Abstract
Studies on the psychosocial and emotional burden of psoriasis have been extensive; however, there is limited knowledge and awareness of patients’ attitude and behavior towards psoriasis treatment. To understand psoriasis patients’ attitude and behavior towards treatment of psoriasis, especially those treated with biologics, a multi‐stage study qualitative and quantitative methodology was conducted among psoriasis patients. An online survey was conducted with 45 moderate‐to‐severe psoriasis patients each in Australia, Japan, South Korea, and Taiwan for 20 min. This was followed by qualitative in‐depth interviews conducted among psoriasis patients in Australia (n = 3) and Japan (n = 2) for 60 min. All of the findings were workshopped with key opinion leaders and patient advisory groups to identify potential solutions addressing patients’ unmet needs. Five common insights were identified across the region, highlighting patients’ attitude and behavior towards psoriasis treatment, especially for those treated with biologics. These insights comprised the following: (i) one of the key factors driving patients’ treatment choice included their ability to enjoy clear skin for longer period (68%); (ii) bio‐maintenance patients had a higher expectation (4.9 months) of how long their skin could stay clear, compared to their pre‐biologics initiation days (2.9 months); (iii) once a good response is achieved, bio‐maintenance patients were more concerned about symptoms returning (44%) than development of side‐effects (19%); (iv) bio‐maintenance patients felt psychologically and physically affected during flare‐ups despite being on more efficacious treatment; and (v) bio‐maintenance patients still felt they were at risk of flare‐ups (4.5/7), almost similar risk perception as non‐biologics patients (4.9/7). Findings from this study showed that psoriasis patients look for treatment with the least risk of flare‐ups so that they were able to enjoy clear skin for a long time.
Keywords: biologics, flare‐ups, psoriasis, psoriasis treatment, quality of life
1. INTRODUCTION
Psoriasis is a chronic, immune‐mediated inflammatory skin disease. It affects approximately 2–3% of the population worldwide, with an estimated prevalence of 2.3–6.6% in Australia, 0.34% in Japan, 0.24% in Taiwan, and 0.45% in South Korea. 1 , 2 , 3 , 4
A systematic literature review evaluating the disease burden and quality of life (QoL) of psoriasis in the Asia‐Pacific showed that psoriasis had adverse effects on patients’ QoL. Patients also suffered from anxiety, stress, and depression. 5 , 6 An Asian consensus study highlighted that this burden could be higher in Asia because of cultural reasons and higher levels of social stigma and discrimination due to misconceptions. 7
Resolution of clinical lesions and symptoms is an important feature of an ideal therapy for psoriasis. Although clinicians consider that management of moderate‐to‐severe psoriasis requires systemic biologics or non‐biologics, 8 , 9 many patients are dissatisfied with their therapy. 10 This is mainly due to patients considering their disease as more severe and requiring more intense treatment as minimal disease still affects their QoL. 11 , 12
Increasing knowledge of immunopathogenic pathways of psoriasis has resulted in the development of biologics targeting specific molecular targets such as blockers of tumor necrosis factor‐α, interleukin (IL)‐12/IL‐23 inhibitors, and IL‐17A inhibitors. 13 These biologics have revolutionized moderate‐to‐severe psoriasis treatment with their rapidity of onset, long‐term efficacy, safety profile, and effects on comorbidities. 14
Despite the current literature available on the psychosocial and emotional burden of psoriasis, there is limited knowledge and awareness of patients’ attitude and behavior towards psoriasis treatment, especially those treated with biologics.
Therefore, the primary objective of this study was to uncover the perceptions and attitudes of patients living with psoriasis, especially those treated with biologics (bio‐maintenance). We also aimed to understand psoriasis patients’ anxiety surrounding their treatment experience (such as biologics), as well as their perception of risks and impact on QoL. This study was conducted in Japan, Australia, South Korea, and Taiwan. This knowledge will broadly help communicate to the medical community the emotional and psychosocial burden patients face, through an understanding of their plights based on the narratives of their experiences of living with psoriasis.
2. METHODS
A multi‐stage design comprising both quantitative and qualitative methodologies was conducted. Given it was a multi‐country study and the nature of the study, the protocol and the questionnaire were determined exempted by the Pearl Institutional Review Board in accordance with US Food and Drug Administration 21 CFR 56.104 and DHHS 45 CFR 46.104 regulations. All respondents provided informed consent.
