Abstract
The study was conducted to identify the impact of the pandemic on hypertensive older people’s COVID-19 fear, blood pressure control, and medication adherence. In this descriptive, correlational study, mean medication adherence was taken as 45.6 ± 6.06% based on the literature, with a 5% margin of error, and the sample size was determined as 292 with 95% confidence interval and 80% power. Data were collected from 419 older individuals using a sociodemographic information form, an infodemic-related questionnaire, Fear of COVID-19 Scale, and Medication Adherence Self-Efficacy Scale via Google Forms. The data were analyzed using IBM SPSS Statistics 23 software via independent sample t test, one-way variance analysis, χ2 analysis, and the Pearson correlation coefficient. It was found that, rather than avoiding hospitals during a pandemic, one out of two older people had had their blood pressure checked. One out of every five had abnormal/uncontrolled blood pressure during the pandemic. The infodemic was found to increase concern levels, and those with high fear scores had abnormal/uncontrolled levels of blood pressure. Moreover, a low-level positive correlation was found between medication adherence and the level of fear of COVID-19. As the pandemic continues, older people with hypertension need support in terms of monitoring blood pressure and medication adherence as well as increased awareness about the pandemic.
Subject terms: Diseases, Cardiovascular diseases
Introduction
Hypertension is a major public health issue with a global incidence rate of 40.8% and 32.3% control rate [1]. Its prevalence in Turkey is reported as 31.8%. This rate increases with age, reaching 75% for those 65 and older [2]. One of the most important elements of hypertension management and control is medication adoption. The blood pressure control rate in Turkey and the world is around 25% [3]. Geriatric monitoring for antihypertensive medication adoption and blood pressure is crucial for older people with hard-to-control hypertension.
The World Health Organization declared the COVID-19 outbreak a pandemic on March 11, 2020. The COVID-19 pandemic also gave rise to what is now called an “Infodemic”, or “an outbreak of misinformation”, on a global scale [4]. A great deal of inaccurate information related to the pandemic spread through social media [5]. Spreading faster than the actual virus, this misinformation adversely affected people’s knowledge about COVID-19; fear-inducing misinformation spread much more rapidly than accurate information [4, 5]. The infodemic and the spread of misleading and inaccurate information have had the greatest negative impact on people 65 and older, who are more likely to have chronic illnesses and have a greater COVID-19 mortality rate [6].
In Turkey, the perception that older people, who are in the high-risk group, were somehow “more dangerous” became spread, which spurred an increase in the fear and anxiety around the pandemic. On March 21, 2020, Turkey instated a curfew for people 65 and older to keep the mortality rates, low limiting the time they were allowed to leave their residences [7]. This practice had especially detrimental effects on those older individuals with hypertension due to isolation at home, physical inactivity, fear of receiving healthcare services, and lack of access to medication [8]. The accompanying infodemic caused additional anxiety in hypertensive patients, resulting in a persistent negative impact on adherence to medication and treatment. It is well-reported that regular check-ups, regular use of medication, and lifestyle are essential for managing blood pressure [9, 10]. The infodemic could lead older people to avoid seeking healthcare services and therefore to uncontrolled blood pressure.
Considering that non-adherence to hypertensive medication was a serious problem among older people even in pre-pandemic times [11, 12], it makes sense that the pandemic could have exacerbated these issues [8, 10]. The literature contains many studies on the adherence of older people to antihypertensive medication in the world [9–11] and in Turkey [12, 13]. However, there seem to be no studies on the effect of the COVID-19 infodemic on hypertensive older people and their blood pressure control and adherence to medication, to the best of our knowledge. Therefore, this study was carried out on hypertensive older people to investigate the effect of the pandemic on their fear of this novel disease, blood pressure control, and medication adherence.
Study questions
Has the COVID-19 pandemic caused fear of COVID-19?
Does fear of COVID-19 impact medication adherence in older people?
Methods
Study design
This study was designed as a descriptive, correlational study. Pandemic conditions precluded interviewing older people face to face, so announcements were made on social media and other platforms to reach a study group through snowball sampling. In the study, older people’s medication adherence self-efficacy levels were taken as a reference to determine the sample size [14]. The medication adherence mean was taken as 45.6 ± 6.06% based on the literature, with a 5% margin of error, and the sample size was determined as 292 with a 95% confidence interval and 80% power. Following the call for subjects, data were collected from 419 older people by using Google forms. Following the post hoc power analysis carried out after the study, the sample power was found as 100%. In Turkey, 19.8% of older people use the internet [15]. Therefore, the subjects were local older individuals found by snowball sampling and to whom the public health nursing students had access during their practice. These subjects were either internet users themselves or had internet access through the assistance of family or friends. They were reached through students who had older relatives and who wished to participate by filling out the online form. The link to the form was shared on social media and texted to participants upon request. This minimized selection bias. The data collection took place between October and December 2020.
