Abstract
Background:
Studies to date evaluating biceps tenotomy versus tenodesis in the setting of concomitant rotator cuff repair (RCR) have demonstrated relatively equivalent pain and functional outcomes.
Hypothesis:
It was hypothesized that a significant difference could be demonstrated for pain and functional outcome scores comparing biceps tenotomy versus tenodesis in the setting of RCR if the study was adequately powered.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
The Arthrex Surgical Outcomes System database was queried for patients who underwent arthroscopic biceps tenotomy or tenodesis and concomitant RCR between 2013 and 2021; included patients had a minimum of 2 years of follow-up. Outcomes between treatment types were assessed using the American Shoulder and Elbow Surgeons Shoulder (ASES), Single Assessment Numeric Evaluation (SANE), visual analog scale (VAS) for pain, and Veterans RAND 12-Item Health Survey (VR-12) scores preoperatively and at 3 months, 6 months, 1 year, and 2 years postoperatively. Results were stratified by age at surgery (3 groups: <55, 55-65, >65 years) and sex.
Results:
Overall, 1936 primary RCRs were included for analysis (1537 biceps tenodesis and 399 biceps tenotomy patients). Patients who underwent tenotomy were older and more likely to be female. A greater proportion of female patients aged <55 years and 55 to 65 years received a biceps tenotomy compared with tenodesis (P = .012 and .026, respectively). All scores were comparable between the treatment types preoperatively and at 3 months, 6 months, and 1 year postoperatively. At 2-year follow-up, patients who received a biceps tenodesis had statistically more favorable ASES, SANE, VAS pain, and VR-12 scores (P ≤ .031); however, the differences did not exceed the minimal clinically important difference (MCID) for these measures.
Conclusion:
Our findings indicate that surgeons are more likely to perform a biceps tenotomy in female and older patients. Biceps tenodesis provided improved pain and functional scores compared with tenotomy at 2-year follow-up; however, the benefit did not exceed previously reported MCID for the outcome scores. Both procedures provided improvement in outcomes; thus, the choice of procedure should be a shared decision between the surgeon and patient.
Keywords: biceps tenodesis, biceps tenotomy, rotator cuff repair
Patients with rotator cuff tears have a high incidence of concomitant long head of biceps tendon pathology and associated disability. 28 When performing a rotator cuff repair (RCR) with biceps pathology that necessitates surgical management, the treating surgeon is faced with the choice of performing either a biceps tenotomy or a biceps tenodesis. 23,26 Multiple studies have demonstrated improvement in pain and functional outcomes with either tenotomy or tenodesis. 1,3,10,13,14 Tenotomy offers the advantage of decreased surgical time and avoidance of an extra surgical incision in some cases. Proponents of biceps tenodesis argue that this procedure results in a better cosmetic result (avoidance of a Popeye deformity) and avoids the prolonged cramping that occurs after a biceps tenotomy. 1
Although there are several studies demonstrating improvement in pain and functional outcomes with either procedure, the data available to guide which procedure to perform in the setting of RCR remain deficient. ∥ Recently, Kim et al 13 evaluated their results comparing tenotomy versus tenodesis for patients in the setting of concomitant RCR. They noted improved functional outcomes for both patient cohorts without a significant intergroup difference. 13 However, their study evaluated a total of only 135 patients; thus, it might have been underpowered. To the best of our knowledge, there are no large studies evaluating the outcomes regarding biceps tenodesis versus tenotomy in the setting of a concomitant RCR. There are also no studies that have stratified patient outcomes with regard to age and/or sex of the patient.
The purpose of this study was to compare the pain and functional outcome scores between patients treated with biceps tenotomy versus biceps tenodesis in the setting of RCR. We hypothesized that, after controlling for patient age and sex, there would be no difference in outcomes based on the management of the biceps tendon.
Methods
Database and Patient Selection
After receiving institutional review board approval for this study, we retrospectively queried the Surgical Outcomes System (Arthrex) global database, which includes patients from approximately 267 centers and 3000 surgeons, for patients who had undergone an arthroscopic biceps tenotomy or tenodesis and concomitant RCR between 2013 and 2021. Patients were included in the study if they had a minimum of 2 years of follow-up, with scores from at least 1 of the study outcome measures collected at 2-year follow-up. Excluded were patients missing demographic data (age and sex), those younger than 35 years, and those undergoing open RCR, revision RCR, or rotator cuff debridement without repair.
A total of 1936 patients with primary RCRs met the study inclusion criteria. The biceps tendon was managed with biceps tenotomy in 399 patients (tenotomy group) and biceps tenodesis in 1537 patients (tenodesis group). We stratified the patients in each treatment group by sex and age range: between 35 and 54 years (<55 year group; mean age, 49.3 ± 3.9 years), 55 to 65 years (mean age, 60.2 ± 3.1 years), and >65 years (mean age, 70.3 ± 3.8 years).
Outcome Measures
Functional outcomes were assessed with the American Shoulder and Elbow Surgeons Shoulder (ASES) index and function scores, the Single Assessment Numeric Evaluation (SANE), a 10-point visual analog scale (VAS) for pain, and the Veterans RAND 12-Item Health Survey (VR-12) Mental Component Summary (MCS) and Physical Component Summary (PCS). The ASES index score is the full ASES score comprising assessments of function and pain in equal parts. The ASES function score is a subscore composed of the sum of 10 functional questions (responses graded 0-3 points) from the ASES assessment questionnaire. All outcome measures were collected preoperatively and postoperatively at 3-month, 6-month, 1-year, and 2-year follow-up; the VR-12 was not assessed at 3-month follow-up but was available for all other time points.
Statistical Analysis
We compared the difference between the tenotomy versus tenodesis groups in terms of age group and sex using the chi-square test. Outcome scores at each time point were compared by treatment group, as stratified by age group and sex. The outcome scores had a nonparametric distribution as assessed by the Shapiro-Wilk test; thus, statistical comparisons were made using the Mann-Whitney U test. In addition, we compared the change in preoperative and 2-year postoperative scores (Δ) between treatment groups. All analyses were performed using R Software (Version 3.6.3; R Core Team), with P < .05 indicating statistical significance.
