Abstract
Background:
While surgeons with high caseload volumes deliver higher value care when performing primary anterior cruciate ligament reconstruction (ACLR), the effect of surgeon volume in the revision setting is unknown.
Purposes:
To determine the percentage of revision ACLR procedures that comprise the practice of high-, medium-, and low-volume surgeons and to analyze associated referral and practice patterns.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
We retrospectively investigated all revision ACLR procedures performed between 2015 and 2020 in a single health care system. Surgeons were categorized as low (≤17), medium (18-34), or high (≥35) volume based on the number of annual ACLR procedures performed. Patient characteristics, activity level, referral source, concomitant injuries, graft type, and treatment variables were recorded, and a comparison among surgeon groups was performed.
Results:
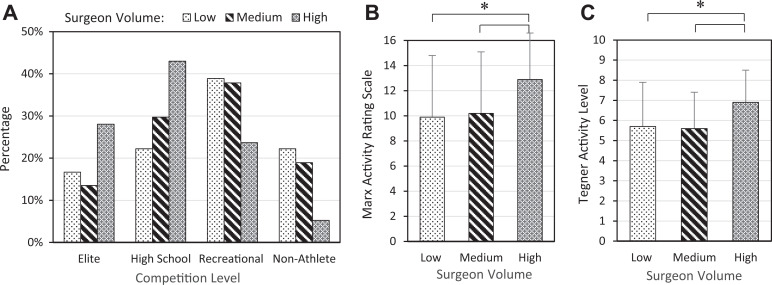
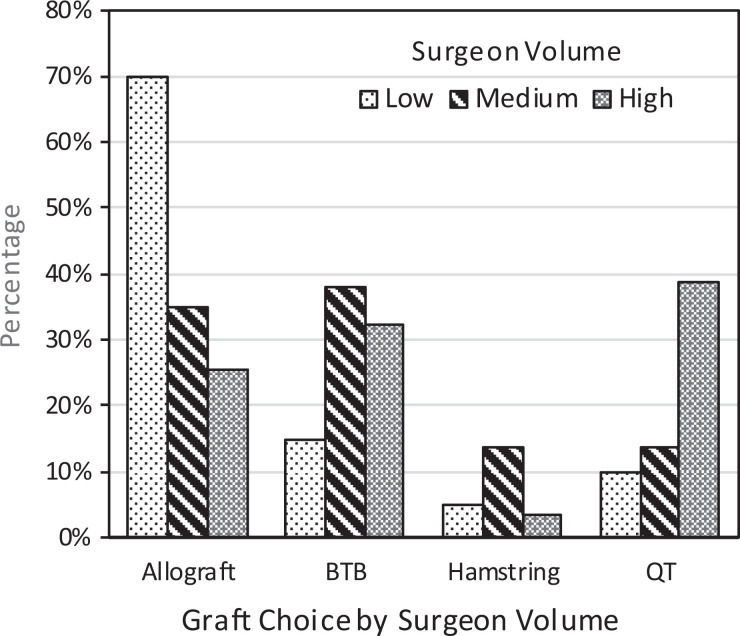
Of 4555 ACLR procedures performed during the study period, 171 (4%) were revisions. The percentage of revision ACLR procedures was significantly higher for high-volume (5%) and medium-volume (4%) surgeons compared with low-volume surgeons (2%) (P < .01). Patients undergoing revision ACLR by a high-volume surgeon had a significantly higher baseline activity level (P = .01). Allografts were used significantly more often by low-volume surgeons (70%) compared with medium-volume (35%) and high-volume (25%) surgeons (P < .01). Bone–patellar tendon–bone (BPTB) and quadriceps tendon (QT) autografts were used significantly more often by high-volume (32% BPTB, 39% QT) and medium-volume (38% BPTB, 14% QT) surgeons compared with low-volume surgeons (15% BPTB, 10% QT) (P < .01). High-volume surgeons were more likely to perform revision on patients with cartilage injuries (P = .01), perform staged revision ACLR (P = .01), and choose meniscal repair (54% high vs 22% medium and 36% low volume; P = .03), despite similar rates of concomitant meniscal tears, compared with low- and medium-volume surgeons.
