Abstract
Background
Laparoscopic appendectomy is the most performed emergency surgical technique worldwide. Transversus abdominis plane (TAP) blocks, which are easier to achieve with ultrasound, are frequently used in multimodal analgesia techniques for this surgery. Quadratus lumborum (QL) block has become a standard block, first used in gynecological and other abdominal surgeries. This study was planned to compare the analgesic efficacy of ultrasound-guided QL and TAP blocks for postoperative analgesia after laparoscopic appendectomy.
Materials and methods
A total of 136 patients aged 18–65 years who underwent laparoscopic appendectomy were randomized and divided into two groups. A volume of 40 ml of local anesthetic containing 0.375% bupivacaine was administered for block applications in group TAP (n = 68) and group QL (n = 68). In addition, a patient-controlled analgesia device was used to administer bolus tramadol hydrochloride at a dose of 10 mg to relieve pain in the postoperative period. Postoperative opioid consumption of patients was recorded as the primary outcome and pain scores (1, 6, 12, 18, 24 h) as the secondary outcome.
Results
Both groups were statistically similar in demographic and surgical data. There were no statistically significant differences between the groups over 24 h in terms of intraoperative remifentanil consumption (p = 0.584), postoperative cumulative opioid consumption (p = 0.807), and pain scores. No complications were observed in either group related to the block.
Conclusion
Ultrasound-guided lateral approach QL block may provide adequate analgesia efficacy in patients undergoing laparoscopic appendectomy, like TAP block, and may be included in multimodal analgesia in pain control.
Keywords: Quadratus lumborum block, Transversus abdominis plane block, Laparoscopic appendectomy, Postoperative pain
Highlights
-
•
We compared the analgesic efficacy of lateral QL and TAP blocks in laparoscopic appendectomy.
-
•
The lateral approach QL block provided similar pain scores and postoperative opioid consumption to TAP block.
-
•
Lateral approach QL and TAP blocks are effective for pain management following laparoscopic appendectomy.
1. Introduction
Laparoscopic appendectomy is the most frequently performed surgery in patients who develop acute appendicitis [1]. This surgical technique is more advantageous than an open appendectomy in terms of fewer complications, less postoperative pain, and a faster return to normal daily activities [2,3]. Even though the laparoscopic technique is minimally invasive, postoperative pain is inevitable. Furthermore, it may affect the patients' mobility and cause them to stay in the hospital for a more extended period [4]. Presently, since it has been determined that interfacial plane blocks reduce postoperative pain and the need for opioid analgesics, interfacial plane blocks have started to be preferred frequently among multimodal analgesia methods in abdominal surgeries [5,6].
Transversus abdominis plane (TAP) block is a simple procedure in which a local anesthetic solution is injected into the abdominal wall's two muscle layers. Regional analgesia is provided on the anterior abdominal wall's skin, muscle, and parietal peritoneum [7]. It was first described by Rafi [8], that three different TAP block techniques are currently used under ultrasound guidance: subcostal, lateral, and posterior approaches [9]. TAP block is a widely used method for postoperative analgesia in laparoscopic appendectomy [10]; it is easy to administer and has a low risk of developing complications. However, there are concerns that it may provide visceral and long-term analgesia [11].
Quadratus lumborum (QL) block was described by Blanco in 2007 [12] and has subsequently been shown in many randomized controlled studies to provide adequate postoperative analgesia and reduce opioid analgesic use [[13], [14], [15]]. It has been reported that the lateral QL block, also called QL1 block, can provide adequate analgesia from T7 to L1 [16]. Furthermore, the lateral QL block technique can be applied easily and in a short time without the need for a different patient position in short-term surgeries such as appendectomies. A lateral QL block allows simultaneous ultrasound guidance with a linear probe like a TAP block, because it is more superficial, making the procedure easier and safer. However, the use of QL block in laparoscopic appendectomy has not yet become widespread. There are no studies that examine the efficacy of lateral QL block in laparoscopic appendectomy. Therefore, this double-blind, randomized, controlled study aimed to compare the effectiveness of ultrasound-guided TAP and QL blocks for postoperative pain relief in patients undergoing laparoscopic appendectomy surgery.
2. Materials and methods
2.1. Study design
Inclusion criteria were determined as patients aged between 18 and 65 years, who underwent laparoscopic appendectomy, and patients with physical status I-III, according to the American Society of Anesthesiologists (ASA). Patients with ASA physical status IV-V, had an abnormality in their abdominal wall anatomy, known local anesthetic allergy, morbid obesity (BMI >40 kg/m2), opioid, alcohol, and substance abuse, psychiatric disease, need for interpreter, and coagulopathy were excluded from the study. All procedures performed in this study involving human participants were conducted by the Declaration of Helsinki (revised in 2013). The trial was approved by the ethics committee board of a training and research hospital (No.: 2020-02-23/2020–35), and informed consent was obtained from all patients for participation in the study and the procedures to be performed. The study was registered at clinicaltrials.gov (NCT05310266) and the Research Registry (Unique Identifying Number 7984 -Link https://www.researchregistry.com/browse-the-registry#home/). Our study followed the Consolidated Standards of Reporting Trials (CONSORT) guidelines [17].