Data collection tools
The study data were collected using the sociodemographic data form prepared by the researchers based on the literature, a questionnaire about the infodemic, the fear of COVID COVID-19 Scale, and Medicine Adherence Self-Efficacy Scale.
Sociodemographic data form
The form consists of a total of 12 questions to determine the sociodemographic characteristics of older people. The questions concern cover age, education level, sex, marital status, presence of chronic illness, as well as details about hypertension such as hypertension treatment, monitoring, healthcare center visits, and the like. The older individuals were asked whether they checked their blood pressure themselves at home during the pandemic, and whether their blood pressure was within normal limits (controlled) at the time; thus, they answered this question retrospectively. The participants were asked seven questions to determine their level of concern and the effects of news about COVID-19 on blood pressure control, any visits to the hospital, and their hypertension. The older people were requested to assign a number between 1 and 10 to their fear in order to identify whether COVID-19 news affected them. Higher scores indicate greater anxiety.
Fear of COVID-19 Scale
In 2020, Ahorsu et al. developed this scale to measure individuals’ level of fear of COVID-19 [16]. The scale was checked for validity and reliability in Turkey the same year by Satıcı et al. [17]. The minimum and maximum scores possible on the scale are 7 and 35, respectively. The scale consists of seven Likert-type questions from 1 to 5 (1: “I completely disagree” to 5: “I completely agree”). Scoring high on the scale indicates a high level of fear of COVID-19. The investigation of the reliability results of the Fear of COVID-19 Scale in this study revealed the Cronbach alfa coefficient as 0.87. The average of the Fear of COVID-19 Scale scores was found as 22.7 ± 6.7 (7–35).
Medication Adherence Self-Efficacy Scale-Short Form (MASES-SF)
Developed in 2003 by Ogedegbe et al. to identify the level of self-efficacy in adherence to medication, this scale was revised and examined by Fernandez et al. (2008) for validity and reliability [16, 18, 19]. In Turkey, work on the validity and reliability of the scale was carried out by Hacıhasanoğlu et al. in 2012 [20]. Scoring on the scale is between 1 and 4, the lowest possible score being 13, and the highest 52. A higher score indicates greater adherence to medication. In this study, the reliability coefficient of the scale was found as 0.92, which is quite high. The average score of the participants on the Medication Adherence Self-Efficacy Scale (MASES) was 39.53 ± 8.77 (13.00–52.00).
Data analysis
The data were analyzed using IBM SPSS Statistics 23 software. During the examination of the study data, frequencies were used for the categorical variables (number, percentage), and descriptive statistics (mean, standard deviation) were used for the quantitative variables. The normality assumption of the quantitative variables was examined using the Kolmogorov–Smirnov normality test, which revealed a normal distribution. Therefore, parametric statistical methods were used in this study. The differences between the two independent groups were examined using the independent sample t test. Any differences between more than two independent groups were investigated using one-way variance [ANOVA]. The Tukey test was used in cases where the one-way ANOVA resulted in a difference, to identify which group was the source of the difference. The correlation between independent quantitative variables was interpreted using the Pearson correlation coefficient. The correlation between two independent categorical variables was checked using χ2 analysis. The statistical significance level in the analyses was set at 0.05.
Results
Descriptive characteristics of the participants
The average age of the participants was 70.33 ± 6.93, 67.5% were women, 41.3% had a primary school level of education, 80.4% were married, and 49.9% were living with extended family. While 29.6% of the older people had had hypertension for at least 15 years, 62.5% did not have any chronic illnesses apart from hypertension. Of the older people using antihypertensive medication, 44.6% were on one medication while 21.6% were on at least three (Table 1).
Table 1.
The distribution of the variables regarding the pandemic for older people (n = 419).
| Number | Percentage | |
|---|---|---|
| Age (years) | ||
| ≤65 | 52 | 12.4 |
| 66–74 | 277 | 66.1 |
| ≥75 | 90 | 21.5 |
| Sex | ||
| Femalea | 74 | 27.2 |
| Male | 198 | 72.8 |
| Had blood pressure checked during pandemic | ||
| Yes | 246 | 58.7 |
| No | 173 | 41.3 |
| Visited a hospital during pandemic | ||
| Yes | 280 | 66.8 |
| No | 139 | 33.2 |
| Change in blood pressure during pandemic | ||
| No change | 155 | 37.0 |
| Normal levels, controlled | 186 | 44.4 |
| Abnormal levels/uncontrolled | 78 | 18.6 |
| Changed dosage or timing of antihypertensive medication without consulting a doctor | ||
| Yes | 65 | 15.5 |
| No | 354 | 84.5 |
| How did COVID-19 affect hypertension | ||
| Positively | 34 | 8.1 |
| Negatively | 159 | 37.9 |
| Moderately | 226 | 53.9 |
| Awareness about the COVID-19 pandemic | ||
| Knows | 391 | 93.3 |
| Does not know | 28 | 6.7 |
| Awareness about the effects of the pandemic on their hypertension illness | ||
| Knows | 297 | 70,9 |
| Does not know | 122 | 29,1 |
| Awareness about the effects of the pandemic on health | ||
| Knows | 356 | 85.0 |
| Does not know | 63 | 15.0 |
| Source of Information (n = 356) | ||
| Internet | 31 | 8.7 |
| TV | 168 | 47.2 |
| People around them | 63 | 17.7 |
| Healthcare staff | 76 | 21.3 |
| Other | 18 | 5.1 |
| Whether news in the media/social media influenced their decision to have hypertension checked | ||
| Yes | 255 | 60.9 |
| No | 164 | 39.1 |
| Whether Coronavirus news on social media affected their blood pressure control | ||
| Yes | 206 | 49.2 |
| No | 213 | 50.8 |
| Whether coronavirus news caused health-related concerns | ||
| Concerned | 350 | 83.5 |
| Unconcerned | 69 | 16.5 |
aSome participants did not answer this question.