The Behavior Change Wheel is an evidence‐based framework to understand behavior and comprises of three layers and at the hub of the wheel are the COM‐B dimensions. It was developed from 19 frameworks of Behavioral change identified in academic literature and arrived at by a consensus by behavioral theorists. It has been applied extensively in identifying and understanding effective methods of changing a range of health‐related behaviors. 15 There are interactions between three components Capability, Opportunity, and Motivation (“COM”) contributing to Behavior (“B”). Capability includes both psychological (knowledge) and physical (strength, skills) aspects, Opportunity entails both social and physical or environmental influences and Motivation encompasses both automatic (emotion, impulses) or reflective aspects (beliefs and intentions). The COM‐B framework was applied in the design of the research questions and analysis to understand the Capability, Opportunity, and Motivation towards flare‐ups among psoriasis patients and to identify the behavioral gaps.
2.1. Phase 1: Quantitative methodology
2.1.1. Study design and participants
Potential psoriasis patients were recruited through an existing Web‐based consumer panel (Kantar Profiles or Medilead) via opt‐in email, co‐registration with panel partners, e‐newsletter campaigns, banner placements, physician referrals, or internal and external affiliate networks. The inclusion criteria of eligible psoriasis patients include (i) aged 18 years and older; (ii) residing in Australia, Japan, South Korea, or Taiwan; (iii) self‐reported physician diagnosis of psoriasis; (iv) currently receiving treatment for psoriasis; (v) experienced at least one flare‐up in the past 12 months; and (vi) do not have tuberculosis, hepatitis B or C.
A 20‐min online survey was conducted with 45 moderate‐to‐severe psoriasis patients each in Australia, Japan, South Korea, and Taiwan (total sample size = 180). All participants explicitly agreed to join the panel and provided online informed consent to participate in the study. The participants completed the survey in either English, Japanese, Korean, or Traditional Chinese.
Patients were further split into two categories (i) bio‐maintenance patients; and (ii) non‐biologic patients (bio‐naïve/stop patients). The inclusion criteria for both these categories are highlighted in Table S1. The total number of patients recruited under bio‐maintenance patients and non‐biologic patients’ categories are mentioned in Table 1.
TABLE 1.
Total number of psoriasis patients recruited in the quantitative survey
| Bio‐maintenance patients | Non‐biologics patients | |
|---|---|---|
| Australia | 29 | 16 |
| Japan | 24 | 21 |
| South Korea | 30 | 15 |
| Taiwan | 37 | 8 |
| Total | 120 | 60 |
2.1.2. Statistical analysis
The data from the quantitative survey was descriptive in nature with proportion/percentage or average being reported. Paired t‐test was also used to determine if there was a mean difference between the number of months of clear skin before and after biologics.
2.2. Phase 2: Qualitative in‐depth interviews
To gain a narrative around psoriasis patients’ experience, qualitative telephonic, or Web‐based in‐depth interviews were conducted in Australia (n = 3) and Japan (n = 2) for 60 min. For Japan, the respondents were contacted by Medilead’s health‐care panel (Web‐based) to obtain their permission to participate. A similar approach was taken for recruitment of psoriasis patients from Australia, except the panel used to recruit these respondents was the Kantar Profiles panel.
The inclusion criteria of the patients in the qualitative phase were similar to the bio‐maintenance patients in the quantitative phase. All of the patients provided informed consent prior to participating.
2.3. Phase 3: Advisory board
Findings from phase 1 and 2 were workshopped with key opinion leaders (KOL)/experts and patient advisory groups (PAG) to identify potential solutions addressing the unmet needs of psoriasis patients (Tables S2 and S3). In addition to the PAG in the key regions of interest (Australia, Japan, South Korea, and Taiwan), PAG from Mainland China, Hong Kong, and Singapore also participated in the advisory board meeting for knowledge and experience sharing on the key survey insights in comparison to their respective regions.
3. RESULTS
3.1. One of the key factors driving psoriasis patients’ treatment choice includes the need to have clear skin for a long period of time
Across the region, 68% of psoriasis patients emphasized having clear skin for a longer period as a key driver of treatment choice for psoriasis. This was followed by fast skin clearance (54%), safety (54%), and doctor’s recommendation (45%) (Figure 1a). The highest proportion of patients who considered having clear skin for a long period of time as a key factor were from Japan (80%), and the lowest from Australia (47%) (Figure 1a). Additionally, having clear skin was a key driver of treatment choice for both non‐biologics (62%) and bio‐maintenance patients (70%) (Figure 1b).
FIGURE 1.
