Abstract
Online health-specific goal challenge groups gather people with the same health concerns and provide an environment to keep on track, exchange experiences, and compete for achievements. We examine how group health status composition influences social contact, and how both group health status composition and social contact affect individual health achievement. Using longitudinal data from 2479 online health challenge group users and their corresponding group information, we found that (a) compared with individual health status, group conditions (average weight status and member affiliation) are more strongly connected with social contact; (b) different mechanisms affect whether people participate in social contact and increase their participation, and weight loss; and (c) average group condition influences individuals’ weight loss through social contact. We emphasize the effect of group composition and the social contact process in health enhancement.
Keywords: Goal-attaining groups, health communication, social contact, social influence, weight management
With the popularization of online health communities such as FatSecret and breastcancer.org, people with similar health concerns gather together, keep on track, exchange experiences, and compete for achievements. Although achieving better health is an individual goal, it is broadly recognized that social groups are impactful during the process, even if people bond with strangers or are only provided with virtual cues.1,2 The question that remains unanswered is what group characteristics are beneficial for individual health achievement, and how social contact affects the process. Online health-specific goal challenge groups, which allow members to compare health status and interact with each other, provide opportunities to carefully examine the group factors, and interactive dynamics that make a group more successful.
Focusing on online weight loss goal challenge groups, we explored how group compositions and the relationship between individual status and social contact affect individual health outcomes. Overall, this is a fruitful and necessary extension of research on both health management and social identification in groups. Our results are instructive for the design of health communities and group-based intervention.
Literature review
Online health-specific goal challenge groups
Online health-specific goal challenge groups are online groups that afford members a place for health goal tracking, competition, and discussion. Different from online health communities, goal challenge groups make personal statuses more transparent and health goals more explicit. In these groups, members update their goal-attaining processes at regular intervals, watch their up-to-date rankings compared with other members, and communicate with other members based on social cues. This facilitates the comparison and identification process. It also provides opportunities to observe the dynamic relationship among group compositions, social contact, and health goal achievement. Compared to individual goal achievement and social support environments, groups with a competitive setting can dramatically enhance health behavior.3–5 However, only limited research examines the health enhancement process through the practices of goal challenge groups.
Individual health goal achievement in social groups
Improving one’s health status is usually an individual pursuit, but it is broadly recognized that social relationships and social contexts in the goal-achieving procedure have powerful effects.1,2 Serving as an “important and underappreciated” route to individual health, 6 it is necessary to see how structured group-level characteristics, especially average demographic levels and diversity, act through the social identification process.
Social identity arises from comparing oneself to accessible group characteristics such as gender and ethnicity and classifying oneself into social categories. 7 Through the comparison and evaluation process, people generate the concepts of “I” and “We.” Identity and identity comparison within a community influence various individual attitudes and behaviors including involvement, internalization, and attitude toward change. 8
Although the comparison to accessible characteristics does not represent the full scope of social identification, 9 it should not be ignored in the context of online health goal-achieving groups because highlighting others’ statuses without deeper contact is effective enough to differentiate individuals’ goal satisfaction, goal acceptance, and final performance.10,11 Further, the sensation of engaging in online communities heavily relies on textual cues not only the language people use to communicate but also information cues presented in those communities.
In the context of online health intervention, several characteristics of group status composition have been highlighted as closely related to the comparison process. One group of researchers considers the diversity of members’ health status. According to the social identification process, a group plays a role when it manifests a prototype in a member’s cognition. A central approach to facilitating prototype perception is to maximize within-group similarities and between-group dissimilarities. 12 Empirical studies support the notion that member similarity is beneficial. Under a controlled experiment, Centola 10 found that the exposure to health innovations and the adoption of health behavior were much more likely when participants were in a homogeneous rather than a heterogeneous network. It is easier for homogeneous groups to trigger downward comparison, which substantially encourages health behavior. 3
The discrepancy between individual and group statuses also plays a role. Maladaptation emerges when there are mismatches between person and environment. 13 When low health status individuals meet higher health status people, their body dissatisfaction will increase and they may motivate themselves to exercise more.14,15 On the other hand, when high-status people are with lower-status members, appearance evaluations will also be activated. 16 However, the existing literature has conflicting findings on whether upward or downward comparison is more effective. Rancourt et al. 15 showed that upward comparison is better for improving dieting and exercising thoughts. In the context of food consumption, downward comparison is more influential. 3
Social contact and health enhancement
At the same time, it is necessary to look at the role of social contact. As another key pathway through which social networks affect health outcomes, 6 social contact describes levels of participation within a community. A considerable amount of literature supports the beneficial influence of social contact on weight loss (e.g. Kim et al., 17 Pappa et al. 18 ). Through social contact, people can empower themselves and correspondingly enhance their well-being. 19 Engaging in group interactions could further help people gain feedback, encouragement, useful information, and suggestions for coping strategies, 20 which are all crucial for health. Even if their actions are not reciprocated, their communicative behavior is still a powerful factor that can help overcome health risks. 21
Generally speaking, social contact intertwines with both group and individual factors, and it substantially affects health outcomes. We propose that group-level characteristics influence individual health outcomes through individual contact behavior. First, as a socializing behavior, social contact is determined by comparison with other group members. 22 Second, the quality of exchanges could mediate the individual–group fit’s effect on both member and team performance.23,24 Without group communication, collective-oriented groups’ performance becomes poorer. 25 Third, the salience of group characteristics depends on temporal stages of individual engagement. 26 At the beginning of group selection and goal setting, global environmental factors dominate. Once people commit to joining a group and start the process of goal attainment, the original match becomes part of the background. The socialization process then acts as an additional determinant, easing individual–group fit and aiding performance.