Sample size calculation was performed before the study. The strength analysis was based on the average postoperative opioid consumption, which was its primary outcome. A pilot study was conducted with 15 patients from each group to determine the minimal sample size. The mean cumulative opioid dose was 57.14 ± 31.16 mg/kg in the Group TAP and 73.39 ± 34.27 mg/kg in the Group QL. An effect size of 0.790 and α error = 0.05 with a power of 80% was assumed so that each group had at least 68 participants. Considering a possible 20% dropout rate, 84 patients were recruited in each group for the study. The G*Power 3.1.9.2 program was used to calculate the sample size of the study.
To avoid selection bias, patients were randomly assigned to one of the QL and TAP groups via a computer-assisted randomization system, conducted by an anesthesia nurse (SK) who was not included in the study before induction of anesthesia. Before surgery, patients were informed about the pain assessment process and trained on using the patient-controlled analgesia (PCA) pump to relieve postoperative pain. An anesthesiologist (YP), who was not included in the study, and had at least five years of experience in this field, performed the block technique determined according to randomization after intubation. The anesthesiologists (GS, GOY), who were study coordinators, patients, surgeons, and anesthesia nurses that had monitored the patients' pain scores and opioid consumption data during the postoperative period, were also unaware of the assigned treatment.
2.2. General anesthesia
Before the surgery, 22-gauge vascular access was established in all patients, and infusion with 2–4 ml/kg/h Ringer lactate solution was started. Standard monitoring was achieved with electrocardiography (ECG), noninvasive blood pressure, and peripheral oxygen saturation (SpO2). After monitoring, 0.03–0.05 mg/kg of midazolam was administered for premedication. During induction, 2 μg/kg fentanyl, 2–3 mg/kg propofol, and 0.6–0.8 mg/kg rocuronium were administered, and the patients were intubated after 2 min of mask ventilation. Anesthesia was maintained by infusion of sevoflurane with a minimum alveolar concentration (MAC) of 0.8–1% and iv remifentanil at a dose of 0.05–0.1 μg/kg/min in 3 L of 40% air + O2 mixture.
During surgery, hypotension (mean arterial pressure <65 mm Hg or 20% decrease from baseline) was treated with a bolus of crystalloid fluid or with an iv bolus of ephedrine 5–10 mg, bradycardia (HR < 45 beats min) with 0.5 mg of atropine iv. At the end of the surgery, anesthesia maintenance was terminated, and patients were decurarized with 0.04 mg/kg neostigmine and 0.01 mg/kg atropine. For the prevention of nausea and vomiting, ondansetron 4 mg was given. After extubation, patients stayed in the recovery room for 15 min. They were followed up and sent to the ward when their modified Aldrete score was ≥9.
2.3. Bilateral TAP and QL blocks
The blocks were performed using ultrasound guidance before the surgical procedure, following the induction of anesthesia. TAP and QL blocks were performed by an anesthesiologist with at least five years of experience in this field. For blocks, 0.375%, 20 ml of bupivacaine was used for each side (40 ml total). Block application was performed using a 100 mm 22-gauge needle (Stimupleks Ultra 360 30° - BRA-04892510-01/B. Braun Melsungen AG, Japan) and a linear multifrequency 12 L probe of the ultrasonography device (Esaote MyLabSeven/Esaote S·P.A, Genoa-Italy) after aseptic conditions were achieved in the operation area.
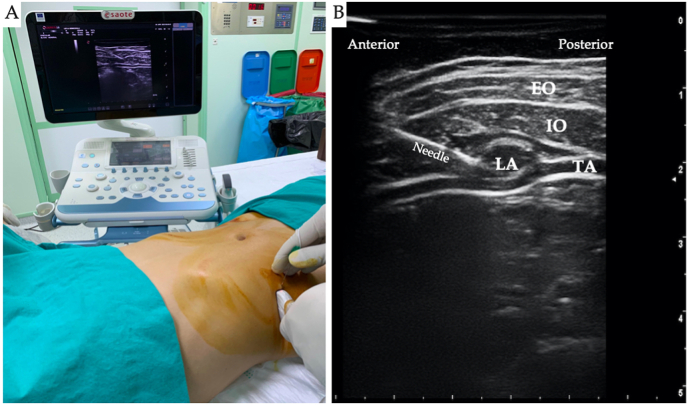
For the lateral QL block, the linear probe was placed at the mid-axillary line on the crista iliaca. After the abdominal wall muscles were defined as three layers, the probe was moved posteriorly. The transversal fascia, the thoracolumbar fascia, and the quadratus lumborum muscle were identified. Subsequently, the needle was advanced between the middle layer of the thoracolumbar fascia and the quadratus lumborum muscle using the in-plane technique. After confirmation of its location by hydro-dissection, 20 ml of 0.375% bupivacaine was injected on both sides (Fig. 1).
Fig. 1.
(A) Location of the transducer with the lateral QL block; (B) An ultrasound image obtained immediately after injection of local anesthetics. EO, external oblique; IO, internal oblique; TA, transversus abdominis; QL, quadratus lumborum; LA, local anesthetics.