In addition to quantifying statistically significant differences, we compared the difference between the mean score of patients undergoing biceps tenotomy and tenodesis and the minimal clinically important difference (MCID) as reported in studies by Cvetanovich et al, 7 Kim et al, 12 and Tashjian et al 27 of patients undergoing arthroscopic RCR. In cases in which more than 1 of these studies reported an MCID for a given outcome score, the lowest reported MCID was used to assess clinical significance. The statistical power to detect a difference equivalent to the lowest reported MCID between tenotomy and tenodesis groups was calculated using G*Power (Version 3.1.9.6) with an α = .05. For the power analysis, we considered the sample sizes as the smallest number of patients with available data for each age group and sex (eg, men <55 years: n = 31 for tenotomy, n = 238 for tenodesis).
Results
The results of the power analysis are shown in Table 1. Adequate (≥80%) statistical power was present to detect the MCID for nearly all outcome measures; only the MCID for the SANE score in women aged <55 years was underpowered.
Table 1.
Study Power to Detect the Lowest Reported MCID for the Included Outcome Measures a
| Study Power b | |||
|---|---|---|---|
| ASES (MCID, 11.1-27.1 points) |
SANE (MCID, 13-16.9 points) |
VAS Pain (MCID, 1.5-2.4 points) |
|
| Overall | 100.0 | 100.0 | 100.0 |
| Age <55 y | |||
| Male | 96.6 | 80.5 | 99.5 |
| Female | 93.7 | 73.9 | 98.6 |
| Age 55-65 y | |||
| Male | 100.0 | 99.1 | 100.0 |
| Female | 100.0 | 97.0 | 100.0 |
| Age >65 y | |||
| Male | 100.0 | 97.4 | 100.0 |
| Female | 99.9 | 95.6 | 100.0 |
a Values are expressed as percentages. ASES, American Shoulder and Elbow Surgeons; MCID, minimal clinically important difference; SANE, Single Assessment Numeric Evaluation; VAS, visual analog scale.
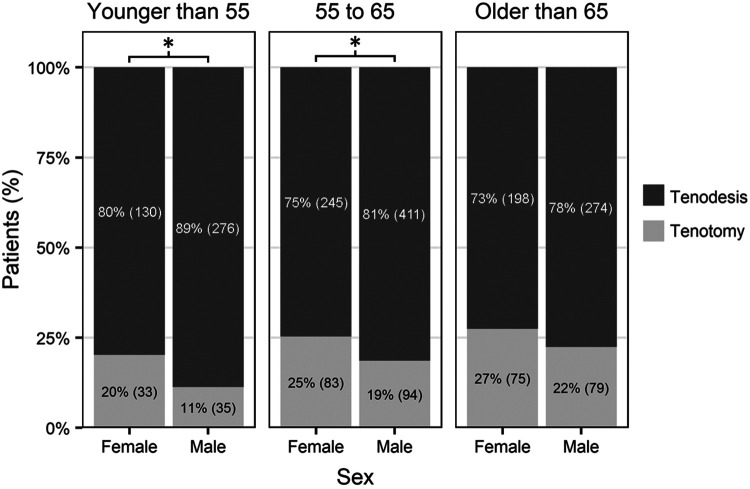
Patients who underwent tenotomy were older (62.6 ± 8.1 vs 60.3 ± 8.8 years; P < .001) and more likely to be female (48% vs 37%; P < .001) compared with those who underwent tenodesis. The tenotomy group had a greater proportion of women younger than 55 years (20% vs 11%; P = .012) and between 55 and 65 years (25% vs 19%; P = .026) compared with their male counterparts (Figure 1).
Figure 1.
Age and sex distribution of patients undergoing tenotomy versus tenodesis. *Statistically significant difference by sex within age group (P < .05).
Overall Outcomes
Pain and functional outcomes were comparable between the tenotomy and tenodesis patients preoperatively and at 3 months, 6 months, and 1 year postoperatively (Table 2). At the 2-year follow-up, the tenodesis group had significantly better scores on all outcome measures compared with the tenotomy group: ASES function (26.4 ± 5.2 vs 25.9 ± 5.4; P = .011), ASES index (88.6 ± 16.2 vs 87.2 ± 16.6; P = .008), SANE (80.6 ± 25.7 vs 76.0 ± 29.1; P = .005), VAS pain (1.1 ± 1.8 vs 1.2 ± 1.9; P = .031), VR-12 MCS (55.1 ± 8.5 vs 54.1 ± 8.8; P = .021), and VR-12 PCS (48.4 ± 8.3 vs 47.2 ± 8.5; P = .003) (Table 2). However, none of these differences surpassed the previously reported MCID threshold (Table 1). 5,11,21
Table 2.
