Abstract
The menisci are crescent-shaped, fibrocartilaginous structures that play a crucial role in the load transition and distribution of the contact forces along the tibiofemoral articulation. Meniscal extrusion (ME) is a radiological finding, especially in magnetic resonance imaging (MRI) scans, for which there has been growing interest in recent years. ME, in the coronary plane, is defined as the maximum distance of the most distal end of the meniscus from the border of the tibial plateau, where the tibial eminences are the most prominent, without taking into account the osteophytes. Although there is still controversy in the literature in respect of the optimal cutoff value, a threshold of 3 mm is considered significant. ME has no specific clinical finding or sign and it is encountered in many knee pathologies. It is associated with either rapidly progressive knee osteoarthritis or early onset of knee osteoarthritis and increased morbidity. In this review, we delineate the clinical significance of ME in various knee pathologies, as well as when, why and how it should be managed. To the best of our knowledge, this is the first study to elaborate on these topics.
Keywords: Meniscal extrusion, Centralization, Knee osteoarthritis, Root tears, Anterior cruciate ligament reconstruction (ACLR), Meniscal allograft transplantation (MAT)
Introduction
The menisci are crescent-shaped, fibrocartilaginous structures located between femoral and tibial condyles, which are important for load transmission and distribution, shock absorption, secondary stability and proprioception of the knee joint [1]. The medial meniscus covers 50–60% of the medial tibial plateau, and the lateral meniscus covers 70–80% of the lateral tibial plateau. Meniscal injury decreases their functional properties, resulting in degeneration of the knee joint [2]. However, it is still controversial whether meniscal pathology leads to osteoarthritis (OA), or vice versa. Meniscal tears are grossly divided into degenerative and traumatic [3]. Degenerative tears occur mainly in the medial meniscus and are most commonly encountered in older patients without any history of significant trauma [4]. On the contrary, traumatic tears usually involve the lateral meniscus after an acute traumatic episode with concomitant ligamentous injury, especially anterior cruciate ligament tear, in younger patients [5]. Most of the meniscus pathologies have recently been correlated with meniscal extrusion [3, 6].
The term meniscal extrusion (ME) is used to describe the radial meniscal body displacement beyond the peripheral tibial plateau margin [7, 8]. A threshold of 3 mm, which was initially introduced, is most commonly used to define a significant ME [8]. Nevertheless, there is still controversy in the literature regarding the optimal threshold, as a few studies have proposed a value lower than 3 mm [9, 10], whereas other researchers suggest that a cutoff value higher than 3 mm is optimal [11–13]. Moreover, instead of a single value, Miller et al. defined significant ME as when more than 25% of the meniscal body width extends beyond the tibial limit [14–17]. Magnetic resonance imaging (MRI) is the method of choice for the detection and evaluation of ME (Fig. 1), although it may underestimate ME, as the assessment is routinely not performed under weight-bearing conditions [18–20]. Therefore, ultrasound (U/S) was recently introduced as a reliable alternative to MRI for the evaluation of ME, which also offers the possibility for dynamically assessing ME in various positions, as well as in a weight-bearing state, in an inexpensive and feasible manner [20–22]. Interest in ME has grown exponentially in recent years, as it is associated with several pathologies, such as knee OA, meniscal posterior root tears (MPRT), post-anterior cruciate ligament reconstruction (ACLR) and post-meniscal allograft transplantation (MAT) [6, 23, 24]. More importantly, it leads to rapid progression of the degenerative process of the knee as well as substantial morbidity and pain [25–28]. However, knowledge regarding the management of ME remains limited. Therefore, with this article we aim to provide an up-to-date review of the literature with an emphasis on the clinical significance and new concepts in the treatment and reduction of ME in the different knee pathologies in which it is encountered.
Fig. 1.

Magnetic resonance imaging (MRI) mid-coronal view of the right knee, where the tibial eminences are most prominent. Medial meniscal extrusion (MME) is measured 5.6 mm
Knee pathologies and ME
Osteoarthritis
ME can occur in knee OA [8, 10], and its presence is significantly correlated with increased articular cartilage loss in the tibiofemoral joint and osteophyte formation [29, 30]. Hart et al. [31] showed that lateral ME was associated with worsening of patellofemoral joint OA features at 2-year follow-up. Several studies also argue that the presence of ME is predictive of knee OA progression [32–34]. Results regarding the correlation of ME with pain in knee OA remain controversial. While many studies have shown a positive association [35–38], other studies investigating the association between ultrasound features, including ME, and pain in a series of osteoarthritic knees found no correlation between pathological ME (> 3 mm) and pain in knee OA. [39–41]. Kijima et al. [42] found that in knees with the same grade of knee OA, extrusion of the medial meniscus was greater in patients who experienced pain in comparison with painless knee OA. They then measured the medial meniscal extrusion (MME) with U/S under weight-bearing and reported a cutoff value of MME for knee pain of 4.3 mm, with sensitivity of 84% and specificity of 85% [43]. In addition, given that the presence of severe ME promotes rapid progression of knee OA [44, 45], the importance of inhibiting this process and delaying the inevitable total knee replacement (TKR) is critical.
Conservative treatment constitutes the first line of therapy in mild or moderate knee OA [46, 47]. Treatment with glucosamine, chondroitin sulfate and licofelone has been found beneficial in patients with knee OA and ME, as it may lead to alleviation of symptoms and reduce cartilage volume loss over time. However, it remains unknown whether it is capable of delaying or modifying OA progression, and further research is warranted [32, 48, 49]. Lateral wedge insoles have been found to reduce MME and could also supplement a conservative treatment of knee OA, as they could potentially delay the degenerative process [50]. However, arthroscopic debridement and osteotomies around the knee are also being employed in some instances in moderate knee OA before a TKR is required [51, 52]. Wang et al. [53], in a retrospective review of 131 patients who had undergone arthroscopic surgery for knee OA and were followed up for 4 years, found that in regard to pain relief, arthroscopic surgery was also beneficial in patients with major MME (> 3 mm). Goto et al. [54] showed that varus alignment factors, and specifically medial proximal tibial angle (MPTA), were significantly related to the extent of MME, especially as the knee OA grade progressed. Therefore, they suggested that this type of OA patient, with MME and varus malalignment with a low MPTA, could benefit primarily from an early intervention with high tibial osteotomy (HTO), thus delaying the progression of knee OA. Astur et al. [55] verified this hypothesis by performing 66 HTO, where they measured ME with MRI preoperatively and postoperatively, and found that at 6 weeks postoperatively, the ME had decreased from a mean of 3.9 ± 0.6 mm to a mean of 0.9 ± 0.5 mm. Furthermore, at 2-year follow-up, patients experienced significantly less pain, with improved clinical outcomes.
Meniscal posterior root tear—meniscotibial ligament lesions
ME is strongly correlated with posterior root tears of the menisci [6]. MPRT are defined as an avulsion fracture or a radial lesion occurring within 1 cm of the bony tibial attachment [56]. This pattern completely disrupts the continuity of the circumferential fibers, leading to the loss of the hoop tension and substantial ME, thus promoting rapid progression of knee OA [1, 57]. Management of the MPRT consists of nonoperative treatment, partial meniscectomy and root repair, and primarily aims to prevent the development of OA [58]. Nonoperative treatment is associated with poor clinical outcomes, especially in the presence of a large ME [59], and exacerbation of OA with a higher incidence of subsequent arthroplasty over 5 years of follow-up [60]. Therefore, nonoperative treatment should be reserved for nonsurgical candidates [61].
Historically, MPRT were treated with partial meniscectomy. However, several studies showed that partial meniscectomy, particularly when the ME was profound [62, 63], failed to prevent the progression of OA, as it creates a meniscus-deficient state, and leads to significant functional impairment with high rates of arthroplasty [24, 60]. Consequently, partial meniscectomy is only utilized for symptomatic MPRT (catching/locking) when a root repair, due to excessive degenerative changes and poor quality of meniscal tissue, is contraindicated [61, 64].
Currently, MPRT repair constitutes the treatment of choice, since it restores the hoop tension and the joint kinematics [65], halts the progression of OA and lowers the rate of arthroplasty [66, 67]. Root repair is indicated when varus malalignment is minimal (< 5°), the cartilage wear is not advanced (Outerbridge grade 1–2) and it can be performed arthroscopically either with a transtibial pullout technique or with suture anchors, each with its respective advantages and disadvantages [58]. Although meta-analyses validate the superiority of root repair over partial meniscectomy in terms of clinical outcomes, they also highlight the inability of root repair to successfully reduce ME [68, 69]. One way to reduce postoperative ME is by early intervention, specifically within 3 months after the MPRT [70–72]. However, it has also been hypothesized that MPRT is not the sole contributing factor predisposing to ME. Also taking into consideration that residual ME after MPRT repair correlates with worse outcomes regarding both clinical parameters and OA progression [72, 73], a better understanding of the causality of ME is needed in order to appropriately address it.
