Abstract
Background
Ethical decision-making confidence develops from clinical expertise and is a core competency for nurse leaders. No tool exists to measure confidence levels in nurse leaders based upon an ethical decision-making framework.
Aims
The objective of this research was to compare ethical decision-making among nurse leaders in the U.S. and three German-speaking countries in Europe by developing and testing a newly constructed Ethical Decision-Making Confidence (EDMC) scale.
Methods
The cross-sectional survey included 18 theory-derived questions on ethical decision-making confidence which were used to develop the scale.
Participants
A convenience sample of nurse leaders from the U.S. and three German-speaking countries in Europe who self-identified as holding a leadership position.
Ethical Considerations
Ethical approval was given by the IRB Board of a U.S. university. Participation in the survey implied voluntary consent.
Results
The scale’s item structure dimensionality and subscale’s reliability were analyzed and compared between nurse leaders from all four countries. A principal component analysis (PCA) produced a 15-item bi-dimensional EDMC scale yielding a skill-related (9-item) and a behavior-related (6-item) confidence dimension. EDMC subscales showed good-to-excellent internal consistency. In both subscales, U.S. nurse leaders rated their mean EDMC score higher than their German-speaking counterparts in Europe.
Discussion
This exploratory study is the first of its kind to focus on nurse leaders’ confidence regarding ethical decision-making in an international context. An overarching factor structure was identified, which is shared by the two samples of nurse leaders and to examine (sub)scales’ psychometric properties.
Conclusion
This newly developed scale is an effective tool for measuring ethical decision-making confidence in nurse leaders. The promising results of this study should be replicated to ensure validity and reliability of the EDMC scale measuring skill-related and behavior-related concepts and include nurse leaders from various cultural, social, and demographic groups.
Keywords: moral distress, professional ethics, ethics and leadership/management, moral/ethical climate of organizations, moral sensitivity
Introduction
This article describes the development and psychometric evaluation of an Ethical Decision-Making Confidence (EDMC) scale for nurse leaders. In this study, the scale was used to measure and compare the EDMC of nurse leaders from the U.S. and three German-speaking European countries. Unlike scenario-based ethical cases used in other social sciences, this scale offers bi-dimensionality that yields both skill- and behavior-related dimensions.
Background
Ethical issues occur frequently in today’s complex healthcare settings. Nurse leaders, whether involved in direct patient care or administrative roles, are impacted by challenging ethical cases. While the literature offers innumerable publications focusing on moral distress and ethical decision-making competence in nurses,1–6 there is very little written specifically on nurse leaders. It is postulated that nurse leaders must be competent in ethical decision-making to successfully maneuver today’s healthcare setting which includes managing advances in technology, practicing within economical constraints that often appear diametrically opposed to delivering quality patient care, and facing complex ethical situations.
Much like the hands-on skills nurses need to master in order to deliver safe quality patient care, nurses must also develop the skills necessary to effectively advocate for their patients. Like hands-on skills, soft-skills such as self-management and interpersonal relationships 7 need to be developed and mastered so that nurses possess ethical confidence when facing ethically challenging patient situations. 8 Building on these skills, nurse leaders have the additional responsibility to be a resource, preceptor, mentor, and role model for their peers and charges. Stanley and Stanley 9 offer a global definition of the nurse leader; specifically, “[t]hey are found across the spectrum of health organizations, often at the highest level for clinical interaction, but not commonly at the highest management level.” p. 1730. As such, nurse leaders provide direction and support, motivate, coordinate, demonstrate critical and reflective thinking skills, apply intra- and interdisciplinary peer supervision, act as the liaison to and effectively communicate with other departments in interdisciplinary care, among many others.10,11 The position of a nurse leader includes, but is not limited to, nurse practitioners, clinical nurse specialists, nurse executives, chief nursing officers, and head nurses.
Confidence can best be defined as a quality or state of being certain and this certainty results from having faith or belief in one’s powers and a willingness and/or ability to act. 12 It is also important to acknowledge that confidence is not an absolute. Rather, confidence occurs along a continuum and is situational, being influenced by both the situation and task required, and is driven by a conviction to overcome obstacles allowing one to do what is perceived as right. 13 Ethical decision-making confidence develops from clinical expertise and is a core competency for nurse leaders which allows them to effectively manage hierarchical challenges, model interprofessional communications, 14 and advocate for multi-professional consensus in difficult ethical situations.
Founded on the premise that self-confidence is not an absolute, to assess the participants’ confidence in their ethical decision-making competencies, the EDMC Scale was developed using the Phases of Development of Core Competency for Ethical Decision-Making by Hamric and Delgado. 14 The phases of competency are Phase 1: Knowledge Development—Moral Sensitivity, Phase 2: Knowledge Application, Phase 3: Creating an Ethical Environment, and Phase 4: Promoting Social Justice Within the Health Care System. 11 Described as an evolutionary process, the framework is designed to instill foundational concepts in Phases 1 and 2, while Phases 3 and 4 position the nurse to lead and enact ethical decision-making in the healthcare setting. In each phase of the ethical decision-making competency framework, specific knowledge and correlating skills or behaviors are identified. 14
The authors were unable to locate other published ethical decision-making scales designed to measure confidence levels in nurse leaders based upon an ethical decision-making framework. Data base searches were conducted using the terms “nursing,” “nurs* leader,” “ethical decision-making,” “ethical decision-making confidence,” and “ethical decision-making scale”. One study published in 1989 utilized an investigator-designed “Nursing Ethical Decision-Making Scale” for neonatal nurses, without publishing the scale itself. 15 Other publications revealed scales that were developed by other professions including counseling 16 and business management. 17 However, unlike self-assessed confidence, these scales focus on evaluating actions and responsibilities specific to ethical violations.17–19
Aims
As part of a larger study investigating moral distress reported by nurse leaders, the aims of this exploratory study were (a) to develop a tool to measure EDMC of nurse leaders, (b) evaluate its psychometric properties between nurse leaders from the U.S. and three German-speaking European countries, and finally (c) compare nurse leaders’ EDMC in participating countries.