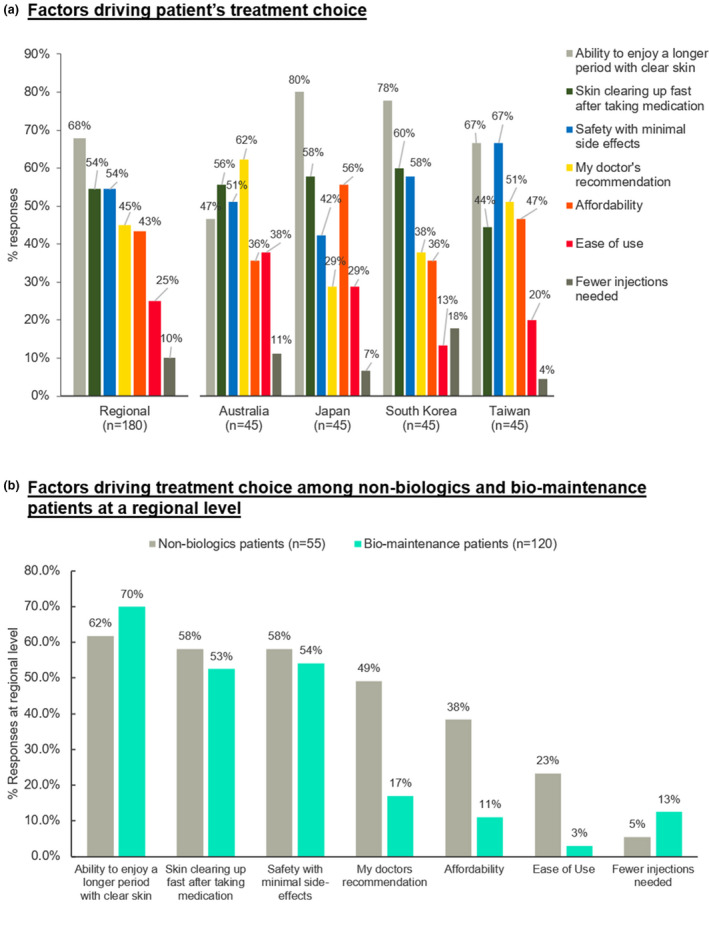
Factors considered within the top three drivers by all psoriasis patients in influencing treatment choice in the region. (a) Factors driving patients’ treatment choice. (b) Factors driving treatment choice among non‐biologics and bio‐maintenance at a regional level
An Australian patient mentioned, “[after biologics] it was clear within a few months and it has been clear for the last year…I am happy now and I can see my future continuing to be happy. If I can get 3–4 years of being clear, I’ll be incredibly happy.” They also highlighted the potential need for PAG support to deal with flare‐ups and achieve clear skin, where a patient said, “I would like to minimize my flare‐ups further and if possible, stay clear for entire life. I am hopeful to be able to do so with the support of my dermatologist, parents and information sharing through patient advocacy group.”
3.2. Bio‐maintenance patients have higher expectation of how long their skin can stay clear compared to pre‐biologics initiation days
Across the region, patients on biologics (bio‐maintenance) expected their skin to be clear for 4.9 months on average, compared to their expectation of 2.9 months in their pre‐biologic initiation days (p = 0.012). This expectation was highest in Australia (5.8 months), followed by Taiwan (5 months), South Korea (4.4 months), and Japan (4.2 months) (Table 2). This higher expectation on duration of clear skin was based on patients’ experience with biologics. For example, a patient from Japan stated that “Since the biologic shots, I don’t have the condition of skin peeling off anymore. If possible, I want the effect to last forever.” Additionally, an Australian patient on biologics said, “after biologics injection, I would like to be clear longer”.
TABLE 2.
Expected duration of clear skin before and after biologics: regional and national level overview
| Number of months | Regional (n = 120) | Australia b (n = 29) | Japan b (n = 24) | South Korea (n = 30) | Taiwan (n = 37) |
|---|---|---|---|---|---|
| Before biologics | 2.9 | 0.9 a | 2.4 | 3.5 | 4.5 a |
| After biologics | 4.9 | 5.8 a | 4.2 | 4.4 | 5.0 a |
Outliers (one in Australia and four in Taiwan) with “indefinite” expectation of clear skin (>99 months) were removed from average calculation.
Small sample size.
3.3. When a flare develops, patients approached them in different ways depending on the region
When psoriasis patients encountered flare‐ups, patients visited the doctor straightaway in Japan and South Korea (49%). In Taiwan, the majority of the patients self‐managed at first but visited the doctor when they did not get better (40%) or visited the doctor straightaway (38%). Australian patients had a very different behavior with 38% of them self‐managing the flare and not visiting a doctor. Only 4% of Australian patients visited the doctor straightaway (Figure 2).
FIGURE 2.