Among the participants, 58.7% reported having their blood pressure checked during the pandemic while 18.6% reported having abnormal/uncontrolled levels, and 15.5% had changed the timing or dosage of their medication without consulting a doctor. On a scale of 0 to 10, the average score for the concern older people felt as a result of news related to COVID-19 was found as 6.95 ± 2.52 (1–10). In the study, 37.9% reported having been affected negatively by the COVID-19 pandemic and 53.9% partially. The pandemic-related news on social media was observed to have impacted the hypertension control of 49.2% of the participants, while 83.5% were concerned for their health, and 85% stated they were aware of the health-related effects of the pandemic. Of those with such awareness, 47.2% reported receiving their information from the TV while 21.3% mentioned healthcare workers as the source of their information.
A statistically meaningful correlation was found between hypertension control and going to a hospital center, making changes to the medication dosage or timing without consulting a doctor, COVID-19 affecting hypertension, knowing the effects of COVID-19 on hypertension, and the news in the media/social media impacting the decision to get checked at a hospital during the pandemic (p < 0.05; Table 2). Thus, the blood pressure control rate was significantly higher in older people who went to a hospital during the pandemic, had their blood pressure checked, made a change in how they take their antihypertensive medication, and were aware of the effects of the pandemic on health.
Table 2.
The distribution of pandemic-related variables based on BP control.
| Whether they had BP checked during pandemic | χ2 | p | ||||
|---|---|---|---|---|---|---|
| Yes | No | |||||
| Number | Percentage | Number | Percentage | |||
| Visited a hospital during pandemic | ||||||
| Yes | 202 | 72.1 | 78 | 27.9 | 62.815 | 0.000* |
| No | 44 | 31.7 | 95 | 68.3 | ||
| Change in blood pressure during pandemic | ||||||
| No change | 71 | 45.8 | 84 | 54.2 | 17.449 | 0.000* |
| Normal levels/controlled | 126 | 67.7 | 60 | 32.3 | ||
| Abnormal levels/uncontrolled | 49 | 62.8 | 29 | 37.2 | ||
| Changed dosage/timing of antihypertensive medication without consulting a doctor | ||||||
| Yes | 48 | 73.8 | 17 | 26.2 | 7.270 | 0.007* |
| No | 198 | 55.9 | 156 | 44.1 | ||
| How did COVID-19 affect hypertension | ||||||
| Positively | 24 | 70.6 | 10 | 29.4 | 9.991 | 0.007* |
| Negatively | 105 | 66.0 | 54 | 34.0 | ||
| Moderately | 117 | 51.8 | 109 | 48.2 | ||
| Awareness about the COVID-19 pandemic | ||||||
| Knows | 229 | 58.6 | 162 | 41.4 | 0.050 | 0.824 |
| Does not know | 17 | 60.7 | 11 | 39.3 | ||
| Awareness about the effects of the pandemic on their hypertension | ||||||
| Knows | 185 | 62.3 | 112 | 37.7 | 5.388 | 0.020* |
| Does not know | 61 | 50.0 | 61 | 50.0 | ||
| Awareness about the effects of the pandemic on health | ||||||
| Knows | 222 | 62.4 | 134 | 37.6 | 13.000 | 0.000* |
| Does not know | 24 | 38.1 | 39 | 61.9 | ||
| Whether news in the media/social media influenced their decision to have hypertension checked | ||||||
| Yes | 176 | 69.0 | 79 | 31.0 | 28.559 | 0.000* |
| No | 70 | 42.7 | 94 | 57.3 | ||
| Whether Coronavirus news on social media affected their blood pressure control | ||||||
| Yes | 133 | 64.6 | 73 | 35.4 | 5.725 | 0.017* |
| No | 113 | 53.1 | 100 | 46.9 | ||
| Whether coronavirus news caused health-related concerns | ||||||
| Concerned | 205 | 58.6 | 145 | 41.4 | 0.017 | 0.896 |
| Unconcerned | 41 | 59.4 | 28 | 40.6 | ||
| Mean | SD | Mean | SD | t | p | |
| News about COIVD-19 concerns about hypertension | 6.83 | 2.59 | 7.13 | 2.42 | −1.208 | 0.228 |
*p < 0.05 (statistical significance).
