Abstract
Introduction
and importance: Aortic infective endocarditis is a well described fatal disease that develops along the edges of the heart valves, although it can affect native and prosthetic valves, infection seldom affects a previously normal ones. Aortic root abscess as a complication of normal native aortic valve endocarditis is less recognized and described, it is a potentially fatal condition, which the diagnosis is based on clinical, biology, echocardiography and especially the intraoperative findings. Both native and prosthetic valve infection can be complicated by an aortic abscess, associated with a significant mortality rate, which often requires surgical intervention
Case report
We report here a case of young man, with no major pathological history, non-systemic or valvular predisposing diseases, was admitted for the assessment of a prolonged fever with no obvious cause, and in whom an aortic abscess was suspected on an echocardiography and confirmed by transesophageal echocardiography and histopathology, complicating a negative blood culture infective endocarditis.
Conclusion
Up to date, the incidence of infective endocarditis continues to rise, with a significant rate of mortality and complications, however the physiopathology mechanism remain insufficiently studied.
Keywords: Native, aortic, Abscess, Sepsis
Highlights
-
•
The echocardiographic features play an important role in the diagnosis of aortic abscess, as well as the management of this serious condition.
-
•
Aortic root abscess complicating a normal native aortic valve endocarditis is rare and not well described.
-
•
The effective approach for patients with IE periannular extension involves a multidisciplinary approach, with surgical treatment playing a major role.
1. Introduction
In recent years, the epidemiology of endocarditis has changed considerably, it was previously only seen in younger rheumatic valve disease patients, as the incidence of rheumatic fever diminishes in developed countries, it is becoming more prevalent among the elderly and people who have prosthetic heart valves or cardiovascular implanted devices [1]. The incidence of infective endocarditis is estimated to be around 3–10 episodes per 100000 person years [1], staphylococcus aureus is the most incriminated microorganism, meanwhile the incidence, the risk factors and clinical characteristics of endocarditis in patients with no underlying heart disease remains undetermined and reported in only in few reports.
Besides, abscess of the aortic root is a recognized consequence of endocarditis, patients who have had aortic root surgery and/or aortic valve replacement are more likely to develop this condition with a rate of 10–37% of people [2], it necessitates firstly an accurate diagnosis based on transesophageal echocardiography most preferred imaging technique [3], and secondly a well-thought-out management strategy and prompt intervention [4]. It's a dangerous illness that comes with a slew of complications and a substantially greater death and morbidity rate.
The occurrence of aortic root abscess on native normal aortic valve endocarditis, on the other hand, is uncommon, with limited data.
Our case report was written according to CARE guidelines [5].
2. Case presentation
A 51 year-old man, not known smoker or intravenous drug user, with no previous medical issues, no history of recent surgery, no recent dental procedures, presented to the cardiology unit with a two-week history of recurrent fever (38.5–39.5 °C). He was thoroughly evaluated in various hospitals, with negative test, and therefore the diagnosis of undetermined sepsis was retained.
On presentation he was apyretic, his sitting arterial pressure: 110/65 mmhg, his heart beat: 85 bpm, respiratory rate: 145 cpm, Sa O2 97%, capillary glycemia: 1 g/l, the cardiovascular examination detected a diastolic murmur classified 4/6th on the right sternal edge, without heart failure sign.
His EKJ showed sinus rhythm without conduction abnormalities, dilated left ventricule on transthoracic echocardiography, with normal wall motion, and ejection fraction 50%, Thin, trileaflet aortic valve with a suspicious hyperechoic image at the non-coronary cusp, responsible for an eccentric aortic regurgitation, the mitral, tricuspid and pulmonary valves were visualized on all sections, with no suspicious images of infective endocarditis, a transesophageal echocardiogram (video) was performed confirming what we found on echocardiography. Moreover an aortic abscess was find behind the non-coronary cusp (Fig. 1, Fig. 2) measuring (7*17mm) perforating this latter and causing a significant aortic regurgitation (Fig. 3). There weren't obvious signs of an inflammatory response, the white blood cell count of 12000/mm3 and C reactive protein (CRP) of 23 g/l, ferritin level of 123 g/l and inflammatory anemia at 8.9 g/dl,the renal function and the immunological tests were normal as showed in Table 1,there was no evidence of a pathogen entry point, blood cultures were reported negative, they were no signs of embolism complication on the scan, therefore note that the patient does not have an immunodepression or autoimmune disease profile, finally there were not enough criteria to make a diagnosis of definite endocarditis according to the modified Duke criteria.