Current study
We explored the influence of group compositions and social contact on individual health outcomes. Using data from online weight loss goal challenge groups, we extend the previous work on social identification and health management in several ways.
First, we employed a longitudinal study, which better describes the interaction, development, and variation across socialization. This is important because, in health issues, people appraise their power and influence relative to others moment by moment, and then adjust their subsequent behavior. 27 Longitudinal analysis can further distinguish between social influence and social selection mechanisms. Influence-driven contagion is related to social norms and social learning, whereas selection-driven health diffusion processes are governed by similarity and complementary attraction mechanisms. Aral et al. 28 found that election and impact evenly explain the perceived behavioral contagion, which is overestimated by 300%–700% in traditional models.
Second, existing health intervention strategies usually take an individual-centric perspective, neglecting the interactions and influences between individuals and other group members. However, it is still unclear how group dynamics influence individual in-group activity and health outcomes.
Third, previous studies have mainly used experimental settings to conduct health interventions and surveys to measure relative behaviors. The external validity of such studies is unknown. With the prevalence of social networking sites, it is possible to observe the health communication process unobstructively on one hand while updating the existing findings in the new digital setting on the other. If self-organized online groups are effective at creating positive health outcomes, organizations and individuals can utilize this cost-effective method to implement interventions.
Finally, we particularly focused on health-specific goal-attaining groups. Little is known about the group dynamics or influence mechanisms of this health-specific community. Meanwhile, the context of our study is weight loss. Different from adopting health innovations,3,10 weight management requires continuous effort and changes in both attitude and physical behavior. Given that there are substantive intention–behavior gaps, 29 we go beyond merely looking into intentions and adoptions to physical changes and long-term maintenance. This can be seen as a fruitful and necessary extension of both health management and goal-oriented group dynamics research.
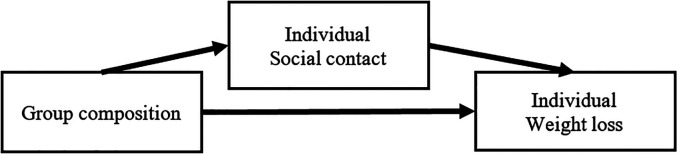
Based on our literature review, we hypothesized that group composition (the diversity of members’ health status and the fit between individual and group health status) should be related to individual weight loss, whereas social contact should mediate the relationship between group composition and individual weight loss (see Figure 1).
Figure 1.
Conceptual mediation model.
Methods
Data collection
The online weight management community we focused on in this study is Bohee community. It is the largest Chinese online weight management community, and a majority of its users are young women. 30 It provides diverse social networking services, such as a forum, personal homepage (with blogs and self-tracking services), and health-specific goal challenge groups. Health-specific goal challenge groups at Bohee, which are the focus of this study, were first established in October 2007. Before the goal challenge groups were closed down in February 2012, 1057 groups had been set up and 45,814 members had joined.
Bohee offered two main services for goal challenge groups. One was the group discussion, which was in a discussion forum format, and the other was goal challenge activities. Group managers could set up weight loss tasks such as exercise, weight loss, or body shaping in a specific period. Users in Bohee are free to select whether or not to join the goal challenge groups and which group to join. They can access each groups’ information at the home page of challenge groups or by URLs promoted by other Bohee users. Members registered in the group task were expected to report their current body information (weight, waistline, etc.) in a given interval. Sorted by weight change volume, all the reported data (original weight, target weight, current weight, weight loss, and ranking) for each interval were shown in a sheet format on the group’s main page.
Using an automatic scraping Python program, we collected all goal attainment information, including group information, member information, group discussion, and task achievement tables. To enrich the user information, we also extracted profile information and self-tracking weight statistics from each user’s publicly available personal pages.
