Abstract
Aim
To assess the beneficial and adverse effects on the dental and periodontal issues of periodontal–orthodontic treatment of teeth with pathological tooth flaring, drifting, and elongation in patients with severe periodontitis.
Materials and methods
Nine databases were searched in April 2020 for randomized/non‐randomized clinical studies. After duplicate study selection, data extraction, and risk‐of‐bias assessment, random‐effect meta‐analyses of mean differences (MDs) and their 95% confidence intervals (CIs) were performed, followed by subgroup/meta‐regression analyses.
Results
A total of 30 randomized and non‐randomized clinical studies including 914 patients (29.7% male; mean age 43.4 years) were identified. Orthodontic treatment of pathologically migrated teeth was associated with clinical attachment gain (−0.24 mm; seven studies), pocket probing depth reduction (−0.23 mm; seven studies), marginal bone gain (−0.36 mm; seven studies), and papilla height gain (−1.42 mm; two studies) without considerable adverse effects, while patient sex, gingival phenotype, baseline disease severity, interval between periodontal and orthodontic treatment, and orthodontic treatment duration affected the results. Greater marginal bone level gains were seen by additional circumferential fiberotomy (two studies; MD = –0.98 mm; 95% CI = –1.87 to −0.10 mm; p = .03), but the quality of evidence was low.
Conclusions
Limited evidence of poor quality indicates that orthodontic treatment might be associated with small improvements of periodontal parameters, which do not seem to affect prognosis, but more research is needed.
Keywords: clinical attachment level, orthodontic treatment, periodontal disease, pocket probing depth, systematic review
Clinical Relevance.
Scientific rationale for study: This systematic review aimed to analyse the effect of periodontal‐orthodontic treatment on the periodontal status of pathologically migrated teeth after severe periodontitis.
Principal findings: The included studies reported very small improvements in clinical attachment level, pocket probing depth, marginal bone level, and papilla height after treatment, with no considerable adverse effects in the short or long term. The effect of periodontal‐orthodontic treatment of pathologically migrated teeth on periodontal parameters was associated with the baseline characteristics of patients and treatment duration.
Practical implications: Periodontal‐orthodontic treatment for pathologically migrated teeth seems to have minimal positive effects on periodontal parameters and negligible adverse effects, but only limited evidence from small studies currently exists.
1. INTRODUCTION
1.1. Background
Severe periodontitis is the sixth most prevalent disease in the world (Kassebaum et al., 2014), with more than 700 million people across the world affected by it. Among the corollaries of severe periodontal disease, pathologic tooth migration holds a prominent place, as it is often seen to impair both function and aesthetics (Martinez‐Canut et al., 1997; Brunsvold, 2005) as well as to negatively influence the long‐term prognosis of teeth (Kwok & Caton, 2007). As per the current definition of periodontitis, a number of complexity factors—including bite collapse, drifting, and flaring—are accepted as having serious impact on the prognosis of the dentition and at the disease management level as well (Papapanou et al., 2018). In the past, it had been postulated that, as a result of pathological tooth migration, both occlusal trauma and periodontitis are aggravated, resulting eventually in greater loss of attachment, extrusion, and mobility of the displaced teeth (Serio & Hawley, 1999). There exists, indeed, evidence of a link between traumatic occlusal forces and attachment loss but not with non/carious cervical lesions and gingival recession (Jepsen et al., 2018). It is therefore reasonable that patients suffering from pathological tooth migration are often recommended by their dentist to seek orthodontic therapy (Brunsvold, 2005).
As more adults seek orthodontic treatment, orthodontists are seeing more patients with periodontal problems (McKiernan et al., 1992). Orthodontic treatment of periodontally healthy adolescent and adult patients has been linked to a mostly transient inflammatory process of the periodontium (Bollen et al., 2008; Freitas et al., 2014; Papageorgiou, Xavier, et al., 2018) and a minimal insult to the periodontal tissues (Bollen et al., 2008; Papageorgiou, Papadelli, & Eliades, 2018). At the same time, research indicates that a periodontally reduced but healthy periodontium can tolerate well orthodontic tooth movement with no additional treatment‐induced attachment loss (Ericsson et al., 1977; Wennström et al., 1987). This has also been confirmed immunologically, as orthodontic movement of periodontally compromised, inflammation‐free teeth was not followed by increase in parameters of tissue destruction such as matrix metalloproteinases (Almeida et al., 2015). Orthodontic correction of pathological malpositioned teeth can relieve occlusal trauma, stabilize the dentition, and improve the periodontal status (Diedrich, 1996; Weston et al., 2008; Gkantidis et al., 2010). However, the influence of intrusion of periodontally extruded teeth on periodontal tissues remains controversial (Boyd et al., 1989; Serio & Hawley, 1999; Weston et al., 2008). Recent studies have suggested that light intrusive forces can be used to correct pathological extrusion and migration (Garat et al., 2005; Ogihara & Wang, 2010). But many other issues might complicate the orthodontic treatment of a periodontal patient with pathologic tooth migration: for example, periodic periodontal maintenance, strength and direction of orthodontic force, and surveillance of periodontal status (Diedrich, 1996; Gkantidis et al., 2010). Therefore, it remains unclear whether orthodontic treatment can be safely performed on pathologically migrated teeth and what the short‐ and long‐term implications on the prognosis of the dentition are.
1.2. Objective
The aim of this systematic review was to critically assess the evidence derived from randomized and non‐randomized clinical studies on human patients with severe (stage IV) periodontitis undergoing orthodontic treatment to correct pathologically migrated teeth in terms of periodontal beneficial effects and adverse effects.
2. MATERIALS AND METHODS
2.1. Protocol development and focused question
This review's protocol was made a priori and registered in PROSPERO (CRD42019131589) with all post hoc changes transparently reported (Appendix 1). The conduct and reporting of this review is guided by the Cochrane Handbook (Higgins et al., 2020) and the PRISMA statement (Page et al., 2021), respectively. The focused question this review tried to answer is as follows: “What is the influence of periodontal–orthodontic treatment of pathologically migrated teeth in patients with severe periodontitis on the periodontal status?”
2.2. Eligibility criteria
Based on the Participants–Intervention–Comparison–Outcome–Study design schema, and as few randomized clinical trials (RCTs) exist on this matter, we included RCTs and non‐randomized clinical studies (S), on human patients of any age, sex, and ethnicity with severe (stage IV) periodontal disease burdened with additional complexity factors such as pathologically migrated teeth, posterior bite collapse, secondary occlusal trauma, drifting, and flaring (P), receiving comprehensive periodontal–orthodontic treatment (I), compared to no treatment or other treatment regimens (C), without any limitations on language, publication year, or status. The inclusion of non‐randomized studies was judged imperative due to the lack of randomized trials in order to identify the range of possible outcomes for severe (stage IV) periodontitis patients receiving periodontal–orthodontic treatment and as a means to identify patient‐ or treatment‐related factors. Excluded were non‐clinical studies, animal studies, case reports/series (defined as studies with less than 10 patients), and studies where periodontal disease was left untreated. The primary outcome (O) for this review was the clinical attachment level (CAL) gain during treatment. Secondary outcomes pertaining to both efficacy and safety included changes in tooth loss, change in pocket probing depth (PPD), marginal bone level (MBL), gingival profile (such as gingival recession and papilla conditions), tooth mobility, treatment outcomes (including stability), root resorption, and patient‐reported outcome measures (PROM).
2.3. Information sources and search
Eight electronic databases were searched without restrictions from inception to 15 April 2020 (Appendix 2), while open‐access databases specifically covering grey literature (Directory of Open Access Journals, Digital Dissertations, metaRegister of Controlled Trials, WHO, Google Scholar), and the reference/citation lists of included articles or existing systematic reviews were manually searched.
2.4. Study selection, data collection, and risk of bias
Two authors (Spyridon N. Papageorgiou and Georgios N. Antonoglou) screened the titles and/or abstracts of search hits to exclude obviously inappropriate studies, prior to checking their full texts. Any differences between the two reviewers were resolved by discussion with another author (Theodore Eliades).
Data from included studies were collected independently by two authors (Spyridon N. Papageorgiou and Georgios N. Antonoglou) with the same way to resolve discrepancies using pre‐defined/piloted forms covering (i) study characteristics (design, clinical setting, and country), (ii) patient characteristics (age, sex, and smoking), (iii) baseline disease characteristics (periodontal disease and pathologic tooth migration), (iv) treatment details (tissue regeneration, time between periodontal–orthodontic phases, any adjuncts used, and retention measures), and (v) outcome details (type of outcome and time of measurement).
The risk of bias (ROB) of randomized trials or non‐randomized comparative (multi‐group) clinical studies was assessed according to Cochrane guidelines with the RoB 2.0 (Sterne et al., 2019) and the ROBINS‐I (Risk Of Bias In Non‐randomised Studies of Interventions) tool (Sterne et al., 2016), respectively. The internal validity (with extension to the ROB) of single‐group cohort studies was assessed with a custom tool based on the ROBINS‐I tool and the Joanna Briggs Institute checklist for cohort studies (http://joannabriggs-webdev.org/research/critical-appraisal-tools.html). All studies were appraised independently by two authors (Spyridon N. Papageorgiou, Georgios N. Antonoglou), with any differences being resolved by a third author (Theodore Eliades).
