Abstract
Purpose
Virtual reality (VR) can be useful in explaining diseases and complications that affect children in order to improve medical communications with this vulnerable patient group. So far, children and young people’s responses to high‐end medical VR environments have never been assessed.
Methods
An unprecedented number of 320 children and young people were given the opportunity to interact with a VR application displaying original ophthalmic volume data via a commercially available tethered head‐mounted display (HMD). Participants completed three surveys: demographics and experience with VR, usability and perceived utility of this technology and the Simulator Sickness Questionnaire. The second survey also probed participants for suggestions on improvements and whether this system could be useful for increasing engagement in science.
Results
A total of 206 sets of surveys were received. 165 children and young people (84 female) aged 12–18 years (mean, 15 years) completed surveys that could be used for analysis. 69 participants (47.59%) were VR‐naïve, and 76 (52.41%) reported that they had previous VR experience. Results show that VR facilitated understanding of ophthalmological complications and was reasonably tolerated. Lastly, exposure to VR raised children and young people’s awareness and interest in science.
Conclusions
The VR platform used was successfully utilized and was well accepted in children to display and interact with volume‐rendered 3D ophthalmological data. Virtual reality (VR) is suitable as a novel image display platform in ophthalmology to engage children and young people.
Keywords: children, virtual reality, ray casting, optical coherence tomography, volume rendering, point‐cloud data
Introduction
There has been a dramatic increase in myopia among school‐age children in East and Southeast Asia over recent decades (Dolgin 2015; Yam et al. 2020). Since efforts to date have been insufficient, myopia‐associated complications will increase so that the vulnerable patient group of children in particular will be exposed to vision‐threatening myopic eye complications such as choroidal neovascularization, cataract, glaucoma, macular degeneration and retinal detachment (Cooper & Tkatchenko 2018).
Although promising results have been obtained thanks to new therapeutic procedures (e.g. intravitreal injection of anti‐vascular endothelial growth factors and the advancement of vitreoretinal surgery), these interventions represent a considerable impact (Ohno‐Matsui et al. 2016; Cheung et al. 2017). Thus, one of the most difficult aspects for health professionals is to communicate a sight‐threatening disease to the child and their family (Stein et al. 2019).
In these situations, it is beneficial that today's children and young people are being exposed to digital technologies from birth and that this digitalization has contributed to virtual reality (VR) classroom sessions (Kyaw et al. 2019; Lorenzo‐Alvarez et al. 2019; Sattar et al. 2019). In parallel to developments in technology and evidence for VR as a tool of surgical education, non‐invasive optical coherence tomography (OCT) has become one of the most popular imaging techniques in ophthalmology (Huang et al. 1991; Fujimoto and Huang, 2016). In this way, it has become possible for non‐ophthalmologists to navigate and interact with OCT data in real time and in a compelling three‐dimensional virtual space (Maloca et al. 2018). Virtual reality (VR) could therefore prove to be a useful tool in making a disease more comprehensible and accessible to children and young people and to prepare them for medical interventions. Further to patient communication, VR (and augmented reality) has the potential to increase interest in and engagement with science in young people (Stratos et al. 2016; Zimmerman et al. 2016; Kersting et al. 2020). It is of interest then to additionally probe the potential of an ophthalmological VR experience to engage and motivate the next generation of medical students: children and young people.
Although VR is already being used to reduce pain and anxiety in children (Eijlers et al. 2019), there is little knowledge of whether they can tolerate such an application. Here we go a step further and investigate the feasibility, usability and tolerability of medical virtual reality in children and young people, which have never previously been assessed. Therefore, the aim of this study was to assess children and young people’s responses to an ophthalmological VR experience, with a focus on whether it can facilitate understanding, increases interest in science generally and is well‐tolerated in this young population.
Materials and methods
Participants and anonymization
Sixteen local school classes at grammar school level were invited to the public VR exhibition free of charge and without compensation. This research followed the tenets of the Declaration of Helsinki. The use of the data was approved by the local ethics committee Nordwest‐ und Zentralschweiz Basel, Switzerland (EKNZ‐ID:2016‐01948 and 2016‐01948).
Inclusion criteria were all participants who showed adequate reading ability and comprehension, volunteered to participate, complied with instructions and followed the safety guidelines faithfully after explanation of the nature and possible consequences of the study.
Exclusion criteria included children being under twelve years of age, any general disability that would preclude the participant’s adequate comprehension of the consent and any known adverse reaction to VR or other digital technologies. Refractive errors (i.e. the requirement of spectacles or contact lenses), other health conditions or medical history were not considered in this study, and completion of the surveys was not mandatory.
Attainment of consent
The privacy rights of the study participants were always respected. All teachers provided informed consent for all children as their guardians, as the VR presentation was part of a regular school program. Thus, written informed consent from each participant was not required. Therefore, it was possible to waive additional requirements to obtain permission from parents or guardians.
Affirmative agreement to participate in this research was obtained from all participants. Participants were also given the opportunity to ask questions and the local instructors explained anything that was not clear. All teachers involved had the opportunity to receive information about the study, ask questions, participate personally and agree or disagree with their student's participation in the research study. The corresponding teacher was always present and available to their class as a companion and supervisor. The data of the study participants were recorded anonymously so that no separate authorization was required under the Swiss Human Research Act. To maintain anonymity, the name, date of birth, school class or other personal data were explicitly not recorded. Only age and gender were noted. The forms were collected by the local support team and processed further in a separate location by a second independent team having no contact with the participants, to ensure participants could not be recognized by their responses. In addition, questions were asked to assess the digital immersion of the participants.
