publications missing important information; and (5) studies with non-standard anti-H. pylori regimens (regimens those are not antibacterial drugs + bismuth + proton pump inhibitors (PPIs) or antibacterial drugs + PPIs)
Literature Search and Data Extraction
We systematically searched the PubMed, Cochrane Library, and EMBASE databases from January 2000 to October 2021; “Helicobacter pylori” and “rifaximin” were used as medical subject terms, “Helicobacter pylori”, “Helicobacter nemestrinae”, “Campylobacter pylori”, “Campylobacter pylori subsp. Pylori”, “Campylobacter pyloridis and rifaximin”, “Xifaxan”, “Redactiv”, “L105”, and “L-105,4-Deoxy-4’-methylpyrido(1’,2’-1,2)imidazo (5,4C)rifamycin” were used as free terms. Medical subject and free terms were combined for the study search. We have also searched for possible missing literature from other sources (monographs, reviews, etc.)
The literature screening and data extraction were performed independently by two investigators according to the inclusion and exclusion criteria. Any disagreement was resolved by discussion and consultation with the third investigator.
Then, we extracted data including the first author’s name, publication year, number of patients in the treatment and control groups, patient demographics, intervention methods, treatment duration.
The primary outcomes of this research include H. pylori eradication and adverse drug reaction (ADR).
Assessment of Risk of Bias
The methodological quality of the RCTs was assessed according to the Cochrane Systematic Assessment Manual version 5.1 Risk of Bias Assessment Tool and the Jadad scale. A study with a Jadad scale score of 3 or more was considered as a high-quality study that can be acceptable. The quality of the SATs was assessed by the MINORS scale, with scores less than 9 implied low-quality, scores between 9 and 12 implied moderate quality, while those more than 12 implied high-quality.9 The MINORS scale was completed by two investigators and then averaged as the scale process is complicated. The results were cross-checked.
Statistics Analysis
Data analyses were based on aggregated data if available. We extracted data from the included researches. We calculated responder proportions with 95% CI using suitable model (fixed effects inverse variance weight model or random effects inverse variance weight model) with a double arcsine transformation. Heterogeneity was quantified by use of the I2 statistic.
In brief, we performed data-analysis of the RCTs via RevMan 5.4 software provided by the Cochrane Collaboration Network. The risk ratio (RR) for effectiveness, RRADR for safety and associated 95% confidence intervals (95% CIs) were calculated for the count data measure. The data analysis of SATs were analyzed by STATA12 software, the eradication rates were calculated for effectiveness, rADR for safety and their 95% CIs were used for count data measure. The pooled eradication rates of the SATs were compared with the ideal treatment target meeting the following criteria: the eradication rate by ITTA up to 90% was defined as the ideal goal10; up to 80% was defined as the minimum ideal target.11,12 If the eradication rate by ITTA was less than 80%, it was considered as unacceptable.
The study heterogeneity was measured by Q test and I2. The details, according to the Cochrane Handbook, were as follows:13 P ≥0.10 (Q test) and I2 ≤ 40% suggesting low heterogeneity among studies and fixed effects inverse variance weight model was adopted in the statistical process; P ≥ 0.10 and 40%< I2 ≤60% had moderate heterogeneity and random effects inverse variance weight model was adopted; and P < 0.10 and I2 >60% or P <0.10 and 40%< I2 ≤60% suggesting the heterogeneity was large and the pooled analysis was not appropriate; in this case, descriptive analysis or subgroup analysis were conducted. Whether there was a statistically significant difference between the control and treatment groups depended on the test level (P=0.05).
Results
Characteristics of the Included Studies
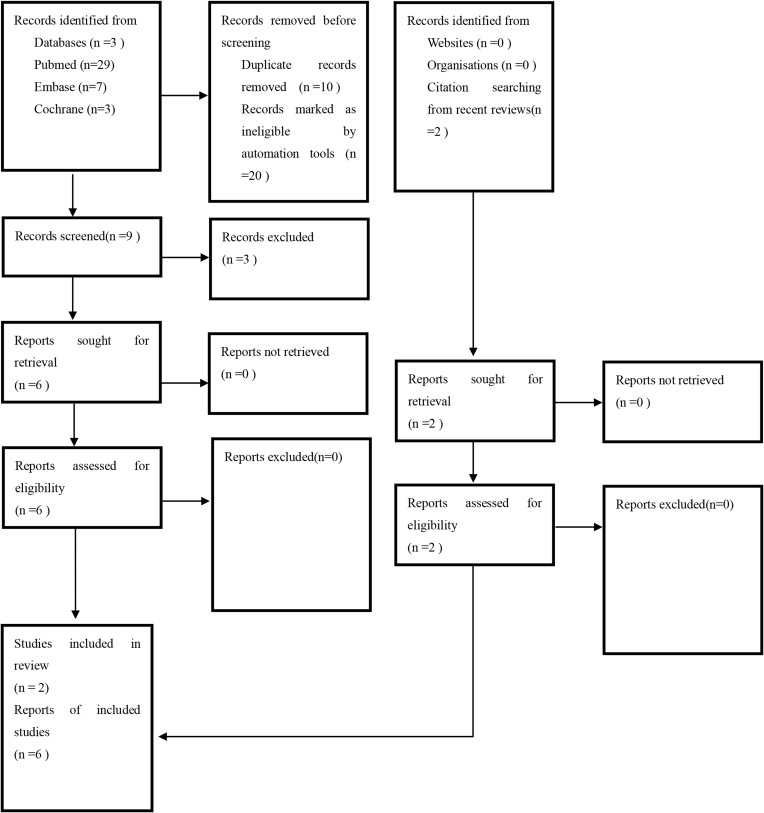
The selection process is shown in Figure 1.
Figure 1.
Flowchart of the details of the study.