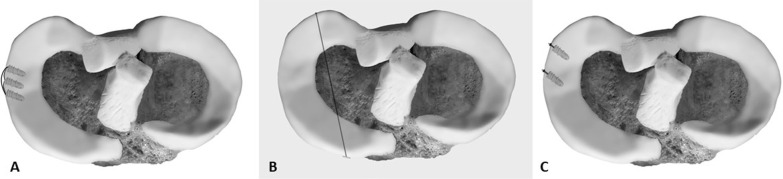
Current research has directed its focus to meniscotibial ligaments (MTL), which stabilize on the tibial plateau and centralize the meniscus, as an additional potential causative factor for ME. Krych et al. [74] retrospectively analyzed MRI series with isolated ME without concomitant serious knee pathologies, and found that isolated significant ME (> 3 mm) was associated with MTL abnormalities. In another study where they examined MRI series both before and after medial MPRT, they showed that MTL disruption and ME predated the MPRT, thus emphasizing the potential role that MTL could play as a causal factor of ME, and even suggesting that disruption of MTL should be addressed alongside MPRT repair in order to reduce ME [75]. Debieux et al. [13] proved biomechanically that ME is possible with intact meniscal roots and that centralization of the meniscus restores the tibiofemoral contact pressures back to normal. In a biomechanical study, Paletta et at. [76] showed that induction of MTL lesions in cadaveric knees resulted in ME after only a few cycles of loading and that repair of the lesion led to a significant reduction of ME. Furthermore, they performed an open MTL repair in 15 patients with meniscal tear and medial ME through a mini-incision with three interconnecting suture anchors (Fig. 2a), and found that postoperative ME was significantly reduced. Koga et al. [77] performed arthroscopic centralization of nine extruded lateral menisci with the use of suture anchors, and ME was significantly reduced in 2 years of follow-up.
Fig. 2.
a Meniscotibial ligament repair with three interconnected suture anchors, b centralization with a transtibial tunnel or c with isolated suture anchors (usually with two or three suture anchors)
Several other techniques of meniscal centralization with suture anchors as well as with transtibial tunnel, with or without prior meniscal release from its capsular attachments, have also been described in technical notes (Fig. 2b, c) [78–82]. However, to date there is still no well-designed clinical trial available to ascertain the effectiveness of centralization in reducing ME.
Anterior cruciate ligament reconstruction
The ACL is the main restrictor in the anterior tibial translation, while the posterior part of the medial meniscus (MM) acts as a secondary stabilizer [83, 84]. The lateral meniscus (LM) is a secondary stabilizer in the knee joint during pivot-shift loading [85]. The goal of the anatomic reconstruction of the ACL rupture is to replicate the normal knee anatomy. However, the incidence of severe knee OA is much higher in patients who have been subjected to ACLR than individuals with intact ACL [86, 87]. It has been shown from studies that the risk for TKA after ACLR is seven times greater than in normal individuals [88].
The incidence of meniscal tears associated with ACL injury is as high as 79%, with the LM being affected more often than the MM in acute situations [89]. It is known that ACL and meniscal function cannot be fully restored even after surgical repair [86, 90]. To the best of our knowledge, the exact clinical significance of ME after ACLR has not yet been clearly elucidated, although efforts are continuously being made to minimize this phenomenon. ME depends largely on the severity and type of tear [87, 89, 91]. After ACLR, extrusion of the ΜΜ is more frequently seen than that of the LM. Moreover, extrusion of the LM does not improve after ACLR unless the meniscal tear is repaired [87, 92]. In addition, when there is ACL rupture and the preoperative extrusion of the LM is 1.1 mm, the surgeon should consider the possibility of a complete posterior root tear (PRT) of the LM. This value is identified as the optimal cutoff point for a complete PRT of the LM and has 100% sensitivity and 83% specificity [92]. In a recent study by Tsujii et al., it was shown that after concurrent ACLR and meniscal repair, the lateral extrusion of the LM was correlated with its healing status. If the repaired meniscus failed to heal, lateral extrusion progressed significantly [92]. However, its posterior extrusion progressed significantly regardless of the healing status [90]. The mechanical damage of the meniscus caused by extrusion seems to change the loading-bearing capacity of the tibiofemoral compartments, leading to the destruction of the articular cartilage as well the subchondral bone, ultimately contributing to the development or progression of OA [87, 89, 92].
An inappropriate tibial tunnel may also cause extrusion of the LM. A more posterolateral placement of the tibial tunnel aperture may induce extrusion of the LM following ACLR. The primary site of destruction is the soft tissue fibers which couple the deep layers of the ACL to the LM and the LM to the tibial plateau. These fibers specifically act on the LM anterior root attachment itself, explaining the reduction in the ultimate failure of the anterior root strength of the LM with disruption of these fibers [87, 93]. A novel technique has been developed based on a measurement grid in order to determine the precise aperture of the tibial tunnel. According to this technique, a more posterolateral position of the tibial tunnel aperture within the ACL footprint reduces the RTD (reference point to tibial tunnel distance) and increases the extrusion of the LM following ACLR [93].
Comparative studies between normal knees and knees with ACL rupture demonstrated that the posterior extrusion of the MM during knee flexion is almost the same [83, 94]. It was also shown that after ACLR, without concomitant tears of the menisci, the anteroposterior and radial extrusion of the MM tended to increase compared with preoperative levels, but all measurements remained below the threshold value of 3 mm [24, 44, 95]. These findings suggest that the tension of the graft and the excessive external rotation of the tibia are also factors that can affect the condition of the MM. Therefore, ACL rupture alone cannot cause the posterior extrusion of the MM, and the ACLR alone does not directly cause distinct damage to the MM. As a result, post-traumatic transposition and degeneration of the MM may not be completely prevented by ACLR alone. However, further investigation is needed to evaluate the effect of the ACLR on the restoration of the MM function [88].
Degenerative lesions of the knee joint are more commonly present during concurrent ACLR with meniscectomy than with intact or repaired menisci. The concurrent ACLR with repair of the menisci has shown good clinical and functional results and less risk of reoperation during the follow-up periods [83, 87]. However, over a long-term period, the degenerative changes in the articular cartilage worsened, especially in the lateral tibial plateau, regardless of the healing status of the meniscus [85, 87, 90]. Furthermore, Lee et al. (ACLR + LM tears left in situ) showed narrowing of 0.33 mm of the lateral joint space at 3 years postoperatively, and Shelbourne et al. (ACLR + LM tears left in situ) showed narrowing of 1.0 mm at 10-year follow-up [96, 97]. Tsujii et al. (ACLR + LM tear repair) demonstrated that the narrowing was only 0.04 mm at 3.4 years postoperatively, whereas another study showed widening of 0.1 mm at 3.5 years postoperatively [85, 90].
Although there is a need for longer follow-up periods, the currently available data suggest a benefit of concomitant ACLR with the repair of longitudinal, radial, posterior horn and posterior root tears of the menisci, because the combination can even better reduce their shape and extrusion [92, 98–100]. Winkler et al. showed that the difference in the extrusion of the LM between a healthy knee and a knee with combined injury was not statistically significant. Based on these findings, they concluded that the all-inside repair of the radial tear of the LM could help maintain its dynamic behavior, thus reducing the biomechanical stress exerted on the adjacent cartilage [89]. Another promising surgical approach for reducing the ME is the arthroscopic centralization of the extruded meniscus at the point where the capsule adjacent to the meniscus is repaired at the border of the tibial plateau [98, 101]. There is no established optimal surgical technique at present for restoring ME to normal values, and thus there will be a strong need for more effective and refined techniques.
Meniscal allograft transplantation
To address the problems of patients with meniscectomy, efforts are constantly being made to develop techniques that aim at meniscal regeneration or development of meniscal scaffolds. MAT is a potential surgical procedure for young, active patients with symptomatic meniscal insufficiency that does not respond to conservative treatment [102, 103]. The early results of MAT are encouraging, as pain relief and improved knee function are reported [15–17, 62, 104–109]. In fact, MAT supporters claim that it restores the biomechanical properties of the endogenous meniscus, prevents or slows cartilage damage, especially if the MAT is performed immediately, and improves long-term outcomes [17, 110, 111].
