Abstract
Objectives
Determine prevalence of increased signal intensity of the lateral collateral ligament (LCL) of the knee on MRI and decreased echogenicity on ultrasound, and compare with cadaveric histologic evaluation.
Methods
After IRB approval of this prospective study with informed consent, patients having knee MRI were additionally evaluated with ultrasound. Signal intensities of LCL on MRI (low, intermediate, high), echogenicity at ultrasound (hyperechoic, hypoechoic, anechoic), and extent of findings were assessed. Descriptive statistics, Wilcoxon signed ranked test, and intraclass correlation coefficient (ICC) were calculated. Two cadaveric knees were imaged with MRI and ultrasound, including histologic LCL evaluation.
Results
Seventy‐three subjects were included (39 males, 34 females; mean age 48 ± 14 years) with 77 knee examinations. On MRI, low, intermediate, and high signals were present in 21% (16/77), 75% (58/77), and 4% (3/77), respectively. On ultrasound, echogenicity was assessed as hyperechoic, hypoechoic, and anechoic in 62% (48/77), 38% (29/77), and 0% (0/77), respectively. Mean length of increased signal was 8.6 mm (±4.9) on MRI, and 6.5 mm (±4.8) on ultrasound. The ICC showed a good to excellent intermodality reliability (0.735–0.899) without statistically significant difference for interreader measurements (P = .163–.795). Histology evaluation showed transition of ligament fibers to fibrocartilage at its insertion with increased connective tissue mucin corresponding to MRI and ultrasound findings.
Conclusions
Increased signal intensity of the proximal LCL on ultrasound and MRI is common and corresponds to normal connective tissue mucin.
Keywords: diagnostic imaging, knee, ligaments, magnetic resonance imaging, ultrasonography
Abbreviations
- ICC
intraclass correlation coefficient
- LCL
lateral collateral ligament
- MR
magnetic resonance
The lateral (or fibular) collateral ligament of the knee is the primary stabilizer to varus instability of the knee. 1 , 2 Anatomically, it extends from the lateral femoral epicondyle to the fibular head. 3 , 4 It is considered as part of the posterolateral corner complex. 3 , 5 A complete tear or avulsion of the lateral collateral ligament is the most significant predictor at magnetic resonance (MR) imaging of posterolateral corner instability. 6
On imaging a normal lateral collateral ligament, shows low signal intensity on MR and appears hyperechoic and fibrillar on ultrasound. 7 , 8 Changes in appearances on both imaging modalities might be attributed to true pathologies or artifacts, i.e., partial volume effect, magic angle, or anisotropy. 7 , 8 , 9 However, an MR study with histologic correlation has shown that signal abnormalities at the proximal attachment site of the lateral collateral ligament are a common and normal finding. 7 Comparable findings using ultrasound have not been described.
In our clinical practice, we observed decreased echogenicity at the proximal attachment site of the lateral collateral ligament on ultrasound without referable symptoms. Thus, our purpose was to determine the prevalence of decreased echogenicity on ultrasound and increased signal intensity on MR imaging involving the proximal lateral collateral ligament of the knee, correlating with cadaveric histologic evaluation.
Materials and Methods
Inclusion and Exclusion Criteria
Institutional Review Board approval was obtained to prospectively evaluate consecutive patients referred for routine knee MR examinations additionally with ultrasound on the same day. All subjects were included after obtaining their written informed consent. Patients were included between March 2018 and August 2019. Exclusion criteria included patients under the age of 21 years, history of knee trauma, lateral knee symptoms, knee arthroplasty, and non‐routine MR examinations of the knee, e.g. tumor protocol (Figure 1).
Figure 1.
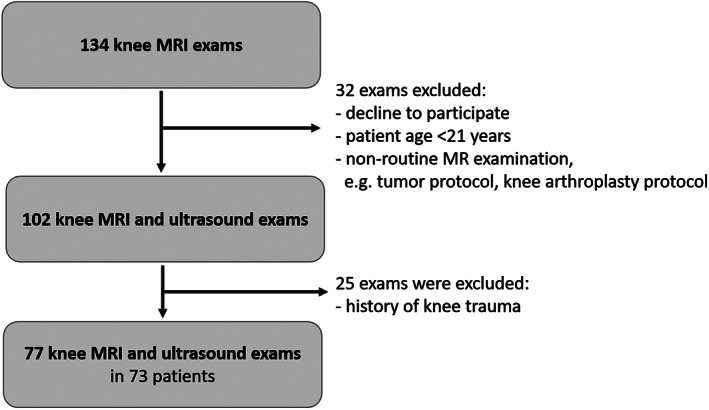
Flow chart shows number of participants and those excluded according to the inclusion criteria.
