Abstract
Background
Difficult laryngoscopy/intubation can cause a multitude of issues, including hypoxia, brain damage, and even death if not addressed swiftly. The Modified Mallampati test (MMT) is frequently used to predict difficult airway in patients with no clear difficult airway signal, despite its limited predictive power, in patients with no obvious difficult airway signal. Cormack and Lehane grading (CLG) is the gold standard, however it is not utilized before anesthesia.
Objective
To compare modified Mallampati classification (MMC) with Cormack and Lehane grading in predicting difficult laryngoscopy among patients who took general anesthesia.
Method
An institutionally based cross sectional survey study of 141 elective surgical patients with no obvious difficult airway sign was conducted from February to April 2021. The correlation between MMC and CLG was computed using spearman's correlation coefficient, and the area under the curve (AUC) for MMT was assessed using receiver operating characteristics (ROC) curve analysis.
Result
The incidence of difficult laryngoscopy and intubation, respectively, was 14.9% and 9.2%. The Spearman correlation coefficient (ρ) was 0.330, with a significance level of 0.001. The AUCs for difficult laryngoscopy and intubation, respectively, were 0.705 and 0.726. MMT had 47.6% sensitivity and 93.3% specificity for difficult laryngoscopy and 53.8% and 91.4% specificity for difficult intubation, respectively.
Conclusion
and Recommendation: There was little correlation between MMC and CLG. MMT sensitivity was similarly low. As a result, as part of the screening test for difficult airway, extra clinical tests are required.
Keywords: Difficult laryngoscopy, Modified Mallampati classification, Cormak and lehane grading, Difficult intubation
Highlights
-
•
Effective preoperative airway assessment reduces the difficulties of laryngoscopy and airway-related problems.
-
•
The modified Mallampati air way assessment is routinely used.
-
•
Cormack and Lehane grading is the gold standard for assessing airways.
-
•
This study compares the Mallampati and Lehan's grading techniques for predicting difficult laryngoscopy.
1. Introduction
One of the daily activities of anesthetic practice is airway management. Difficult airway is a troublesome and potentially fatal phenomena that anesthetists face in their work (see Fig. 1).
Fig. 1.
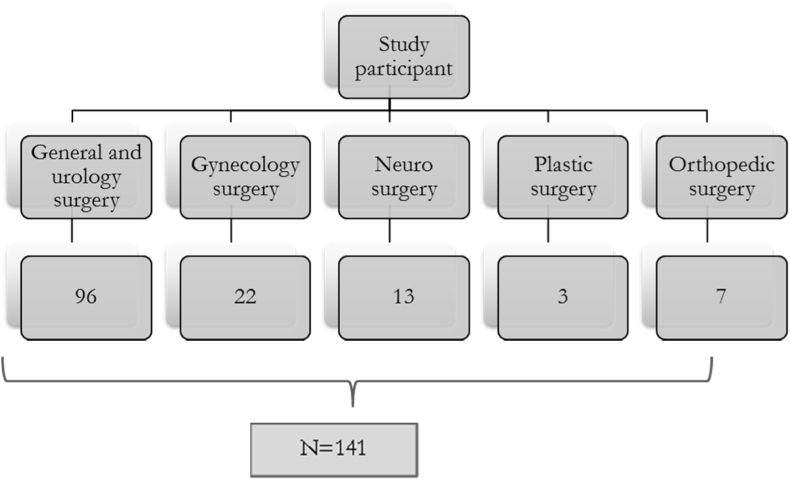
Sample size determination in three months in Werabie comprehensive specialized hospital.
Airway management using direct laryngoscopy is one of the daily tasks of anesthetist. Difficult laryngoscopy/intubation may cause various complications likes hypoxia, brain damage or even death if it is not managed early [[1], [2], [3]]. From all anesthesia related deaths, 30%–40% deaths are due to the inability to manage a difficult airway.(1) From more than half to one-third of cardiac arrests while performing general anesthesia, it is due to difficult airway which results in inadequate oxygenation and/or ventilation(4). Difficult laryngoscopy causes sore throat and serious airway trauma as well as aspiration of gastric contents or Mendelson syndrome (5). In 17% of difficult airway there is no documented preoperative airway assessment [1] and this is why difficult airway harms the patient due to inadequate preparation for such difficulties.
Globally, the prevalence of difficult laryngoscopy was reported to be between 1.5% and 20%, [2]. The variation in patient's characteristics that arises from their race or ethnicity causes the difference in the incidence of difficult laryngoscopy and difficult intubation from population to population [6]. To predict its presence, different physical examination tests have been used by anesthetists. Among these tests, Mallampati scoring is the most frequently used clinical bed side tests in the assessment of airway [2], [4], [6], [7].
Cormack and Lehane grading is a gold standard to predict difficult laryngoscopy and tracheal intubation. But this is done after induction and muscle relaxation, and not good to predict difficult laryngoscopy before induction.
Anticipating difficult airway in the preoperative period and preparedness to manage it is an important task of anesthetist. Among bed side clinical tests, most widely used and applicable one is modified Mallampati test. Its sensitivity, specificity, positive and negative predictive value in predicting difficult airway is studied by different researchers. But the diagnostic accuracy of MMT in predicting difficult laryngoscopy is variable [8]. Khatiwada S. et al. (2017) expressed its sensitivity is as higher [8], and other researchers as low ([1], [2], [9], [10]).