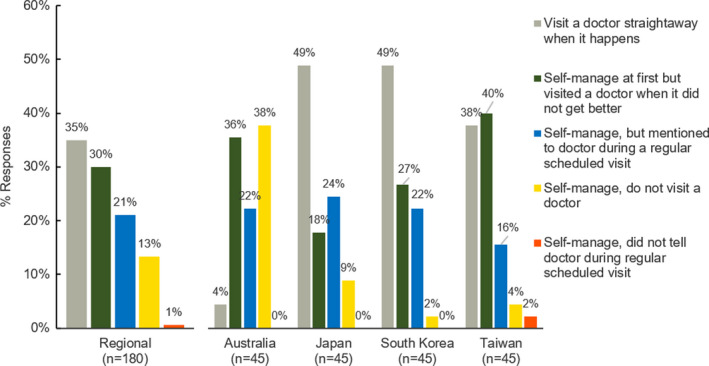
Ways of managing flare‐ups by psoriasis patients when they encounter them: a regional and national level overview
3.4. Once good response is achieved, bio‐maintenance patients are more concerned about symptoms returning than the development of side‐effects
Across the region, 44% of bio‐maintenance patients were anxious about the return of their symptoms such as flare‐ups when they had clear or almost clear skin. The concern regarding the return of their symptoms was highest in Taiwan (49%), followed by Australia (48%), South Korea (43%), and Japan (33%) (Figure 3a). An Australian patient on biologics said, “I am now worried that flare‐ups might return if I am not able to continue with the treatment in future”.
FIGURE 3.
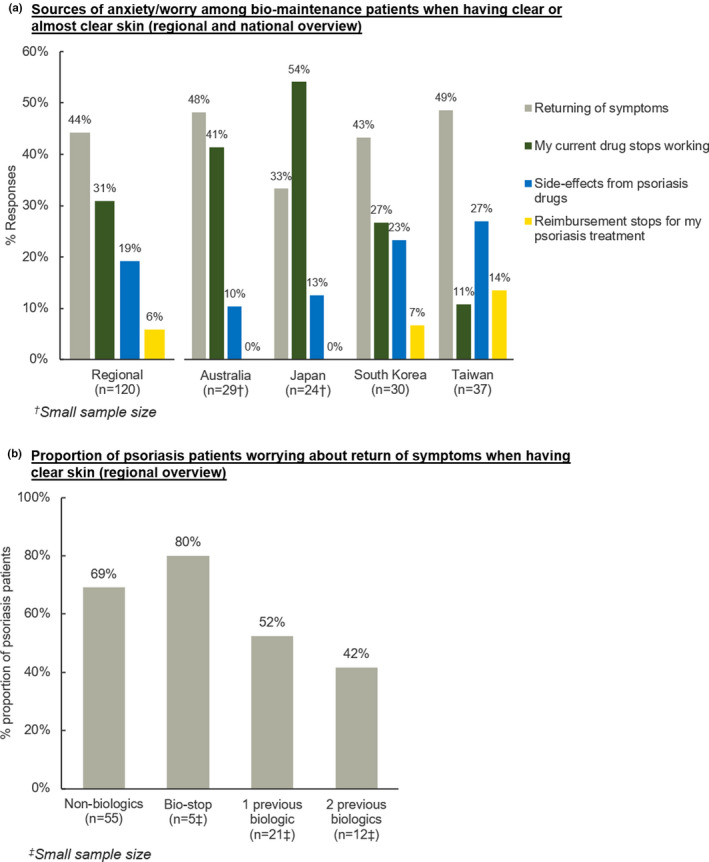
Psoriasis patients’ concerns when having clear skin. (a) Sources of anxiety/worry among bio‐maintenance patients when having clear or almost clear skin (regional and national overview). (b) Proportion of psoriasis patients worrying about return of symptoms when having clear skin (regional overview)
Besides the worry about return of symptoms or the worry that their current drug would stop working, another source of anxiety included side‐effects from drugs across the region (19%), with Taiwan having the highest proportion of patients who expressed this concern (27%) (Figure 3a).
This concern of returning symptoms was higher among non‐biologic patients (69%) and those who had stopped taking biologics (80%). It was also the greatest worry among bio‐maintenance patients who previously failed one previous biologic (52%) and two previous biologics (42%) (Figure 3b).
3.5. Bio‐maintenance patients also reportedly felt psychologically and physically affected during flare‐ups despite being on a more efficacious treatment
Across the region, the top three impacts from flare‐ups described by bio‐maintenance patients included loss of confidence (29%) and feeling sad or moody (26%) as well as feeling pain (26%) (Figure 4a).
FIGURE 4.