Imaging and Image Review
Ultrasound imaging of the lateral collateral ligament was performed in supine position by one fellowship‐trained musculoskeletal radiologist with 7 years of experience. The order of the examinations was performed randomly (MR examination followed by ultrasound or ultrasound followed by MR examination). The radiologist performing the ultrasound examination was blinded for the images and results of the MR examination.
For the ultrasound examination (Philips, Model CX50) a cushion was placed under the knee to simulate the slightly flexed knee position in the MR knee coil. Using a 12–5 MHz linear transducer placed over the lateral knee in a coronal oblique plane, the lateral collateral ligament was identified as a fairly uniform structure extending from the femur to the fibula in the expected location of the lateral collateral ligament. Characteristic bone landmarks, such as the popliteus groove of the femur and the fibular head assisted in its identification. Static and cine images were obtained in short and long axes of the lateral collateral ligament. Ultrasound examination also included color Doppler assessment of the lateral collateral ligament.
The routine knee MR imaging protocol consisted of axial T1‐weighted TSE non‐fat‐saturated (TR 500, TE 17), axial T2‐weighted fat‐saturated (TR 3000, TE 60), coronal intermediate‐weighted fat‐saturated (TR 2300–12,000, TE 39), sagittal intermediate‐weighted TSE non‐fat‐saturated (TR 5000, TE 30), and axial intermediate‐weighted fat‐saturated (TR 3122, TE 30). The MR examination was performed at one of four different scanners (1.5 or 3 Tesla, Philips, and Siemens scanners).
The MR and ultrasound images were evaluated independently and randomized by two fellowship‐trained musculoskeletal radiologists (23 and 7 years of experience) on Food and Drug Administration‐approved PACS workstations. Signal intensity of the proximal aspect of the lateral collateral ligament was evaluated on fluid‐sensitive MR sequences (low, intermediate, high), and echogenicity on ultrasound (hyperechoic, hypoechoic, anechoic) in comparison to the distal portion of the ligament. In case of discrepancy regarding the echogenicity between both readers, a third reader was used as an adjudicator (15 years of experience). Additionally, the extent of the above‐described finding was measured (length: proximal to distal; and width: medial to lateral) on MRI and ultrasound.
Cadaveric Specimens and Histology
Two cadaveric knees were imaged with MR imaging and ultrasound. Followed by a dissection of the lateral collateral ligament (Figure 2) on both knees and a histologic evaluation. The anatomic specimen included the proximal 2/3 of the lateral collateral ligament and its bony insertional area of the lateral femoral epicondyle. The histological evaluations were performed by an experienced musculoskeletal pathologist (26 years of experience) who was blinded regarding the MR imaging findings. Decalcified specimens were longitudinally sectioned, processed for histology, and stained with alcian blue and hematoxylin and eosin.
Figure 2.
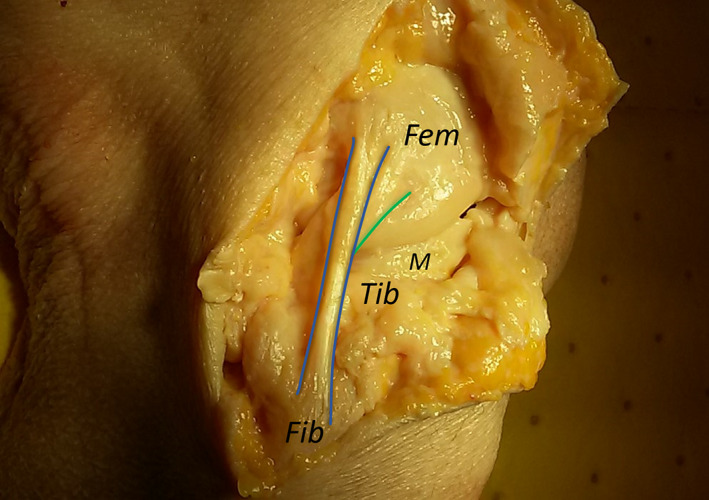
Right middle age female cadaveric knee shows the lateral collateral ligament (blue lines). The ligament extends from the lateral femoral epicondyle (Fem) to the fibular head (Fib). Note the proximity to the popliteal tendon (green line). Tib, Tibia; M, lateral Meniscus.