2.5. Data analysis
An effort was made to extract or calculate missing data whenever possible (Appendix 1). As the outcome of periodontal–orthodontic treatment is bound to be affected by patient‐ and treatment‐related characteristics, a random‐effects model was a priori deemed appropriate to calculate the average distribution of true effects, based on clinical and statistical reasoning (Papageorgiou, 2014a), and a restricted maximum likelihood (REML) variance estimator with improved performance was used according to recent guidance (Langan et al., 2019).
The primary analysis was based on direct meta‐analyses from randomized trials and non‐randomized comparative (multi‐group) cohort studies using mean differences (MDs) for continuous outcomes or relative risks for binary outcomes and their corresponding 95% confidence intervals (CIs). For the secondary analysis, indirect meta‐analyses were performed with data from randomized trials and non‐randomized multi‐group cohort studies (using only arms pertaining to combined periodontal–orthodontic treatment), as well as non‐randomized single‐group cohort studies to calculate the average pooled effect of treatment on the various outcomes.
The extent and impact of between‐study heterogeneity was assessed by inspecting the forest plots and by calculating the τ 2 (absolute heterogeneity) or the I 2 statistics (relative heterogeneity). I 2 defines the proportion of total variability in the result explained by heterogeneity, and not chance, while the heterogeneity's direction (localization on the forest plot) and uncertainty around heterogeneity estimates (Higgins et al., 2003) was also considered. The 95% random‐effects predictive intervals were initially planned to incorporate observed heterogeneity, but could not be calculated (Appendix 1).
2.6. Additional analyses and ROB across studies
Possible sources of heterogeneity were a priori planned to be sought through several random‐effects subgroup analyses and random‐effects meta‐regression (both with the REML estimator) in meta‐analyses of at least five trials, but could ultimately be performed only partly because of incomplete data/reporting (Appendix 1) for patient age, sex, smoking, baseline disease severity, use of tissue regeneration, interval between periodontal–orthodontic treatment, duration of orthodontic treatment, and duration of post‐treatment follow‐up. Reporting biases (including the possibility of publication bias) were assessed with contour‐enhanced funnel plots and Egger's test for meta‐analyses with ≥7 studies.
The overall quality of meta‐evidence (i.e., the strength of clinical recommendations) from the direct analysis was rated using the Grades of Recommendations, Assessment, Development and Evaluation (GRADE) approach (Guyatt et al., 2011) following recent guidance on combining randomized with non‐randomized studies (Schünemann et al., 2019) and the summary‐of‐findings table format by Carrasco‐Labra et al. (2016). The produced forest plots were augmented with contours denoting the magnitude of the observed effects (Appendix 1) to assess heterogeneity, clinical relevance, and imprecision (Papageorgiou, 2014b).
Robustness of the results was checked for meta‐analyses of ≥5 studies with sensitivity analyses based on the inclusion of (i) comparative (multi‐group) versus single‐group cohort studies, (ii) prospective versus retrospective studies, and (iii) studies with adequate versus inadequate samples, with the cut‐off set at 20 patients/study. All analyses were run in Stata version 14.0 (StataCorp LP, College Station, TX) by one author (Spyridon N. Papageorgiou) and the dataset was openly provided (Papageorgiou, Antonoglou, et al., 2020). All p‐values were two‐sided with α = 5%, except for the test of between‐studies or between‐subgroups heterogeneity, where the α‐value was set as 10% (Ioannidis, 2008).
3. RESULTS
3.1. Study selection
A total of 2586 hits were retrieved by the literature database search, and another seven records were identified manually (Figure 1). After removing duplicates and eliminating non‐relevant reports by title/abstracts, 325 full‐text papers were checked against the eligibility criteria (Appendix 3). In the end, 33 publications pertaining to 30 unique studies were included in this review.
FIGURE 1.
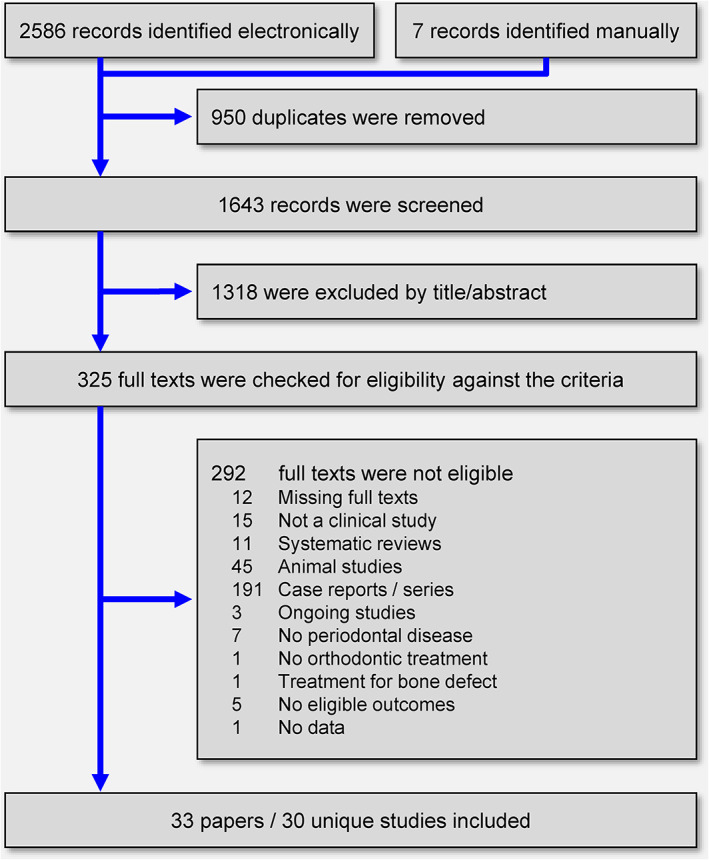
PRISMA flowchart for the identification and selection of eligible studies [Colour figure can be viewed at wileyonlinelibrary.com]
3.2. Characteristics of included studies
These included 30 studies were of various designs (Tables 1 and 2): 6 (20%) were RCTs (2 of parallel design and 4 of within‐person design), 6 (20%) were non‐randomized comparative (multi‐group) cohort studies (1 prospective, 2 retrospective, and 3 with unclear design), and 18 (60%) were non‐randomized single‐group cohort studies (5 prospective, 7 retrospective, and 6 with unclear design). Regarding the studies' setting, 17 (57%) were conducted in university clinics, 8 (27%) in private practices/clinics, 1 (3%) in a hospital, while 4 (13%) did not specify the setting. The included studies were conducted in 14 different countries (Brazil, China, Egypt, France, Hong Kong, Italy, South Korea, Lithuania, Norway, Poland, Sweden, and Thailand) and published as journal papers in English in 25 (83%) cases (2 being bilingual in English and Bosnian/French), 4 in Chinese, and 1 in Polish.
TABLE 1.