Cormack and Lehane determined the most widely used methods of classifying the degree of visualization of the vocal cord during direct laryngoscopy, in which laryngoscopic view is graded as grade I to grade IV [9,10,and11]]. This grading system is performed after induction of anesthesia and during direct laryngoscopy. Standard description of the laryngeal view is the best view of larynx with optimal head and neck positioning, optimum blade length and position, optimal external laryngeal manipulation and muscle relaxation (or abolition of glottic reflexes) [12].
Based on laryngeal structure view by direct laryngoscopy, Cormack and Lehane put Grade I: when the entire glottis is visible, Grade II: when posterior commissure of the glottis is visible, Grade III: when epiglottis only is visible, and Grade IV: when any portion laryngeal structure is invisible ([4,5,7,[10], [11], [12], [13]]).
Cormack and Lehane grade 3 and 4 are considered as difficult laryngoscopy (11, 12, and 14). In the C–L grading system, the degree of laryngeal aperture visualization during direct laryngoscopy had not clearly described. In grade 2 laryngeal view, portions of the vocal cord structure may be visible or only the arytenoid cartilages may be visible. Therefore grade 2 can be divided as grade 2a and 2b. when portion of the vocal cord is visible, we call it as grade 2a and when the arytenoid cartilage only is visible, it is considered as grade 2b. From grade 2 views, around 20% are Grade 2b [11].
Difficult laryngoscopy is said to be when unable to visualize the vocal cords, which includes Grades 2B, 3 and 4(7). From patients with grade 2b view, intubation is difficult in two-thirds of them, whereas from patients with grade 2a views, the prevalence of difficult intubation is around 4% [11].
There are multiple methods available to assess the airway difficulty used by anesthetists. However, the ideal and universally acceptable classification system is still ongoing [8]. Difficult laryngoscopy and intubation can be predicted in the preoperative period by using clinical assessments. Modified Mallampati classification is one of the tests used commonly [14].
Mallampati classification was first developed by Mallampati and later modified by Samson in 1987 [10]. Modified Mallampati classification has four classes. MMC is assigned after viewing oropharyngeal structure. This is done by putting the patient sitting up straight position with the head in neutral position. Then the patient opens the mouth maximally and protrude tongue out [10,15].
Modified Mallampati classes are assigned as Class I if hard palate, Soft palate, uvula, tonsillar fauces and pillars are visible; Class II if hard palate, Soft palate, fauces and uvula-tip may be masked-are visible; Class III if hard palate, Soft palate and base of uvula are visible; Class IV if hard palate only is visible and Soft palate is not visible at all. MM Class III and IV are considered as difficult laryngoscopy. [[9], [10], [11]] and [[16], [17], [18], [19]] There is also additional MMC which is called Class zero. If any part of the epiglottis is visible when the patient open his/her mouth and protrude the tongue during airway assessment, we call it class zero [19].
Appropriate preoperative airway assessment to identify persons at risk of difficult airway is a critical responsibility in preparing for the challenges ahead. MMT is most widely used as a method for preoperative airway examination. However, when used alone, it has a low predictive value, especially in people who have no obvious difficult airway sign, as documented by many writers. Despite the fact that anesthetists at Werabie comprehensive specialized hospital used the modified Mallampati test to predict difficult laryngoscopy and intubation in patients with no obvious difficult airway indicator and if class I and II were found, no one was prepared for difficult airway because it was thought to be simple.
Is it possible that such modified Mallampati classes correspond to Cormack and Lehane's grades? Which is the gold standard in patients who have no obvious risk factors for a difficult airway? Or are there issues with airway management and related complications due to a lack of preparation for the upcoming challenges?
As a result, this study would examine how well preoperatively estimated MMC matched with Cormack and Lehane grade during laryngoscopy, as well as how common difficult laryngoscopy and intubation were in patients with no obvious difficult airway sign.
2. Methods
It is an institutional-based Cross Sectional study conducted at Werabie comprehensive specialized hospital From February 2021–April 2021. This study has been registered with the Research Registration Unique Identifying Number (UIN):7689. https://www.researchregistry.com/browse-the-registry#home.This study is reported according to STROCSS 2021 guideline [21].
2.1. Study setting and period
This research was carried out at Werabie Comprehensive Specialized Hospital, a public hospital in the SNNPRs. It began operating in 2007 and is located 178 km from Addis Ababa. It serves a population of about 5 million people from the surrounding region with a wide range of outpatient and inpatient treatments. It provides general and specialized services such as neonatal intensive care unit (NICU), pediatric intensive care unit (PICU), adult intensive care unit (AICU), surgery, gynecology and obstetrics, ENT, neurology, maxillofacial, plastic, and orthopedic surgeries. The research took place between February and April of 2021.
2.2. Study design
Hospital-based cross sectional study design was employed.
2.3. Source population
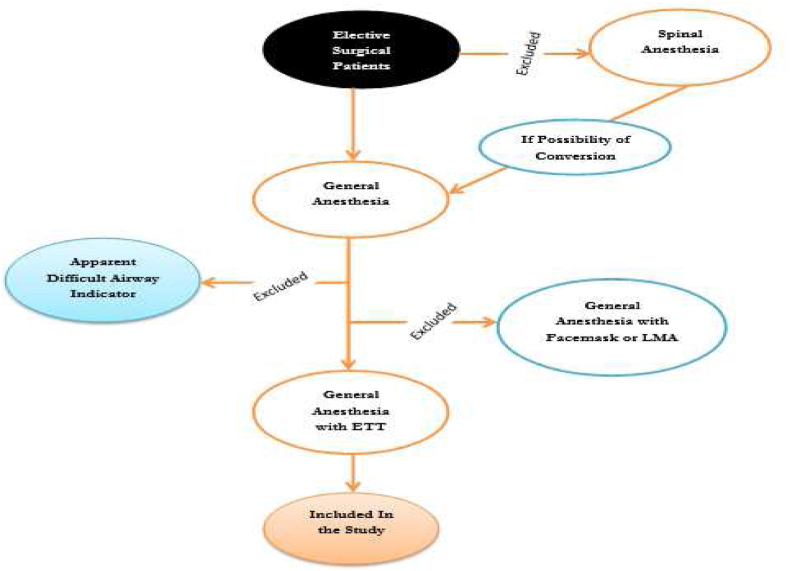
All patients who were undergone elective surgery with general anesthesia at Werabie comprehensive specialized hospital were selected.