Venue
During the Zurich Film Festival 2018 (a platform for promising filmmakers from around the globe), a virtual reality application was publicly presented in close collaboration with the Institute of Molecular and Clinical Ophthalmology Basel (IOB), Basel, Switzerland, and the University of Basel, Switzerland. The goal of the event was to make current and interdisciplinary computer research accessible to a broad audience and to engage the public with filmmaking and science, to promote dialogue and interest in science and to discuss its implementation and possible consequences. In this context, a science exhibition was organized, operated by the non‐profit organization Eye On Science, Zurich, Switzerland, under the patronage of the Swiss National Science Foundation (SNSF), the University of Zurich (UZH), Switzerland, the Swiss Federal Institute of Technology (ETH), Zurich, Switzerland, and their joint project Life Science Zurich.
Procedures
All participants used the VR application voluntarily and followed the same procedure. Each participant was individually trained by an experienced operator in the use of the VR application before the experience and accompanied throughout to ensure safety at all times. Participants were able to pause or stop the experience at any moment. The use of spectacles or contact lenses was allowed. The time of the exposure to the VR experience typically lasted between five and fifteen minutes. After the VR experience, the participant could rest on a comfortable seat and had the opportunity to contact the instructor directly if necessary, so that the greatest possible surveillance was always guaranteed.
After exposure to the VR environment, three surveys were completed on a voluntary basis by the participants. These were a ‘Demographics and Experience’ (with VR) survey, a ‘Virtual Reality Reactions’ survey on their perception of the current VR application and the ‘Simulator Sickness Questionnaire’ (Kennedy et al. 2001). The topics covered in the surveys can be found in the forthcoming figures and the supplemental information file (see Supporting information S1, Table S1). In order to further develop the VR application, participants were asked to provide suggestions with regard to the usability for future VR improvements (see Supplementary File S2, Table S2a‐c).
Virtual reality environment
A VR application (SpectoVR version 2.2; Center for medical Image Analysis & Navigation, University of Basel, Switzerland) that allowed the import and display of 3D volumetric data was provided. To ensure the best possible interactive VR immersion, two independent and site‐separated VR rooms were created in room‐scale to enhance the feeling of immersion (each had an approximate size of 3 m × 3 m × 3 m). The projection of the image data was carried out by using two commercially approved, unmodified, independent and tethered head‐mounted displays (HMDs) with an image resolution of 1080 × 1200 pixel per eye, thus, 2160 × 1200, a nominal field of view ~110° and tracking system lighthouse with two base stations in total emitting 60Hz pulsed infrared lasers, wired connection using HDMI 1.4 (HTC Vive, Xindian District, New Taipei City, Taiwan). The application was deployed and operated by two separated high‐end laptops (XMG high‐end notebook, Schenker Technologies GmbH, Leipzig, Germany; Windows 10 home, 64bit, 32 RAM, NVIDIA GeForce GTX 1080 8192MB GDDR5, CPU Intel® CoreTM i7‐6700K CPU @ 4.00 GHZ, 4 cores and ROG Zephyrus Thin & Light Gaming Laptop, 15.6" Full HD 120Hz, Intel Core i7‐7700HQ Processor, NVIDIA GeForce GTX 1080 8GB Max Q, 16GB DDR4, 512GB PCIe SSD, Windows 10 Professional – GX501VI‐XS74). Both computers were able to deliver the images at a rate of 180 frames per second (90 frames per second to each eye) to provide high realism and clarity of the visualization which was enhanced by a simultaneous advanced ray casting visualization to render shadows cast in real time.
VR models
Three different medical VR models were made available (Fig. 1): (A) a peripheral retinal tear in a human eye, generated from swept source optical coherence tomography (SS‐OCT) volume data (6 mm × 6 mm × 2.6 mm volume scan, Triton DRI Swept Source OCT, Topcon, Tokyo, Japan). Without treatment, such a lesion can lead to retinal detachment and blindness; (B) a computed tomography, helical bone skull scan of a skier who suffered a right orbit fracture trauma; and (C) a vessel model derived from a normal mini‐pig eye obtained by micro‐Xray computed tomography (Skyscan 1172, Bruker MicroCT, Kontich, Belgium) after post‐mortem injection of a contrast agent (Angiofil, Fumedica AG, Muri, Switzerland) to display the vascular architecture of an eye. Each data model could be loaded into the VR environment and explored separately by the user (i.e. a single model per time unit), whereby the order was not predetermined, to offer the participants the greatest possible freedom of choice.
Fig. 1.
