Abstract
Background/Objectives
Telephone follow‐up calls could optimize the transition from the emergency department (ED) to home for older patients. However, the effects on hospital return rates are not clear. We investigated whether telephone follow‐up reduces unplanned hospitalizations and/or unplanned ED return visits within 30 days of ED discharge.
Design
Pragmatic randomized controlled trial with allocation by month; odd months intervention group, even months control group.
Setting
Two ED locations of a non‐academic teaching hospital in The Netherlands.
Participants
Community‐dwelling adults aged ≥70 years, discharged home from the ED were randomized to the intervention group (N = 4732) or control group (N = 5104).
Intervention
Intervention group patients: semi‐scripted telephone call from an ED nurse within 24 h after discharge to identify post‐discharge problems and review discharge instructions. Control group patients: scripted satisfaction survey telephone call.
Measurements
Primary outcome: total number of unplanned hospitalizations and/or ED return visits within 30 days of ED discharge. Secondary outcomes: separate numbers of unplanned hospitalizations and ED return visits. Subgroup analysis by age, sex, living condition, and degree of crowding in the ED at discharge.
Results
Overall, 42% were males, and median age was 78 years. In the intervention group, 1516 of 4732 patients (32%) consented, and in the control group 1659 of 5104 (33%) patients. Unplanned 30‐day hospitalization and/or ED return visit was found in 16% of intervention group patients and 14% of control group patients (odds ratio 1.16; 95% confidence interval: 0.96–1.42). Also, no statistically significant differences were found in secondary outcome measures. Within the subgroups, the intervention did not have beneficial effects for the intervention group.
Conclusion
Telephone follow‐up after ED discharge in older patients did not result in reduction of unplanned hospital admissions and/or ED return visits within 30 days. These results raise the question of whether other outcomes could be improved by post‐discharge ED telephone follow‐up.
Keywords: emergency department, geriatric, older patients, post‐discharge follow‐up, telephone
Key Points
Telephone follow‐up in older emergency department (ED) patients did not reduce unplanned hospital admissions and ED return visits 30 days after ED discharge.
Why Does this Paper Matter?
Telephone follow‐up is used for optimizing transitional care; however, it does not reduce unplanned hospital returns in older ED patients.
INTRODUCTION
The number of older patients visiting emergency departments (EDs) is increasing. 1 , 2 Studies following older patients after discharge from the ED have reported that 10–22% have an unplanned ED return visit within 1 month. 1 , 2 , 3 , 4 In addition, these patients appeared to be at increased risk of hospitalization, loss of functional independence, and death. 1 , 2 , 3 , 5 , 6 , 7
In general, ED return visits and hospital admissions are viewed as unfavorable and have been identified as a quality indicator of care. 3 , 8 , 9 , 10 Although unplanned ED return visits could be solely considered as an indicator of functional decline, 3 , 11 they may also be a result of inadequate care transitions from the ED to home. 1 , 2 , 12 , 13 The transition to home after ED discharge involves communication of complex information concerning the diagnosis, discharge instructions, medication use, and follow‐up care at a time when patients are easily distracted by anxiety, stress, or discomfort, causing difficulties in perceiving and processing this information. 12 , 14 , 15 This may be even more complicated when the ED is crowded and ED personnel experiences time pressure while delivering discharge information. 12 , 15 Older adults may have a higher risk of poor understanding of discharge instructions, because of cognitive and sensory impairments. 12 , 16 , 17
Telephone follow‐up has been identified as a practical and inexpensive method to offer transitional care in the post‐ED discharge period. 14 , 18 , 19 , 20 , 21 By repeating discharge information and providing additional care during a telephone follow‐up call, it is likely that this intervention could prevent ED return visits that are due to misunderstanding of information, anxiety, or lack of support. 12 , 22 , 23 , 24 Currently, an increasing number of hospitals have started to implement this service. 25 However, up to now only a few studies examined the feasibility and effectiveness of telephone follow‐up for older patients after discharge from the ED. 4 , 18 , 20 , 21 , 26 , 27 , 28 A recent systematic review on this topic could not demonstrate a benefit of the intervention, but only two high‐quality studies met eligibility criteria for this review. 4 , 21 , 27 Only one large randomized controlled trial (RCT) assessed the effect of telephone follow‐up for older patients on hospitalization and ED return visits within 30 days after ED discharge, reporting no benefit of the intervention. 4 However, the study investigated the effect on both planned and unplanned admissions and return visits. These could be considered opposite outcomes, as return to the hospital for a planned admission or ED visit implies discharge plan adherence, whereas unplanned hospital returns may result from failure to comply with discharge instructions or insufficient (transitional) care. Combining these opposite outcomes could obscure a beneficial effect of telephone follow‐up on unplanned hospital returns.
Therefore, the objective of this study was to examine the effects of a telephone follow‐up call for community‐dwelling patients aged 70 years and older after discharge from the ED on unplanned hospital admissions and/or ED return visits within 30 days.