Most authors agree that the transplanted menisci are extruded more frequently than endogenous menisci [15, 102, 105]. It should be highlighted that the clinical significance of meniscal allograft extrusion has not yet been clearly elucidated, since it is difficult to draw firm conclusions. For instance, an oversized allograft achieves adequate coverage of the tibial plateau while exhibiting a large amount of extrusion, whereas the opposite applies for undersized or shrunken allografts [112]. Meniscal allograft extrusion causes incongruity with the femoral condyle, and therefore the allograft cannot perform normal load transmission and shock absorption. This condition may lead to increased cartilage degeneration, progressive OA and allograft failure, as mentioned in several biomechanical studies [17, 111]. Moreover, it has been shown that allograft extrusion does not correlate with clinical outcomes and tends to be stable postoperatively during follow-up [62, 108, 113]. In addition, it has been shown that after lateral MAT, the extrusion is correlated with the progression of joint space narrowing (JSN) during long-term follow-up, while after medial MAT, JSN is observed during medium-term follow-up [114]. Finally, meniscal allograft extrusion is also associated with subchondral bone marrow lesions and cysts [2, 115].
MAT is not a simple surgical procedure, has a high learning curve, and if it is not performed under certain indications (Table 1) it fails, leaving both the surgeon and the patient dissatisfied [106, 109]. For these reasons, certain contraindications have been introduced (Table 2) [102, 103, 105–109]. Despite the advances in surgical techniques and the improved methods for the estimation of the implant size, MAT is successful in only up to 75% of patients [2, 16, 109]. There is no consensus whether medial or lateral MAT is superior in terms of medium-term (5–10 years) and long-term (> 10 years) survival. In a recent meta-analysis, the percentages of medium-term and long-term survival after medial MAT were 85.8% and 52.6%, respectively, whereas after lateral MAT they were 89.2% and 56.6%, respectively [116]. The survival of the graft depends substantially on the condition of the articular cartilage [117–119].
Table 1.
| 1. Previous subtotal or total meniscectomy with persistent pain and swelling that does not respond to conservative treatment |
| 2. Age ≤ 60 years (Lee-2020) < 55 years (Kim-2017, Kim-2018) < 50 years (Jang-2011) < 45 years (Ha-2010, Ha-2014) |
| 3. Normal axis of the lower limb as shown in the scanogram |
| 4. Absence of knee instability |
| 5. Damage of the articular cartilage up to grade 2 according to the Outerbridge classification |
| 6. Knee OA grade ≤ 2 according to the Kellgren–Lawrence or Ahlbäck classification* |
OA osteoarthritis
*Localized articular cartilage degeneration of stage 3 or 4, which is limited to the area covered by the meniscus, is not considered a contraindication for meniscal transplantation (Kim-2017, Kim-2018, Lee-2020)
Table 2.
| 1. Age > 60 years |
| 2. Poor axial alignment of the lower limb (varus/valgus > 3ο or 5ο) |
| 3. Immature skeleton |
| 4. Knee OA of grade ≥ 3 according to the Kellgren–Lawrence or Ahlbäck classification |
| 5. Diffuse degeneration of the articular cartilage |
| 6. Knee instability |
| 7. BMI > 35 |
| 8. Inflammatory joint disease |
| 9. Disease of the synovial membrane |
| 10. Recent septic arthritis or untreated septic arthritis |
| 11. Metabolic disorders or the presence of crystals |
| 12. Previous osteotomy for mechanical axis correction |
| 13. ACL insufficiency |
OA osteoarthritis, BMI body mass index, ACL anterior cruciate ligament
Several preoperative and intraoperative factors (Table 3) are associated with the absolute value of allograft extrusion [16, 102, 106, 109, 120]. This suggests that if patients with minimal degeneration and accurate indications undergo MAT with a well-placed graft, the graft extrusion will be minimal and the results will remain unchanged. However, evaluation by absolute value alone may be limited due to differences in implant size, bone and cartilage condition, and individual patient characteristics. Therefore, the relative values may be significant [17].
Table 3.
| 1. Size mismatch between the affected joint surface and the allograft |
| 2. Excessive peripheral suture tension |
| 3. Nonanatomical placement of the allograft |
| 4. Pre-existing osteophytes on the tibial plateau |
| 5. Loss of fixation of the anterior and posterior horns |
| 6. Non-repair of meniscotibial ligaments and popliteomeniscal fascicles |
| 7. Bony inclination of the allograft |
| 8. Position of the bone bridge |
| 9. Fixation of the allograft |
| 10. Recipient–donor mismatch |
Many techniques have been described for meniscal transplantation, but the most commonly used are (a) the suture-only technique, (b) bone-plug technique, (c) keyhole technique and (d) bridge-in-slot technique [102, 104, 111]. The results as to which technique is superior to the others remain controversial. Most transplantations have been performed with the bone-plug technique because previous studies have shown its superiority in load-bearing function, resistance to hoop stresses, similar contact mechanics to endogenous menisci and lower extrusion rates compared with the other techniques [109, 111]. On the other hand, the suture-only technique has its own advantages and is therefore chosen by many surgeons [104, 111].
Although meniscal allografts that are secured with the suture-only technique tend to show a greater degree of extrusion than the bony-fixation techniques, bony-fixation techniques still show high extrusion rates (25–50%). Therefore, improvements in surgical techniques are necessary [102, 109].
Several strategies have been proposed to reduce allograft extrusion. Although the ultimate cause is unknown, it is quite common to see a subluxated joint capsule in the symptomatic meniscectomized compartment. This is probably why capsulodesis is so effective in minimizing extrusion. Another successful strategy is osteophyte resection. Osteophyte removal > 2 mm at the edge of the lateral tibial plateau can reduce extrusion after lateral MAT [109, 121, 122]. Correct estimation of the allograft size is also important. It has been suggested that a 5–10% reduction of implant size from the estimated one reduces postoperative extrusion [2, 105, 123]. And finally, the proper anatomical placement of the allograft is essential. Nonanatomical placement of the meniscal allograft > 5 mm relative to the endogenous meniscus adversely affects the mechanical contacts of the knee, which may affect the allograft's ability to prevent articular cartilage degeneration [16, 124]. Improper positioning of the posterior horn causes a similar deviation to the anterior horn. Therefore, proper placement of the posterior horn is critical to the anatomical repair of the meniscus [125–127].
Conclusion
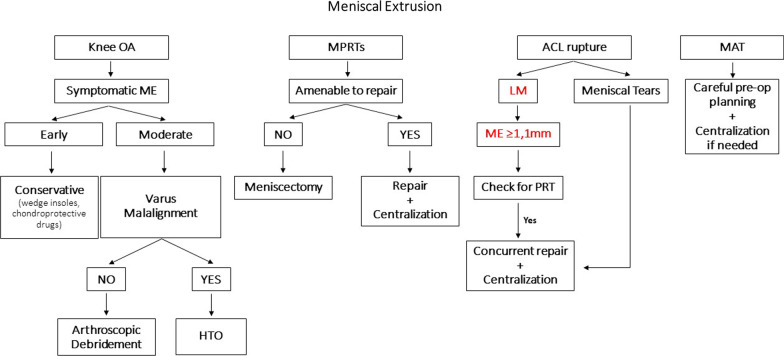
ME is found in several knee pathologies and is well correlated with rapid knee OA progression as well as increased morbidity. Therefore, care should be taken to manage it appropriately and successfully reduce it. Although in mild/moderate knee OA there is still no specific treatment targeting ME, the established conservative and operative treatment modalities seem equally successful in delaying the progression of OA and improving symptoms when ME is also present. Future research should focus on the role of additional centralization of the meniscus during arthroscopic debridement for the treatment of moderate knee OA. Although it has never been reported, it is worth researching, as it could have a beneficial effect. MPRT should be repaired earlier than 3 months after diagnosis. Furthermore, supplementary centralization of the meniscus appears to be able to adequately reduce the ME, as it also addresses potential MTL lesions. However, more research with high-quality studies is needed in order to refine the technique and validate its long-term results in reducing ME. Post-ACLR ME is also a concern and should be prevented by repairing concurrent meniscal tears and centralizing the meniscus along with the ACLR. Finally, meniscal allografts often result in extrusion, thus potentially reducing the clinical benefits of transplantation. Careful preoperative planning for correct sizing and accurate placement of the allograft is critical for preventing ME. Moreover, centralization of the allograft can be performed to help stabilize it on the tibial plateau; however, there are not yet sufficient data in the literature to support its benefits. Finally, we provide a proposed treatment algorithm based on the information retrieved from the literature that could help guide clinicians in the management of ME on the aforementioned knee pathologies (Fig. 3).
Fig. 3.