Some characteristics of the participants related to fear of COVID-19 and medication commitment/adherence
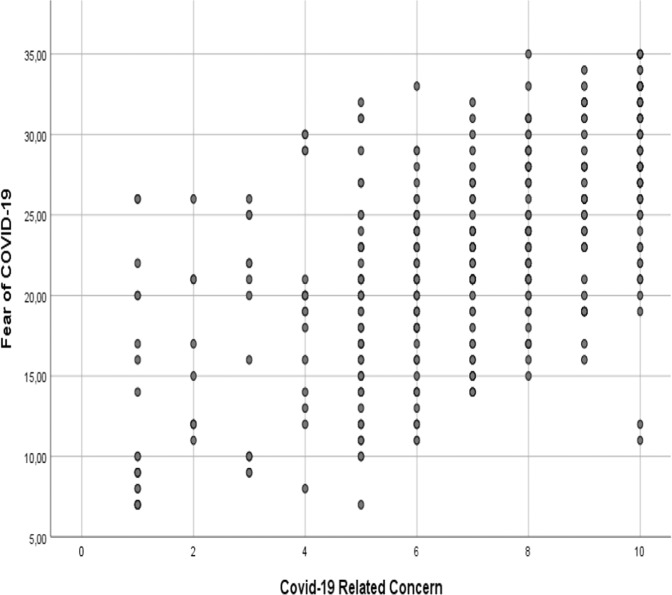
The Fear of COVID-19 Scale scores displayed statistically significant differences based on changes in blood pressure, changes in taking medication, how their hypertension was affected by COVID-19, whether news in the media/social media had an effect on whether they went to healthcare centers, and had their blood pressure checked or whether their hypertension was controlled, whether they were concerned about their health during the pandemic (p < 0.05, Table 3). Therefore, older people whose hypertension was uncontrolled, who made changes to their medication adherence, who did not seek check-up services due to the pandemic, and who were worried by pandemic-related news and its effect on their health were found to have meaningfully higher scores on the Fear of COVID-19 Scale. A moderately positive, statistically significant correlation was found between the Fear of COVID-19 Scale scores and the level of concern related to news of the virus and hypertension (r = 0.641, p < 0.05; Fig. 1).
Table 3.
The distribution of pandemic-related variables and Fear of COVID-19 Scale scores and Medication Adherence Self-Efficacy Scale average scores.
| Fear of COVID-19 Scale | Medication Adherence Self-Efficacy | |||||
|---|---|---|---|---|---|---|
| Mean | SD | Stat. analysis | Mean | SD | Stat. analysis | |
| Had blood pressure checked during pandemic | ||||||
| Yes | 22.88 | 6.50 | t = 0.509 | 39.94 | 8.39 | t = 1.137 |
| No | 22.54 | 7.07 | p = 0.611 | 38.95 | 9.29 | p = 0.256 |
| Visited a hospital during pandemic | ||||||
| Yes | 23.13 | 6.41 | t = 1.676 | 40.31 | 8.16 | t = 2.575 |
| No | 21.96 | 7.31 | p = 0.095 | 37.98 | 9.74 | p = 0.010* |
| Change in blood pressure during pandemic | ||||||
| No change | 21.63 | 7.16 | F = 8.348 | 38.62 | 9.35 | F = 2.005 |
| Normal levels/controlled | 22.56 | 6.33 | p = 0.000* | 40.47 | 8.32 | p = 0.136 |
| Abnormal levels/uncontrolled | 25.36 | 6.14 | 3–1.2 | 39.12 | 8.53 | |
| Changed dosage or timing of antihypertensive medication without consulting a doctor | ||||||
| Yes | 24.29 | 5.53 | t = 2.365 | 39.49 | 7.50 | t = −0.048 |
| No | 22.45 | 6.90 | p = 0.020* | 39.54 | 9.00 | p = 0.966 |
| How did COVID-19 affect hypertension | ||||||
| Positively | 23.50 | 6.67 | F = 22.185 | 39.50 | 9.31 | F = 0.120 |
| Negatively | 25.25 | 5.91 | p = 0.000* | 39.80 | 8.03 | p = 0.887 |
| Moderately | 20.85 | 6.72 | 2–3 | 39.35 | 9.22 | |
| Awareness about the COVID-19 pandemic | ||||||
| Knows | 22.76 | 6.67 | t = 0.309 | 39.88 | 8.61 | t = 3.015 |
| Does not know | 22.36 | 7.65 | p = 0.757 | 34.75 | 9.79 | p = 0.003* |
| Awareness about the effects of the pandemic on their hypertension | ||||||
| Knows | 22.61 | 6.66 | t = −0.607 | 39.92 | 8.52 | t = 1.414 |
| Does not know | 23.05 | 6.93 | p = 0.544 | 38.59 | 9.35 | p = 0.158 |
| Awareness about the effects of the pandemic on health | ||||||
| Knows | 22.53 | 6.58 | t = −1.475 | 39.90 | 8.65 | t = 2.027 |
| Does not know | 23.89 | 7.47 | p = 0.141 | 37.48 | 9.26 | p = 0.043* |