Outcomes of Patients in the Tenotomy and Tenodesis Groups a
| Tenotomy (n = 399) | Tenodesis (n = 1537) | ||||
|---|---|---|---|---|---|
| Outcome Measure | % (n) | Mean ± SD | % (n) | Mean ± SD | P |
| Preoperative | |||||
| ASES function | 92.5 (369) | 13.5 ± 5.9 | 90.6 (1392) | 14.1 ± 5.9 | .042 |
| ASES index | 92.2 (368) | 47.6 ± 18.1 | 90.5 (1391) | 49.3 ± 18.3 | .090 |
| SANE | 92.5 (369) | 36.5 ± 20.6 | 90.3 (1388) | 37.8 ± 21.2 | .263 |
| VAS pain | 93.2 (372) | 5.0 ± 2.4 | 92.3 (1418) | 4.8 ± 2.4 | .222 |
| VR-12 MCS | 92.0 (367) | 51.1 ± 11.5 | 88.5 (1360) | 52.6 ± 10.7 | .050 |
| VR-12 PCS | 92.0 (367) | 37.3 ± 7.9 | 88.5 (1360) | 36.8 ± 8.0 | .327 |
| 3 months b | |||||
| ASES function | 92.5 (369) | 17.4 ± 6.2 | 90.7 (1394) | 16.8 ± 6.2 | .072 |
| ASES index | 92.5 (369) | 68.2 ± 17.3 | 90.7 (1394) | 67.6 ± 16.5 | .371 |
| SANE | 92.2 (368) | 56.1 ± 21.8 | 90.4 (1390) | 55.0 ± 21.5 | .354 |
| VAS pain | 93.7 (374) | 2.2 ± 1.9 | 91.9 (1413) | 2.1 ± 1.9 | .437 |
| 6 months | |||||
| ASES function | 90.7 (362) | 22.9 ± 5.7 | 87.7 (1348) | 22.7 ± 5.6 | .328 |
| ASES index | 90.7 (362) | 81.5 ± 15.6 | 87.7 (1348) | 80.9 ± 15.8 | .508 |
| SANE | 90.7 (362) | 71.9 ± 23.5 | 87.8 (1350) | 72.0 ± 22.0 | .584 |
| VAS pain | 92.0 (367) | 1.3 ± 1.6 | 89.1 (1370) | 1.4 ± 1.7 | .862 |
| VR-12 MCS | 90.0 (359) | 54.7 ± 9.4 | 87.0 (1337) | 55.3 ± 9.1 | .157 |
| VR-12 PCS | 90.0 (359) | 44.9 ± 8.5 | 87.0 (1337) | 45.2 ± 8.0 | .780 |
| 1 year | |||||
| ASES function | 90.0 (359) | 25.6 ± 5.3 | 87.2 (1341) | 25.9 ± 4.8 | .274 |
| ASES index | 90.0 (359) | 86.9 ± 15.6 | 87.2 (1341) | 87.8 ± 14.6 | .434 |
| SANE | 90.0 (359) | 77.9 ± 25.4 | 87.5 (1345) | 79.2 ± 24.5 | .364 |
| VAS pain | 90.5 (361) | 1.2 ± 1.7 | 88.0 (1353) | 1.1 ± 1.6 | .511 |
| VR-12 MCS | 89.5 (357) | 55.1 ± 8.4 | 86.9 (1335) | 55.5 ± 8.6 | .326 |
| VR-12 PCS | 89.5 (357) | 47.6 ± 7.9 | 86.9 (1335) | 48.0 ± 8.0 | .293 |
| 2 years | |||||
| ASES function | 98.5 (393) | 25.9 ± 5.4 | 98.7 (1517) | 26.4 ± 5.2 | .011 |
| ASES index | 98.5 (393) | 87.2 ± 16.6 | 98.7 (1517) | 88.6 ± 16.2 | .008 |
| SANE | 98.5 (393) | 76.0 ± 29.1 | 98.8 (1518) | 80.6 ± 25.7 | .005 |
| VAS pain | 100.0 (399) | 1.2 ± 1.9 | 100.0 (1537) | 1.1 ± 1.8 | .031 |
| VR-12 MCS | 98.7 (394) | 54.1 ± 8.8 | 97.6 (1500) | 55.1 ± 8.5 | .021 |
| VR-12 PCS | 98.7 (394) | 47.2 ± 8.5 | 97.6 (1500) | 48.4 ± 8.3 | .003 |
| Δ (preoperative to 2 y) | |||||
| ASES function | 91.7 (366) | 12.5 ± 6.7 | 89.4 (1374) | 12.4 ± 6.7 | .728 |
| ASES index | 91.5 (365) | 39.7 ± 19.7 | 89.3 (1373) | 39.5 ± 20.1 | .813 |
| SANE | 91.7 (366) | 39.7 ± 34.3 | 89.2 (1371) | 43.0 ± 32.2 | .175 |
| VAS pain | 93.2 (372) | -3.8 ± 2.6 | 92.3 (1418) | -3.7 ± 2.6 | .801 |
| VR-12 MCS | 91.5 (365) | 3.1 ± 11.0 | 86.9 (1335) | 2.7 ± 10.6 | .541 |
| VR-12 PCS | 91.5 (365) | 10.1 ± 8.4 | 86.9 (1335) | 11.6 ± 9.0 | .005 |
a Boldface P values indicate statistically significant difference between treatment groups (P < .05). ASES, American Shoulder and Elbow Surgeons; SANE, Single Assessment Numeric Evaluation; VAS, visual analog scale; VR-12, Veterans RAND 12-Item Health Survey; MCS, mental component score; PCS, physical component score.
b The 3-month postoperative VR-12 scores were not assessed.
Outcomes Stratified by Age Group and Sex
At the 2-year follow-up, patients aged under 55 years in the tenodesis group had significantly higher VR-12 MCS scores compared with their counterparts in the tenotomy group (men: 54.6 ± 9.2 vs 52.1 ± 9.2; P = .046; women: 53.3 ± 10.1 vs 49.2 ± 11.5; P = .038), and the female patients had significantly higher VR-12 PCS scores (47.8 ± 9.0 vs 42.8 ± 10.4; P = .013) (Table 3). This was not true for the male patients in that age group (49.0 ± 7.9 vs 48.0 ± 9.7; P = .656). No differences were noted on any outcome measure at any time in patients (male or female) aged 55 to 65 years (Table 4). Male patients aged >65 years old who underwent tenodesis had a significantly higher 2-year SANE score (84.0 ± 23.1 vs 72.4 ± 32.0; P = .003) than their counterparts who underwent tenotomy, although this was not the case for the female patients (74.6 ± 32.4 vs 74.8 ± 31.3; P = .696). In addition, men >65 years old had slightly better ASES function and VAS scores, which approached significance but were not above the MCID (Table 5).
Table 3.