Methods
Design, participants, and data collection
The study design was a cross-sectional online survey. The online survey was implemented using the Qualtrics survey platform. The convenience sample included nurse leaders who self-identified as holding a leadership position (see demographics table) and were from the U.S. and three German-speaking European countries (Germany-DE, Austria-AT, and Switzerland-CH). Supported by an academic affiliation between a U.S. and an Austrian university, the U.S. author initiated making this an international project to compare moral distress in nurse leaders. Recruitment was done using professional nursing organization listservs. U.S. participants were solicited through the national Doctor of Nursing Practice (DNP) Association. 20 German-speaking German, Swiss, and Austrian nurse leaders belonging to professional nursing organizations in their country received an e-invitation facilitated by the European Principal Investigator. Twenty-three European nursing organizations disseminated the survey: Germany (7), Austria (6), Switzerland (10). The geographic variations in practice settings, educational levels, and nurse leader titles and roles, prohibited access to any national figures. Furthermore, it cannot be estimated how many members within each nursing organization would self-report as being in a leadership role.
The e-invite outlined the study and contained an embedded hyperlink and QR code for ease of access to the Qualtrics survey. Participation in the survey was voluntary and participant’s anonymity was ensured in compliance with current data privacy regulations. The survey remained open from May 2018 to September 2018.
Scale development and survey items
The skills and behaviors derived from Hamric and Delgado’s 14 phases of competency were used to construct the 18-item EDMC Scale. Specifically, Phase 1 is focused on the development of foundational ethical knowledge, skills and cognitive mastery which are represented in questions 1–6 of the EDMC scale. Still foundational, Phase 2 is focused on the application of knowledge through the use of correct ethical language and decision-making frameworks which is reflected in questions 7–11. Phase 3 (questions 12–16) advances the ethical influence to improve the healthcare environment through mentoring, role modeling, and preventative ethics. The final two questions (questions 17 and 18) on the EDMC Scale integrate Phase 4 competencies of social justice, advocacy, and policy reform that take place beyond one’s institution. Applying a five-point Likert-type scale, the participants rated their confidence specific to the ethical skill or behavior from 1-very low to 5-very high per item. (Table 1)
Table 1.
Items of the applied ethical decision-making confidence scale.
| Items (“Please rate your confidence in your ability to…”) |
|---|
| 1. Recognize a genuine ethical dilemma in practice |
| 2. Make a sound ethical decision |
| 3. Explain your ethical decisions using correct ethical terminology and language |
| 4. Provide a clear statement of the personal values that guide your ethical decision-making and practice |
| 5. Articulate legal guidelines related to complex ethical issues in patient care (i.e., assisted suicide, informed consent, research involving minors) |
| 6. Articulate the difference between ethical dilemmas, moral distress, issues related to interprofessional collaboration and communication, difficult patients, etc. |
| 7. Articulate the definition of moral distress and provide an example of your experience of moral distress in your practice |
| 8. Identify ethical issues in complex patient care (i.e., identify scenarios requiring ethical decision-making and/or ethical consult team guidance |
| 9. Apply ethical decision-making models or structured processes to complex clinical problems |
| 10. Participate in and/or guide mediation related to complex clinical problems involving ethical dilemmas or moral distress |
| 11. Recognize and manage moral distress in self and others |
| 12. Role model collaborative problem solving in complex clinical problems involving ethical dilemmas or moral distress |
| 13. Engage in preventative ethics initiatives to address the ethical environment in your practice area |
| 14. Mentor others to develop ethical practice behaviors |
| 15. Address barriers to ethical practice through systems changes |
| 16. Use preventative ethics to decrease unit level moral distress |
| 17. Engage in health policy initiatives supporting social justice |
| 18. Provide leadership at the unit, organizational, local, state and federal level for policy change initiatives to address social justice issues in health care |
Notes: five-point Likert-type scale: 1-very low, 2-low, 3-moderate, 4-high, 5-very high per item.
Statistical analysis
Statistical analyses were conducted using IBM SPSS 27. Common univariate statistics (absolute/relative frequencies, mean, standard deviation, range) were used to describe sample characteristics. Five-point Likert-type variables were treated as quasi-metric data.
To explore the structure of the EDMC Scale, thereby pursuing the aim to identify a reduced, simple and interpretable scale structure while allowing to-be-identified components to be correlated, principal component analysis (PCA) applying an oblique (promax) rotation method was carried out for total sample and separately by country. Kaiser–Meyer–Olkin (KMO) measure was used to estimate PCA solution’s fit and adequacy of the included variables. After examination of item correlation matrices, scree plot and Kaiser Eigenvalue criteria were used to extract the optimal number of components. The procedures to group items to index variables (i.e., components, factors) were based on statistical and theoretical criteria following several common recommendations for item assignment21,22,23: (1) items with the highest factor loadings were assigned to the respected components, (2) loadings with >0.50 were considered as relevant, (3) necessary difference in case of relevant cross-loading items was set to 0.30, (4) a shared, overarching structure of components and alignments of items between the PCA for German-speaking European countries and USA was pursued, and (5) affirmative decisions were based on EDMC theoretical foundation and assumptions.
After identifying the scale’s shared structure based on the juxtaposition of the separated PCA solutions by country, mean index variables (i.e., the sum of ratings divided by the number of items per respondent), representing the initial five-point Likert-type scales (1-very low to 5-very high) were computed in favor of the interpretability of statistical scale score comparisons of EDMC in the German-speaking European countries and U.S. sample.
Psychometric properties in terms of subscales’ univariate statistics (mean, standard deviation, range) and internal consistency (standardized) Cronbach α, corrected item-scale correlation, α if item deleted) were examined. Finally, and recurring to the phenomena measured, differences between German-speaking European countries and U.S. nurse leaders were analyzed applying student t-tests for independent samples. Statistical significance was set to α = 0.05 (two-sided).