| Whether news in the media/social media influenced their decision to have hypertension checked | ||||||
| Yes | 23.35 | 6.50 | t = 2.330 | 39.80 | 8.48 | t = 0.772 |
| No | 21.79 | 6.99 | p = 0.020* | 39.12 | 9.23 | p = 0.441 |
| Whether Coronavirus news on social media affected their blood pressure control | ||||||
| Yes | 24.96 | 5.59 | t = 7.032 | 39.66 | 8.05 | t = 0.277 |
| No | 20.59 | 7.06 | p = 0.000* | 39.42 | 9.44 | p = 0.782 |
| Whether coronavirus news caused health-related concerns | ||||||
| Concerned | 23.75 | 6.02 | t = 6.217 | 40.31 | 8.32 | t = 4.176 |
| Unconcerned | 17.59 | 7.78 | p = 0.000* | 35.58 | 9.97 | p = 0.000* |
F one-way analysis of variance, t independent samples t test, Var variance (Tukey test).
*p < 0.05.
Bold characters ınclude statistically significant results.
Fig. 1.
Correlation between COVID-19-related concern and fear of COVID-19.
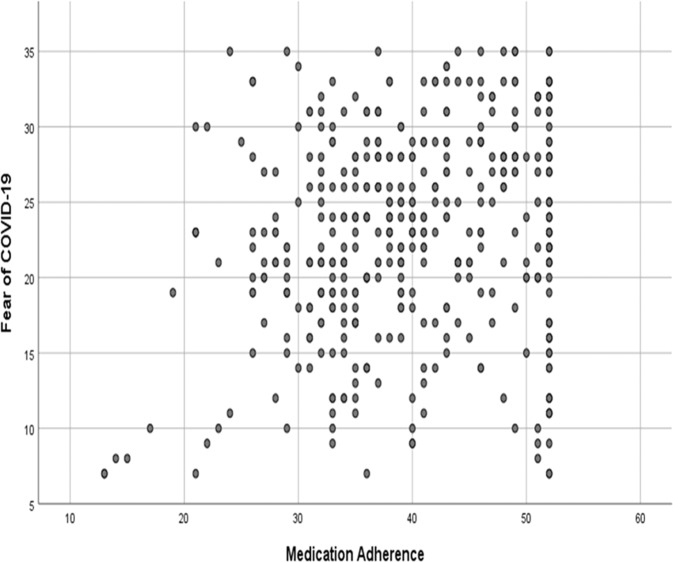
The MASES scores displayed statistically significant differences based on having gone to a hospital during the pandemic, being aware of the COVID-19 pandemic, knowing about the effects of COVID-19 on health, and being concerned for their health based on news about the coronavirus (p < 0.05). Accordingly, those who visited a hospital during the pandemic, those aware of the COVID-19 pandemic and its effects on health, and those concerned about their health were found to have meaningfully higher scores on the MASES scores. A statistically significant, low-level positive correlation was found between the MASES scores and the Fear of COVID-19 Scale scores (r = 0.196, p = 0.000; Fig. 2).
Fig. 2.
Correlation between fear of COVID-19 and medication adherence.
Discussion
The majority of the older people (85%) state that they became aware of the effects of the pandemic on health through the news on social media and are concerned about their health (83.5%). In a study by Wolf et al. (2020), it was found that adults in the US with chronic disease are concerned about becoming infected with the coronavirus (24.6%), and that nearly one-third are not able accurately to describe the symptoms (28.3%) or measures to prevent infection (32.0%) [21]. In another study, Aydın (2020) found that most or all of the news content broadcast in Turkey within a week after the first case was inaccurate or misleading [22]. The information pollution and misleading advice on social media was reported to have a potentially detrimental effect on public health, as it caused people to take up incorrect practices [4, 23]. In our study, the older people reported getting the majority of their news about the virus from TV, which shows that the media plays an important role in establishing a culture of fear around contagious diseases. Considering 35% percent of the older people in Turkey cannot read and write, which effectively restricts their access to accurate information from written sources, they are limited to audiovisual media as a source of information. Whether accurate or inaccurate, the information in the media is thought to heighten older people’s concerns related to the pandemic.