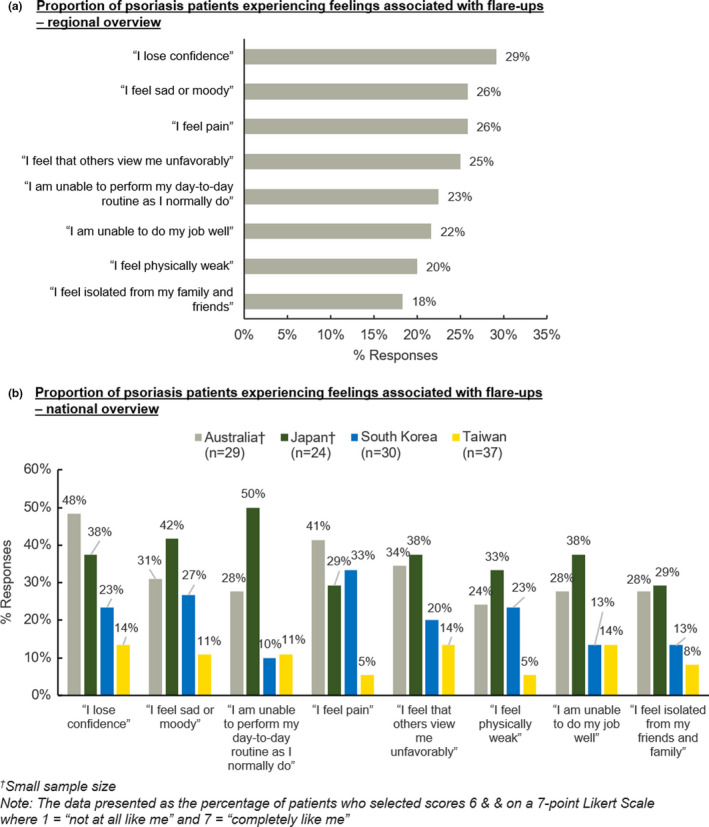
Feelings perceived by psoriasis patients when they experienced flare‐ups. (a) Proportion of psoriasis patients experiencing feelings associated with flare‐ups: regional overview. (b) Proportion of psoriasis patients experiencing feelings associated with flare‐ups: national overview. †Small sample size. The data presented as the percentage of patients who selected score 6 and on a 7‐point Likert scale where 1 was “not at all like me” and 7 “completely like me”
At least four in 10 bio‐maintenance patients in Australia reported losing confidence (48%) and feeling pain (41%) (Figure 4b). An Australian patient mentioned, “I feel like screaming. My friends will not understand me because they have not been through flare‐ups except for my mom. It’s not just the physical pain I am feeling but my heart too”.
In Japan, 50% of patients mentioned that due to psoriasis they were unable to perform their day‐to‐day activities normally (Figure 4b). A Japanese patient said, “I think one of the biggest problems is the difficulty in working and it’s what other people with psoriasis are equally suffering from as well. There’s no guarantee that people at work would understand the symptoms.”
Additionally, 33% of bio‐maintenance patients in South Korea felt physical pain, while 14% of Taiwanese patients felt that others viewed them unfavorably and were unable to perform their job well (Figure 4b).
3.6. Bio‐maintenance patients still felt that they were at moderate risk of flare‐ups, almost similar risk perception as non‐biologics patients, despite being on more effective treatment
Across the region, despite being on effective treatment, bio‐maintenance patients rated themselves with moderate risk of flare‐ups on a scale rating (4.5/7), similarly to non‐biologics patients (4.9/7). Bio‐maintenance patients in Taiwan rated themselves higher in the risk of flare‐ups compared to non‐biologics patients (4.5 vs 3.9 respectively) (Table S4).
3.7. Advisory board meeting highlighted the need for more education on psoriasis and tools to facilitate share decision‐making and flare‐up anxiety
The key findings of the quantitative survey were shared with the expert panel of the advisory board. The panel reconvened and the following recommendations were made to better equip the patients to manage flare‐ups in the future. The advisory board recommended to educate patients on psoriasis, on avoidance of its triggers and stressors, and importantly how to best manage flare‐ups. The advisory board also suggested that depending on the patient’s experience with psoriasis and their health literacy, information could be provided through different media such as visual booklets, YouTube videos, or well‐represented Web‐based information.
4. DISCUSSION
The qualitative and quantitative phases confirmed that the key factor driving psoriasis patients’ treatment choice across the region was the need to have clear/almost clear skin. A discrete choice study in the USA with 300 moderate‐to‐severe psoriasis patients also revealed that clear skin was the key driver of their treatment choices. 16 Additionally, Smith et al. 17 showed that the most common reason for a treatment change in psoriasis patients has been poor control or flare‐ups of psoriasis, highlighting the importance of having clear skin among psoriasis patients.