Proposed treatment algorithm for meniscal extrusion (ME) in different knee pathologies (OA osteoarthritis, ME meniscal extrusion, HTO high tibial osteotomy, MPRTs meniscal posterior root tears, ACL anterior cruciate ligament reconstruction, LM lateral meniscus, PRT posterior root tear, MAT meniscal allograft transplantation)
Acknowledgements
Not applicable.
Author contributions
VA conceived the idea for the study and supervised the whole study process. TK and DG designed the manuscript and helped to draft the manuscript and review it. MK, VSI and GP participated in the study design and helped to draft the manuscript. All authors read and approved the final manuscript.
Funding
The authors did not receive funding for this study.
Declarations
Ethics approval and consent to participate
This study was exempted from the requirement for local institutional review board approval as it is a narrative review of the literature.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Krych AJ, Bernard CD, Kennedy NI, Tagliero AJ, Camp CL, Levy BA, et al. Medial versus lateral meniscus root tears: is there a difference in injury presentation, treatment decisions, and surgical repair outcomes? Arthroscopy. 2020;36(4):1135–1141. doi: 10.1016/j.arthro.2019.11.098. [DOI] [PubMed] [Google Scholar]
- 2.Łuczkiewicz P, Daszkiewicz K, Chróścielewski J, Witkowski W, Kuik L. High meniscal slope angle as a risk factor for meniscal allograft extrusion. Med Hypotheses. 2017;1(101):48–51. doi: 10.1016/j.mehy.2017.02.003. [DOI] [PubMed] [Google Scholar]
- 3.Ozeki N, Seil R, Krych AJ, Koga H. Surgical treatment of complex meniscus tear and disease: state of the art. J ISAKOS. 2021;6(1):35–45. doi: 10.1136/jisakos-2019-000380. [DOI] [PubMed] [Google Scholar]
- 4.Beaufils P, Becker R, Kopf S, Englund M, Verdonk R, Ollivier M, et al. Surgical management of degenerative meniscus lesions: the 2016 ESSKA meniscus consensus. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2017;25(2):335–346. doi: 10.1007/s00167-016-4407-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kopf S, Beaufils P, Hirschmann MT, Rotigliano N, Ollivier M, Pereira H, et al. Management of traumatic meniscus tears: the 2019 ESSKA meniscus consensus. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2020;28(4):1177–1194. doi: 10.1007/s00167-020-05847-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Swamy N, Wadhwa V, Bajaj G, Chhabra A, Pandey T. Medial meniscal extrusion: detection, evaluation and clinical implications. Eur J Radiol. 2018;1(102):115–124. doi: 10.1016/j.ejrad.2018.03.007. [DOI] [PubMed] [Google Scholar]
- 7.Karpinski K, Diermeier T, Willinger L, Imhoff AB, Achtnich A, Petersen W. No dynamic extrusion of the medial meniscus in ultrasound examination in patients with confirmed root tear lesion. Knee Surg Sports Traumatol Arthrosc. 2019;27(10):3311–3317. doi: 10.1007/s00167-018-5341-4. [DOI] [PubMed] [Google Scholar]
- 8.Costa CR, Morrison WB, Carrino JA. Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear? AJR Am J Roentgenol. 2004;183(1):17–23. doi: 10.2214/ajr.183.1.1830017. [DOI] [PubMed] [Google Scholar]
- 9.Muzaffar N, Kirmani O, Ahsan M, Ahmad S. Meniscal extrusion in the knee: should only 3 mm extrusion be considered significant? an assessment by MRI and arthroscopy. Malays Orthop J. 2015;9(2):17–20. doi: 10.5704/MOJ.1507.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Okada K, Yamaguchi S, Sato Y, Enomoto T, Ogawa Y, Ohtori S, et al. Comparison of meniscal extrusion and osteophyte formation at the intercondylar notch as a predictive biomarker for incidence of knee osteoarthritis-Data from the Osteoarthritis Initiative- J Orthop Sci. 2019;24(1):121–127. doi: 10.1016/j.jos.2018.08.003. [DOI] [PubMed] [Google Scholar]
- 11.Chiba D, Sasaki E, Ota S, Maeda S, Sugiyama D, Nakaji S, et al. US detection of medial meniscus extrusion can predict the risk of developing radiographic knee osteoarthritis: a 5-year cohort study. Eur Radiol. 2020;30(7):3996–4004. doi: 10.1007/s00330-020-06749-1. [DOI] [PubMed] [Google Scholar]
- 12.Svensson F, Felson DT, Turkiewicz A, Guermazi A, Roemer FW, Neuman P, et al. Scrutinizing the cut-off for “pathological” meniscal body extrusion on knee MRI. Eur Radiol. 2019;29(5):2616–2623. doi: 10.1007/s00330-018-5914-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Debieux P, Jimenez AE, Novaretti JV, Kaleka CC, Kriscenski DE, Astur DC, et al. Medial meniscal extrusion greater than 4 mm reduces medial tibiofemoral compartment contact area: a biomechanical analysis of tibiofemoral contact area and pressures with varying amounts of meniscal extrusion. Knee Surg Sports Traumatol Arthrosc. 2020 doi: 10.1007/s00167-020-06363-0. [DOI] [PubMed] [Google Scholar]
- 14.Miller TT, Staron RB, Feldman F, Çepel E. Meniscal position on routine MR imaging of the knee. Skeletal Radiol. 1997;26(7):424–427. doi: 10.1007/s002560050259. [DOI] [PubMed] [Google Scholar]
- 15.Abat F, Gelber PE, Erquicia JI, Pelfort X, Gonzalez-Lucena G, Monllau JC. Suture-only fixation technique leads to a higher degree of extrusion than bony fixation in meniscal allograft transplantation. Am J Sports Med. 2012;40(7):1591–1596. doi: 10.1177/0363546512446674. [DOI] [PubMed] [Google Scholar]
- 16.Lee BS, Kim JM, Kim JM, Kim KA, Bin SI. Patient-related risk factors for the extrusion of lateral meniscal allograft transplants. Arthroscopy. 2015;31(4):699–706. doi: 10.1016/j.arthro.2014.10.016. [DOI] [PubMed] [Google Scholar]
- 17.Lee SM, Bin SI, Kim JM, Lee BS, Park JG. Absolute meniscal extrusion after lateral meniscal allograft transplantation does not progress during long-term follow-up: average of 10.3 years’ follow-up longitudinal magnetic resonance imaging study. Am J Sports Med. 2020;48(2):326–333. doi: 10.1177/0363546519889046. [DOI] [PubMed] [Google Scholar]
- 18.Patel R, Eltgroth M, Souza RB, Zhang CA, Majumdar S, Link TM, et al. Loaded versus unloaded magnetic resonance imaging (MRI) of the knee: Effect on meniscus extrusion in healthy volunteers and patients with osteoarthritis. Eur J Radiol Open. 2016;20(3):100–107. doi: 10.1016/j.ejro.2016.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rowland G, Mar D, McIff T, Nelson J. Evaluation of meniscal extrusion with posterior root disruption and repair using ultrasound. Knee. 2016;23(4):627–630. doi: 10.1016/j.knee.2016.04.008. [DOI] [PubMed] [Google Scholar]
- 20.Ishii Y, Ishikawa M, Kurumadani H, Hayashi S, Nakamae A, Nakasa T, et al. Increase in medial meniscal extrusion in the weight-bearing position observed on ultrasonography correlates with lateral thrust in early-stage knee osteoarthritis. J Orthop Sci. 2020;25(4):640–646. doi: 10.1016/j.jos.2019.07.003. [DOI] [PubMed] [Google Scholar]
- 21.Winkler. Sonographic evaluation of lateral meniscal extrusion: implementation and validation|SpringerLink [Internet]. 2021. https://link.springer.com/article/10.1007%2Fs00402-020-03683-1. Accessed 22 May 2021. [DOI] [PMC free article] [PubMed]
- 22.Nogueira-Barbosa MH, Gregio-Junior E, Lorenzato MM, Guermazi A, Roemer FW, Chagas-Neto FA, et al. Ultrasound assessment of medial meniscal extrusion: a validation study using MRI as reference standard. Am J Roentgenol. 2015;204(3):584–588. doi: 10.2214/AJR.14.12522. [DOI] [PubMed] [Google Scholar]
