1. Introduction
Monkeypox is a zoological virus caused by the monkeypox virus, which is an orthopoxvirus (genera) and Chordopoxvirinae (subfamily) and a close subgroup of variola viruses (smallpox). It is classified as ACDP Hazard Group-3 pathogen in the UK. Monkeypox was first discovered in Monkeys in 1958, which was further spread to humans in 1970. The first human case was reported in the Democratic Republic of Congo (DRC) and then in Central and Western African countries [1].
In 2003, there was an outbreak in the US with 47 confirmed cases that were spread due to the import of animals like Gambian giant rats, squirrels, striped mice, and dormice that spread viruses to pet prairie dogs. 7 cases have been reported in the UK in 2018, 2019, and 2021. In 2021, 3 confirmed cases reported the travel history to Nigeria, and in 2018, an HCP contracted the infection through a confirmed case [2].
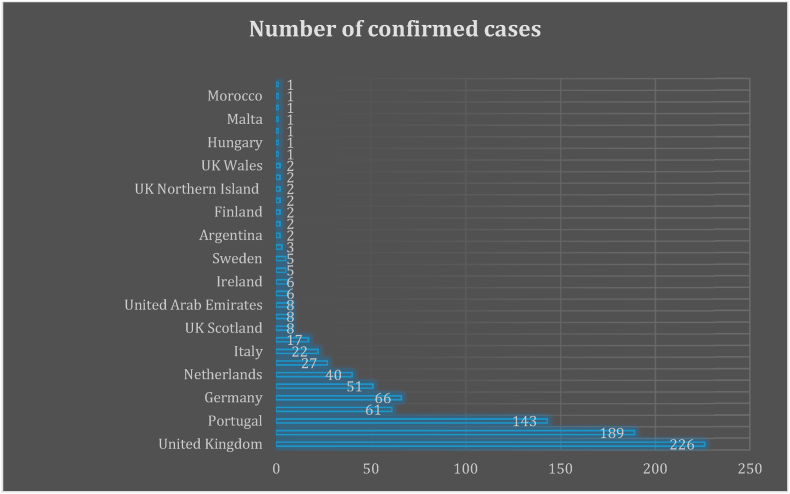
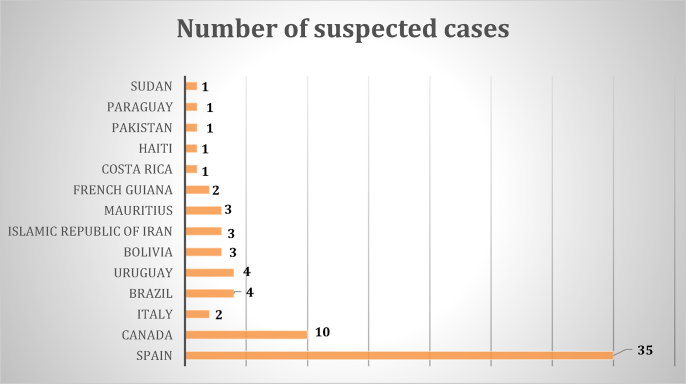
Now in 2022, there has been a notable surge in the cases. The 1st case was reported in the UK on May 7. As of 2 June, 226 confirmed cases were reported from the UK, Portugal reported 143 confirmed cases, Spain reported 189 confirmed and 35 suspected cases, the US reported 27confirmed cases [[3], [4], [5]]. Further number of cases are given in Fig-1, Fig-2
Fig-1.
Number of confirmed cases.
Fig-2.
Number of suspected cases.
Transmission: is due to.
-
●
Large respiratory droplets,
-
●
Infected animal or human,
-
●
Lesion materials,
-
●
Body fluids,
-
●
Indirect contact with lesion materials,
-
●
Contact with clothing or linens,
-
●
Human to human Through nosocomial & household, and
-
●
Wild meat preparation [6].
Notable cases were identified among gay, bisexuals, and men who have sex with men [6].
Symptoms
-
●
Fever-temp of >100.4 (38 C)
-
●
Rash (macular, papular, vesicular, pustular, popular, or localized, discrete or confluent)
-
●
Lymphadenopathy-preauricular, axillary, cervical, and inguinal.
-
●
Mouth sores, sore throat
-
●
Headache
-
●
Muscle aches and backaches
- ●
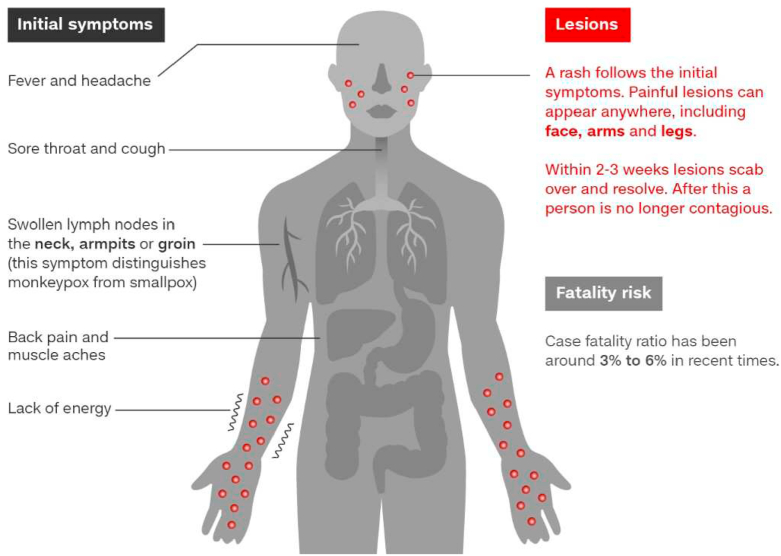
Fig-3.
Stages of recovery.
Fig-4.