2.4. Study population
All patients who were undergone elective surgery with general anesthesia with ETT at Werabie comprehensive specialized hospital were included.
2.5. Dependent variables
Difficult laryngoscopy, Difficult intubation.
2.6. Independent variables
MMC, CLG, Sociodemographic data, Types of surgery, BMI.
2.7. Operational definitions
Endotracheal tube: a tube use to insert into the trachea to provide artificial ventilation.
ASA classification: this is patient's physical status evaluation and based on the physical status of the patient it has six classes: class I, II, III, IV, V, and VI.
Body mass index: weight of the patient divided by height square. This is important to classify the patient as obese, overweight or normal.
Fixed Atlantooccipital joint: inability of atlantooccipital joint (the joint between the occipital bone and the first cervical vertebra) to slide.
Direct laryngoscopy: the procedure performed to visualize vocal cord using laryngoscope.
Prayer's sign: also known as diabetic stiff hand syndrome. It is inability of approximating one or more of the digits when the patient attempt to approximate palmar surface of the proximal and distal interphalangeal joints with palms pressed together and digits abducted.
Difficult laryngoscopy: inability to visualize the vocal cord during direct laryngoscopy after induction and muscle relaxation. CLG III and IV are considered as difficult laryngoscopy.
Apparent difficult airway indicator: any mass in the mouth, large anterior neck mass, short neck, fixed atlantooccipital joint and cervical vertebrae, maxillofacial trauma, Protruded teeth, temporomandibular joint ankylosis, burn contracture on the neck.
Difficult intubation: >3 attempts or 10 min is required to intubate the patient using direct laryngoscopy by experienced anesthetist (minimum of one year experience).
Huge goiter: class III goiter which means large goiter mass visible without palpation on normal position of head with pressure causes pressure marks and retrosternal extension occurred.
Modified Mallampati test: test used to predict difficult airway by viewing oropharyngeal structure. Based on this test, there are five classes viz: 0, I, II, III and IV.
Sensitivity: the conditional probability of correctly identifying difficult airway (difficult intubation and laryngoscopy) by modified Mallampati test or how correctly MMT correctly diagnose the presence of difficult airway.
Specificity: the probability of correctly diagnose or identify not being difficult airway by modified Mallampati test.
Positive predictive value: the probability of being difficult airway for MMT predicted difficult airway.
Negative predictive value: it is the probability of not being difficult airway for MMT predicted not being difficult airway.
2.8. Inclusion criteria
ASA class I & II, age of 18–65 years, BMI<30, Patients taking general anesthesia with ETT.
2.9. Exclusion criteria
DM patients with prayers sign, Patients with immobile atlantooccipital joint and cervical vertebrae, Patient with oral mass, Patient with maxillofacial trauma, Large anterior neck mass like huge goiter, Protruded teeth, TMJ ankylosis, Burn contracture on the neck., Those intubated with anesthetist whose experience was less than one year.
2.10. Sample size determination
During situational analysis, 144 patients were found in three months in Werabie comprehensive specialized hospital. Therefore, all eligible study participants in the study period were included. During the study period 141 eligible study participants were found.
3. Sampling technique
Study participant selection procedure.
All patients who fit the inclusion criteria in the study period were included.
3.1. Data collection technique
For data collecting, trained data collectors and a supervisor were assigned. Before the data collection began, the data collector informed the study participants about the study's purpose, their right to participate or not participate in the study, and that there would be no harm to them, but that no reward could be given in exchange for their participation.
Then, after obtaining signed informed consent, MMT was performed in the corridor by a qualified anesthetist while the patients changed their clothes. The data collector questioned the anesthetist on the table which structure of the larynx was examined by providing a diagrammatic representation of the larynx during direct laryngoscopy. The supervisor kept an eye on the data gathering process and the accuracy of each patient's information. Pre-testing of the data collecting tool (the questionnaire) was performed on 14 patients who were not included in the main trial and no changes to the questionnaire were required. For analysis, incomplete data was not added into the database. Before analyzing the data, it was cleaned up and cross-checked.
4. Data quality control
4.1. Data collectors were trained by principal investigator
For data collecting, trained data collectors and a supervisor were assigned. Data was collected in selected study participants from February to April 2021 using a pretested questionnaire. All materials used for data collection were organized sequentially, and data was stored in a safe and secure location.
4.2. Data analysis and interpretation
SPSS version 24 was used to check, code, enter, and analyze data. Frequency, mean, and standard deviation were used to analyze and express demographic data. Cross tabulation and the spearman correlation coefficient were used to show the correlation between MMC and CLG. For MMC and CLG, a ROC curve analysis was performed. Projected essay laryngoscopy and intubation (MMC I and II), and predicted difficult laryngoscopy and intubation (MMC III and IV) and sensitivity and specificity, positive and negative predictive, positive and negative likelihood were all calculated using a two-by-two table. Cross tabulation was used to calculate MMC's ration and accuracy value. The p-value is used to calculate the area under the curve.