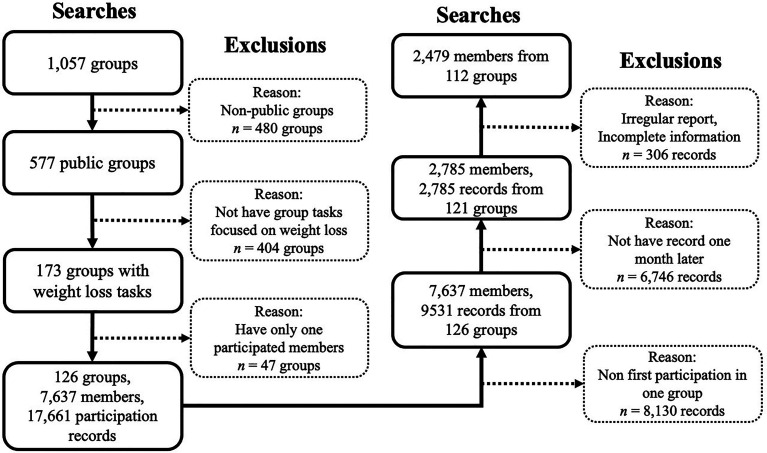
We filtered out the groups that did not concentrate on weight loss and did not set up goal-attaining tasks. Because people could participate in multiple groups and be exposed to various group environments, we focused on their first registration of a challenge task in a group. Then, we selected those who recorded their weight around a month later (30 ± 5 days), whether in the groups or from self-tracking services on their personal pages. This resulted in a sample of 2479 participants whose statuses and corresponding group information were included in our analysis. The detailed data cleaning process is shown in Figure 2.
Figure 2.
Data cleaning process.
Measurements
We focused on both individual- and group-level variables. From a longitudinal perspective, our data were divided into four phases: before registration (Time 0), individual and group health status upon registration (Time 1), individual and group participation during the month (Times 1–2), and individual health status one month after registration (Time 2).
Individual weight status
Two variables described individual weight status. The first, individual BMI (I_BMI), was calculated by dividing each person’s weight by their height squared. Higher BMI indicates lower health status. We calculated the variable weight change for a given individual by subtracting the Times 1’s BMIs from Time 2’s BMI.
The second variable, target difficulty (Time 1), reflected the level of difficulty a user settled for in terms of their health intervention. At registration, users had to report their target weight and current weight. We measured target difficulty by dividing the difference between current weight and target weight by current weight. A greater target difficulty score meant that a user settled on a harder goal.
We included each individual’s condition before Time 1 to control for the influence of participation history. We measured membership length (Time 0) as the number of days since registration, log transformed. Past participation (Time 0) was defined as the existing number of weight recordings in all goal challenge groups before Time 1.
User affiliation
User affiliation (Time 1) reflected users’ positions in the group. We coded this variable as 1 = unassigned member (65.06%), 2 = subgroup member (31.3%), 3 = subgroup leader (1.0%), and 4 = group manager (2.6%). A group manager is a creator or assistant creator of each group. They are all ordinary users in the Bohee community rather than officials or professionals. They were responsible for designing regulations and organizing member participation. Within each group, members could be assigned to different subgroups based on levels of original and target weights, participation history, or similar interests. Subgroup leaders voluntarily coordinated subgroup members. Notably, setting up subgroups was not compulsory among this weight loss community. Some groups had no subgroups, and many members were unassigned in groups containing subgroups.
Social contact
Social contact (Times 1–2) was reflected by individual in-group communicative activities. We measured this based on the number of posts the user posted in the group during the period (also referred to as out-replies). In addition, in-replies—that is, the number of replies people received during the period—were also taken into analysis.
Place of report
This variable was collected at Time 2. Some users did not report their weight directly in the groups after a month (due to the task period limitation or concerns about self-disclosure); we classified these users as 1 = reported in a group (22.4%) or 0 = reported on the self-profile page (77.6%).
Group-level variables
Group condition was determined by summarizing the weight status of the group members. Group elevation (Time 1) was represented by the group means of users’ BMIs. Because the context of this study was weight loss, a relatively high group elevation score indicated greater mean weight and an unhealthy group condition. Group diversity (Time 1) was represented by the standard deviation of the members’ BMIs. We further identified users whose BMIs were either above 24 or below 18.5 (the boundaries of healthy weight), then calculated the percentages of such users in each group to find groups’ levels of abnormal weight conditions (Group % Above 24, Group % Below 18.5). To explore the role of the individual–group fit, we analyzed the interaction between centralized individual weight and group elevation. Group participation is the number of weight recordings by all members during the period. It indicates the size of the group participation.
Analysis
We analyzed our data in three steps. In the first step, we explored how individual–group status influences social contact. Considering that social contacts were highly skewed (a majority of users did not participate, or only participated once), we applied the zero-hurdle model. 31 This model is beneficial for overdispersed data and is good at distinguishing between and identifying the probability of detecting a positive count from zero and the probability of detecting a positive count among those already activated. First, we applied the zero-hurdle model based on probit regression, then we found the zero-truncated negative binomial regression for the count data.
In the second step of our data analysis, we explored how individual–group status contributed to the final weight change. We employed a hierarchical linear model for analysis identifying variables at either the user or group level.