Statistical Analysis
Statistical analyses were performed with SPSS software (version 22.0; SPSS, Chicago, IL, USA). Descriptive statistics were calculated (mean, standard deviation, range, and percentage). Interreader reliability was calculated using Wilcoxon signed ranked test and intraclass correlation coefficient (ICC). A P value less than .05 was considered statistically significant for the Wilcoxon signed ranked test. According to Rosner for the interreader reliability an ICC value of >0.75 is considered excellent, 0.40–0.75 fair to good, and <0.40 poor. 10
Results
Demographics
The study group of 73 subjects with 77 knees consisted of 53% male (39/73) and 47% female (34/73) subjects (Table 1). Thirty‐five right and forty‐two left knees were examined, with four bilateral examinations. The mean age of the subjects was 48 years (range 22–81 years; standard deviation 14 years). Both cadaveric knees were from a female.
Table 1.
Demographic of Included Patients
| Number of Subjects | Number of Exams | Side | Gender | Age |
|---|---|---|---|---|
| 73 | 77 (including 4 bilateral exams) | 35 Right knees | 53% Male (39/73) | Mean 48 years ±14 (range 22–81 years) |
| 42 Left knees | 47% Female (34/73) |
Imaging Results of Subjects
On ultrasound, results from both readers including adjudication showed echogenicity as hyperechoic in 61% (47/77) (Figure 3), hypoechoic in 39% (30/77) (Figure 4), and anechoic in 0% (0/77) of cases (Table 2). Results from both readers showed MR signal intensity of the proximal attachment site of the lateral collateral ligament as, low in 21% (16/77) (Figure 3) and 6% (5/77), intermediate in 75% (58/77) (Figure 4) and 83% (64/77), and high in 4% (3/77) and 10% (8/77) of cases for Readers 1 and 2, respectively. The mean length of decreased echogenicity on ultrasound was 6.5 mm (±4.8) and width was 6.1 mm (±2.6). The mean length of increased MR signal was 8.6 mm (±4.9) and width was 5.3 mm (±2.3). The measurement details for both readers are depicted in Table 3. Although the decreased echogenicity/increased signal intensity area was not as commonly identified on ultrasound as on MR imaging with fair to good intermodality reliability (ICC = 0.445–0.511), if present there was no statistically significant difference between the measurements of both readers (P = .163–.795) and the ICC for measurements showed a good to excellent intermodality reliability (0.735–0.899). Reader one noted flow on color Doppler imaging in two cases (2/77), and reader two in none (0/77).
Figure 3.
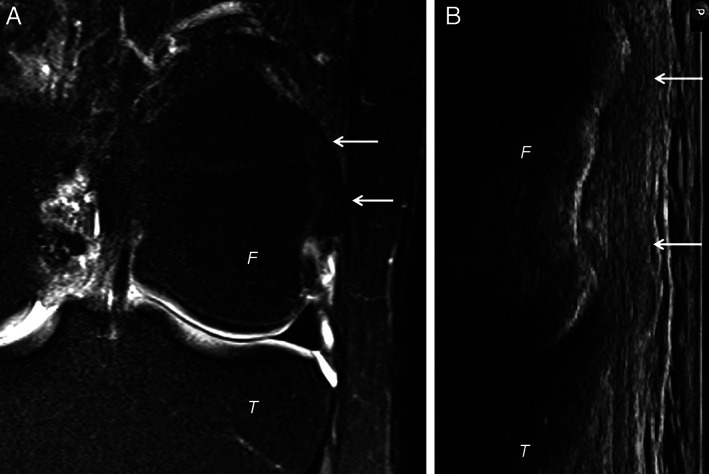
Left knee of a 28‐year‐old female showing on (A) coronal intermediate‐weighted MR imaging a homogenous low signal intensity of the lateral collateral ligament (arrows). Ultrasound image (B) rotated similar to the MR image orientation shows an equivalent homogenous hyperechoic lateral collateral ligament (arrows) at the proximal insertion site. F, Femur; T, Tibia.