We also explored whether the effects of telephone follow‐up were different for subgroups of patients at high risk for hospital return, including older age, 3 , 6 , 29 male sex, 3 , 6 , 30 and living alone, 1 , 2 , 31 , 32 and for patients who were discharged when the ED was busy.
METHODS
Study design
In this pragmatic RCT, patients aged 70 years and older were randomized according to the month of their ED visit; patients included in odd months received an intervention telephone call and patients included in even months received a satisfaction survey telephone call.
The Medical Ethics Review Committee of Haaglanden Medical Center (HMC) approved the study, which closely followed routine care (METC Zuidwest Holland, nr. 17‐028). The trial was conducted in adherence to the Consolidated Standards of Reporting Trials 33 and registered in the Netherlands Trial Register (Trial NL6598).
Participants
Patients were eligible if they were discharged from one of the EDs of HMC to an unassisted living environment during the trial period from February 1, 2018, to July 1, 2019.
The exclusion criteria were: hospital admission, discharge to nursing home or another care facility or assisted living environment, and planned follow‐up appointment at an outpatient clinic or ED within 24 h. A planned follow‐up appointment was an appointment after the index ED visit that could be foreseen at the time of ED discharge. 34
Of patients with more than one ED visit during the study period, only the first telephone call was included. If a patient had more than one ED return visit or hospital admission during the 30‐day follow‐up period, only the first unplanned ED return visit or hospital admission was counted.
Hospital admissions and ED return visits were defined as unplanned if they could not be foreseen at the time of discharge from the index ED visit. 34
Setting
The trial was performed in two EDs of HMC, a non‐academic, inner‐city teaching hospital in The Hague, The Netherlands. In 2018, location Westeinde received 53,000 patients of which 18% were 70 years or older and location Bronovo received 28,000 patients of which 25% were ≥70 years.
Procedures
Telephone follow‐up was integrated in the daily practice of the EDs. Every morning ED nurses received a list with hospital numbers and destinations of all patients aged 70 years and older who had been discharged from the ED during the previous 24 h.
Per patient, trained ED nurses made a maximum of three call attempts at different times of the day during quiet moments of their shift. The nurse explained the nature of the telephone call and asked for consent to participate. If the patient was not available or able to answer the phone, a spouse, family member, or caregiver received the explanation and the request to participate. Informed consent was noted in the case report form (CRF), integrated in the patient's electronic medical file. After indicating in the CRF whether it was an even or odd month, the questionnaire of the matching month opened (see Files S1 and S2).
The calling nurses were not blinded to the intervention.
Telephone follow‐up was not possible in case of a non‐existing telephone number, lack of a working telephone, missing notes in the electronic medical records (EMR), electronic hospital system (EHS) malfunctioning, and advanced impaired cognition, severe language barrier, and deafness in patients without an available spouse or caregiver. A patient was defined as having advanced impaired cognition if the diagnosis of dementia or impaired cognition was recorded in the patient's EMR, and the patient was not able to understand information or to have a structured conversation during the ED visit. If patients were not reached or not approached, the reason was indicated in the CRF.
To investigate the healthcare use of participants during the 30 days after ED discharge, we performed a second telephone call after 30 days between October 2018 and March 2019.
Intervention
Participants in the intervention group received a semi‐scripted telephone call from a trained ED nurse to identify post‐discharge problems and to offer additional information. ED nurses were taught how to adapt the conversation to the patient's health problem (File S1). Participants were asked to repeat the discharge instructions to explore whether more explanation was needed. Advice was given if the patient was not feeling well. When indicated, additional assistance was offered, for example, the pharmacy was called to deliver medication to the patient's home, or home care services were arranged. Participants who reported serious symptoms were advised to visit their general practitioner (GP) or to revisit the ED.
Participants in the control group received a scripted survey that assessed satisfaction with their ED visit (File S2). The five questions were derived from a validated patient satisfaction questionnaire (Picker Patient Experience Questionnaire [PPE‐15]). 35 Participants were not asked about their well‐being or about post‐discharge problems. Trained ED nurses performed the satisfaction survey calls, assisted by trained final year medical and nursing students between October 2018 and March 2019. The purpose of these calls was to control for any effect that a telephone call from the hospital might have. Only patients who turned out to be unwell during the satisfaction survey call or who had urgent medical questions received targeted medical advice.
Training and monitoring of telephone calls
Fifty‐seven ED nurses and nine medical and nursing students, who made the telephone calls, received study training. The script questions were explained and interviewers were taught how to interpret and score the patients' answers. In the presence of one researcher, the ED nurses and students performed a number of trial conversations (ranging from 3 to 15, depending on their performance) to familiarize them with the scripts, before they started to include patients. To ensure script adherence, one researcher regularly attended the telephone conversations, reviewed the CRFs, and provided feedback to the interviewers as needed.
