Abstract
Objective:
The use of Common Data Elements (CDEs) is growing in medical research; CDEs have demonstrated benefit in maximizing the impact of existing research infrastructure and funding. However, the field of burn care does not have a standard set of CDEs. The objective of this study is to examine the extent of common data collected in current burn databases.
Methods:
This study examines the data dictionaries of six U.S. burn databases to ascertain the extent of common data. This was assessed from a quantitative and qualitative perspective. Thirty-two demographic and clinical data elements were examined. The number of databases that collect each data element was calculated. The data values for each data element were compared across the six databases for common terminology. Finally, the data prompts of the data elements were examined for common language and structure.
Results:
Five (16%) of the thirty-two data elements are collected by all six burn databases; additionally, five data elements (16%) are present in only one database. Furthermore, there are considerable variations in data values and prompts used among the burn databases. Only one of the thirty-two data elements (age) contains the same data values across all databases.
Conclusions:
The burn databases examined show minimal evidence of common data. There is a need to develop CDEs and standardized coding to enhance interoperability of burn databases.
Keywords: common data elements, burn, database, interoperability, outcomes
Introduction
Burns are a global public health problem. In 2004, close to 11 million people worldwide were burned severely enough to require medical attention. Non-fatal burns are a leading cause of morbidity, including prolonged hospitalization, disfigurement, and disability.1 With improvements in burn survival,2,3 it is important to define and understand the health needs of the burn survivor population to optimize their path to recovery and improve their quality of life. Clinical advances are dependent upon existing research infrastructure and funding climate. Therefore, the burn care community is compelled to maximize the utility of their clinical and research initiatives. Many fields have turned to common data elements (CDEs) to better leverage existing efforts to greater effect.4 CDEs are defined as data elements that are common to multiple data sets across different studies.4 CDEs have multiple potential benefits. To start, it is desirable to link existing databases in order to provide the most complete picture of the burn survivor’s experience. Data connecting the circumstances of injury, initial interventions, early rehabilitation and long-term outcomes of burn survivors are currently limited. Several databases exist that are accumulating information on different aspects of the clinical course of survivors; CDEs would enable the linkage of these databases. Additionally, CDEs enable the synthesis of findings across studies that foster comparative effectiveness research, which includes meta-analysis. Separately, database research is enhanced by use of CDEs that enable linkage and comparisons between datasets. In other populations, CDEs have enabled studies using data from multiple trials.5 Pooling data from multiple sources can result in stronger results obtained through more efficient mode.6 However, the ability to link and compare databases is dependent upon the use of consistent definitions of demographic and clinical characteristics. The first step in the process of implementing CDEs is to assess the extent of common data in current burn databases. Therefore, the purpose of this study is to examine congruity in the demographic and clinical information among current burn databases.
Methods
This study examines the data dictionaries of six commonly used burn databases in the United States to ascertain the extent of common data.
Databases
Databases were selected for review that contain burn-specific information cited in peer review publications, and have accessible data dictionaries or collection forms. Six burn databases were chosen for this study: the National Burn Repository (NBR), the Burn Model System National Database (BMS), the pediatric American Burns Association/Shriners Hospitals for Children Burn Outcome Questionnaires (BOQ), the Young Adult Burn Outcome Questionnaire (YABOQ), the Life Impact Burn Recovery Evaluation Profile (LIBRE), and Uniform Data System for Medical Rehabilitation (UDSMR). Brief descriptions of each of the databases are listed below:
The NBR, an American Burn Association database, aggregates information on patients treated at contributing burn centers with a focus on data regarding the circumstances of the injury and acute hospitalization. Data collection has recently expanded to include quality improvement data (e.g. Burn Quality Improvement Program).7 Entry criteria include admission to a burn center.8
The BMS database contains prospectively collected data on burn survivors from all age groups. Data is collected at National Institute on Disability, Independent Living and Rehabilitation Research (NIDILRR) funded burn centers and focuses on long-term recovery. To be enrolled, subjects must meet at least one of the following current inclusion criteria: (1) 0-64 years of age with a burn injury ≥20% TBSA, (2) ≥65 years of age with a burn injury ≥10% TBSA, (3) burn injury to the face/neck, hands, or feet, (4) high-voltage electrical burn injury. All subjects need to have undergone an operative intervention for wound closure. Data collection time points include acute hospital discharge and 6, 12, and 24 months post-injury. More recently, data collection was added every 5 years following injury.9
The BOQ database contains patient and family-reported outcomes data from burn survivors and normative samples. Subjects are enrolled near the end of their acute hospital course or in the outpatient clinic. The BOQ has three different sets of scales for varying age groups: 0-5 years (parent proxy reported), 5-18 years (parent proxy reported), and 11-18 years (child-reported). For the purposes of this analysis, databases are treated as one because of their similar demographic and clinical elements10–12.
The YABOQ database contains information from young adult burn survivors (19-30 years) as well as a normative age matched sample without burns and has a focus on long-term burn outcomes and recovery. Similar to the other BOQs, subjects are recruited from the hospital or the outpatient burn clinic.13
The LIBRE database collects information from a national sample of adult, community-dwelling burn survivors and focuses on community reintegration and social participation outcomes.14
UDSMR is a national database of inpatient rehabilitation facilities. It contains demographic, clinical, and functional data from approximately 70% of U.S. inpatient rehabilitation facilities. These data include the Functional Independence Measure (FIM), a validated instrument that assesses function.15
The NBR, BMS, and UDSMR database dictionaries were accessed from their respective websites.8,9,15 The BOQ and YABOQ data dictionaries were accessed by contacting the multi-center burn outcome group, led by Clinical Research at the Shriners Hospital for Children-Boston and the Sumner Redstone Burn Center at the Massachusetts General Hospital.16 The data dictionary for LIBRE was accessed by contacting the LIBRE Project at Boston University.14
Data Definitions: Data Elements, Data Values and Data Prompts
A data element is defined as a logical unit of information involving one type of data that has a name, precise definition, and defined values. For example, Race and Inhalation Injury are data elements. A data value is defined as the set of permissible values or responses for that data element. For example, the data element ‘Race’ can include data values such as ‘White’, ‘Pacific Islander’, or ‘Asian’. A data prompt is the specific wording of the prompt or question associated with each data element and value. For example, “What is your age?” or “Age:” are data prompts for the data element ‘Age’.
In total, thirty-two data elements were examined in this study, consisting of fourteen demographic and eighteen clinical elements. The demographic data included: gender/sex, age, ethnicity/race, accommodation (i.e. house/apartment, school dormitory, nursing home etc.), living with (i.e. alone or with someone), work status, school status, occupation, highest level of education, marital status, guardian(s) occupation, guardian(s) highest level of education, disability income, and insurance. The clinical data included: injury date, admission date, burn etiology, total body surface area (TBSA) burned, TBSA grafted, burn thickness, anatomic injury location, inhalation injury, associated non-burn injury, geographic injury location (location of injury: e.g. home, workplace), circumstances of injury (e.g. intentional employment-related, non-intentional non-work related), discharge disposition, length of stay, total ICU days, ventilator days, comorbid conditions, alcohol use, and drug use. The data values and data prompts for each data element were examined for each of the six databases.
Analysis
The purpose of the analysis was to assess the extent of shared data elements, data values, and data prompts among the six examined databases. This was assessed from a quantitative and qualitative perspective. Thirty-two data elements were examined. The number of databases that collect each data element was calculated. The data values for each data element were compared across the six databases for common terminology. Finally, the data prompts of the data elements were examined for common language and structure. Qualitative differences in the data were explored in more detail to highlight meaningful differences between datasets.
Results
There are discrepancies across all databases in the presence of data elements. Most data elements are not found within all, or even most, of the databases (Table 1). Five (16%) of the thirty-two data elements are present in all six databases (age, gender/sex, ethnicity/race, injury date, anatomic injury location). Six data elements are found in five of the six databases, while eight elements are found in four of the six databases, and seven elements are found in three of the six databases. There are five data elements that are present in only one of the six databases (TBSA grafted, ICU days, disability income, guardian occupation, guardian highest level of education).