Outcomes of Tenotomy Versus Tenodesis in Patients Aged <55 Years a
| Men | Women | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Tenotomy | Tenodesis | Tenotomy | Tenodesis | |||||||
| Outcome Measure | n | Mean ± SD | n | Mean ± SD | P | n | Mean ± SD | n | Mean ± SD | P |
| Preoperative | ||||||||||
| ASES function | 31 | 13.6 ± 5.7 | 245 | 14.0 ± 6.0 | .664 | 30 | 10.8 ± 6.0 | 119 | 12.7 ± 5.4 | .052 |
| ASES index | 31 | 46.8 ± 19.9 | 244 | 48.7 ± 19.1 | .625 | 30 | 35.8 ± 16.4 | 119 | 44.0 ± 17.2 | .011 |
| SANE | 31 | 34.7 ± 20.1 | 245 | 36.9 ± 20.8 | .642 | 30 | 33.8 ± 22.7 | 118 | 37.3 ± 21.7 | .485 |
| VAS pain | 31 | 5.2 ± 2.6 | 252 | 4.9 ± 2.5 | .623 | 30 | 6.4 ± 1.8 | 120 | 5.4 ± 2.2 | .020 |
| VR-12 MCS | 31 | 49.3 ± 11.9 | 242 | 50.9 ± 11.3 | .461 | 29 | 45.3 ± 12.6 | 115 | 50.2 ± 12.6 | .051 |
| VR-12 PCS | 31 | 37.7 ± 8.7 | 242 | 36.9 ± 8.2 | .752 | 29 | 34.0 ± 7.2 | 115 | 34.8 ± 7.5 | .525 |
| 2 years | ||||||||||
| ASES function | 35 | 26.4 ± 5.4 | 272 | 26.2 ± 5.3 | .682 | 32 | 23.5 ± 7.6 | 126 | 25.5 ± 6.0 | .100 |
| ASES index | 35 | 87.4 ± 17.6 | 272 | 87.3 ± 16.7 | .809 | 32 | 78.1 ± 22.1 | 126 | 85.3 ± 18.6 | .056 |
| SANE | 35 | 75.5 ± 27.0 | 272 | 82.3 ± 20.7 | .153 | 32 | 70.4 ± 29.2 | 126 | 78.0 ± 27.7 | .061 |
| VAS pain | 35 | 1.3 ± 1.8 | 276 | 1.3 ± 1.8 | .773 | 33 | 2.2 ± 2.6 | 130 | 1.5 ± 2.1 | .332 |
| VR-12 MCS | 35 | 52.1 ± 9.2 | 270 | 54.6 ± 9.2 | .046 | 32 | 49.2 ± 11.5 | 125 | 53.3 ± 10.1 | .038 |
| VR-12 PCS | 35 | 48.0 ± 9.7 | 270 | 49.0 ± 7.9 | .656 | 32 | 42.8 ± 10.4 | 125 | 47.8 ± 9.0 | .013 |
| Δ (preoperative to 2 y) | ||||||||||
| ASES function | 31 | 12.5 ± 6.3 | 242 | 12.1 ± 6.4 | .699 | 30 | 12.4 ± 8.2 | 115 | 13.2 ± 6.5 | .634 |
| ASES index | 31 | 39.6 ± 19.4 | 241 | 38.6 ± 20.9 | .991 | 30 | 42.7 ± 22.2 | 115 | 42.5 ± 21.1 | .907 |
| SANE | 31 | 43.9 ± 29.2 | 242 | 46.1 ± 26.1 | .945 | 30 | 38.2 ± 31.8 | 114 | 40.8 ± 31.7 | .672 |
| VAS pain | 31 | -3.7 ± 2.4 | 252 | -3.6 ± 2.8 | .859 | 30 | -4.4 ± 2.4 | 120 | -4.0 ± 2.7 | .479 |
| VR-12 MCS | 31 | 2.1 ± 12.5 | 238 | 3.9 ± 11.7 | .486 | 29 | 4.2 ± 11.6 | 111 | 3.1 ± 12.5 | .732 |
| VR-12 PCS | 31 | 10.0 ± 10.3 | 238 | 12.2 ± 9.0 | .484 | 29 | 9.6 ± 9.3 | 111 | 13.5 ± 8.6 | .061 |
a Boldface P values indicate statistically significant difference by sex between treatment groups (P < .05). ASES, American Shoulder and Elbow Surgeons; MCS, Mental Component Summary; PCS, Physical Component Summary; SANE, Single Assessment Numeric Evaluation; VAS, visual analog scale; VR-12, Veterans RAND 12-Item Health Survey.
Table 4.
Outcomes of Tenotomy Versus Tenodesis in Patients Aged 55 to 65 Years a
| Men | Women | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Tenotomy | Tenodesis | Tenotomy | Tenodesis | |||||||
| Outcome Measure | n | Mean ± SD | n | Mean ± SD | P | n | Mean ± SD | n | Mean ± SD | P |
| Preoperative | ||||||||||
| ASES function | 89 | 14.4 ± 5.8 | 374 | 14.9 ± 6.0 | .331 | 77 | 12.7 ± 5.4 | 211 | 13.0 ± 5.9 | .846 |
| ASES index | 89 | 51.3 ± 16.8 | 374 | 51.7 ± 17.4 | .778 | 77 | 45.7 ± 17.2 | 211 | 44.7 ± 18.3 | .744 |
| SANE | 89 | 35.1 ± 17.3 | 372 | 36.7 ± 19.8 | .441 | 77 | 37.1 ± 22.8 | 212 | 35.8 ± 22.5 | .712 |
| VAS pain | 91 | 4.6 ± 2.2 | 380 | 4.6 ± 2.3 | .998 | 77 | 5.1 ± 2.3 | 215 | 5.4 ± 2.4 | .619 |
| VR-12 MCS | 89 | 51.2 ± 12.2 | 364 | 53.1 ± 9.8 | .488 | 76 | 50.7 ± 12.4 | 203 | 50.7 ± 11.9 | .998 |
| VR-12 PCS | 89 | 38.5 ± 7.3 | 364 | 37.7 ± 7.8 | .357 | 76 | 36.2 ± 7.5 | 203 | 35.3 ± 8.4 | .325 |
| 2 years | ||||||||||
| ASES function | 92 | 26.6 ± 4.9 | 407 | 26.8 ± 5.0 | .372 | 82 | 26.1 ± 5.4 | 240 | 25.7 ± 5.8 | .753 |
| ASES index | 92 | 89.5 ± 14.6 | 407 | 89.5 ± 15.7 | .300 | 82 | 87.8 ± 17.2 | 240 | 87.3 ± 17.4 | .980 |
| SANE | 92 | 78.9 ± 26.4 | 406 | 81.8 ± 24.1 | .252 | 82 | 79.6 ± 27.9 | 240 | 79.0 ± 28.3 | .661 |