Conclusion:
In this registry study of an integrated health care system, high-volume surgeons were more likely to perform revision ACLR on patients with higher activity and competition levels. Additionally, high-volume surgeons more commonly performed staged revision ACLR, chose meniscus-sparing surgery, and favored the use of autografts compared with low-volume surgeons.
Keywords: ACL, anterior cruciate ligament, revision, ACL reconstruction, practice patterns
When anterior cruciate ligament (ACL) reconstruction (ACLR) is performed by high-volume surgeons, lower rates of reoperations, readmissions, and infections and decreased costs have been demonstrated. 7,11,18,19 Various causes of ACLR failure, including recurrent trauma, patient-related factors, graft choice, and technical errors, have commonly been discussed and have been studied in multiple prospective registries. 3,6,20 However, surgeon expertise and case volume have not been reported or discussed. 12
Given the greater level of technical expertise required in performing revision ACLR, practice patterns for revision ACLR are likely different among surgeons with various surgical volumes. In the primary ACLR setting, high-volume surgeons have been shown to more effectively utilize hospital resources. 5,19 Additionally, for primary ACLR, surgeons with higher volumes have been shown to more commonly use autografts and repair the meniscus when concomitant meniscal injuries are present. 4,8 While the effect of surgeon volume on revision ACLR practices has not been studied, this knowledge would be useful for improving the delivery of high-quality care.
The purpose of this study was to determine the percentage of revision ACLR procedures that comprise the practice of high-, medium-, and low-volume ACLR surgeons; additionally, we aimed to assess referral patterns and descriptive, injury, and treatment variables in each group. It was hypothesized that high-volume surgeons would perform more revision ACLR procedures annually than would medium- and low-volume surgeons; additionally, revision ACLR for high-volume surgeons would more commonly consist of patients with complex pathology referred from other providers and health care systems.
Methods
After receiving institutional review board approval, we conducted a retrospective database review of all primary and revision ACLR procedures performed between January 1, 2015, and January 31, 2020, within a single health care system. Patients are prospectively entered into this database, which includes all ACLR procedures performed within the 12 facilities making up the system. All ACLR procedures performed during the study period were included in this study. All patients provided written informed consent prior to ACLR.
Surgeons were categorized by the number of annual ACLR procedures performed as low (≤17), medium (18-34), or high (≥35) volume. This cutoff has been previously described to determine clinically meaningful annual volume thresholds based on the risk of subsequent knee surgery after ACLR as opposed to an arbitrarily defined volume cutoff point. 18 Additionally, using this method, more similar percentages of surgeons in each category (46% low volume, 29% medium volume, and 25% high volume) were found in the database.
All revision ACLR procedures, defined as those in which a second ACLR procedure was performed after primary ACLR, were recorded. Both the referral source for each revision ACLR procedure and whether multiple revisions had been performed were recorded. All cases in which the referral source was available were included in the final analysis. There were 2 revision ACLR procedures with an unknown referral source that were identified and subsequently excluded. Referral source was defined as being from outside the participating health care system, within the participating health care system, and self-referral (cases in which primary ACLR was performed by the surgeon performing revision ACLR). Descriptive data including age at the time of primary and revision ACLR, baseline activity level (competition level, Marx activity rating scale score, and Tegner activity scale score), and time from graft failure or previous ACLR to revision ACLR were recorded. For analysis of the competition level, all athletes competing at the collegiate level or higher were considered “elite.” Injury data including total concomitant injuries, meniscal tears, cartilage injuries, and multiligament knee injuries were recorded. Finally, treatment data including graft type, whether staged revision ACLR was performed, and type of treatment for concomitant injuries were collected for each revision ACLR procedure.
For statistical analysis, group and subgroup comparisons among surgeons with different caseload volumes (low, medium, and high) were performed using the chi-square test for categorical variables. A 1-way analysis of variance with post hoc Tukey analysis or the Kruskal-Wallis test was used for parametric or nonparametric continuous variables, respectively. For detection of the percentage of revision ACLR procedures in the practices of low-, medium-, and high-volume surgeons, a post hoc power analysis demonstrated a power of 0.98 for a difference of ≥2% between groups. Statistical analysis was performed using SPSS Statistics (Version 26; IBM Corp), with the threshold for significance set at P < .05.