Ethical considerations
Ethical approval for the research was given by the IRB of a U.S. university (Ref. #18–036). Survey respondents were notified in the introduction to the survey that their participation implied voluntary consent. Surveys were written in both English and German.
Results
Sample characteristics
A total of 316 nurse leaders participated in the online survey, including 225 and 91 respondents from German-speaking European countries (Austria-AT, Germany-DE, Switzerland-CH) and U.S., respectively (Table 2). Among the total sample, 82.2% identified as female. On average, nurse leaders were 46 years of age, reported being a registered nurse for 23 years, and had worked for about 11 years in a nurse leader, advanced nursing, or nurse executive role. An average of 40 h of work per week was reported. While the working hours are comparable between the subsamples, the sample of U.S. nurse leaders consisted of more females, as well as older respondents and worked longer as registered nurses as well as nurse leaders on average.
Table 2.
Basic sample characteristics.
| Characteristic | AT-DE-CH | U.S. | Total |
|---|---|---|---|
| Female % (n) | 78.9% (176) | 90.1% (82) | 82.2% (258) |
| Age in years x̄ (SD), Ra | 42.9 (10.6), 19–63 | 55.1 (9.2), 30–81 | 46.4 (11.6), 19–81 |
| Current occupation | |||
| Nurse practitioner % (n) | 41.8% (94) | 46.2% (42) | 43.0% (136) |
| Clinical nurse specialist % (n) | 27.6% (62) | 5.5% (5) | 21.2% (67) |
| Nurse educator % (n) | 10.7% (24) | 25.3% (23) | 14.9% (47) |
| Chief clinical/Nursing officer % (n) | — | 4.4% (4) | 1.3% (4) |
| Director of nursing % (n) | 9.3% (21) | 4.4% (4) | 7.9% (25) |
| Deputy director of nursing % (n) | 4.9% (11) | — | 3.5% (11) |
| Other % (n) | 5.8% (13) | 14.3% (13) | 8.2% (26) |
| Nursing degree (highest) | |||
| PhD % (n) | 4.9% (11) | 1.1% (1) | 3.8% (12) |
| DNP % (n) | 0.9% (2) | 89.0% (81) | 26.3% (83) |
| MSN % (n) | 42.7% (96) | 8.8% (8) | 32.9% (104) |
| BSN % (n) | 17.3% (39) | — | 12.3% (39) |
| PR educ. Nursing/DN Mgmt. % (n) | 16.4% (37) | — | 11.7% (37) |
| Other % (n) | 17.8% (40) | 1.1% (1) | 13.0% (41) |
| Type of health care Facility | |||
| Outpatient practice clinic % (n) | 2.2% (5) | 25.3% (23) | 8.9% (28) |
| Hospital, acute care facility % (n) | 68.9% (155) | 28.6% (23) | 57.3% (181) |
| LTC/Nursing/Elderly home % (n) | 9.8% (22) | 1.1% (1) | 7.3% (23) |
| Home health care, CNS % (n) | 8.0% (18) | 1.1% (1) | 6.0% (19) |
| Higher education % (n) | — | 33.0% (30) | 9.5% (30) |
| Other % (n) | 11.1% (25) | 11.0% (10) | 11.1% (35) |
| Years registered nurse χ (SD), Ra | 19.8 (10.8), 0–43 | 29.9 (10.9), 6–60 | 22.7 (11.7), 0–60 |
| Years nurse leader, AN/Executive x̄ (SD), Ra | 8.8 (7.7), 0–43 | 16.8 (10.3), 0–48 | 11.1 (9.3), 0–48 |
| Average weekly working hours x̄ (SD), Ra | 38.3 (9.9), 0–60 | 42.5 (15.4), 0–80 | 39.5 (11.9), 0–80 |
| Number of participants | 225 | 91 | 316 |
| Austria % (n) | 12.0% (27) | — | 8.5% (27) |
| Germany % (n) | 50.7% (114) | — | 36.1% (114) |
| Switzerland % (n) | 37.3% (84) | — | 26.6% (84) |
Notes: x̄ Mean, SD Standard Deviation, Ra Range, % valid percentage, n absolute number, - not applicable; AT Austria, DE Germany, CH Switzerland, PhD Doctor of Philosophy, DNP Doctor of Nursing Practice, MSN Master of Science in Nursing, BSN Bachelor of Science in Nursing, PR Post-Registration, DN Mngt. Diploma Nursing Management, Educ. Education, LTC Long-term Care, CNS Community Nursing Service, AN Advanced Nursing.
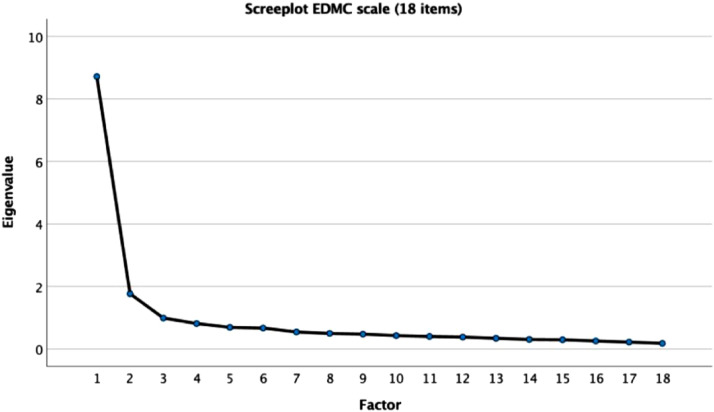
Principal component analysis
A factor analysis was conducted on the 18-item EDMC Scale in order to explore its factor structure and determine its dimensionality. A PCA with oblique promax rotation was performed for the total sample at first. The results of this PCA solution (Table 3) served as the basis for the consecutive analyses for the German-speaking European and U.S. subsamples. Referring to the total sample model, the correlation matrix demonstrates a reasonable factorability, such as groups of variables with rather high between-item correlations. A KMO measure of sampling adequacy of 0.931 indicates that both items and the complete model seem to be suitable for factor analysis. Bartlett’s test of sphericity was significantly different from zero (χ2 = 3407.27; p < 0.001) adding to the prerequisite of an overall satisfactory between-item correlation. Both scree plot (Figure 1) and Kaiser eigenvalue criterion >1.0 identified a two-factor solution, cumulatively explaining 58.23% of the total variance. Twelve items load on the first component (Eigenvalue = 8.71), six items on the second component (Eigenvalue = 1.77). Overall, factor loadings ranging from 0.536–0.889 were observed. All but four item communalities (h2) amounted to more than 0.50 and all four respected h2 were greater than 0.40.