5. Results
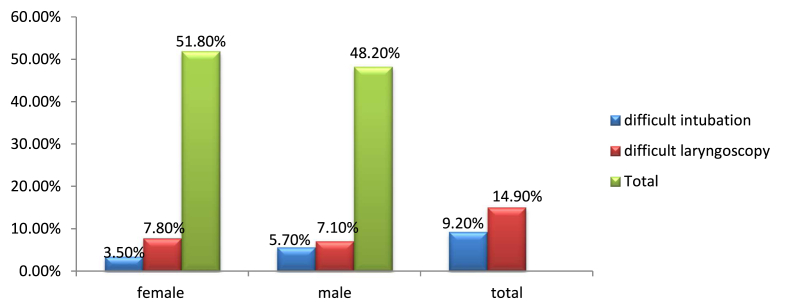
A total of 141 study participants were included in this investigation, all of them met the inclusion criteria and volunteered by giving their consent. Frequency, percentage, mean, and standard deviation were used to express their sociodemographic data. The majority of those who took part in the study were women (51.8%). The study participants' average age was 39.50 (±12.03) years, with a minimum of 18 and a maximum of 63 years. The average BMI was 22.68(±3.00), with a low of 16.50 and a high of 29.38. (Table 1).
Table 1.
Sociodemographic data of the study participants.
| Male | Female | Total | |
|---|---|---|---|
| N (f (%)) | 68 (48.2%) | 73 (51.8%) | 141(100%) |
| Age (mean SD) | 40.46 12.59 | 38.62 ± 11.50 | 39.50 ± 12.03 |
| Weight (mean SD) | 61.00 8.78 | 58.55 ± 8.45 | 59.73 ± 8.67 |
| Height (mean SD) | 1.65 0.096 | 1.59 ± 0.10 | 1.62 ± .11 |
| BMI (mean ± SD) | 22.26 2.34 | 23.06 ± 3.48 | 22.68 ± 3.00 |
SD = standard deviation, f = frequency, Age = age of the patient in years, weight = weight of the patient in kg, Height = height of the patient in meter, BMI = body mass index of the patient.
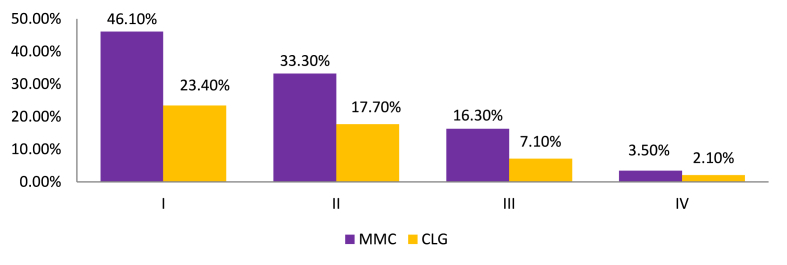
The majority of our study participants were in general surgery and urology, accounting for 96 (68.1%), while the least one was in plastic surgery, accounting for 3% (2.1%). MMT was done on each trial participant prior to induction to predict difficult laryngoscopy and intubation. The bulk of the 141 study participants had modified Mallampati class I, accounting for 65 (46.1%) of the total (Table 2). Cormack and Lehane laryngoscopic grade was assessed after induction during direct laryngoscopy. Grade I Cormack and Lehane received the highest score out of all the other grades (Table 2).
Table 2.
Frequency and percentage of Modified Mallampati classes and Cormack and Lehane Grades.
| Grade or class | MMC | CLG |
|---|---|---|
| 0 | 1(0.7%) | Not applied |
| I | 65(46.1%) | 62(44.0%) |
| II | 47(33.3%) | 57(40.4%) |
| III | 23(16.3%) | 17(12.1%) |
| IV | 5(3.5%) | 5(3.5%) |
| Total | 141(100.0%) | 141(100.0%) |
MMC = modified Mallampati class, CLG= Cormack and Lehane Grade.
For 141 study participants, the match between Modified Mallampati classes and Cormack and Lehane grades was assessed (see Fig. 2). Cormack and Lehane grade I were partnered with modified Mallampati class 0. Approximately half of the 46.10% MMC I were classified as CLG I, while the remaining 22.7% were classified as CLG II and III. CLG IV was assigned to more than half of MMC IV (2.1% out of 3.5%) (Table 3 and Fig. 3).
Fig. 2.
Study participant selection procedure.
Table 3.
Comparison of modified Mallampati classes to cormack and lehane grades.
| Cormack And Lehane Grades |
Total | |||||
|---|---|---|---|---|---|---|
| grade I | grade II | grade III | grade IV | |||
| Modified Mallampati Classes | class 0 | 1(0.7%) | 0(0.0%) | 0(0.0%) | 0(0.0%) | 1(0.7%) |
| class I | 33(23.4%) | 29(20.6%) | 3(2.1%) | 0(0.0%) | 65(46.1%) | |
| class II | 20(14.2%) | 25(17.7%) | 2(1.4%) | 0(0.0%) | 47(33.3%) | |
| class III | 8(5.7%) | 3(2.1%) | 10(7.1%) | 2(1.4%) | 23(16.3%) | |
| class IV | 0(0.0%) | 0(0.0%) | 2(1.4%) | 3(2.1%) | 5(3.5%) | |
| Total | 62(44.0%) | 57(40.4%) | 17(12.1%) | 5(3.5%) | 141(100.0%) | |
The correlation between modified Mallampati classes and Cormack and Lehane grades were evaluated using spearman correlation coefficient. Spearman correlation coefficient (ρ) was 0.330 with p-value of 0.00 for (2-tailed) and 0.00 for (1-tailed) (Table 4).