In the third step, we explored how individual–group status along with social contact contributed to final weight changes. Given our literature review and the results of the first step, we conducted mediation analyses among the group elevation and out replies and tested the robustness of the mediation model. All analyses were conducted using R.
Results
The descriptive statistics are shown in Table 1. Based on the BMI classification, 32 at Time 1, 125 (4.71%) users’ BMIs were below 18.5 (underweight), 1873 (70.52%) users had BMIs between 18.5 and 24.9 (normal weight), 540 (20.33%) users had BMIs between 25 and 29.9 (overweight), and 105 (3.95%) users had BMIs of 30 or greater (obese). At Time 2, 159 (5.99%) users are below 18.5, 1938 (72.97%) users are between 18.5 and 24.9, 470 (17.70%) users had BMIs between 25 and 29.9, and 76 (2.86%) users had BMIs of 30 or greater. National surveys in 2009 showed 7.4% of female adults were underweight, 26.1% were overweight and 4.7% were obese, 33 with an average BMI of 23.16 ± 3.37. 34
Table 1.
Descriptive statistics.
| Variables | Mean/Percentage | SD | Min | Max |
|---|---|---|---|---|
| Time 0 | ||||
| # Past participation | 29.68 | 22.11 | 1 | 80 |
| Membership length (Days) | 223.77 | 311.48 | 0 | 2190 |
| Target difficulty (%) | 0.17 | 0.09 | 0 | 0.56 |
| Time 1 | ||||
| User affiliation (%) | ||||
| Unassigned member | 65.06 | |||
| Subgroup member | 31.3 | |||
| Subgroup leader | 1.0 | |||
| Group manager | 2.6 | |||
| I_BMI Time 1 (kg/m2) | 23.16 | 3.37 | 15.24 | 37.46 |
| Group % Above 24 (%) | 0.40 | 0.49 | 0 | 1 |
| Group % Below 18.5 (%) | 0.03 | 0.18 | 0 | 1 |
| Group Diversity (kg/m2) | 2.74 | 0.71 | 0.12 | 7.62 |
| Group Elevation (kg/m2) | 22.85 | 1.71 | 15.39 | 29.52 |
| Time 1–2 | ||||
| # Out replies | 1.65 | 6.42 | 0 | 132 |
| # In replies | 1.95 | 13.23 | 0 | 428 |
| # Group participation | 67.63 | 52.88 | 1 | 341 |
| Time 2 | ||||
| I_BMI Time 2 (kg/m2) | 22.69 | 3.20 | 14 | 36.8 |
| Weight Change (kg/m2) | −0.02 | 0.03 | −0.13 | 0.15 |
| Place of Report (%) | ||||
| Reported in a group | 22.4 | |||
| Reported on the self-profile page | 77.6 |
Second, we examined factors influencing social contacts (see Table 2 for results). In terms of user affiliation, higher group position greatly increased social contacts (Exp[β]in−replies, 1 = 1.472, p < 0.001; Exp[β]in−replies, 2 = 1.984, p < 0.001; Exp[β]out−replies, 1 = 1.554, p < 0.001; Exp[β]out−replies, 2 = 2.095, p < 0.001). Membership length was detrimental for contact initiation, but beneficial for increases in contacts (Exp[β]in−replies, 1 = 0.920, p < 0.01; Exp[β]in−replies, 2 = 1.314, p < 0.001; Exp[β]out−replies, 1 = 0.968, p > 0.05; Exp[β]out−replies, 2 = 1.336, p < 0.05). Target difficulty was positively related to increased in- and out-replies (Exp[β]in−replies = 14.822, p < 0.05; Exp[β]out−replies = 47.630, p < 0.05). That means a harder weight-loss goal corresponds to more social contact. In terms of weight conditions, individual weight at Time 1 showed a nonsignificant relationship with all social contact behaviors (p > 0.05). Instead, group elevation activated users to participate. The greater a group’s mean weight, the more possible it was for members to initiate communication within the group (Exp[β]in−replies = 1.225, p < 0.001; Exp[β]out−replies = 1.173, p < 0.05). However, this trend was reversed when group elevations were extremely high (i.e. percentage of members’ BMI above 24, Exp[β]in−replies = 0.262, p < 0.001; Exp[β]out−replies = 0.308, p < 0.001). At the same time, we detected conflicting effects of the percentage of members whose BMIs were below 18.5 (Exp[β]in−replies = 0.000, p < 0.001; Exp[β]out−replies = 0.001, p < 0.001). People in a group containing slimmer members decreased their in and out-replies. We also observed an interaction effect of individual–group fit on the initiation of in-replies (Exp[β]in−replies = 0.989, p < 0.05). Simple slope analysis further showed that when individual weights were relatively low, a greater average level of group weight increased the possibility of receiving replies (β = 0.23, p < 0.05). When individual’s initial weights were relatively high, this group effect was nonsignificant (β = 0.16, p = 0.07).
Table 2.