- 23.Foreman SC, Liu Y, Nevitt MC, Neumann J, Joseph GB, Lane NE, et al. Meniscal root tears and extrusion are significantly associated with the development of accelerated knee osteoarthritis: data from the osteoarthritis initiative. CARTILAGE. 2020;21:1947603520934525. doi: 10.1177/1947603520934525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee DH, Lee BS, Kim JM, Yang KS, Cha EJ, Park JH, et al. Predictors of degenerative medial meniscus extrusion: radial component and knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2011;19(2):222–229. doi: 10.1007/s00167-010-1274-2. [DOI] [PubMed] [Google Scholar]
- 25.Oo WM, Linklater JM, Bennell KL, Pryke D, Yu S, Fu K, et al. Are OMERACT knee osteoarthritis ultrasound scores associated with pain severity, other symptoms, and radiographic and magnetic resonance imaging findings? J Rheumatol. 2021;48(2):270–278. doi: 10.3899/jrheum.191291. [DOI] [PubMed] [Google Scholar]
- 26.Chiba D, Maeda S, Sasaki E, Ota S, Nakaji S, Tsuda E, et al. Meniscal extrusion seen on ultrasonography affects the development of radiographic knee osteoarthritis: a 3-year prospective cohort study. Clin Rheumatol. 2017;36(11):2557–2564. doi: 10.1007/s10067-017-3803-6. [DOI] [PubMed] [Google Scholar]
- 27.Kim JY, Bin SI, Kim JM, Lee BS, Oh SM, Park MH. Tear gap and severity of osteoarthritis are associated with meniscal extrusion in degenerative medial meniscus posterior root tears. Orthop Traumatol Surg Res. 2019;105(7):1395–1399. doi: 10.1016/j.otsr.2019.09.015. [DOI] [PubMed] [Google Scholar]
- 28.Everhart JS, Magnussen RA, Abouljoud MM, Regalado LE, Kaeding CC, Flanigan DC. Meniscus tears accelerate joint space loss and lateral meniscal extrusion increases risk of knee arthroplasty in middle-aged adults. J Orthop Res. 2020;38(11):2495–2504. doi: 10.1002/jor.24672. [DOI] [PubMed] [Google Scholar]
- 29.Roemer FW, Kwoh CK, Hannon MJ, Green SM, Jakicic JM, Boudreau R, et al. Risk factors for magnetic resonance imaging–detected patellofemoral and tibiofemoral cartilage loss during a six-month period: the Joints On Glucosamine study. Arthritis Rheum. 2012;64(6):1888–1898. doi: 10.1002/art.34353. [DOI] [PubMed] [Google Scholar]
- 30.Kim DH, Lee GC, Kim HH, Cha DH. Correlation between meniscal extrusion and symptom duration, alignment, and arthritic changes in medial meniscus posterior root tear: research article. Knee Surg Relat Res. 2020 doi: 10.1186/s43019-019-0019-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hart HF, Crossley KM, Felson D, Jarraya M, Guermazi A, Roemer F, et al. Relation of meniscus pathology to prevalence and worsening of patellofemoral joint osteoarthritis: the multicenter osteoarthritis study. Osteoarthritis Cartilage. 2018;26(7):912–919. doi: 10.1016/j.joca.2017.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roubille C, Martel-Pelletier J, Abram F, Dorais M, Delorme P, Raynauld JP, et al. Impact of disease treatments on the progression of knee osteoarthritis structural changes related to meniscal extrusion: data from the OAI progression cohort. Semin Arthritis Rheum. 2015;45(3):257–267. doi: 10.1016/j.semarthrit.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 33.Liu Y, Joseph GB, Foreman SC, Li X, Lane NE, Nevitt MC, et al. Determining a threshold of medial meniscal extrusion for prediction of knee pain and cartilage damage progression over 4 years: data from the osteoarthritis initiative. Am J Roentgenol. 2020;216(5):1318–1328. doi: 10.2214/AJR.20.23864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Teichtahl AJ, Cicuttini FM, Abram F, Wang Y, Pelletier JP, Dodin P, et al. Meniscal extrusion and bone marrow lesions are associated with incident and progressive knee osteoarthritis. Osteoarthritis Cartilage. 2017;25(7):1076–1083. doi: 10.1016/j.joca.2017.02.792. [DOI] [PubMed] [Google Scholar]
- 35.Naredo E, Cabero F, Palop MJ, Collado P, Cruz A, Crespo M. Ultrasonographic findings in knee osteoarthritis: a comparative study with clinical and radiographic assessment. Osteoarthritis Cartilage. 2005;13(7):568–574. doi: 10.1016/j.joca.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 36.Chan KKW, Sit RWS, Wu RWK, Ngai AHY. Clinical, radiological and ultrasonographic findings related to knee pain in osteoarthritis. PLoS ONE. 2014;9(3):e92901. doi: 10.1371/journal.pone.0092901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Malas FÜ, Kara M, Kaymak B, Akıncı A, Özçakar L. Ultrasonographic evaluation in symptomatic knee osteoarthritis: clinical and radiological correlation. Int J Rheum Dis. 2014;17(5):536–540. doi: 10.1111/1756-185X.12190. [DOI] [PubMed] [Google Scholar]
- 38.Magnusson K, Turkiewicz A, Kumm J, Zhang F, Englund M. The relationship between MRI features and knee pain over 6 years in knees without radiographic osteoarthritis at baseline. Arthritis Care Res. 2020 doi: 10.1002/acr.24394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wu PT, Shao CJ, Wu KC, Wu TT, Chern TC, Kuo LC, et al. Pain in patients with equal radiographic grades of osteoarthritis in both knees: the value of gray scale ultrasound. Osteoarthritis Cartilage. 2012;20(12):1507–1513. doi: 10.1016/j.joca.2012.08.021. [DOI] [PubMed] [Google Scholar]
- 40.Bevers K, Bijlsma JW, Vriezekolk JE, van den Ende CH, den Broeder AA. Ultrasonographic features in symptomatic osteoarthritis of the knee and relation with pain. Rheumatol Oxf Engl. 2014;53(9):1625–1629. doi: 10.1093/rheumatology/keu030. [DOI] [PubMed] [Google Scholar]
- 41.Podlipská J, Koski JM, Kaukinen P, Haapea M, Tervonen O, Arokoski JP, et al. Structure-symptom relationship with wide-area ultrasound scanning of knee osteoarthritis. Sci Rep. 2017;15(7):44470. doi: 10.1038/srep44470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kijima H, Yamada S, Nozaka K, Saito H, Shimada Y. Relationship between pain and medial meniscal extrusion in knee osteoarthritis. Adv Orthop. 2015 doi: 10.1155/2015/210972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kijima H, Miyakoshi N, Kasukawa Y, Ishikawa Y, Kinoshita H, Ohuchi K, et al. Cut-off value of medial meniscal extrusion for knee pain. Adv Orthop. 2017 doi: 10.1155/2017/6793026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Berthiaume MJ, Raynauld JP, Martel-Pelletier J, Labonté F, Beaudoin G, Bloch DA, et al. Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis. 2005;64(4):556–563. doi: 10.1136/ard.2004.023796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Driban JB, Ward RJ, Eaton CB, Lo GH, Price LL, Lu B, et al. Meniscal extrusion or subchondral damage characterize incident accelerated osteoarthritis: data from the osteoarthritis initiative. Clin Anat N Y N. 2015;28(6):792–799. doi: 10.1002/ca.22590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bannuru RR, Osani MC, Vaysbrot EE, Arden NK, Bennell K, Bierma-Zeinstra SMA, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. 2019;27(11):1578–1589. doi: 10.1016/j.joca.2019.06.011. [DOI] [PubMed] [Google Scholar]
- 47.Primorac D, Molnar V, Matišić V, Hudetz D, Jeleč Ž, Rod E, et al. Comprehensive review of knee osteoarthritis pharmacological treatment and the latest professional societies’ guidelines. Pharmaceuticals. 2021;14(3):205. doi: 10.3390/ph14030205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Raynauld JP, Pelletier JP, Abram F, Dodin P, Delorme P, Martel-Pelletier J. Long-term effects of glucosamine and chondroitin sulfate on the progression of structural changes in knee osteoarthritis: six-year followup data from the osteoarthritis initiative. Arthritis Care Res. 2016;68(10):1560–1566. doi: 10.1002/acr.22866. [DOI] [PubMed] [Google Scholar]