Characteristics of included randomized clinical trials and non‐randomized multi‐group comparative cohort studies
| Study | Design; setting; country a | Patients (M/F); age b ; smokers | Perio | PTM | Tx | Time | P‐OTx | OTx | Ret | Outcome c |
|---|---|---|---|---|---|---|---|---|---|---|
| Randomized studies | ||||||||||
| Attia et al. (2019) | RCTwp; Uni; EG | G1‐2: 15 (4/11); (25.0–37.0); 0% | SCP | Yes; BDef |
G1: PTx/GTR/OTx/Laser G2: PTx/GTR/OTx |
Pre‐PTx Mid‐OTx (6.0/9.0 months) |
NR | Misc. | NR | BMD/CAL/PPD |
| Liu et al. (2008) | RCTwp; Uni; CN | G1‐2: 21 (8/13); 32.3; NR | SCP | Yes |
G1: PTx/OTx/FiTo G2: PTx/OTx |
Pre‐PTx Post‐OTx |
7.0–14.0d | Misc. | Splint | CAL/MBL/Mobility/PPD/RL |
| Puttaravuttiporn (2018b) | RCTpa; Uni; TH | G1‐2: 36 (0/36); 42.3; 0% | NR | Yes |
G1: PTx/OTx/bite‐wafer G2: PTx/OTx |
Pre‐OTx Post‐OTx FU (1.0 & 7.0 months) |
NR | Misc | Splint | BMD/MBL/MBTh/Mobility/RL |
| Ren (2019) | RCTwp; Uni; HK | G1‐2: 27 (5/22); 47.0; 0% | SCP | Yes |
G1: PTx/OTx/Laser G2: PTx/OTx |
Pre‐OTx Mid‐OTx (up to 6.0 months) |
NR | Misc | NR | AEs/BF/CAL/Pain/PPD/REC |
| Shi et al. (2003) | RCTwp; Uni; CN | G1‐2: 16 (4/12); 36.6; NR | SCP | Yes |
G1: PTx/OTx/FiTo G2: PTx/OTx |
Pre‐PTx Post‐OTx |
NR | Misc (Intr) | NR | MBL |
| Zasciurinskiene et al. (2018, 2019) | RCTpa; Pract; LT |
G1: 25 (9/16); 47.3; 4% G2: 25 (6/19); 43.5; 4% |
SCP | Yes |
G1: PTx + OTx d G2: PTx/OTx d |
Pre‐PTx Post‐OTx (20.7 months) |
G1: 0 G2: >3 months |
Misc (Intr/Retr) | Splint & Plate | CAL/MBL/PPD/REC/RL |
| Non‐randomized multi‐group comparative cohort studies | ||||||||||
| Attia et al. (2012) | uNRS; Uni; EG | G1‐3: 15 (5/10); (25.0–48.0); 0% | SCP | Elongated/crowded |
G1: PTx/GTR/OTx G2: PTx/GTR/OTx G3: PTx/GTR |
Pre‐PTx Mid‐Tx (6.0/12.0 months) |
G1: 0 months G2: 2 months |
Misc (Intr) | NR | BDef/CAL/PPD/BMD |
| Boyer et al. (2011) | rNRS; Uni; FR |
G1: 15 (4/11); 42.8; NR G2: 11 (NR); NR; NR |
SCP | Yes |
G1: PTx/OTx G2: PTx |
Pre‐PTx Post‐OTx FU (16.0 years) |
≥2.0 months | NR | Splint | MBL |
| El‐Attar (2019) | uNRS; Uni; EG | G1‐2: 14 (NR); 31.9; NR | AgP | ANT; BDef |
G1: PTx/OTx/GTR G2: PTx/OTx |
Pre‐OTx Post‐OTx (10.0–12.0 months) FU (3.0/6.0/9.0 months) |
NR | Intr | Splint | BMD/MBL/PPD |
| Eliasson et al. (1982) | uNRS; Uni; SE | G1‐2: 20 (9/11); 41.2; NR | SCP | Mx ANT |
G1: PTx/OTx G2: PTx |
Pre‐PTx Pre‐OTx Post‐OTx |
4.0–6.0 months | Misc. | Splint | MBL/PPD |
| Han (2015) e | rNRS; Uni; KR | G1‐2: 10 (6/4); 56.7; 0% | SCP | Yes | G1‐2: PTx/OTx |
Pre‐OTx Post‐OTx (4.5 months) |
NR | Misc | Splint | MBL/PPD |
| Roccuzzo et al. (2018) | pNRS; Pract; IT | G1‐3: 36 (14/22); 53.9; 11% | SCP | Yes |
G1: PTx/GTR1/OTx G2: PTx/GTR2/OTx G3: PTx/GTR3/OTx |
Pre PTx FU (9.0–10.0 years) |
8.0–12.0 months | Misc | Splint | AEs/% PPD ≥ 7/Deepest PPD/PPD/Pus/TTHNO(LS) |
Abbreviations: AEs, adverse events; AgP, aggressive periodontitis; ANT, anterior teeth; BDef, bone defect; BF, bite force; BMD, bone mineral density; CAL, clinical attachment level; FiTo, circumferential fiberotomy; FU, follow‐up; G, group; GTR, guided tissue regeneration; Intr, intrude; MBL, marginal bone level; MBTh, marginal bone thickness; Misc, miscellaneous; Mx, maxilla; NR, not reported; OTx, orthodontic treatment; Perio, periodontitis; pNRS, prospective non‐randomized multi‐group comparative cohort study; PPD, pocket probing depth; Pract, private practice/clinic; PTM, pathologic tooth migration; PTx, periodontal treatment; RCTpa, randomized clinical trial (parallel design); RCTwp, randomized clinical trial (within‐person design); REC, recession; Retr, retrude; RL, root length; rNRS, retrospective non‐randomized multi‐group comparative cohort study; SCP, severe chronic periodontitis; TTHNO(LS), number of lost teeth given; Uni, university clinic; uNRS, non‐randomized multi‐group comparative cohort study with unclear design; y, year.
Countries given with their alpha‐2 codes.
Age is given as mean (one value) or range (in parenthesis).
Full‐mouth scores including non‐perio/ non‐migrated teeth excluded.
The experimental group received only subgingival debridement, while the control group also received final periodontal treatment before the start of orthodontic treatment.
Subsample of the study (only with pathologic tooth migration) included, provided for a previous review (Papageorgiou, Koletsi, et al., 2020).
TABLE 2.
Characteristics of included single‐group cohort studies
| Study | Design; setting; country a | Patients (M/F); age b ; smokers | Perio | PTM | PTx/OTx | Time | P‐OTx Time | OTx | Ret | Outcome c |
|---|---|---|---|---|---|---|---|---|---|---|
| Aimetti et al. (2020) | rSGC; Prac; IT | G: 21 (5/16); 52.6; 14% | SCP (S IV) | Mx/Mn ANT | G: PTx/(GTR)/OTx |
Pre PTx Aft PTx Post OTx (18.6 months) FU (≥10.0 years) |
6 months | Mostly Intr/Retr | NR | CAL/MBL/PPD/REC/RL/TTHNO(Nr) |
| Artun and Urbye (1988) | rSGC d ; Uni; NO | G: 24 (3/21); 42.6; NR | NR | Yes | G: PTx/OTx |
Aft PTx FU (13.5 months) |
NR | Align | Splint | MBL/PulpNecr/RL |
| Avantaggiato (2010) | rSGC d ; NR; IT | G: 26 (9/17); 44.3; NR | SCP | Yes; MDia | G: PTx/OTx |
Aft PTx Post OTx (15.0 months) FU (16.0 months) |
NR | Align/SC | Splint | MBL/TTHNO(LS)/SUCC |
| Cao (2015) | uSGC; Uni; CN | G: 14 (3/11); (22.0–41.0); 0% | SCP | Mx ANT | G: PTx/OTx/FiTo +(GTR) |
Pre OTx Post OTx (19.0 months) GTR + 6.0 months |
NR | Intr/align | Spint | BDef/CAL/MBTh/PPD |
| Cardaropoli (2001) and Corrente (2003) | uSGC; Pract; IT | G: 10 (2/8); (33.0–53.0); NR | SCP | Mx ANT | G: PTx/OTx |
Pre PTx Post OTx (10.0 months) |
7.0–10.0 days | Intr/align | Spint | AEs/BDef/CAL/CCL/MBL/PPD/RL |
| Cardaropoli (2004) | uSGC; Pract; IT | G: 28 (6/22); 44.8; NR | SCP | Mx ANT; MDia; PapLos; BDef | G: PTx/OTx |
Pre PTx Post OTx (11.7 months) FU (1.0 years) |
7.0–10.0 days | Intr/align/SC | ML Splint | CAL/CPBL/PapInd/PPD |
| Carvalho (2018) | pSGC e ; Uni; BR | G: 10 (1/9); 22.9; 0% | AgP | Yes | G: PTx/OTx |
Pre OTx Post OTx (18.9 months) FU (4.0 months) |
NR | Intr/align/SC | VFR | CAL/CAL ≥ 3/CAL ≥ 5/CEJPapil/PPD/PPD ≥ 4/PPD ≥ 6/REC |
| Czochrowska (2010) | rSGC; Pract; PL | G: 33 (NR); 46.3; NR | SCP/AGP | Yes | G: PTx/OTx |
Pre PTx Post OTx (16.0 months) FU (21.0 months) |
NR | Misc. | Splint & Plate | CAL/PROM/TTHNO(LS) |
| Ghezzi (2008) | uSGC; NR; IT | G: 14 (NR); NR; 0% | NR | Yes; MDia; BDef | G: PTx/GTR/OTx |
Pre PTx/GTR Pre OTx Post OTx |
1.0 years | Misc | Splint | CAL/PapInd/PPD |
| Ghezzi (2013) | pSGC; Pract; IT | G: 10 (4/6); 46.9; NR | SCP/AGP | Yes; MDia | G: PTx/GTR/OTx |
Pre PTx Post OTx (9.0 months) |
1.0 months | Intr/SC | Splint | CAL/PPD/REC |
| Jiao (2019) | rSGC; Uni; CN | G: 24 (8/16); (18.0–35.0); 0% | AgP (S IV) | Assumed from context | G: PTx/OTx |
Pre OTx Post OTx (18.0 months) |
≥4.5 months | Intr/Retr | Splint & VFR | MBL/PPD |
| Kim (2014) | pSGC; NR; KR | G: 15 (2/13); 51.8; NR | NR | Mx ANT | G: PTx/OTx |
Pre PTx Post OTx |
NR | Misc. | Splint | IEdgPapil/MBL/PapInd |
| Lihong (2014) | uSGC; Uni; CN | G: 13 (4/9); 36.8; NR | SCP | Mx ANT; MDia; PapLos | G: PTx/OTx |
Pre PTx PTx + 3.0 months Post OTx (17.7 months) |
3.0 months | Align/SC | Plate | CPBL/PapInd/PapHeig/PPD |
| Puttaravuttiporn (2018a) | uSGC; Uni; TH | G: 30 (0/30); 46.3; NR | NR | Mx ANT elongation | G: PTx/OTx |
Pre PTx Mid OTx (1 years) |
1.0 months | Intr | NR | RL/Root volume |
| Re (2000) | rSGC; NR; IT | G: 257 (78/189); 44.2; NR | NR | Mx/Mn ANT | G: PTx (w/wo surgery)/OTx |
Pre PTx Post OTx (10.0 months) FU (2.0–12.0 years) |
7.0 days | Intr/Retr | Splint/FPD | PPD |
| Re (2004) | pSGC; Pract; IT | G: 28 (NR); (29.0–60.0); NR | NR | Mx ANT; BDef | G: PTx/OTx |
Pre PTx Post OTx (11.7 months) FU (1.0 years) |
7.0–10.0 days | Intr/align | ML Splint | PPD/REC |
| Ya (2017) | rSGC; Uni; CN | G: 12 (4/8); 25.6; NR | AgP | Yes | G: PTx/OTx |
Pre PTx Mid OTx (6.0 months) Post OTx FU (6.0 months) |
3.0 months | Misc | NR | CAL/IEdgPapil/PPD |
| Zhang et al. (2017) | pSGC f ; Hosp; CN | G1: 59 (38/21); 36.5; 58% | SCP | Elongated/malaligned | G1: PTx/OTx |
Pre PTx Mid OTx (6.0/18.0 months) FU (2.0 years) |
NR | Misc | VFR | CAL/Mobility/PPD/Relapse |
Abbreviations: AEs, adverse events; AgP, aggressive periodontitis; ANT, anterior teeth; BDef, bone defect; CAL, clinical attachment level; CCL, clinical crown length; CPBL, contact point to bone level; PapInd, papilla index; CEJPapil, cementoenamel junction to papilla; FiTo, circumferential fiberotomy; FPD, fixed partial denture; FU, follow‐up; G, group; GTR, guided tissue regeneration; Hosp, hospital; Intr, intrude; MBL, marginal bone level; MBTh, marginal bone thickness; MDia, maxillary diastema; Misc, miscellaneous; ML, Maryland; Mx, maxilla; Mn, mandible; NR, not reported; OTx, orthodontic treatment; PapHeig, papilla height; PapLos, interdental papilla loss; Perio, periodontitis; PPD, pocket probing depth; Pract, private practice/clinic; PROM, patient reported outcome measure; IEdgPapil, incisal edge to papilla; pSGC, prospective single group cohort study; PTM, pathologic tooth migration; PTx, periodontal treatment; PulpNecr, pulp necrosis; REC, recession; Retr, retrude; RL, root length; rSGC, retrospective single group cohort study; S, stage; SC, space closure; SCP, severe chronic periodontitis; SUCC, treatment success; TTHNO(LS), number of lost teeth given; TTHNO(Nr), number of existing teeth given; Uni, university clinic; uSGC, single group cohort study with unclear design; VFR, vacuum formed retainer; y, year.