Influence of individual-group fit on support-related behavior using zero hurdle modeling.
| Independent variables | # Out replies | # In replies | ||
|---|---|---|---|---|
| Zero hurdlea | Counta | Zero hurdlea | Counta | |
| (Intercept) | 0.643** | 0.000 | 0.330*** | 0.000 |
| # Past participation | 0.951 | 1.182 | 0.921* | 1.082 |
| Membership lengthb | 0.920** | 1.314*** | 0.968 | 1.336* |
| User affiliation | 1.472*** | 1.984*** | 1.554*** | 2.095*** |
| Target difficulty | 0.621 | 14.822* | 1.011 | 47.630* |
| I_BMI Time 1 | 1.000 | 1.001 | 1.012 | 0.919 |
| Group % Above 24 | 0.262*** | 0.090 | 0.308** | 0.279 |
| Group % Below 18.5 | 0.545 | 0.000*** | 0.198* | 0.001* |
| Group Diversity | 0.969 | 0.928 | 1.024 | 0.987 |
| Group Elevation | 1.225*** | 1.223 | 1.173* | 0.973 |
| Group Elevation × I_BMI | 0.995 | 1.009 | 0.989* | 1.014 |
| Group participation | 1.008 | 0.846 | 1.007 | 1.272 |
| Observations | 2479 | 2479 | ||
| Log Likelihood | −3141.605 | −2230 | ||
| Akaike Information Criteria | 6333.21 | 4462.69 | ||
| R 2 | 0.776 | 0.871 | ||
*p < 0.1; **p < 0.05; ***p < 0.01.
Exponentiated coefficients.
Log transformation.
We tested factors contributing to the final weight change in the third step of our analysis. As shown in the right column of Table 3, weight gain was positively related to users’ membership length (β = 0.171, p < 0.001). Weight loss was related to past participation in goal challenge groups (β = −0.106, p < 0.05), out-replies (β = −0.232, p < 0.01), whether people disclosed their weight in the group at Time 2 (β = −0.370, p < 0.01), and the percentage of underweight members within the group (β = −2.571, p < 0.01). Individual–group fit also played a role (β = 0.019, p < 0.001). Simple slope analysis showed that when individual weight was relatively low, a higher average level of group weight status updates had a beneficial influence on weight loss (β = −0.22, p < 0.05). When individual initial weight was relatively high, this effect was nonsignificant (β = −0.09, p > 0.05).
Table 3.
Hieratical linear analysis results.
| Independent variables | Dependent variable | ||
|---|---|---|---|
| # Out repliesc | Weight Change (Model 1) | Weight Change (Model 2) | |
| (Intercept) | −0.594** | −1.035*** | −0.983*** |
| # Past participation | −0.044 | −0.106* | −0.106* |
| Membership lengthb | −0.118*** | 0.178*** | 0.171*** |
| User affiliation | 0.466*** | −0.006 | 0.007 |
| Target difficulty | −0.744 | −0.705 | −0.747 |
| I_BMI Time 1 | −0.005 | −0.152*** | −0.153*** |
| Group % Above 24 | −1.609** | 0.176 | 0.121 |
| Group % Below 18.5 | 0.218 | −2.602** | −2.571** |
| Group Diversity | −0.090 | 0.059 | 0.053 |
| Group Elevation | 0.276*** | −0.163** | −0.152* |
| Group Elevation × I_BMI | −0.005 | 0.019*** | 0.019*** |
| Group participation | −0.052 | 0.061 | 0.061 |
| Place of Report | −0.391*** | −0.370*** | |
| # In repliesc | 0.104 | 0.244* | |
| # Out repliesc | −0.232** | ||
| Observations | 2479 | ||
| Log Likelihood | −1361.27 | −4819.477 | −4817.60 |
| Akaike Inf. Crit. | 2748.54 | 9670.96 | 9669.19 |
| conditional R2 | 0.292 | 0.166 | 0.169 |
Log transformation.
Binary coding, probit regression is applied.
Based on the results of the previous step and the right column of Table 3, we conducted a mediation test with 1000 bootstraps among group elevation, out-replies, and weight change at Time 2. The results showed that the influence of group elevation on weight change was mediated by out-replies (see Tables 3 and 4). Group elevation was beneficial for out-replies, and out-replies increased the likelihood of weight loss.
Table 4.
Mediation test of group elevation on weight change mediated by out replies.
| Variables | Estimate | 95% CI |
|---|---|---|
| Average causal mediation effect | −0.02** | (−0.04, 0.00) |
| Average direct effect | −0.15* | (−0.31, 0.00) |
| Total effect | −0.17* | (−0.33, −0.02) |
| Prop. mediated | 0.11* | (0.01, 0.66) |
Discussion
Using data from online user logs, we explored how individual and group factors intertwine with each other to influence sequential group participation and individual health outcomes.