Fig. 3.
Modified Mallampati Class (MMC) to Cormack and Lehane Grade (CLG) comparison.
The prevalence of difficult laryngoscopy and difficult intubation was 14.9% and 9.2%, respectively, in our study population with no obvious difficult airway indicator. Males were shown to have a higher rate of difficult intubation than females. In general surgery and urology, the majority of difficult intubation and laryngoscopy cases were found. Intubation was difficult 7.8% of the time, while laryngoscopy was difficult 12.10% of the time (Fig. 4).
Fig. 4.
Distribution of difficult laryngoscopy and intubation among male and female study participants.
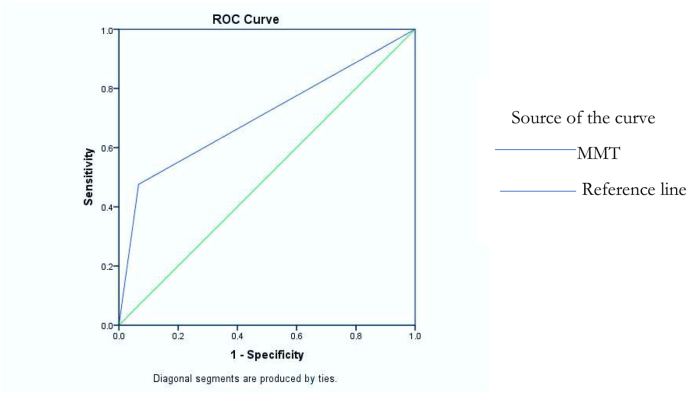
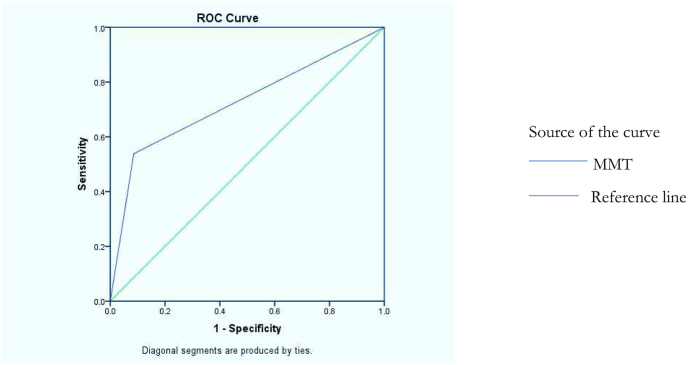
Sensitivity and specificity of modified Mallampati test (MMT) in predicting difficult laryngoscopy were 47.6% and 93.3% respectively, and in predicting and difficult intubation were 53.8% and 91.4% respectively. Positive predictive value, Negative predictive value, Positive likelihood ratio, Negative likelihood ratio and Accuracy were also expressed (Table 5). The area under the curve was also determined using ROC curve for MMT against difficult laryngoscopy and intubation (Fig. 5, Fig. 6).
Table 4.
The correlation between MMC and CLG.
| CLG | ||
|---|---|---|
| MMC | Spearman's rho () Correlation Coefficient | 0.330** |
| p-value (2-tailed) | 0.00 | |
| p-value (1-tailed) | 0.00 | |
**Correlation is significant at the 0.01 level (2-tailed/1-tailed). MMC = modified Mallampati class, CLG = cormack and lehane grade.
Table 5.
Sensitivity, specificity, Positive predictive value, Negative predictive value, Positive likelihood ratio, Negative likelihood ratio, accuracy and area under the curve of modified Mallampati test in predicting difficult laryngoscopy and difficult intubation.
| Sn | Sp | PPV | NPV | PLR | NLR | Accuracy | AUC | P-value | 95% CI | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| MMTa | |||||||||||
| DL | 47.6% | 93.3% | 55.6% | 91.1% | 7.10 | 0.56 | 87.94% | 0.705 | 0.003 | 0.564–0.845 | |
| DI | 53.8% | 91.4% | 38.9% | 95.1% | 6.26 | 0.51 | 86.52% | 0.726 | 0.007 | 0.555–0.897 | |
Modified Mallampati test,DL = difficult laryngoscopy, DI = difficult intubation, Sn = sensitivity, Sp = specificity, PPV = positive predictive value, NPV = negative predictive value, PLR = positive likelihood ratio, NLR = negative likelihood ratio, AUC = area under the curve, CI = confidence interval.
Fig. 5.
Distribution of difficult laryngoscopy and intubation among different specialty of surgery.
Fig. 6.
Receiver operating curve for modified Mallampati test against difficult laryngoscopy in the study population.
With our MMT, 18 trial subjects were diagnosed with difficult laryngoscopy, while 11 were misdiagnosed as having easy laryngoscopy. However, ten of the participants with difficult laryngoscopy were accurately identified. With the modified Mallampati test, 18 research participants were misdiagnosed as having difficult intubation and 6 study participants were misdiagnosed as having easy intubation. Only 7 difficult intubations were accurately identified/projected out of 18 predicted difficult intubations (Table 6).
Table 6.