Data collection
Demographic data, data related to the patients' ED visits, and data concerning ED return visits and hospitalizations within 30 days after ED discharge were abstracted from the EHS by an information technology specialist, who was not involved in the study, and organized by a researcher who was blinded to the study groups. For data abstraction, we adhered to the methods as described by Worster. 36
Outcomes
The primary outcome was the total number of unplanned hospital admissions and unplanned ED return visits within 30 days after ED discharge. If a patient was hospitalized via the ED after an ED return visit, only the hospital admission was counted for the primary outcome.
Secondary outcomes were the separate numbers of unplanned hospitalizations and unplanned ED return visits within 30 days. If a patient was hospitalized after an ED return visit, both the ED return visit and the hospital admission were counted for the secondary outcomes.
One researcher, who was blinded to the patients' study group, checked in the patients' EMR whether or not the hospital admissions and ED return visits were unplanned.
To investigate whether patients returned to other hospitals than HMC, the numbers of self‐reported ED return visits and hospital admissions to other hospitals were asked during the 30‐day follow‐up calls. To determine the validity of self‐reports, an agreement rate was calculated. The agreement rate was the proportion of subjects whose reported ED visit or hospitalization status was similar to that reported in the EHS.
While conducting the study, but before analysis, we further specified the primary outcome measure from both planned and unplanned hospital admissions to the combined outcome of unplanned hospital admissions and/or unplanned ED return visits. We believed that reducing only unplanned hospital returns would be beneficial, as these could be a result of nonadherence with discharge instructions, in contrast to planned returns. We have added unplanned ED return visits to the primary outcome, as we expected the intervention to mainly reduce ED return visits for patient‐related reasons, such as misunderstanding of discharge information, uncertainty, or lack of support, which did not always require hospitalization.
Subgroups of interest
Additionally, we examined the effects of the intervention in subgroups of patients at high risk for hospital return including age 3 , 6 , 29 (≥ or <median age of 78 years), sex, 3 , 6 , 30 and living condition (whether or not living alone). 1 , 2 , 31 , 32 Although the degree of ED crowding was not associated with increased unplanned hospital return in the literature, our experience is that it can negatively influence communication. In a busy ED, personnel experiences time pressure while delivering discharge information, and older patients could be more easily distracted. 12 , 15 Degree of crowding in the ED at discharge was measured with the National Emergency Department OverCrowding Scale (NEDOCS < or ≥ 60). The NEDOCS converts a data set into a score that correlates accurately with the degree of crowding as perceived by the staff working at that time. 37 If the NEDOCS is 60 or higher, the department is considered to be busy. 38
Sample size
The sample size was based on a pilot study of 544 patients, conducted in HMC, reporting a difference of 3% in all hospital admissions after 30 days between the intervention and the control group. We considered a 3% difference in unplanned hospital admissions and/or ED return visits between the groups of clinical relevance. With a power of 80% and a significance level of 0.05, we needed a sample size of 2049 patients per group to find a significant difference in unplanned hospital admissions and/or ED return visits within 30 days.
Analyses plan and statistical methods
Per‐protocol analysis of the data was performed. If patients in the control group received additional advice during the satisfaction survey call, it was noted in the CRF. These patients were not excluded from analysis, as they did receive the control intervention.
Statistical significance was tested using the Chi‐square tests, with a p‐value ≤0.05. Results were tabulated with the odds ratios (OR) calculated, including 95% confidence intervals (CI).
Data were analyzed using SPSS, version 26.
RESULTS
The trial ran from February 1, 2018, to July 1, 2019, when the study was stopped prematurely due to unforeseen closure of one of the ED locations.
During the study period, 9836 community‐dwelling patients aged 70 years and older were discharged home from the ED, 4732 in odd months, and 5104 in even months (Figure 1). Due to shortage of staff, trained ED nurses were not able to call 40% of eligible patients in the intervention group and 36% of patients in the control group (p < 0.001). In the intervention group, 32% could not be reached, compared with 31% in the control group (p = 0.42). In total, 3175 patients (1827 from location Westeinde and 1348 from location Bronovo) were included and allocated to the intervention (n = 1516) or the control (n = 1659) group as presented in the flowchart in Figure 1.
FIGURE 1.