Figure 4.
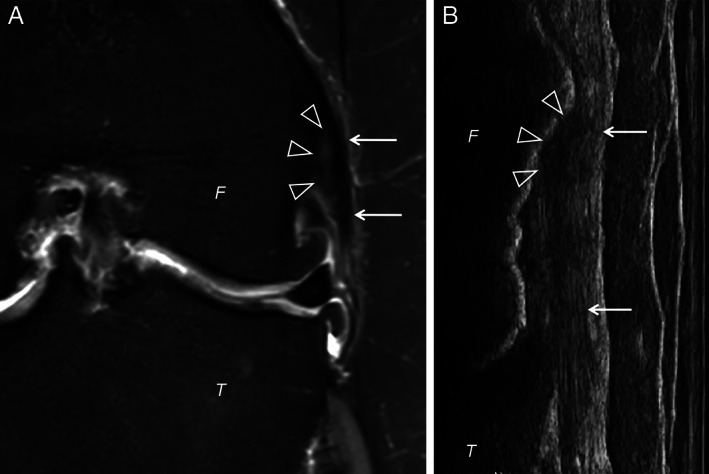
Left knee of a 73‐year‐old female showing on (A) coronal intermediate‐weighted imaging a focal hyperintense area (arrowheads) at the insertion of the lateral collateral ligament (arrows). Ultrasound image (B) rotated similar to the MR image orientation shows an equivalent hypoechoic area (arrowheads) at the lateral collateral ligament (arrows) proximal insertion site. F, Femur; T, Tibia.
Table 2.
MR Imaging Signal Intensity and Echogenicity on Ultrasound of the Proximal Attachment Site of the Lateral Collateral Ligament
| MR Imaging Signal Intensity | Ultrasound Echogenicity | |||||
|---|---|---|---|---|---|---|
| Reader 1 | Reader 2 | Reader 1 | Reader 2 | Adjudicator | ||
| Low | 16 (21%) | 5 (6%) | Hyperechoic | 48 (62%) | 28 (36%) | 47 (61%) |
| Intermediate | 58 (75%) | 64 (83%) | Hypoechoic | 29 (38%) | 48 (62%) | 30 (39%) |
| High | 3 (4%) | 8 (10%) | Anechoic | 0 (0%) | 1 (1%) | 0 (0%) |
| ICC | 0.609 | ICC | 0.621–0.665 | |||
Table 3.
Results of the Measurements of the Signal Intensity and Echogenicity Changes at the Proximal Attachment Site of the Lateral Collateral Ligament
| MR Imaging Signal Intensity | Ultrasound Echogenicity | |||||
|---|---|---|---|---|---|---|
| Reader 1 | Reader 2 | P value | Reader 1 | Reader 2 | P value | |
| Length (proximal to distal) | 8.5 ± 4.6 (1.4–17.4) | 5.3 ± 2.3 (0.8–12.2) | .795 | 6.5 ± 4.8 (0.8–17.1) | 7.9 ± 3.8 (2.7–18.2) | .795 |
| Width (medial to lateral) | 5.3 ± 2.3 (1.5–11.0) | 4.8 ± 1.5 (1.7–8.2) | .221 | 6.1 ± 2.6 (0.7–11.0) | 5.0 ± 1.4 (2.3–8.3) | .163 |
The values depict Mean ± Standard deviation (and range) in millimeter.
Results of Cadaveric Specimens
Both lateral collateral ligaments showed decreased echogenicity on ultrasound images and increased signal intensity on MR images at the proximal portion of the ligament. Histology evaluation showed transition of ligament fibers to fibrocartilage at the insertion site with increased connective tissue mucin staining with alcian blue corresponding to the findings on MR imaging and ultrasound (Figure 5).
Figure 5.