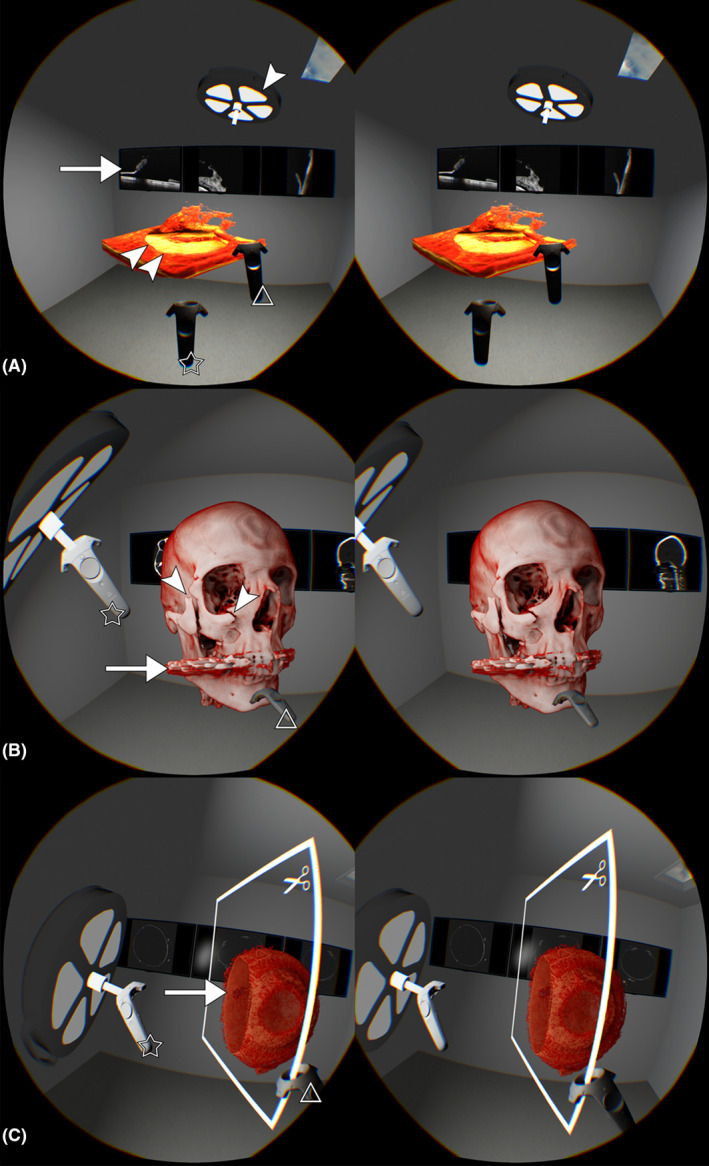
Stereoscopic display of the virtual reality environment (VR) and three VR models from this study (images can be fused for stereoscopic experience). (A) Volume‐rendered OCT data of a peripheral retinal tear in a human eye. The retina model was freely floating in space and could be observed from all sides. It was navigated by the right handle (triangle) and the left handle was freely available inside the VR space in this illustration. The edge of the retina tear was clearly depicted (double arrow heads). Above the VR model, the ray casting light (white arrow head) was positioned for better illumination, and the projection of the shadow below the tear is visible on the yellowish displayed retinal pigment epithelium (RPE). In the background on the wall, the conventional cross‐sectional OCT images (white arrow) were displayed. (B) VR display of a computed tomography (CT) scan of a skull of a skier who presented after a ski accident showing several fractures and dislocated bone fragments in the right skull hemisphere. The ray casting light was centred with the left handle (star) in the direction of the fractures (arrow heads) on the skull. The right handle (triangle) positioned the skull towards the light to improve the representation of the dislocated fractures in 3D. In the area of the teeth, radial artefact signals were visible, typical for metallic tooth fillings (arrow). Conventional CT images were placed in the background. (C) A VR vessel model of a healthy mini‐pig’s eye imaged with micro‐computed tomography after contrast agent was injected into the vessels is depicted. The ray casting light was centred with the left handle (star) on the eye to illuminate it well. The eye model consisted only of vessels, whereby the model was cut using a VR cut plane with the right handle (triangle). This allowed for an inside view to visualize the posterior opening in the area of the optic disc (arrow) and the retinal vessels, among others. At the front right, the cavity in the pupil was made visible.
Analysis
Because participation in the survey was voluntary, some survey responses were incomplete, where the number of valid responses to each question ranged between 131 and 165. We define valid responses as those where the participant selected a single option or wrote a legible response, as appropriate. Where a participant selected multiple options, or their response was illegible, this question was excluded from the analysis. As such, alongside absolute frequencies, responses to questions are represented as percentages out of the number of participants who gave a valid response to that specific question. To better understand participants’ perceptions and expectations of the VR experience, we wanted to gauge their familiarity with other forms of digital technology, that is mobile and gaming devices.
Results
From a total of 320 participants who experienced the VR simulations, 203 eligible participants (aged 12–18 years) completed the surveys, resulting in up to 165 valid responses for each question (51.56%). See Table S1 for the number of respondents for each question in the Demographics and Experience survey and the Virtual Reality Reactions survey.
Demographics and experience survey
Eighty‐four participants (58.33%) identified themselves as female and 60 participants (41.67%) as male. The mean age was 15.0 years (range, 12–18 years). 89 (61.81%) reported that they used spectacles or contact lenses.
Mobile and gaming device ownership and usage
One hundred and forty‐one participants (98.60%) reported that they owned a mobile phone. Of these, 115 (81.56%) had an iPhone, whereas 25 (17.73%) had an Android Phone, and one (0.71%) owned a different system. The mean duration of mobile phone ownership was 4.40 years (range, 1–8 years).