Countries given with their alpha‐2 codes.
Age is given as mean (one value) or range (in parenthesis).
Full‐mouth scores included non‐perio/non‐migrated teeth excluded.
Untreated teeth of the same patient used as control group.
One study arm without periodontal disease omitted.
Only one trial arm (with pathologic tooth migration) from a three‐arm trial was included and is regarded as a prospective cohort study.
The eligible studies included a total of 914 patients, to a median sample size of 21 patients/study (range 10–257 patients/study). Among the 25 studies reporting the patients' gender, 29.7% were male (237 of the total 799), while from the 22 studies reporting mean age, the average across studies was 43.4 years (range of average age 22.9–56.7 years). Only 13 of studies reported on the smoking status of included patients, 9 (69%) included only non‐smokers and the remaining 4 had 4%–58% smokers.
All included studies reported on patients with severe periodontal disease burdened with a series of complexity factors such as bite collapse, drifting, or flaring, which led to the need for combined periodontal–orthodontic treatment (at at least one arm per study) with/without tissue regeneration and adjunct procedures. Studies reported data (i) prior to the periodontal treatment, (ii) prior to the orthodontic treatment, (iii) during orthodontic treatment, (iv) after completion of the orthodontic treatment, and (v) after an additional follow‐up period. The interval between periodontal and orthodontic treatment varied greatly ranging from no interval (directly after periodontal treatment) to 1 year. The mean duration of orthodontic treatment was 14.1 months (from the 15 studies reporting this; range 4.5–20.7 months), and the median follow‐up after orthodontic treatment was 16.0 months (from the 15 studies reporting this; range 4 months to 16 years). Limited information about the actual scope of orthodontic treatment was provided, though it often included tooth alignment, intrusion, retraction, and space closure, while post‐treatment retention was achieved with wire splints, plates, vacuum‐formed retainers, Maryland splints, or fixed partial prostheses. Conflicts of interest among included studies were checked only for those with potential financial interests from treatment (those including grafts, lasers, or bite‐wafers) (Appendix 4). Seven out of the 10 studies with adjuncts reported no conflict, while 3 (all using guided tissue regeneration) gave no statement of potential conflicts.
Treatment outcomes related to efficacy that were measured included CAL, PPD, MBL, marginal bone thickness or density, bone defect fill, interdental papilla presence or position, bite force, and treatment success (absence of pain, infection, suppuration, and further bone loss). Additionally, outcomes related to adverse effects were measured including tooth loss, gingival recession, pulp necrosis, root resorption, and PROMs.
3.3. ROB within studies
ROB was assessed separately for randomized trials (Table 3), non‐randomized comparative (multi‐group) cohort studies (Table 4), and non‐randomized single‐group cohort studies (Table 5). The majority of included randomized trials (83%) were in high ROB and one was in low ROB. The major problems pertained to selection of the reported results (high bias in 67%), measurement of the outcome (50%), randomization (33%), and missing data (17%). All included non‐randomized comparative (multi‐group) cohort studies were in either serious or critical ROB, with the most problematic domains being confounding (problematic in all trials), measurement of outcome (67%), and selection of participants (17%). Finally, potential issues were found for all identified non‐randomized single‐group cohort studies, with the most problematic domains being study design, lack of adequate measurement/controlling for confounders, incomplete reporting, problematic patient selection procedures, lack of objective outcome measurement, issues with the sample size inadequacy and statistical analysis, and limited follow‐up post treatment.
TABLE 3.
Risk of bias of included randomized trials with the RoB 2.0 tool
| Domain | Item | Attia et al. (2019) | Liu et al. (2008) | Puttaravuttiporn (2018) | Ren (2019) | Shi et al. (2003) | Zasciurinskiene (2019) |
|---|---|---|---|---|---|---|---|
| Domain 1. Randomization process | 1.1 | PY | PY | Y | Y | PY | Y |
| 1.2 | Y | PN | PY | Y | PN | NI | |
| 1.3 | Y | N | PY | N | NI | PN | |
| 1.0 Assessor's judgement | Some concerns | High | Some concerns | Low | High | Some concerns | |
| Domain 2. Deviations from intended interventions | 2.1 | PN | Y | PN | N | PY | Y |
| 2.2 | Y | Y | PY | N | PY | Y | |
| 2.3 | PN | PN | PN | NA | NI | PY | |
| 2.4 | NA | NA | NA | NA | NA | PN | |
| 2.5 | NA | NA | NA | NA | NA | PN | |
| 2.6 | PY | PY | PY | Y | PY | PY | |
| 2.7 | NA | NA | NA | NA | NA | NA | |
| 2.0 Assessor's judgement | Low | Low | Low | Low | Some concerns | Some concerns | |
| Domain 3. Missing outcome data | 3.1 | Y | PY | PY | PN | NI | PN |
| 3.2 | NA | NA | NA | PN | PN | PN | |
| 3.3 | NA | NA | NA | PN | NI | PN | |
| 3.4 | NA | NA | NA | NA | NI | NA | |
| 3.0 Assessor's judgement | Low | Low | Low | Low | High | Low | |
| Domain 4. Measurement of the outcome | 4.1 | N | N | N | N | PN | N |
| 4.2 | PN | PN | PN | PN | PN | PN | |
| 4.3 | PY | PY | N | N | PY | PN | |
| 4.4 | PY | PY | NA | NA | PY | NA | |
| 4.5 | NI | PY | NA | NA | PY | NA | |
| 4.0 Assessor's judgement | High | High | Low | Low | High | Low | |
| Domain 5. Selection of the reported result | 5.1 | NI | NI | NI | Y | NI | NI |
| 5.2 | PY | N | PY | PN | PN | PY | |
| 5.3 | N | N | N | PN | PY | N | |
| 5.0 Assessor's judgement | High | Some concerns | High | Low | High | High | |
| Overall judgement | High | High | High | Low | High | High | |
Abbreviations: N, no; NA, not applicable; NI, no information; PN, probably not; PY, probably yes; Y, yes.
TABLE 4.