Clinical Randomized Controlled Trials
Three included studies (Table 1)15,17,19 were conducted in three countries from Asia (South Korea) and Europe (Poland and Turkey), ranging from 2011 to 2018. All patients were adults, of which 486 were in the control group and 168 in the treatment group, and both without the rescue treatment. In the control group, all patients received the first-line regimens (five triple amoxicillin-containing regimens and one quadruple tetracycline-containing regimen) for H. pylori eradication. In the treatment group, there were two triple and one quadruple rifaximin-containing regimens. The duration was 7 –14 days. Breath tests were conducted 4 to 6 weeks after the completion of treatment in all cases.
Table 1.
Main Characteristics of the Including Trials
| 1. The Randomized Controlled Trials | ||||||||||||||
| Study | Year | Country | Case of rifaximin (Co/Tr) | Average age (Co/Tr) | IT | Treatment endpoint detection | Controlled regimen | Treatment regime | Duration | Eradication (ITT) controlled/ Tr | Eradication (PP) controlled/ Tr | ADR (Co/Tr) | Conclusion | |
| Konrad15 | 2018 | Poland | 30/32 | 42.6 ±8.2/45.4 ±11.010 | Y | 6 weeks after the therapy both tests (LHBT and 13C-UBT) were repeated | P 40 mg bid, A 1000 mg bid, M 500 mg bid | P40 mg bid, A 1000 mg bid, R 400 mg tid | 10d | 19/30 | 19/30 | 3/30 | Combination of A and R may be effective in the treatment of patients of HP infection | |
| 19/32 | 19/28 | 0/32 | ||||||||||||
| Sezgin17 | 2016 | Turkey | 259/38 | (45.1 ± 13.5/43.0 ± 13.4/44.3 ± 12.2)/47.0 ± 12.3 | Y | At least 4 weeks after the completion of treatment, eradication was confirmed by the urea breath test. | 1.Ra 20 mg bid, A 1000 mg bid, C 500 mg bid 2.Ra 20 mg bid, A 1000 mg bid, M 500 mg tid 3.Ra 20 mg bid, B 300mg qid, T 500 mg qid, M 500 mg tid | Ra 20 mg bid, A 1000 mg bid, R 400 mg bid | 14d | 132/259 | 132/229 | 6/259 | It was observed that eradication results of classical triple and quadruple therapy schedules were once again quite insufficient. | |
| 16/42 | 16/37 | 0/42 | ||||||||||||
| Choi19 | 2011 | Korea | 197/98 | (55.6 ± 16.2/55.5 ± 11.1)/52.7 ± 12.5 | Y | After the treatment (in 4–6 weeks) by ammonia breath test. | 1.O 20mg bid, A1g bid, C500mg; bid 2.O 20 mg bid, A 1g bid, Le 200 mg bid | O 20 mg bid, A 1 g bid, Le 200 mg bid, R 400 mg bid | 7 d | 141/197 | 141/177 | 90/197 | The L and R based regimen comes up to the standard triple therapy, but has a limited efficacy in a Korean cohort. The R containing regimen has a very high safety profile for Hp eradication therapy. | |
| 73/98 | 73/91 | 37/91 | ||||||||||||
| 2. The Single Arm Trials | ||||||||||||||
| Author | Year | Country | Cases of rifaximin | Average age | IT | Gender (M/F) | Complication | Treatment endpoint detection | Therapeutic regime | Duration | Eradication (ITT) | Eradication (PP) | ADR | Conclusion |
| Kim14 | 2020 | Korea | 27 | 55.5±13.8 | Y | 20:07 | Benign gastric ulcer: 8 | A 13C-urea breath test performed 4 weeks after therapy completion | R:600 mg bid, A: 1000 mg bid, C:500 mg bid, a standard PPI dose (P:40 mg, E:40 mg, L 30 mg, O:20 mg, Ra:20 mg) bid. | 14d | 19/27 | 19/22 | ITT:6/27 (22.22%) PP:5/22 (22.73%) | The findings of this study show the limitations of R-based quadruple therapy. |
| Duodenal ulcer:4 | ||||||||||||||
| Gastric dysplasia or cancer: 5 | ||||||||||||||
| Non-ulcer dyspepsia:10 | ||||||||||||||
| Konrad15 | 2018 | Poland | 32 | 45.4 ±11.010 | Y | 10:18 | - | 6 weeks after the therapy both tests (LHBT and 13C-UBT) were repeated | P: 40 mg bid, A:1000 mg bid, R: 400 mg tid | 10d | 19/32 | 19/28 | ITT:0/32 (0.00%) | Combination of A and R may be effective in the treatment of Hp infection. |
| PP:0/28 (0.00%) | ||||||||||||||
| Ramasa16 | 2017 | Spain | 40 | 44 ± 15 | Y | 19:21 | Non investigated dyspepsia 24 | The 13c-urea breath test at least 4 weeks after the end of treatment | R: 400 mg tid, C: 500 mg bid, A:1 g bid, O:20 mg bid | 10d | 22/40 | 22/36 | ITT:27/40 (67.50%) | Acceptable Hp eradication rates are not achieved with R associated with standard triple therapy for 10 days. |
| Functional dyspepsia15 | PP:27/36 (75.00%) | |||||||||||||
| Gastric ulcer 1 | ||||||||||||||
| Sezgin17 | 2016 | Turkey | 38 | 47.0 ± 12.3 | Y | 22:20 | Peptic ulcer:7 | At least 4 weeks after the completion of treatment, eradication was confirmed by the urea breath test. | Ra:20 mg bid, A:1000 mg bid, R:400 mg bid | 14 d | 16/42 | 16/37 | ITT:0/42 (0.00%) | It was observed that eradication results of classical triple and quadruple therapy schedules were once again quite insufficient. |