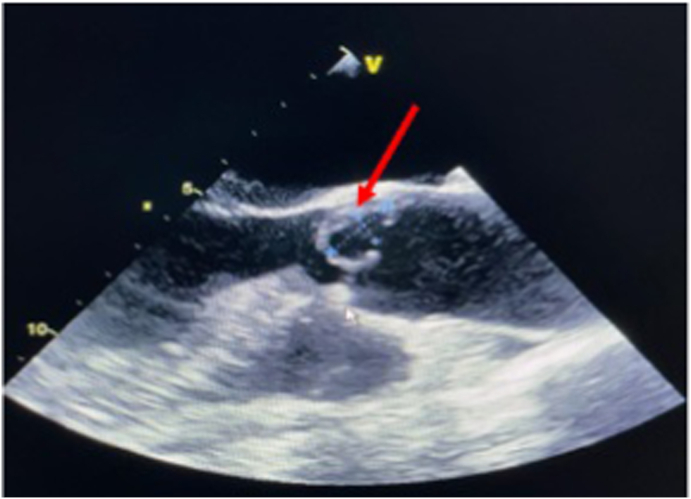
Fig. 1.
Midesophageal-aortic valve short-axis view showing aortic root abscess (arrowheads) in relation to noncoronary cusp.
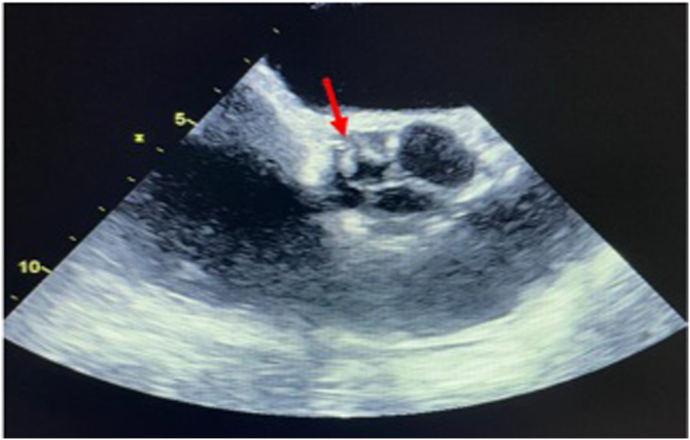
Fig. 2.
Midesophageal-aortic valve short-axis view showing a heterogeneous hyperechoic lesions with perivalvular thickening.
Fig. 3.
Midesophageal-LV long-axis view showing a severe aortic regurgitation.
Table 1.
Blood test results.
| Admission | Discharge | Normal range | |
|---|---|---|---|
| White Blood cell | 12000 | 10000 | 4000-10000/ul |
| Hemoglobin level | 8.4 | 10 | 13–17 g/dl |
| Paletet count | 221000 | 241000 | 150000-400000/ul |
| CRP | 23 | 12 | 0–5mg/l |
| Ferritin | 123 | 100–200 mg/l | |
| Creatinine | 7.6 | 8.00 | 6–12mg/l |
| Procalcitonin | 1.5 | 0.6 | <0.5 g/l |
| Rheumatoid factor | 72 | – | 20ui/l |
| TP | 83 | 90 | 70–100% |
| INR | 1,1 | 0.99 | |
| ASAT | 26 | – | 5-34 ui/l |
| ALAT | 11 | – | 0-55 ui/l |
| Blood cultures | negatives |
The patient was referred for emergency surgery, the abscess was debrided, and the aortic valve was replaced. Fibrinoid necrosis and exudates with acute inflammatory cells around colonies of coagulase-negative staphylococcus were seen on histopathology of explanted aortic valve tissue, confirming the diagnosis of aortic abscess. The patient completed 6 weeks of six weeks of antibiotic therapy with vancomycin and aminoglycosides stopped at day 15.