When asked about their typical mobile phone usage per day, 34 (21.94%) said they used their phone for 0–1 h, while 92 (59.35%) used their phone for 2–3 h, and 29 (18.71%) used their phone for 3–4 h. One hundred thirty‐two (92.31%) reported that they had free access to a computer, 108 (75.52%) said that they played games on their mobile, 59 (41.26%) said that they played games on their computer.
When asked how many hours they played games per day, 134 (83.75%) said they played games for 0–1 h, while 22 (13.75%) played games for 2–3 h, and 4 (2.50%) played games for 3–4 h.
VR ownership and usage
69 participants (47.59%) reported that they had never used VR before, and 76 (52.41%) reported that they had previous VR experience (20 participants did not provide responses). 14 (9.66%) said that they had access to VR in their family home, and 37 (25.34%) said that their friends had VR equipment.
Interest in/relationship with science
To investigate whether this ophthalmology VR experience increased children and young peoples’ interest in science, participants rated their levels of interest before and after the experience. Regarding levels of interest in science before this VR experience, 34 (23.94%) reported it to be low, 64 (45.07%) said medium and 44 (30.99%) said high. In terms of their level of interest in science after the VR experience, 14 (10.00%) said low, 65 (46.43%) said medium and 61 (43.57%) said high. See Fig. 2 for a representation of how these responses changed between the two time‐points. The VR experience increased 40 (25.00%) participants’ interest in science: 21 (13.13%) from low to medium, 17 (10.63%) from medium to high, and 2 (1.25%) from low to high. One hundred and eighteen (73.75%) participant’s interest remained the same, and the interest decreased in 2 (1.25%) participants.
Fig. 2.
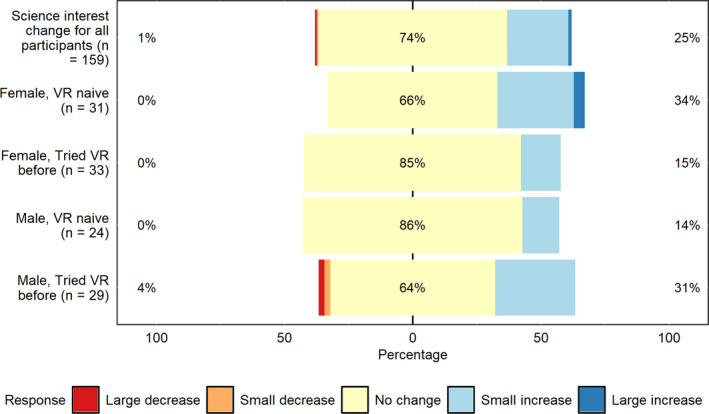
Participants’ change in their level of interest in science following their ophthalmology VR experience. The top bar shows this change for the whole sample (159 valid responses), while the four other bars indicate changes as a function of gender and VR experience. Percentages on the left relate to decreases in interest, whereas percentages on the right indicate increases in interest. Large increases/decreases indicate changes between ‘low’ and ‘high’. Small increases/decreases relate to changes between ‘low’ and ‘medium’, or ‘medium’ and ‘high’.
Figure 2 also shows these changes in science interest as a function of previous use of VR and gender. Inspection of the figure suggests the two participants whose level of interest in science increased from low to high following the VR experience were two females who had not used VR before. In contrast, the two participants whose level of interest in science decreased from high or medium to low were two males who had used VR before.
In terms of support for similar (VR) events, eleven (7.86%) reported low, 32 (22.86%) said medium and 97 (69.29%) said high. Relatedly, 21 (14.58%) said they had a scientist in their family, and 46 (31.94%) reported that they had a physician in their family. In terms of coding/programming experience, 38 (26.57%) said that they can code, and 54 (39.42%) said that they were interested in coding. Finally, when asked whether they could imagine themselves as a scientist, 61 (42.96%) said low, 54 (38.03%) said medium and 27 (19.01%) said high.
Simulator sickness questionnaire (SSQ)
As reported in a previous study, a simulator disease questionnaire (SSQ) was used to assess the extent to which the VR technology induced side effects in adults (Maloca et al. 2018). In the current study, 133 participants provided complete responses for the SSQ questions, so only these participants’ data were included in this specific analysis. The proportions of participants answering ‘none’, ‘light’, ‘moderate’ and ‘heavy’ to each of the SSQ symptoms are shown in Fig. 3. Inspection of the figure suggests that the most prevalent symptoms were fatigue, eye strain and ‘fullness of the head’, with 22%, 17% and 15% of participants reporting ‘moderate’ or ‘heavy’ symptoms, respectively.
Fig. 3.