Risk of bias of included non‐randomized multi‐group comparative cohort studies with the ROBINS‐I tool
| Domain | Reference | Attia et al. (2012) | Boyer et al. (2011) | El‐Attar (2019) | Han (2015) | Roccuzzo et al. (2018) | Zhang et al. (2017) |
|---|---|---|---|---|---|---|---|
| 1. Confounding | 1.1 | PY | PY | PY | PY | PY | PY |
| 1.2 | PN | PN | PN | PN | PN | PN | |
| 1.3 | N | N | N | N | N | N | |
| 1.4 | PN | PN | PY | PN | PN | PN | |
| 1.5 | NA | NA | Y | NA | NA | NA | |
| 1.6 | N | N | N | N | N | N | |
| 1.7 | N | N | PY | N | N | N | |
| 1.8 | NA | NA | PY | NA | NA | NA | |
| Judgement | Serious | Serious | Moderate | Serious | Serious | Serious | |
| 2. Selection of participants into the study | 2.1 | NI | NI | PY | NI | NI | NI |
| 2.2 | NA | NA | Y | NA | NA | NA | |
| 2.3 | NA | NA | Y | NA | NA | NA | |
| 2.4 | NI | NI | Y | PY | NI | NI | |
| 2.5 | NA | NA | NA | NA | NA | NA | |
| Judgement | NI | NI | Critical | NI | NI | NI | |
| 3. Classification of interventions | 3.1 | Y | Y | Y | Y | Y | Y |
| 3.2 | Y | Y | Y | Y | Y | Y | |
| 3.3 | N | N | N | N | N | N | |
| Judgement | Low | Low | Low | Low | Low | Low | |
| 4. Deviations from intended interventions | 4.1 | NI | NI | NI | NI | NI | NI |
| 4.2 | NA | NA | NA | NA | NA | NA | |
| 4.3 | NI | NI | NI | NI | Y | NI | |
| 4.4 | PY | NI | PY | PY | Y | NI | |
| 4.5 | NI | NI | NI | NI | PY | NI | |
| 4.6 | NA | NA | NA | NA | NA | NA | |
| Judgement | NI | NI | NI | NI | Low | NI | |
| 5. Missing data | 5.1 | PY | PY | PY | PY | PY | PY |
| 5.2 | PN | PN | PN | PN | PN | PN | |
| 5.3 | NI | NI | NI | NI | NI | NI | |
| 5.4 | NA | NΑ | NΑ | NΑ | NΑ | NΑ | |
| 5.5 | NΑ | NΑ | NΑ | NΑ | NΑ | NΑ | |
| Judgement | NI | NI | NI | NI | NI | NI | |
| 6. Measurement of outcomes | 6.1 | PY | PY | PY | PY | PY | PY |
| 6.2 | PY | PY | PN | PN | PY | PY | |
| 6.3 | PY | PY | PY | PY | PY | PY | |
| 6.4 | PN | PN | PN | PN | PN | PN | |
| Judgement | Moderate | Moderate | Low | Low | Moderate | Moderate | |
| 7. Selection of the reported result | 7.1 | PN | PN | PN | PN | PN | PN |
| 7.2 | PN | PN | PN | PN | PN | PN | |
| 7.3 | PN | PN | PN | PN | PN | PN | |
| Judgement | Low | Low | Low | Low | Low | Low | |
| Overall | Judgement | Serious | Serious | Critical | Serious | Serious | Serious |
Abbreviations: N, no; NA, not applicable; NI, no information; PN, probably not; PY, probably yes; Y, yes.
TABLE 5.
Assessment of internal validity/sources of bias of included non‐randomized single‐group cohort studies with a custom tool
| Study | Prosp‐ective | Age rep'd | Sex rep'd | Severity rep'd | Smokers rep'd | PTx details rep'd | OTx details rep'd | Pt selection by outcome | Outcome blinded? | Appropriate analysis? | Adequate sample (≥20)? | Adequate follow‐up (≥1 year) | All data/results reported? |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Aimetti et al. (2020) | No | Yes | Yes | Yes | Yes | Yes | Yes | Partly | No | Yes | Yes | Yes | Yes |
| Artun and Urbye (1988) | No | No | No | Partly | No | Partly | Partly | No | No | No | Yes | Yes | No |
| Avantaggiato (2010) | No | Yes | Yes | No | No | No | No | No | No | No | Yes | Yes | No |
| Cao (2015) | Unclear | Partly | Yes | Yes | Yes | Yes | Yes | No | No | Yes | No | Partly | Yes |
| Cardaropoli (2001) and Corrente (2003) | Unclear | Yes | Yes | Yes | No | Partly | Partly | No | No | Yes | No | No | Yes |
| Cardaropoli (2004) | Unclear | Yes | Yes | Yes | No | Yes | Yes | No | No | Partly | Yes | Yes | Yes |
| Carvalho (2018) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | Partly | No | Partly | Yes |
| Czochrowska (2010) | No | Yes | No | No | No | No | No | No | No | No | Yes | Yes | No |
| Ghezzi (2008) | Unclear | No | No | Yes | Yes | Yes | Yes | No | No | Yes | No | No | Yes |
| Ghezzi (2013) | Yes | Yes | Yes | Yes | No | Yes | Yes | No | No | Yes | No | No | Yes |
| Jiao (2019) | No | Partly | Yes | No | Yes | Yes | Yes | Yes | No | Yes | Yes | No | No |
| Kim (2014) | Yes | Yes | Yes | Yes | No | No | No | No | No | No | No | No | Partly |
| Lihong (2014) | Unclear | Yes | Yes | Partly | No | Partly | Partly | No | No | Partly | No | No | Partly |
| Puttaravuttiporn (2018a) | Unclear | Yes | Yes | No | No | Partly | Yes | No | Yes | Partly | Yes | No | Yes |
| Re (2000) | No | Yes | Yes | Yes | No | Yes | Yes | No | No | Partly | Yes | Yes | Yes |
| Re (2004) | Yes | Partly | No | Yes | No | Partly | Partly | No | No | Partly | Yes | Yes | Yes |
| Ya (2017) | No | Yes | Yes | Yes | No | No | No | No | No | No | No | Partly | Yes |
| Zhang et al. (2017) | Yes | Yes | Yes | Yes | Yes | Yes | Partly | No | No | No | Yes | Yes | Yes |
Abbreviations: OTx, orthodontic treatment; Pt, patient; PTx, periodontal treatment; rep'd, reported.
3.4. Results of individual studies
This review included aggregate data provided in the report of included studies, except for two studies (Han, 2015; Roccuzzo et al., 2018) where raw data were available (one provided for a previous review of braces vs. aligners, and the other providing raw data in tables), and these were re‐analysed (Appendix 5–6b). Except for some omitted outcomes not included in the protocol (Appendix 7), all outcomes that were eligible according to the review's protocols were used in the primary analysis (direct comparisons using multi‐group studies; Appendix 8; Table 6) or the secondary analysis (indirect pooling across both multi‐ and single‐group studies; Table 7).
TABLE 6.
Summary of findings table according to the GRADE approach
| Anticipated absolute effects (95% CI) | |||||
|---|---|---|---|---|---|
| Outcome [observation period] studies (patients) | Control group a | Experimental group | Difference in experimental group | Quality of the evidence (GRADE) b | What happens with experimental treatment |
| PTx | PTx‐OTx | ||||
|
PPD [Pre‐PTx → Post‐OTx] 1 study c (20 patients) |
−0.9 mm | — | Same amount (0.4 mm less to 0.4 mm more) | ⊕ ◯ ◯ ◯ very low d , e due to bias, imprecision | Little to no difference in PPD change |
|
MBL (% root‐length) [Pre‐PTx → Post‐OTx] 1 study c (20 patients) |
+0.2% | — | 0.6% less (2.8% less to 1.6% more) | ⊕ ◯ ◯ ◯ very low d , e due to bias, imprecision | Little to no difference in MBL change |
| PTx‐OTx | Pre(PTx) f ‐OTx | ||||
|
CAL [Pre‐PTx → Post‐OTx] 1 study g (50 patients) |
−0.4 mm | 0.1 mm greater improvement (0.2 mm less to 0.3 mm more) | ⊕ ⊕ ⊕ ◯ moderate h due to bias | Little to no difference in CAL change | |
|
Siters with PPD reduction [Pre‐PTx → Post‐OTx] 1 study g (50 patients) |
36.4% | — | 11.4% less sites (30.1% less to 7.3% more) | ⊕ ⊕ ⊕ ◯ moderate h due to bias | Little to no difference in PPD change |
|
MBL [Pre‐PTx → Post‐OTx] 1 study g (50 patients) |
−0.1 mm | — |
0.1 mm less MBL improvement (0.4 mm less to 0.2 mm more) |
⊕ ⊕ ⊕ ◯ moderate h due to bias | Little to no difference in MBL change |
|
Sites with recession [Pre‐PTx → Post‐OTx] 1 study g (50 patients) |
20.2% | — | 9.3% less sites (27.0% less to 8.4% more) | ⊕ ⊕ ⊕ ◯ moderate h due to bias | Little to no difference in recession development |
| PTx‐OTx | PTx‐OTx + fiberotomy | ||||
|
CAL [Pre‐PTx → Post‐OTx] 1 study i (52 patients) |
−0.2 mm | — | 0.6 mm greater decrease (0.2 to 1.1 mm greater) | ⊕ ⊕ ⊕ ◯ moderate h due to bias | Might lead to greater CAL decrease |
|
PPD [Pre‐PTx → Post‐OTx] 1 study i (52 patients) |
−0.3 mm | — | Same amount (0.5 mm less to 0.4 mm more) | ⊕ ⊕ ⊕ ◯ moderate h due to bias | Little to no difference in PPD change |
|
MBL [Pre‐PTx → Post‐OTx] |
−0.4 mm | — | 1.0 greater MBL improvement (0.1 to 1.9 mm greater) | ⊕ ⊕ ◯ ◯ low k due to bias | Might lead to greater MBL improvement |
Note: Intervention: periodontal/orthodontic treatment combined orthodontic with different timing or adjunct use of circumferential fiberotomy; Population: patients with severe periodontal disease and pathologic tooth migration; Setting: university clinics and private practice (China, Lithuania, Sweden).
Abbreviations: CAL, clinical attachment level; CI, confidence interval; GRADE, Grading of Recommendations Assessment, Development and Evaluation; MBL, marginal bone level; OTx, orthodontic treatment; PPD, pocket probing depth; PTx, periodontal treatment.
Response in the control group is based on the response of included studies (or random‐effects meta‐analysis of the control response).
Starts from “high”.
Contributing studies: Eliasson (2012).
Downgraded by two levels for bias due to the inclusion of non‐randomized studies with critical/serious risk of bias.
Downgraded by one level for imprecision due to the inclusion of an inadequate sample.
The experimental group received only subgingival debridement, while the control group also received final periodontal treatment before the start of orthodontic treatment.