Distribution of true positive, true negative, false negative and false positive in both difficult intubation and difficult laryngoscopy.
| DL(N = 141) | DI(N = 141) | |
|---|---|---|
| TP | 10 | 7 |
| TN | 112 | 117 |
| FP | 8 | 11 |
| FN | 11 | 6 |
TP = true positive, TN = true negative, FN = false negative, FP = false positive, DL = difficult laryngoscopy, DI = difficult intubation.
6. Discussion
In our study participant the correlation between modified Mallampati class and Cormack and Lehane grade was low. Sensitivity and positive predictive value was also low.
The incidence of MMC class 0, part of epiglottis is visible while conducting MMT, in our study participants was 0.7% whereas Prakash S. et al. determined it as 1.7% [6]. Our result of MMC 0 corresponded with Cormack and Lehane Grade I, and according to Ezri T et al. (2001), MMC class zero, the incidence was 1.18%, had a grade I laryngoscopy [19]. Variation in the incidence could be linked to sample size and demographic variation.
MMC I was found in 46.1% (65) of our research subjects who had no obvious difficult airway sign. Only 23.4% (33) of the participants had CLG I and 2.1% (CLG III) had difficult laryngoscopy. MMC II was found in 33.3% of the research participants. CLG II was found in 17.7% of these people, and difficult laryngoscopy was found in 1.4% of them. MMC III was found in 16.3% of research participants, while CLG III was found in 7.1%. A total of 8.5% of MMC III patients reported a difficult laryngoscopy. The remaining 7.8% had no difficult laryngoscopy. 3.5% of the study participants had MMC IV. From these, 2.1% had CLG IV. In our study participants, all MMC IV patients had difficult laryngoscopy and intubation. In the cross section study conducted by Ezri T. et al. (2001), MMC I was associated with 3.2% difficult laryngoscopy (CLG III) [19]. Cross sectional study conducted by Murugesan K. et al. (2018) showed that 1.351% difficult laryngoscopy was found from MMC I. From MMC II, only 25.71% had Cormack Lehane grade II and 4.285% had difficult laryngoscopy [4]. From this we can say that class to grade relationship varies from population to population and predicted easy laryngoscopy and intubation may become difficult.
The correlation between MMC and CLG in our study participants was observed using spearman's rank correlation coefficient. The spearman's correlation coefficient was found to be 0.330 with p-value of 0.00 for (2-tailed) and 0.00 for (1-tailed) which was statistically significant. But the strength of relation is still low. And this is in line with the result expressed by Nassir KK.et al. (2011) with spearman's correlation coefficient (p) of 0.335 [5]. But in prospective cross sectional study conducted in 29 Indian population by Sanyal R. et al. (2018) [10], the Spearman correlation coefficient between Mallampati and Cormack & Lehane classification was higher with the magnitude of 0.8. This difference might be due difference in the characteristics of our study participants.
In our study population who had no apparent difficult airway indicator, the prevalence of difficult laryngoscope and difficult intubation were 14.9% and 9.2% respectively. This difficult laryngoscopy result is in line with the result determined by Tamrie T. et al. [18], Sanyal R. et al. [10] which were 13.6% and 14% respectively. But the prevalence of difficult intubation was higher compared with the result determined through cross sectional study conducted by Tamrie T. et al. [18], and KOH L.D.K. et al. [19] (9.2% Vs 5% and 6.9% respectively). This discrepancy might be aroused from difference in patient characteristics, individual skill and availability of different airway equipment. The prevalence of difficult laryngoscopy in our study was higher compared with the result determined by Butler P. J. and Dhara S. S. (1992) (14% Vs 8.2%) [20]. And this is may be due to variation in patient characteristics.
In the study area, the only practiced preoperative test in predicting difficult airway was MMT and its sensitivity in predicting difficult laryngoscopy and intubation in the study participants who had no apparent difficult airway indicator was low with the magnitude of 47.6% and 53.8% respectively. The Sensitivity determined by sanyal R. et al. [10], KOH L. K. D. et al. [7] and Selvi O. et al. [2] were similar with our result with the magnitudes of 42.86%, 45% and 43.24% respectively. Nasir KK. et al. [5] also found low sensitivity which was 25.52%. On the other hand, in the cross sectional study conducted by Khatiwada S. et al. (2017) [19], highest sensitivity in predicting difficult laryngoscopy was reported with the magnitude of 83%(8). This discrepancy may be related to variation in patient characteristics and assessment technique.
Specificity of MMT for difficult laryngoscopy and intubation in our study participants was higher, which was 93.3% and 91.4% respectively. Similarly, KOH L.D.K. et al. [19], and Selvi O. et al. [2] pointed out that specificity of MMT for difficult laryngoscopy was 92% and 95.65% respectively. Positive predictive value was 55.6% for difficult laryngoscopy and 38.9% for difficult intubation. Positive predictive value for difficult laryngoscopy determine by Butler P. J. and Dhara S. S. (1992) [20] was 21%.
Negative predictive value, Positive likelihood ratio, Negative likelihood ratio and Accuracy of modified Mallampati test (MMT) in our study participants was found to be 91.1%, 7.10, 0.56 and 87.94% respectively for difficult laryngoscopy and 95.1%, 6.26, 0.51 and 86.52% respectively for difficult in The area under the curve (AUC) was determined using ROC curve analysis for MMT against difficult laryngoscopy and difficult intubation. The AUC against difficult laryngoscopy was found to be 0.705 which is acceptable discrimination and statistically significant (p-value = 0.003; 95% CI = 0.564 & 0.845) and against difficult intubation was found to be 0.726. It is acceptable discrimination and statistically significant (p-value = 0.007; 95% CI = 0.555 & 0.897). This is similar with AUC determined by Tamrie T. et al. [18] which was 0.746 for difficult intubation and 0.731 for difficult laryngoscopy.