Symptoms of small pox (Adapted from Centers of Disease Control and Prevention, World Health Organization, Graphic: Natalie Leung, CNN).
It usually begins with flu-like illness and swelling of lymph nodes, which progresses to a widespread rash on the face and body. A rash starts from the face and spreads to other areas such as genitals, etc. The rash then forms a lesion or scab that falls off. The rash may look like syphilis or chickenpox which may present confusion in diagnosis. Sites of lesions include face, scalp, trunk, limbs, palm, glans pens, scrotum, soles, hands (including nail beds), labia majora, penile shaft, arms & legs.
The incubation period is typically 6–16 days and up to 21 days. When the scab falls, the person is no longer infectious.
Complications: Pneumonitis, Encephalitis, Sight-threatening keratitis, Secondary bacterial infections, Low mood & emotional lability, Ulcerated inguinal lesions with delayed healing, Deep tissue abscess, Conjunctivitis, Painful disruption of thumbnail due to sublingual lesions, and Pruritis and contact dermatitis [7].
Treatment
There is no specific treatment for monkeypox. It is said that the chickenpox vaccine is 85% effective in preventing infection. Antivirals like cidofovir, brincidofovir (orally, 200 mg/week) and tecovirimat (Orally, 600 mg BD for 2 weeks) are being used. These drugs are approved for use for Smallpox in the US. No trials have been reported but both the drugs have proved efficacy against orthopoxviruses. The side effects of this treatment include nephrotoxicity and cytomegalovirus infections, transaminitis (ALT 127–550 U/L), nausea, and abdominal discomfort. No patient is reported to complete the course of Brincidofovir due to the side effects. Hence, tecovirimat is preferred. The days of hospitalization ranged from 10 to 39 days in severe cases [8].
Recommendations
-
●
For individuals with clinical symptoms, the HCP should consider monkeypox as a differential diagnosis.
-
●
Patients with otherwise unexplained rash who had a history of travel in the last 21 days to any country, should be considered screening for monkeypox.
-
●
The suspected cases should be isolated and tested. The test results should be notified promptly.
-
●
Backward and forward contact tracing to be practiced for positive cases.
-
●
Advice smallpox vaccination for high-risk close contacts after the consideration of risk-benefit assessment.
-
●
The infectivity of patients with positive respiratory swabs and crusted skin lesions remained undetermined.
-
●
Isolate the suspected patient in a negative pressure room, and ensure that the staff around is using PPE.
-
●
Appropriate respiratory isolation for both suspected and confirmed cases.
-
●
Scabs are infectious, therefore care must be taken to avoid infection when handling, bedding, clothing, and so on.
Precautionary measures
-
●
Wash hands frequently with soap and water especially after visiting the infected patients.
-
●
Don't share bedding, clothing, towels & utensils with infected patients.
-
●
Maintain respiratory etiquette.
-
●
Thoroughly cook meat before eating.
-
●
Avoid contact with wild animals especially stray ones that are found sick or dead.
Points to contemplate
-
•
Most reported cases are in the age group of 30–40 years with males more affected than females.
-
•
The country of acquisition- Nigeria, UK.
-
•
Symptoms include fever, headache, rashes, lesions, lymphadenopathy, chills & exhaustion. The number of concurrent lesions ranges from 10 to 150.
-
•
It is usually self-limiting with symptoms lasting for 2–4 weeks. Generally, cases are mild and recover in weeks.
-
•
The death rate depends on the type, the reported fatality was 3.6% in the West African clade and 1–10% in the Congo basin. The mortality is higher in children, young adults, and immunocompromised patients.
-
•
The young adults had no pre-e siting comorbidities and none had received pre-exposure to smallpox vaccine.
Sources of funding
None.
Ethical approval
Not required.
Consent
Not required.
Author contribution
Both authors contributed equally.
Registration of research studies
Not applicable.
Name of the registry:
Unique Identifying number or registration ID:
Hyperlink to your specific registration (must be publicly accessible and will be checked):
Guarantor
Nabeela Fatima.
Declaration of competing interest
None.
References
- 1.Marennikova S.S., Šeluhina E.M., Mal'Ceva N.N., Čimiškjan K.L., Macevič G.R. Isolation and properties of the causal agent of a new variola-like disease (monkeypox) in man. Bull. World Health Organ. 1972;46(5):599. [PMC free article] [PubMed] [Google Scholar]
- 2.CDC Monkeypox in the United States. 2021. https://www.cdc.gov/poxvirus/monkeypox/outbreak/us-outbreaks.html
- 3.UK Health Security Agency Monkeypox cases confirmed in England: latest updates. May 2022. https://www.gov.uk/government/news/monkeypox-cases-confirmed-in-england-latest-updates
- 4.Portugal identifies five monkeypox infections, Spain has 23 suspected cases. Reuters. May 2022. https://www.reuters.com/business/healthcare-pharmaceuticals/portugal-identifies-five-monkeypox-infections-spain-has-23-suspected-cases-2022-05-18
- 5.Centers for Disease Control and Prevention Outbreak from imported mammals. 2003. https://www.cdc.gov/poxvirus/monkeypox/outbreak/us-outbreaks.html
- 6.Mahase E. Monkeypox: what Do We Know about the Outbreaks in Europe and North America?. [DOI] [PubMed]
- 7.Learned L.A., Reynolds M.G., Wassa D.W., Li Y., Olson V.A., Karem K., Stempora L.L., Braden Z.H., Kline R., Likos A., Libama F. Extended interhuman transmission of monkeypox in a hospital community in the Republic of the Congo. Am. J. Trop. Med. Hyg. 2003;73(2):428–434. 2005 Aug 1. [PubMed] [Google Scholar]
- 8.UK Health Security Agency Monkeypox. https://www.gov.uk/guidance/monkeypox#treatment