The current study findings were shared with the experts and they echoed the need to reflect on what patients want from psoriasis treatment which, based on current and previous studies, was the need to have clear skin and persistent control of flare‐ups. Thus, there is a need for physicians to be aware of patient preferences in treatment of psoriasis and their drivers for treatment choice due to its impact on their physical and psychological wellbeing. Furthermore, given the unmet need to have persistent control of flare‐ups among psoriasis patients, physicians could potentially choose advanced therapies which could provide least risk of flare‐ups. 18
While patients across the region expressed a desire for persistent control of flare‐ups, their expectations on the duration of biologics’ ability to have persistent control of flare‐ups varied by region. The expectation of how long patients could have clear skin was higher among bio‐maintenance patients compared to non‐biologics patients. This expectation was the highest in Australia, followed by Taiwan, South Korea, and Japan. As highlighted by an expert from Australia, one potential reason for higher expectation on duration of clear skin could be that most Australian patients were knowledgeable about biologics and expected good efficacy.
In addition, experts from South Korea and Taiwan highlighted that psoriasis patients had to go through a tedious course of conventional (non‐biologics) therapies to qualify for the reimbursement criteria for biologics. This was also applicable to Australia and Japan.
The reimbursement criteria differ by region. In Australia, patients should have failed standard courses of non‐biological systemic therapy and/or phototherapy. 19 In Taiwan, patients for biologics are those who had failed, were intolerant of or contraindicated to two out of three conventional systemic agents and phototherapy, each for 12 weeks. 20 In South Korea, biologics reimbursement guidelines limit the prescription of biologics to patients who failed phototherapy for 3 months or oral therapeutic agents for 3 months. 21
Thus, the lengthy process to access biologics across regions could be an explanation for higher expectation of duration of clear skin compared to non‐biologics. Regional differences may also explain why Australians rarely visited their doctors straightaway and tended to self‐manage flares, while this was the reverse in other regions.
When psoriasis patients had clear skin, they had anxiety about flare‐ups or relapse of the disease. Interestingly, the fear of symptoms returning or drugs stopping working were higher than the anxiety about side‐effects from the treatments. Also, bio‐maintenance patients reported to be anxious of return of their flare‐ups even when they had clear or almost clear skin. This concern was highest in Taiwan, and Taiwan’s biologics reimbursement policy was highlighted as a possible explanation by a panel expert.
In Taiwan, psoriasis patients need to stop biologics after 2 years even if their symptoms were well‐controlled during the time period. This reimbursement limitation could potentially be associated with bio‐maintenance patients’ anxiety of return of symptoms even if they have clear or almost clear skin. This limitation could also be potentially associated with Taiwanese bio‐maintenance patients rating themselves higher in the risk of flare‐ups as compared to non‐biologics patients in contrast to other regions.
Across the region, bio‐maintenance patients who were affected by flare‐ups also felt physical pain, loss of confidence, sad or moody, and that others viewed them unfavorably. The highest proportion of psoriasis patients in Australia felt pain and loss of confidence in themselves. A survey by the “Get Psorted Get Connected” peer‐support program also showed that 81% of respondents felt embarrassed, 75% unattractive, and 54% depressed. 22
In Japan, the majority of patients with flare‐ups highlighted that it impacted their daily activities, thereby decreasing their quality of life. A study by Mabuchi et al. 23 showed that psoriasis impacted the QoL of patients in Japan.
The majority of patients in South Korea felt physical pain with flare‐ups. The bio‐maintenance patients in Taiwan suggested that flare‐ups resulted in loss of confidence, that others viewed them unfavorably, and were also unable to perform their job well. Thus, psoriasis patients experienced anxiety related to their symptoms and this was true even for bio‐maintenance patients who might have higher expectations for clear skin compared to non‐biologic users. Hence, psoriasis symptoms severely impacted psoriasis patients’ psychosocial wellbeing even among bio‐maintenance patients.
The advisory group, that included dermatologists and leaders of psoriasis patient advocacy groups, discussed that one way to address this unmet need was to start with patient education on psoriasis, how to manage its triggers, and importantly how to best manage flare‐ups and progress towards shared decision‐making. In shared decision‐making, patients’ perspectives and values would be considered in cooperation with health‐care professionals before making treatment decisions. There was also a need to make the physicians aware of the anxiety of the bio‐maintenance patients, addressing their expectations and working towards reducing patients’ anxiety levels.
One of the key limitations of this study was the definition of “flare‐ups” which was broader and patient‐reported rather than obtained clinically (Table S5). This study also did not address the difference between flare‐ups during the treatment or flare‐ups” after stopping the treatment.
Another limitation of this study was the relatively small sample size for both the quantitative and qualitative phases of the study as well as patient recruitment based on a predetermined set of characteristics to capture the perceptions of psoriasis patients. As this was a descriptive exploratory study that sought to provide foundation information on the emotional and psychosocial impacts among psoriasis patients, a formal sample size and power calculation was not performed. Thus, the sample was not standardized and might not be representative of the general population of psoriasis patients living in the regions where the study was conducted. Further research on a larger sample size including more detailed patient information would be warranted to further enhance the robustness of the knowledge in this area.