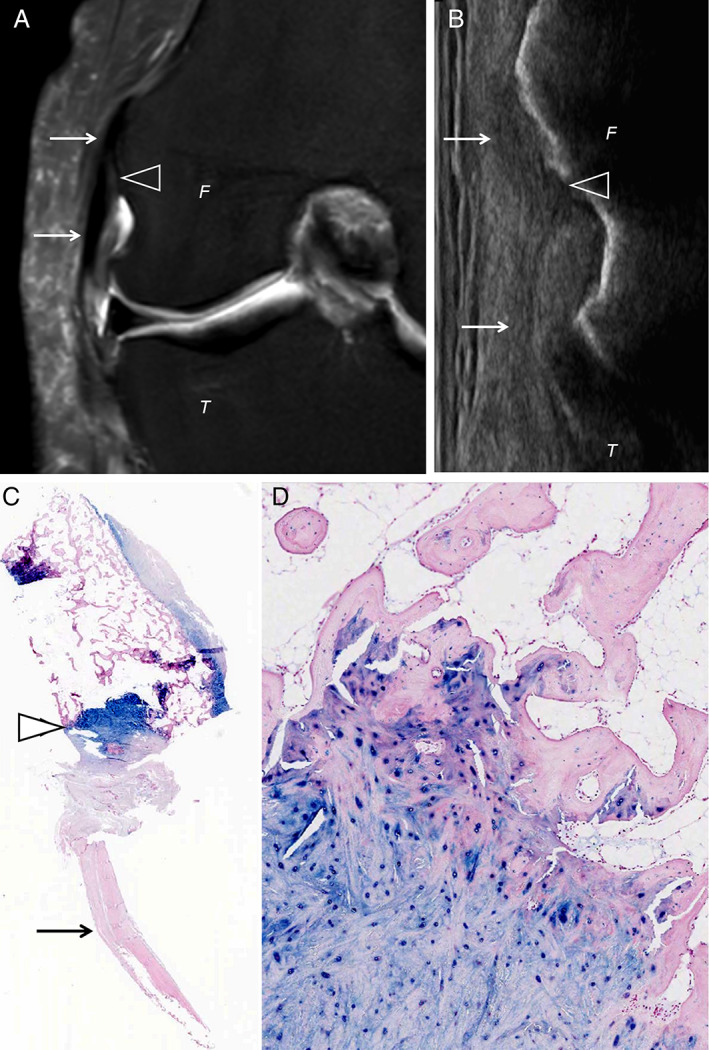
Middle‐age female cadaveric specimen with MR imaging, ultrasound, and histology of the right knee at the proximal insertion of the lateral collateral ligament (arrows). A, Coronal intermediate‐weighted imaging shows a focal hyperintense area (arrowhead) at the insertion of the lateral collateral ligament (arrows). Ultrasound image (B) rotated similar to the MR image orientation shows an equivalent hypoechoic area (arrowhead) at proximal insertion site of the lateral collateral ligament (arrows). Histologic specimen stained with alcian blue (C) highlights connective tissue mucin (myxoid matrix) within the fibrocartilage of the insertion site (arrowhead) with the ligament at the image bottom (arrow) (original magnification ×1). Higher power image (D) depicts fibrocartilage with alcian blue staining inserting into femoral bone at the image top (original magnification ×200). F, Femur; T, Tibia.
Discussion
Ultrasound and MR imaging can be used to assess various ligaments including the lateral collateral ligament at the knee. In our study, we found decreased echogenicity of the proximal lateral collateral ligament on ultrasound and increased signal intensity on MR imaging to be a common imaging finding. Histologically, these echogenicity or signal changes corresponded to normal connective tissue mucin. There was correlation between measurements using ultrasound and MR imaging.