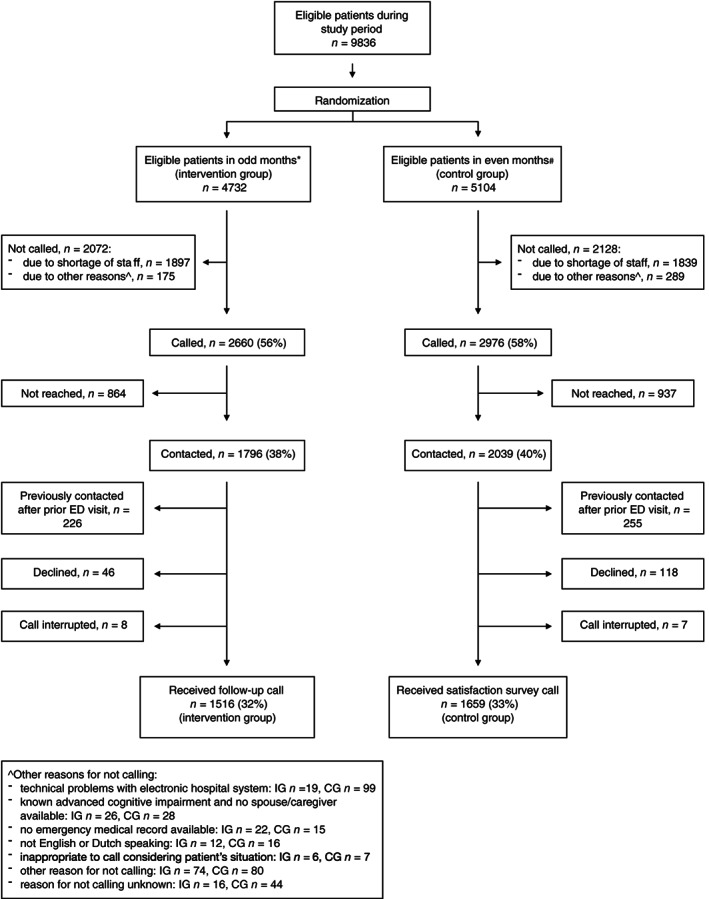
Flow diagram of enrollment and study groups. CG, control group; IG, intervention group; n, number. *Eight odd months during the study period; #9 even months during the study period
In both groups, the median age of the participants was 78 years and 42% were males. Other baseline characteristics were also well balanced between the study groups (Table 1). Baseline characteristics of the participants did not differ from those of patients who were not called (data not shown).
TABLE 1.
Baseline patient and clinical characteristics of patients in the intervention and control groups
| Intervention group | Control group | |
|---|---|---|
| (N = 1516) | (N = 1659) | |
| Age in years, median (IQR) | 78 (73–83) | 78 (73–83) |
| Male sex, % (n) | 42 (635) | 42 (694) |
| Living alone, % (n) a | 31 (475) | 30 (496) |
| Mode of referral, % (n) | ||
| Ambulance | 25 (382) | 26 (434) |
| General practitioner | 35 (527) | 33 (550) |
| Transport by ambulance, % (n) | 33 (500) | 33 (555) |
| Triage category urgent, % (n) b | 72 (1091) | 70 (1167) |
| ED visit at daytime, % (n) | 73 (1113) | 70 (1162) |
| Length of ED stay in minutes, median (IQR) | 151 (113–210) | 154 (108–209) |
| NEDOCS at discharge ≥60, c % (n) | 36 (540) | 30 (491) |
Abbreviations: ED, emergency department; IQR, interquartile range; NEDOCS, National Emergency Department OverCrowding Scale.
Living condition unknown in 327 intervention group patients and 367 control group patients.
Triage category urgent: red, orange, and yellow according to Manchester Triage System.
NEDOCS at discharge was missing in 5 intervention group patients and 175 control group patients due to technical malfunction of electronic hospital system on days that patients were discharged from the ED.
Of all 3175 patients, 239/1516 (16%) in the intervention group and 230/1659 (14%) in the control group had an unplanned hospital admission and/or unplanned ED return visit within 30 days after ED discharge (OR 1.16, 95% CI: 0.96–1.42) (Figure 2). Separate rates of unplanned hospital admissions and unplanned ED return visits were also not significantly different between the groups (Figures S1 and S2).
FIGURE 2.
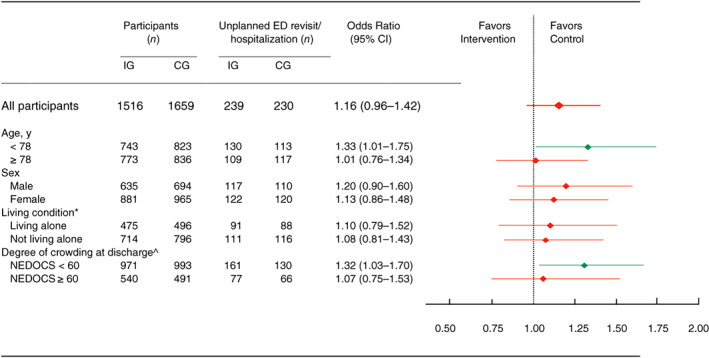
Risk of unplanned hospitalization and/or ED return visit within 30 days, depending on the study group. CG, control group; CI, confidence interval; ED, emergency department; IG, intervention group; NEDOCS, National Emergency Department OverCrowding Scale. *Living condition unknown in 327 intervention group patients and 367 control group patients. ^NEDOCS at discharge unknown in 5 intervention group patients and 175 control group patients
In both groups, more than half of the hospital admissions and almost all ED return visits were unplanned (Tables S1 and S2).