The findings obtained under the quantitative phase of the study was self‐reported and subjected to recall bias, and data validation could not be performed. Furthermore, as this study phase was conducted via a Web‐based survey, psoriasis patients without access to the Internet or comfortable with online administration could be underrepresented.
Although this study highlighted how some shared decision‐making tools could help address psoriasis patients’ unmet needs, there was a need to conduct prospective validation studies in the future; wherein one could measure how the different shared decision‐making tools could help address psoriasis patients unmet needs, such as the need for persistent control of flare‐ups or reduce bio‐maintenance patients’ anxiety towards flare‐ups or discuss with patients which treatment modality they could choose to control the flare‐ups or prevent the triggers.
Findings from this study show that psoriasis patients sought treatment with the least risk of flare‐ups so that they would be able to enjoy clear skin for longer periods of time. Even when they started advanced therapies such as biologics, their anxiety and fear of flare‐ups persisted, and as a source of anxiety was higher than the fear of side‐effects. Two potential ways highlighted by the advisory board to alleviate these fears included education and shared decision‐making.
In the future, insights on the attitudes and behavioral barriers among psoriasis patients, through the COM‐B framework, could be brought into a Behavior Change workshop to design bespoke interventions to address behavioral barriers that will help physicians to manage patients optimally.
CONFLICT OF INTEREST
Kantar Health received funding from Janssen Asia‐Pacific for the conduct of the study and development of the manuscript. B.W. and B.Y.L. are employees of Janssen Asia‐Pacific. R.G. is an employee of Kantar Health. P.F.P. reports involvement in clinical trials or has served as part of an advisory committee and/or speaker for AstraZeneca, Galderma, Dermira, Boehringer Ingelheim, Pfizer, CSL, OncoSec, Eli Lilly, UCB, Abbvie, BMS, Eisai, miRagen, Regeneron, Sun Pharma, Novartis, Leo, Janssen, Arena, Roche, Xoma, Kyowa Hakko Kirin, GSK, Amgen, Sanofi, Merch, La Roche Posay, Avene, Celgene, and Schering Plough. Y.H.H. has conducted clinical trials while serving as a principal investigator for Galderma, Eli‐Lilly, Novartis Pharmaceuticals, and Janssen‐Cilag Pharmaceuticals; received honoraria for serving as an advisory board member for Pfizer Limited, AbbVie, and Celgene; and received speaking fees from AbbVie, Eli‐Lilly, and Novartis Pharmaceuticals Corporation. Y.T. has been a consultant, scientific adviser, investigator, and/or speaker for AbbVie, Boehringer‐Ingelheim, Amgen, Eisai, Eli Lilly and Company, Janssen, Kyowa Kirin, LEO Pharma, Maruho, Meiji Seika Pharma, UCB, Sun Pharma, Mitsubishi Tanabe Pharma, Novartis, Torii Pharmaceutical, and Taiho Pharmaceutical. The remaining authors declare no competing interests.
Supporting information
Supplementary Material
ACKNOWLEDGMENTS
The authors acknowledge the support provided by Dr. Shikha Singh, from Kantar Health who helped to develop the manuscript and support for this assistance was funded by Janssen Asia‐Pacific. This study was funded by Janssen Asia‐Pacific.