- 49.Raynauld JP, Martel-Pelletier J, Bias P, Laufer S, Haraoui B, Choquette D, et al. Protective effects of licofelone, a 5-lipoxygenase and cyclo-oxygenase inhibitor, versus naproxen on cartilage loss in knee osteoarthritis: a first multicentre clinical trial using quantitative MRI. Ann Rheum Dis. 2009;68(6):938–947. doi: 10.1136/ard.2008.088732. [DOI] [PubMed] [Google Scholar]
- 50.Ishii Y, Deie M, Fujita N, Kurumadani H, Ishikawa M, Nakamae A, et al. Effects of lateral wedge insole application on medial compartment knee osteoarthritis severity evaluated by ultrasound. Knee. 2017;24(6):1408–1413. doi: 10.1016/j.knee.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 51.Phua JKS, Razak HRBA, Mitra AK. Arthroscopic procedures could delay the need for a subsequent knee arthroplasty in older patients with end-stage osteoarthritis. J Orthop Surg Hong Kong. 2020;28(1):2309499020906745. doi: 10.1177/2309499020906745. [DOI] [PubMed] [Google Scholar]
- 52.McCormack DJ, Puttock D, Godsiff SP. Medial compartment osteoarthritis of the knee: a review of surgical options. EFORT Open Rev. 2021;6(2):113–117. doi: 10.1302/2058-5241.6.200102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wang YX, Li ZL, Li J, Zhao ZD, Wang HR, Hou C, et al. Effect of medial meniscus extrusion on arthroscopic surgery outcome in the osteoarthritic knee associated with medial meniscus tear: a minimum 4-year follow-up. Chin Med J (Engl) 2019;132(21):2550–2558. doi: 10.1097/CM9.0000000000000492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Goto N, Okazaki K, Akiyama T, Akasaki Y, Mizu-uchi H, Hamai S, et al. Alignment factors affecting the medial meniscus extrusion increases the risk of osteoarthritis development. Knee Surg Sports Traumatol Arthrosc. 2019;27(8):2617–2623. doi: 10.1007/s00167-018-5286-7. [DOI] [PubMed] [Google Scholar]
- 55.Astur DC, Novaretti JV, Gomes ML, Rodrigues AG, Kaleka CC, Cavalcante ELB, et al. Medial opening wedge high tibial osteotomy decreases medial meniscal extrusion and improves clinical outcomes and return to activity. Orthop J Sports Med. 2020 doi: 10.1177/2325967120913531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bhatia S, LaPrade CM, Ellman MB, LaPrade RF. Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med. 2014;42(12):3016–3030. doi: 10.1177/0363546514524162. [DOI] [PubMed] [Google Scholar]
- 57.Jarraya M, Roemer FW, Englund M, Crema MD, Gale HI, Hayashi D, et al. Meniscus morphology: does tear type matter? A narrative review with focus on relevance for osteoarthritis research. Semin Arthritis Rheum. 2017;46(5):552–561. doi: 10.1016/j.semarthrit.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 58.LaPrade RF, LaPrade CM, James EW. Recent advances in posterior meniscal root repair techniques. J Am Acad Orthop Surg. 2015;23(2):71–76. doi: 10.5435/JAAOS-D-14-00003. [DOI] [PubMed] [Google Scholar]
- 59.Kwak YH, Lee S, Lee MC, Han HS. Large meniscus extrusion ratio is a poor prognostic factor of conservative treatment for medial meniscus posterior root tear. Knee Surg Sports Traumatol Arthrosc. 2018;26(3):781–786. doi: 10.1007/s00167-017-4441-x. [DOI] [PubMed] [Google Scholar]
- 60.Krych AJ, Reardon PJ, Johnson NR, Mohan R, Peter L, Levy BA, et al. Non-operative management of medial meniscus posterior horn root tears is associated with worsening arthritis and poor clinical outcome at 5-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):383–389. doi: 10.1007/s00167-016-4359-8. [DOI] [PubMed] [Google Scholar]
- 61.Pache S, Aman ZS, Kennedy M, Nakama GY, Moatshe G, Ziegler C, et al. Meniscal root tears: current concepts review. Arch Bone Jt Surg. 2018;6(4):250–259. [PMC free article] [PubMed] [Google Scholar]
- 62.Kim SJ, Choi CH, Chun YM, Kim SH, Lee SK, Jang J, et al. Relationship between preoperative extrusion of the medial meniscus and surgical outcomes after partial meniscectomy. Am J Sports Med. 2017;45(8):1864–1871. doi: 10.1177/0363546517697302. [DOI] [PubMed] [Google Scholar]
- 63.Novaretti JV, Astur DC, Cavalcante ELB, Kaleka CC, Amaro JT, Cohen M. Preoperative meniscal extrusion predicts unsatisfactory clinical outcomes and progression of osteoarthritis after isolated partial medial meniscectomy: a 5-year follow-up study. J Knee Surg. 2020 doi: 10.1055/s-0040-1715109. [DOI] [PubMed] [Google Scholar]
- 64.Strauss EJ, Day MS, Ryan M, Jazrawi L. Evaluation, treatment, and outcomes of meniscal root tears: a critical analysis review. JBJS Rev. 2016;4(8):e4. doi: 10.2106/JBJS.RVW.15.00082. [DOI] [PubMed] [Google Scholar]
- 65.Kodama Y, Furumatsu T, Masuda S, Okazaki Y, Kamatsuki Y, Okazaki Y, et al. Transtibial fixation for medial meniscus posterior root tear reduces posterior extrusion and physiological translation of the medial meniscus in middle-aged and elderly patients. Knee Surg Sports Traumatol Arthrosc. 2020;28(11):3416–3425. doi: 10.1007/s00167-019-05810-x. [DOI] [PubMed] [Google Scholar]
- 66.Stein T, Mehling AP, Welsch F, von Eisenhart-Rothe R, Jäger A. Long-term outcome after arthroscopic meniscal repair versus arthroscopic partial meniscectomy for traumatic meniscal tears. Am J Sports Med. 2010;38(8):1542–1548. doi: 10.1177/0363546510364052. [DOI] [PubMed] [Google Scholar]
- 67.Yanagisawa S, Kimura M, Hagiwara K, Ogoshi A. Association between postoperative meniscal extrusion and clinical outcomes of the pullout fixation technique for medial meniscus posterior root tear. Asia-Pac J Sports Med Arthrosc Rehabil Technol. 2020;1(21):27–31. doi: 10.1016/j.asmart.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chung KS, Ha JK, Ra HJ, Kim JG. A meta-analysis of clinical and radiographic outcomes of posterior horn medial meniscus root repairs. Knee Surg Sports Traumatol Arthrosc. 2016;24(5):1455–1468. doi: 10.1007/s00167-015-3832-0. [DOI] [PubMed] [Google Scholar]
- 69.Feucht MJ, Kühle J, Bode G, Mehl J, Schmal H, Südkamp NP, et al. Arthroscopic transtibial pullout repair for posterior medial meniscus root tears: a systematic review of clinical, radiographic, and second-look arthroscopic results. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2015;31(9):1808–1816. doi: 10.1016/j.arthro.2015.03.022. [DOI] [PubMed] [Google Scholar]
- 70.Jeon SW, Jung M, Choi CH, Kim SG, Kim SH. Factors related to meniscal extrusion and cartilage lesions in medial meniscus root tears. J Knee Surg. 2021;34(2):178–186. doi: 10.1055/s-0039-1693708. [DOI] [PubMed] [Google Scholar]
- 71.Furumatsu T, Kodama Y, Kamatsuki Y, Hino T, Okazaki Y, Ozaki T. Meniscal extrusion progresses shortly after the medial meniscus posterior root tear. Knee Surg Relat Res. 2017;29(4):295–301. doi: 10.5792/ksrr.17.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Moon HS, Choi CH, Jung M, Lee DY, Hong SP, Kim SH. Early surgical repair of medial meniscus posterior root tear minimizes the progression of meniscal extrusion: 2-year follow-up of clinical and radiographic parameters after arthroscopic transtibial pull-out repair. Am J Sports Med. 2020;48(11):2692–2702. doi: 10.1177/0363546520940715. [DOI] [PubMed] [Google Scholar]
- 73.Chung KS, Ha JK, Ra HJ, Nam GW, Kim JG. Pullout Fixation of posterior medial meniscus root tears: correlation between meniscus extrusion and midterm clinical results. Am J Sports Med. 2017;45(1):42–49. doi: 10.1177/0363546516662445. [DOI] [PubMed] [Google Scholar]
- 74.Krych AJ, Bernard CD, Leland DP, Camp CL, Johnson AC, Finnoff JT, et al. Isolated meniscus extrusion associated with meniscotibial ligament abnormality. Knee Surg Sports Traumatol Arthrosc. 2020;28(11):3599–3605. doi: 10.1007/s00167-019-05612-1. [DOI] [PubMed] [Google Scholar]