In this study, a positive correlation was found between news about the coronavirus and hypertensive older people’s level of anxiety about their illness as well as the level of their fear of COVID-19 (r = 0.641; p < 0.05). A study in China found that about 35% of people were psychologically impacted by the pandemic [24]. In Wang’s study, it was reported that fear of COVID-19 could even be a risk factor for suicidal tendencies among older individuals [25]. In their study, whose findings support ours, Doğan and Düzel (2020) found that 63.8% of their study participants stated the constant broadcast of virus-related news in the media heightened their fear of the disease, and adversely affected their mental state (60.4%) [26]. Our findings are similar to those found in the literature. The pandemic seems to have a negative impact on the older population’s concerns about their existing illnesses.
The Fear of COVID-19 Scale scores was meaningfully higher for older people who had abnormal/uncontrolled blood pressure, whose decision to get checked was affected by the news in the media/social media, and who changed their medication dosage or timing without consulting a doctor (p < 0.05). The hypertension treatment and control rates prior to the pandemic have been found to be lower in developing countries. Research shows that blood pressure control rates were 51.5% in Kenya [27], 49.7% in India, and 30% in Turkey [28, 29]. In our study, it was found that about one in every five older individuals (18.6%) had abnormal/uncontrolled blood pressure. News on social media that hypertension could increase vulnerability to COVID-19 and worsen the prognosis was reported to be a cause for concern [30, 31]. Even though evidence related to the correlation between hypertension and the progression of COVID-19 and the mortality rates is inconclusive [32], this continues to be a source of anxiety for patients. The infodemic on social media may have impacted the blood pressure levels of the older people in our study.
The literature shows that the COVID-19 pandemic has led to decreased numbers of visits to the outpatient centers in healthcare systems [33, 34]. In Baum’s study, a 56% fall was observed in the visits to clinics during the first 10 weeks of the pandemic compared to 10 weeks prior [34]. In their 2020 study, Alexander et al. also reported a 50.1% decrease in blood pressure assessments and 36.9% in cholesterol checks [35]. Another study found a decrease in the rate of patients seeking healthcare services due to myocardial infarctions [36]. Similar reports were made during the SARS outbreak regarding people avoiding hospitals for fear of becoming infected with the virus, and that the decrease in visiting patient rates remained low for the following 4 years [37]. The news of “older people dying/transmitting more”, which was overly age-focused, led to deep fear and feelings of isolation [5].
In our study, older people who visited healthcare centers during the pandemic, whether they had controlled or uncontrolled hypertension, who changed the timing or dosage of their medication without consulting their doctor, whose hypertension control was influenced by COVID-19-related social media, and who were knowledgeable about the effects of the pandemic on health were significantly more likely to have their blood pressure checked (p < 0.05, Table 2). Our study diverges from the literature with these findings. In our study, we found that the greater the fear felt by older individuals due to the pandemic, the greater the likelihood of visiting a hospital.
Another common reason for uncontrolled hypertension is a lack of medication adherence. Studies have found that concerns and beliefs about medication can affect the therapeutic doctor–patient relationship and medication/treatment adherence. Studies carried out using the MASES have found average scores varying between 27.62 ± 5.79 and 45.05 ± 6 [11–13]. In our study, the average MASES score among hypertensive older people was found as 39.53 ± 8.77 (13.00–52.00). The results of our study are within the range given above. In this study, a low-level positive correlation was found between fear of COVID-19 and medication adherence (r = 0.196; p = 0.000). Furthermore, older people who are aware of the COVID-19 pandemic and its effects on health, who are concerned for their health and who visited a hospital during the pandemic were found to have better medication adherence. This could imply that the infodemic about the pandemic and the resulting fear were factors increasing medication adherence.
Limitations
The subjects in the study were local older individuals to whom the public health nursing students had access during their practice. These subjects were either internet users themselves or had internet access through the assistance of family or friends. This is a limitation. Furthermore, older people’s adherence to medication was assessed using only the MASES-SF, and no other tool.
Conclusions
In our study, it was found that one out of every two older people had their blood pressure checked during the pandemic and that one out of every five older people had abnormal/uncontrolled blood pressure. It was also observed that the news on social media about the pandemic heightened the health-related concerns of most of the older people, that older people were aware of the effects of the pandemic on health, and that nearly half of those aware received their information from the TV. It was found that as the infodemic heightened older people’s concerns about their hypertension, their fear of COVID-19 level increased, and that older people with high fear of COVID-19 scores had abnormal/uncontrolled blood pressure levels. Furthermore, older people whose decision to get their health checked had been influenced by the news on media/social media had meaningfully higher scores on the Fear of COVID-19 Scale; those aware of COVID-19 and its effects on health, who were concerned for their health and visited a healthcare center were found to have better medication adherence. A low-level positive correlation was found between medication adherence and the fear of COVID-19.
Since older people could be exposed to misinformation impacting their hypertension control, physicians and nurses should offer information and education, as well as support via homecare teams especially for older people at home during the pandemic, on hypertension and medication adherence. Awareness should also be raised among older people about the infodemic. Since media sources frequently offer inaccurate information about chronic illnesses and health-related issues, it could be advisable to offer health literacy training geared toward older people.