Our patient made a complete recovery after antibiotics and successful surgery care.
3. Discussion
The pathophysiology of infective endocarditis involves complex interactions between circulating microorganisms, the injured valvular endothelium, and the host's immune defenses. The epidemiology of infective endocarditis has been subjected to important modifications during the last decades, it affects more often older, prosthetic devices and pacemaker leads implantation [6].
Infective endocarditis without previously known predisposing heart disease was reported in few cases, however its physiopathologic mechanism remain poorly studied. Reviewing the literature reports, we find that elderly age patients, diabetes mellitus and severe renal damages are the most risk factors seen in patients with endocarditis with no previously detected heart disease. Furthermore, we note a dominance of the aortic site and Staphylococcal was the most common etiologic agent [[7], [8], [9], [10]].
According to a Korean study carried out by Byung Joo Sun and al [7], between March 1, 2000 and December 31, 2009, among 249 patients with no previous medical history of underlying heart disease when hospitalized for infective endocarditis, only 64 patients had developed vegetation in structurally normal valve, while 185 had clinically silent valvular or congenital heart disease, higher age (>60 years old), higher rate of diabetes higher euroscore (European System for Cardiac Operative Risk Evaluation) and severe renal failure were associated with infective endocarditis involving normal valves. Viridans streptococci and staphylococcal agent were the most incriminating etiological agents found, affecting the aortic and tricuspid valves the most. The sources of the infection were diverse including firstly Community-acquired and secondly Health care–associated and non-nosocomial health care–associated, moreover, the mortality rate was higher in the infective endocarditis involving structurally normal valves.
Other cases of staphylococcus epidermis endocarditis with normal valve disease were reported in a 50-year-old lady on steroid therapy for chronic liver disease [8], a 71-year-old male with no underlying chronic illness [9], and a 32 year old male who underwent vasectomy recently [10], in the both first cases, the host's defenses were likely insufficient (Steroids, chronic liver disease, and old age), as for the young men, the vasectomy was incriminated. A poor dental status, hemodialysis, central venous catheters and an immunocompromised status were found in the other reported cases.
None of the factors listed above had our patient, he is an immunocompetent host, does not use intravenous or immunosuppressive drugs, no history of recent surgery, in addition he doesn't showed evidence of pre-existing valvular damage at surgery which make our case unique.
So we suppose that the potential invasiveness of coagulase-negative staphylococcus bacteria is more likely to be the main predisposing factor. This bacteria that should not be considered as normal human flora or contaminants as reported in these researches [[11], [12], [13]].
Aside from, our patient present an aortic root abscess which is a complication of infective endocarditis that affects 10–37% of people [2], more likely in patients with a prosthetic valve endocarditis comparing to those with native endocarditis. Although advances have improved the diagnostic accuracy for the valve disease, morbidity and mortality remain remarkably high.
In this deadly condition, there is a limited research available concerning the prevalence and the risk factors of occurrence, but according to a study conducted by the International Collaboration on Endocarditis Merged Database, 69 cases out of 311 with aortic endocarditis developed a periannular abscess who had definite aortic valve endocarditis [14], this rate increases in patients with a prosthesis [15].
In another a cross-sectional comparative study between two groups of 285 patients with definite infective endocarditis classified in two groups according the presence of an aortic root abscess carried out by Kareem Mahmoud et al. [16], the aortic abscess was present in 61 patients (21.4%), moreover, mechanical prosthesis, bicuspid aortic valve, prior infective endocarditis, aortic paravalvular leak, aortic valve vegetations were all considerably greater in aortic root abscess patients. None of these were present in our patient.
In a retrospective review of 16 referral hospitals from 1992 to 2003, Anguera et al. found aortic root abscess in 201 patients out of 2055 native aortic valve IE (9.8%) [17], and in the same issue, Anguera et al. found aortic abscess in 150 patients (17%) out of over 872 prosthetic aortic valve IE in the same registry.
Once aortic abscesses discovered, immediate surgery is essential since antibiotics alone will not be able to control the infection, and surgery is the only way to cure the infection. In a study carried out by Kang DH and al [18], we note that early surgery in patients with infective endocarditis and extensive vegetations greatly reduced systemic embolism and death when compared to conventional treatment.Extensive debridement of all infected and devitalized tissue, the closure of the defect with a patch and aortic valve replacement are common surgical treatments [19].