| VAS pain | 94 | 1.0 ± 1.4 | 411 | 1.1 ± 1.8 | .364 | 83 | 1.1 ± 1.9 | 245 | 1.1 ± 1.8 | .492 |
| VR-12 MCS | 93 | 54.0 ± 9.6 | 404 | 55.3 ± 8.5 | .356 | 82 | 54.2 ± 8.5 | 236 | 54.2 ± 8.8 | .981 |
| VR-12 PCS | 93 | 48.9 ± 7.0 | 404 | 49.2 ± 7.6 | .264 | 82 | 47.6 ± 8.3 | 236 | 47.2 ± 9.5 | .745 |
| Δ (preoperative to 2 y) | ||||||||||
| ASES function | 88 | 12.6 ± 5.8 | 370 | 12.0 ± 6.6 | .554 | 76 | 13.4 ± 7.0 | 207 | 12.7 ± 7.0 | .386 |
| ASES index | 88 | 39.5 ± 16.7 | 370 | 38.2 ± 19.1 | .728 | 76 | 42.0 ± 21.6 | 207 | 42.8 ± 20.1 | .977 |
| SANE | 88 | 44.8 ± 29.1 | 367 | 45.2 ± 31.3 | .703 | 76 | 42.9 ± 34.5 | 208 | 43.5 ± 33.2 | .952 |
| VAS pain | 91 | -3.7 ± 2.2 | 380 | -3.6 ± 2.5 | .866 | 77 | -4.0 ± 2.8 | 215 | -4.3 ± 2.4 | .687 |
| VR-12 MCS | 89 | 3.0 ± 12.7 | 360 | 2.4 ± 10.1 | .919 | 75 | 3.7 ± 9.7 | 198 | 3.3 ± 11.4 | .663 |
| VR-12 PCS | 89 | 10.6 ± 8.0 | 360 | 11.6 ± 8.6 | .248 | 75 | 11.3 ± 8.3 | 198 | 11.8 ± 9.2 | .417 |
a ASES, American Shoulder and Elbow Surgeons; MCS, Mental Component Summary; PCS, Physical Component Summary; SANE, Single Assessment Numeric Evaluation; VAS, visual analog scale; VR-12, Veterans RAND 12-Item Health Survey.
Table 5.
Outcomes of Tenotomy Versus Tenodesis in Patients Aged >65 Years a
| Men | Women | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Tenotomy | Tenodesis | Tenotomy | Tenodesis | |||||||
| Outcome Measure | n | Mean ± SD | n | Mean ± SD | P | n | Mean ± SD | n | Mean ± SD | P |
| Preoperative | ||||||||||
| ASES function | 73 | 14.8 ± 6.0 | 257 | 15.1 ± 5.8 | .629 | 69 | 12.8 ± 6.2 | 183 | 13.5 ± 5.7 | .388 |
| ASES index | 73 | 52.4 ± 18.0 | 257 | 53.2 ± 17.3 | .763 | 68 | 45.3 ± 18.2 | 183 | 48.7 ± 18.9 | .246 |
| SANE | 73 | 37.9 ± 22.4 | 255 | 38.3 ± 20.1 | .729 | 69 | 38.3 ± 19.7 | 183 | 42.9 ± 23.2 | .148 |
| VAS pain | 75 | 4.5 ± 2.5 | 261 | 4.4 ± 2.3 | .719 | 68 | 5.2 ± 2.5 | 187 | 4.8 ± 2.5 | .380 |
| VR-12 MCS | 74 | 53.5 ± 9.1 | 249 | 54.7 ± 9.3 | .247 | 68 | 52.0 ± 10.4 | 184 | 54.2 ± 10.1 | .094 |
| VR-12 PCS | 74 | 39.2 ± 7.7 | 249 | 37.6 ± 7.4 | .077 | 68 | 35.8 ± 8.4 | 184 | 36.6 ± 8.6 | .452 |
| 2 years | ||||||||||
| ASES function | 78 | 26.1 ± 5.1 | 272 | 27.1 ± 4.7 | .076 | 74 | 25.4 ± 4.9 | 197 | 26.5 ± 4.9 | .036 |
| ASES index | 78 | 87.6 ± 16.9 | 272 | 90.6 ± 14.9 | .125 | 74 | 87.1 ± 14.0 | 197 | 89.2 ± 15.0 | .077 |
| SANE | 78 | 72.4 ± 32.0 | 273 | 84.0 ± 23.1 | .003 | 74 | 74.8 ± 31.3 | 198 | 74.6 ± 32.4 | .696 |
| VAS pain | 79 | 1.3 ± 2.1 | 274 | 0.9 ± 1.7 | .061 | 75 | 1.2 ± 1.8 | 198 | 1.0 ± 1.6 | .339 |
| VR-12 MCS | 78 | 57.0 ± 6.8 | 268 | 56.9 ± 6.7 | .973 | 74 | 54.2 ± 7.6 | 194 | 55.5 ± 7.8 | .113 |
| VR-12 PCS | 78 | 47.0 ± 8.6 | 268 | 48.3 ± 8.0 | .269 | 74 | 46.3 ± 8.4 | 194 | 47.6 ± 8.5 | .173 |
| Δ (preoperative to 2 y) | ||||||||||
| ASES function | 73 | 11.2 ± 7.0 | 255 | 11.9 ± 6.5 | .556 | 68 | 12.6 ± 6.3 | 182 | 13.0 ± 6.9 | .528 |
| ASES index | 73 | 34.8 ± 21.5 | 255 | 37.2 ± 18.5 | .437 | 67 | 41.2 ± 18.0 | 182 | 40.8 ± 21.8 | .969 |
| SANE | 73 | 33.3 ± 39 | 254 | 45.7 ± 28.7 | .027 | 68 | 35.0 ± 37.3 | 183 | 31.2 ± 41.3 | .568 |
| VAS pain | 75 | -3.3 ± 2.8 | 261 | -3.4 ± 2.3 | .605 | 68 | -3.9 ± 2.7 | 187 | -3.8 ± 2.8 | .765 |
| VR-12 MCS | 74 | 3.8 ± 9.2 | 244 | 2.3 ± 8.9 | .153 | 67 | 1.9 ± 11.1 | 181 | 1.5 ± 9.7 | .831 |
| VR-12 PCS | 74 | 8.0 ± 8.1 | 244 | 10.4 ± 8.7 | .053 | 67 | 10.9 ± 8.0 | 181 | 11.1 ± 10.2 | .827 |
a Boldface P values indicate statistically significant difference by sex between treatment groups (P < .05). ASES, American Shoulder and Elbow Surgeons; MCS, Mental Component Summary; PCS, Physical Component Summary; SANE, Single Assessment Numeric Evaluation; VAS, visual analog scale; VR-12, Veterans RAND 12-Item Health Survey.