We found that rather than individual health condition, group status composition is more beneficial to push members to participate. Among the individual factors, rather than individual weight status, user affiliation and time engaged in the community enhanced social contact. This is because these are indicators of how people engage in the community. Moreover, when attached to social statuses in the online community, people will increase their commitment to the online groups 35 and become motivated for future participation. 36
Among the group factors, the average level of group health is beneficial for social contact initiation. This is because a comfortable and balanced environment is the fundamental basis for effective communication. In goal challenge groups, members are susceptible to weight comparisons because they gather with the same health goal. Thus, a low-comparison situation can smooth nerves and facilitate social contact. However, although groups with more underweight members exhibited fewer replies, people situated in these groups enjoyed greater weight loss. These results suggest that group health status has a contradictory influence on social contact and weight loss. A worse level of average group health can motivate the social communication process but hamper individual goal pursuit. A meta-analysis also provided evidence that cooperative settings in health intervention groups make members feel related, but decrease their competence satisfaction. 37 The beneficial influence of upward comparison (i.e. comparing self to people who are better-off) rather than downward comparison was also found in previous literature.15,38 Upward comparison increases the possibilities of participating in physical activity and exercising thoughts.
Furthermore, our individual–group fit results showed that group elevation is more effective when the focal individual has relatively low weight. Specifically, such a health discrepancy is important for the initiation of in-replies and final weight loss. This result indicates that a downward comparison process is beneficial when people pursue weight loss in goal-challenge groups. Meng et al.’s 3 study of food consumption also found that downward comparison mediates individual–group discrepancy and health achievement. Meanwhile, contrary to previous literature, 10 we did not find a significant influence of group diversity. The first possible reason was although diversified members existed within one group, the psychological process of upward comparison was dominant. 15 Second, the diversity effect was mitigated by the effect of the individual–group fit. The diversity effect highlights possible exposure to people different from themselves. 39 This can be revealed by the distance between the individual and the group. The third reason is the variation of group diversity was small in our current setting. Members gathered based on self-selection rather than assignment. Possible bias during the selection process might also have contributed to less group diversity. This bears further investigation.
When looking at the relationship between social contact and weight loss, our results revealed that delivering messages is helpful for weight loss. Out-replies reflect engagement, social capital, and prosocial preference, which all contribute to the health-achieving process.17,18 Furthermore, through communicative behavior, people can develop self-esteem and well-being, 19 which further improve health. Vaananen et al. 40 found that women’s health conditions can benefit from providing support to their partners. The situation of weight loss is similar, considering that members in weight loss goal-challenge groups are mostly women. Similarly, Hether et al. 41 found that providing support among other social media use behavior is the most effective factor in health-related outcomes.
Furthermore, the mediation relationship emphasized the role of social contact in explaining how group elevation influences individual weight conditions. As a distant influencer, social norms encourage an individual to participate. Then, people can gain efficacy and finally achieve successful weight loss through participation. Social influence literature has emphasized the potent effect between group status and individual status.10,12 However, weight change cannot be achieved by merely identifying self as an in-group member or adopting the norms of being healthy. This study shows that social participation as one mediating path can help individuals internalize such social norms and help achieve beneficial outcomes.
Implications
This research is rich in its implications. Theoretically, we explored the dynamic process in health intervention groups. We answered the question of whether individual or group factors affect individual health outcomes more. Our results showed that group influence is more vital because it directs social contact within groups. Our study also extends our understanding of goal-related groups and how they enhance health. Such groups are helpful due to the social identification process. Our results are practically informative for health interventions and in designing goal-attaining groups. By allocating members to appropriate small groups based on their health and social statuses, providing effective group-related information to members, and facilitating in-group contact, intervention designers can enable members to achieve their health goals better.
Limitations and future research
However, we cannot ignore the limitations of our research. First, we only concentrated on user activity in goal-challenge groups. Considering that alliances of such goal-attaining groups were loose, we cannot ignore the influences of users’ activities and the support they gained elsewhere on the same platform (e.g. discussion forums, or contact messages). Further, the findings are applicable only to people with normal weights because the majority of our sample were not overweight. The psychological and behavioral processes for obesity management are different and warrant future investigation.
Second, we only took user-generated content into the analysis. Although this had the advantage of unobstructed observation, we do not know whether users’ self-reporting was honest. Moreover, we can only draw conclusions based on behavior logs and observable social clues. It is possible that participants may interpret the digital discrepancy differently, leading to reversed outcomes. 42 Further, we did not control members’ selection bias for participation, and we cannot trace the status of people who dropped out. Considerable data also were excluded during the data-cleaning process. To cross-validate our findings, it would be necessary to implement experimental and survey methods and to measure members’ psychological processes.
Third, our observation window was restricted to one month. Future studies should investigate how these factors influence health outcomes in the long term and how they contribute to the health maintenance process.
Finally, we acknowledge that the differences in our findings compared to previous literature might be due to the context. Weight loss is one specific health outcome. It is an individualistic goal. Further, it cannot be achieved by merely adopting a new attitude and new behavior, but by continuously devoting physical effort to the issue. To extend our understanding of the group process during health enhancement, we should consider other types of goal settings such as cooperative goals, and other health outcomes such as self-tracking and food intake to discover how goal types affect the findings.