For the lateral TAP block, the probe was placed on the midaxillary line in the abdomen, and three specific abdominal wall muscles were defined as the external oblique, internal oblique, and transversus abdominis. After imaging the needle with the in-plane technique, it was advanced in the same plane from the anterolateral side to the posteromedial side. After checking for the presence of blood and air with a negative aspiration test and hydro-dissection with 2–3 ml of saline, 20 ml of 0.375% bupivacaine was injected on both sides between the internal oblique muscle and the border of the transversus abdominis muscle. Blocks were considered successful when the local anesthetic appeared to be correctly distributed under the sonographic image, allowing dissection of the fascia plane. The contralateral block was performed using the same procedures (Fig. 2).
Fig. 2.
(A) Location of the transducer with the TAP block; (B) An ultrasound image obtained during injection of local anesthetics. EO, external oblique; IO, internal oblique; TA, transversus abdominis; LA, local anesthetics.
2.4. Postoperative pain management
Postoperative analgesia was achieved using a multimodal analgesia regimen. Patients in both groups received 30 mg of iv tenoxicam as a non-steroidal anti-inflammatory drug (NSAID) every 12 h. They also received iv tramadol hydrochloride infusions through a PCA device (CADD-Legacy PCA Ambulatory Infusion Pump, Model 6300, Smiths Medical, St. Paul, USA). After the tramadol solution (5 mg/ml) was prepared, the PCA demand dose was adjusted to 10 mg and the lock time to 15 min. No basal infusion was administered, with the maximum daily amount was set at 400 mg. The time of admission of the patient to the recovery room was accepted as t = 0, and hemodynamic parameters and pain scores were recorded at the postoperative 1, 6, 12, 18, and 24 h by anesthesia nurses (ZAT, DO) who were blinded to the group distribution. Postoperative pain was assessed using numerical rating scale values (NRS, 0–10; 0 = no pain and 10 = excruciating pain). Additionally, the amount of opioid consumption in patients, at certain time intervals, and in total, were also recorded. IV meperidine (1 mg) was administered as rescue analgesia to patients with a pain score >4 after PCA use. Furthermore, postoperative nausea and vomiting (PONV) was evaluated using a numerical scale. (0 = no nausea-vomiting, 1 = mild nausea, 2 = severe nausea or vomiting once, 3 = vomiting more than once) If the PONV score was ≥2, 4 mg of ondansetron iv was given as a rescue antiemetic.
2.5. Outcome measurements
The study's primary outcome measure was total tramadol hydrochloride consumption over 24 h. Secondary outcome measures were static and dynamic NRS scores at 1, 6, 12, 18, and 24 h postoperatively. Furthermore, postoperative rescue analgesic requirements and adverse events such as nausea and vomiting were recorded.
2.6. Statistical analysis
Data collected in the study were evaluated using the IBM-SPSS 22.00 program (International Business Machines®- Statistical Package for Social Sciences) for Windows 10. The Kolmogorov-Smirnov test was used to check the normality of the data distributions. For descriptive statistics, categorical variables are given as percentages (%) and numerical variables as mean ± standard deviation. In comparing the quantitative data of the two groups when the normality conditions were met, the two-sample independent t-test was used. Fisher's exact test was used when the variables were qualitative. The Mann-Whitney U test was used for quantitative variable data comparisons when normality conditions were not met. The statistical significance level of alpha was accepted as p < 0.05.
3. Results
All patients included in the study (n = 168) were randomized into two groups, with 84 patients in each arm. The total follow-up period for the patients was 24 h postoperatively. Twenty-nine patients were discharged before the completion of the postoperative 24-h follow-up, two patients underwent laparotomy due to intra-abdominal abscess, and one patient was withdrawn from the study after the surgery (Fig. 3). Consequently, 32 patients were excluded from the study after randomization, 136 patients completed the study, and their data were analyzed. There was no statistically significant difference between the demographic and surgical data (Table 1). Similarly, there was no difference between the groups regarding intraoperative remifentanil requirement (p = 0.584). Both block groups had similar tramadol hydrochloride consumption at postoperative 1, 6, 12, 18, and 24 h (p > 0.05) (Table 2). There was no significant difference between the groups regarding pain scores at all time points (Table 3). Postoperative rescue analgesic needs did not differ between the groups (p = 0.356). Nausea and vomiting scores were similar in the QL and TAP groups, and there was no significant difference between the groups (p = 0.774) (Table 2). Complications related to the block, such as vascular puncture, hematoma, and local anesthetic toxicity, were not observed.
Fig. 3.
Flow chart of the study. QL, quadratus lumborum; TAP, transversus abdominis plane.
Table 1.
Comparison of the demographical and clinical data.
| QL group (n = 68) | TAP group (n = 68) | P value | |
|---|---|---|---|
| Age | 28.81 ± 8.81 | 27.24 ± 7.38 | 0.261 |
| Gender | |||
| Female | 22 (32.4%) | 17 (25.0%) | 0.343 |
| Male | 46 (67.6%) | 51 (75.0%) | |
| Height | 172.82 ± 5.80 | 173.79 ± 5.64 | 0.325 |
| Weight | 71.35 ± 8.89 | 69.94 ± 9.38 | 0.370 |
| BMI | 23.79 ± 1.83 | 23.08 ± 2.33 | 0.050 |
| ASA | |||
| I | 31 (45.6%) | 27 (39.7%) | |
| II | 36 (45.6%) | 38 (55.9%) | 0.514 |
| III | 1 (1.5%) | 3 (4.4%) | |
| Duration of surgery (min) | 70.17 ± 12.83 | 72.76 ± 14.46 | 0.272 |
| Duration of anesthesia (min) | 93.94 ± 12.26 | 96.85 ± 14.70 | 0.212 |
| İntraoperative remifentanil use (μg/kg/min) | 0.043 ± 0.014 | 0.045 ± 0.013 | 0.584 |
| Length of hospital stay (day) | 26.86 ± 2.75 | 27.80 ± 3.23 | 0,070 |
Data are presented as mean standard deviation (SD) or number (%).