Summary
What is known about this topic
It is established in the literature that older people have an increased level of fear of COVID-19. However, studies exploring the relationship between older individuals’ fear of COVID-19 and their medication adherence are rare.
What this study adds
This study contributes new information to the literature as a relationship is established between older people’s fear of COVID-19 and their adherence to medication.
The chronic illnesses older people experience are ones requiring constant monitoring. The limitations set in place by the government on older people and fear of contracting COVID-19 had a negative effect on medication adherence.
Acknowledgements
Thanks to all the researchers and participants in this study.
Author contributions
AÖ and İAA contributed to the study design. AÖ carried out the data collection. AÖ and İAA carried out the data analyses. AÖ and İAA were involved in the paper preparation. Both authors have read and approved the final paper.
Data availability
As per ethics approval, full interview transcripts are only available to the research team.
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Ethics committee approval was received from REDACTED University Non-invasive Research Ethics Committee (Number REDACTED). Written approval was received from the Ministry of Health Scientific Research Platform prior to data collection. An explanation preceded the questions in the survey to clarify the intent and content of the study, and to inform the prospective participant about the voluntary nature of their participation.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Chow CK, Teo KK, Rangarajan S, Islam S, Gupta R, Avezum A, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310:959–68. doi: 10.1001/jama.2013.184182. [DOI] [PubMed] [Google Scholar]
- 2.Alp Ç, Sarak T, Çiftçi A, Kabalcı M. Approach to hypertension in the elderly. TJCL. 2018;9:233–6. [Google Scholar]
- 3.Jankowska-Polańska B, Uchmanowicz I, Dudek K, Mazur G. Relationship between patient knowledge and medication adherence among patient with hypertension. Patient Prefer Adherence. 2016;10:2437–47. doi: 10.2147/PPA.S117269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O’Connor C, Murphy M. Going viral: doctors must tackle fake news in the covid-19 pandemic. BMJ. 2020;369:1587. doi: 10.1136/bmj.m1587. [DOI] [PubMed] [Google Scholar]
- 5.Garfin DR, Silver RC, Holman A. The novel coronavirus (COVID-2019) outbreak: amplification of public health consequences by media exposure. Health Psychol. 2020;39:355–7. doi: 10.1037/hea0000875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fingerman KL, Pillemer K. Continuity and changes in attitudes, health care, and caregiving for older adults during the COVID-19 pandemic. J Gerontol B Psychol Sci Soc Sci. 2021;76:e187–9. doi: 10.1093/geronb/gbaa231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gencer N. Being elderly in covid-19 process: evaluations on curfew for 65-year-old and over citizens and spiritual social work. TJSWR. 2020;4:35–42. [Google Scholar]
- 8.Ferdinand KC, Vo TN, Echols MR. State-of-the-art review: hypertension practice guidelines in the era of COVID-19. Am J Prev Cardiol. 2020;2:10038. doi: 10.1016/j.ajpc.2020.100038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fang J, Chang T, Wang G, Loustalot F. Association between cost-related medication nonadherence and hypertension management among US adults. Am J Hypertens. 2020;33:879–86. doi: 10.1093/ajh/hpaa072. [DOI] [PubMed] [Google Scholar]
- 10.Tajeu GS, Muntner P. Cost-related antihypertensive medication nonadherence: action in the time of COVID-19 and beyond. Am J Hypertens. 2020;33:816–8. doi: 10.1093/ajh/hpaa085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lo SH, Chau JP, Woo J, Thompson DR, Choi KC. Adherence to antihypertensive medication in older adults with hypertension. Eur J Clin Nutr. 2016;31:296. doi: 10.1097/JCN.0000000000000251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Öztaş Ö, Korkmaz GA. The elderly medication use behaviors that cause medication non-compliance and ıts association with their health literacy levels. HUHEMFAD. 2019;6:132–40. doi: 10.31125/hunhemsire.630763. [DOI] [Google Scholar]
- 13.Demirtürk E, Aşılar RH. The effect of depression on adherence to antihypertensive medications in elderly individuals with hypertension. J Vasc Nurs. 2018;36:129–39. doi: 10.1016/j.jvn.2018.06.001. [DOI] [PubMed] [Google Scholar]
- 14.Özdemir Ö, Akyüz A, Doruk H. Compliance with drug treatment in geriatric patients with hypertension. Med J Bakırköy. 2016;12:195–201. [Google Scholar]
- 15.Göker H, Tekedere H, Arpacı F. Analysis of the relationship between loneliness perceptions and social media usage among elderly living at home. Third Sect Soc Economic Rev. 2020;55:1631–44. [Google Scholar]