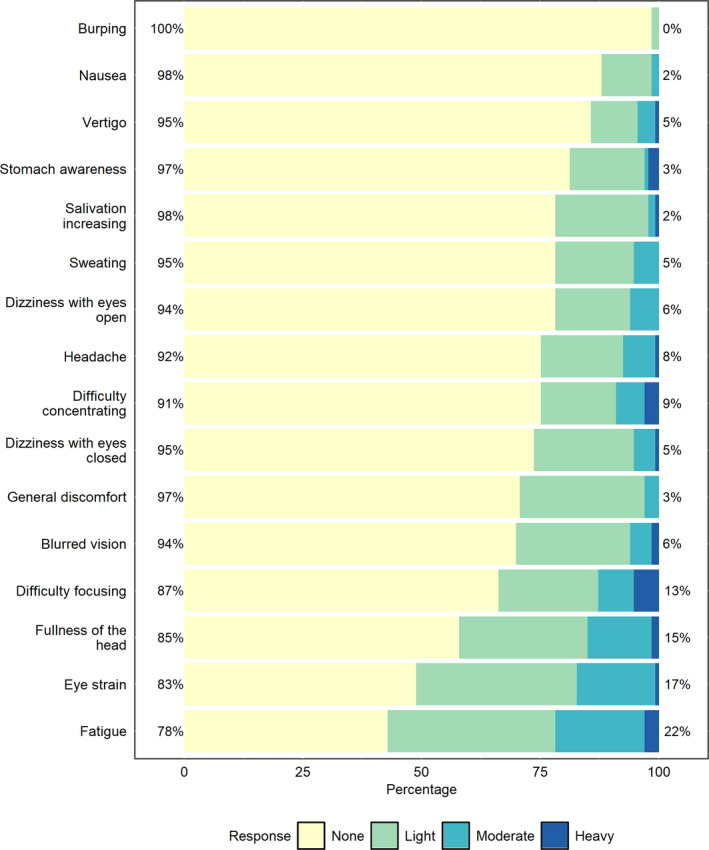
Responses to the Simulator Sickness Questionnaire. Percentages on the left relate to the number of people who indicated ‘none’ or ‘light’ symptoms, whereas percentages on the right indicate ‘moderate’ or ‘heavy’ responses.
The mean total score of 30.43 (SD = 30.20) on the SSQ was rather high, as a traditional interpretation of the SSQ scale indicates scores of 10 or above to represent significant symptoms. To interrogate this further, we conducted a more detailed examination of responses. According to the rating scale for total SSQ scores, 15 participants (11.28%) had ‘no symptoms’, 12 (9.02%) had ‘negligible symptoms’, and 7 (5.26%) had ‘minimal symptoms’. However, 21 participants (15.79%) had ‘significant symptoms’, for 5 participants (3.76%), ‘symptoms are a concern’, and finally, for 73 participants (54.89%), the SSQ indicated that the VR system was ‘a problem simulator’.
Influence of previous VR exposure
We tested the possibility that the SSQ scores varied as a function of previous exposure to VR (see Fig. 4). A Mann–Whitney–Wilcoxon test revealed no statistically reliable differences between the groups (W = 2441, p = 0.300).
Fig. 4.
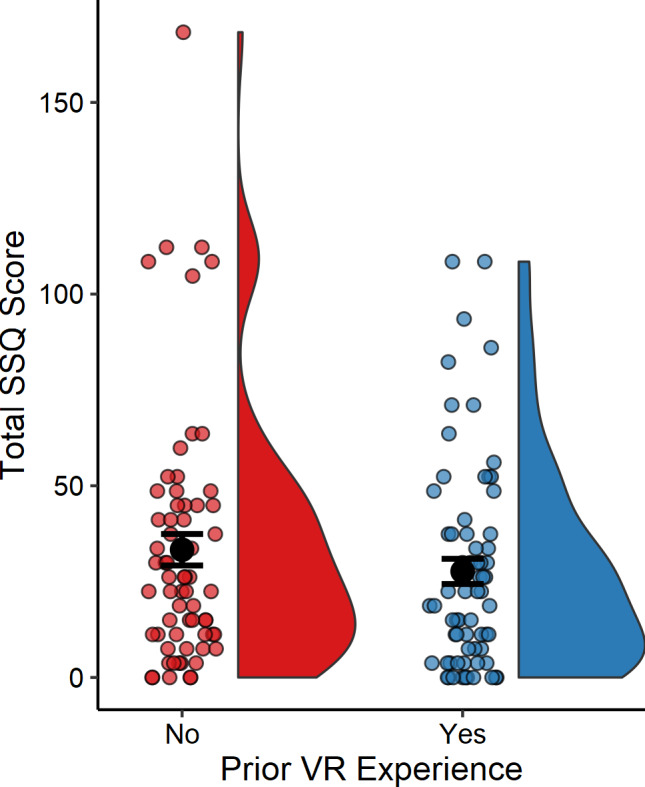
Participant’s total SSQ scores according to whether they had or had not experienced virtual reality before. Smaller coloured circles represent the scores of individual participants, whereas the larger black circles indicate the means for each group. Error bars indicate standard error, and the data distributions are represented to the right of each mean.
Virtual reality reactions survey
Participants were asked to rate their experiences of the VR application across twelve items. These items explored the participants’ perceptions of the value of the VR application – from perspectives on clinical value (training pedagogy and patient understanding) through to enjoyment. The level of agreement to each question (shown as a summary statement) is represented in Fig. 5.
Fig. 5.