Delta Analysis
The relative improvement in pain scores and the majority of the functional outcome scores were comparable between the tenotomy and tenodesis groups, regardless of sex and age group (Tables 3 -5). In general, the tenotomy group started with lower functional outcome scores (except for the VR-12 PCS) and had lower scores postoperatively compared with the tenodesis group. However, preoperative to 2-year improvement in SANE score for men aged >65 years was significantly better for tenodesis compared with tenotomy (Δ = 45.7 ± 28.7 vs 33.3 ± 39.0 points; P = .027) (Table 5). This was not the case for female patients (P = .568). Of note, the greater improvement in VR-12 PCS scores for tenodesis compared with tenotomy in female patients aged <55 years approached significance (Δ = 13.5 ± 8.6 vs 9.6 ± 9.3 points; P = .061) (Table 3). No other significant differences regarding improvement in outcome scores were identified in these stratified cohorts at 2-year follow-up.
Discussion
We found that biceps tenodesis resulted in significantly improved pain and functional scores at 2-year follow-up compared with tenotomy for each patient subgroup. However, the benefit did not exceed the previously reported MCID for these outcome measures. Despite more favorable outcomes in young, female patients who receive a tenodesis compared with a tenotomy, surgeons perform a tenotomy in young female patients at a greater rate compared with their male counterparts. Older male patients compared with younger men were more likely to receive a tenotomy despite significantly improved functional outcome scores noted with tenodesis. This study represents the largest comparative cohort study to date reviewing biceps tenotomy versus tenodesis in the setting of concomitant RCR, with a total of 1537 tenodesis patients and 399 tenotomy patients included for review.
One prospective randomized controlled trial has been published demonstrating improved pain scores for patients with biceps tenotomy compared with biceps tenodesis 3 months after surgery, but there was no difference in pain scores 2 years after surgery. 3 To date, most studies (including large meta-analyses) have not been able to demonstrate a consistent difference in pain or functional outcome scores when comparing these 2 procedures in the setting of concomitant rotator cuff repair. 13,14,16,18 –21,23,25 As a result, authors have concluded that the decision to proceed with tenotomy or tenodesis should be based on patient and surgeon preferences. However, all these studies are likely underpowered: the largest study had 252 patients included (202 tenotomy and 50 treated with tenodesis). 5 The other studies ranged from 20 to 151 patients. 13,14,16,18 –21,23,25 An appropriately powered study may be able to detect a difference in pain scores and/or functional outcomes when comparing these 2 procedures.
Recently, 7 systematic reviews have been performed comparing biceps tenotomy versus tenodesis. 2,4,15,17,22,24,30 Most of these reviews did not demonstrate a significant functional difference between these 2 procedures. Popeye deformity and cramping were more common after tenotomy than with tenodesis. The review by Liu et al 17 demonstrated decreased supination strength and worse Constant and Simple Shoulder Test scores after tenotomy. Ahmed et al 2 and Zhou et al 30 similarly demonstrated lower Constant scores after tenotomy.
In contrast to previous studies, the results of this study demonstrated significantly improved VAS pain and functional outcomes (ASES, SANE, VR-12) scores for patients with biceps tenodesis compared with biceps tenotomy in patients with concomitant rotator cuff repair at 2-year follow-up. However, differences between procedures at 2-year follow-up did not exceed the MCID. Therefore, the presence of a clinical benefit for patients who receive biceps tenodesis over tenotomy remains uncertain. This study also demonstrated that patients undergoing tenotomy were more likely to be older than 65 years. In patients younger than 65, tenotomy was used at a greater rate in female compared with male patients. This trend regarding the surgical procedure is concerning given that, when stratified according to age and sex, older male patients (>65 years) had improved functional outcome scores with a tenodesis, as was the case with female patients between the ages of 35 and 54 years. Instead of relying on conventional generalizations for patient selection, surgeons should consider individualized discussion with each patient and choose between tenotomy and tenodesis according to the patient’s preferences (eg, physical activity, cosmesis, recovery period).
The data from this study also suggest a procedural choice bias in favor of tenodesis compared with tenotomy. Of the 1936 RCRs included, a biceps tenotomy was only performed in 21% (n = 399) of cases. Tenodesis may be more common due to patient preference, surgeon preference, and/or industry influence. Based on the data presented herein, surgeons who strongly prefer (or perform only) biceps tenodesis may consider performing biceps tenotomy in selected patients.
