Abstract
Inflammatory myofibroblastic tumor (IMT) is an uncommon chest pathology. Treatment primarily focuses on surgical resection for diagnostic and therapeutic purposes. However, there are instances in which alternative therapies with steroids, chemotherapy, or radiation are necessary. We discuss a case of recurrent IMT for which very low dose radiation proved an effective treatment.
Keywords: cancer, thoracic, radiation, oncology
Introduction
Inflammatory myofibroblastic tumor is a rare and benign entity that belongs to the broader group of inflammatory pseudotumors. It has a reported incidence of 0.04%–1%, in patients with resected lung nodules. 1 Initially discovered in the lung but since has been reported involving various locations and organs, these lesions share a common histologic appearance characterized by spindle cell proliferation with a prominent inflammatory infiltrate composed primarily of polyclonal plasma cells.2,3 IMT was originally defined as an inflammatory condition, typically seen after recurrent respiratory infections. Now it is seen as an intermediate neoplastic condition, with small risk of metastasis and tendency to locally recur. 4 Case series documenting aggressive behavior, such as metastasis, and links to chromosomal translocations of the anaplastic lymphoma kinase (ALK) have led to IMT being considered a true neoplasm. 2 Patients usually have vague or non-specific symptoms at presentation and many patients are asymptomatic, with a tumor discovered incidentally via imaging. Surgery has been the standard treatment whenever feasible, however, radiation, chemotherapy, and steroids have been tried in small numbers of case reports. We report a case of recurrent IMT being treated successfully with very low-dose radiation therapy.
Case Report
A 60-year-old female presented with multiple bilateral pulmonary nodules that were identified on computed tomography (CT) imaging of the chest. CT guided biopsy was non-diagnostic, so a video-assisted thoracoscopic surgery was performed with resection of the two largest nodules in the left upper lobe and the right lower lobe. Histopathological examination of the excisional biopsies showed a well-circumscribed lesion with dense fibrosis and numerous plasma cells and lymphocytes (Figure 1). Kappa/lambda in situ hybridization was polyclonal, ruling out a plasma cell neoplasm. The IgG4 positivity rate was low, ruling out IgG4 fibroinflammatory disease. The histology was most consistent with IMT, and while ALK-1 was negative, it is expected to be negative in 50% of IMTs. Five years later the patient developed progression of the nodular opacity in the lingula (Figure 2) similarly to what was seen on initial presentation. Both CT and endobronchial ultrasound guided needle biopsies were non-diagnostic, with the biopsy showing only histiocytes and benign bronchial cells (Figure 3). Steroid therapy was deferred due to her morbid obesity and poorly controlled diabetes. Surgical treatment was not pursued due to her poor functional status and prior surgical history. The lingular lesion was treated with low dose (4 Gy at 2 Gy/fraction) radiation therapy. This treatment regimen was extrapolated from the treatment paradigm for indolent lymphoma because the IMT plasma cells we expect to be similarly radiosensitive. In follicular lymphoma and MALT lymphoma the same fractionation has been shown to provide local control for up to 70% of patients and in this specific case was unlikely to cause much toxicity. If restaging scans did not show at least a partial response, then the plan would have been to deliver a higher dose of 24 Gy at 2 Gy/fraction. 5 The patient was simulated using a 4D CT scan and the gross tumor volume (GTV) using all 10 phases of the 4DCT scan to outline the tumor. A 0.5 cm uniform expansion was used to great the clinical target volume (CTV) and another 0.5 cm uniform margin was used to create the planned target volume (PTV). The patient underwent daily image guidance with CBCT for each of the two treatments. A follow up scan after 3 months showed a partial response and subsequent CT imaging 6 months later (Figure 3) without any further treatment showed near complete resolution of the lesion. Since then, patient has had multiple CT imaging which showed stable lingular lesion with waxing and waning ground glass opacities in other areas.