QL, quadratus lumborum; TAP, transversus abdominis plane; BMI, body mass index; ASA, American Society of Anesthesiologists.
Table 2.
Postoperative opioid consumptions (mg) and PONV data.
| QL group |
TAP group |
P value | |
|---|---|---|---|
| (n = 68) | (n = 68) | ||
| Postoperative opioid consumption | |||
| 0–6 h | 34.85 ± 36.67 | 36.47 ± 42.83 | 0.716 |
| 6–12 h | 18.38 ± 17.92 | 19.71 ± 23.43 | 0.701 |
| 12–18 h | 11.76 ± 11.45 | 12.06 ± 11.40 | 0.868 |
| 18–24 h | 6.03 ± 8.12 | 5.59 ± 7.20 | 0.927 |
| 0–24 h (cumulative) | 71.03 ± 51.80 | 73.82 ± 54.60 | 0.807 |
| Rescue analgesia requirement | 19 (27.9%) | 24 (35.3%) | 0.356 |
| PONV | |||
| 0 (no nausea/no vomiting) | 53 (77.9%) | 48 (70.6%) | 0.774 |
| 1 (mild nausea) | 12 (17.6%) | 15 (22.1%) | |
| 2 (severe nausea) | 2 (2.9%) | 3 (4.4%) | |
| 3 (vomiting) | 1 (1.5%) | 2 (2.9%) | |
Data are presented as mean standard deviation (SD) or number(%).
QL, Quadratus lumborum; TAP, Transversus abdominis plane; PONV, Postoperative nausea and vomiting.
Table 3.
Pain NRS scores at rest and during movement in the postoperative 24 h.
| QL group |
TAP group |
P value | ||
|---|---|---|---|---|
| (n = 68) | (n = 68) | |||
| Postoperative NRS at rest | ||||
| 1 h | 2 (0–5) | 2 (0–5) | 0.730 | |
| 6 h | 2 (0–4) | 2 (0–3) | 0.834 | |
| 12 h | 1.5 (0–3) | 1 (0–3) | 0.864 | |
| 18 h | 1 (0–3) | 1 (0–3) | 0.387 | |
| 24 h | 0.5 (0–2) | 1 (0–2) | 0.072 | |
| Postoperative NRS during movement | ||||
| 1 h | 3 (0–5) | 2 (0–5) | 0.819 | |
| 6 h | 2.5 (0–5) | 2 (0–4) | 0.227 | |
| 12 h | 2 (0–3) | 2 (0–3) | 0.838 | |
| 18 h | 1 (0–3) | 1 (0–3) | 0.491 | |
| 24 h | 1 (0–3) | 1 (0–2) | 0.859 | |
Data are presented as median (interquartile range).
QL, Quadratus lumborum; TAP, Transversus abdominis plane, NRS, Numerical rating scale; h, hour.
4. Discussion
This randomized controlled, double-blind clinical trial demonstrated that lateral QL and TAP blocks for laparoscopic appendectomy reduced postoperative visceral and incisional pain to a similar extent. Furthermore, the study results found no statistically significant differences between opioid consumption and pain scores in all postoperative periods. This study is, to our knowledge, the first prospective randomized controlled trial to compare the analgesic efficacy of TAP and QL blocks in laparoscopic appendectomy.
Appendicitis surgery is the most frequently performed procedure in general surgery worldwide [1,18]. Video-assisted laparoscopic surgery is associated with less pain, faster recovery, and shorter hospital stays than open surgery [2,19,20]. Postoperative pain in laparoscopic appendectomy occurs due to parietal and visceral peritoneal stimulation from appendicitis and tissue trauma associated with surgery and pneumoperitoneum [10]. Inadequate analgesia or adverse effects related to the use of high-dose opioid analgesics to provide analgesia may prolong surgical recovery. Abdominal wall blocks are frequently used for postoperative analgesia in laparoscopic surgeries. In the enhanced recovery after surgery (ERAS) protocol, a multimodal analgesic approach, including abdominal wall blocks, is recommended in abdominal surgery [21,22].
Ultrasound-guided TAP block has been used for many abdominal surgeries. Clinical studies and meta-analyses have shown that it provides analgesic efficacy after abdominal laparotomy and laparoscopy [23,24]. Three types of ultrasound-guided approaches are currently defined for TAP block: the anterior oblique subcostal, midaxillary, and posterior approach. In the mid-axillary and posterior TAP block approach, excellent posterior distribution of local anesthetic is obtained from the quadratus lumborum to the paravertebral space. The block area obtained in these two approaches can reach T12-L2 and even T5-L1 vertebral levels [25]. Therefore, a TAP block can provide optimal analgesia after laparoscopic or open appendectomy. It was reported that the application of TAP block effectively reduced postoperative opioid consumption and pain scores in patients compared with the control group. Furthermore, we found that TAP block successfully reduced postoperative pain when combined with multimodal analgesia, and pain scores were relatively low at rest and in motion.