Results
Of 4555 ACLR procedures that were performed during the study period, 171 (4%) were revisions. There were 2 revision ACLR procedures that did not have data on the surgeon who had performed primary ACLR and were secondarily excluded from the analysis of referral source. Of the 171 revisions included in the analysis, 142 were referrals from within the integrated health care system, and 29 were external referrals. The included revision ACLR procedures were performed on 154 patients with a mean age of 22.9 ± 9.3 years. The mean age at the time of primary ACLR was significantly different for patients who subsequently underwent revision by low-volume (23.1 ± 9.3 years), medium-volume (22.0 ± 9.3 years), and high-volume (18.5 ± 6.9 years) surgeons (P = .03). The mean age at the time of revision ACLR was 27.1 ± 11.9, 24.5 ± 9.9, and 21.6 ± 8.4 years for low-, medium-, and high-volume surgeons, respectively, but this difference was not statistically significant.
The percentage of revision ACLR procedures was significantly higher for high-volume (5%) and medium-volume (4%) surgeons compared with low-volume surgeons (2%) (P < .01). There was no statistically significant difference in the number of revisions performed by surgeons who had performed the primary ACLR procedure among the groups. There were no statistically significant differences in the referral source between the surgeon groups (Table 1).
Table 1.
Referral Sources for Revision ACLR (n = 171) a
| Surgeon Volume | |||
|---|---|---|---|
| Low | Medium | High | |
| Outside integrated health care system | 3 (15) | 2 (5) | 24 (21) |
| Within health care system | 4 (20) | 9 (24) | 28 (25) |
| Self-referral | 13 (65) | 26 (70) | 62 (54) |
| Re-revision | 1 (5) | 4 (11) | 11 (10) |
| Total annual cases, n | 20 | 37 | 114 |
a Data are presented as n (%) unless otherwise specified. ACLR, anterior cruciate ligament reconstruction.
Patients undergoing revision by a high-volume surgeon were significantly more likely to have a higher baseline activity level, as defined by the competition level (P = .01), as well as higher Marx and Tegner scores (P < .01 for both) compared with medium- and low-volume surgeons (Figure 1 and Table 2).
Figure 1.
(A) Competition level, (B) Marx activity rating scale score, and (C) Tegner activity scale score of low-volume (≤17 cases per year), medium-volume (18-34 cases per year), and high-volume (≥35 cases per year) surgeons. High-volume surgeons were statistically significantly more likely to perform revision anterior cruciate ligament reconstruction on elite and high school athletes as well as athletes with higher Marx and Tegner scores than were medium- and low-volume surgeons. *Statistically significant difference between groups (P < .05).
Table 2.
Statistically Significant Patient, Injury, and Treatment Variables for Revision ACLR a
| Surgeon Volume | ||||
|---|---|---|---|---|
| Low (n = 20) | Medium (n = 37) | High (n = 114) | P Value | |
| Activity level | [n = 18, not 20.] b | .01 | ||
| Elite | 3 (17) | 5 (14) | 32 (28) | |
| High school | 4 (22) | 11 (30) | 49 (43) | |
| Recreational | 7 (39) | 14 (38) | 27 (24) | |
| Nonathlete | 4 (22) | 7 (19) | 6 (5) | |
| Marx score | 9.9 ± 4.9 | 10.2 ± 4.9 | 12.9 ± 3.7 | <.01 |
| Tegner score | 5.7 ± 2.2 | 5.6 ± 1.8 | 6.9 ± 1.6 | <.01 |
| Graft choice for primary ACLR | <.01 | |||
| Allograft | 10 (50) | 11 (30) | 17 (15) | |
| Autograft | 9 (45) | 26 (70) | 88 (77) | |
| Unknown | 1 (5) | 0 (0) | 9 (8) | |
| Graft choice for revision ACLR | <.01 | |||
| Allograft | 14 (70) | 13 (35) | 29 (25) | |
| BPTB autograft | 3 (15) | 14 (38) | 37 (32) | |
| Hamstring tendon autograft | 1 (5) | 5 (14) | 4 (4) | |
| QT autograft | 2 (10) | 5 (14) | 44 (39) | |
| Cartilage injury | 9 (45) | 13 (35) | 71 (62) | .01 |
| Staged management | 3 (15) | 3 (8) | 37 (33) | .01 |
a Data are presented as n (%) or mean ± SD. b n = 18 for the activity level analysis as data was not available for 2 patients. The rest of the analysis in the table for the low-volume group were done with n = 20. Boldface P values indicate statistically significant differences according to surgeon volume (P < .05; chi-square test for categorical variables and 1-way analysis of variance for continuous variables). ACLR, anterior cruciate ligament reconstruction; BPTB, bone–patellar tendon–bone; QT, quadriceps tendon.