Tada Y, Jo SJ, Huang Y‐H, Wahking B, Lee BY, Gowindah R, et al. Uncovering the unmet needs among psoriasis patients in the Asia‐Pacific region. J Dermatol. 2021;48:1665–1674. 10.1111/1346-8138.16072
REFERENCES
- 1. Kubota K, Kamijima Y, Sato T, Ooba N, Koide D, Iizuka H, et al. Epidemiology of psoriasis and palmoplantar pustulosis: a nationwide study using the Japanese national claims database. BMJ Open. 2015;5:e006450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chiu H‐Y, Wang T‐S, Chen P‐H, Hsu S‐H, Tsai Y‐C, Tsai T‐F. Psoriasis in Taiwan: From epidemiology to new treatments ‐ ScienceDirect. Dermatol Sin. 2018;36:115–23. [Google Scholar]
- 3. Parisi R, Symmons DPM, Griffiths CEM, Ashcroft DM. Global epidemiology of psoriasis: a systematic review of incidence and prevalence. J Invest Dermatol. 2013;133:377–85. [DOI] [PubMed] [Google Scholar]
- 4. Lee JY, Kang S, Park JS, Jo SJ. Prevalence of psoriasis in Korea: a population‐based epidemiological study using the Korean National Health Insurance Database. Ann Dermatol. 2017;29:761–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Schenkel B, Leartsakulpanitch J, Yue N. PSY1 burdens of psoriasis in the Asia pacific region: a literature review. Value Health. 2012;15:A677–8. [Google Scholar]
- 6. Ng CY, Yang Y‐W, Liu S‐H, Lu J‐F, Yang L‐C, Yang C‐H, et al. SF‐36 healty survey on psoriasis quality‐of‐life: a study of 414 Taiwanese patients. J Dermatol. 2015;42:159–65. [DOI] [PubMed] [Google Scholar]
- 7. Imafuku S, Zheng M, Tada Y, Zhang X, Theng C, Thevarajah S, et al. Asian consensus on assessment and management of mild to moderate plaque psoriasis with topical therapy. J Dermatol. 2018;45:805–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Johar A, Thevarajah S, Heng A, Chan LC, Ch’ng CC, Mohd Safdar NA, et al. Position statement on secukinumab in the management of plaque psoriasis: The Malaysian Perspective. Dermatol Res Pract. 2019;2019:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tsai T‐F, Lee C‐H, Huang Y‐H, Chi C‐C, Chang Y‐T, Wong T‐W, et al. Taiwanese Dermatological Association consensus statement on management of psoriasis. Dermatol Sin. 2017;35:66–77. [Google Scholar]
- 10. Armstrong AW, Robertson AD, Wu J, Schupp C, Lebwohl MG. Undertreatment, treatment trends, and treatment dissatisfaction among patients with psoriasis and psoriatic arthritis in the United States: findings from the National Psoriasis Foundation surveys, 2003–2011. JAMA Dermatol. 2013;149:1180–5. [DOI] [PubMed] [Google Scholar]
- 11. Krueger G, Koo J, Lebwohl M, Menter A, Stern RS, Rolstad T. The Impact of Psoriasis on Quality of Life: Results of a 1998 National Psoriasis Foundation Patient‐Membership Survey. Arch Dermatol. 2001;137:280–4. [PubMed] [Google Scholar]
- 12. Yang H‐J, Yang K‐C. Impact of psoriasis on quality of life in Taiwan. Dermatol Sin. 2015;33:146–50. [Google Scholar]
- 13. Vide J, Magina S. Moderate to severe psoriasis treatment challenges through the era of biological drugs. An Bras Dermatol. 2017;92:668–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Carrascosa J‐M, van Doorn MBA, Lahfa M, Nestle FO, Jullien D, Prinz JC. Clinical relevance of immunogenicity of biologics in psoriasis: implications for treatment strategies. J Eur Acad Dermatol Venereol. 2014;28:1424–30. [DOI] [PubMed] [Google Scholar]
- 15. Michie S, Atkins L, West R. The behaviour change wheel book ‐ a guide to designing interventions [Internet]. London: Silverback Publishing. [Google Scholar]
- 16. Poulos C, Gilloteau I, Guana A, et al. PSS68 the most influential drivers of psoriasis patients’ treatment choices: a discrete choice experiment survey in the US. Value Health. 2018;21(Supplement 3):S434–5. [Google Scholar]
- 17. Smith JA, Wehausen B, Richardson I, Zhao Y, Li Y, Herrera V, et al. Treatment changes in patients with moderate to severe psoriasis: a retrospective chart review. J Cutan Med Surg. 2018;22:25–30. [DOI] [PubMed] [Google Scholar]
- 18. Bahner JD, Cao LY, Korman NJ. Biologics in the management of psoriasis. Clin Cosmet Investig Dermatol. 2009;2:111–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Treatment goals for psoriasis: The Australian Psoriasis Treatment Goals Project [Internet]. [cited 2020 Aug 14]. https://www.dermcoll.edu.au/wp‐content/uploads/ACD‐Consensus‐Statement‐Treatment‐goals‐for‐psoriasis‐March‐2017.pdf
- 20. Huang Y‐W, Tsai T‐F. Remission duration and long‐term outcomes in patients with moderate‐to‐severe psoriasis treated by biologics or tofacitinib in controlled clinical trials: a 15‐year single‐center experience. Dermatol Ther. 2019;9:553–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ha D, Lee JY, Kim D, Oh I‐S, Lee E‐K, Shin J‐Y. Healthcare utilization and medical expenditure of Korean psoriasis patients. Medicine. 2018;97:e11070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Peer support program set to empower Australians affected by psoriasis [Internet]. Medianet. 2018. [cited 2020 Aug 14]. https://www.medianet.com.au/releases/168039/. Accessed 20 Jul 2020.
- 23. Mabuchi T, Yamaoka H, Kojima T, Ikoma N, Akasaka E, Ozawa A. Psoriasis affects patient’s quality of life more seriously in female than in male in Japan. Tokai J Exp Clin Med. 2012;37:84–8. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