Given the absence of any factor predisposing to infective endocarditis in our patient, we incriminate the virulence of the germ and therefore this study also illustrates the invasive potential of so-called low-virulence coagulase negative staphylococci, emphasizing the necessity of not presuming that an isolate of these organisms from blood samples signifies skin contamination.
4. Conclusion
Through this case, we aim to highlight an unusual case of aortic root abscess presenting as a complication of a completely normal native aortic valve endocarditis in an immunocompetent young patient without risk factors. To avoid a huge spectrum of systemic complications, early identification and treatment are crucial.
A large proportion of patients with infective endocarditis have no previous history of predisposing heart disease, but they have been inappropriately neglected although the higher mortality and complications rate, so more further investigations are needed to improve the management and clinical outcomes of these patients.
Ethical approval
The ethical committee approval was not required give the article type (case report).However, the written consent to publish the clinical data of the patients was given and is available to check by the handling editor if needed.
Sources of funding
None.
Author contributions
Oumayma Hattab: Study concept, Data collection, Data analysis, Literature research, writing the paper, Benbouchta Karima: Data collection, Data analysis, Amaqdouf Saida: Data collection, Data analysis, Noha El ouafi:Supervision and data validation., Bazid Zakaria: Supervision and data validation.
Trial registry number
This is not an original research project involving human participants in an interventional or an observational study but a case report. This registration is was not required.
Guarantor
Oumayma Hattab.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
None.
Acknowledgments
I would like to express my very great appreciation to my superiors, staff, patient and his family.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.amsu.2022.104004.
Contributor Information
Oumayma Hattab, Email: Hattaboumayma0@gmail.com.
Karima Benbouchta, Email: Karimabenbouchta3971@gmail.com.
Saida Amaqdouf, Email: saida.amaqdouf0@gmail.com.
Noha El ouafi, Email: Pr.elouafi@gmail.com.
Zakaria Bazid, Email: bazidzakaria@gmail.com.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Arora Y.K. Infective endocarditis: an overview. J Cardiol Curr Res. 2018;11(6):281–283. doi: 10.15406/jccr.2018.11.00416. ([PubMed] [Google Scholar]) [DOI] [Google Scholar]
- 2.Weerakkody, Y., Kang, O. Aortic Root Abscess. Reference article, Radiopaedia.org. (Accessed on 05 Mar 2022) https://doi.org/10.53347/rID-60212[PubMed] [Google Scholar].
- 3.Jin X.Y., Yacoub M.H. Anatomical definition of aortic root abscesses by transesophageal echocardiography: planning a surgical strategy using homograft valves. Brecker S.J., editor. Clin. Cardiol. 1995;18:353–359. doi: 10.1002/clc.4960180612. [PubMed] [Google Scholar] [DOI] [PubMed] [Google Scholar]
- 4.Prognostic implications of left ventricular hypertrophy. Vakili BA, Okin PM, Devereux RB. Am. Heart J. 2001;141:334–341. doi: 10.1067/mhj.2001.113218. [PubMed] [Google Scholar] [DOI] [PubMed] [Google Scholar]
- 5.Ds R., et al. CARE guidelines for case reports: explanation and elaboration document. J. Clin. Epidemiol. Sep. 2017;89:218–235. doi: 10.1016/J.JCLINEPI.2017.04.026. [PubMed] [CrossRef] [Google Scholar] [DOI] [PubMed] [Google Scholar]
- 6.Tirumala N.A., Rajasekhar D., Vanajakshamma V., Sreedhar N. A review: garlic effects on the cardiovascular System. J. Cardiol. & Cardiovasc. Ther. 2017;5(2) doi: 10.19080/JOCCT.2017.05.555659. ([PubMed] [Google Scholar]) [DOI] [Google Scholar]