Significant differences in graft choice for revision ACLR were seen, with allografts more frequently used by low-volume (n = 14 [70%]) compared to medium-volume (n = 13 [35%]) and high-volume (n = 29 [25%]) surgeons (P < .01) (Figure 2). Bone–patellar tendon–bone (BPTB) and quadriceps tendon (QT) autografts were more likely to be used by high-volume (n = 37 [32%] and n = 44 [39%], respectively) and medium-volume (n = 14 [38%] and n = 5 [14%], respectively) surgeons compared to low-volume surgeons (n = 3 [15%] and n = 2 [10%], respectively) (P < .01). A significant difference was also seen in graft type utilized for primary ACLR, with allografts and autografts being used for patients subsequently undergoing revision by low-volume surgeons in 50% and 45% of cases, respectively; medium-volume surgeons in 30% and 70%, respectively; and high-volume surgeons in 15% and 77%, respectively (P < .01). Of note, low-volume surgeons performed revision ACLR in elite or high school athletes in 39% of cases but these patients had autografts in 45% of primary ACLR cases, while high-volume surgeons performed revision ACLR in elite or high school athletes in 71% of cases but these athletes had autografts in 77% of primary ACLR cases. A subgroup analysis was conducted and found that in cases of revision ACLR for elite and high school athletes, an autograft was used in 43% of these cases by low-volume surgeons, 75% by medium-volume surgeons, and 78% by high-volume surgeons, although this failed to meet statistical significance (P = .12).
Figure 2.
Graft choice among low-volume (≤17 cases per year), medium-volume (18-34 cases per year), and high-volume (≥35 cases per year) surgeons. BTB, bone-tendon-bone; QT, quadriceps tendon.
There was no statistically significant difference in the percentage of revisions performed with concomitant meniscal tears when stratified by surgeon volume. However, high-volume surgeons were more likely to treat a meniscal tear with repair (54%) or allograft transplantation (7%) compared to medium-volume (22% and 0%, respectively) and low-volume (36% and 0%, respectively) surgeons, while partial meniscectomy was performed more commonly by low-volume (50%) and medium-volume (57%) surgeons compared with high-volume surgeons (24%) (P = .03) (Table 3).
Table 3.
Treatment of Concomitant Meniscal Tears at the Time of Revision ACLR a
| Surgeon Volume | |||
|---|---|---|---|
| Low | Medium | High | |
| Meniscal tear | 14 (70) | 23 (62) | 67 (59) |
| Nonoperative treatment | 2 (14) | 4 (17) | 10 (15) |
| Partial meniscectomy | 7 (50) | 13 (57) | 16 (24) |
| Meniscectomy | 0 (0) | 1 (4) | 0 (0) |
| Repair | 5 (36) | 5 (22) | 36 (54) |
| Allograft transplantation | 0 (0) | 0 (0) | 5 (7) |
a Data are presented as n (%). A significant difference in treatment choice existed according to surgical volume (P = .03). ACLR, anterior cruciate ligament reconstruction.