Table 1:
Comparison of data elements among six burn databases
| Variables | Databases | |||||
|---|---|---|---|---|---|---|
| BMS | BOQ | YABOQ | LIBRE | NBR | UDSMR | |
| Gender/ Sex | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Age | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Ethnicity/ Race | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Accommodation | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Living With | ✓ | ✓ | ✓ | ✓ | ||
| Work Status | ✓ | N/A | ✓ | ✓ | ✓ | |
| School Status | ✓ | ✓ | N/A | N/A | ✓ | |
| Occupation | ✓ | N/A | ✓ | ✓ | ✓ | |
| Highest Level of Education | ✓ | ✓ | N/A | N/A | ||
| Marital Status | ✓ | N/A | ✓ | ✓ | ✓ | ✓ |
| Guardian(s) Occupation | ✓ | N/A | N/A | |||
| Guardian(s) Highest Level of Education | ✓ | N/A | N/A | |||
| Disability Income | ✓ | |||||
| Insurance | ✓ | ✓ | ✓ | ✓ | ||
| Alcohol Use | ✓ | N/A | ✓ | ✓ | ||
| Drug Use | ✓ | N/A | ✓ | ✓ | ||
| Injury Date | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Admission to Care Date | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Burn Etiology | ✓ | ✓ | ✓ | ✓ | ||
| TBSA Burned | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Severity (Burn Thickness) | ✓ | ✓ | ✓ | |||
| Anatomic Injury Location | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Inhalation Injury | ✓ | ✓ | ✓ | ✓ | ||
| Non-Burn Injury | ✓ | ✓ | ✓ | |||
| Geographic Injury Location | ✓ | ✓ | ✓ | |||
| Circumstance of Injury | ✓ | ✓ | ✓ | |||
| TBSA Grafted | ✓ | |||||
| Discharge Disposition | ✓ | ✓ | ✓ | ✓ | ||
| Length of Stay | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Intensive Care Unit Days | ✓ | |||||
| Ventilator Days | ✓ | ✓ | ✓ | ✓ | ||
| Comorbid Conditions | ✓ | ✓ | ✓ | ✓ | ✓ | |
TBSA: Total Body Surface Area Burned
NBR: National Burn Repository
UDSMR: Uniform Data System for Medical Rehabilitation
LIBRE: Life Impact Burn Recovery Evaluation Profile
BOQ: Burn Outcome Questionnaires
YABOQ: Young Adult Burn Outcome Questionnaire
BMS: Burn Model System National Database
In addition to the differing data elements, there are considerable variations in data values used among the burn databases. Among the five variables that all databases collected, differences in values occur in four of the variables (80%). Only one of the elements, ‘age’, contains the same data values across all six databases. Data values exhibit varying levels of detail. For example, in coding the anatomical burn location, ‘buttocks’ and ‘genitals’ are defined as separate anatomic locations in one database, but merged into one variable, ‘perineum’, in another database. Other databases exhibit isolated specificity with regards to coding of burn location, only coding critical areas (face, hands, genitals) burned and not including all anatomical locations. Differences in coding of numeric variables are also noted. TBSA burned was coded continuously in some databases and categorically in others. Additional differences were noted among the databases that coded TBSA burned categorically. Some databases adopt a cutoff of above 5%; some use 0.1-9.9%, 10-19.9%; others use 0-15%, 16-30% etc. There are also differences in the word choices of data values, which may or may not represent real differences in the data. For example, ‘White’ and ‘Caucasian’, were used to describe racial groups in different databases. “Married/Living with Significant Other” is an option for “Marital Status” in one database while “Domestic Partnership” and “Married” are separate options in another database. Differences are also noted within the procedures of coding data values. Only some databases addressed how to code a transgender value within the ‘gender/sex’ element. Three data elements (gender/sex, ethnicity/race, and anatomic injury location) and their data values across all databases are presented in Table 2 as an example of issues of congruity. A complete listing of the data elements and values of all six databases are presented in Appendix A (Adult) and Appendix B (Children).
Table 2:
Comparison of data values across adult burn databases for three data elements
| Variables | BMS | YABOQ | LIBRE | NBR | UDSMR |
|---|---|---|---|---|---|
| Gender/Sex | Male or Female: 1.Male 2. Female For participants who are transgender, chosen gender is coded rather than biological gender. |
Male or Female: 1.Male 2.Female |
Male or Female: 1.Male 2.Female |
Male or Female: 1.Male 2.Female For participants who are transgender, chosen gender is coded rather than biological gender. |
Male or Female: 1.Male 2.Female |
| Ethnicity/Race | Race: 1. Black or African-American 2. Asian 3. Caucasian 4. American Indian/Alaskan Native 5. Native Hawaiian or Other Pacific Islander 6. More than one race 7. Other [text field] Ethnicity: 1. Hispanic or Latino 2. Not Hispanic or Latino |
Race: 1. White, non-Hispanic 2. Black, non-Hispanic 3. Hispanic/Latino 4. Pacific Islander 5. Asian 6. Native American 7. Other |
Race: 1. White 2. Black or African American 3. Asian 4. American Indian or Alaskan Native 5. Native Hawaiian or Pacific Islander 6. Multiracial 7. Other 8. Prefer not to answer Ethnicity: 1. Hispanic or Latino 2. Not Hispanic or Latino |
Allowed to check two races: 1. Asian 2. Native Hawaiian or other Pacific Islander 3. Other race 4. American Indian or Alaskan Native 5. Black or African American 6. Caucasian Ethnicity: 1. Hispanic or Latino 2. Not Hispanic or Latino |
Race / Ethnicity: 1. American Indian or Alaskan Native 2. Asian 3. Black or African American 4. Hispanic or Latino 5. Native Hawaiian or other Pacific Islander 6. White |
| Anatomic Injury Location(Burn) | Location is broken into categories to answer: 1. Head/Face/ Neck: a. Yes b. No c. Unknown 2. Trunk (back, chest, abdomen): a. Yes b. No c. Unknown 3. Perineum (buttock, genitals): a. Yes b. No c. Unknown 4. Shoulder/ Upper Arm /Elbow: a. Right b. Left c. Bilateral d. None e. Unknown 5. Forearm (includes wrist): a. Right b. Left c. Bilateral d. None e. Unknown 6. Hand: a. Right b. Left c. Bilateral d. None e. Unknown 7. Leg: a. Right b. Left c. Bilateral d. None e. Unknown 8. Foot: a. Right b. Left c. Bilateral d. None e. Unknown |
Anatomic burn location is prompted. 1. Face involved a. No b. Yes 2. Hands involved a. No b. Yes 3. Genitals involved a. No b. Yes |
Anatomic burn location is prompted. 1. Back 2. Face 3. Head 4. Neck 5. Hands 6. Feet 7. Legs 8. Torso/Trunk 9. Genitals 10. Arms 11. Other; [text field] |
Anatomic burn location of 2nd and 3rd degree burn: 1. Head 2. Neck 3. Anterior and posterior trunk 4. Buttocks 5. Genitalia 6. Upper arm 7. Lower arm 8. Hand 9. Thigh 10. Leg 11. Foot |
Location can be identified through respective ICD-9 Codes. |
BMS: Burn Model System National Database
YABOQ: Young Adult Burn Outcome Questionnaire
LIBRE: Life Impact Burn Recovery Evaluation Profile
NBR: National Burn Repository
UDSMR: Uniform Data System for Medical Rehabilitation
Data prompts demonstrate inconsistencies across the six databases. For example, each database that collects ‘drug use’ and ‘alcohol use’ information uses a different data prompt. One database uses the CAGE screening questions, while another relies on laboratory tests to assess alcohol and drug use. The level of detail prompted also varies. One database records specific drugs used and another prompts frequency of alcohol and drug use. Finally, only one database collects information on treatment for drug or alcohol issues. Data prompts also demonstrate differences in the queried time period. ‘Living with’ is prompted for several different time points across the different databases: pre-injury, pre-hospitalization, at time of injury, and post-hospitalization. None of the databases collects this information for same time periods.
Discussion
This is the first study to assess the congruity of data elements, data values, and data prompts of multiple burn databases. This study demonstrates significant differences in data collection across all databases. This lack of CDEs has several implications to the field of burn care and research. The incongruity limits the ability to compare findings of different databases. Further, the ability to combine databases to examine similar outcomes is limited. Given the challenges of small sample size studies, CDEs have the potential to improve statistical power to address important clinical queries. This is particularly helpful for uncommon traumatic injuries, diseases, or conditions and especially relevant in the field of burn care given the size of the field and limited resources. The use of CDEs augments the data pool by aggregating data from different systems in a common fashion and enables linkage of databases with different focuses.
Statistical analyses that integrate data from multiple databases are often hindered by a lack of CDEs. For example, propensity score matching is used to estimate the effect of an intervention by determining covariates that are predictors of receiving the intervention. The use of this type of analysis is predicated on co-variables that are clean and consistent. Comparative effectiveness studies rely on sample sizes sufficient for purposes of risk adjustment. The sample size is often achievable when using multiple databases, but this is not possible when covariates are not consistent across the databases. Pooling studies depend on linkages among different datasets at the individual subject level. Congruent variables among different data sets are required to identify predictor variables, risk adjustors, and outcomes. Lack of congruence among data elements hinders the ability to conduct studies that require large sample of combined datasets for adequate power. Finally, a lack of CDEs limits the ability to reliably adjust for potential confounders or evaluate for mediators in multivariable models in cross-sectional and longitudinal studies.
In addition, examination of data elements used in other conditions is an important consideration for the establishment of burn CDEs. Certain domains of long-term outcomes such as post-traumatic stress disorder, neuropathic pain, or impaired mobility may be shared across injury groups. A set of CDEs shared by multiple injury groups would allow for greater comparison across conditions. There is potential for learning from combined datasets that could be applied to improve burn care or optimize care in people with similar problems resulting from different conditions.
The inconsistencies displayed in data elements and values underscore the need for standardization of data syntax and data ontology. Data ontology is a computer science concept, which entails the name, definition, fundamental properties and inter-correlations of a domain or entity. In this case, for example, the data ontologies for TBSA burned are heterogeneous in various burn databases. Some of them adopt a cutoff of above 5%; some use 0.1-9.9%, 10-19.9%; others use 0-15%, 16-30% etc. Moreover, ICD-10 coding for burn size include the following groupings: 0% to 9%, 10-19%, 20-29%, etc.17 This concept extends to new initiatives such as the electronic burn diagram where standard formats could prevent isolated data islands that do not connect and interact with each other.18 To seamlessly harmonize these databases, standardization of data syntax and data ontology is essential.