On the other hand, QL block has been widely used for postoperative analgesia in many abdominal surgical procedures [[26], [27], [28]]. After the definition of QL block, various approaches such as posterior, lateral, and transmuscular have been described. However, we still do not know whether all of these approaches completely relieve somatic and visceral pain. Although there is no clear opinion on this subject, some clinical and cadaveric studies with QL block suggest that local anesthetic may provide more effective analgesia by spreading to the paravertebral area in the posterior and lateral QL block [26,29]. In general, it has been reported that the block area is observed between T4 and L1 in cadaver and volunteer studies [18,30]. Many randomized controlled clinical studies comparing QL and TAP blocks in abdominal surgery have also been performed with posterior QL blocks [[31], [32], [33]]. Studies with anterior or lateral approach QL blocks are limited in the literature.
A randomized controlled study compared QL and TAP blocks for postoperative analgesia after cesarean section. Although pain scores were similar between the two groups, opioid consumption was higher in the TAP block group [34]. Therefore, the similarity in the pain scores of the two groups may be due to higher opioid consumption in the TAP block group. Although there was no statistical difference between the groups, the amount of opioid consumption was higher in the TAP block group. In another study comparing posteromedial QL and TAP blocks in laparoscopic colorectal surgery, morphine consumption and VAS scores were significantly lower with patient satisfaction higher in the QL group [32]. Clinical studies in laparoscopic surgeries have shown that the QL block with a posterior approach is superior to the TAP block. However, posterior QL and subcostal TAP blocks were compared in a study performed in laparoscopic cholecystectomy. Similar to our study, no differences were found between the two groups regarding pain scores and opioid consumption [35].
Although there is no clear view on this subject, a magnetic resonance imaging study comparing the posterior and lateral QL blocks approach found that the posterior approach showed greater spread from the lateral QL block to the paravertebral space [30,36]. The anterior, lateral, and posterior QL blocks were compared in a cadaver study. It was shown that there was a similar spread, especially in posterior and lateral OL blocks, after 20 ml of dye injection [29]. In a clinical study comparing the lateral and posterior approach of QL blocks in laparoscopic cholecystectomy, it was found that there was no difference between the two groups in VAS scores and opioid consumption, supporting the result of this cadaveric study [37].
Very recently, TAP block, QL block, and control groups were compared in terms of analgesic efficacy in laparoscopic sleeve gastrectomy; similar to our study, no significant differences were found between VAS scores, intraoperative remifentanil consumption, postoperative rescue analgesia requirements, and PONV in the patients who underwent QL and TAP blocks [38]. The lateral QL block is more straightforward and relatively superficial than the posterior approach. Patients do not need to be positioned in any specific manner to perform a block while under anesthesia. For example, it can be performed in the supine position and under general anesthesia in a short time. Both blocks were performed in the supine position after anesthesia induction. Thus, we eliminated the stress effect and made patients blind to group allocation. In this study, we used 0.375%, 40 ml of bupivacaine in both groups to standardize the amount of local anesthetic between the groups and obtain an adequate sensory block. Throughout the study, we observed no local anesthetic complications in either group. During the study, among opioid-related adverse events, the incidence of PONV was low in both groups. This result may be due to less opioid consumption as a result of adequate analgesia. Our patients were also given prophylactic antiemetics at the end of surgery.
In the last 20 years, significant research has been done on transversus abdominis plane blocks. The term TAP block encompasses a variety of approaches that result in different somatic and visceral anesthetic coverage. Contrary to previous perspectives, the present study has shown [10,39] that TAP block provides similar postoperative analgesic effects in laparoscopic appendectomy to lateral QL block. This result also revealed that the lateral TAP block, previously recommended only for open appendectomy, should be reconsidered for the laparoscopic technique as well. As a result, the obtained data may change the perspective in choosing the abdominal wall block type in this procedure [40]. Of the three approaches, only posterior TAP has been reported to spread local anesthetic into the paravertebral spaces. However, due to the results obtained in our study, future studies are needed to compare posterior TAP to lateral QL blocks, as well as, lateral TAP block to other approaches in laparoscopic appendectomy.
The study has some limitations. First, there was no non-intervention control group in the study. Second, we did not test dermatomal analgesia after block because the procedures were performed under general anesthesia. However, we used ultrasound guidance and an echogenic needle to ensure local anesthetic was delivered to the correct area. Moreover, it is not difficult to circumvent existing limitations. Blocks can be performed on the patient in the preoperative period, in which the affected dermatomal areas can be determined. In addition, a control group that did not undergo block and received only iv PCA opioid infusion in the postoperative period could also be added to the study.
5. Conclusion
The study determined that lateral QL and TAP blocks provided equivalent analgesia and postoperative opioid consumption in laparoscopic appendectomy. Therefore, we believe that both blocks provide effective pain management after laparoscopic appendectomy. However, TAP block may be preferred over lateral QL block due to the ease of imaging with ultrasound and more clinical experience associated with that technique.