A subgroup analysis demonstrated that there was no significant difference in meniscal tear treatment between medium- and low-volume surgeons (P = .78). High-volume surgeons were more likely to perform revision ACLR on patients with cartilage injuries (n = 71 [62%]) (P = .01); however, there was no statistically significant difference in the type of treatment for concomitant cartilage injuries by surgeon volume. Finally, high-volume surgeons were found to be more likely to perform staged revision ACLR (n = 37 [33%]) compared with low-volume (n = 3 [15%]) and medium-volume (n = 3 [8%]) surgeons (P = .01). No significant differences were identified regarding patient age at the time of revision ACLR (P = .13), time from ACLR graft failure to revision ACLR (P = .92), time between most recent ACLR and revision ACLR (P = .79), total concomitant injuries (P = .88), or multiligament injuries (P = .59).
Discussion
The main finding of this study was that practice patterns for revision ACLR varied significantly among surgeons with different surgical volumes. Low-volume surgeons were found to perform fewer revision ACLR procedures and utilize significantly more allografts compared with high- and medium-volume surgeons, while high- and medium-volume surgeons were more likely to use QT and BPTB autografts. High-volume surgeons were more likely to perform meniscus-sparing procedures, perform more staged revisions, and treat patients with concomitant cartilage injuries compared to medium- and low-volume surgeons. High-volume surgeons were more likely to perform revision ACLR on patients of higher activity and competition levels than were low- and medium-volume surgeons.
The study findings indicated that the percentage of revision ACLR procedures was significantly higher for high-volume (5%) and medium-volume (4%) surgeons compared with low-volume surgeons (2%). These findings are similar to prior reports in the literature, with rerupture rates reported as low as 3.5%, even when revision ACLR was performed by experienced surgeons. 2,7,9,10 While previous studies have reported that revision ACLR is more likely to be performed by a different surgeon from the one performing the primary ACLR procedure, particularly when a low-volume surgeon performed the primary ACLR, we did not find any difference in the referral source within this study cohort. 21 A similar number of revisions were performed by the same surgeons who performed the primary ACLR procedures among high-, medium-, and low-volume surgeons in this study. This contradicts current evidence that high-volume surgeons perform higher quality primary ACLR, as the need for revision ACLR may be similar, despite surgeon volume. However, this study only captured patients who underwent revision ACLR; an analysis of the number of patients with ACLR failure who did not elect to undergo revision surgery may yield different results. In the current study, high-volume surgeons were more likely to perform revision on patients with cartilage injuries as well as choose meniscus-preserving surgery. Recent studies from the Multicenter Orthopaedic Outcomes Network and Multicenter ACL Revision Study (MARS) groups demonstrated meniscal and cartilage injuries in 90% of patients at the time of revision ACLR. 1,13 Furthermore, the predilection for meniscus preservation seen in the current study aligns with prior literature demonstrating an increased incidence of meniscal repair procedures by higher volume surgeons in the primary ACLR setting. 25
In the current study, while there was no difference in the rate of revisions performed by the same surgeon who performed the primary ACLR procedure, high-level athletes more commonly had revision ACLR performed by high-volume surgeons. This may provide an explanation for prior findings reported in the literature demonstrating that patients change surgeons 75% of the time when primary ACLR was performed by a low-volume surgeon compared with 21% of the time when primary ACLR was performed by a high-volume surgeon. 21 This may be a result of high-level athletes desiring treatment by perceived experts, particularly after experiencing ACLR failure.