The lateral collateral ligament is an important stabilizer of the knee, especially for varus instability and for the posterolateral corner. 1 , 2 , 6 Compared to other ligaments of the knee (e.g. anterior/posterior cruciate ligament, medial collateral ligament), lateral collateral ligament injuries are less common and usually involve multiple structures of the posterolateral corner. 6 , 11 , 12 Early diagnosis and treatment are crucial to decrease the risk of chronic instability or even the risk of anterior cruciate ligament graft failure. 2 , 6
Imaging of the lateral collateral ligament is mostly performed via MR imaging or ultrasound. A normal lateral collateral ligament shows uniformly low signal intensity on MR and is hyperechoic and fibrillar on ultrasound. 5 , 8 However, Lee et al described signal abnormalities in the proximal portion of the lateral collateral ligament on MR to be common and a normal finding. 7 They described 88% of ligaments with an intermediate and 6% with a high signal intensity on MR. This is comparable to our study with 75–83% intermediate and 4–10% high‐intensity ligaments on MR imaging. Our study additionally investigated the presence of this finding on ultrasound. While present in 39% of subjects in our study in ultrasound, the proximal lateral collateral ligament findings were more commonly identified in MR imaging. However, if changes of echogenicity were visible on ultrasound their dimensions correlated to the measurements on MR images. The higher number of lateral collateral ligament findings on MRI may relate to routine coronal imaging that is not in plane with the orientation of the lateral collateral ligament. 4 , 5 Thus, the MR images might have been more prone to artifacts, e.g. partial volume effect, compared to the anatomically oriented ultrasound examination in our study. Magic angle artifact might have also influenced the signal intensity of the lateral collateral ligament, although the orientation of the lateral collateral ligament is much lower than 55 degrees. 13 , 14 Additionally, we examined images from intermediate‐weighted fat‐saturated imaging with short TE (≤30 ms) which is known to rarely see the magic angle artefact at 0°–20° to B0 in all sequences. 7 , 13 Alternatively, the ultrasound findings may be subtle or subjective at retrospective image review in spite of the use of cine clips. Additionally, high signal intensity on MR imaging does not necessarily have to correspond to decreased echogenicity on ultrasound.
Chen et al reported of an association of signal abnormalities of the lateral collateral ligament in patients with a higher grade of osteoarthritis in the lateral compartment. 15 Neither the study by Lee et al nor our study identified degeneration or tear of the ligament at histology. 7 Thus, without the disruption of the fibers or periligamentous reaction, e.g. edema or hematoma, the imaging finding of MR signal or ultrasound echogenicity changes can in our opinion be interpreted as a normal and clinically insignificant finding.
We acknowledge some limitations in our study. Although this was a prospective study, our subjects were not presumably asymptomatic and a true prevalence of imaging findings cannot be determined. There was also lack of surgical or histologic correlation except for the two cadaveric knees. There was no clinical or specific demographic information available regarding the cadaveric knees. Retrospective review of ultrasound images also presents inherent limitations although cine clips were also included in image assessment.
Conclusion
Decreased echogenicity and increased signal intensity of the proximal lateral collateral ligament of the knee on ultrasound and MR imaging, respectively, are common imaging findings that most likely correspond histologically to normal connective tissue mucin. Such findings should not be mistaken for ligament pathology in patients without lateral symptoms.
Acknowledgments
The authors would like to acknowledge the body donor of the cadaveric knees and Dean Mueller of the anatomical science department (Anatomical Sciences, University of Michigan, Ann Arbor, MI) for their help. The contribution of body donors is immensely helpful to the progress of science. We are grateful and honored by our donors' contribution.
Open Access Funding provided by Universitat Zurich.
The study was funded by Freiwillige Akademische Gesellschaft, Gottfried und Julia Bangerter‐Rhyner‐Stiftung, Schweizerische Gesellschaft für Radiologie and Universität Basel.
The authors declare that they have no conflict of interest.