Contributing studies: Zasciurinskiene et al. (2018).
Downgraded by one levels for bias due to high risk of bias for the included randomized study.
Contributing studies: Liu et al. (2008).
Contributing studies: Shi et al. (2003).
Downgraded by two levels for bias due to high risk of bias for both included randomized studies.
TABLE 7.
Indirect meta‐analyses on the average pooled effect of orthodontic‐periodontal treatment from single‐group cohort studies and multi‐group randomized or non‐randomized clinical trials
| Outcome | Period | n a | Pooled average | p‐Value | I 2 (95% CI) | Modifying factors (Appendix 15) |
|---|---|---|---|---|---|---|
| CAL |
Pre‐PTx →Post‐OTx |
5 | −3.95 (−5.79, −2.11) | <.001 | 98% (95%, 100%) | OTx duration |
|
Pre‐OTx →Post‐OTx |
7 | −0.24 (−0.38, −0.10) | <.001 | 79% (33%, 96%) | — | |
|
Post‐OTx →FU (4‐12 months) |
3 | 0.05 (−0.20, 0.29) | .70 | 77% (17%, 99%) | — | |
| PPD |
Pre‐PTx →Post‐OTx |
8 b | −2.97 (−3.93, −2.01) | <.001 | 99% (99%, 100%) |
Baseline PPD Interval between PTx‐OTx OTx duration |
|
Pre‐OTx →Post‐OTx |
7 | −0.23 (−0.49, 0.04) | .09 | 95% (85%, 99%) | % of male patients | |
|
Post‐OTx →FU (4‐144 months) |
5 | 0.09 (−0.04, 0.22) | .18 | 76% (24%, 96%) | FU duration | |
| Sites with PPD5‐6 |
Pre‐PTx →Post‐OTx |
2 | −0.92 (−1.76, −0.07) | .03 | 0% (0%, 100%) | — |
|
Pre‐OTx →Post‐OTx |
2 | −1.25 (−8.07, 5.57) | .72 | 87% (9%, 100%) | — | |
| MBL |
Pre‐PTx →Post‐OTx |
2 | 1.03 (−11.86, 13.93) | .50 | 100% (NC) | — |
|
Pre‐OTx →Post‐OTx |
7 | −0.36 (−0.59, −0.13) | .002 | 88% (68%, 97%) | — | |
| Papilla height |
Pre‐OTx →Post‐OTx |
2 | −1.42 (−1.98, −0.86) | <.001 | 94% (NC) | — |
| Recession |
Pre‐PTx →Post‐OTx |
3 | −0.53 (−2.07, 1.01) | .50 | 98% (91%, 100%) | Gingiva phenotype (through crown width/length ratio) |
|
Pre‐OTx →Post‐OTx |
2 | 0.09 (−0.01, 0.20) | .09 | 0% (0%, 100%) | — | |
|
Post‐OTx →FU (4‐12 months) |
2 | 0.01 (−0.08, 0.10) | .81 | 0% (0%, 99%) | — | |
| Root length |
Pre‐PTx →Post‐OTx |
2 | −0.51 (−0.79, −0.23) | <.001 | 65% (0%, 100%) | — |
|
Pre‐OTx →Post‐OTx |
2 | −0.49 (−1.04, 0.06) | .08 | 71% (0%, 100%) | — |
Abbreviations: CAL, clinical attachment level; CI, confidence interval; FU, follow up; MBL, marginal bone level; OTx, orthodontic treatment; PPD, pocket probing depth; PTx, periodontal treatment.
Multiple trial arms (different periodontal treatments or follow‐ups) were pooled together for the main analysis. They are analysed separately for treatment‐related modifying factors.
One small study was omitted, as it was the only out of the original nine that showed a great increase instead of a decrease through treatment.
3.5. Synthesis of the results—Primary (direct) analysis
3.5.1. Treatment efficacy
A combined periodontal–orthodontic treatment was compared with only periodontal treatment in three studies with different protocols and observation periods. One of these (Attia et al., 2012) found that combined treatment showed a better response mid‐treatment in terms of percentage gain in CAL (13.3%), PPD (12.2%), and mineral density (11.8%) compared to periodontal monotreatment. However, this was a very small (n = 15) non‐randomized trial with high ROB and limited follow‐up. The other two non‐randomized studies (Eliasson et al., 1982; Boyer et al., 2011) found no difference in percentage MBL reduction. A larger (n = 50) randomized trial (Zasciurinskiene et al., 2018) compared experimental orthodontic treatment after only subgingival debridement with continuation of periodontal treatment after the orthodontic treatment to orthodontic treatment after finalized periodontal phase and found no statistically significant differences in CAL, PPD, MBL, and recessions. Orthodontic treatment with conventional braces was found in one small (n = 10) retrospective study (Han, 2015) to be more efficient in reducing PPD than treatment with thermoplastic aligners (difference of −1.6 mm), but this should again be seen with caution, due to the study's high ROB. Adjunct use of laser during orthodontic treatment was found to be associated with a better response mid‐treatment in terms of percentage gain in CAL (20.9%), PPD (11.8%), and mineral density (16.2%) compared to no laser, but the contributing small (n = 15) study (Attia et al., 2019) was likewise in high ROB. Simultaneous guided tissue regeneration as part of the combined periodontal–orthodontic treatment did not seem to be associated with considerable benefits, apart from a small increase in bone mineral density (El‐Attar et al., 2019).
Finally, meta‐analysis of two small randomized trials from China (Shi et al., 2003; Liu et al., 2008) (n = 16 and n = 21, respectively) indicated that adjunct circumferential fiberotomy during orthodontic treatment was associated with improved levels of marginal bone (MD = −0.98 mm; 95% CI = –1.87 to −0.10 mm; p = .03) with considerable heterogeneity (τ 2 [95% CI] = 0.32 [0 to 53.08]/I 2 [95% CI] = 77% [0%–100%]), which does not enable accurate quantification of the actual benefit. However, these two trials were in high ROB and were non‐transparently reported, and therefore, these results should be seen with caution.
3.5.2. Adverse effects and PROMs
As far as adverse effects and PROMs are concerned, no significant effect was seen on tooth loss, root resorption, tooth mobility, pain during orthodontic treatment, and recession development according to the adjunct use of fiberotomy, guided tissue regeneration, laser, bite wafer, or the timing of orthodontic treatment relative to the completion of periodontal treatment (Appendix 8).
3.5.3. Quality of evidence and additional analyses
The GRADE summary‐of‐findings table for selected outcomes from the direct analysis is given in Table 6. The quality of evidence regarding (a) a combined periodontal‐orthodontic versus periodontal treatment alone and (b) the timing of orthodontic treatment ranged from moderate to very low, due to bias and imprecision from limited sample sizes. Likewise, the potential benefits of fiberotomy were supported by evidence of moderate to low quality due to the high ROB of included trials. Therefore, our confidence in current estimates is low, and future research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change estimates.
No subgroup/meta‐regression analyses, reporting bias assessments, and sensitivity analyses could be performed due to the small number of existing studies.
3.6. Synthesis of the results—Secondary (indirect) analysis
3.6.1. Treatment efficacy and related factors
The average observed changes in CAL, PPD, and papilla height, pooled via meta‐analyses across all studies, can be seen in Table 7 and Appendices 9–14, while possible related factors are shown in Appendix 15.
Clinical attachment level was reduced on average with a CAL gain of 3.95 mm (MD = –3.95 mm; 95% CI = –5.79 to −2.11 mm; Appendix 9) during combined periodontal–orthodontic treatment, while a CAL gain of 0.24 mm (MD = –0.24 mm; 95 CI = –0.38 to −0.10 mm; Appendix 10) was seen during orthodontic treatment alone. Similar to PPD, CAL gain was associated with the duration of orthodontic treatment, with CAL gains being 0.39 mm smaller (coefficient = 0.39 mm; 95% CI = –0.09 to 0.86 mm; p = .08) for each additional month (see meta‐regression in Appendix 15).
PPD was reduced on average by −2.97 mm (95% CI = –3.93 to −2.01 mm; Appendix 11) during combined periodontal–orthodontic treatment, while a reduction of −0.23 mm (95 CI = −0.49 to 0.04; Appendix 10) was seen during orthodontic treatment alone. Reduction in PPD seen during combined treatment seemed to be associated with patient sex (as percentage of male patients in the sample), with additional −0.18 mm reduction in PPD (95% CI = −0.37 to −0.01; p = .06) for each extra 10% of the sample being male. Additionally, an association was seen between baseline PPD severity and treatment‐related reduction in PPD (coefficient = −0.82 mm; 95% CI = −1.16 to −0.48 mm; p = .001). Finally, greater PPD reductions were seen for smaller intervals between periodontal and orthodontic treatment after a minimum healing period (with PPD reduction being 0.13 mm smaller [95% CI = 0.05–0.20 mm; p = .006] for each additional interval week) and durations of orthodontic treatment (with PPD reductions being 0.25 mm smaller [95% CI = 0.04–0.45 mm; p = 0.03] for each additional duration month). Follow‐up after orthodontic treatment was associated with PPD increases of about 0.14 mm for every additional five follow‐up years (95% CI = 0.01–0.28 mm; p = .04).
Finally, a small improvement in MBL of around 0.36 mm (95% CI = 0.13–0.59 mm; Appendix 14) and a modest improvement in papilla height of about 1.42 mm (95% CI = 0.86–1.98 mm) were seen after periodontal–orthodontic treatment, though without any modifying factors.