From a clinical perspective, robust, reliable, and accurate data is essential for quality improvement initiatives in burn care. Without high quality data, it is difficult to assess the quality of care, let alone to measure the effectiveness of quality improvement interventions. Continuous improvement in burn care is highly dependent on measuring what works and what does not by consistently assessing and reassessing care quality through clinical databases. With the creation of burn specific CDEs, the validity and reliability for database linking will be potentially strengthened. Furthermore, the scale of data collection efforts could be multiplied to accelerate improvement efforts. Just as the American College of Surgeons developed the National Surgical Quality Improvement Program, the American Burn Association developed the Burn Quality Improvement Program,7 whose efforts have the potential to significantly accelerate creation of CDEs and linking different databases. As we move rapidly towards value based purchasing, it is imperative to deliver high quality burn care at a lower cost by fast-tracking quality improvement efforts through better data collection and a new standardization process. Furthermore, the American Burn Association’s efforts to harmonize data elements with the National Burn Repository8 and Burn Quality Improvement Program7 are significant efforts in the direction of creating CDEs in the field of burns. These efforts should be used as a starting point for future widespread burn CDE development.
The process of developing CDEs requires significant broad-based efforts and is not without its challenges; however, lessons can be learned from other fields that have already developed CDEs. The National Institute of Neurological Disorders and Stroke (NINDS) has outlined a process for creating CDEs; some already established CDEs used a variation of this method.19,20 The NINDS facilitates and manages the creation of new CDEs under the umbrella of the NINDS CDEs Team. The first step is reviewing all current data collection practices, including relevant literature and studies, and clinical data standards. Concurrently, a working group representing a wide range of experts in the field is formed to examine data elements and data values with the goal of defining the scope and content of the CDEs. In an iterative process, multiple drafts of the CDEs are proposed and revised until finalized and subsequently published. This process takes anywhere from a few months to over a year. Thereafter, the process includes regular reevaluation and revision of the published CDEs to maintain up to date standards. NINDS is the exemplar branch within NIH in leading CDEs development in multiple disease and injury groups and as such offers lessons for the burn community on the path forward.
Finally, the quest for CDEs in burn databases is but a subset of an overarching initiative long in gestation within the American Burn Association Committee on Organization and Delivery of Burn Care. This committee has been advancing ABA-sanctioned standards for “data syntax” and “data ontology” for all software employed in the burn care clinical community. The fact that burn databases are not currently interoperable foreshadows a missed future and lost opportunity as technology continues to advance into many aspects of burn care.
Some limitations should be considered for this study. There is no authoritative list of burn databases, so this study is limited by the authors’ discretion for databases chosen for this paper; however, common burn-specific databases with peer reviewed publications that include a range of clinical and socio-demographic data were included. Moreover, the main purpose of this study was to assess the extent of synchronicity among common burn databases and this aim is achieved with a representative sample of databases. Also this study only examined databases currently in use. Older versions of databases were not included in this study; however the databases chosen are representative of inconsistencies in data and multiple versions of the same database would likely only add to the lack of uniformity. The purpose of this study was to examine the extent of linkage and therefore only clinical and demographic data elements were used to assess this question. This study did not include outcome measures. Ultimately, there are many benefits to the burn community deciding on common outcome measures and this should be a part of any future efforts to create burn CDEs.
Conclusion
There are many discrepancies between burn databases both in terms of the relative presence of different data elements and use of different data values. In order to promote interoperability of database information for future clinical and research studies, the creation of CDEs for burns is important. Finally, we recommend the creation of a working group to develop CDEs in burn care. This responsibility should ideally rest with a consortium of stakeholders in the burn community.
Figure 1:
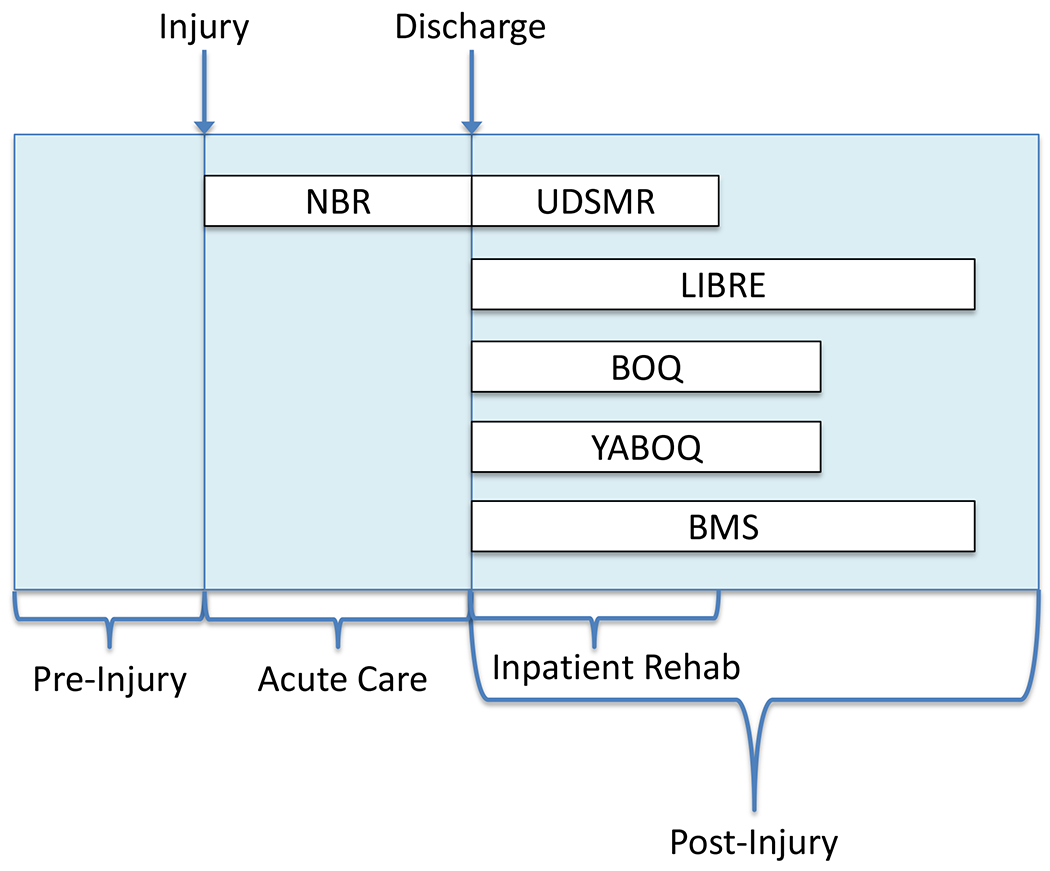
Data collection timeline by database
NBR: National Burn Repository
UDSMR: Uniform Data System for Medical Rehabilitation
LIBRE: Life Impact Burn Recovery Evaluation Profile
BOQ: Burn Outcome Questionnaires
YABOQ: Young Adult Burn Outcome Questionnaires
BMS: Burn Model System National Database
Acknowledgments
The contents of this manuscript were developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research, NIDILRR grants # 90DP0035 and #90DP0055. NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this manuscript do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should not assume endorsement by the Federal Government. This work was also supported in part by the Shriners Hospitals for Children #70011.