- 16.Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The Fear of COVID-19 Scale: development and initial validation. Int J Ment Health Addict. 2022;20:1537–45. [DOI] [PMC free article] [PubMed]
- 17.Satici B, Gocek-Tekin E, Deniz ME, Satici SA. Adaptation of the Fear of COVID-19 Scale: its association with psychological distress and life satisfaction in Turkey. Int J Ment Health Addict. 2021;19:1980–88. [DOI] [PMC free article] [PubMed]
- 18.Ogedegbe G, Mancuso CA, Allegrante JP, Charlson ME. Development and evaluation of Medication Adherence Self-Efficacy Scale in hypertensive African–American patients. J Clin Epidemiol. 2003;56:520–9. doi: 10.1016/S0895-4356(03)00053-2. [DOI] [PubMed] [Google Scholar]
- 19.Fernandez S, Chaplin W, Schoenthaler AM, Ogedegbe G. Revision and validation of the Medication Adherence Self-Efficacy Scale (MASES) in hypertensive African Americans. J Behav Med. 2008;31:453–62. doi: 10.1007/s10865-008-9170-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hacihasanoglu R, Gözüm S, Çapik C. Validity of the Turkish version of the Medication Adherence Self-Efficacy Scale-short form in hypertensive patients. Anatol J Cardiol. 2012;12:241–8. doi: 10.5152/akd.2012.068. [DOI] [PubMed] [Google Scholar]
- 21.Wolf MS, Serper M, Opsasnick L, O’Conor RM, Curtis L, Benavente JY, et al. Awareness, attitudes, and actions related to COVID-19 among adults with chronic conditions at the onset of the U.S. outbreak: a cross-sectional survey. Ann Intern Med. 2020;173:100–9. doi: 10.7326/M20-1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aydin AF. Disinformation in social media in post-truth period: the covid-19 (new coronavirus) pandem process. Asya Stud. 2020;4:76–90. doi: 10.31455/asya.740420. [DOI] [Google Scholar]
- 23.Evanega, S., Lynas, M., Adams, J. & Smolenyak, K. Coronavirus misinformation: quantifying sources and themes in the COVID-19 ‘infodemic’ JMIR Preprints. 19/10/2020:25143.
- 24.Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020;33:e100213. doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Env Res Pub. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Doğan MM, Düzel B. Fear-anxiety levels in Covid-19. Turkish Stud. 2020;15:739–52. [Google Scholar]
- 27.Mohamed SF, Mutua MK, Wamai R, Wekesah F, Haregu T, Juma P, et al. Prevalence, awareness, treatment and control of hypertension and their determinants: results from a national survey in Kenya. BMC Public Health. 2018;18:1–10. doi: 10.1186/s12889-017-4524-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jose AP, Prabhakaran D. World hypertension day: contemporary issues faced in India. Indian J Med Res. 2019;149:567–70. doi: 10.4103/ijmr.IJMR_549_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dastan I, Erem A, Cetinkaya V. Awareness, treatment, control of hypertension, and associated factors: results from a Turkish national study. Clin Exp Hypertens. 2018;40:90–98. doi: 10.1080/10641963.2017.1334797. [DOI] [PubMed] [Google Scholar]
- 30.Lau D, McAlister FA. Implications of the COVID-19 pandemic for cardiovascular disease and risk-factor management. Can J Cardiol. 2020;37:722–32. doi: 10.1016/j.cjca.2020.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Love JS, Blumenberg A, Horowitz Z. The parallel pandemic: medical misinformation and COVID-19: Primum non nocere. J Gen Intern Med. 2020;35:2435–6. doi: 10.1007/s11606-020-05897-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mancia G, Rea F, Ludergnani M, Apolone G, Corrao G. Renin–angiotensin–aldosterone system blockers and the risk of Covid-19. N Engl J Med. 2020;382:2431–40. doi: 10.1056/NEJMoa2006923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hartnett KP, Kite-Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J, et al. Impact of the COVID-19 pandemic on emergency department visits – United States, January 1, 2019–May 30, 2020. Morb Mortal Wkly Rep. 2020;69:699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Baum A, Kaboli PJ, Schwartz MD. Reduced in-person and increased telehealth outpatient visits during the COVID-19 pandemic. Ann Intern Med. 2021;174:129–31. doi: 10.7326/M20-3026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alexander GC, Tajanlangit M, Heyward J, Mansour O, Qato DM, Stafford RS. Use and content of primary care office-based vs telemedicine care visits during the COVID-19 pandemic in the US. JAMA. 2020;3:1–11. doi: 10.1001/jamanetworkopen.2020.21476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Solomon MD, McNulty EJ, Rana JS, Leong K, Lee C, Sung SH, et al. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383:691–3. doi: 10.1056/NEJMc2015630. [DOI] [PubMed] [Google Scholar]
- 37.Chu D, Chen RC, Ku CY, Chou P. The impact of SARS on hospital performance. BMC Health Serv Res. 2008;8:1–6. doi: 10.1186/1472-6963-8-228. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
As per ethics approval, full interview transcripts are only available to the research team.