In subgroups according to sex and living condition, there was no effect of the telephone intervention on unplanned hospitalization and/or ED return visits (Figure 2). However, in the subgroup of patients aged <78 years, intervention group patients had more unplanned hospital admissions and/or ED return visits than control group patients (18% vs 14%; OR 1.33, 95% CI: 1.01–1.75). A similar effect was seen in the subgroup with NEDOCS < 60 at discharge (17% vs 13%; OR 1.32, 95% CI: 1.03–1.70).
In the control group, 77 of the 1659 patients (4.6%) received some form of advice or information in addition to the satisfaction survey. After excluding these patients from analysis, the results of the primary and secondary outcomes remained unchanged (data not shown).
None of the 304 patients who were called again after 30 days reported an unplanned hospital admission or ED return visit in another hospital than HMC. The agreement rate between self‐reported ED return visits and hospital admissions and EHS data was 96%.
DISCUSSION
This pragmatic RCT examined whether a telephone follow‐up call to older community‐dwelling adults within 24 h after discharge home from the ED reduced the number of unplanned hospital admissions and/or ED return visits within 30 days compared with a satisfaction survey telephone call. No difference was found between groups.
In addition, no reduction of unplanned hospital admissions and/or ED return visits was found in any of the subgroups.
These results are in line with the findings of our recent systematic review, examining the effects of telephone follow‐up on health‐related outcomes in older ED patients, which found no demonstrable effects on health services utilization, and understanding of and compliance with discharge instructions. 27 The results are also in line with the RCT of Biese et al., reporting no effect of a telephone follow‐up call for older patients on hospitalization or ED return visits after discharge.
In Biese's trial, patients with cognitive impairment or psychiatric diagnoses were excluded, despite that these patients are at high risk of hospital return. Moreover, the effect of telephone follow‐up on unplanned hospital admissions and ED return visits was not investigated. 4 Although these limitations were overcome in our current trial, the results were similar.
The limited telephone accessibility of patients was a limitation of Biese's trial that we could not overcome. Our success rates of reaching eligible patients were in line with other studies. 4 , 14 , 39
In our study, trained ED nurses were not able to call 36% of the eligible patients in the intervention group due to shortage of staff. In the control group more patients were called, as trained students were available during 3 even months of the study period to conduct satisfaction survey calls. Although some studies reported no time restrictions, others, especially studies that had not appointed a dedicated nurse to make the telephone calls, mentioned comparable problems. 40
Although we found no effect of telephone follow‐up in the total group of patients, subgroup analysis revealed that in patients aged <78 years and those who left the ED when the NEDOCS was below 60, intervention group patients returned more often to the ED within 30 days than control group patients. Although this effect is reported in previous studies, 41 these results ask for further investigation, as our subgroup analysis was not powered to detect differences between subgroups.
Although a beneficial effect on hospital returns was not found, there are data suggesting that telephone follow‐up improves patient satisfaction, 20 and feelings of loneliness and depressive symptoms in older patients at risk, who were discharged from the ED. 42 This could be examined in future research.
In a short review, Nasser et al. reported that telephone follow‐up could identify non‐compliance with discharge instructions in older ED patients, 28 which may provide insight into which patients may need extra support.
Strengths and weaknesses
To our knowledge, this is the largest study investigating the effects of telephone follow‐up in older adults after discharge from the ED. Moreover, this is the first study that focused on the effect of telephone follow‐up on unplanned hospital admissions and unplanned ED return visits and explored the effects in subgroups of patients at high risk for hospital return. Patients were included all year round and the telephone calls were integrated in the daily routine of the ED nurses.
In this pragmatic RCT, participants were randomized according to the month of their ED visit. Because telephone follow‐up was integrated into the daily practice of our EDs and multiple nurses were conducting the telephone calls at the same time, it was not feasible to allocate participants randomly to the study groups. However, baseline characteristics of the study groups were found to be similar. More importantly, outcome measures were abstracted from the EHS by researchers who were blinded to the study groups.
We had no data on hospital admissions and ED visits in other hospitals. However, based on the interviews after 30 days with 304 study patients, we found that none of them had an unplanned hospital admission or ED visit in any hospital other than HMC. Moreover, the agreement rate between self‐reported hospital returns and EHS data was high.
It could be seen as a methodological limitation that we changed the primary outcome measure during the study from all hospital admissions to unplanned hospital admissions and/or ED return visits. However, we think that focusing on unplanned hospital admissions and/or ED return visits is a strength, as we believed that reducing only unplanned hospital returns would be beneficial.
Due to the closure of one of the study sites, we were able to reach only 77% of the calculated sample size. With the current sample size, we would have been able to find a statistically significant difference of 4% in unplanned hospital admissions and/or ED return visits between the study groups. However, based on the results that tend to show an adverse effect of the intervention, it is unlikely that we would have shown a 3% benefit of the intervention with the full sample size.
During the patients' index ED visits, we were not able to collect more health determinants that could have identified individuals at high risk of hospital return and potentially poor‐quality transitions. 43 , 44 These include comorbid health conditions, medication burden, cognitive and physical functioning, health literacy, and living circumstances. Patients at risk and their caregivers may have high needs for social support and additional explanations and care, which could be addressed with telephone follow‐up. Evaluating the effects of a telephone intervention in these subgroups in future research is important.