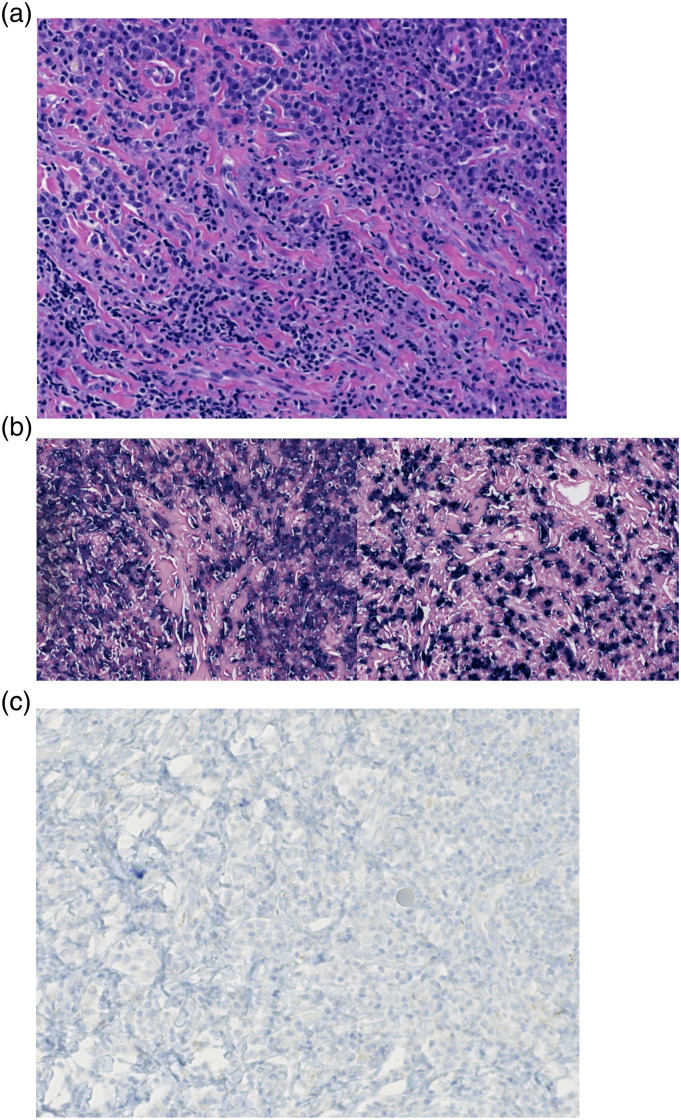
Figure 1.
(a) H&E stain reveals a well-circumscribed mass composed of numerous plasma cells and lymphocytes in a background of dense fibrosis. (b) In-situ hybridization for kappa (left) and lambda (right) light chains shows a polyclonal mix of plasma cells. (c) An immunostain for ALK-1 is negative and ALK FISH is negative for a translocation.
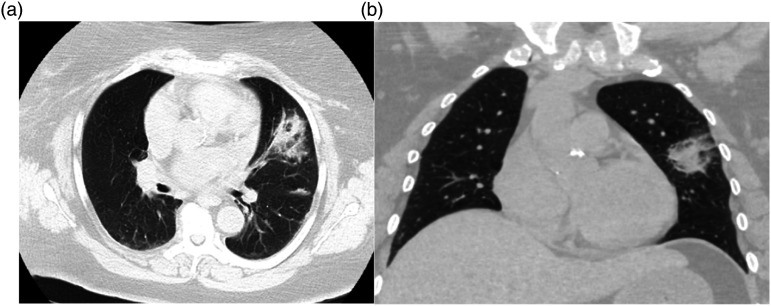
Figure 2.
CT imaging showing new nodular opacity in the lingula in cross section (a) and coronal plane (b).