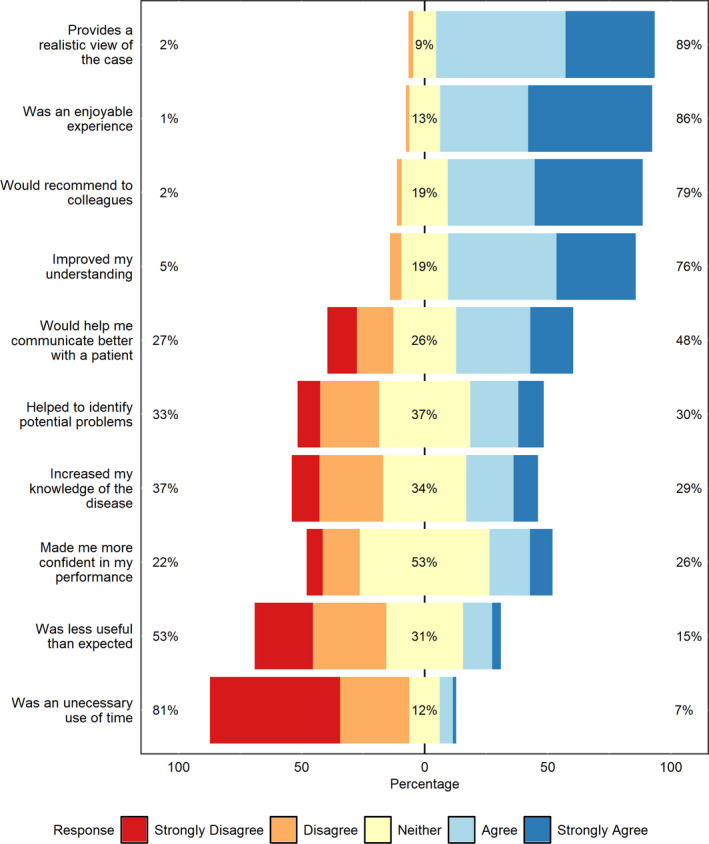
Responses to the Virtual Reality Reactions survey. Percentages on the left relate to the number of people who answered ‘strongly disagree’ or ‘agree’, whereas percentages on the right indicate ‘agree’ or ‘strongly disagree’ responses. Percentages in the centre relate to ‘neither agree nor disagree’ responses.
Participants were able to answer free entry questions about VR, such as their assessment of VR in general, what the strengths of the VR application used in this study were and what improvements were desired. Table S2a‐c summarizes the results of the free statements. The answers received show that above all, a relatively realistic visualization was appreciated, with the possibility of interactivity in the sense that objects were made accessible and their size could be changed in a quite easy to use and safe environment. The main indicated weaknesses included image blurriness and moderate image display resolution, a relatively uncomfortable HMD and the lack of possible options such as changing the colour and the contrast of the model or missing marking. Participants commented that it would also be desirable if the user's face would be represented within the VR room.
Discussion
The fact that myopia has already reached epidemic proportions highlights the unmet need and the great challenge of explaining associated diseases in a way that is accessible to lay people, particularly for children. (Ohno‐Matsui et al. 2016; Failo et al. 2018). In this context, VR has been shown to be a well‐tolerated ophthalmological image display platform for adults, representing medical data in an immersive and intuitive way (Maloca et al. 2018). This novel VR display could be used, for example, to communicate issues surrounding myopic complications such as a retinal tear or the need for repeated anti‐vascular endothelial growth factor (VEGF) injections.
Therefore, this study aimed to broaden the scope at investigating the response of children to a professional VR‐based medical environment serving as a potential computer‐generated communication platform. Specifically, we investigated whether this application could facilitate communication, increase an interest in science and be well‐tolerated physically. This is significant since there were no such assessments of medical VR environments in this vulnerable group in existing literature to our knowledge. Compared to other surveys (Phillips et al. 2016; Zha et al. 2019), this study showed a high response rate for a survey (51.56%), an important indicator of the survey quality for this young cohort since no incentives were applied.
Overall, the data revealed that the VR application aroused great interest and was successfully accepted. With regard to tolerability, the effect of the VR experience in children and young people was more pronounced than in our previous research displaying the same VR retinal tear model to trained adults (ophthalmologists) (Maloca et al. 2018). The SSQ scores showed higher than ‘minimal symptoms’ for 75% of children and young people. The most common symptoms were fatigue, eye strain and ‘head fullness’, which could indicate that the new visual experience was unfamiliar or taxing, although the use of digital media in this group was relatively high as previously reported (Hosokawa & Katsura 2018). The side effects with regard to the other categories of symptoms such as nausea (Bos et al. 2018) and disorientation were negligible (Kim et al. 2018). Simulator sickness questionnaire (SSQ) scores did not significantly differ between those who had used VR before and those who had not.
It should be noted that this sample had additional VR models on offer compared to the adults in our previous study, namely a skull with a right orbital fracture and a healthy mini‐pig’s eye. This could be partly responsible for the larger reactions as the skull was very realistic and could be greatly enlarged in VR. Previous studies reporting children’s responses to SSQs following a VR experience reported little to no symptoms, which suggests that it may be the nature of the models displayed in VR rather than VR itself that contributed to higher SSQ scores in our sample (Parsons et al. 2007; Tychsen & Foeller 2020; Araiza‐Alba et al. 2021).
However, no participants ended the experience early due to discomfort (Tychsen & Foeller, 2020). The skull and mini‐pig eye models were included with the intention of capturing the attention and interest of the young participants during the science festival, though this may have been misguided. We therefore recommend that any medical VR models displayed to children and young people during patient communication are relevant and appropriate to the particular topic.
Despite the occurrence of symptoms in some participants, the Virtual Reality Reactions survey showed that the majority of children found the experience to be an enjoyable one (86%) that they would recommend (79%), as adults had reported in previous work (Maloca et al. 2018). There was also a majority agreement (76%) that the VR application enhanced their understanding of the topic, and half of participants (48%) agreed that the VR application would help with patient communication. Most participants disagreed that it was an unnecessary use of time (81%). This good result testifies that an important goal was achieved to establish and facilitate communication between ophthalmological VR scientists and children and young people.