Table 3.
Principal component analysis (total sample).
| Items | Factor loading | Communality | |
|---|---|---|---|
| F1 | F2 | ||
| 1. Recognize a genuine ethical dilemma in practice | 0.681 | 0.471 | |
| 2. Make a sound ethical decision | 0.755 | 0.581 | |
| 3. Explain your ethical decisions using correct ethical terminology and language | 0.775 | 0.614 | |
| 4. Provide a clear statement of the personal values that guide your EDM and practice | 0.845 | 0.612 | |
| 5. Articulate legal guidelines related to complex ethical issues in patient care | 0.668 | 0.462 | |
| 6. Articulate the difference between ethical dilemmas, moral distress, issues related to inter-professional collaboration and communication, difficult patients, etc. | 0.876 | 0.655 | |
| 7. Articulate the definition of moral distress and provide an example in your practice | 0.837 | 0.650 | |
| 8. Identify ethical issues in complex patient care | 0.831 | 0.641 | |
| 9. Apply ethical decision-making models or structured processes to complex clinical problems | 0.575 | 0.610 | |
| 10. Participate in and/or guide mediation related to complex clinical problems involving ethical dilemmas or moral distress | 0.536 | 0.478 | |
| 11. Recognize and manage moral distress in self and others | 0.675 | 0.466 | |
| 12. Role model collaborative problem solving in complex clinical problems involving ethical dilemmas or moral distress | 0.540 | 0.500 | |
| 13. Engage in preventative ethics initiatives to address the ethical environment in your practice area | 0.717 | 0.598 | |
| 14. Mentor others to develop ethical practice behaviors | 0.626 | 0.649 | |
| 15. Address barriers to ethical practice through systems changes | 0.799 | 0.649 | |
| 16. Use preventative ethics to decrease unit level moral distress | 0.714 | 0.602 | |
| 17. Engage in health policy initiatives supporting social justice | 0.889 | 0.623 | |
| 18. Provide leadership at the unit, organizational, local, state and federal level for policy change initiatives to address social justice issues in health care | 0.852 | 0.613 | |
| Eigenvalue (rotated) | 8.71 | 1.77 | |
| % of explanatory variance (rotated) | 48.41 | 9.82 | |
| Kaiser–Meyer–Olkin | 0.931 | ||
| Bartlett’s (chi2; p) | 3407.27; p < 0.001 | ||
Notes: promax rotation, wording of items was shortened in favor of layout features, factor loading based on muster matrix.
Figure 1.
Scree Plot for EDMC Scale (PCA). Notes: EDMC Ethical Decision-Making Confidence, PCA principal component analysis.
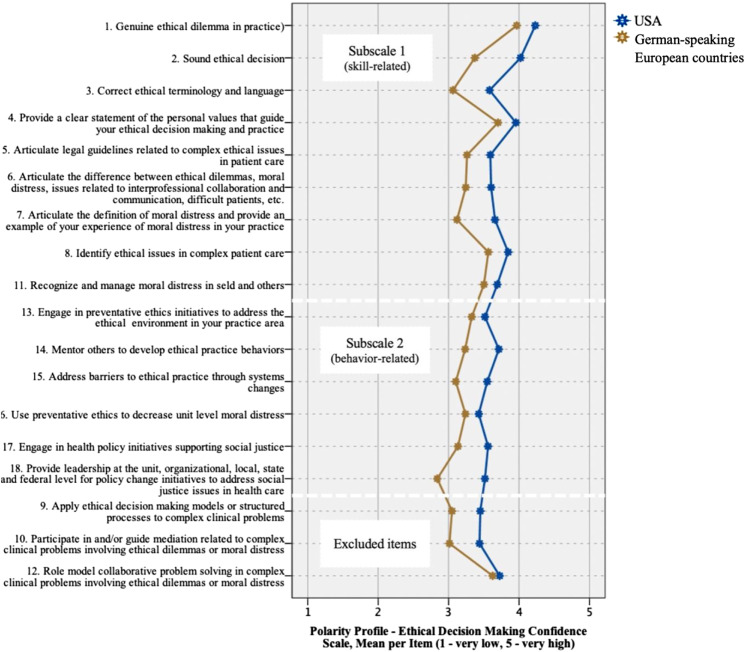
Final two-factor structure, reliability, and statistical comparisons by country
After deriving the two-component structure based on the data of the total sample, PCA was repeated within both subsamples: German-speaking European countries and the U.S. In order to identify an overarching, shared factor structure of the two subsamples, both PCA solutions were evaluated within, as well as compared between, the models.
Each PCA’s statistical properties relating to correlation matrices, communalities, KMO and Bartlett’s test of sphericity proved sufficient in terms of factorability and suitability (Supplementary Table 1). While the overall structure of the two-component solutions was comparable, three items differed in terms of their component alignment between the German-speaking European and U.S. subsample (“Item nine Apply ethical decision-making models or structured processes to complex clinical problems”, “Item 10 Participate in and/or guide mediation related to complex clinical problems involving ethical dilemmas or moral distress”, and “Item 12 Role model collaborative problem solving in complex clinical problems involving ethical dilemmas or moral distress”) and were excluded in favor of an overarching, shared factor structure (Supplementary Table 2).
The remaining 15 items were categorized along the identified components as subscale 1 and 2. Referring to the theoretical foundation of the initial item construction, subscale 1 (9 items) is best defined as the “Skill-related confidence dimension” and subscale 2 (six items) as “Behavior-related confidence dimension.” Table 4 presents the shared, final two-factor structure for the EDMC Scale.