Ethical approval
The trial was approved by the ethics committee board of Health Sciences University, Bakırköy Dr. Sadi Konuk Training and Research Hospital (Reference Number: 2020-02-23/2020–35), and informed consent was obtained from all patients for participation in the study and the procedures to be performed.
Sources of funding
The authors declare that no source of funding was used for the research, and no sponsors were used in the collection, analysis and interpretation of the data.
Author contribution
(I) Conception and design: Gokhan Sertcakacilar, Gunes Ozlem Yildiz (II) Administrative support: Gokhan Sertcakacilar, Gunes Ozlem Yildiz (III) Provision of study materials or patients: Gokhan Sertcakacilar, Gunes Ozlem Yildiz (IV) Collection and assembly of data: Gokhan Sertcakacilar, Gunes Ozlem Yildiz(V) Data analysis and interpretation: Gokhan Sertcakacilar, Gunes Ozlem Yildiz (VI) Manuscript writing: Gokhan Sertcakacilar, Gunes Ozlem Yildiz (VII) Final approval of manuscript: Gokhan Sertcakacilar, Gunes Ozlem Yildiz.
Trail registry number
-
1.
Name of the registry: Research Registry
-
2.
Unique Identifying number or registration ID: UIN 7984
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked):
Guarantor
Dr. Gokhan Sertcakacilar.
Dr. Gunes Ozlem Yildiz.
Assoc. Prof. Dr. Gulsum Oya Hergunsel
Consent
Informed consent was obtained from all patients for participation in the study and the procedures to be performed. In addition, written informed consent was obtained from the patient for the publication of this study and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal upon request.
Annals of medicine and surgery
The following information is required for submission. Please note that failure to respond to these questions/statements will mean your submission will be returned. If you have nothing to declare in any of these categories then this should be stated.
Provenance and peer review
Not commissioned, externally peer reviewed.
Declaration of competing interest
The authors declare that they have no financial or personal relationship with any (biased) person or organization that could improperly influence their work.
Acknowledgement
The authors want to thank Dr. Yaser Pektaş from University of Health Science, Bakırköy Dr. Sadi Konuk Training and Research Hospital, Istanbul, Turkey for providing the ultrasound photos.
Footnotes
This study was performed in University of Health Sciences, Bakırköy Dr. Sadi Konuk Education and Research Hospital, Department of Anesthesiology and Reanimation, Istanbul, Turkey.
The study was registered to clinicaltrials.gov(NCT05310266).
The study was registered to Research Registry (Unique Identifying Number 7984 -Linkhttps://www.researchregistry.com/browse-the-registry#home/).
Contributor Information
Gokhan Sertcakacilar, Email: drgokhansertcakacilar@gmail.com.
Gunes Ozlem Yildiz, Email: drgunesim@hotmail.com.
References
- 1.Jawaid M., Raza S.M., Alam S.N., Manzar S. On-call emergency workload of a general surgical team. J. Emergencies, Trauma, Shock. 2009;2(1):15–18. doi: 10.4103/0974-2700.44677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li X., Zhang J., Sang L., Zhang W., Chu Z., Li X., et al. Laparoscopic versus conventional appendectomy-a meta-analysis of randomized controlled trials. BMC Gastroenterol. 2010;10:129. doi: 10.1186/1471-230X-10-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pedersen A.G., Petersen O.B., Wara P., Rønning H., Qvist N., Lauberg S. Randomized clinical trial of laparoscopic versus open appendicectomy. Br. J. Surg. 2001;88(2):200–205. doi: 10.1046/j.1365-2168.2001.01652.x. [DOI] [PubMed] [Google Scholar]
- 4.Sabbagh C., Brehant O., Dupont H., Browet F., Pequignot A., Regimbeau J.M. The feasibility of short-stay laparoscopic appendectomy for acute appendicitis:a prospective cohort study. Surg. Endosc. 2012;26(9):2630–2638. doi: 10.1007/s00464-012-2244-1. [DOI] [PubMed] [Google Scholar]
- 5.Ra Y.S., Kim C.H., Lee G.Y., Han J.I. The analgesic effect of the ultrasound-guided transverse abdominis plane block after laparoscopic cholecystectomy. Korean J Anesthesiol. 2010;58:362–368. doi: 10.4097/kjae.2010.58.4.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McDonnell J.G., O'Donnell B., Curley G., Heffernan A., Power C., Laffey J.G. The analgesic efficacy of transversus abdominis plane block after abdominal surgery:a prospective randomized controlled trial. Anesth. Analg. 2007;104(1):193–197. doi: 10.1213/01.ane.0000250223.49963.0f. [DOI] [PubMed] [Google Scholar]