On the other hand, the AUC determined by Selvi O. et al. was 0.694 (95% CI = 0.650 & 0.737) [2] which was indicator of poor discrimination compared to our result.
6.1. Limitation of study
-
●
Limitation of the study is that in this study we don't address CLG 2a and 2b about their contribution for difficult intubation. The presence of covid-19 pandemic affects the available number of our study participants.
6.2. Strength of study
-
•
Participants were homogenous (i.e. participants have similar or identical traits). The strength of this study is that all patients who fulfilled inclusion criteria in the study period were included in the study.
-
•
Anesthetists who handle airway in our study participants had a minimum of one year experience and this reduce experience related difficulties.
7. Conclusion and recommendations
7.1. Conclusion
In conclusion, this study found that there was little link between MMC and CLG in Werabie comprehensive specialized hospital. The sensitivity of MMT was also low. The sensitivity and positive predictive value of MMT was low. And relying only on MMC for those who have no apparent difficult airway indicator will lead to unanticipated difficulties and inadequate preparation.
7.2. Recommendation
Difficult airway causes morbidity and mortality in our surgical patients if we do not identify and manage it timely. Therefore, every anesthetist should add other assessment tool in addition to MMT during their preanesthetic evaluation.
Always anesthetists should make themselves ready for any difficulties at any time with skill and equipment even if MMC class I & II. Different difficult airway management equipment should be available in the OR in difficult airway cart.
Training should be given for anesthetists about additional airway assessment tool and their application.
Consent for publications
Not applicable.
Provenance and peer review
Not commissioned, externally peer reviewed.
Availability of data and materials
Data and materials will be shared upon reasonable request.
Ethical clearance
Ethical clearance was obtained from the ethical clearance committee of Addis Ababa University, department of anesthesia and permission was obtained from Werabie comprehensive specialized hospital before the start of the study.
Ethical approval
Ethical clearance was obtained from Health science college, Addis Ababa University ethical clearance committee.
Reference number for Ethical approval: No 14/2021.
Please state any sources of funding for your research
Funded by Addis Ababa University.
Author contribution
-
1.
Desalegn Yemam: as a team member He developed the proposal, trained the data collectors, analysed the data & wrote the result and interpreted the result.
-
2.
Zewetir Ashebir: as a team member He developed the proposal, trained the data collectors, analysed the data & wrote the result and interpreted the result and corresponding Author
-
3.
Eyayalem Melese: as a team member He developed the proposal, trained the data collectors, analysed the data & wrote the result and interpreted the result, over all he leads the research team
Registration of research studies
-
1.
Name of the registry: Research Registration
-
2.
Unique Identifying number or registration ID: 7689
-
3.
Hyper link: https://www.researchregistry.com/browse-the-registry#home
Guarantor
We will take responsibility for the research work. We participated in the study's conduct, have access to the data, and made the conscious decision to publish.
-
1.
Mr ZEWETIR ASHEBIR
Senior Anesthetist, Lecturer, Department of Anesthesia, School of Medicine, College Of Health Sciences, Addis Ababa University Email: zewetir76@gmail.com zewetir.asheber@aau.edu.et: Tele. +251911317055.
-
2.
MR EYAYALEM MELESE GOSHU
Senior Anesthetist, Assistant Professor, Department of Anesthesia, School of Medicine.
College Of Health Sciences, Addis Ababa University Email: eyayalem.melese@aau.edu.et/eyayalem@yahoo.com: Tele.+251913002201.
Consent
During the conduct of this research, all research requirements were met. The first element of the questioner was written consent. We got signed consent from all participants in this study. and it is also included in the text.
Declaration of competing interest
The authors declare that there is no conflict of interests.
Acknowledgement
We would like to convey our heartfelt gratitude to the administrators and staff coordinators of Werabe Comprehensive Specialized Hospital, as well as Addis Ababa University, for providing us with an ethical clearance, research fund, internet, and library service.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2022.103912.