| Non-ulcer dyspepsia:31 | PP:0/37 (0.00%) | |||||||||||||
| Other (family history for gastric cancer, patient request):4 | ||||||||||||||
| Yun18 | 2012 | Korea | 47 | 53±13 | N | - | - | Eradication of Hp was determined by the urea breath test performed 4 weeks after treatment. | R:200 mg tid, Le: 500 mg qd, P:20 mg bid | 7d | 26/47 | 26/40 | ITT:6/47(12.77%) | R plus Le-based regimen could be an alternative rescue therapy in patients with resistance to both triple and quadruple regimens for the eradication of Hp. |
| PP:6/40(15.00%) | ||||||||||||||
| Choi19 | 2011 | Korea | 98 | 52.7 ± 12.5 | Y | 59:39 | Gastric ulcer:44 Duodenal ulcer:29 Both:2 Gastritis:23 | Eradication of Hp was assessed by the 13C-UBT at 6 weeks after completion of treatment. | O: 20 mg bid, A: 1 g bid, Le:200 mg bid, R: 400 mg bid | 7d | 73/98 | 73/91 | ITT:37/98 (37.76%) PP:37/91 (40.66%) | The Le and R based regimen comes up to the standard triple therapy, but has a limited efficacy in a Korean cohort. The R containing regimen has a very high safety profile for Hp eradication therapy. |
| Nizhevich20 | 2011 | Russian | 41 | 14.5 ± 1.4 | Y | 14:27 | - | After the treatment (in 4–6 weeks) by ammonia breath test. | B (8 mg/kg/day, qd) for 14 days, R:(800mg/day) and F (10 mg/kg /day, qd) or N (15 mg/kg /day, bid) | 10d | 35/41 | - | 0/41 (0%) | The combination of R, B and furazolidone/nifuratel was an effective and tolerable regimen for initial Hp eradication. |
| Gasbarrini 121 | 2006 | Italy | 24 | 39 ± 13 | Y | 13:11 | - | A 13 C-urea breath test 4 weeks after the end of therapy | R tablets 400 mg tid, E: 40 mg qd, C: 500 mg bid. | 7d | 14/24 | - | 13/24 (54.17%) | R-based therapy showed optimal compliance but a limited eradication rate compared to standard first-line treatment. |
| Gasbarrini 221 | 2006 | Italy | 24 | 40± 11 | Y | 15:09 | - | A 13 C-urea breath test 4 weeks after the end of therapy | Le:500 mg qd, R tablets 400 mg tid, E: 40 mg qd. | 7d | 10/24 | - | 10/24 (41.67%) | R-based therapy showed optimal compliance but a limited eradication rate compared to standard first-line treatment. |
Abbreviations: Co, controlled group; Tr, treatment group; d, days; ADR, adverse drug reaction, IT, Initial treatment; R, rifaximin; A, amoxicillin; C, claritromicin; P, pantoprazole; E, esomeprazole; L, lansoprazole; O, omeprazole; Ra, rabeprazole; Le, levofloxacin; B, bismuth subcitrate; M, metronidazole; T, tetracycline; M, male; F, female; Hp, H. pylori; d, day; Y, yes; N, no.
Single-Arm Clinical Trials
Nine studies from eight literatures were included (Table 1)14–21, which were conducted in six countries in Asia (South Korea) and Europe (Turkey, Russia, Spain, Italy and Poland), ranging from 2006 to 2020. All these countries are located in the Northern Hemisphere. Only one study was conducted in teenagers (aged 14.5 ± 1.4 years), and 8 studies were conducted in adults. The sample size of the treatment group ranged from 24 to 98, with a total of 371 patients. The patients’ sexes were recorded from eight studies, including 172 males and 152 females in total. One study was the rescue treatment; the rest were initial treatment. Three studies used quadruple regimens, and six used triple regimens. The treatment duration was 7–14 days.
Evaluation of Literature Quality
Three clinical RCTs with scores between 4 and 5 by the JADAD scale were of high quality (Supplementary Table 1). They were also assessed by the Cochrane Bias Assessment Tool, 1 was at unclear risk and 2 were at low risk, all are acceptable (Supplementary Table 2). However, the main information, including “random method” and “other bias content”, were poorly described. The MINORS scale was used to evaluate the quality of nine SATs. The scores ranged from 9.5 to 11.5, indicating moderate quality (Supplementary Table 3). The major problems were that some delayed adverse effects might not be observed in such a short follow-up period, and it is difficult to estimate sample size that might produce a significant positive effect.
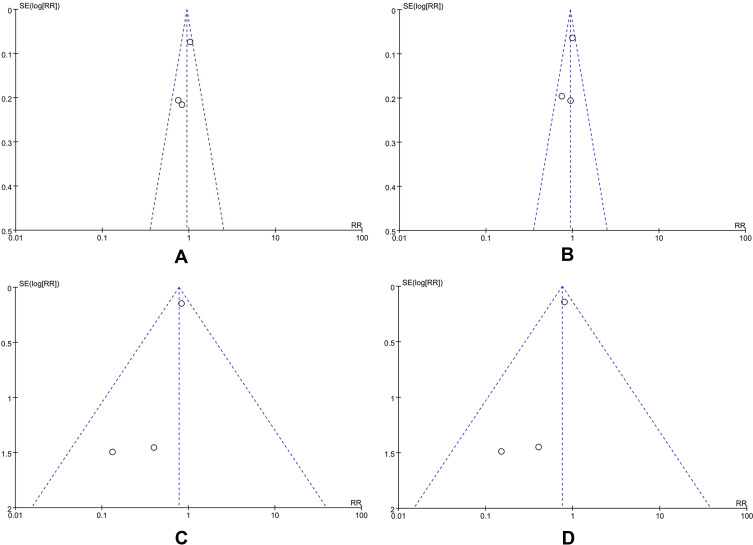
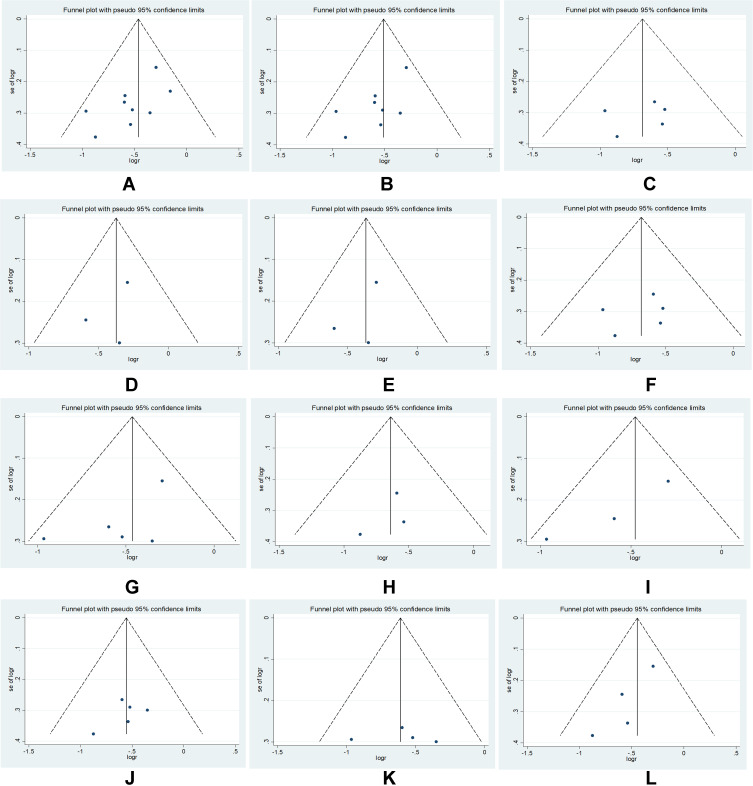
In RCTs and SATs (effectiveness and safety by ITT and PP analysis), the funnel plots were out of range, suggesting obvious publication bias (Figures 2 and 3).