Telephone follow‐up and communication of discharge information in the ED can be regarded as socially complex interventions that could be influenced by patient and contextual factors, but also by confounders at the level of the healthcare providers. 41 , 45 , 46 Training ED physicians and nurses in geriatric competencies, including communication skills and shared decision‐making, could enhance a potential beneficial effect of telephone follow‐up.
CONCLUSION
This study did not find a beneficial effect of a telephone follow‐up call on reducing unplanned hospital admissions and/or ED return visits. Based on the results of this large study, a previous RCT, and a systematic review, we advise not to introduce telephone follow‐up to reduce unplanned hospital admissions and ED return visits in older patients. 4 , 21 , 27 Future studies could evaluate the effects of this intervention on other health‐related outcomes.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.
AUTHOR CONTRIBUTIONS
Merel van Loon‐van Gaalen and M. Christien van der Linden devised the study design, which was further developed with advice from Jacobijn Gussekloo and Roos C. van der Mast. Merel van Loon‐van Gaalen supervised the data collection. Merel van Loon‐van Gaalen and M. Christien van der Linden managed the data, including quality control. Merel van Loon‐van Gaalen analyzed and interpreted the data and M. Christien van der Linden, Jacobijn Gussekloo, and Roos C. van der Mast provided statistical advice. Merel van Loon‐van Gaalen drafted the manuscript. All authors have contributed to the manuscript and all authors read and approved the final version of the manuscript. Merel van Loon‐van Gaalen takes responsibility for the article as a whole.
SPONSOR'S ROLE
The Jacobus Foundation in The Hague, The Netherlands, funded this study. The Jacobus Foundation supports education and research projects with a focus on Neurology and Psychiatry. The sponsor had neither a role in the design and conduct of the study, nor in the data collection, analysis and interpretation of the data, and preparation of the manuscript.
Supporting information
Figure S1 Risk of unplanned hospitalization within 30 days depending on the study group.
Figure S2. Risk of unplanned ED return visit within 30 days depending on the study group.
Table S1. Number of unplanned and planned hospital admissions depending on the study group
Table S2. Number of unplanned and planned ED return visits depending on the study group.
File S1. Translation of the telephone follow‐up questionnaire in the emergency medical records of emergency department patients aged ≥70 years.
File S2. Translation of the satisfaction survey questionnaire in the emergency medical records of emergency department patients aged ≥70 years.
ACKNOWLEDGMENTS
This study was funded by the Jacobus Foundation, The Hague, The Netherlands. We would like to thank Fabio Bruna, IT‐specialist at HMC, for composing the research database and Laura Bakker, emergency physician at HMC, for her help with the data collection.
van Loon‐van Gaalen M, van der Linden MC, Gussekloo J, van der Mast RC. Telephone follow‐up to reduce unplanned hospital returns for older emergency department patients: A randomized trial. J Am Geriatr Soc. 2021;69(11):3157–3166. 10.1111/jgs.17336
Funding information Jacobus Foundation
REFERENCES
- 1. Aminzadeh F, Dalziel WB. Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med. 2002;39:238‐247. [DOI] [PubMed] [Google Scholar]
- 2. Arendts G, Fitzhardinge S, Pronk K, Hutton M, Nagree Y, Donaldson M. Derivation of a nomogram to estimate probability of revisit in at‐risk older adults discharged from the emergency department. Intern Emerg Med. 2013;8:249‐254. [DOI] [PubMed] [Google Scholar]
- 3. de Gelder J, Lucke JA, de Groot B, et al. Predictors and outcomes of revisits in older adults discharged from the emergency department. J Am Geriatr Soc. 2018;66:735‐741. [DOI] [PubMed] [Google Scholar]
- 4. Biese KJ, Busby‐Whitehead J, Cai J, et al. Telephone follow‐up for older adults discharged to home from the emergency department: a pragmatic randomized controlled trial. J Am Geriatr Soc. 2018;66:452‐458. [DOI] [PubMed] [Google Scholar]
- 5. Caplan GA, Brown A, Croker WD, Doolan J. Risk of admission within 4 weeks of discharge of elderly patients from the emergency department—the DEED study. Discharge of elderly from emergency department. Age Ageing. 1998;27:697‐702. [DOI] [PubMed] [Google Scholar]
- 6. Lowthian J, Straney LD, Brand CA, et al. Unplanned early return to the emergency department by older patients: the Safe Elderly Emergency Department Discharge (SEED) project. Age Ageing. 2016;45:255‐261. [DOI] [PubMed] [Google Scholar]
- 7. McCusker J, Roberge D, Vadeboncoeur A, Verdon J. Safety of discharge of seniors from the emergency department to the community. Healthc Q. 2009;12:24‐32. [DOI] [PubMed] [Google Scholar]