List of Abbreviations
- MMC
Modified Mallampati Classification
- MMT
Modified Mallampati Test
- CLG
Coramack and Lehane Grading
- C-Lg
Cormack and Lehane Gradig
- MP
Mallampati
- MM
Modified Mallampati
- CL
Cormack and Lehane
- ASA
American Society of Anesthesiologist
- ETT
Endotracheal Tube
- BMI
Body Mass Index
- EGD
Extraglotic Device
- DI
Difficult Intubation
- BMV
Bag and Mask Ventilation
- AUC
Area under the Curve
- ROC
Receiver Operating Curve
- AAU
Addis Ababa University
- DL
Difficult Laryngoscopy
- WCSH
Werabie Comprehensive Specialized Hospital
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Hester C.E., Dietrich S.A., White S.W., Secrest J.A., Lindgren K.R., Smith T. A comparison of preoperative airway assessment techniques: the modified Mallampati and the upper lip bite test. AANA J. (Am. Assoc. Nurse Anesth.) 2007;75(3):177–182. [PubMed] [Google Scholar]
- 2.Selvi O., Kahraman T., Senturk O., Tulgar S., Serifsoy E., Ozer Z. Evaluation of the reliability of preoperative descriptive airway assessment tests in prediction of the Cormack-Lehane score: a prospective randomized clinical study. J. Clin. Anesth. 2017;36:21–26. doi: 10.1016/j.jclinane.2016.08.006. [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 3.Wajekar A., Chellam S., Toal P. Prediction of ease of laryngoscopy and intubation-role of upper lip bite test, modified Mallampati classification, and thyromental distance in various combinations. J. Fam. Med. Prim. Care. 2015;4(1):101. doi: 10.4103/2249-4863.152264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murugesan K., Arunachalam R., Rajarajan N. Correlative study between modified Mallampati score with Cormack Lehane and POGO scoring. Int. Arch. Integr. Med. 2018;5(4):119–125. [Google Scholar]
- 5.Nasir K.K., Shahani A.S., Maqbool M.S. Correlative value of airway assessment by Mallampati classification and Cormack and Lehane grading. Rawal Med. J. 2011;36(1):2–6. [Google Scholar]
- 6.Prakash S., Kumar A., Bhandari S., Mullick P., Singh R., Gogia A.R. Difficult laryngoscopy and intubation in the Indian population: an assessment of anatomical and clinical risk factors. Indian J. Anaesth. 2013;57(6):569–575. doi: 10.4103/0019-5049.123329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Koh L.K.D., Kong C.F., Ip-Yam P.C. The modified Cormack-Lehane score for the grading of direct laryngoscopy: evaluation in the Asian population. Anaesth. Intensive Care. 2002;30(1):48–51. doi: 10.1177/0310057X0203000109. [DOI] [PubMed] [Google Scholar]
- 8.Khatiwada S., Bhattarai B., Pokharel K., Acharya R. Prediction of difficult airway among patients requiring endotracheal intubation in a tertiary care hospital in eastern Nepal. J. Nepal Med. Assoc. JNMA. 2017;56(207):314–318. [PubMed] [Google Scholar]
- 9.Roth D., Nl P., Lee A., Hovhannisyan K., Am W., Arrich J., et al. 2018. Airway Physical Examination Tests for Detection of Difficult Airway Management in Apparently Normal Adult Patients (Review) 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sanyal R., Ray S., Chakraverty P., Bhattacharya M.K. Comparision of airway assessment by Mallampati classification and cormack and lehane grading in Indian population. Indian J. Clin. Anaesth. 2019;6(1):140–142. [Google Scholar]
- 11.Ron M., Walls M.F.M. In: Manual of emergency airway management fourth. fourth ed. DeStefano F., editor. Lippincott Williams & Wilkins, a Wolters Kluwer business; Philadelphia: 2012. p. 10. [Google Scholar]
- 12.Us R., Shetty S.R., G U., Venkateswaran R., Ks Y., S R., et al. 2007. Workshop on Difficult Airway Management. [Google Scholar]
- 13.Ouchi K., Hosokawa R., Yamanaka H., Nakajima Y., Nakamura Y., Kishimoto J. Mallampati test with phonation, tongue protrusion and supine position is most correlated with Cormack–Lehane test. Odontology. 2020;108(4):617–625. doi: 10.1007/s10266-020-00490-3. [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 14.Sharma D., Prabhakar H., Bithal P.K., Ali Z., Singh G.P., Rath G.P., et al. Predicting difficult laryngoscopy in acromegaly: a comparison of upper lip bite test with modified Mallampati classification. J. Neurosurg. Anesthesiol. 2010;22(2):138–143. doi: 10.1097/ANA.0b013e3181ce6a60. [DOI] [PubMed] [Google Scholar]
- 15.Jack Meitei A., Kumar Behera K., Anita Devi N., Sarat Singh S., Eshori Devi L., Ratan Singh N., et al. A comparative study of the modified Mallampati classification with the ratio of patient's height to thyromental distance and upper lip bite test in predicting difficult laryngoscopy. IOSR J. Dent Med. Sci. e-ISSN. 2018;17(4):66–71. [Internet] (Available from: www.iosrjournals.org) [Google Scholar]
- 16.Orebaugh S.L., Bigeleisen P.E. In: Atlas of Airway Management. second ed. Brown B., editor. LIPPINCOTT WILLIAMS & WILKINS, a WOLTERS KLUWER busines; Philadelphia: 2012. [Google Scholar]
- 17.Adamus M., Fritscherova S., Hrabalek L., Gabrhelik T., Zapletalova J., Janout V. Mallampati test as a predictor of laryngoscopic view. Biomed. Pap. 2010;154(4):339–344. doi: 10.5507/bp.2010.051. [DOI] [PubMed] [Google Scholar]
- 18.Tamire T., Demelash H., Admasu W. Predictive values of preoperative tests for difficult laryngoscopy and intubation in adult patients at tikur Anbessa specialized hospital. Anesthesiology Res. Pract. 2019;2019 doi: 10.1155/2019/1790413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ezri T., Warters R.D., Szmuk P., Saad-Eddin H., Geva D., Katz J., et al. The incidence of class “zero” airway and the impact of Mallampati score, age, sex, and body mass index on prediction of laryngoscopy grade. Anesth. Analg. 2001;93(4):1073–1075. doi: 10.1097/00000539-200110000-00055. [DOI] [PubMed] [Google Scholar]
- 20.Butler P.J., Dhara S.S. Prediction of difficult laryngoscopy: an assessment of the thyromental distance and Mallampati predictive tests. Anaesth. Intensive Care. 1992;20(2):139–142. doi: 10.1177/0310057X9202000202. [DOI] [PubMed] [Google Scholar]
- 21.Mathew G., Agha R., for the Strocss Group Strocss 2021: strengthening the Reporting of cohort, cross-sectional and case-control studies in Surgery. Int. J. Surg. 2021;96 doi: 10.1016/j.ijsu.2021.106165. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data and materials will be shared upon reasonable request.