Limitations
A limitation of this study is that it was a retrospective review, and the findings are therefore subject to lack of control over exposure factor, covariates, and potential confounders such as type of tenodesis implant (suture anchors, endobutton, bone tunnels, tenodesis screw) and/or location of tenodesis (intra-articular, suprapectoral, subpectoral). Because this is a retrospective review, patients included may not be representative of the general population and there is likely a selection bias. Furthermore, a greater proportion of female patients received a biceps tenotomy in the younger than 55 years and 55- to 65-year age groups, potentially introducing selection bias. We attempted to control for this by comparing outcomes after stratifiying our cohort based on age and sex. There were likely other factors that were considered but not recorded in the database that may have affected the surgeons’ decisions to perform a tenodesis or tenotomy. For example, we were unable to stratify the data according to the type of biceps pathology present and compare the results of tenotomy and tenodesis with no treatment. Furthermore, data regarding size of the rotator cuff tear, postoperative infection, nerve injury, muscle cramping, cosmesis, and strength were not available for comparison of tenotomy versus tenodesis given the nature of the database. Finally, recall bias and misclassification bias are also potentially present, given the nature of this global database with several surgeon contributors.
Conclusion
Biceps tenodesis generally resulted in significantly improved pain and functional scores compared with tenotomy for each patient subgroup at 2-year follow-up. However, the benefit did not exceed previously reported MCID for outcome scores after RCR. Despite more favorable outcomes in young female patients who received a tenodesis compared with a tenotomy, surgeons perform a tenotomy in young female patients at a greater rate compared with in their male counterparts. Compared with younger men, older male patients were more likely to receive a tenotomy despite significantly improved functional outcome scores noted with tenodesis. Both procedures provide improvement in pain and functional outcomes. Therefore, the choice of procedure should be a shared decision between the surgeon and patient.
Acknowledgment
The authors thank the OMeGA Medical Grants Association for supporting the University of Florida Shoulder and Elbow Surgery Fellowship, thus helping make this work possible.
Final revision submitted April 6, 2022; accepted May 12, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: R.C.S. has received education payments from MedInc, speaking fees from Acumed, and hospitality payments from Integra LifeSciences. T.W.W. has received consulting fees and royalties from Exactech. K.W.F. has received education payments from Exactech; consulting fees from Arthrex, Exactech, and Flexion Therapeutics; speaking fees from Arthrex, Arthrosurface, and CGG Medical; honoraria from Arthrosurface and Baudax Bio; and hospitality payments from Rotation Medical. J.O.W. has received education payments from Pinnacle and hospitality payments from Acumed and Zimmer Biomet. R.P.R. has received grant support from Arthrex and education payments from Arthrex and Smith & Nephew. M.W.M. has received education payments from Fortis Surgical and speaking fees from Arthrex. M.C.F. has received hospitality payments from Arthrex. J.J.K. has received consulting fees from Exactech and hospitality payments from Integra LifeSciences. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of Florida (ref. No. IRB202100420).
References
- 1. Aflatooni JO, Meeks BD, Froehle AW, Bonner KF. Biceps tenotomy versus tenodesis: patient-reported outcomes and satisfaction. J Orthop Surg Res. 2020;15(1):56. doi:10.1186/s13018-020-1581-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ahmed AF, Toubasi A, Mahmoud S, Ahmed GO, Al Ateeq Al Dosari M, Zikria BA. Long head of biceps tenotomy versus tenodesis: a systematic review and meta-analysis of randomized controlled trials. Shoulder Elbow. 2021;13(6):583–591. doi:10.1177/1758573220942923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Belay ES, Wittstein JR, Garrigues GE, et al. Biceps tenotomy has earlier pain relief compared to biceps tenodesis: a randomized prospective study. Knee Surg Sports Traumatol Arthrosc. 2019;27(12):4032–4037. doi:10.1007/s00167-019-05682 -1 [DOI] [PubMed] [Google Scholar]
- 4. Belk JW, Kraeutler MJ, Houck DA, Chrisman AN, Scillia AJ, McCarty EC. Biceps tenodesis versus tenotomy: a systematic review and meta-analysis of level I randomized controlled trials. J Shoulder Elbow Surg. 2021;30(5):951–960. doi:10.1016/j.jse.2020.11.012 [DOI] [PubMed] [Google Scholar]
- 5. Biz C, Vinanti GB, Rossato A, Arnaldi E, Aldegheri R. Prospective study of three surgical procedures for long head biceps tendinopathy associated with rotator cuff tears. Muscles Ligaments Tendons J. 2012;2(2):133–136. [PMC free article] [PubMed] [Google Scholar]
- 6. Cho NS, Cha SW, Rhee YG. Funnel tenotomy versus intracuff tenodesis for lesions of the long head of the biceps tendon associated with rotator cuff tears. Am J Sports Med. 2014;42(5):1161–1168. doi:10.1177/0363546514523719 [DOI] [PubMed] [Google Scholar]
- 7. Cvetanovich GL, Gowd AK, Liu JN, et al. Establishing clinically significant outcome after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2019;28(5):939–948. doi:10.1016/j.jse.2018.10.013 [DOI] [PubMed] [Google Scholar]
- 8. De Carli A, Vadalà A, Zanzotto E, et al. Reparable rotator cuff tears with concomitant long-head biceps lesions: tenotomy or tenotomy/tenodesis? Knee Surg Sports Traumatol Arthrosc. 2012;20(12):2553–2558. doi:10.1007/s00167-012-1918-5 [DOI] [PubMed] [Google Scholar]