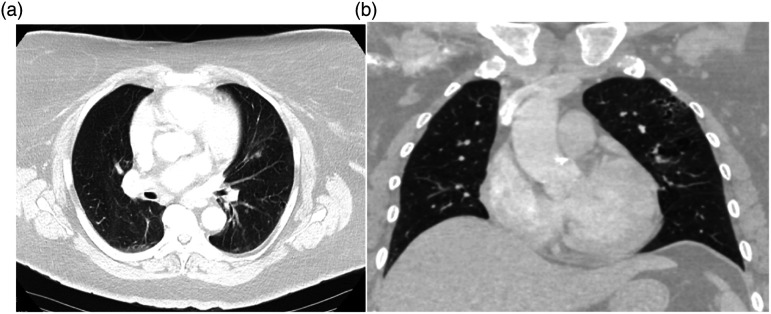
Figure 3.
CT imaging showing resolution of previously seen nodular opacity in the lingula post radiation therapy in cross section (a) and coronal view (b).
Discussion
The treatment of IMT has long been centered on surgical resection, in part because needle biopsies or frozen section samples commonly provide inconclusive results, but also as resection is therapeutic. Surgical resection is often the only way to obtain an accurate diagnosis. 3 However, in instances where surgery is not an option, other treatment modalities have been tried such as corticosteroids, chemotherapy, and radiation therapy. Due to the low prevalence of IMT, there is not enough evidence that exists to make conclusions regarding the efficacy of such treatments. ALK inhibitors such as Crizotinib may be important in the approximately 50% of IMTs containing ALK rearrangements. 2 Given their histological appearance as a chronic inflammatory process, steroids have been tried with mixed success, possibly more effective in children. 4 Radiation therapy has been reported successful in a few cases but using much higher doses of 40–50 Gy. 6 In the present case, we utilized very low dose of radiotherapy (4 Gy) and demonstrated an excellent response.
Conclusion
Surgical resection remains the treatment of choice, with the most evidence, due to its diagnostic and therapeutic nature. However, trialing very low-dose radiation therapy is a potential option in cases where surgery is contraindicated, or lesions are not anatomically resectable.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: Our institution does not require ethical approval for reporting individual cases or case series.
Informed Consent: Verbal informed consent was obtained from the patient for their anonymized information to be published in this article.
ORCID iDs
Hamel Patel https://orcid.org/0000-0001-5843-1020
Stephanie Rothweiler https://orcid.org/0000-0001-5075-7616
References
- 1.Schweckendiek D, Inci I, Schneiter D, et al. Inflammatory Myofibroblastic Tumor of the Lung: Two Progressing Pulmonary Nodules in a 25-Year-Old Adult with a Moraxella catharalis Infection. Ann Thorac Surg 2015; 100: e123–e124. [DOI] [PubMed] [Google Scholar]
- 2.Gleason BC, Hornick JL. Inflammatory myofibroblastic tumours: where are we now? J Clin Pathol 2008; 61: 428–437. [DOI] [PubMed] [Google Scholar]
- 3.Panagiotopoulos N, Patrini D, Gvinianidze L, et al. Inflammatory myofibroblastic tumour of the lung: a reactive lesion or a true neoplasm? J Thoracic Disease 2015; 7(5): 908–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hammas N, Chbani L, Rami M, et al. A rare tumor of the lung: inflammatory myofibroblastic tumor. Diagn Pathol 2012; 7(1): 83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Illidge T, Specht L, Yahalom J, et al. Modern radiation therapy for nodal non-Hodgkin lymphoma-target definition and dose guidelines from the International Lymphoma Radiation Oncology Group. Int Journal Radiation Oncology, Biology, Physics 2014; 89(1): 49–58. [DOI] [PubMed] [Google Scholar]
- 6.Imperato JP, Folkman J, Sagerman RH, et al. Treatment of plasma cell granuloma of the lung with radiation therapy. A report of two cases and a review of the literature. Cancer 1986; 57(11): 2127–2129. [DOI] [PubMed] [Google Scholar]