Figure 2.
Publication bias of randomized controlled trials (Funnel plot). (A) The effectiveness of rifaximin-containing vs controlled group (ITTA). (B) The effectiveness of rifaximin-containing vs controlled group (PPA). (C) The safety of rifaximin-containing vs controlled group (ITTA). (D) The safety of rifaximin-containing vs controlled group (PPA).
Abbreviations: ITTA, intention-to-treat analysis; PPA, per-protocol analysis.
Figure 3.
Publication bias of single arm trials with the effectiveness by ITTA (Funnel plot). (A) Rifaximin-containing regimen. (B) The adults. (C) European adult patients. (D) Asian adult patients. (E) Quadruple rifaximin-containing. (F) Triple rifaximin-containing. (G) Rifaximin-containing with amoxicillin. (H) Rifaximin-containing without amoxicillin. (I) Rifaximin above 1g/d. (J) Rifaximin below 1g/d. (K) Rifaximin-containing more than 10d. (L) Rifaximin-containing less than 10d.
Abbreviation: ITTA, intention to treat analysis.
Effectiveness and Safety Profile
Clinical Randomized Controlled Studies
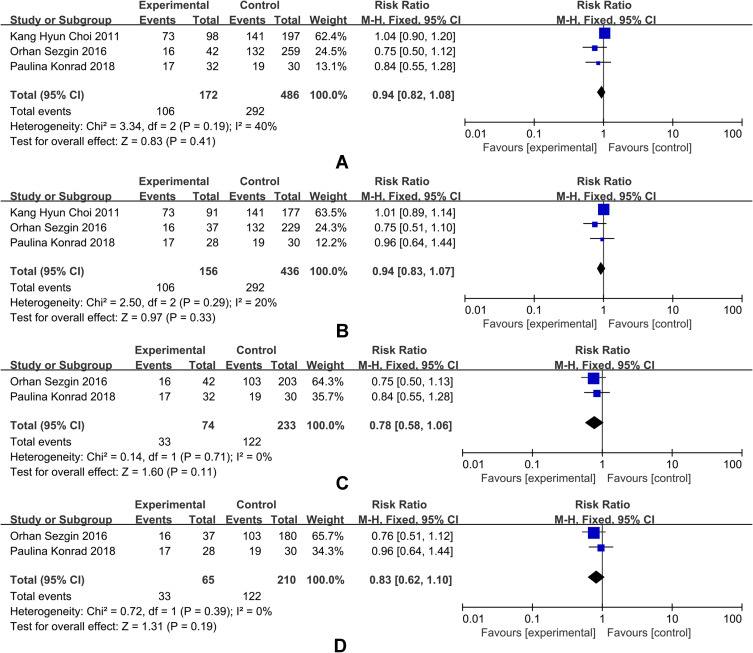
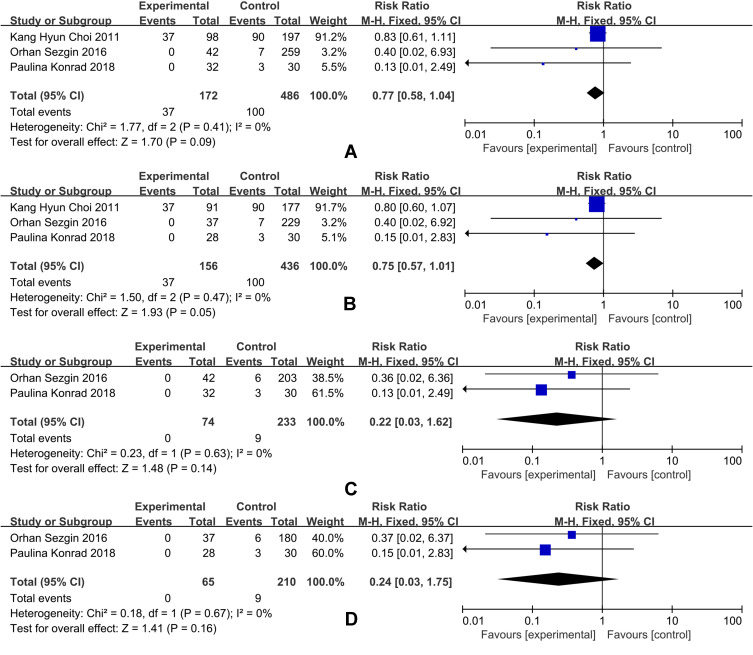
For rifaximin-containing regimens, the efficacy and safety were compared with those of the first-line triple or quadruple regimens in three studies showing low heterogeneity. Compared with the control group, the difference in eradication rate was not statistically significant (pooled RR for ITTA= 0.94, P = 0.41, 95% CI [0.82–1.08]; pooled RR for PPA = 0.94, P = 0.33, 95% CI [0.83–1.07]) (Figure 4), and similar observations were also seen in safety (pooled RR for ITTA = 0.77, P = 0.09, 95% CI [0.58–1.04]; pooled RR for PPA = 0.75, P = 0.05, 95% CI [0.57–1.01]) (Figure 5). The subgroup analysis showed that the efficacy of the rifaximin-containing triple regimen was consistent with those of the first-line triple regimen (pooled RR for ITTA = 0.78, P=0.11, 95% CI [0.51–1.06]; pooled RR for PPA = 0.83, P=0.19, 95% CI [0.62–1.10]) (Figure 4), similar to the trend in safety analysis (pooled RR for ITTA = 0.22, P = 0.14, 95% CI [0.03–1.62]; pooled RR for PPA = 0.24, P = 0.16, 95% CI [0.03–1.75]) (Figure 5).