Table 4.
Final two-factor structure for EDMC.
| Factor structure (reduced, unambiguous, German-speaking European countries and U.S.) |
|---|
| Factor 1: Ethical decision-making confidence subscale—“skill-related confidence dimension” |
| 1. Recognize a genuine ethical dilemma in practice |
| 2. Make a sound ethical decision |
| 3. Explain your ethical decisions using correct ethical terminology and language |
| 4. Provide a clear statement of the personal values that guide your EDM and practice |
| 5. Articulate legal guidelines related to complex ethical issues in patient care |
| 6. Articulate the difference between ethical dilemmas, moral distress, issues related to inter-professional collaboration and communication, difficult patients, etc. |
| 7. Articulate the definition of moral distress and provide an example in your practice |
| 8. Identify ethical issues in complex patient care |
| 11. Recognize and manage moral distress in self and others |
| Factor 2: Ethical decision-making confidence subscale—“behavior-related confidence dimension” |
| 13. Engage in preventative ethics initiatives to address the ethical environment in your practice area |
| 14. Mentor others to develop ethical practice behaviors |
| 15. Address barriers to ethical practice through systems changes |
| 16. Use preventative ethics to decrease unit level moral distress |
| 17. Engage in health policy initiatives supporting social justice |
| 18. Provide leadership at the unit. Organizational, local, state and federal level for policy change initiatives to address social justice issues in health care |
Excluded items: Apply ethical decision-making models or structured processes to complex clinical problems,” “Participate in and/or guide mediation related to complex clinical problems involving ethical dilemmas or moral distress,” “Role model collaborative problem solving in complex clinical problems involving ethical dilemmas or moral distress”
Notes: EDMC Ethical Decision-Making Confidence.
In the next step, mean index variables each were computed for each of the two subscales representing the initial item rating (1-very low to 5-very high). Subscale means and reliability measures in terms of internal consistency were analyzed for total, German-speaking European countries, and U.S. sample (Table 5).
Table 5.
Reliability and statistical comparisons by country.
| EDMC subscale | AT-DE-CH | U.S. | Total |
|---|---|---|---|
| Skill-related confidence dimension—1 (very low) to 5 (very high) | |||
| Cronbach α | 0.884 | 0.938 | 0.908 |
| x̄ (SD), Ra | 3.42 (0.6), 1.7–5.0 | 3.80 (0.7), 2.2–5.0 | 3.53 (0.6), 1.8–5.0 |
| T, p, CI 95% of mean difference | 5.02, <0.001, 0.22–0.48 | ||
| Behavior-related confidence dimension—1 (very low) to 5 (very high) | |||
| Cronbach α | 0.851 | 0.911 | 0.874 |
| x̄ (SD), Ra | 3.15 (0.7), 1.0–5.0 | 3.55 (0.7), 2.0–5.0 | 3.3 (0.8), 1.0–5.0 |
| T, p (df), CI 95% of mean difference | 4.51, <0.001, 0.23–0.58 | ||
Notes: x̄ Mean, SD Standard Deviation, Ra Range, α alpha (internal consistency), T Student T-test, p significance level, df degrees of freedom, CI 95% confidence interval; AT Austria, DE Germany, CH Switzerland.
Overall, consistency coefficients (Cronbach α) between 0.851 and 0.938 were observed, with the reliability statistics tend slightly lower in the German-speaking European countries' sample in both subscales. Additional analyses of corrected item-scale correlation and Cronbach α if item deleted further indicated that all items correlated well with total item’s average, and that deletion of certain items would not lead to any increase of internal consistency, respectively (Supplementary Table 3).
Difference in subscale means between German-speaking European countries and the U.S. were examined using Student t-test for independent samples. Overall, U.S. nurse leaders rated their skill-related (Δ = 0.38, p < 0.001, CI 95% 0.22–0.48) as well as their behavior-related (Δ = 0.40, p < 0.001, 0.23–0.58) EDMC significantly higher than their European counterparts. The single item means, inclusive of those deleted for the subscale development, of the two EDMC subscales are presented separately by country in Figure 2. All but two items (Item 12 and 13) displayed significant differences between the subsamples indicating consistently higher confidence of U.S. rather than German-speaking European countries’ nurse leaders. Further details can be found in Supplementary Table 4.
Figure 2.
EDMC Scale Polarity Profile Displaying Item-Means by Country. Notes: EDMC Ethical Decision-Making Confidence.
Discussion
This paper describes the development, factor structure, and psychometric analysis of a researcher-developed scale aimed at measuring confidence in ethical decision-making among U.S. and German-speaking European countries’ nurse leaders. To our knowledge, this exploratory study is the first of its kind to focus on nurse leaders’ confidence regarding ethical decision-making in an international context.
The 18 items of the EDMC Scale were subject to a PCA within survey data samples of 91 U.S. and 225 German-speaking European countries’ nurse leaders. The ultimate aim was to identify an overarching factor structure, which is shared by the two samples of nurse leaders and to examine (sub)scales’ psychometric properties. This was pursued by (1) running the PCA and identifying the number of factors in the total sample, (2) repeating the PCA in both samples separately, (3) comparing and identifying a shared and reduced factor structure between the samples, and (4) subsequently analyzing (sub)scales psychometric properties.
The PCA for the total sample indicated that the applied EDMC Scale with its 18 items measures multiple dimensions on the EDMC. As evidenced in the results presented, a two-factor solution was identified to explain the factor structure of the constructed EDMC Scale for the total sample, but also for the U.S. and German-speaking samples. Overall, PCA statistical indices indicated an adequate suitability and appropriate fit of the data in terms of the amount of explained variance, high and unambiguous factor loadings, as well as satisfactory communality measures.22,24
Although the overall statistical properties of the PCAs in the subsamples were sufficient and suitable, the explained variances differed between the data sets. While the two factors explained more than 68% in the U.S. sample, a lesser but still acceptably high 25 share of 54% of total variance could be attributed to the two factors in the German-speaking European sample. Hence, these findings indicate that the two-factor solution seems to be even more decisive and stable for U.S. nurse leaders. This might be partially explained by a rather homogeneous U.S. sample, while the German-speaking European country samples include nurses from three different countries, cultures, and health care delivery systems.