Appendix A:
Adult Burn Databases and Elements
| Variables | BMS | YABOQ | LIBRE | NBR | UDSMR | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Data Collection | Patient/Guardian Reported | Medical Abstraction | Patient/Guardian Reported | Medical Abstraction | Patient/Guardian Reported | Medical Abstraction | Patient/Guardian Reported | Medical Abstraction | Patient/Guardian Reported | Medical Abstraction |
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Inclusion Criteria | Age: All age groups TBSA: ≥ 10% TBSA (≥ 65YRS); ≥ 20% TBSA (≥19; ≤64); or, electrical related burns; or, critical area burns Language Requirements: None Location: Burn Model Systems Extra: Wound closure surgery |
Age: 19-30; Injury after 17th birthday TBSA: >20% TBSA; or, critical area burns Language Req.: Yes (English) Location: Receiving care at Fraser Outpatient Center (MGH) Extra: Able to provide informed consent and injury occurred within 3 years of consent. |
Age: ≥18 TBSA: ≥5% TBSA; or, critical area burns Language Req.: Yes (English) Location: Lives in US or Canada Extra: None |
Age: All age groups TBSA: None Language Req.: N/A Location: ABA verified burn centers Extra: Sustaining one or more skin injuries with diagnosis code(requiring care at burn treatment facility); And, hospital admission defined as burn/trauma; or, patient transfer via EMS from one hospital to another hospital; or, death due to burn injury. |
Age: All age groups TBSA: None Language Req.: N/A Location: Participating inpatient rehabilitation facility Extra: Etiologic diagnosis of burns (941-946.5) |
|||||
| Gender/Sex | Male or Female: 1.Male 2. Female For participants who are transgender, chosen gender is coded rather than biological gender. |
Male or Female: 1.Male 2.Female |
Male or Female: 1.Male 2.Female |
Male or Female: 1.Male 2.Female For participants who are transgender, chosen gender is coded rather than biological gender. |
Male or Female: 1.Male 2.Female |
|||||
| Age | Date of birth is prompted; Age calculation is based on recorded date of burn injury and recorded date of birth. |
Date of birth is prompted; Age calculation is based on recorded date of burn injury and recorded date of birth. | Year of birth is prompted. Age estimation is based on recorded year of burn injury and recorded date of birth. | Date of birth is prompted; if left blank, age is to be input with units: 1.<1 Day unit is hours 2.<1 month unit is days 3. <3 years unit is months 4. <90 years unit is years 5. > or = 90 years is one group Age calculation can be from recorded date of burn injury and recorded date of birth. |
Date of birth is prompted. Age calculation is based on recorded date of burn injury and recorded date of birth. | |||||
| Ethnicity/Race | Race: 1. Black or African-American 2. Asian 3. Caucasian 4. American Indian/Alaskan Native 5. Native Hawaiian or Other Pacific Islander 6. More than one race 7. Other [text field] Ethnicity: 1. Hispanic or Latino 2. Not Hispanic or Latino |
Race: 1. White, non-Hispanic 2. Black, non-Hispanic 3. Hispanic/Latino 4. Pacific Islander 5. Asian 6. Native American 7. Other |
Race: 1. White 2. Black or African American 3. Asian 4. American Indian or Alaskan Native 5. Native Hawaiian or Pacific Islander 6. Multiracial 7. Other 8. Prefer not to answer Ethnicity: 1. Hispanic or Latino 2. Not Hispanic or Latino |
Allowed to check two races. 1. Asian 2. Native Hawaiian or other Pacific Islander 3. Other race 4. American Indian or Alaskan Native 5. Black or African American 6. Caucasian Ethnicity: 1. Hispanic or Latino 2. Not Hispanic or Latino |
Race / Ethnicity: 1. American Indian or Alaskan Native 2. Asian 3. Black or African American 4. Hispanic or Latino 5. Native Hawaiian or other Pacific Islander 6. White |
|||||
| Accommodation | Living situation at time of and post- injury is prompted. 1. House 2. Apartment 3. Mobile home 4. Institution 5. Homeless 6. Other |
Not Prompted | Current residence is prompted. 1. House 2. Apartment 3. Mobile Home 4. Institution 5. Homeless 6. Unknown 7. Other |
Housing at time of injury is prompted. 1. House/apartment 2. School dormitory 3. Skilled nursing facility 4. Adult group home 5. Institution/ prison 6. Homeless |
Admission location is prompted. 1. Home 2. Board & care 3. Transitional living 4. Intermediate care (nursing home) 5. Skilled nursing facility (nursing home) 6. Acute unit of your own facility. 7. Acute unit of another facility 8. Chronic hospital 9. Rehabilitation facility 10. Other 11. Alternate level of care (ALC) unit 12. Sub-acute setting 13. Assisted living residence |
|||||
| Living With | Living with for pre-and post-hospital is prompted. 1. Alone 2. Spouse/partner/significant other 3. Friend 4. Parent or step-parent 5. Other relative (siblings, grandparents) 6. Others, not part of family 7. Guardian 8. Young children 9. Adult children 10. Don’t know |
Not Prompted | Not Prompted | Living situation at time of injury is prompted. 1. Alone 2. Spouse, partner, or significant other 3. Parents 4. Other family member 5. Other, not listed |
Pre-hospital living with situation is prompted if admission is from home. 1. Alone 2. Family/ relatives 3. Friends 4. Attendant 5. Other |
|||||
| Work Status | Prompted employment status at time of burn and post-burn. 1. Working 2. Not working; looking for work 3. Not working; not looking for work 4. Homemaker/ caregiver 5. Volunteer 6. Retired |
Current work status outside of home is prompted. 1. Part-time 2. Full-time 3. Not currently working |
Current work status is prompted. 1. Working 2. Not working 3. Homemaker/ caregiver 4. Volunteer 5. Retired |
Not Prompted | Pre-hospital vocational effort is prompted. 1. Full time 2. Part time 3. Adjusted workload |
|||||
| Occupation | Occupation is prompted as [text field]; categories are presented in annotations1. | Job title is prompted; [text field] | Not Prompted | Occupation fields listed below in annotation2; Patient is allowed to choose a secondary occupation. | Pre-hospital vocational category is prompted. 1. Employed 2. Sheltered 3. Student 4. Homemaker 5. Not working 6. Retired for age 7. Retired for disability |
|||||
| Marital Status | Marital status is prompted. 1. Married (living with common- law or with a partner) 2. Separated 3. Divorced 4. Widowed 5. Single (not married) |
Marital status is prompted. 1. Married/live with significant other 2. Divorced/ separated 3. Widowed 4. Single (never married) |
Marital status is prompted. 1. Married/live with significant other 2. Divorced/ separated 3. Widowed 4. Single, never married |
Marital status is prompted. 1. Single 2. Married 3. Domestic partnership 4. Separated 5. Divorced 6. Widowed |
Marital status is prompted. 1. Never married 2. Married 3. Widowed 4. Separated 5. Divorced |
|||||
| Disability Income | Disability insurance or private Long Term Disability Insurance is prompted. Choose all that apply: 1. I am not receiving disability income 2. Social security disability 3. Private long term insurance disability income 4. Supplemental Security Income (SSI) 5. Worker’s compensation 6. Other, [text field] |
Not Prompted | Not Prompted | Not Prompted | Not Prompted | |||||
| Insurance | Primary sponsor is prompted. 1. Medicare 2. Medicaid (DSHS) 3. Private insurance 4. Worker’s compensation (L&J) 5. HMO/PPO/Pre-paid/ Managed Care 6. Champus/ Tri-Care 7. Self-pay 8. Indigent (public support; charity care) 9. VA 10. Other 11. Philanthropy (private support or private foundation) 12. Not applicable (no burn care costs) |
Current health insurance coverage is prompted. 1. Private or group health insurance or a health plan that you , your employer, or someone else provides for you 2. Other, [text field] 3. I don’t have any health insurance coverage |
Not Prompted | Primary source of payment for hospital care is prompted. 1. Medicaid 2. Not billed (for any reason) 3. Self-pay/ uninsured 4. Private/ commercial insurance 5. No fault automobile 6. Medicare 7. Other government 8. Worker’s compensation 9. Charity 10. Pending or uncovered |
Primary and secondary insurance is prompted. 1. Blue Cross 2. Medicare non-MCO 3. Medicaid non-MCO 4. Commercial insurance 5. MCO HMO 6. Worker’s compensation 7. Crippled children’s services 8. Developmental disabilities services 9. State vocational rehabilitation 10. Private pay 11. Employee courtesy 12. Unreimbursed 13. Champus 14. Other 15. None 16. No fault auto insurance 17. Medicare MCO 18. Medicaid MCO |
|||||
| Alcohol Use | CAGE test for alcohol abuse is prompted at discharge and follow ups. 1. Yes 2. No 3. Declined to answer/refused |
Alcohol problem is prompted in review of systems. 1. Had it 2. Get treatment 3. Activities limited. |
Not Prompted | Use of alcohol by the patient at the time of injury is prompted. 1. No (not tested) 2. No (tested) 3. Yes (tested-below legal limit) 4. Yes (tested-above legal limit) 5. Yes (not tested-clinical assessment or patient report but not tested) |
Not Prompted | |||||
| Drug Use | CAGE test for alcohol abuse is prompted at discharge and follow ups. 1. Yes 2. No 3. Declined to answer/refused 4. Unknown |