Figure 4.
Forest plot for the effectiveness of randomized controlled trials with rifaximin-containing regimens. (A) Rifaximin-containing vs controlled group (ITTA). (B) Rifaximin-containing vs controlled group (PPA). (C) Rifaximin-containing triple vs standard triple regimen (ITTA). (D) Rifaximin-containing triple vs standard triple regimen (PPA).
Abbreviations: ITTA, intention-to-treat analysis; PPA, per-protocol analysis; RR, risk ratio.
Figure 5.
Forest plot for the safety of randomized controlled trials with rifaximin-containing regimens. (A) Rifaximin-containing vs controlled group (ITTA). (B) Rifaximin-containing vs controlled group (PPA). (C) Rifaximin-containing triple vs standard triple regimen (ITTA). (D) Rifaximin-containing triple vs standard triple regimen, (PPA).
Abbreviations: ITTA, intention-to-treat analysis; PPA, per-protocol analysis; RR, risk ratio.
Clinical Single-Arm Trials
Overall
A total of nine studies were included. Due to the high heterogeneity (I2=80.6%, P =0.00), the result could not be pooled. The eradication rate by ITTA of each study varied with regions and populations, from 38.1% to 85.4%.
The manifestations of ADR were mainly gastrointestinal discomfort. The overall incidence of ADR in all studies on ITTA and PPA basis showed high heterogeneous (Table 1), and the distribution range was wide (rADR ITT: 0–0.675: rADR PP: 0–0.75 respectively by ITTA and PPA).
Subgroup Analysis
In the subgroups (different regions, triple or quadruple, with or without amoxicillin, different duration and the rifaximin dose), the effectiveness analysis was carried out in order to reduce the high heterogeneity among these studies. However, in a few subgroups, the results cannot still be pooled due to the heterogeneity (Table 2 and Supplementary Figure 1).
Table 2.
Subgroup Analysis of Clinical Single-Arm Trials
| Item | Intention-to-Treat Analysis | Per-Protocol Analysis | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Quantity of Studies | Heterogeneity | Pooled | r | 95% CI | P | Quantity of Studies | Heterogeneity | Pooled | r | 95% CI | P | |
| Adults and pediatric patients | ||||||||||||
| The pediatric | 1 | – | N | 0.854 | [0.746–0.962] | |||||||
| The adult | 8 | I2=71.8, P =0.001 | N | 0.381–0.745 | [0.223–0.617] to [0.532–0.876] | 6 | I2=78.4, P=0.000 | N | 0.432–0.864 | [0.272–0.592] to [0.721–1.007] | ||
| Geographical distribution (adults) | ||||||||||||
| European | 5 | I2=26.7, P =0.243 | Y | 0.499 | 0.423–0.575 | 0.000 | 3 | I2=57.0, P =0.100 | Y | 0.572 | 0.427–0.716 | 0.000 |
| Asian | 3 | I2=61.0, P =0.077 | N | 0.553–0.745 | [0.411–0.695] to [0.532–0.876] | 3 | I2=55.9, P =0.100 | Y | 0.778 | 0.672–0.884 | 0.000 | |
| Asia (initial treatment) | 2 | I2=0, P =0.677 | Y | 0.737 | 0.660–0.814 | 0.000 | 2 | I2=0, P =0.461 | Y | 0.817 | 0.746–0.888 | 0.000 |
| Triple or quadruple regimen (adults) | ||||||||||||
| Triple | 5 | I2=28.4, P =0.232 | Y | 0.502 | 0.428–0.576 | 0.000 | 3 | I2=63, P =0.067 | N | 0.432–0.679 | [0.272–0.592] to [0.506–0.852] | |
| Quadruple | 3 | I2=57.3, P =0.100 | Y | 0.677 | 0.558–0.796 | 0.000 | 3 | I2=66.2%, P =0.01 | N | 0.611–0.864 | [0.452–0.770] to [0.721–1.007] | |
| With or without amoxicillin(adults) | ||||||||||||
| With amoxicillin | 5 | I2=79.7, P =0.001 | N | 0.381–0.745 | [0.234–0.528] to [0.532–0.876] | 5 | I2= 82.0, P =0.000 | N | 0.432–0.864 | [0.272–0.592] to [0.721–1.007] | ||
| Without amoxicillin | 3 | I2=0.0, P =0.442 | Y | 0.526 | 0.426–0.626 | 0.000 | 1 | – | 0.553 | 0.411–0.695 | ||
| Rifaximin dosage (adults) | ||||||||||||
| Above 1 g/d | 5 | I2=16.2, P =0.311 | Y | 0.576 | 0.497–0.654 | 0.000 | 3 | I2=65.8, P =0.054 | N | 0.611–0.864 | [0.452–0.770] to [0.721–1.007] | |
| Below 1 g/d | 3 | I2=89.5, P =0.000 | N | 0.381–0.745 | [0.234–0.528] to [0.659–0.831] | 3 | I2=88.3, P =0.000 | N | 0.432–0.802 | [0.272–0.592] to [0.720–0.884] | ||
| Duration (adults) | ||||||||||||
| Over 10 days | 4 | I2=64.2, P =0.039 | N | 0.381–0.704 | [0.234–0.528] to [0.532–0.876] | 4 | I2=81.3, P =0.001 | N | 0.432–0.864 | [0.272–0.592] to [0.721–1.007] | ||
| Below 10 days | 4 | I2=75.3, P =0.007 | N | 0.420–0.745 | [0.223–0.617] to [0.659–0.831] | 2 | I2=57.8, P =0.078 | N | 0.650–0.802 | [0.502–0.798] to [0.720–0.884] | ||
Abbreviations: Y, yes; N, no; r, eradication rate.