In this study, low-volume surgeons were more likely to use allografts for revision ACLR compared with medium- and high-volume surgeons. Low-volume surgeons utilized allografts more often than all other autograft options combined (70% of cases), while medium- and high-volume surgeons only used allografts in 35% and 25% of their cases, respectively. Prior studies have consistently demonstrated better outcome scores and lower graft failure rates with autografts compared with allografts for revision ACLR. 14 –17,23,24 The MARS group showed that the use of autografts for revision ACLR resulted in improved International Knee Documentation Committee scores, Knee injury and Osteoarthritis Outcome Score values in the Sport and Recreation and Quality of Life subscales, and 2-year Marx scores compared with use of allografts. 15 The authors also found that patients undergoing revision ACLR with an autograft were 2.8 times less likely to sustain a subsequent graft rupture compared with those with an allograft. 15 A follow-up study by the MARS group showed that autografts had a decreased risk of graft failure compared with allografts at 6-year follow-up. 14 This was supported by one study that showed that recurrent graft failures requiring multiple revision ACLR procedures are associated with the use of allografts for the first revision compared to single graft failures in which autografts are predominant. 23
A recent study evaluating factors that influence graft choice concluded that the revising surgeon had the largest effect on graft choice. The authors showed that if the prior graft type was an autograft, then an allograft was 3.6 times more likely to be chosen for revision. 16 These findings conflict with those of the current study, as a significant difference was seen in the graft type used at the time of primary ACLR, with allografts more commonly used in patients undergoing revision by low-volume compared with high-volume surgeons; nonetheless, an autograft was used more commonly by high-volume surgeons in the revision setting. The approach to revision ACLR is controversial and surgeon dependent but should be tailored to the patient while taking into account risks for revision ACLR failure. Finally, our study results are consistent with a recent report that QT autografts are becoming increasingly used for revision ACLR. 22
While all revision ACLR procedures in a single health care system were included in this study, these results may not be generalizable to patients in other practice settings. The categorization of surgeon volume was determined based on the literature, but it is unknown what the clinically relevant thresholds are for surgeon ACLR volume. This study only considered surgeon volume but did not account for surgeon experience, which may play a role in the treatment approach to revision ACLR. Additionally, this study did not evaluate variables such as age at the time of primary ACLR and its association with ACLR failure or postoperative outcomes after revision ACLR, which was beyond the scope of this study. Last, there may be other confounding factors that have not been assessed, as factors for ACLR graft failure are numerous.
Conclusion
In this registry study of an integrated health care system, high-volume surgeons were more likely to perform revision ACLR on patients with higher activity and competition levels. Additionally, high-volume surgeons more commonly performed staged revision ACLR, chose meniscus-sparing surgery, and favored the use of autografts over allografts compared with low-volume surgeons. In value-based health care, these data may be used to allow targeted interventions with the aim of improving clinical outcomes in patients undergoing ACLR.
Footnotes
Final revision submitted February 16, 2022; accepted March 31, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: J.D.H. has received grant support from Arthrex; education payments from Mid-Atlantic Surgical Systems, Pylant Medical, and Smith & Nephew; and hospitality payments from SI-BONE. V.M. has received consulting fees from Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of Pittsburgh (No. 19030196).
References
- 1. Borchers JR, Kaeding CC, Pedroza AD, et al. Intra-articular findings in primary and revision anterior cruciate ligament reconstruction surgery: a comparison of the MOON and MARS study groups. Am J Sports Med. 2011;39(9):1889–1893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Erickson BJ, Cvetanovich GL, Frank RM, Riff AJ, Bach BRJ. Revision ACL reconstruction: a critical analysis review. JBJS Rev. 2017;5(6):e1. [DOI] [PubMed] [Google Scholar]
- 3. Granan L-P, Bahr R, Steindal K, Furnes O, Engebretsen L. Development of a national cruciate ligament surgery registry: the Norwegian National Knee Ligament Registry. Am J Sports Med. 2008;36(2):308–315. [DOI] [PubMed] [Google Scholar]