Drug problem is prompted in review of systems. 1. Had it 2. Get treatment 3. Activities limited |
Not Prompted | Drug usage prior to burn injury is prompted. 1. Not tested 2. No drug use, tested 3. Yes, prescription drug-tested 4. Yes, illegal drug-tested 5. Not known/not recorded (If suspected but not proven) Drug(s) found in blood/urine is prompted. 1. Barbiturates 2. Cannabis 3. Dissociative agents 4. Opiates 5. Sedatives 6. Stimulants 7. Tricyclic antidepressants 8. Other drugs |
Not Prompted | |||||
| Injury Date | Date of burn injury is prompted at discharge. | Date and time of burn injury is prompted. | Injury month, year, and time (listed below) since the burn is prompted. 1. <3 Years 2. 3-10 Years 3. >10 Years |
Date and time of burn injury is prompted. | Burn injury date prompted as onset of impairment. | |||||
| Admission to Care Date | Date of admission to Burn Model System is prompted. If applicable, date of second admission to Burn Model System is prompted at discharge. |
Date and time of admission to burn unit is prompted. | Not Prompted. | Admission date and time to burn center is prompted. | Admission date is prompted; defined as the date that the patient begins receiving covered Medicare services in an inpatient rehabilitation facility. | |||||
| Etiology | Primary etiology is prompted. 1. Fire/flame 2. Scald 3. Contact with hot object 4. Grease 5. Tar 6. Chemical 7. Hydrofluoric acid 8. Electricity 9. Radiation 10. UV light 11. Other burn 12. Flash burn 13. Unknown |
Not Prompted | Not Prompted | Etiology of burn injury is prompted. 1. Scald* 2. Flame* 3. Contact* 4. Electrical* 5. Chemical / corrosion* 6. Flash* 7. Other* *Each category is broken down into specific subcategories. |
Prompted as etiologic diagnosis ICD 9 codes. | |||||
| Total Body Surface Area (TBSA) | Numeric | Numeric | Numeric | Numeric | Not Prompted | |||||
| Severity (Burn Thickness) | Not prompted | 3rd degree burn percent is prompted. | Not Prompted | Prompted 2nd degree is defined as: 1. Burn involving a portion of the dermis. 2. Burn that heals spontaneously and does not require grafting for closure ,and 3. Burn that did not develop granulation. 3rd degree is defined as: 1. Burn involving the entirety of the dermis. 2. Burn requiring closure by excision and grafting, or 3. Burn that developed granulation tissue. |
Not Prompted | |||||
| Anatomic Injury Location (Burn) | Location is broken into categories to answer: 1. Head/Face/ Neck: a. Yes b. No c. Unknown 2. Trunk (back, chest, abdomen): a. Yes b. No c. Unknown 3. Perineum (buttock, genitals): a. Yes b. No c. Unknown 4. Shoulder/ Upper Arm /Elbow: a. Right b. Left c. Bilateral d. None e. Unknown 5. Forearm (includes wrist): a. Right b. Left c. Bilateral d. None e. Unknown 6. Hand: a. Right b. Left c. Bilateral d. None e. Unknown 7. Leg: a. Right b. Left c. Bilateral d. None e. Unknown 8. Foot: a. Right d. Left c. Bilateral d. None e. Unknown |
Anatomic burn location is prompted. 1. Face involved a. No b. Yes 2. Hands involved a. No b. Yes 3. Genitals involved a. No b. Yes |
Anatomic burn location is prompted. 1. Back 2. Face 3. Head 4. Neck 5. Hands 6. Feet 7. Legs 8. Torso/Trunk 9. Genitals 10. Arms 11. Other; [text field] |
Anatomic burn location of 2nd and 3rd degree burn: 1. Head 2. Neck 3. Anterior and posterior trunk 4. Buttocks 5. Genitalia 6. Upper arm 7. Lower arm 8. Hand 9. Thigh 10. Leg 11. Foot |
Location can be identified through respective ICD-9 Codes. | |||||
| Inhalation Injury | Inhalation injury is prompted. 1. Yes 2. No 3. Unknown |
Inhalation injury is prompted. 1. No 2. Yes |
Not Prompted | Inhalation injury is prompted. 1. No 2. Yes; with cutaneous burn injury 3. Yes; without cutaneous burn injury |
Not Prompted | |||||
| Non-Burn Injury | Not Prompted | Not Prompted | Not Prompted | Non-burn injury prompted and non-burn related cutaneous injury are prompted. 1. Toxic epidermal necrolysis/Stevens-Johnson Syndrome 2. Purpura Fulminans 3. Necrotizing soft tissue infection 4. Soft tissue de-gloving 5. Friction burn/crush (i.e. road rash) |
Prompted as ICD 9 codes. | |||||
| Geographic Injury Location | Location of injury is prompted. 1. Patient’s home 2. Other private dwelling 3. Patient’s place of work 4. Other building or structure 5. Conveyance (automobile, plane, etc.) 6. Other 7. Missing/unknown |
Not Prompted | Not Prompted | Incident location is prompted. 1. Zip or postal code 2. Country 3. State 4. County 5. City |
Not Prompted | |||||
| Circumstance of Injury | Circumstance of injury is prompted at discharge. 1. Non-intentional employment related 2. Non-intentional non-work related 3. Non-intentional recreation 4. Non-intentional non-specified 5. Suspected assault-domestic 6. Suspected assault-nondomestic 7. Suspected self-inflicted/ suicide 8. Suspected arson 9. Unknown Circumstance of injury is prompted again at follow ups. 1. Non-intentional employment related 2. Non-intentional non-work related 3. Non-intentional recreation 4. Non-intentional non-specified 5. Don’t know |
Not Prompted | Not Prompted | Circumstance of injury is prompted. Form Type A: 1. Accidental injury: employment related 2. Accidental injury: non-employment 3. Accidental: recreation 4. Accidental: unknown circumstance 5. Suspected arson 6. Suspected assault/abuse 7. Suspected self-inflicted 8. Other Form Type B: 1. Yes,primary occupation 2. Yes, secondary occupation 3. Not work-related |
Not Prompted | |||||
| Total Body Surface Area Grafted | Numeric | Not Prompted | Not Prompted | Not Prompted | Not Prompted | |||||
| Disposition of Discharge | Alive at discharge is prompted. 1. Yes 2. No Disposition is prompted. 1. Died, burn related 2. AMA/unable to complete treatment 3. Discharged, patient home 4. Discharged, other home 5. Discharged, extended care facility 6. Discharged, other rehab (not model system) 7. Discharged, institution 8. Discharged, drug/alcohol treatment center 9. Discharged, shelter 10. Discharged, street 11. Died, non-burn related 12. Other 13. Unknown |
Not Prompted | Not Prompted | Disposition of discharge is prompted. 1. Discharged home (prior living situation or with family members) with no home services. 2. Discharged home with home services 3. Discharged/ transferred to skilled nursing facility (SNF)/nursing home 4. Discharged/transferred to long-term care facility (e.g. Ventilator weaning/ 5. custodial care) Discharged to foster care 6. Discharged to alternate caregiver. 7. Transferred as inpatient to another acute burn facility 8. Transferred as inpatient to another hospital (non-burn) 9. Transferred to inpatient psychiatry unit 10. Transferred to inpatient rehabilitation facility 11. Discharged to jail or prison 12. Discharged to street (patient without home) 13. Died in hospital 14. Transferred to hospice care 15. Left against medical advice or discontinued care |
Discharge to living setting is prompted. 1. Home 2. Board and care 3. Transitional living 4. Intermediate care 5. Skilled nursing facility 6. Acute unit of own facility 7. Acute unit of another facility 8. Chronic hospital 9. Rehabilitation facility 10. Other 11. Died 12. Alternate level of care unit 13. Sub acute setting 14. Assisted living residence |
|||||
| Length of Stay | Length of hospital stay is prompted (based on date of admission and date of discharge). | Length of hospital stay can be calculated from date of admission and discharge from hospital for acute burn injury. | Not Prompted | Length of hospital stay can be calculated from date of admission and date of discharge. | Length of inpatient rehabilitation facility stay can be calculated from date of admission and date of discharge. | |||||
| Total ICU Days | Not Prompted | Not Prompted | Not Prompted | Number of days in ICU level care is prompted; partial days rounded up. Requires nurse to patient ratio of 1:1 or 1:2 and a bed at the ICU level at the designated hospital. | Not Prompted | |||||
| Ventilator Days | Numeric | Numeric; excludes days in surgery. | Not Prompted | Measured in days with partial days rounding up. Includes positive pressure, mechanical assistance via an artificial airway. Excludes OR time and up to 4 hours post-op, non-invasive means of ventilary support, and patients with artificial airways without positive pressure assistance. Allows for multiple start and stop dates in the calculations. | Not Prompted | |||||
| Comorbid Conditions | Another major injury that requires hospitalization (besides burn injury): 1. Yes 2. No 3. Don’t know |
Conditions prior to burn injury are prompted. 1. Had it 2. Get treatment 3. Activities limited a. Asthma b. Attention deficit hyperactivity disorder (ADHD) c. Chronic allergies or sinus trouble d. Diabetes e. Epilepsy (seizure disorder) f. Hearing problem g. Heart problem h. Learning problem i. Sleep problem j. Speech problems k. Vision problems l. Depression m. Drug problem n. Alcohol problem o. Smoking habit p. Pregnancy q. Anemia r. High blood pressure s. Stomach problems (ulcer) t. Liver problems u. Kidney problems v. Other medical problem |