The eradication rate by ITTA in European pediatric patients was 85.4% (95% CI [0.746–0.962]), which was significantly higher than that of adults in Europe (pooled r=0.499, P =0.000, 95% CI [0.423–0.575] by ITTA).
The subgroup analysis in adults showed that the pooled eradication rate (pooled r=0.499) in European adult patients might be lower than that in Asian adult patients (r=0.553–0.745). Among them, as the 95% CI range is higher and with no overlap, the differences for eradication rate between European (pooled r=0.499, P=0.000, 95% CI [0.423–0.575] by ITTA, pooled r=0.572, P=0.000, 95% CI [0.427–0.716] by PPA) and Asian-naïve patients (pooled r=0.737, P=0.000, 95% CI [0.660–0.814] by ITTA, pooled r=0.817, P=0.000, 95% CI [0.746–0.888] by PPA) were statistically significant.
For the adult population, the quadruple rifaximin-containing regimens (pooled r=0.677, P=0.000, 95% CI [0.558–0.796] by ITTA) may have a higher eradication rate than that of the triple regimens (pooled r=0.502, P=0.000, 95% CI [0.428–0.576] by ITTA). However, as their 95% CI overlap, the difference in eradication rate between both groups was not statistically significant.
So far, as the results cannot be pooled and compared directly, there is no evidence implying that rifaximin-containing regimens have obvious dose–effect relationship. Meanwhile, it has not yet been proved that adding amoxicillin or prolonging treatment duration could improve the effectiveness of these regimens obviously.
Overall, the eradication rates by ITTA in adults, whether the data were pooled or not, may not meet the ideal or at least the minimum ideal target. Only one study showed that the eradication rate by ITTA in the pediatric can achieve the minimum ideal target rather than the ideal target.
Discussion
The Kyoto Global Consensus highlighted that H. pylori gastritis should be defined as an infectious disease and its harmful effects on public health worldwide be considered. Based on this view, it should offer the effective and safe eradication therapy to H. pylori infected individuals unless there are competing considerations. Given health status is diverse at different times and in different areas, the eradication rates may be optimized based on patients’ region and race. The conclusions of this study should not be interpreted without considering specific times, region and populations.
In this study, it showed no statistically significant differences of effectiveness and safety between rifaximin-containing and triple or quadruple first-line regimens. It also showed similar results between rifaximin-containing triple and first-line triple regimen in subgroup analysis. Significantly, the physicians are using the first-line triple regimens only in a few areas recently, because the H. pylori resistance rates to clarithromycin and metronidazole are more than 15% in most areas of the world that can cause the low eradication rates of triple regimen. Many countries do not recommend the use of the first-line triple regimen currently. The same effectiveness of the first-line triple regimen cannot fully prove rifaximin-containing regimen is effective enough at present. Based on this, it fails to justify a practice to apply these regimens with low eradication rates in most areas worldwide.In addition, the sample size was extremely limited. Therefore, based on the results of RCTs meta-analysis, rifaximin-containing regimens are not recommended currently.
The results of the systematic review on SATs are also not satisfactory. First, there was high heterogeneity in the eradication rates among the studies. Pediatric patients were excluded, and the distribution of eradication rate by ITTA remains wide, showing high instability with the efficacy of rifaximin-containing regimens. However, it was found that rifaximin-containing regimen may be more effective in pediatrics than in adults in the same region. Interestingly, H. pylori antibiotic resistance rate in pediatrics is similar to or even higher than that in adults,22 so the eradication rate among analogous regimens is expected to be close to that of adult patients.23 The result did not show it that may be because rifaximin plays its primary role in the gastrointestinal tract, which limits its wide use in pediatric patients and leads to higher sensitivity to H. pylori than the other antibiotics (amoxicillin, clarithromycin) those are commonly used in children. It is necessary to conduct further research by including larger sample size.
In this study, the eradication rate of Asian-naïve patients was significantly higher than that in Europe. It may due to the differences in socioeconomic development and H. pylori resistance among these regions. The resistance rate to rifaximin is less reported than that of other rifamycins, and is mainly reported by some countries in Asia (Bangladesh, Indonesia, Nepal), from 30% to 65%.8 However, there are no reports in Europe and Korea and the results may partly reflect the differences of resistance rates. In addition, adults from four European countries were from Eastern and Southern Europe and the result may not reflect the situation in Western and Northern Europe, where H. pylori resistance to antimicrobial drugs is lower traditionally.22,24,25 Therefore, this result may be more representative if more trials are from wider area. Whether the pooled or single research, the eradication rates fail to meet the minimum ideal target of the eradication rate, the rifaximin-containing regimens in adults may not be recommended, although the eradication rate in Asia was higher than that in Europe.