- 75.Krych AJ, LaPrade MD, Hevesi M, Rhodes NG, Johnson AC, Camp CL, et al. Investigating the chronology of meniscus root tears: do medial meniscus posterior root tears cause extrusion or the other way around? Orthop J Sports Med. 2020 doi: 10.1177/2325967120961368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Paletta GA, Crane DM, Konicek J, Piepenbrink M, Higgins LD, Milner JD, et al. Surgical treatment of meniscal extrusion: a biomechanical study on the role of the medial meniscotibial ligaments with early clinical validation. Orthop J Sports Med. 2020;8(7):2325967120936672. doi: 10.1177/2325967120936672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Koga H, Muneta T, Watanabe T, Mochizuki T, Horie M, Nakamura T, et al. Two-year outcomes after arthroscopic lateral meniscus centralization. Arthroscopy. 2016;32(10):2000–2008. doi: 10.1016/j.arthro.2016.01.052. [DOI] [PubMed] [Google Scholar]
- 78.Chernchujit B, Prasetia R. Arthroscopic direct meniscal extrusion reduction: surgical tips to reduce persistent meniscal extrusion in meniscal root repair. Eur J Orthop Surg Traumatol. 2018;28(4):727–734. doi: 10.1007/s00590-018-2138-6. [DOI] [PubMed] [Google Scholar]
- 79.Chernchujit B, Agrawal S. Arthroscopic all-inside medial meniscus extrusion reduction. Arthrosc Tech. 2019;8(5):e495–501. doi: 10.1016/j.eats.2019.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Dean RS, DePhillipo NN, Monson JK, LaPrade RF. Peripheral stabilization suture to address meniscal extrusion in a revision meniscal root repair: surgical technique and rehabilitation protocol. Arthrosc Tech. 2020;9(8):e1211–e1218. doi: 10.1016/j.eats.2020.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.DePhillipo NN, Kennedy MI, Chahla J, LaPrade RF. Type II medial meniscus root repair with peripheral release for addressing meniscal extrusion. Arthrosc Tech. 2019;8(9):e941–e946. doi: 10.1016/j.eats.2019.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Leafblad ND, Smith PA, Stuart MJ, Krych AJ. Arthroscopic centralization of the extruded medial meniscus. Arthrosc Tech. 2021;10(1):e43–e48. doi: 10.1016/j.eats.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Okazaki Y, Furumatsu T, Miyazawa S, Kodama Y, Kamatsuki Y, Hino T, et al. Meniscal repair concurrent with anterior cruciate ligament reconstruction restores posterior shift of the medial meniscus in the knee-flexed position. Knee Surg Sports Traumatol Arthrosc. 2019;27(2):361–368. doi: 10.1007/s00167-018-5157-2. [DOI] [PubMed] [Google Scholar]
- 84.Jacob G, An S, Kumar G, Varghese J. Percutaneous arthroscopic assisted knee medial collateral ligament repair. Arthrosc Tech. 2020;9(10):e1511–e1517. doi: 10.1016/j.eats.2020.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tsujii A, Yonetani Y, Kinugasa K, Matsuo T, Yoneda K, Ohori T, et al. Outcomes more than 2 years after meniscal repair for radial/flap tears of the posterior lateral meniscus combined with anterior cruciate ligament reconstruction. Am J Sports Med. 2019;47(12):2888–2894. doi: 10.1177/0363546519869955. [DOI] [PubMed] [Google Scholar]
- 86.Delincé P, Ghafil D. Anterior cruciate ligament tears: conservative or surgical treatment? A critical review of the literature. Knee Surg Sports Traumatol Arthrosc. 2012;20(1):48–61. doi: 10.1007/s00167-011-1614-x. [DOI] [PubMed] [Google Scholar]
- 87.Kashihara N, Furumatsu T, Kodama Y, Tanaka T, Ozaki T. Concurrent lateral meniscal repair with anterior cruciate ligament reconstruction induces the extrusion of the lateral meniscus: assessments of magnetic resonance images. Acta Med Okayama. 2016;70(6):441–448. doi: 10.18926/AMO/54806. [DOI] [PubMed] [Google Scholar]
- 88.Narazaki S, Furumatsu T, Tanaka T, Fujii M, Miyazawa S, Inoue H, et al. Postoperative change in the length and extrusion of the medial meniscus after anterior cruciate ligament reconstruction. Int Orthop. 2015;39(12):2481–2487. doi: 10.1007/s00264-015-2704-z. [DOI] [PubMed] [Google Scholar]
- 89.Winkler PW, Wierer G, Csapo R, Hepperger C, Heinzle B, Imhoff AB, et al. Quantitative evaluation of dynamic lateral meniscal extrusion after radial tear repair. Orthop J Sports Med. 2020;8(4):2325967120914568. doi: 10.1177/2325967120914568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Tsujii A, Yonetani Y, Kinugasa K, Matsuo T, Yoneda K, Ohori T, et al. Outcomes more than 2 years after meniscal repair for longitudinal tears of the lateral meniscus combined with anterior cruciate ligament reconstruction. Am J Sports Med. 2021;49(3):684–692. doi: 10.1177/0363546520981976. [DOI] [PubMed] [Google Scholar]
- 91.Ichiba A, Makuya K. Radial displacement of the lateral meniscus before and after anterior cruciate ligament reconstruction. Arch Orthop Trauma Surg. 2012;132(3):321–327. doi: 10.1007/s00402-011-1371-9. [DOI] [PubMed] [Google Scholar]
- 92.Kamatsuki Y, Furumatsu T, Fujii M, Kodama Y, Miyazawa S, Hino T, et al. Complete tear of the lateral meniscus posterior root is associated with meniscal extrusion in anterior cruciate ligament deficient knees. J Orthop Res Off Publ Orthop Res Soc. 2018;36(7):1894–1900. doi: 10.1002/jor.23861. [DOI] [PubMed] [Google Scholar]
- 93.Kodama Y, Furumatsu T, Miyazawa S, Fujii M, Tanaka T, Inoue H, et al. Location of the tibial tunnel aperture affects extrusion of the lateral meniscus following reconstruction of the anterior cruciate ligament. J Orthop Res. 2017;35(8):1625–1633. doi: 10.1002/jor.23450. [DOI] [PubMed] [Google Scholar]
- 94.Shefelbine SJ, Ma CB, Lee KY, Schrumpf MA, Patel P, Safran MR, et al. MRI analysis of in vivo meniscal and tibiofemoral kinematics in ACL-deficient and normal knees. J Orthop Res Off Publ Orthop Res Soc. 2006;24(6):1208–1217. doi: 10.1002/jor.20139. [DOI] [PubMed] [Google Scholar]
- 95.Wenger A, Englund M, Wirth W, Hudelmaier M, Kwoh K, Eckstein F, et al. Relationship of 3D meniscal morphology and position with knee pain in subjects with knee osteoarthritis: a pilot study. Eur Radiol. 2012;22(1):211–220. doi: 10.1007/s00330-011-2234-z. [DOI] [PubMed] [Google Scholar]
- 96.Lee DW, Jang HW, Lee SR, Park JH, Ha JK, Kim JG. Clinical, radiological, and morphological evaluations of posterior horn tears of the lateral meniscus left in situ during anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42(2):327–335. doi: 10.1177/0363546513508374. [DOI] [PubMed] [Google Scholar]
- 97.Shelbourne KD, Roberson TA, Gray T. Long-term evaluation of posterior lateral meniscus root tears left in situ at the time of anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39(7):1439–1443. doi: 10.1177/0363546511398212. [DOI] [PubMed] [Google Scholar]
- 98.Katagiri H, Miyatake K, Nakagawa Y, Otabe K, Ohara T, Shioda M, et al. The effect of a longitudinal tear of the medial meniscus on medial meniscal extrusion in anterior cruciate ligament injury patients. Knee. 2019;26(6):1292–1298. doi: 10.1016/j.knee.2019.07.019. [DOI] [PubMed] [Google Scholar]
- 99.Zhang ZZ, Zhou YF, Luo H, Zhang HZ, Chen Z, Jiang C, et al. A novel surgical technique for arthroscopic repair of type II posterior lateral meniscal root tear. Knee. 2020;27(5):1560–1566. doi: 10.1016/j.knee.2020.07.100. [DOI] [PubMed] [Google Scholar]