Conclusions
This study investigated the group process in online goal challenge groups. Results reveal that one group compositions and user affiliation are important for social contact and individual weight change, although the direction is contradictory. Further, group compositions contribute to weight loss through the social contact process. This study complements the literature about goal-related groups and health management. It is also indicative for setting goal-attaining groups for health interventions.
Footnotes
Conflict of interest: The authors have no conflicts of interest to declare.
Contributorship: YZ is responsible for research design, data collection, analysis, and manuscript writing. JZ is responsible for project management and ethical approval gaining. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Ethical approval: Approval for the study was granted by City University of Hong Kong. Due to the online community is already closed. No informed consent was gained from the users. We ensured that only publicly available data was used in the analysis and all data were anonymized to avoid identification. Only aggregative group-level information for selected anonymized participants were available for this publication.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the the Research Grants Council of the Hong Kong SAR, China, The National Social Science Fund of China, City University of Hong Kong, The Fundamental Research Funds for the Central Universities, (grant number CityU PDFS2021-1H10, GRF 11505119, 19ZDA324, SRG 7005702, 011014370119).
Guarantor: JZ.
ORCID iD: Yixin Zhou https://orcid.org/0000-0001-8192-9556
References
- 1.Laranjo L. The influence of social networking sites on health behavior change: a systematic review and meta-analysis. J Am Med Inform Assoc 2015; 22: 243–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Webb TL, Joseph J, Yardley L, et al. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res 2010; 12: e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meng J, Peng W, Shin SY, et al. Online self-tracking groups to increase fruit and vegetable intake: a small-scale study on mechanisms of group effect on behavior change. J Med Internet Res 2017; 19: e63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Merchant G, Weibel N, Pina L, et al. Face-to-Face and online networks: college students’ experiences in a weight-loss trial. J Health Commun 2017; 22: 75–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Newman MW, Lauterbach D, Munson SA, et al. It’s not that i don’t have problems, i’m just not putting them on Facebook: challenges and opportunities in using online social networks for health. In: Proceedings of the ACM 2011 Conference on Computer Supported Cooperative Work. New York: Association for Computing Machinery, 2011, pp.341–350. [Google Scholar]
- 6.Berkman L, Glass T, Brissette I, et al. From social integration to health: Durkheim in the new millennium. Soc Sci Med 2000; 51: 843–857. [DOI] [PubMed] [Google Scholar]
- 7.Ashforth BE, Mael F. Social identity theory and the organization. Acad Manage Rev 1989; 14: 20–39. [Google Scholar]
- 8.Foreman P, Whetten DA. Members’ identification with multiple-identity organizations. Organ Sci 2002; 13: 618–635. [Google Scholar]
- 9.Guillaume YRF, Brodbeck FC, Riketta M. Surface- and deep-level dissimilarity effects on social integration and individual effectiveness related outcomes in work groups: a meta-analytic integration. J Occup Organ Psychol 2012; 85: 80–115. [Google Scholar]
- 10.Centola D. An experimental study of homophily in the adoption of health behavior. Science 2011; 334: 1269–1272. [DOI] [PubMed] [Google Scholar]
- 11.Earley PC, Kanfer R. The influence of component participation and role models on goal acceptance, goal satisfaction, and performance. Organ Behav Hum Decis Process 1985; 36: 378–390. [Google Scholar]
- 12.Hogg MA, Terry DJ. Social identity and self-categorization processes in organizational contexts. Acad Manage Rev 2000; 25: 121–140. [Google Scholar]
- 13.Edwards JR, Caplan RD, Van Harrison R. Person-environment fit theory: conceptual foundations, empirical evidence, and directions for future research. In: Cooper CL. (ed) Theories of Organizational Stress. Oxford: Oxford University Press, 1998, pp.28–67. [Google Scholar]
- 14.Chow CM, Tan CC. Weight status, negative body talk, and body dissatisfaction: a dyadic analysis of male friends. J Health Psychol 2016; 21: 1567–1606 [DOI] [PubMed] [Google Scholar]
- 15.Rancourt D, Leahey TM, LaRose JG, et al. Effects of weight-focused social comparisons on diet and activity outcomes in overweight and obese young women. Obesity 2015; 23: 85–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O’Brien KS, Caputi P, Minto R, et al. Upward and downward physical appearance comparisons: development of scales and examination of predictive qualities. Body Image 2009; 6: 201–206. [DOI] [PubMed] [Google Scholar]