To identify a factor structure which is shared between the two international samples, only those items, which load on the same factor in both data sets were used to compute the final two subscales of EDMC. As a consequence, three items ended up being excluded from the subscales. Interestingly, the content of all three excluded items refers to ethical decision-making dealing with complex clinical problems. In light of the comparative nature of this international study, some plausible explanations might relate to culture, management and leadership, nursing-educational differences and, most notably, to culturally biased concepts and understandings of the term “clinical problems”. The authors did not operationally define the term “clinical problems” in the survey since nurse leader roles and experiences can be highly diverse. Despite this diversity, moral distress in nurses remains a common experience, 26 and necessitates that nurse leaders possess EDMC. 14 There is abundant literature reporting common causes of moral distress in nurses which include providing care that is deemed excessive or futile, feelings of powerlessness, poor team communication, poor leadership, witnessing unethical and/or incompetent clinicians, burdensome technology, and delayed or ignored end-of-life decisions in both acute and post-acute care settings.26–31
Started by a number of political reform processes, the three German-speaking countries in Europe are currently in flux to reform nursing education by academizing and professionalizing the nursing education process. Each country is at a different stage on the change continuum, and none are near completion. Historically seen as a practical profession in parts of Europe, nursing education is being redefined as an academic profession, such as the Nursing Professions Act 2017 in Germany which became effective 1 January 2020. 32 With this push for increasing degree educated nurses (DENs) in Europe, confusion and uncertainty are present in the predominately vocationally trained nursing staff. In 2018, the U.S. reported 57% of nurses had graduated with a bachelor degree, 33 compared to 1% of German nurses. 32
In addition to external factors, key sample characteristics may also contribute to the differential perception of clinical problems between the U.S. and the German-speaking samples. While only 5.8% of the nurse leaders in the German-speaking European countries hold a Doctor of Philosophy (PhD) or Doctor of Nursing Practice (DNP), more than 90% of the U.S. respondents possessed these terminal degrees. Research shows that educational attainment and didactic content with high practical relevance are positively associated with higher self-esteem and ethical confidence,34–36 which may at least partially explain the different factor structure between the U.S. and German-speaking samples. Another explanation may be that the U.S. sample (16.8 years) has on average been working as nurse leaders more than twice as long as the European nurse leaders (8.8 years), giving the U.S. sample the benefit of experience.
The remaining 15 items displayed a similar factor structure in both samples. These were categorized along the identified two components, computed as mean index variables, and finally labeled as “Skill-related confidence dimension (9 items)” and “Behavior-related confidence dimension (6 items)”. Drawing upon the framework of ethical decision-making by Hamric and Delgado, 14 the former scale consists of items that refer to skills based on foundational concepts in ethical decision-making, whereas the latter comprises items that predominantly address behavioral dimensions. Hence, the two identified confidence dimensions support and represent the theoretical foundation by Hamric and Delgado. Specifically, our identified Skill-related confidence dimensions, containing items such as “recognizing ethical dilemmas” or “making sound ethical decisions,” correlate with Hamric and Delgado’s Phases 1 and 2 allowing the nurse to acquire these skill sets and apply them in patient care settings. The items identified under the Behavior-related confidence dimensions, such as “engaging in health policy initiatives supporting social justice” or “providing leadership,” correspond to Hamric and Delgado’s Phases 3 and 4. These behavior sets build on the skill-related confidence dimensions and take them to the next level of patient advocacy, mentorship, effective communication, and conflict resolution.
Internal consistency and reliability were established and proved good-to-excellent for both subscales in both international samples. Reliability measures of both subscales were slightly lower in the German-speaking European countries' sample indicating that the underlying correlational structure might be affected by the heterogeneous sample of German, Swiss, and Austrian nurse leaders. Regarding the subscales’ mean index scores, U.S. nurse leaders rated both their skill- and behavior-related EDMC significantly higher than their German-speaking European counterparts. Beside the above-mentioned explanatory potential of higher proportions of participants with terminal degrees in the U.S., this finding may be due to the fact that the U.S. nurse leaders in our sample have significantly more and longer experience in nursing as well as leadership roles, and therefore, may be more confident in ethical decision-making.
Limitations
Despite our valuable findings, several limitations must be acknowledged. First, data came from a parental study, which applied a convenience sampling method rather than a random sampling strategy. The final sample sizes of the U.S. and German-speaking European countries’ subsamples were rather low, and the U.S. sample size was less than half of the collective European respondents. Additionally, the latter subsample was comprised of Austrian, German, and Swiss participants, whereby selected sample characteristics varied between the three countries. This subsample’s heterogeneity and the applied convenience sampling method may not be representative of the population and restricts the external validity of the findings. Our findings constitute exploratory results as the original study was not specifically designed as a scale development study and our approach represents a data-driven approach. Our findings will have to withstand future replication and further testing, including implementing typical procedures in scale development. Hence, we strive for further examination of our proposed EDMC Scale applying interpretative research methods (e.g., Delphi method with cognitive interviews) or comparative case study research (e.g., on a macro-, meso-, and micro-level) with a selected sample of U.S. and German-speaking European nurse leaders to analyze content validity as well as replicating our study in a larger more representative sample including additional measures of related phenomena. This would not only enable testing the identified factor structure within a Confirmatory Factor Analysis, but also determining and examining further relevant measures of validity, that is, concurrent, convergent, or discriminant validity.
Conclusion
The unique contribution of our work is that we have developed a tool to measure EDMC from the explicit perspective of nurse leaders, evaluated the psychometric properties, and compared nurse leaders’ EDMC in the U.S. and three German-speaking countries in Europe. We believe that our analysis revealed promising results for further studies about EDMC in nurses holding leadership roles. These promising results should be replicated by further studies to ensure validity and reliability of the EDMC scale measuring skill-related and behavior-related concepts. Additional studies using our EDMC scale in same, or different international settings may help to compare socio-demographic differences while further solidifying its validity and reliability. Since this scale was validated in both English and German, it has the ability to be implemented in populations of either language.