- 8. Hughes G. A&E quality indicators. Emerg Med J. 2012;29:90. [DOI] [PubMed] [Google Scholar]
- 9. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee‐for‐service program. N Engl J Med. 2009;360:1418‐1428. [DOI] [PubMed] [Google Scholar]
- 10. Trivedy CR, Cooke MW. Unscheduled return visits (URV) in adults to the emergency department (ED): a rapid evidence assessment policy review. Emerg Med J. 2015;32:324‐329. [DOI] [PubMed] [Google Scholar]
- 11. Driesen B, Merten H, Wagner C, Bonjer HJ, Nanayakkara PWB. Unplanned return presentations of older patients to the emergency department: a root cause analysis. BMC Geriatr. 2020;20:365. 10.1186/s12877-020-01770-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hastings SN, Barrett A, Weinberger M, et al. Older patients' understanding of emergency department discharge information and its relationship with adverse outcomes. J Patient Saf. 2011;7:19‐25. [DOI] [PubMed] [Google Scholar]
- 13. Engel KG, Buckley BA, Forth VE, et al. Patient understanding of emergency department discharge instructions: where are knowledge deficits greatest? Acad Emerg Med. 2012;19:e1035‐e1044. [DOI] [PubMed] [Google Scholar]
- 14. Zavala S, Shaffer C. Do patients understand discharge instructions? J Emerg Nurs. 2011;37:138‐140. [DOI] [PubMed] [Google Scholar]
- 15. Engel KG, Heisler M, Smith DM, Robinson CH, Forman JH, Ubel PA. Patient comprehension of emergency department care and instructions: are patients aware of when they do not understand? Ann Emerg Med. 2009;53:454‐461. [DOI] [PubMed] [Google Scholar]
- 16. Bartlett G, Blais R, Tamblyn R, Clermont RJ, MacGibbon B. Impact of patient communication problems on the risk of preventable adverse events in acute care settings. CMAJ. 2008;178:1555‐1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Han JH, Bryce SN, Ely EW, et al. The effect of cognitive impairment on the accuracy of the presenting complaint and discharge instruction comprehension in older emergency department patients. Ann Emerg Med. 2011;57:662‐671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Jones JS, Young MS, LaFleur RA, Brown MD. Effectiveness of an organized follow‐up system for elder patients released from the emergency department. Acad Emerg Med. 1997;4:1147‐1152. [DOI] [PubMed] [Google Scholar]
- 19. Racine AD, Alderman EM, Avner JR. Effect of telephone calls from primary care practices on follow‐up visits after pediatric emergency department visits: evidence from the Pediatric Emergency Department Links to Primary Care (PEDLPC) randomized controlled trial. Arch Pediatr Adolesc Med. 2009;163:505‐511. [DOI] [PubMed] [Google Scholar]
- 20. Poncia HDM, Ryan J, Carver M. Next day telephone follow up of the elderly: a needs assessment and critical incident monitoring tool for the accident and emergency department. J Accid Emerg Med. 2000;17:337‐340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Biese K, Lamantia M, Shofer F, et al. A randomized trial exploring the effect of a telephone call follow‐up on care plan compliance among older adults discharged home from the emergency department. Acad Emerg Med. 2014;21:188‐195. [DOI] [PubMed] [Google Scholar]
- 22. Wu CL, Wang FT, Chiang YC, et al. Unplanned emergency department revisits within 72 hours to a secondary teaching referral hospital in Taiwan. J Emerg Med. 2010;38:512‐517. [DOI] [PubMed] [Google Scholar]
- 23. Šteinmiller J, Routasalo P, Suominen T. Older people in the emergency department: a literature review. Int J Older People Nurs. 2015;10:284‐305. [DOI] [PubMed] [Google Scholar]
- 24. Sheikh S. Risk factors associated with emergency department recidivism in the older adult. West J Emerg Med. 2019;20:931‐938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. American College of Emergency Physicians; American Geriatrics Society; Emergency Nurses Association; Society for Academic Emergency Medicine; Geriatric Emergency Department Guidelines Task Force . Geriatric emergency department guidelines. Ann Emerg Med. 2014;63:e7‐e25. [DOI] [PubMed] [Google Scholar]
- 26. Morse L, Xiong L, Ramirez‐Zohfeld V, Dresden S, Lindquist LA. Tele‐follow‐up of older adult patients from the Geriatric Emergency Department Innovation (GEDI) program. Geriatrics. 2019;4:18. 10.3390/geriatrics4010018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. van Loon‐van Gaalen M, van Winsen B, van der Linden MC, Gussekloo J, van der Mast RC. The effect of a telephone follow‐up call for older patients, discharged home from the emergency department on health‐related outcomes: a systematic review of controlled studies. Int J Emerg Med. 2021;14:13. 10.1186/s12245-021-00336-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Nasser L, Stratton T. BET 1: follow‐up phone calls and compliance with discharge instructions in elderly patients discharged from the emergency department. Emerg Med J. 2019;36:126‐127. [DOI] [PubMed] [Google Scholar]