Not Prompted | Pre-existing co-morbid factors are prompted. 1. Other 2. Alcoholism 3. Arthritis 4. Ascites within 30 days 5. Bleeding disorder 6. Chemotherapy for cancer within 30 days 7. Congenital anomalies 8. Congestive heart failure 9. Current smoker 10. Currently requiring or on dialysis 11. CVA/residual neurological deficit 12. Diabetes Mellitus 13. Disseminated cancer 14. Do Not Resuscitate (DNR) status 15. Esophageal varices 16. Functionally dependent health status 17. History of angina within past 1 month 18. History of myocardial infarction within past 6 months 19. History of revascularization / amputation for PVD 20. Hypertension requiring medication 21. Prematurity 22. Obesity 23. Respiratory disease 24. Steroid use 25. Cirrhosis 26. Dementia 27. Major psychiatric illness 28. Drug dependence 29. Pre-hospital cardiac Arrest with resuscitative efforts by healthcare provider 30. Wheel chair dependent |
Prompted as ICD 9 codes; [text field] | |||||
Annotations
Current BMS provided Categories: Census Industrial and Occupational Classification Codes: Fields of Occupation in BMS: Executive, Administrative, and Managerial/ Professional Specialty/ Technicians and Related Support/Sales/ Administrative Support Including Clerical/ Private Household/ Farming, Forestry, and Fishing/ Precision Production, Craft, and Repair/ Machine Operators, Assemblers, and Inspectors/ Transportation and Material Moving / Handlers, Equipment Cleaners, Helpers, and Laborers/ Military Occupations
Fields of occupation in NBR: Business and Financial Operations Occupations/Architecture and Engineering Occupations/Community and Social Services Occupation/Education, Training, and Library Occupations/ Healthcare Practitioners and Technical Occupations/ Fire Fighter/Protective Service Operations (Non-Fire Fighter)/Building and Grounds Cleaning and Maintenance/Sales and Related Occupations/Farming, Fishing, and Forestry Occupations/Installation, Maintenance, and Repair Occupations/Transportations and Material Moving Occupations/Management Occupations/Computer and Mathematical Occupations/ Life, Physical, and Social Science Occupations/Legal Occupations/Arts, Design, Entertainment, Sports and Media/Healthcare support Occupations/Food Preparation and Serving Related/ Personal Care and Service Occupations/ Office and Administrative Support Occupations/Constructions and Extraction Occupations/Production Occupations/Military Specific Occupations/Homemaker/Student/Unemployed
Appendix B:
Pediatric Burn Databases and Elements
| Variables | BMS | BOQ (0-4; 5-18, 11-18 0-18 indicates all) |
NBR | UDSMR | ||||
|---|---|---|---|---|---|---|---|---|
| Data Collection | Patient/ Guardian Reported | Medical Abstraction | Patient/ Guardian Reported | Medical Abstraction | Patient/ Guardian Reported | Medical Abstraction | Patient / Guardian Reported | Medical Abstraction |
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Inclusion Criteria | Age: All age groups TBSA: ≥ 10% TBSA (≥ 65YRS); ≥ 20% TBSA (≥19; ≤64); or, electrical related burns; or, critical area burns Language Requirements: None Location: Burn Model Systems Extra: Wound closure surgery |
Age: 0-18 TBSA: ≥ 5% TBSA; or, critical area burns Language Req.: Yes (English, Spanish) Location: Shriners hospital for burn care Extra: None |
Age: All age groups TBSA: None Language Req.: N/A Location: ABA verified burn centers Extra: Sustaining one or more skin injuries with diagnosis code(requiring care at burn treatment facility); And, hospital admission defined as burn/trauma; or, patient transfer via EMS from one hospital to another hospital; or, death due to burn injury. |
Age: All age groups TBSA: None Language Req.: N/A Location: Participating inpatient rehabilitation facility Extra: Etiologic diagnosis of burns (941-946.5) |
||||
| Gender/Sex | Male or Female: 1. Male 2. Female For participants who are transgender, chosen gender is coded rather than biological gender. |
(0-18) Male or Female: 1. Male 2. Female |
Male or Female: 1. Male 2. Female For participants who are transgender, chosen gender is coded rather than biological gender. |
Male or Female: 1. Male 2. Female |
||||
| Age | Date of birth is prompted; Age calculation is based on recorded date of burn injury and recorded date of birth. |
(0-18) Date of birth is prompted; Age calculation is based on recorded date of burn injury and recorded date of birth. |
Date of birth is prompted; if left blank, age is to be input with units: 1.<1 Day unit is hours 2.<1 month unit is days 3. <3 years unit is months 4. <90 years unit is years 5. > or = 90 years is one group Age calculation can be from recorded date of burn injury and recorded date of birth. |
Date of birth is prompted; Age calculation is based on recorded date of burn injury and recorded date of birth. |
||||
| Ethnicity/ Race | Race: 1. Black or African-American 2. Asian 3. Caucasian 4. American Indian/Alaskan Native 5. Native Hawaiian or Other Pacific Islander 6. More than one race 7. Other [text field] Ethnicity: 1. Hispanic or Latino 2. Not Hispanic or Latino |
(0-18) Race Form A: 1. White; non-Hispanic 2. Black; non-Hispanic 3. Hispanic/Latino 4. Pacific Islander 5. Asian 6. Native American 7. Other, [text field] Race Form B: 1. Asian 2. Black 2. Not documented 4. Hispanic 5. Indian 6. Other 7. White |
Allowed to check two races. 1. Asian 2. Native Hawaiian or other Pacific Islander 3. Other race 4. American Indian or Alaskan Native 5. Black or African American 6. Caucasian Ethnicity 1. Hispanic or Latino 2. Not Hispanic or Latino |
Race / Ethnicity: American Indian or Alaska Native 1. Asian 2. Black or African American 3. Hispanic or Latino 4. Native Hawaiian or other Pacific Islander 5. White |
||||
| Accommodation | Living situation at time of injury and post-injury is prompted. 1. House 2. Apartment 3. Mobile home 4. Institution 5. Homeless 6. Other |
(0-18) Change before/after burn is prompted. 1. There is a change, and it is mostly due to the burn. 2. There is a change, and it is partly due to the burn. 3. There is a change, but it is not related to the burn. 4. No change in this child’s living situation. |
Housing at time of injury is prompted. 1. House / apartment 2. School dormitory 3. Skilled nursing facility 4. Adult group home 5. Institution / prison 6. Homeless |
Admission location is prompted. 1. Home 2. Board & care 3. Transitional living 4. Intermediate care (nursing home) 5. Skilled nursing facility (nursing home) 6. Acute unit of your own facility. 7. Acute unit of another facility 8. Chronic hospital 9. Rehabilitation facility 10. Other 11. Alternate level of care (ALC) unit 12. Sub-acute setting 13. Assisted living residence |
||||
| Living With | Living with for post-hospital is prompted. 1. Parent or step-parent 2. Other relative (siblings, grandparents) 3. Others, not part of family 4. Guardian Living with for pre- and post-hospital is prompted. 1. Alone 2. Spouse/partner/significant other 3. Friend 4. Parent or step-parent 5. Other relative (siblings, grandparents) 6. Others, not part of family 7. Guardian 8. Young children 9. Adult children 10. Declined to answer/refused |
(0-18) Living with for pre- and post-hospital is prompted. 1. Mother/stepmother 2. Father/stepfather 3. Grandparent (how many?) [text field] 4. Brother or sister (how many?) [text field] 5. Aunt or uncle (how many?) [text field] 6. Other[text field] |
Living situation at time of burn is prompted. 1. Alone 2. Spouse, partner, or significant other 3. Parents 4. Other family member 5. Other, not listed |
Pre-hospital living with situation is prompted if admission is from home. 1. Alone 2. Family/ relatives 3. Friends 4. Attendant 5. Other |
||||
| School Status | School status at follow up is prompted. 1. In school 2. Not in school 3. Declined to answer/refused 4. Missing/unknown Current school status is prompted. 1. In school a. Same program full time b. Same program part time c. New program full time d. New program part time e. Did not resume school f. Returned to individual program, home school g. Not in school h. Reason for not being in school is prompted. a. Burn related b. Other medical problems c. Emotional/social d. Legal/jail e. Substance abuse f. Personal choice g. Other h. Not applicable (going to school) School status at time of burn injury is prompted. 1. In school 2. Not in school 3. Declined to answer/refused Reason for not being in school at time of burn injury is prompted. 1. Medical problems 2. Emotional/social 3. Legal/jail 4. Substance abuse 5. Personal choice 6. Not applicable (working or going to school) 7. Declined to answer/refused |
(0-4) Not Prompted (5-18) Reason for not being in school is prompted. 1. Too young 2. Burn injury 3. Other [text field] (11-18) Reason for not being in school is prompted. 1. Burn injury 2. Other [text field] |