Supplemental Material
Supplemental Material, sj-pdf-1-nej-10.1177_09697330211065847 for Ethical decision-making confidence scale for nurse leaders: Psychometric evaluation by Lorri Birkholz, Patrick Kutschar, Firuzan Sari Kundt in Nursing Ethics
Acknowledgements
Special thanks go out to Dr. Rebecca Poston for her contribution to the development of the original study and Dr. Nancy Sweeney for her editing services.
Author contributions: L. B. served as the principal investigator for the US arm of this research project and made substantial contributions to the acquisition, analysis and interpretation of data while drafting the research note and revising it critically for important intellectual content. The final approval of the version to be published is given by the first author – she agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.P. K. was responsible for the data analysis of this research project, prepared and interpreted the results, made substantial contributions to all sections of this article and revised the research note critically for important intellectual content.F. S. K. served as research assistant for the research study while revising it for important intellectual content, data management and analysis, added to all sections of this manuscript, expanded the discussion and conclusion sections as well as provided final proof-reading and editing.M. B.-H. served as the principal investigator for the European arm of this research project and made substantial contributions to the acquisition, analysis and interpretation of data while drafting the research note and revising it critically for important intellectual content. The pre-final approval of the version to be published is given by the last author.
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The authors declare that there is no conflict of interest and agree to be accountable for all aspects of the research note.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval of the research presented was given by the IRB Board of Old Dominion University in Norfolk, VA, USA by reference number 18-036.
Informed consent: Survey respondents were notified in the introduction to the survey that their participation implied consent. Clicking on the link and completing the survey was entirely voluntary and served as implied consent to participate.
Data availability: The dataset supporting the conclusions of this article is not available in a public repository but is available from the authors upon reasonable request.
Supplemental Material: Supplemental material for this article is available online.
ORCID iDs
Lorri Birkholz https://orcid.org/0000-0002-2383-1689
Patrick Kutschar https://orcid.org/0000-0002-2029-2552
References
- 1.Al-Majid S, Carlson N, Kiyohara M, et al. Assessing the degree of satisfaction and compassion fatigue among critical care, oncology, and charge nurses. JONA: J Nurs Adm 2018; 48(6): 310–315. DOI: 10.1097/NNA.0000000000000620 10.1097/NNA.0000000000000620. [DOI] [PubMed] [Google Scholar]
- 2.Wocial LD, Weaver MT. Development and psychometric testing of a new tool for detecting moral distress: the moral distress thermometer. J Adv Nurs 2013; 69(1): 167–174. doi: 10.1111/j.1365-2648.2012.06036.x. [DOI] [PubMed] [Google Scholar]
- 3.Lown BA. Mission critical: nursing leadership for compassion to sustain staff well-being. Nurs Adm Q 2018; 42(3): 217–222. DOI: 10.1097/NAQ.0000000000000302 10.1097/NAQ.0000000000000302. [DOI] [PubMed] [Google Scholar]
- 4.Epstein E, Delgado S. Understanding and addressing moral distress. OJIN 2010; 15(3): Manuscript 1. doi: 10.3912/OJIN.Vol15No03Man1 [DOI] [Google Scholar]
- 5.Pavlish C, Brown-Saltzman K, So L, et al. Support: an evidence-based model for leaders addressing moral distress. JONA: J Nurs Adm 2016; 46(6): 313–320. DOI: 10.1097/NNA.0000000000000351 10.1097/NNA.0000000000000351. [DOI] [PubMed] [Google Scholar]
- 6.Rodney PA. What we know about moral distress. AJN, Am J Nurs 2017; 117(2): S7–S10. DOI: 10.1097/01.NAJ.0000512204.85973.04 10.1097/01.NAJ.0000512204.85973.04. [DOI] [PubMed] [Google Scholar]
- 7.Softskills.com. List of Soft Skills. https://esoftskills.com/wp-content/uploads/2019/08/List-of-Soft-Skills-PDF.pdf (2019, accessed 06 April 2021). [Google Scholar]
- 8.Lechasseur K, Caux C, Dollé S, et al. Ethical competence: an integrative review. Nurs Ethics 2018; 25(6): 694–706. DOI: 10.1177/0969733016667773 10.1177/0969733016667773. [DOI] [PubMed] [Google Scholar]
- 9.Stanley D, Stanley K. Clinical leadership and nursing explored: a literature search. J Clinical Nursing 2018; 27(9–10): 1730–1743. DOI: 10.1111/jocn.14145 10.1111/jocn.14145. [DOI] [PubMed] [Google Scholar]
- 10.Heinen M, Oostveen C, Peters J, et al. An integrative review of leadership competencies and attributes in advanced nursing practice. J Adv Nurs 2019; 75(11): 2378–2392. DOI: 10.1111/jan.14092 10.1111/jan.14092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Dossary R, 2017, Leadership in Nursing, Contemporary Leadership Challenges. Aida Alvinius, IntechOpen, DOI: 10.5772/65308. Available from: https://www.intechopen.com/books/contemporary-leadership-challenges/leadership-in-nursing. Accessed on April 6, 2021 [DOI] [Google Scholar]
- 12.Webster M. Confidence. https://www.merriam-webster.com/dictionary/ confidence (2021). Accessed 18 April 2021.