- 29. LaMantia MA, Platts‐Mills TF, Biese K, et al. Predicting hospital admission and returns to the emergency department for elderly patients. Acad Emerg Med. 2010;17:252‐259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Graf CE, Giannelli SV, Herrmann FR, et al. Identification of older patients at risk of unplanned readmission after discharge from the emergency department – comparison of two screening tools. Swiss Med Wkly. 2012;141:w13327. [DOI] [PubMed] [Google Scholar]
- 31. McCusker J, Cardin S, Bellavance F, Belzile E. Return to the emergency department among elders: patterns and predictors. Acad Emerg Med. 2000;7:249‐259. [DOI] [PubMed] [Google Scholar]
- 32. McCusker J, Healey E, Bellavance F, Connolly B. Predictors of repeat emergency department visits by elders. Acad Emerg Med. 1997;4:581‐588. [DOI] [PubMed] [Google Scholar]
- 33. Schulz KF, Altman DG, Moher D, CONSORT Group . CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. PLoS Med. 2010;7:e1000251. 10.1371/journal.pmed.1000251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Landrum L, Weinrich S. Readmission data for outcomes measurement: identifying and strengthening the empirical base. Qual Manag Health Care. 2006;15:83‐95. [DOI] [PubMed] [Google Scholar]
- 35. de Vos MS, Hamming JF, Boosman H, Marang‐van de Mheen PJ. The association between complications, incidents, and patient experience: retrospective linkage of routine patient experience surveys and safety data. J Patient Saf. 2021;17:e91‐e97. [DOI] [PubMed] [Google Scholar]
- 36. Worster A, Haines T. Advanced statistics: understanding medical record review (MRR) studies. Acad Emerg Med. 2004;11:187‐192. [PubMed] [Google Scholar]
- 37. Van Der Linden MC, Van Loon M, Gaakeer MI, Richards JR, Derlet RW, Van Der Linden N. A different crowd, a different crowding level? The predefined thresholds of crowding scales may not be optimal for all emergency departments. Int Emerg Nurs. 2018;41:25‐30. [DOI] [PubMed] [Google Scholar]
- 38. Weiss SJ, Derlet R, Arndahl J, et al. Estimating the degree of emergency department overcrowding in academic medical centers: results of the National ED Overcrowding Study (NEDOCS). Acad Emerg Med. 2004;11:38‐50. [DOI] [PubMed] [Google Scholar]
- 39. Cochran VY, Blair B, Wissinger L, Nuss TD. Lessons learned from implementation of postdischarge telephone calls at Baylor Health Care System. J Nurs Adm. 2012;42:40‐46. [DOI] [PubMed] [Google Scholar]
- 40. Bahr SJ, Solverson S, Schlidt A, Hack D, Smith JL, Ryan P. Integrated literature review of postdischarge telephone calls. West J Nurs Res. 2014;36:84‐104. [DOI] [PubMed] [Google Scholar]
- 41. Crede SH, O'Keeffe C, Mason S, et al. What is the evidence for the management of patients along the pathway from the emergency department to acute admission to reduce unplanned attendance and admission? An evidence synthesis. BMC Health Serv Res. 2017;17:355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lowthian JA, Lennox A, Curtis A, et al. HOspitals and patients WoRking in Unity (HOW R U?): telephone peer support to improve older patients' quality of life after emergency department discharge in Melbourne, Australia—a multicentre prospective feasibility study. BMJ Open. 2018;8:e020321. 10.1136/bmjopen-2017-020321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hwang U, Hastings SN, Ramos K. Improving emergency department discharge care with telephone follow‐up. Does it connect? J Am Geriatr Soc. 2018;66:436‐438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Carpenter CR, Shelton E, Fowler S, et al. Risk factors and screening instruments to predict adverse outcomes for undifferentiated older emergency department patients: a systematic review and meta‐analysis. Acad Emerg Med. 2015;22:1‐21. [DOI] [PubMed] [Google Scholar]
- 45. Nielsen LM, Gregersen Østergaard L, Maribo T, Kirkegaard H, Petersen KS. Returning to everyday life after discharge from a short‐stay unit at the emergency department—a qualitative study of elderly patients' experiences. Int J Qual Stud Health Well‐being. 2019;14:1563428. 10.1080/17482631.2018.1563428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Carpenter CR, Malone ML. Avoiding therapeutic nihilism from complex geriatric intervention “negative” trials: STRIDE lessons. J Am Geriatr Soc. 2020;68:2752‐2756. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 Risk of unplanned hospitalization within 30 days depending on the study group.
Figure S2. Risk of unplanned ED return visit within 30 days depending on the study group.
Table S1. Number of unplanned and planned hospital admissions depending on the study group
Table S2. Number of unplanned and planned ED return visits depending on the study group.
File S1. Translation of the telephone follow‐up questionnaire in the emergency medical records of emergency department patients aged ≥70 years.
File S2. Translation of the satisfaction survey questionnaire in the emergency medical records of emergency department patients aged ≥70 years.