Not Prompted | Pre-hospital vocational status is prompted. 1. Employed 2. Sheltered 3. Student 4. Homemaker 5. Not working 6. Retired for age 7. Retired for disability Pre-hospital vocational effort is prompted. 1. Full time 2. Part time 3. Adjusted workload |
||||
| Highest Level of Education | Years of education completed is prompted. Form Type A: 1. 1 year or less 2. 2 years 3. 3 years 4. 4 years 5. 5 years 6. 6 years 7. 7 years 8. 8 years 9. 9 years 10. 10 years 11. 11 or 12 years; no diploma 12. High school diploma 13. Other Form Type B: 1. Preschool completed 2. 1 year or less 3. 2 years 4. 3 years 5. Not applicable (child is too young for school) |
(0-4) Not Prompted (5-18 & 11-18) Highest grade level is prompted. 1. Nursery 2. K 3. 1 4. 2 5. 3 6. 4 7. 5 8. 6 9. 7 10. 8 11. 9 12. 10 13. 11 14. 12 |
Not Prompted | Not Prompted | ||||
| Guardian(s) Occupation | Not Prompted | (0-18) Guardian’s work status is prompted. 1. No 2. Yes, occupation [text field] |
Not Prompted | Not Prompted | ||||
| Guardian(s) Highest Level of Education | Not Prompted | (0-18) Guardians’ highest level of education is prompted. 1. 8th Grade or less 2. Some high school 3. Graduated from high school 4. Technical school or Associates degree 5. Some college 6. Graduated from college 7. Graduate school or Professional degree |
Not Prompted | Not Prompted | ||||
| Disability Income | Disability insurance or Private Long Term Disability insurance is prompted. Choose all that apply: 1. My child is not receiving disability income 2. Social security disability 3. Private long term insurance disability income 4. Supplemental security income (SSI) 5. Worker’s compensation 6. Other Disability income due to burn injury is prompted. 1. Yes, my child is receiving disability income due to his/her burn injury 2. No, my child is not receiving disability income due to his/her burn injury |
(0-18) Not Prompted |
Not Prompted | Not Prompted | ||||
| Insurance | Primary sponsor is prompted. 1. Medicare 2. Medicaid (DSHS) 3. Private insurance 4. Worker’s compensation (L&J) 5. HMO/PPO/Pre-paid/Managed Care 6. Champus/Tri-Care 7. Self-pay 8. Indigent (public support; charity care) 9. VA 10. Other 11. Philanthropy 12. Not applicable (no burn care costs) |
(0-18) Not Prompted |
1. Medicaid 2. Not billed (for any reason) 3. Self-pay/ uninsured 4. Private/ commercial insurance 5. No fault automobile 6. Medicare 7. Other government 8. Workers compensation 9. Charity 10. Pending or uncovered |
Primary and secondary insurance is prompted. 1. Blue Cross 2. Medicare non-MCO 3. Medicaid non-MCO 4. Commercial insurance 5. MCO HMO 6. Worker’s compensation 7. Crippled children’s services 8. Developmental disabilities service 9. State vocational rehabilitation 10. Private pay 11. Employee courtesy 12. Unreimbursed 13. Champus 14. Other 15. None 16. No fault auto insurance 17. Medicare MCO 18. Medicaid MCO |
||||
| Injury Date | Date of burn injury is prompted at discharge. | (0-18) Date of burn injury is prompted. |
Date and time of burn injury is prompted. | Burn injury date prompted as onset of impairment. | ||||
| Admission to Care Date | Date of admission to Burn Model System is prompted. If applicable, date of second admission to burn model system is prompted at discharge. |
(0-18) Date of admission to Burn Unit is prompted. |
Admission date and time to burn center is prompted. | Admission date is prompted; defined as the date that the patient begins receiving covered Medicare services in an inpatient rehabilitation facility. | ||||
| Etiology | Primary etiology is prompted. 1. Fire/Flame 2. Scald 3. Contact with hot object 4. Grease 5. Tar 6. Chemical 7. Hydrofluoric acid 8. Electricity 9. Radiation 10. UV light 11. Other burn 12. Flash burn 13. Unknown |
(0-18) Etiology is prompted. 1. Chemical 2. Contact with hot object 3. Electrical 4. Fire/flame 5. Other burn 6. Other non-burn 7. Radiation 8. Scald 9. Skin disease 10. Unknown |
Etiology of burn injury is prompted. 1. Scald* 2. Flame* 3. Contact* 4. Electrical* 5. Chemical / corrosion* 6. Flash* 7. Other* *Each of these categories is broken down into more specific subcategories |
Prompted as etiologic diagnosis ICD 9 codes. | ||||
| Total Body Surface Area (TBSA) | Numeric | (0-18) Total admit TBSA and discharge TBSA are prompted (Numeric). |
Numeric | Not Prompted | ||||
| Severity (Burn Thickness) | Not Prompted | (0-18) 2nd degree and 3rd degree percentage is prompted for area of the body. 1. Head 2. Neck 3. Ant. trunk 4. Post. trunk 5. R. buttock 6. L. buttock 7. Genitalia 8. R.U. arm 9. L.U. arm 10. R.L. arm 11. L.L. arm 12. R. hand 13. L. hand 14. R. thigh 15. L. thigh 16. R. leg 17. R. foot 18. L. foot |
Prompted 2nd degree is defined as: 1. Burn involving a portion of the dermis. 2. Burn that heals spontaneously and does not require grafting for closure ,and 3. Burn that did not develop granulation. 3rd degree is defined as: 1. Burn involving the entirety of the dermis. 2. Burn requiring closure by excision and grafting, or 3. Burn that developed granulation tissue. |
Not Prompted | ||||
| Anatomic Injury Location (Burn) | Location is broken into categories to answer: 1. Head/Face/ Neck: a. Yes b. No c. Unknown 2. Trunk (back, chest, abdomen): a. Yes b. No c. Unknown 3. Perineum (buttock, genitals): a. Yes b. No c. Unknown 4. Shoulder/ Upper Arm /Elbow: a. Right b. Left c. Bilateral d. None e. Unknown 5. Forearm (includes wrist): a. Right b. Left c. Bilateral d. None e. Unknown 6. Hand: a. Right b. Left c. Bilateral d. None e. Unknown 7. Leg: a. Right b. Left c. Bilateral d. None e. Unknown 8. Foot: a. Right b. Left c. Bilateral d. None e. Unknown |
(0-18) Description of injury is prompted. 1. Head 2. Neck 3. Ant. trunk 4. Post. trunk 5. R. buttock 6. L. buttock 7. Genitalia 8. R.U. arm 9. L.U. arm 10. R.L. arm 11. L.L. arm 12. R. hand 13. L. hand 14. R. thigh 15. L. thigh 16. R. leg 17. L. leg 18. R. foot 19. L. foot |
Anatomic burn location of 2nd and 3rd degree burn: 1. Head 2. Neck 3. Anterior and posterior trunk 4. Buttocks 5. Genitalia 6. Upper arm 7. Lower arm 8. Hand 9. Thigh 10. Leg 11. Foot |
Location can be identified through respective ICD-9 Codes. | ||||
| Inhalation Injury | Inhalation injury is prompted. 1. Yes 2. No 3. Unknown |
(0-18) Inhalation injury is prompted. 1. Yes 2. No If yes, based on: 1. CO poisoning 2. Clinical findings 3. Fiber optic broach 4. History 5. Pulmonary functioning tests 6. Xenon scanning CaHGB level is also determined. |
Inhalation injury is prompted. 1. No 2. Yes; with cutaneous burn Injury 3. Yes; without cutaneous burn injury |
Not Prompted | ||||
| Non-Burn Injury | Not Prompted | (0-18) Non-burn injury is prompted; [text field] |
Non-burn injury and non-burn related cutaneous injury are prompted. 1. Toxic Epidermal Necrolysis/Stevens-Johnson Syndrome 2. Purpura Fulminans 3. Necrotizing Soft Tissue Infection 4. Soft Tissue De-gloving 5. Friction Burn/Crush (i.e. Road Rash) |
Prompted as ICD 9 codes. | ||||
| Geographic Injury Location | Location of injury is prompted. 1. Patient’s home 2. Other private dwelling 3. Patient’s place of work 4. Other building or structure 5. Conveyance (automobile, plane, etc.) 6. Other 7. Missing/unknown |
(0-18) Location of city, state, county/zip where injury occurred is also prompted. 1. Home 2. Farm 3. Mine and quarry 4. Industrial place and premises 5. Places for recreation/sport (outdoor) 6. Street and highway (road) 7. Public building (school) 8. Residential institution (jail) 9. Other specified places: [text field] 10. Unspecified places |
Incident location is prompted. 1. Zip or postal code 2. Country 3. State 4. County 5. City |
Not Prompted | ||||
| Circumstances of Injury | Circumstance of injury is prompted at discharge. 1. Non-intentional employment related 2. Non-intentional non-work related 3. Non-intentional recreation 4. Non-intentional non-specified 5. Suspected assault-domestic 6. Suspected self-inflicted/suicide 7. Suspected arson 8. Unknown Circumstance of injury is also prompted at follow ups. 1. Non-recreation 2. Recreation 3. Non-specified 4. Don’t know |
(0-18) Circumstance of injury is prompted. 1. Accident work related 2. Accident non work related 3. Accident recreation 4. Accident unspecified 5. Other 6. Suspect child abuse 7. Suspect self-inflicted 8. Suspect arson 9. Suspect assault / abuse (adult) Description of event is prompted as [text field]. |
Circumstance of injury is prompted. Form Type A: 1. Accidental injury: employment related 2. Accidental injury: non-employment 3. Accidental: recreation 4. Accidental: unknown circumstance 5. Suspected arson 6. Suspected assault/abuse 7. Suspected self-inflicted 8. Other Form Type B: 1. Yes, primary occupation 2. Yes, secondary occupation 3. Not work-related |
Not Prompted | ||||
| Total Body Surface Area Grafted | Numeric | (0-18) Not Prompted |
Not Prompted | Not Prompted | ||||
| Disposition of Discharge | Alive at discharge is prompted. 1. Yes 2. No Disposition is prompted. 1. Died, burn related 2. AMA/unable to complete treatment 3. Discharged, patient home 4. Discharged, other home 5. Discharged, extended care facility 6. Discharged, other rehab facility (not model system) 7. Discharged, institution 8. Discharged, drug/alcohol treatment center 9. Discharged, shelter 10. Discharged, street 11. Died, non-burn related 12. Other 13. Missing/unknown |