- 4. Inacio MCS, Paxton EW, Maletis GB, et al. Patient and surgeon characteristics associated with primary anterior cruciate ligament reconstruction graft selection. Am J Sports Med. 2011;40(2):339–345. [DOI] [PubMed] [Google Scholar]
- 5. Jain N, Pietrobon R, Guller U, et al. Effect of provider volume on resource utilization for surgical procedures of the knee. Knee Surg Sports Traumatol Arthrosc. 2005;13(4):302–312. [DOI] [PubMed] [Google Scholar]
- 6. Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, Spindler KP. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43(7):1583–1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Leroux T, Wasserstein D, Dwyer T, et al. The epidemiology of revision anterior cruciate ligament reconstruction in Ontario, Canada. Am J Sports Med. 2014;42(11):2666–2672. [DOI] [PubMed] [Google Scholar]
- 8. Li LT, Boskshan SL, DeFroda SF, et al. High case volume predicts greater odds of autograft use and meniscal repair for anterior cruciate ligament reconstruction. Arthroscopy. Published online August 21, 2020. doi: 10.1016/j.arthro.2020.08.011 [DOI] [PubMed] [Google Scholar]
- 9. Lind M, Lund B, Fauno P, et al. Medium to long-term follow-up after ACL revision. Knee Surg Sports Traumatol Arthrosc. 2012;20(1):166–172. [DOI] [PubMed] [Google Scholar]
- 10. Lind M, Menhert F, Pedersen AB. Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the Danish registry for knee ligament reconstructions. Am J Sports Med. 2012;40(7):1551–1557. [DOI] [PubMed] [Google Scholar]
- 11. Lyman S, Koulouvaris P, Sherman S, et al. Epidemiology of anterior cruciate ligament reconstruction: trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am. 2009;91(10):2321–2328. [DOI] [PubMed] [Google Scholar]
- 12. Magnussen RA, Trojani C, Granan L-P, et al. Patient demographics and surgical characteristics in ACL revision: a comparison of French, Norwegian, and North American cohorts. Knee Surg Sports Traumatol Arthrosc. 2015;23(8):2339–2348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. MARS Group. Descriptive epidemiology of the Multicenter ACL Revision Study (MARS) cohort. Am J Sports Med. 2010;38(10):1979–1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. MARS Group. Effect of graft choice on the 6 year outcome of revision anterior cruciate ligament reconstruction in the Multicenter ACL Revision Study (MARS) cohort. Orthop J Sports Med. 2019;7(7)(suppl 5):2325967119S2325900281. [Google Scholar]
- 15. MARS Group. Effect of graft choice on the outcome of revision anterior cruciate ligament reconstruction in the Multicenter ACL Revision Study (MARS) cohort. Am J Sports Med. 2014;42(10):2301–2310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. MARS Group. Factors influencing graft choice in revision anterior cruciate ligament reconstruction in the MARS group. J Knee Surg. 2016;29(6):458–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rahardja R, Zhu M, Love H, et al. Effect of graft choice on revision and contralateral anterior cruciate ligament reconstruction: results from the New Zealand ACL Registry. Am J Sports Med. 2020;48(1):63–69. [DOI] [PubMed] [Google Scholar]
- 18. Schairer WW, Marx RG, Dempsey B, Ge Y, Lyman S. The relation between volume of ACL reconstruction and future knee surgery. Orthop J Sports Med. 2017;5(7)(suppl 6):2325967117S2325900298. [Google Scholar]
- 19. Scott DJ, Sherman S, Dhawan A, et al. Quantifying the economic impact of provider volume through adverse events: the case of sports medicine. Orthop J Sports Med. 2015;3(3):2325967115574476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Spindler KP. The Multicenter ACL Revision Study (MARS): a prospective longitudinal cohort to define outcomes and independent predictors of outcomes for revision anterior cruciate ligament reconstruction. J Knee Surg. 2007;20(4):303–307. [DOI] [PubMed] [Google Scholar]
- 21. Sutherland K, Clatworthy M, Chang K, Rahardja R, Young SW. Risk factors for revision anterior cruciate ligament reconstruction and frequency with which patients change surgeons. Orthop J Sports Med. 2019;7(11):2325967119880487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Winkler PW, Vivacqua T, Thomassen S, et al. Quadriceps tendon autograft is becoming increasingly popular in revision ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2022;30(1):149–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Winkler PW, Wagala NN, Hughes JD, Lesniak BP, Musahl V. A high tibial slope, allograft use, and poor patient-reported outcome scores are associated with multiple ACL graft failures. Knee Surg Sports Traumatol Arthrosc. 2022;30(1):139–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wright RW, Magnussen RA, Dunn WR, Spindler KP. Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: a systematic review. J Bone Joint Surg Am. 2011;93(12):1159–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wyatt RW, Inacio MC, Liddle KD, Maletis GB. Factors associated with meniscus repair in patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41(12):2766–2771. [DOI] [PubMed] [Google Scholar]