- 7.Sun B.J., Choi S.-W., Park K.-H., Jang J.Y., Kim D.-H., Song J.-M.…Song J.-K. Infective endocarditis involving apparently structurally normal valves in patients without previously recognized predisposing heart disease. J. Am. Coll. Cardiol. 2015;65(3):307–309. doi: 10.1016/j.jacc.2014.10.046. [PubMed] [Google Scholar] [DOI] [PubMed] [Google Scholar]
- 8.Bernadet P., Auvergnat J.C., Donzeau J.P., et al. Endocardites bactériennes A Staphylococcus epidermidis. Deux observations. Nouv. Presse Med. 1979;8:167.1–1673 13. ([PubMed] [Google Scholar]) [PubMed] [Google Scholar]
- 9.Laine J.L., Morand P., Potier N., et al. Endocardite bactérienne de l'orifice pulmonaire sans atteinte tricuspidienne. Sem. Hop. Paris. 1972;48:565–570. [PubMed] [Google Scholar] [PubMed] [Google Scholar]
- 10.Dan M., Marien G.J., Goldsand G. Endocarditis caused by Staphylococcus warneri on a normal aortic valve following vasectomy. Can. Med. Assoc. J. 1984 Aug 1;131(3):211–213. ([PubMed] [Google Scholar]) [PMC free article] [PubMed] [Google Scholar]
- 11.Natsis N.E., Cohen P.R. Coagulase-negative Staphylococcus skin and soft tissue infections. Am. J. Clin. Dermatol. 2018;19:671–677. doi: 10.1007/s40257-018-0362-9. ([PubMed] [Google Scholar]) [DOI] [PubMed] [Google Scholar]
- 12.Becker K., Heilmann C., Peters G. Coagulase-negative staphylococci. Clin. Microbiol. Rev. 2014 Oct;27(4):870–926. doi: 10.1128/CMR.00109-13. PMID: 25278577; PMCID: PMC4187637., [PubMed] [Google Scholar] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Noshak M.A., Rezaee M.A., Hasani A., Mirzaii M. The role of the coagulase-negative staphylococci (CoNS) in infective endocarditis; A narrative review from 2000 to 2020. Curr. Pharmaceut. Biotechnol. 2020;21(12):1140–1153. doi: 10.2174/1389201021666200423110359. PMID: 32324510., [PubMed] [Google Scholar] [DOI] [PubMed] [Google Scholar]
- 14.Dillon J.C., Feigenbaum H., Konecke L.L., et al. Echocardiographic manifestations of valvular vegetations. Am. Heart J. 1973;86:698–704(. doi: 10.1016/0002-8703(73)90350-5. [PubMed] [Google Scholar]) [DOI] [PubMed] [Google Scholar]
- 15.Anguera I., Miro J.M., Cabell C.H., et al. Clinical characteristics and outcome of aortic endocarditis with periannular abscess in the international collaboration on endocarditis merged database. Am. J. Cardiol. 2005;96(7):976–981(. doi: 10.1016/j.amjcard.2005.05.056. [PubMed] [Google Scholar]) [DOI] [PubMed] [Google Scholar]
- 16.Mahmoud K., Hammouda T., Kandil H., et al. Prevalence and predictors of aortic root abscess among patients with left-sided infective endocarditis: a cross-sectional comparative study. Egypt. Heart J. 2020;72:62. doi: 10.1186/s43044-020-00098-6. [PubMed] [Google Scholar] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anguera I., Miro J.M., Evangelista A., Cabell C.H., San Roman J.A., Vilacosta I., et al. Periannular complications in infective endocarditis involving native aortic valves. Am. J. Cardiol. 2006;98(9):1254–1260. doi: 10.1016/j.amjcard.2006.06.016. [PubMed] [Google Scholar] [DOI] [PubMed] [Google Scholar]
- 18.Kang D.H., Kim Y.J., Kim S.H., et al. Early surgery versus conventional treatment for infective endocarditis. N. Engl. J. Med. 2012;366(26):2466–2473. doi: 10.1056/NEJMoa1112843. [PubMed] [Google Scholar] [DOI] [PubMed] [Google Scholar]
- 19.Kaan Kirali, Sabit Sarikaya. Yucel ozen: surgery for aortic root abscess: a 15-year experience. Tex. Heart Inst. J. 2016 Feb;43(1):20–28. doi: 10.14503/THIJ-14-4747. Published online 2016 Feb 1, [PubMed] [Google Scholar] [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.