Our results from the Demographics and Experience survey suggest that the ophthalmology VR application increased the level of interest in science of 25% of the children and young people, while approximately 33% maintained a medium interest and another 33% maintained a high interest level. Further exploration indicated that the only two participants whose interest in science increased from low to high were both females who were VR‐naïve, while the only two participants whose interest decreased were both males who had used VR before. These differences, while small, may warrant future investigation. Most of the children (92%) had medium‐high support for the idea of similar VR events.
The study also revealed important lessons to improve the usability of the method. Participants reported weaknesses with the experience that were mainly of technical hardware origin, such as moderate wearing comfort, image blur and light reflections within the head‐mounted display (HMD). Considering the rapid technical development, this shortcoming should soon be eliminated with the newer generation of hardware.
One limitation of the study was that no ophthalmologic examination was performed before the experience in order to capture any errors in binocularity or refraction and relate the findings to the results. However, we believe that the results of these examinations would have only marginally influenced our findings. Another limitation was that the most recent generation of HMDs were not available at the time of the study as they would have provided a higher image resolution. Furthermore, for data traffic performance reasons, a tethered HMD version was used so that the freedom of movement could still have been restricted. However, a constant high data flow rate with 180 frames per second was allowed and the VR systems were usable for more than seven hours per day during three days without any interruption.
Conclusions
This study showed that an ophthalmological VR application was successfully accepted in children and young people. The digital VR environment was perceived as a positive and safe experience and is recommended as an interactive platform for the communication of diseases, such as retinal pathologies. As children frequently respond better to visuals, VR can represent a vivid tool in the explanation of the serious illness of a family member or themselves, or prepare them for medical interventions. Care should be taken to present relevant and appropriate medical VR models to children and young people.
Supporting information
Table S1. The number of respondents for each question on the demographics and experience survey and the virtual reality reactions survey.
Table S2 a. Free answers virtual reality reactions survey. The number of respondents for each question are shown.
Table S2 b. Free answers virtual reality reactions survey. The number of respondents for each question are shown.
Table S2 c. Free answers virtual reality reactions survey. The number of respondents for each question are shown.
Adnan Tufail received a portion of funding from the Department of Health’s NIHR Biomedical Research Centre for Ophthalmology at Moorfields Eye Hospital and UCL Institute of Ophthalmology, United Kingdom, and is a consultant for Heidelberg Engineering. Peter Maloca owns intellectual properties on speckle denoising. Peter Maloca and Pascal Hasler receive lecture fees from Heidelberg. Dr. Scholl is member of the Scientific Advisory Board of: Astellas Institute for Regenerative Medicine; Gensight Biologics; Ionis Pharmaceuticals, Inc.; Gyroscope Therapeutics Ltd.; Janssen Research & Development, LLC (Johnson & Johnson); and Pharma Research & Early Development (pRED) of F. Hoffmann‐La Roche Ltd; Novartis Pharma AG (CORE). Dr. Scholl is paid consultant of: Boehringer Ingelheim Pharma GmbH & Co; Gerson Lehrman Group; and Guidepoint. Dr. Scholl is member of the Data Monitoring and Safety Board/Committee of Belite Bio and ReNeuron Group Plc/Ora Inc. and member of the Steering Committee of Novo Nordisk (FOCUS trial). Dr. Scholl is co‐director of the Institute of Molecular and Clinical Ophthalmology Basel (IOB) which is constituted as a non‐profit foundation and receives funding from the University of Basel, the University Hospital Basel, Novartis, and the government of Basel‐Stadt. These arrangements have been reviewed and approved by the University of Basel (Universitätsspital Basel, USB) in accordance with its conflict of interest policies.
Dr. Scholl is principal investigator of grants at the USB sponsored by the following entities: IVERIC bio (Ophthotech Corporation); Kinarus AG; and Novartis Pharma AG. Grants at USB are negotiated and administered by the institution (USB) which receives them on its proper accounts. Philippe C Cattin is the owner of the described method and his work has been funded by the Werner Siemens Foundation through the MIRACLE project. Others: none.
All data relevant to the study are included in the article.
The authors thank the individuals and their teachers, the Zurich Film Festival, especially Nadja Schildknecht and Karl Spoerri, the Swiss National Science Foundation (SNSF), the University of Zurich (UZH), Swiss Federal Institute of Technology (ETH) and Life Science Zurich for the valuable support. The authors thank Jolanda Burri for her data curation.