- 7.Karaman T., Ozsoy A.Z., Karaman S., Dogru S., Tapar H., Sahin A., et al. The effects of transversus abdominis plane block on analgesic and anesthetic consumption during total abdominal hysterectomy: a randomized controlled study. Rev. Bras. Anestesiol. 2018;68(3):285–291. doi: 10.1016/j.bjan.2017.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rafi A.N. Abdominal field block: a new approach via the lumbar triangle. Anaesthesia. 2001;56(10):1024–1026. doi: 10.1046/j.1365-2044.2001.02279-40.x. [DOI] [PubMed] [Google Scholar]
- 9.Walter E.J., Smith P., Albertyn R., Uncles D.R. Ultrasound imaging for transversus abdominis blocks. Anaesthesia. 2008;63(2):211. doi: 10.1111/j.1365-2044.2007.05424.x. [DOI] [PubMed] [Google Scholar]
- 10.Tupper-Carey D.A., Fathil S.M., Tan Y.K., Kan Y.M., Cheong C.Y., Siddiqui F.J., et al. A randomised controlled trial investigating the analgesic efficacy of transversus abdominis plane block for adult laparoscopic appendicectomy. Singap. Med. J. 2017;58(8):481–487. doi: 10.11622/smedj.2016068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baeriswyl M., Kirkham K.R., Kern C., Albrecht E. The analgesic efficacy of ultrasound-guided transversus abdominis plane block in adult patients: a meta-analysis. Anesth. Analg. 2015;121(6):1640–1654. doi: 10.1213/ANE.0000000000000967. [DOI] [PubMed] [Google Scholar]
- 12.Blanco R. 271. Tap block under ultrasound guidance: the description of a “no pops” technique. Reg. Anesth. Pain Med. 2007;32:130. [Google Scholar]
- 13.Aygun H., Kavrut Ozturk N., Pamukcu A.S., Inal A., Kiziloglu I., Thomas D.T., et al. Comparison of ultrasound guided Erector Spinae Plane Block and quadratus lumborum block for postoperative analgesia in laparoscopic cholecystectomy patients; a prospective randomized study. J. Clin. Anesth. 2020;62 doi: 10.1016/j.jclinane.2019.109696. [DOI] [PubMed] [Google Scholar]
- 14.Deng W., Long X., Li M., Li C., Guo L., Xu G., et al. Quadratus lumborum block versus transversus abdominis plane block for postoperative pain management after laparoscopic colorectal surgery: a randomized controlled trial. Medicine (Baltim.) 2019;98(52) doi: 10.1097/MD.0000000000018448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.İpek C.B., Kara D., Yılmaz S., Yeşiltaş S., Esen A., Dooply S., et al. Comparison of ultrasound-guided transversus abdominis plane block, quadratus lumborum block, and caudal epidural block for perioperative analgesia in pediatric lower abdominal surgery. Turk. J. Med. Sci. 2019;49(5):1395–1402. doi: 10.3906/sag-1812-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ueshima H., Otake H., Lin J.A. Ultrasound-guided quadratus lumborum block: an updated review of anatomy and techniques. BioMed Res. Int. 2017;2017 doi: 10.1155/2017/2752876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.LauJWY, Rosin D., Agha R. The CONSORT (CONsolidated standards of reporting trials) 2010 guideline. Int. J. Surg. 2021;93:2900565–2900566. Avaialble online: http://www.journal-surgery.net/article/S1743-9191%2811%2900565-6/fulltext. [Google Scholar]
- 18.B. Siam, A. Al-Kurd, N. Simanovsky, H. Awesat, Y. Cohn, B. Helou, et al. Comparison of appendectomy outcomes between senior general surgeons and general surgery residents, JAMA Surg 152 (7) 2017 679-685. doi:10.1001/jamasurg.2017.0578. [DOI] [PMC free article] [PubMed]
- 19.Pedersen A.G., Petersen O.B., Wara P., Rønning H., Qvist N., Laurberg S. Randomized clinical trial of laparoscopic versus open appendicectomy. Br. J. Surg. 2001;88(2):200–205. doi: 10.1046/j.1365-2168.2001.01652.x. [DOI] [PubMed] [Google Scholar]
- 20.Sabbagh C., Brehant O., Dupont H., Browet F., Pequignot A., Regimbeau J.M. The feasibility of short-stay laparoscopic appendectomy for acute appendicitis: a prospective cohort study. Surg. Endosc. 2012;26(9):2630–2638. doi: 10.1007/s00464-012-2244-1. [DOI] [PubMed] [Google Scholar]
- 21.Kim A.J., Yong R.J., Urman R.D. The role of transversus abdominis plane blocks in enhanced recovery after surgery pathways for open and laparoscopic colorectal surgery. J. Laparoendosc. Adv. Surg. Tech. 2017;27(9):909–914. doi: 10.1089/lap.2017.0337. [DOI] [PubMed] [Google Scholar]
- 22.Akerman M., Pejčić N., Veličković I.A. Review of the quadratus lumborum block and ERAS. Front. Med. 2018;5:44. doi: 10.3389/fmed.2018.00044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jalali S.M., Bahri M.H., Yazd S.M.M., Karoobi M., Shababi N. Efficacy of laparoscopic transversus abdominis plane block on postoperative pain management and surgery side effects in laparoscopic bariatric surgeries. Langenbeck's Arch. Surg. 2022;407(2):549–557. doi: 10.1007/s00423-021-02400-9. [DOI] [PubMed] [Google Scholar]
- 24.Baeriswyl M., Kirkham K.R., Kern C., Albrecht E. The analgesic efficacy of ultrasound-guided transversus abdominis plane block in adult patients: a meta-analysis. Anesth. Analg. 2015;121(6):1640–1654. doi: 10.1213/ANE.0000000000000967. [DOI] [PubMed] [Google Scholar]