- 17.Kim H, Ray CD, Veluscek AM. Complementary support from facilitators and peers for promoting mHealth engagement and weight loss. J Health Commun 2017; 22: 905–912. [DOI] [PubMed] [Google Scholar]
- 18.Pappa GL, Cunha TO, Bicalho PV, et al. Factors associated with weight change in online weight management communities: a case study in the LoseIt Reddit community. J Med Internet Res 2017; 19: e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van Uden-Kraan CF, Drossaert CH, Taal E, et al. Self-Reported differences in empowerment between lurkers and posters in online patient support groups. J Med Internet Res 2008; 10: e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Albrecht TL, Goldsmith DJ, Thompson T. Social support, social networks, and health. In: Handbook of Health Communication. New York: Routledge, 2003, pp.263–284. [Google Scholar]
- 21.Batson CD. Altruism and prosocial behavior. In: Gilbert DT, Fiske ST, Lindzey G. (eds) The Handbook of Social Psychology. New York: McGraw-Hill, 1998, pp.282–316. [Google Scholar]
- 22.Tajfel H, Turner JC. The social identity theory of intergroup behavior. In: Psychology of Intergrop Relations. New York: Psychology Press, 2004, pp.276–293. [Google Scholar]
- 23.Chun JU, Cho K, Sosik JJ. A multilevel study of group-focused and individual-focused transformational leadership, social exchange relationships, and performance in teams. J Organ Behav 2016; 37: 374–396. [Google Scholar]
- 24.Zhang Z, Wang M, Shi J. Leader-follower congruence in proactive personality and work outcomes: the mediating role of leader-member exchange. Acad Manage J 2012; 55: 111–130. [Google Scholar]
- 25.Thurmer JL, Wieber F, Gollwitzer PM. Planning and performance in small groups: collective implementation intentions enhance group goal striving. Front Psychol 2017; 8: 603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jansen KJ, Kristof-Brown A. Toward a multidimensional theory of person-environment fit. J Manage Issues 2006; 18: 193–212. [Google Scholar]
- 27.Friedkin NE. A formal theory of reflected appraisals in the evolution of power. Adm Sci Q 2011; 56: 501–529. [Google Scholar]
- 28.Aral S, Muchnik L, Sundararajan A. Distinguishing influence-based contagion from homophily-driven diffusion in dynamic networks. Proc Natl Acad Sci 2009; 106: 21544–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sheeran P, Webb TL. The intention-behavior gap. Soc Personal Psychol Compass 2016; 10: 503–518. [Google Scholar]
- 30.Shituxingzhevia. Health and Weight Loss App: Bohee Health vs Qingjia Weight Loss Competitor Analysis Report. Product One Hundred, http://www.chanpin100.com/article/107494 (2018, accessed 4 January 2022).
- 31.Zeileis A, Kleiber C, Jackman S. Regression models for count data in R. J Stat Softw 2008; 27: 1–25. [Google Scholar]
- 32.Consultation WHO. Obesity: preventing and managing the global epidemic. World Health Organ Tech Rep Ser 2000; 894: 1–253. [PubMed] [Google Scholar]
- 33.Non-Communicable Diseases Risk Factor Collaboration. Adult nutrition status and disease in China, https://globalnutritionreport.org/resources/nutrition-profiles/asia/eastern-asia/china/ (2022).
- 34.Jaacks LM, Gordon-Larsen P, Mayer-Davis EJ, et al. Age, period and cohort effects on adult body mass Index and overweight from 1991 to 2009 in China: the China health and nutrition survey. Int J Epidemiol 2013; 42: 828–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ren Y, Kraut R, Kiesler S, et al. Encouraging commitment in online communities. In: Building Successful Online Communities: Evidence-Based Social Design. Cambridge: The MIT Press, 2012, pp.77–124. [Google Scholar]
- 36.Restivo M, Rijt A. Experimental study of informal rewards in peer production. PLoS One 2012; 7: e34358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gillison FB, Rouse P, Standage M, et al. A meta-analysis of techniques to promote motivation for health behaviour change from a self-determination theory perspective. Health Psychol Rev 2019; 13: 110–130. [DOI] [PubMed] [Google Scholar]
- 38.Huang G, Sun M, Jiang LC. Core social network size is associated with physical activity participation for fitness app users: the role of social comparison and social support. Comput Hum Behav 2022; 129: 107169. [Google Scholar]
- 39.Pampel FC, Krueger PM, Denney JT. Socioeconomic disparities in health behaviors. Annu Rev Sociol 2010; 36: 349–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vaananen A, Buunk BP, Kivimaki M, et al. When it is better to give than to receive: long-term health effects of perceived reciprocity in support exchange. J Pers Soc Psychol 2005; 89: 176–193. [DOI] [PubMed] [Google Scholar]
- 41.Hether HJ, Murphy ST, Valente TW. It’s better to give than to receive: the role of social support, trust, and participation on health-related social networking sites. J Health Commun 2014; 19: 1424–1439. [DOI] [PubMed] [Google Scholar]
- 42.Dibb B, Yardley L. How does social comparison within a self-help group influence adjustment to chronic illness? A longitudinal study. Soc Sci Med 2006; 63: 1602–1613. [DOI] [PubMed] [Google Scholar]