Currently, the guidelines and consensus suggest that quadruple therapy is more suitable for areas with high resistance rate to H. pylori.3,4 It illustrates the quadruple eradication regimens may serve as a trend due to their higher eradication rate. The results of this study indicate that the quadruple rifaximin-containing might be with higher eradication rate than the triple regimens. However, this difference is not statistically significant at present. Following the trend, if more studies are included in the future, the current conclusion may be changed.
Amoxicillin is the most important antibiotic in current first-line regimens as its low resistance rate and strong antibacterial effect.11,24 In the study, when the adults were given rifaximin-containing regimen, pooled eradication rate of amoxicillin-free treatment was far below the ideal target. While in amoxicillin-containing regimens, higher heterogeneity showed that their eradication rates were unstable. However, the result of this study suggests that amoxicillin was given at adequate doses does not seem to significantly improve the eradication rate. The similar situation occurred in duration subgroups. The distribution of eradication rates by ITT and PP analysis (the distribution of the 95% Cl was wide and overlapped materially between the two groups) did not show the trend that lengthening treatment duration increase the eradication rate in rifaximin groups.In addition, certain drugs, such as amoxicillin and metronidazole, yield a positive dose–effect relationship about H. pylori eradication. In our study, regimens with rifaximin above 1 g/d did not achieve the expected outcome (pooled r=0.576, P=0.000, 95% CI [0.497–0.654] by ITTA), but rifaximin below 1 g/d could still yield high eradication rates in some patients (r=0.745, 95% CI [0.659–0.831] by ITTA).
In general, the results of the systematic review are not satisfactory. Our findings do not prove the availability of the regimens. Compared with other rifamycin, rifaximin does not seem to show the same effect.8 A similar situation occurs when furazolidone, another non-absorbable antibacterial agent, was used to eradicate H. pylori.26 The mechanism is unclear yet, the possible explanation may be that non-absorbable antibiotics are lack of the gastric mucosal transfer process, may reduce the duration of H. pylori exposed to the agents, resulting in insufficient eradication efficacy.27 It is valid to consider making floating drug delivery system in stomach to increase the retention time.
Our study has some limitations. First, the studies and patients enrolled in this research were insufficient. Only three RCTs were included in the study, with 172 patients in the rifaximin group and 486 patients in the control group. As the sample size was small, there were obvious publication biases, which may affect the accuracy of the results. Next, in the clinical studies, clinical heterogeneity, such as the different interventions, may have influence on the results. Then, in SATs, clinical heterogeneity and other factors may have led to high statistical heterogeneity. Thus, descriptive evaluation could be a suitable way to objectively evaluate these results, which may reduce the accuracy of results. Finally, some known factors currently that may have impacts on eradication rates do not seem to be taken into account in these studies, such as oral H. pylori colonization rates28,29 and bile reflux gastric disease.30 In addition, another advantage of rifaximin, which can reduce bacterial toxins and alleviate the inflammatory response in stomach, has not been evaluated at all.
Conclusion
In conclusion, rifaximin-containing regimens should not be recommended for H. pylori eradication currently from this research as the eradication rates almost fail to meet the minimum ideal or ideal target and with unstable safety. Further researches on this topic are still needed through modifying the existing regimens to achieve satisfactory treatment target, especially in the regions having better effectiveness now (Russia and South Korea).
Acknowledgment
We will show our gratitude to Dr Yin Liu for the linguistic revision.
Funding Statement
No funding supported this manuscript.
Data Sharing Statement
All data are reflected in the manuscript.
Disclosure
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Ji CR, Liu J, Li YY, et al. Safety of furazolidone-containing regimen in Helicobacter pylori infection: a systematic review and meta-analysis. BMJ Open. 2020;10:e037375. doi: 10.1136/bmjopen-2020-037375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.O’Connor A, O’Morain CA, Ford AC. Population screening and treatment of Helicobacter pylori infection. Nat Rev Gastroenterol Hepatol. 2017;14(4):230–240. doi: 10.1038/nrgastro.2016.195 [DOI] [PubMed] [Google Scholar]
- 3.Chey WD, Leontiadis GI, Howden CW, Moss ST. ACG clinical guideline: treatment of Helicobacter pylori infection. Am J Gastroenterol. 2017;112:212–238. doi: 10.1038/ajg.2016.563 [DOI] [PubMed] [Google Scholar]
- 4.Malfertheiner P, Megraud F, O’Morain CA, et al; European Helicobacter and Microbiota Study Group and Consensus Panel. Management of Helicobacter pylori infection-The Maastricht V/Florence consensus report. Gut. 2017;66(1):6–30. doi: 10.1136/gutjnl-2016-312288 [DOI] [PubMed] [Google Scholar]
- 5.DuPont HL, Pelosini I. Review article: the antimicrobial effects of rifaximin on the gut microbiota. Aliment Pharmacol Ther. 2016;43:3–10. [DOI] [PubMed] [Google Scholar]
- 6.Scarpignato C, Pelosini I. Rifaximin, a poorly absorbed antibiotic: pharmacology and clinical potential. Chemotherapy. 2005;51(1):36–66. doi: 10.1159/000081990 [DOI] [PubMed] [Google Scholar]
- 7.Shayto RH, Mrad RA, Sharara AI. Use of rifaximin in gastrointestinal and liver diseases. World J Gastroenterol. 2016;22(29):6638–6651. doi: 10.3748/wjg.v22.i29.6638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boyanova L, Markovska R, Hadzhiyski P, Kandilarov N, Mitov I. Rifamycin use for treatment of Helicobacter pylori infection: a review of recent data. Future Microbiol. 2020;15(12):1185–1196. doi: 10.2217/fmb-2020-0084 [DOI] [PubMed] [Google Scholar]
- 9.Morvan A, Bouguennec N, Graveleau N. ACL injuries before 15 years of age: could the young become an athlete? Arch Orthop Trauma Surg. 2020;140:1055–1063. doi: 10.1007/s00402-020-03404-8 [DOI] [PubMed] [Google Scholar]
- 10.Zhang M. High antibiotic resistance rate: a difficult issue for Helicobacter pylori eradication treatment. World J Gastroenterol. 2015;21(48):13432–13437. doi: 10.3748/wjg.v21.i48.13432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang JC, Lu CW, Lin CJ. Treatment of Helicobacter pylori infection: current status and future concepts. World J Gastroenterol. 2014;20(18):5283–5293. doi: 10.3748/wjg.v20.i18.5283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gisbert JP, Calvet X. Review article: rifabutin in the treatment of refractory Helicobacter pylori infection. Aliment Pharmacol Ther. 2012;35:209–221. doi: 10.1111/j.1365-2036.2011.04937.x [DOI] [PubMed] [Google Scholar]
- 13.Higgins J, Thomas J. Cochrane handbook for systematic reviews of interventions [DB/OL]. Available from: https://training.cochrane.org/handbook/current/chapter-07. Accessed October 21, 2021.