Peter M. Maloca and Emily A. Williams have contributed equally to this study
References
- Araiza‐Alba P, Keane T, Matthews B, Simpson K, Strugnell G, Chen WS & Kaufman J (2021): The potential of 360‐degree virtual reality videos to teach water‐safety skills to children. Comput Educ 163: 104096. [Google Scholar]
- Bos JE, van Leeuwen RB & Bruintjes TD (2018): Motion sickness in motion: from carsickness to cybersickness. Ned Tijdschr Geneeskd 162: D1760. [PubMed] [Google Scholar]
- Cheung CMG, Arnold JJ, Holz FG et al. (2017): Myopic choroidal neovascularization: review, guidance, and consensus statement on management. Ophthalmology 124: 1690–1711. [DOI] [PubMed] [Google Scholar]
- Cooper J & Tkatchenko AV (2018): A Review of current concepts of the etiology and treatment of myopia. Eye Contact Lens 44: 231–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolgin E (2015): The myopia boom. Nature 519: 276–278. [DOI] [PubMed] [Google Scholar]
- Eijlers R, Utens E, Staals LM et al. (2019): Systematic review and meta‐analysis of virtual reality in pediatrics: effects on pain and anxiety. Anesth Analg 129: 1344–1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Failo A, Beals‐Erickson SE & Venuti P (2018): Coping strategies and emotional well‐being in children with disease‐related pain. J Child Health Care 22: 84–96. [DOI] [PubMed] [Google Scholar]
- Fujimoto J & Huang D. (2016): Foreword: 25 years of optical coherence tomography. Invest Opthalmol Vis Sci 57: OCTi–OCTii. [DOI] [PubMed] [Google Scholar]
- Hosokawa R & Katsura T (2018): Association between mobile technology use and child adjustment in early elementary school age. PLoS One 13: e0199959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang D, Swanson EA, Lin CP et al. (1991): Optical coherence tomography. Science (New York, N.Y.) 254: 1178‐1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy RSDJ, Compton DE, Stanney KM, Lanham S & Harm DL. (2001): Configural scoring of simulator sickness, cybersickness and space adaptation syndrome: similarities and differences? NASA Johnson Space Center 2001.
- Kersting M, Steier R & Venville G (2020): Exploring participant engagement during an astrophysics virtual reality experience at a science festival. Int J Sci Educ Part B 11(1): 17–34. 10.1080/21548455.2020.1857458 [DOI] [Google Scholar]
- Kim HK, Park J, Choi Y & Choe M (2018): Virtual reality sickness questionnaire (VRSQ): Motion sickness measurement index in a virtual reality environment. Appl Ergonom 69: 66–73. [DOI] [PubMed] [Google Scholar]
- Kyaw BM, Saxena N, Posadzki P et al. (2019): Virtual reality for health professions education: systematic review and meta‐analysis by the digital health education collaboration. J Med Intern Res 21: e12959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorenzo‐Alvarez R, Rudolphi‐Solero T, Ruiz‐Gomez MJ & Sendra‐Portero F (2019): Medical student education for abdominal radiographs in a 3D virtual classroom versus traditional classroom: a randomized controlled trial. AJR Am J Roentgenol 213: 644–650. [DOI] [PubMed] [Google Scholar]
- Maloca PM, de Carvalho JER, Heeren T et al. (2018): High‐performance virtual reality volume rendering of original optical coherence tomography point‐cloud data enhanced with real‐time ray casting. Transl Vis Sci Technol 7: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohno‐Matsui K, Lai TY, Lai CC & Cheung CM (2016): Updates of pathologic myopia. Prog Retinal Eye Res 52: 156–187. [DOI] [PubMed] [Google Scholar]
- Parsons TD, Bowerly T, Buckwalter JG & Rizzo AA (2007): A controlled clinical comparison of attention performance in children with ADHD in a virtual reality classroom compared to standard neuropsychological methods. Child Neuropsychol 13: 363–381. [DOI] [PubMed] [Google Scholar]
- Phillips AW, Reddy S & Durning SJ (2016): Improving response rates and evaluating nonresponse bias in surveys: AMEE Guide No. 102. Med Teach 38: 217–228. [DOI] [PubMed] [Google Scholar]
- Sattar MU, Palaniappan S, Lokman A, Hassan A, Shah N & Riaz Z (2019): Effects of Virtual Reality training on medical students' learning motivation and competency. Pakistan J Med Sci 35: 852–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein A, Dalton L, Rapa E et al. (2019): Communication with children and adolescents about the diagnosis of their own life‐threatening condition. Lancet (London, England) 393: 1150–1163. [DOI] [PubMed] [Google Scholar]
- Stratos A, Loukas R, Dimitris M, Konstantinos G, Dimitris M & George C (2016): A virtual reality application to attract young talents to manufacturing. Proc CIRP 57: 134–139. [Google Scholar]
- Tychsen L & Foeller P (2020): Effects of immersive virtual reality headset viewing on young children: visuomotor function, postural stability, and motion sickness. Am J Ophthalmol 209: 151–159. [DOI] [PubMed] [Google Scholar]
- Yam JC, Tang SM, Kam KW et al. (2020): High prevalence of myopia in children and their parents in Hong Kong Chinese Population: the Hong Kong Children Eye Study. Acta Ophthalmol 98: e639–e648. [DOI] [PubMed] [Google Scholar]
- Zha N, Alabousi M, Katz DS, Su J & Patlas M (2019): Factors affecting response rates in medical imaging survey studies. Acad Radiol 27: 421–427. [DOI] [PubMed] [Google Scholar]
- Zimmerman H, Land S & Jung YJ (2016): Using augmented reality to support ChildreŽ s situational interest and science learning during context‐sensitive informal mobile learning. Adv Intelligent Syst Comput 406: 101–119. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. The number of respondents for each question on the demographics and experience survey and the virtual reality reactions survey.
Table S2 a. Free answers virtual reality reactions survey. The number of respondents for each question are shown.
Table S2 b. Free answers virtual reality reactions survey. The number of respondents for each question are shown.
Table S2 c. Free answers virtual reality reactions survey. The number of respondents for each question are shown.