3.6.2. Adverse effects and related factors
Orthodontic treatment of pathologically migrated teeth was associated with a small amount of root resorption of about 0.51 mm (95% CI = 0.23–0.79), which is clinically irrelevant, but was overall not necessarily associated with gingival recessions. However, one study (Re et al., 2004) judging periodontal phenotype by the crown width/crown length ratio found that improvement of gingival recessions was dependent on gingival phenotype, with wide‐thick periodontal phenotype (crown width/length ≤ 0.66) being associated with greater improvement by 0.47 mm (95% CI = 0–0.95 mm; p = .05).
Additionally, several single studies separately reported on adverse effects after orthodontic treatment. Ten to twelve years after orthodontic treatment, half of the patients had lost at least one tooth in the study of Roccuzzo et al. (2018), but a non‐significant reduction in the number of teeth after orthodontic treatment was seen by Aimetti et al. (2020). The latter study also reported an 8% (n = 3) rate for adverse events at 10 years of follow‐up, which pertained to pulp necrosis (n = 2) and root fracture (n = 1). Pulp necrosis was likewise reported after 13.5 months of follow‐up for 25% (6 out of 24) of the included patients by Artun and Urbye (1988). Finally, 2 years after combined periodontal–orthodontic treatment by Zhang et al. (2017), 15% of the patients (9 of 59) showed a relapse (i.e., did not maintain good periodontal health and good occlusion without migration), while 33% (19 of 58) of periodontally treated patients without initial tooth migration had relapsed into tooth inflammation, tooth migration, and changes in occlusal relationship.
3.6.3. Reporting biases and sensitivity analyses
We expect the current review to be less prone to publication bias because of the wide unrestricted search of multiple databases without limitations to published papers and the extensive manual search of grey literature sources (like Digital Dissertations, metaRregister, GoogleScholar, etc). The formal assessment of reporting biases (including possible publication bias) and the sensitivity analyses according to design characteristics are seen in Appendix 16. Signs of reporting bias were seen for the effect of orthodontic treatment on CAL (Egger's p = .09), but the funnel plot did not indicate publication bias (Appendix 17) but rather “small‐study effects”. On the other side, significantly different (p < .10) treatment‐induced effects on CAL, MBL, and PPD were seen between studies with large/small sample size, prospective/retrospective nature, and multi‐group/single‐group nature. Therefore, future clinical recommendations should be based on methodologically sound studies to minimize bias.
4. DISCUSSION
4.1. Results in context
This systematic review collates and critically appraises randomized and non‐randomized clinical studies on the effects of orthodontic treatment on patients with previous severe periodontitis and pathologically migrated teeth. Thirty studies (half of them being uncontrolled single‐group cohort studies) with a total of 914 patients (29.7% male; mean age 43.4 years) were included and assessed for periodontal–orthodontic treatment, which was compared with periodontal monotherapy, or evaluated the use of additional procedures (such as guided tissue regeneration or fiberotomy) and adjuncts (such as laser or bite‐wafer).
Data from indirect pooling of single‐group cohort studies indicated that combined periodontal–orthodontic treatment might be associated with minimal improvement of the periodontal condition in terms of CAL, PPD, MBL, and papilla height (Table 7). This might be interpreted as due to a relative intrusion of the orthodontically treated teeth within the alveolar bone, which might facilitate a gain in clinical attachment. This stands in stark contrast to the effects of orthodontic treatment on periodontally healthy patients, where a minimal loss of clinical attachment and marginal bone is seen (Bollen et al., 2008; Papageorgiou, Papadelli, & Eliades, 2018). Possible explanations for this might include an increased blood flow to periodontium, dental pulp, and alveolar bone, which might promote restoration of periodontal tissues (Figueira et al., 2009). This is supported by the findings of an included study (Zhang et al., 2017), which were only partly reported in the review's tables (as the omitted study arms pertained to periodontic patients without tooth migration and periodontally healthy patients). In that, the periodontal indices of stage IV periodontitis groups receiving combined periodontal–orthodontic treatment greatly improved without any significant difference to the periodontally healthy groups, indicating that the combined treatment group recovered faster than the group that underwent periodontal monotherapy. The efficacy of non‐surgical and surgical periodontal treatment has been previously documented in classical studies, with maximum pocket reduction and CAL gains, after 1 year, being observed in pockets initially deeper than 5 mm (Kaldahl et al., 1996; Cobb, 2002). Nowadays, with advanced regenerative periodontal treatment approaches, we are able to predictably increase the margins of pocket reduction and CAL gain after treatment when performed after appropriate case selection (Reynolds et al., 2015; Cortellini et al., 2017; Nibali et al., 2020). Nonetheless, significant gains such as those observed after the combined periodontal–orthodontic treatment in the present study (indirect meta‐analyses; Table 7) may be comparable only with optimal treatment outcomes which vary across several factors such as surgical technique, biomaterials, and experience of the operator. Additionally, a favourable response in the cytokine profile of patients receiving combination treatment was seen, but this might be a confounder due to reinforced oral hygiene monitoring during fixed appliance therapy.
Similar findings were reported by another recently published systematic review prepared for the same European Federation of Periodontology (EFP) workshop (Martin et al., 2021), which compared the effect of orthodontic treatment between treated periodontitis patients with a healthy but reduced periodontium and non‐periodontitis patients. The authors of this review concluded that orthodontic tooth movement had no significant impact on periodontal outcomes and did not interfere with periodontal healing. It must be noted here, however, that their review was limited to indirect meta‐analyses and only in the comparison between periodontally treated and periodontally healthy patients, whereas this review focused only on the former—and therefore was based on a wider data pool.
Interestingly, an inverse relationship was seen between orthodontic treatment duration and periodontal gains in favour of reduced treatment durations, which might implicate longer treatments and the extended inflammation risk due to the added plaque burden from the orthodontic appliances (Chhibber et al., 2018). It might therefore be prudent to take this into account when planning the desired tooth movements and selecting the appropriate orthodontic appliances (Chhibber et al., 2018; Papageorgiou et al., 2016; Papageorgiou, Koletsi, et al., 2020). This dose–response relationship between the duration of orthodontic treatment and periodontal response might be helpful in terms of epidemiological association but needs to be further studied.
Equally importantly, the long‐term prognosis of pathologically migrated teeth does not seem to be endangered by their orthodontic realignment. Roccuzzo et al. (Roccuzzo et al., 2018) reported that 10 years after periodontal treatment, guided tissue regeneration of bony defects, and orthodontic alignment of pathologically migrated teeth, the mean number of teeth lost per patient was 0.64 ± 0.70. Similarly, Aimetti et al. (2020) reported that no anterior tooth with pathological tooth migration that underwent orthodontic treatment was lost because of periodontitis recurrence during the 11‐year‐average period of supportive periodontal therapy. Furthermore, Zhang et al. (2017) found that patients with initially pathologically migrated teeth treated orthodontically showed less relapse of periodontal inflammation/migration than did patients who received periodontal monotherapy (15% vs. 33%). This might indicate that a harmonious occlusion with balanced occlusal contacts might be beneficial to avoid occlusal trauma or periodontal breakdown and might help the long‐term prognosis of teeth. However, it must be stressed here that after orthodontic alignment, the vast majority of studies included a definite stabilization protocol (usually with a wire splint), which might have confounded these data.
4.2. Strengths and limitations
This review has several strengths, including its a priori protocol (Sideri et al., 2018), the comprehensive literature search, the use of modern, up‐to‐date methods for study appraisal (Sterne et al., 2016; Sterne et al., 2019) or data analysis (Langan et al., 2019), the application of the GRADE approach to assess the strength of provided recommendations (Guyatt et al., 2011), and the transparent provision of all data (Papageorgiou, Antonoglou, et al., 2020).
Some limitations also do exist in the present review. For one, ideally randomized trials comparing combined periodontal–orthodontic treatment with periodontal monotherapy should have been included in this review. However, owing to the lack of studies, also “weaker” non‐randomized study designs were included, which, together with other methodological issues (lack of pre‐registration, careful patient selection, blinding, and a priori sample size calculations), might have introduced bias in the results (Papageorgiou et al., 2015; Papageorgiou et al., 2017; Papageorgiou et al., 2019). Ideally, trials randomizing severe (stage IV) periodontitis patients to either periodontal–orthodontic treatment or periodontal treatment alone should be used to better evaluate the added benefits of orthodontic treatment. Furthermore, many included studies assessed outcome mid‐treatment, directly post treatment, or shortly after the combined periodontal–orthodontic treatment, which could have an effect on the measured outcomes, since orthodontic treatment might still be ongoing and a longer period might be needed for definitive healing and tissue regeneration (Sanz et al., 2012; Hoffmann et al., 2016). Healing after non‐surgical and surgical periodontal treatment (i.e., stabilization of attachment level and pocket depth) might take place even 12 months or more after treatment completion, and thereafter additional factors such as oral hygiene may come in play regarding the condition of previously affected tissues. If one wants to identify the different benefits attributed solely to orthodontic treatment after periodontal treatment, a sufficient amount of time may be required for healing phenomena after periodontal treatment to conclude before orthodontic treatment commences. Therefore, periodontal measurements before periodontal treatment, after periodontal treatment, before initiation of orthodontic treatment, during orthodontic treatment (with 6‐month intervals), and about 1 year after completion of orthodontic treatment might be appropriate to gauge the effect of each treatment separately. Evidence of bias was possibly seen in the sensitivity analyses of the current review (Appendix 16) according to sample size and study design, and therefore it is important that future prospective multi‐arm studies with adequate sample and follow‐up are incorporated in the existing evidence base. Inclusion of non‐randomized studies in meta‐analysis is not considered prohibitory, provided robust bias appraisal has been performed, and recent guidance has been provided about how to appropriately incorporate such designs (Schünemann et al., 2019). Also, a heterogeneous response among studies was seen for most outcomes in the indirect analyses, which is to be expected because of the wide spectrum of baseline severity/appliances/clinical settings. Furthermore, most meta‐analyses were based predominantly on small trials, which might affect the precision of the estimates (Cappelleri et al., 1996). Additionally, the small number of trials that were ultimately included in the meta‐analyses and their incomplete reporting of results and potential confounders like level of case severity, oral hygiene, treatment timing, post‐alignment finishing, and retention regimens, precluded the conduct of many analyses for subgroups and meta‐regressions.