(0-18) Disposition of discharge is prompted. Form Type A: 1. Home 2. Skilled nursing facility 3. On-site housing 4. SHC Outpatient rehab/OTPT 5. Rehab off-site SHC housing 6. SHC exercise rehab program 7. Rehab off-site hotel 8. Wellness program 9. Ronald McDonald house 10. Other (specify): [text field] Form Type B: 1. Home 2. Not done/doc. 3. Rehab 4. Death 5. Died during treatment 6. Skilled nursing facility 7. Transfer to acute burn facility 8. Discharged against medical advice 9. Nursing home 10. Rehab center 11. Other |
Disposition of discharge is prompted. 1. Discharged home (prior living situation or with family members) with no home services. 2. Discharged home with home services 3. Discharged/ transferred to skilled nursing facility (SNF)/ Nursing home 4. Discharged/ transferred to long-term care facility (e.g. Ventilator weaning/ Custodial care) 5. Discharged to foster care 6. Discharged to alternate caregiver. 7. Transferred as inpatient to another acute burn facility 8. Transferred as inpatient to another hospital (non-burn) 9. Transferred to inpatient psychiatry unit 10. Transferred to inpatient rehabilitation facility 11. Discharged to jail or prison 12. Discharged to street (patient without home) 13. Died in hospital 14. Transferred to hospice care 15. Left against medical advice or discontinued care |
Discharge to living setting is prompted. 1. Home 2. Board and care 3. Transitional living 4. Intermediate care 5. Skilled nursing facility 6. Acute unit of own facility 7. Acute unit of another facility 8. Chronic hospital 9. Rehabilitation facility 10. Other 11. Died 12. Alternate level of care unit 13. Sub acute setting 14. Assisted living residence |
||||
| Length of Stay | Length of hospital stay is prompted (based on date of admission and date of discharge). | Length of stay in hospital can be calculated from date of admission and date of discharge. | Length of hospital stay can be calculated from date of admission and date of discharge. | Length of inpatient rehabilitation facility stay can be calculated from date of admission and date of discharge. | ||||
| Total ICU Days | Not Prompted | (0-18) Not Prompted |
Measured in days in ICU level care is prompted; partial days rounded up. Requires nurse to patient ratio of 1:1 or 1:2 and a bed at the ICU level at the designated hospital | Not Prompted. | ||||
| Ventilator Days | Numeric | (0-18) Ventilator support days are prompted; [text field] |
Measured in days with partial days rounding up. Includes positive pressure, mechanical assistance via an artificial airway. Excludes OR time and up to 4 hours post-op, non-invasive means of ventilary support, and patients with artificial airways without positive pressure assistance. Allows for multiple start and stop dates in the calculations. | Not Prompted | ||||
| Comorbid Conditions | Other health problems are prompted. 1. Yes [text field] 2. No Pre-burn physical problem is prompted. 1. Yes 2. No 3. Declined to answer/Refused 4. Unknown Pre-burn psychological issues (i.e. depression, anxiety): 1. Yes 2. No 3. Decline to answer/refused 4. Unknown |
(0-18) Conditions prior to burn injury are prompted. 1. Had it 2. Get treatment 3. Activities limited a. Asthma b. Attention or behavioral problems c. Chronic allergies of sinus Trouble d. Developmental delay e. Mental retardation f. Diabetes g. Epilepsy h. Hearing problem i. Heart problem j. Learning problem k. Sleep problem l. Speech problem m. Vision problem n. Depression o. Other chronic medical problem [text field] |
Pre-existing co-morbid factors are prompted. 1.Other 2. Alcoholism 3. Arthritis 4. Ascites within 30 days 5. Bleeding disorder 6. Chemotherapy for cancer within 30 days 7. Congenital anomalies 8. Congestive heart failure 9. Current smoker 10. Currently requiring or on dialysis 11. CVA/residual neurological deficit 12. Diabetes Mellitus 13. Disseminated cancer 14. Do Not Resuscitate (DNR) status 15. Esophageal varices 16. Functionally dependent health status 17. History of angina within past 1 month 18. History of myocardial infarction within past 6 months 19. History of revascularization / amputation for PVD 20. Hypertension requiring medication 21. Prematurity 22. Obesity 23. Respiratory disease 24. Steroid use 25. Cirrhosis 26. Dementia 27. Major psychiatric illness 28. Drug dependence 29. Pre-hospital cardiac arrest with resuscitative efforts by healthcare provider 30. Wheel chair dependent |
Prompted as ICD 9 codes; [Text field] | ||||
Footnotes
This manuscript was developed to fulfill the objectives of the Organization and Delivery of Burn Care Committee and the Rehabilitation Committee of the American Burn Association.
References
- 1.WHO. Burns Factsheet. http://www.who.int/mediacentre/factsheets/fs365/en/. Published 2016. Accessed November 23, 2016.
- 2.Ryan CM, Schoenfeld DA, Thorpe WP, Sheridan RL, Cassem EH, Tompkins RG. Objective Estimates of the Probability of Death from Burn Injuries. N Engl J Med. 1998;338(6):362–366. doi: 10.1056/NEJM199802053380604. [DOI] [PubMed] [Google Scholar]
- 3.Burn Incidence and Treatment in the United States: 2016. http://ameriburn.org/resources_factsheet.php. Published 2016. Accessed November 11, 2016.
- 4.NIH. Common Data Element (CDE) Resource Portal. https://www.nlm.nih.gov/cde/. Published 2016.
- 5.Lees KR, Bluhmki E, von Kummer R, et al. Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet. 2010;375(9727):1695–1703. doi: 10.1016/S0140-6736(10)60491-6. [DOI] [PubMed] [Google Scholar]
- 6.Galbraith S, Bowden J, Mander A. Accelerated longitudinal designs: An overview of modelling, power, costs and handling missing data. Stat Methods Med Res. 2014:0962280214547150-. doi: 10.1177/0962280214547150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burn Quality Improvement Program. http://www.ameriburn.org/16D-0615-PQ_MK-BQIP_Defs_Edited_May_2_June_15_2016.pdf. Published 2016. Accessed November 11, 2016.
- 8.ABA NBDS National Burn Data Standard: Data Dictionary. http://www.ameriburn.org/NBDS_Final_061615.pdf. Published 2015. Accessed November 11, 2016.
- 9.Standard Operating Procedures. http://burndata.washington.edu/standard-operating-procedures. Published 2016. Accessed November 11, 2016.
- 10.Kazis LE, Liang MH, Lee A, et al. The development, validation, and testing of a health outcomes burn questionnaire for infants and children 5 years of age and younger: American Burn Association/Shriners Hospitals for Children. J Burn Care Rehabil. 2002;23(3):196–207. http://www.ncbi.nlm.nih.gov/pubmed/12032370. [DOI] [PubMed] [Google Scholar]
- 11.Daltroy LH, Liang MH, Phillips CB, et al. American Burn Association/Shriners Hospitals for Children burn outcomes questionnaire: construction and psychometric properties. J Burn Care Rehabil. 2000;21(1 Pt 1):29–39. [DOI] [PubMed] [Google Scholar]
- 12.Meyer WJ, Lee AF, Kazis LE, et al. Adolescent survivors of burn injuries and their parents’ perceptions of recovery outcomes: do they agree or disagree? J Trauma Acute Care Surg. 2012;73(3 Suppl 2):S213–20. doi: 10.1097/TA.0b013e318265c843. [DOI] [PubMed] [Google Scholar]
- 13.Ryan CM, Schneider JC, Kazis LE, et al. Benchmarks for multidimensional recovery after burn injury in young adults: the development, validation, and testing of the American Burn Association/Shriners Hospitals for Children young adult burn outcome questionnaire. J Burn Care Res. 2008;34(3):e121–42. doi: 10.1097/BCR.0b013e31827e7ecf. [DOI] [PubMed] [Google Scholar]
- 14.Contact Us - LIBRE. http://sites.bu.edu/libre/contact-us-2/. Published 2016. Accessed November 11, 2016.
- 15.IRF-PAI. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/InpatientRehabFacPPS/IRFPAI.html. Published 2016. Accessed November 11, 2016.
- 16.Ryan CM, Cartwright S, Schneider JC, Tompkins RG, Kazis LE. The burn outcome questionnaires: Patient and family reported outcome metrics for children of all ages. Burns. 2016;42(5):1144–1145. doi: 10.1016/j.burns.2015.10.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Classification of Diseases, Functioning, and Disability. http://www.cdc.gov/nchs/icd/index.htm. Published 2016. Accessed November 11, 2016.
- 18.Jeng JC. By Fiat: an enlightened approach to The American Burn Association’s sensible quest for a universally accepted electronic Burn Diagram (Lund-Browder Diagram). J Burn Care Res. 2011;32(4):e157. doi: 10.1097/BCR.0b013e3182223f73. [DOI] [PubMed] [Google Scholar]
- 19.NINDS CDE - Spinal Cord Injury. https://www.commondataelements.ninds.nih.gov/SCI.aspx#tab=Data_Standards. Accessed November 11, 2016.
- 20.Maas AI, Harrison-Felix CL, Menon D, et al. Common data elements for traumatic brain injury: Recommendations from the interagency working group on demographics and clinical assessment. Arch Phys Med Rehabil. 2010;91(11):1641–1649. doi: 10.1016/j.apmr.2010.07.232. [DOI] [PubMed] [Google Scholar]