- 100.Zheng T, Song G, Li Y, Zhang Z, Ni Q, Cao Y, et al. Clinical, radiographic, and arthroscopic outcomes of surgical repair for radial and avulsed lesions on the lateral meniscus posterior root during ACL reconstruction: a systematic review. Orthop J Sports Med. 2021;9(3):2325967121989678. doi: 10.1177/2325967121989678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Koga H, Watanabe T, Horie M, Katagiri H, Otabe K, Ohara T, et al. Augmentation of the pullout repair of a medial meniscus posterior root tear by arthroscopic centralization. Arthrosc Tech. 2017;6(4):e1335–e1339. doi: 10.1016/j.eats.2017.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Masferrer-Pino A, Monllau JC, Abat F, Gelber PE. Capsular fixation limits graft extrusion in lateral meniscal allograft transplantation. Int Orthop. 2019;43(11):2549–2556. doi: 10.1007/s00264-019-04398-8. [DOI] [PubMed] [Google Scholar]
- 103.Figueroa F, Figueroa D, Calvo R, Vaisman A, Espregueira-Mendes J. Meniscus allograft transplantation: indications, techniques and outcomes. EFORT Open Rev. 2019;4(4):115–120. doi: 10.1302/2058-5241.4.180052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.González-Lucena G, Gelber PE, Pelfort X, Tey M, Monllau JC. Meniscal allograft transplantation without bone blocks: a 5- to 8-year follow-up of 33 patients. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2010;26(12):1633–1640. doi: 10.1016/j.arthro.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 105.Jang SH, Kim JG, Ha JG, Shim JC. Reducing the size of the meniscal allograft decreases the percentage of extrusion after meniscal allograft transplantation. Arthroscopy. 2011;27(7):914–922. doi: 10.1016/j.arthro.2011.02.017. [DOI] [PubMed] [Google Scholar]
- 106.Kim JH, Lee S, Ha DH, Lee SM, Jung K, Choi W. The effects of graft shrinkage and extrusion on early clinical outcomes after meniscal allograft transplantation. J Orthop Surg. 2018;13(1):181. doi: 10.1186/s13018-018-0892-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ha JK, Shim JC, Kim DW, Lee YS, Ra HJ, Kim JG. Relationship between meniscal extrusion and various clinical findings after meniscus allograft transplantation. Am J Sports Med. 2010;38(12):2448–2455. doi: 10.1177/0363546510375550. [DOI] [PubMed] [Google Scholar]
- 108.Ha JK, Jang HW, Jung JE, Cho SI, Kim JG. Clinical and radiologic outcomes after meniscus allograft transplantation at 1-year and 4-year follow-up. Arthroscopy. 2014;30(11):1424–1429. doi: 10.1016/j.arthro.2014.05.032. [DOI] [PubMed] [Google Scholar]
- 109.Merkely G, Ogura T, Ackermann J, Mestriner AB, Minas T, Gomoll AH. Open meniscal allograft transplantation with transosseous suture fixation of the meniscal body significantly decreases meniscal extrusion rate compared with arthroscopic technique. Arthroscopy. 2019;35(6):1658–1666. doi: 10.1016/j.arthro.2018.11.063. [DOI] [PubMed] [Google Scholar]
- 110.Jiang D, Ao YF, Gong X, Wang YJ, Zheng ZZ, Yu JK. Comparative study on immediate versus delayed meniscus allograft transplantation: 4- to 6-year follow-up. Am J Sports Med. 2014;42(10):2329–2337. doi: 10.1177/0363546514541653. [DOI] [PubMed] [Google Scholar]
- 111.Jauregui JJ, Wu ZD, Meredith S, Griffith C, Packer JD, Henn RF. How should we secure our transplanted meniscus? A Meta-analysis Am J Sports Med. 2018;46(9):2285–2290. doi: 10.1177/0363546517720183. [DOI] [PubMed] [Google Scholar]
- 112.Smith NA, Parkinson B, Hutchinson CE, Costa ML, Spalding T. Is meniscal allograft transplantation chondroprotective? A systematic review of radiological outcomes. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2016;24(9):2923–2935. doi: 10.1007/s00167-015-3573-0. [DOI] [PubMed] [Google Scholar]
- 113.Lee SM, Bin SI, Kim JM, Lee BS, Lee CR, Son DW, et al. Long-term outcomes of meniscal allograft transplantation with and without extrusion: mean 12.3-year follow-up study. Am J Sports Med. 2019;47(4):815–821. doi: 10.1177/0363546518825251. [DOI] [PubMed] [Google Scholar]
- 114.Son DW, Bin SI, Kim JM, Lee BS, Lee CR, Park JG, et al. Extrusions do not affect degenerative morphologic changes in lateral meniscus allografts during midterm follow-ups. Knee Surg Sports Traumatol Arthrosc. 2021;29(4):1197–1205. doi: 10.1007/s00167-020-06120-3. [DOI] [PubMed] [Google Scholar]
- 115.Song JH, Bin SI, Kim JM, Lee BS. Postoperative subchondral bone marrow lesion is associated with graft extrusion after lateral meniscal allograft transplantation. Am J Sports Med. 2020;48(13):3163–3169. doi: 10.1177/0363546520959316. [DOI] [PubMed] [Google Scholar]
- 116.Bin SI, Nha KW, Cheong JY, Shin YS. Midterm and long-term results of medial versus lateral meniscal allograft transplantation: a meta-analysis. Am J Sports Med. 2018;46(5):1243–1250. doi: 10.1177/0363546517709777. [DOI] [PubMed] [Google Scholar]
- 117.Noyes FR, Barber-Westin SD. Long-term survivorship and function of meniscus transplantation. Am J Sports Med. 2016;44(9):2330–2338. doi: 10.1177/0363546516646375. [DOI] [PubMed] [Google Scholar]
- 118.Parkinson B, Smith N, Asplin L, Thompson P, Spalding T. Factors predicting meniscal allograft transplantation failure. Orthop J Sports Med. 2016;4(8):2325967116663185. doi: 10.1177/2325967116663185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Van Der Straeten C, Byttebier P, Eeckhoudt A, Victor J. Meniscal allograft transplantation does not prevent or delay progression of knee osteoarthritis. PLoS ONE. 2016;11(5):e0156183. doi: 10.1371/journal.pone.0156183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Noyes FR, Barber-Westin SD. A systematic review of the incidence and clinical significance of postoperative meniscus transplant extrusion. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):290–302. doi: 10.1007/s00167-014-3329-2. [DOI] [PubMed] [Google Scholar]
- 121.Gelber PE, Torres-Claramunt R, Poggioli F, Pérez-Prieto D, Monllau JC. Polyurethane Meniscal Scaffold: Does Preoperative Remnant Meniscal Extrusion Have an Influence on Postoperative Extrusion and Knee Function? J Knee Surg. 2020 doi: 10.1055/s-0040-1710377. [DOI] [PubMed] [Google Scholar]
- 122.Monllau JC, Ibañez M, Masferrer-Pino A, Gelber PE, Erquicia JI, Pelfort X. Lateral capsular fixation: an implant-free technique to prevent meniscal allograft extrusion. Arthrosc Tech. 2017;6(2):e269–e274. doi: 10.1016/j.eats.2016.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Ahn JH, Kang HW, Yang TY, Lee JY. Multivariate analysis of risk factors of graft extrusion after lateral meniscus allograft transplantation. Arthroscopy. 2016;32(7):1337–1345. doi: 10.1016/j.arthro.2015.12.050. [DOI] [PubMed] [Google Scholar]
- 124.Kim NK, Bin SI, Kim JM, Lee CR, Kim JH. Meniscal extrusion does not progress during the midterm follow-up period after lateral meniscal transplantation. Am J Sports Med. 2017;45(4):900–908. doi: 10.1177/0363546516675605. [DOI] [PubMed] [Google Scholar]
- 125.Yoon JR, Kim TS, Lee YM, Jang HW, Kim YC, Yang JH. Transpatellar approach in lateral meniscal allograft transplantation using the keyhole method: can we prevent graft extrusion? Knee Surg Sports Traumatol Arthrosc. 2011;19(2):214–217. doi: 10.1007/s00167-010-1250-x. [DOI] [PubMed] [Google Scholar]
- 126.Kim YS, Kang KT, Son J, Kwon OR, Choi YJ, Jo SB, et al. Graft extrusion related to the position of allograft in lateral meniscal allograft transplantation: biomechanical comparison between parapatellar and transpatellar approaches using finite element analysis. Arthroscopy. 2015;31(12):2380–2391.e2. doi: 10.1016/j.arthro.2015.06.030. [DOI] [PubMed] [Google Scholar]
- 127.Ren S, Zhang X, You T, Jiang X, Jin D, Zhang W. Clinical and radiologic outcomes after a modified bone plug technique with anatomical meniscal root reinsertion for meniscal allograft transplantation and a minimum 18-month follow-up. J Orthop Surg. 2018;24(13):97. doi: 10.1186/s13018-018-0776-3. [DOI] [PMC free article] [PubMed] [Google Scholar]