- 14.Kim HS, Yoon H, Shin DW, et al. Efficacy of and resistance to rifaximin-based quadruple therapy in Helicobacter pylori eradication. Korean J Helicobacter Up Gastrointest Res. 2020;20(3):218–224. doi: 10.7704/kjhugr.2020.0021 [DOI] [Google Scholar]
- 15.Konrad P, Chojnacki J, Gąsiorowska A, et al. Therapeutic efficacy of amoxicillin and rifaximin in patients with small intestinal bacterial overgrowth and Helicobacter pylori infection. Gastroenterology Rev. 2018;13(3):213–217. doi: 10.5114/pg.2018.74228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ramas M, Donday MG, McNicholla AG, Rudnicki C, Kaczka A, Chojnacki C. Efficacy and safety of rifaximin associated with standard triple therapy (omeprazole, clarithromycin and amoxicillin) for H. pylori eradication: a Phase IV pilot clinical trial. Gastroenterol Hepato. 2017;40(10):658–662. doi: 10.1016/j.gastrohep.2017.05.017 [DOI] [PubMed] [Google Scholar]
- 17.Sezgin O, Aydın MK, Ateş F, Altıntaş E, Üçbilek E, Yaraş S. Addition of rifaximin and N-Acetyl Cysteine to the standard Helicobacter pylori treatment regimens: is it possible to improve outcomes? J Gastric Disord Ther. 2016;2(2):117. [Google Scholar]
- 18.Yun SP, Seon HG, Chang SO, et al. Rifaximin plus levofloxacin-based rescue regimen for the eradication of Helicobacter pylori. Gut Liver. 2012;6(4):452–456. doi: 10.5009/gnl.2012.6.4.452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Choi KH, Chung WC, Lee KM, Paik CN, Kim EJ. Efficacy of levofloxacin and rifaximin based quadruple therapy in Helicobacter pylori associated gastroduodenal disease: a double-blind, randomized controlled trial. J Korean Med Sci. 2011;26:785–790. doi: 10.3346/jkms.2011.26.6.785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nizhevich AA, Shcherbakov PL, Akhmadeeva ÉN, Khasanov RS. Rifaximin in combined treatment of the Helicobacter pylori infection in childhood. Eksp Klin Gastroenterol. 2011;1(1):85–87. [PubMed] [Google Scholar]
- 21.Gasbarrini A, Lauritano EC, Nista EC, et al. Rifaximin-based regimens for eradication of Helicobacter pylori: a pilot study. Dig Dis. 2006;24(1–2):195–200. doi: 10.1159/000090330 [DOI] [PubMed] [Google Scholar]
- 22.Savoldi A, Carrara E, Graham DY, Conti M, Tacconelli E. Prevalence of antibiotic resistance in Helicobacter pylori: a systematic review and meta-analysis in World Health Organization Regions. Gastroenterology. 2018;155(5):1372–1382. doi: 10.1053/j.gastro.2018.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kalach N, Bontems P, Raymond J. Helicobacter pylori infection in children. Helicobacter. 2017;22(Suppl. 1):e12414. doi: 10.1111/hel.12414 [DOI] [PubMed] [Google Scholar]
- 24.Smith SM, O’Morain C, Mcnamara D. Helicobacter pylori resistance to current therapies. Curr Opin Gastroenterol. 2019;35(1):6–13. doi: 10.1097/MOG.0000000000000497 [DOI] [PubMed] [Google Scholar]
- 25.Samantha FT, Soraya MO, Paola BI, et al. Helicobacter pylori drug resistance: therapy changes and challenges. Expert Rev Gastroenterol Hepatol. 2018;12(8):819–827. doi: 10.1080/17474124.2018.1496017 [DOI] [PubMed] [Google Scholar]
- 26.Zhuge L, Wang Y, Wu S, Zhao R, Li Z, Xie Y. Furazolidone treatment for Helicobacter Pylori infection: a systematic review and meta-analysis. Helicobacter. 2018;23(2):e12468. doi: 10.1111/hel.12468 [DOI] [PubMed] [Google Scholar]
- 27.Goddard AF. Review article: factors influencing antibiotic transfer across the gastric mucosa. Aliment Pharmacol Ther. 1998;12:1175–1184. doi: 10.1046/j.1365-2036.1998.00425.x [DOI] [PubMed] [Google Scholar]
- 28.Hou HL, Meng HX, Wen-Jie HU, Wang J-W. The relationship between Helicobacter pylori in oral cavity and the Hp infection in stomach. Zhonghua Kou Qiang Yi Xue Za Zhi. 2003;38(5):327–329. [PubMed] [Google Scholar]
- 29.Krzyżek P, Gościniak G. Oral Helicobacter pylori: interactions with host and microbial flora of the oral cavity. Dent Med Probl. 2018;55(1):75–82. doi: 10.17219/dmp/81259 [DOI] [PubMed] [Google Scholar]
- 30.Shao CH, Zhang QY, Sun YD, et al. Helicobacter pylori protein response to human bile stress. J Med Microbiol. 2008;57(2):151–158. doi: 10.1099/jmm.0.47616-0 [DOI] [PubMed] [Google Scholar]