- 13.Smith L, Mee S. Patient advocacy: breaking down barriers and challenging decisions. Nurs Times. 2017; 113(1): 54–56. [Google Scholar]
- 14.Hamric AB, Delgado SA. Ethical decision making. In: Hamric AB, Hanson CM, Hanson MF, et al. (eds) Advanced Practice Nursing: An Integrative Approach. Saunders: Elsevier, 2013, p. 328–355. [Google Scholar]
- 15.Martin DA. Nurses' involvement in ethical decision-making with severely ill newborns. Issues Compr Pediatr Nurs 1989; 12(6): 463–473. DOI: 10.3109/01460868909026850 10.3109/01460868909026850. [DOI] [PubMed] [Google Scholar]
- 16.Dufrene RL, Glosoff HL. The ethical decision-making scale-revised. Meas Eval Couns Development 2004; 37(1): 2–14. DOI: 10.1080/07481756.2004.11909746 10.1080/07481756.2004.11909746. [DOI] [Google Scholar]
- 17.Krautscheid LC. Embedding microethical dilemmas in high-fidelity simulation scenarios: preparing nursing students for ethical practice. J Nurs Education 2017; 56(1): 55–58. DOI: 10.3928/01484834-20161219-11 10.3928/01484834-20161219-11. [DOI] [PubMed] [Google Scholar]
- 18.Poikkeus T, Numminen O, Suhonen R, et al. A mixed-method systematic review: support for ethical competence of nurses. J Adv Nurs 2014; 70(2): 256–271. DOI: 10.1111/jan.12213. [DOI] [PubMed] [Google Scholar]
- 19.Esmaelzadeh F, Abbaszadeh A, Borhani F, et al. Strengthening ethical decision-making: the experience of Iranian nurses. Nurs Manage. 2017; 24(6): 33–39. DOI: 10.7748/nm.2017.e1610 10.7748/nm.2017.e1610. [DOI] [PubMed] [Google Scholar]
- 20.Doctors of Nursing Practice. Home. https://www.doctorsofnursingpractice.org/ (2021). accessed April 30, 2021. [Google Scholar]
- 21.Izquierdo I, II, Olea J, Abad FJ. Exploratory factor analysis in validation studies: use and recommendations. Psicothema 2014; 26(3): 395–400. [DOI] [PubMed] [Google Scholar]
- 22.Matsunaga M. How to factor-analyze your data right: do’s, don’ts, and how-to’s. Int J Psychol Res 2010; 3(1): 97–110. DOI: 10.21500/20112084.854 10.21500/20112084.854. [DOI] [Google Scholar]
- 23.Field A. Discovering Statistics Using SPSS. 3rd ed. Sage Publications; 2009. [Google Scholar]
- 24.Kaiser HF, Rice J, Little J, et al. Educ Psychol Meas 1974; 34(1): 111–117. DOI: 10.1177/001316447403400115 10.1177/001316447403400115. [DOI] [Google Scholar]
- 25.Streiner DL. Figuring out factors: the use and misuse of factor analysis. Can J Psychiatry 1994; 39(3): 135–140. DOI: 10.1177/070674379403900303 10.1177/070674379403900303. [DOI] [PubMed] [Google Scholar]
- 26.Epstein EJ, Whitehead PB, Prompahakul C, et al. Enhancing understanding of moral distress: the measure of moral distress for health care professionals. AJOB Empirical Bioeth 2019; 10(2): 113–124. DOI: 10.1080/23294515.2019.1586008 10.1080/23294515.2019.1586008. [DOI] [PubMed] [Google Scholar]
- 27.Helmers A, Palmer KD, Greenberg RA. Moral distress: developing strategies from experience. Nurs Ethics 2020; 27(4): 1147–1156. DOI: 10.1177/0969733020906593 10.1177/0969733020906593. [DOI] [PubMed] [Google Scholar]
- 28.Kleinknecht-Dolf M, Spichiger E, Müller M, et al. Advancement of the German version of the moral distress scale for acute care nurses-a mixed methods study. Nurs Open 2017; 4(4): 251–266. DOI: 10.1002/nop2.91 10.1002/nop2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morley G, Ives J, Bradbury-Jones C. Moral distress and austerity: an avoidable ethical challenge in healthcare. Health Care Anal 2019; 27(3): 185–201. DOI: 10.1007/s10728-019-00376-8 10.1007/s10728-019-00376-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schwarzkopf D, Rüddel H, Thomas-Rüddel DO, et al. Perceived nonbeneficial treatment of patients, burnout, and intention to oleave the job among ICU nurses and junior and senior physicians. Crit Care Med 2017; 45(3): e265–e273. DOI: 10.1097/CCM.0000000000002081 10.1097/CCM.0000000000002081. [DOI] [PubMed] [Google Scholar]
- 31.Gágyor I, Heßling A, Heim S, et al. Ethical challenges in primary care: a focus group study with general practitioners, nurses and informal caregivers. Fam Pract 2019; 36(2): 225–230. DOI: 10.1097/CCM.0000000000002081 10.1097/CCM.0000000000002081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pachanov A. Academization of nursing and its possible consequences for hospital management in Germany. Journal of Nursing and Care 2020; 9(4): 1–4. DOI: 10.37421/jnc.2020.9.504. [DOI] [Google Scholar]
- 33.Schnur MB, US Nurses in 2020 : Who We Are and Where We Work. https://www.nursingcenter.com/ncblog/may-2020/u-s-nurses-in-2020 [Google Scholar]
- 34.Grace P. Enhancing nurse moral agency: the leadership promise of doctor of nursing practice preparation. OJIN 2018; 23(1): DOI: 10.3912/OJIN.Vol23No01Man04 10.3912/OJIN.Vol23No01Man04. [DOI] [Google Scholar]
- 35.Van Eckert S, Gaidys U, Martin CR. Self‐esteem among German nurses: does academic education make a difference? J Psychiatr Ment Health Nurs 2012; 19(10): 903–910. DOI: 10.1111/j.1365-2850.2011.01862.x 10.1111/j.1365-2850.2011.01862.x. [DOI] [PubMed] [Google Scholar]
- 36.Rizany I, Hariyati TS, Handayanib H. Factors that affect the development of nurses’ competencies: a systematic review. Enferm Clin. 2017;27(Suppl. Part I):154–157. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-nej-10.1177_09697330211065847 for Ethical decision-making confidence scale for nurse leaders: Psychometric evaluation by Lorri Birkholz, Patrick Kutschar, Firuzan Sari Kundt in Nursing Ethics