- 25.Tsai H.C., Yoshida T., Chuang T.Y., Yang S.F., Chang C.C., Yao H.Y., et al. Transversus abdominis plane block: an updated review of anatomy and techniques. BioMed Res. Int. 2017;2017 doi: 10.1155/2017/8284363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blanco R., Ansari T., Girgis E. Quadratus lumborum block for postoperative pain after caesarean section: a randomised controlled trial. Eur. J. Anaesthesiol. 2015;32(11):812–818. doi: 10.1097/EJA.0000000000000299. [DOI] [PubMed] [Google Scholar]
- 27.Lai R., Luo Q., Lai J., Lu X., Xu M. Ultrasound-guided quadratus lumborum block for perioperative analgesia in robot-assisted partial nephrectomy: a randomized controlled trial. Trials. 2021;22(1):840. doi: 10.1186/s13063-021-05815-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim S.H., Kim H.J., Kim N., Lee B., Song J., Choi Y.S. Effectiveness of quadratus lumborum block for postoperative pain: a systematic review and meta-analysis. Minerva Anestesiol. 2020;86(5):554–564. doi: 10.23736/S0375-9393.20.13975-0. [DOI] [PubMed] [Google Scholar]
- 29.Carline L., McLeod G.A., Lamb C. A cadaver study comparing spread of dye and nerve involvement after three different quadratus lumborum blocks. Br. J. Anaesth. 2016;117(3):387–394. doi: 10.1093/bja/aew224. [DOI] [PubMed] [Google Scholar]
- 30.Tamura T., Kitamura K., Yokota S., Ito S., Shibata Y., Nishiwaki K. Spread of quadratus lumborum block to the paravertebral space via intramuscular injection: a volunteer study. Reg. Anesth. Pain Med. 2018;43(4):372–377. doi: 10.1097/AAP.0000000000000735. [DOI] [PubMed] [Google Scholar]
- 31.Murouchi T., Iwasaki S., Yamakage M. Quadratus lumborum block: analgesic effects and chronological ropivacaine concentrations after laparoscopic surgery. Reg. Anesth. Pain Med. 2016;41(2):146–150. doi: 10.1097/AAP.0000000000000349. [DOI] [PubMed] [Google Scholar]
- 32.Huang D., Song L., Li Y., Xu Z., Li X., Li C. Posteromedial quadratus lumborum block versus transversus abdominal plane block for postoperative analgesia following laparoscopic colorectal surgery: a randomized controlled trial. J. Clin. Anesth. 2020;62 doi: 10.1016/j.jclinane.2020.109716. [DOI] [PubMed] [Google Scholar]
- 33.Liu X., Song T., Chen X., Zhang J., Shan C., Chang L., et al. Quadratus lumborum block versus transversus abdominis plane block for postoperative analgesia in patients undergoing abdominal surgeries: a systematic review and meta-analysis of randomized controlled trials. BMC Anesthesiol. 2020;20(1):53. doi: 10.1186/s12871-020-00967-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Blanco R., Ansari T., Riad W., Shetty N. Quadratus lumborum block versus transversus abdominis plane block for postoperative pain after cesarean delivery: a randomized controlled trial. Reg. Anesth. Pain Med. 2016;41(6):757–762. doi: 10.1097/AAP.0000000000000495. [DOI] [PubMed] [Google Scholar]
- 35.Baytar Ç., Yılmaz C., Karasu D., Topal S. Comparison of ultrasound-guided subcostal transversus abdominis plane block and quadratus lumborum block in laparoscopic cholecystectomy: a prospective, randomized, controlled clinical study. Pain Res. Manag. 2019;2019 doi: 10.1155/2019/2815301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tamura T., Yokota S., Ito S., Shibata Y., Nishiwaki K. Local anesthetic spread into the paravertebral space with two types of quadratus lumborum blocks: a crossover volunteer study. J. Anesth. 2019;33(1):26–32. doi: 10.1007/s00540-018-2578-5. [DOI] [PubMed] [Google Scholar]
- 37.Ökmen K., Metin Ökmen B., Sayan E. Ultrasound-guided lateral versus posterior Quadratus Lumborum Block for postoperative pain after laparoscopic cholecystectomy: a randomized controlled trial. Turk J Surg. 2019;35(1):23–29. doi: 10.5578/turkjsurg.4161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xue Q., Chu Z., Zhu J., Zhang X., Chen H., Liu W., et al. Analgesic efficacy of transverse abdominis plane block and quadratus lumborum block in laparoscopic sleeve gastrectomy: a randomized double-blinded clinical trial. Pain Ther. 2022;10 doi: 10.1007/s40122-022-00373-1. 1007. s40122-022-00373-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tanggaard K., Jensen K., Lenz K., Vazin M., Binzer J., Lindberg-Larsen V.O., et al. A randomised controlled trial of bilateral dual transversus abdominis plane blockade for laparoscopic appendicectomy. Anaesthesia. 2015;70(12):1395–1400. doi: 10.1111/anae.13234. [DOI] [PubMed] [Google Scholar]
- 40.Tran D.Q., Bravo D., Leurcharusmee P., Neal J.M. Transversus abdominis plane block: a narrative review. Anesthesiology. 2019;131(5):1166–1190. doi: 10.1097/ALN.0000000000002842. [DOI] [PubMed] [Google Scholar]