- 9. Hong CK, Chang CH, Hsu KL, Kuan FC, Wang PH, Su WR. Patients older than 55 years prefer biceps tenodesis over tenotomy to the same degree as young patients. J Orthop Sci. 2020;25(3):416–422. doi:10.1016/j.jos.2019.05.007 [DOI] [PubMed] [Google Scholar]
- 10. Hufeland M, Wicke S, Verde PE, Krauspe R, Patzer T. Biceps tenodesis versus tenotomy in isolated LHB lesions: a prospective randomized clinical trial. Arch Orthop Trauma Surg. 2019;139(7):961–970. doi:10.1007/s00402-019-03136-4 [DOI] [PubMed] [Google Scholar]
- 11. Ikemoto RY, Pileggi PE, Murachovsky J, et al. Tenotomy with or without tenodesis of the long head of the biceps using repair of the rotator cuff. Rev Bras Ortop. 2015;47(6):736–740. doi:10.1016/S2255-4971(15)30031-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kim DM, Kim TH, Kholinne E, et al. Minimal clinically important difference, substantial clinical benefit, and patient acceptable symptomatic state after arthroscopic rotator cuff repair. Am J Sports Med. 2020;48(11):2650–2659. doi:10.1177/0363546520943862 [DOI] [PubMed] [Google Scholar]
- 13. Kim J, Nam JH, Kim Y, Kim JS, Kim SH. Long head of the biceps tendon tenotomy versus subpectoral tenodesis in rotator cuff repair. Clin Orthop Surg. 2020;12(3):371–378. doi:10.4055/cios19168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Koh KH, Ahn JH, Kim SM, Yoo JC. Treatment of biceps tendon lesions in the setting of rotator cuff tears: prospective cohort study of tenotomy versus tenodesis. Am J Sports Med. 2010;38(8):1584–1590. doi:10.1177/0363546510364053 [DOI] [PubMed] [Google Scholar]
- 15. Kooistra B, Gurnani N, Weening A, van Deurzen D, van den Bekerom M. Tenotomy or tenodesis for tendinopathy of the long head of the biceps brachii: an updated systematic review and meta-analysis. Arthrosc Sports Med Rehabil. 2021;3(4):e1199–e1209. doi:10.1016/j.asmr.2021.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kukkonen J, Rantakokko J, Virolainen P, Aärimaa V. The effect of biceps procedure on the outcome of rotator cuff reconstruction. ISRN Orthop. 2013;2013:840965. doi:10.1155/2013/840965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Liu H, Song X, Liu P, Yu H, Zhang Q, Guo W. Clinical outcomes of arthroscopic tenodesis versus tenotomy for long head of the biceps tendon lesions: a systematic review and meta-analysis of randomized clinical trials and cohort studies. Orthop J Sports Med. 2021;9(4):2325967121993805. doi:10.1177/2325967121993805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. McCrum CL, Alluri RK, Batech M, Mirzayan R. Complications of biceps tenodesis based on location, fixation, and indication: a review of 1526 shoulders. J Shoulder Elbow Surg. 2019;28(3):461–469. doi:10.1016/j.jse.2018.09.005 [DOI] [PubMed] [Google Scholar]
- 19. Meraner D, Sternberg C, Vega J, Hahne J, Kleine M, Leuzinger J. Arthroscopic tenodesis versus tenotomy of the long head of biceps tendon in simultaneous rotator cuff repair. Arch Orthop Trauma Surg. 2016;136(1):101–106. doi:10.1007/s00402-015-2343-2 [DOI] [PubMed] [Google Scholar]
- 20. Na Y, Zhu Y, Shi Y, et al. A meta-analysis comparing tenotomy or tenodesis for lesions of the long head of the biceps tendon with concomitant reparable rotator cuff tears. J Orthop Surg Res. 2019;14:370. doi:10.1186/s13018-019-1429-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Oh JH, Lee YH, Kim SH, et al. Comparison of treatments for superior labrum-biceps complex lesions with concomitant rotator cuff repair: a prospective, randomized, comparative analysis of debridement, biceps tenotomy, and biceps tenodesis. Arthroscopy. 2016;32(6):958–967. doi:10.1016/j.arthro.2015.11.036 [DOI] [PubMed] [Google Scholar]
- 22. Patel BH, Agarwalla A, Lu Y, et al. Isolated biceps tenodesis and tenotomy: a systematic review of indications and patient satisfaction. Orthopedics. 2021;44(6):333–340. doi:10.3928/01477447-20211001-04 [DOI] [PubMed] [Google Scholar]
- 23. Patel KV, Bravman J, Vidal A, Chrisman A, McCarty E. Biceps tenotomy versus tenodesis. Clin Sports Med. 2016;35(1):93–111. doi:10.1016/j.csm.2015.08.008 [DOI] [PubMed] [Google Scholar]
- 24. Pozzetti Daou J, Nagaya DY, Matsunaga FT, Sugawara Tamaoki MJ. Does biceps tenotomy or tenodesis have better results after surgery? A systematic review and meta-analysis. Clin Orthop Relat Res. 2021;479(7):1561–1573. doi:10.1097/CORR.0000000000001672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sentürk I, Ozalay M, Akpınar S, Leblebici B, Cınar BM, Tuncay C. Clinical and isokinetic comparison between tenotomy and tenodesis in biceps pathologies. Acta Orthop Traumatol Turc. 2011;45(1):41–46. doi:10.3944/AOTT.2011.2308 [DOI] [PubMed] [Google Scholar]
- 26. Shang X, Chen J, Chen S. A meta-analysis comparing tenotomy and tenodesis for treating rotator cuff tears combined with long head of the biceps tendon lesions. PLoS One. 2017;12(10):e0185788. doi:10.1371/journal.pone.0185788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Tashjian RZ, Shin J, Broschinsky K, et al. Minimal clinically important differences in the American Shoulder and Elbow Surgeons, Simple Shoulder Test, and visual analog scale pain scores after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2020;29(7):1406–1411. doi:10.1016/j.jse.2019.11.018 [DOI] [PubMed] [Google Scholar]
- 28. Virk MS, Cole BJ. Proximal biceps tendon and rotator cuff tears. Clin Sports Med. 2016;35(1):153–161. doi:10.1016/j.csm.2015.08.010 [DOI] [PubMed] [Google Scholar]
- 29. Zhang Q, Zhou J, Ge H, Cheng B. Tenotomy or tenodesis for long head biceps lesions in shoulders with reparable rotator cuff tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc. 2015;23(2):464–469. doi:10.1007/s00167-013-2587-8 [DOI] [PubMed] [Google Scholar]
- 30. Zhou P, Liu J, Deng X, Li Z. Biceps tenotomy versus tenodesis for lesions of the long head of the biceps tendon: a systematic review and meta-analysis of randomized controlled trials. Medicine. 2021;100(3):e23993. doi:10.1097/MD.0000000000023993 [DOI] [PMC free article] [PubMed] [Google Scholar]