Anna L. Falkowski, MD, MHBA received grants from the Research Funds of the University of Basel, Swiss Society of Radiology, Gottfried und Julia Bangerter‐Rhyner‐Stiftung, and Freiwillige Akademische Gesellschaft Basel. All sponsors listed above played no role in matters of study design, collection, analysis, interpretation of data, and in the decision to submit the paper for publication.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- 1. Grawe B, Schroeder AJ, Kakazu R, Messer MS. Lateral collateral ligament injury about the knee: anatomy, evaluation, and management. J Am Acad Orthop Surg 2018; 26:e120–e127. 10.5435/jaaos-d-16-00028. [DOI] [PubMed] [Google Scholar]
- 2. Coobs BR, LaPrade RF, Griffith CJ, Nelson BJ. Biomechanical analysis of an isolated fibular (lateral) collateral ligament reconstruction using an autogenous semitendinosus graft. Am J Sports Med 2007; 35:1521–1527. 10.1177/0363546507302217. [DOI] [PubMed] [Google Scholar]
- 3. Chahla J, Moatshe G, Dean CS, LaPrade RF. Posterolateral corner of the knee: current concepts. Arch Bone Jt Surg 2016; 4:97–103. [PMC free article] [PubMed] [Google Scholar]
- 4. Miller TT. Imaging of the medial and lateral ligaments of the knee. Semin Musculoskelet Radiol 2009; 13:340–352. 10.1055/s-0029-1242188. [DOI] [PubMed] [Google Scholar]
- 5. Bolog N, Hodler J. MR imaging of the posterolateral corner of the knee. Skeletal Radiol 2007; 36:715–728. 10.1007/s00256-006-0271-5. [DOI] [PubMed] [Google Scholar]
- 6. Filli L, Rosskopf AB, Sutter R, Fucentese SF, Pfirrmann CWA. MRI predictors of posterolateral corner instability: a decision tree analysis of patients with acute anterior cruciate ligament tear. Radiology 2018; 289:170–180. https://doi.org10.1148/radiol.2018180194. [DOI] [PubMed] [Google Scholar]
- 7. Lee HN, Ahn SE, Park JS, et al. Differences in MR signal intensity of lateral collateral ligament of knee joint on fat‐suppressed proton density‐weighted imaging. Br J Radiol 2016; 89:20150893. 10.1259/bjr.20150893. [DOI] [PubMed] [Google Scholar]
- 8. Jacobson JA, Ruangchaijatuporn T, Khoury V, Magerkurth O. Ultrasound of the knee: common pathology excluding extensor mechanism. Semin Musculoskelet Radiol 2017; 21:102–112. 10.1055/s-0037-1599204. [DOI] [PubMed] [Google Scholar]
- 9. Alves TI, Girish G, Kalume Brigido M, Jacobson JA. US of the knee: scanning techniques, pitfalls, and pathologic conditions. Radiographics 2016; 36:1759–1775. 10.1148/rg.2016160019. [DOI] [PubMed] [Google Scholar]
- 10. Rosner B. In: Rosner B (ed). The Intraclass Correlation Coefficient. 7th ed. Boston: Brooks/Cole, Cengage Learning; 2011. [Google Scholar]
- 11. Bushnell BD, Bitting SS, Crain JM, Boublik M, Schlegel TF. Treatment of magnetic resonance imaging‐documented isolated grade III lateral collateral ligament injuries in National Football League athletes. Am J Sports Med 2010; 38:86–91. 10.1177/0363546509344075. [DOI] [PubMed] [Google Scholar]
- 12. Recondo JA, Salvador E, Villanua JA, Barrera MC, Gervas C, Alustiza JM. Lateral stabilizing structures of the knee: functional anatomy and injuries assessed with MR imaging. Radiographics 2000; 20:S91–S102. 10.1148/radiographics.20.suppl_1.g00oc02s91. [DOI] [PubMed] [Google Scholar]
- 13. Li T, Mirowitz SA. Manifestation of magic angle phenomenon: comparative study on effects of varying echo time and tendon orientation among various MR sequences. Magn Reson Imaging 2003; 21:741–744. 10.1016/s0730-725x(03)00177-2. [DOI] [PubMed] [Google Scholar]
- 14. Richardson ML, Amini B, Richards TL. Some new angles on the magic angle: what MSK radiologists know and don't know about this phenomenon. Skeletal Radiol 2018; 47:1673–1681. 10.1007/s00256-018-3011-8. [DOI] [PubMed] [Google Scholar]
- 15. Chen YH, Carrino JA, Raman SP, Morrison WB, Fayad LM. Atraumatic lateral collateral ligament complex signal abnormalities by magnetic resonance imaging in patients with osteoarthrosis of the knee. J Comput Assist Tomogr 2008; 32:982–986. 10.1097/RCT.0b013e3181635e39. [DOI] [PubMed] [Google Scholar]