5. CONCLUSIONS
Existing evidence on the orthodontic treatment of patients with previous severe periodontal disease and pathological tooth migration is very limited and of poor quality. Orthodontic treatment might be associated with small improvements of periodontal parameters and does not seem to affect long‐term prognosis. But its exact effects on the periodontal tissues, as well as the optimal treatment protocol, remain unclear. Future prospective, long‐term clinical studies are warranted to formulate robust clinical recommendations for the rehabilitation of periodontally compromised dentitions.
CONFLICT OF INTEREST
The authors declare no conflict of interests.
AUTHOR CONTRIBUTIONS
Spyridon N. Papageorgiou, Georgios N. Antonoglou, Theodore Eliades, Dimitrios Michelogiannakis, Lydia Kakali, and Phoebus Madianos contributed to study conception and study design. Spyridon N. Papageorgiou, Georgios N. Antonoglou, and Theodore Eliades contributed to literature searches, study selection, risk‐of‐bias assessment, and data extraction. Spyridon N. Papageorgiou contributed to data analysis, data interpretation, and manuscript drafting. Spyridon N. Papageorgiou, Georgios N. Antonoglou, Theodore Eliades, Dimitrios Michelogiannakis, Lydia Kakali, and Phoebus Madianos contributed to critical revision of the manuscript. All authors approved the final version.
ETHICS STATEMENT
No ethical statement needed for this study.
Supporting information
Data S1. Supplementary information.
ACKNOWLEDGEMENT
Open Access Funding provided by Universitat Zurich. [Correction added on 14 April 2022, after first online publication: CSAL funding statement has been added.]
Papageorgiou, S. N. , Antonoglou, G. N. , Michelogiannakis, D. , Kakali, L. , Eliades, T. , & Madianos, P. (2022). Effect of periodontal–orthodontic treatment of teeth with pathological tooth flaring, drifting, and elongation in patients with severe periodontitis: A systematic review with meta‐analysis. Journal of Clinical Periodontology, 49(S24), 102–120. 10.1111/jcpe.13529
DATA AVAILABILITY STATEMENT
All data from this study are openly available through Zenodo (http://doi.org/10.5281/zenodo.3992750).
REFERENCES
- Aimetti, M. , Garbo, D. , Ercoli, E. , Grigorie, M. M. , Citterio, F. , & Romano, F. (2020). Long‐term prognosis of severely compromised teeth following combined periodontal and orthodontic treatment: A retrospective study. International Journal of Periodontics and Restorative Dentistry, 40, 95–102. 10.11607/prd.4523 [DOI] [PubMed] [Google Scholar]
- Almeida, R. C. , Capelli, J. , & Teles, R. P. (2015). Levels of gingival crevicular fluid matrix metalloproteinases in periodontally compromised teeth under orthodontic forces. The Angle Orthodontist, 85, 1009–1014. 10.2319/101714-744.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Artun, J. , & Urbye, K. S. (1988). The effect of orthodontic treatment on periodontal bone support in patients with advanced loss of marginal periodontium. American Journal of Orthodontics and Dentofacial Orthopedics, 93, 143–148. 10.1016/0889-5406(88)90292-2 [DOI] [PubMed] [Google Scholar]
- Attia, M. S. , Hazzaa, H. H. , Al‐Aziz, F. A. , & Elewa, G. M. (2019). Evaluation of adjunctive use of low‐level diode laser biostimulation with combined orthodontic regenerative therapy. Journal of the International Academy of Periodontology, 21, 63–73. [PubMed] [Google Scholar]
- Attia, M. S. , Shoreibah, E. A. , Ibrahim, S. A. , & Nassar, H. A. (2012). Regenerative therapy of osseous defects combined with orthodontic tooth movement. Journal of the International Academy of Periodontology, 14, 17–25. [PubMed] [Google Scholar]
- Bollen, A. M. , Cunha‐Cruz, J. , Bakko, D. W. , Huang, G. J. , & Hujoel, P. P. (2008). The effects of orthodontic therapy on periodontal health: A systematic review of controlled evidence. Journal of the American Dental Association, 139, 413–422. 10.14219/jada.archive.2008.0184 [DOI] [PubMed] [Google Scholar]
- Boyd, R. L. , Leggot, P. J. , Quinn, R. S. , Eakle, W. S. , & Chambers, D. W. (1989). Periodontal implications of orthodontic treatment in adults with reduced or normal periodontal tissues versus those of adolescents. American Journal of Orthodontics and Dentofacial Orthopedics, 96, 191–198. 10.1016/0889-5406(89)90455-1 [DOI] [PubMed] [Google Scholar]
- Boyer, S. , Fontanel, F. , Danan, M. , et al. (2011). Severe periodontitis and orthodontics: Evaluation of long‐term results. International Orthodontics, 9, 259–273. 10.1016/j.ortho.2011.06.004 [DOI] [PubMed] [Google Scholar]
- Brunsvold, M. A. (2005). Pathologic tooth migration. Journal of Periodontology, 76, 859–866. [DOI] [PubMed] [Google Scholar]
- Cappelleri, J. C. , Ioannidis, J. P. , Schmid, C. H. , de Ferranti, S. D. , Aubert, M. , Chalmers, T. C. , & Lau, J. (1996). Large trials vs meta‐analysis of smaller trials: How do their results compare? JAMA, 276, 1332–1338. [PubMed] [Google Scholar]
- Carrasco‐Labra, A. , Brignardello‐Petersen, R. , Santesso, N. , Neumann, I. , Mustafa, R. A. , Mbuagbaw, L. , Etxeandia Ikobaltzeta, I. , de Stio, C. , McCullagh, L. J. , Alonso‐Coello, P. , Meerpohl, J. J. , Vandvik, P. O. , Brozek, J. L. , Akl, E. A. , Bossuyt, P. , Churchill, R. , Glenton, C. , Rosenbaum, S. , Tugwell, P. , … Schünemann, H. J. (2016). Improving GRADE evidence tables part 1: A randomized trial shows improved understanding of content in summary of findings tables with a new format. Journal of Clinical Epidemiology, 74, 7–18. 10.1016/j.jclinepi.2015.12.007 [DOI] [PubMed] [Google Scholar]
- Chhibber, A. , Agarwal, S. , Yadav, S. , Kuo, C. L. , & Upadhyay, M. (2018). Which orthodontic appliance is best for oral hygiene? A randomized clinical trial. American Journal of Orthodontics and Dentofacial Orthopedics, 153, 175–183. 10.1016/j.ajodo.2017.10.009 [DOI] [PubMed] [Google Scholar]
- Cobb, C. M. (2002). Clinical significance of non‐surgical periodontal therapy: An evidence‐based perspective of scaling and root planing. Journal of Clinical Periodontology, 29(Suppl 2), 6–16. [PubMed] [Google Scholar]
- Cortellini, P. , Buti, J. , Pini Prato, G. , & Tonetti, M. S. (2017). Periodontal regeneration compared with access flap surgery in human intra‐bony defects 20‐year follow‐up of a randomized clinical trial: Tooth retention, periodontitis recurrence and costs. Journal of Clinical Periodontology, 44, 58–66. 10.1111/jcpe.12638 [DOI] [PubMed] [Google Scholar]
- Diedrich, P. R. (1996). Orthodontic procedures improving periodontal prognosis. Dental Clinics of North America, 40, 875–887. [PubMed] [Google Scholar]
- El‐Attar, H. , El‐Kadi, A. , Rabie, A. , Ezz‐el‐Arab, A. , Salah, N. , & Bedair. (2019). Evaluation of the combined orthodontic‐periodontal therapy in the management of extruded anterior teeth in patients with aggressive periodontitis. International Journal of Health Sciences and Research, 9, 25–38. [Google Scholar]
- Eliasson, L. A. , Hugoson, A. , Kurol, J. , & Siwe, H. (1982). The effects of orthodontic treatment on periodontal tissues in patients with reduced periodontal support. European Journal of Orthodontics, 4, 1–9. 10.1093/ejo/4.1.1 [DOI] [PubMed] [Google Scholar]
- Ericsson, I. , Thilander, B. , Lindhe, J. , & Okamoto, H. (1977). The effect of orthodontic tilting movements on the periodontal tissues of infected and non‐infected dentitions in dogs. Journal of Clinical Periodontology, 4, 278–293. 10.1111/j.1600-051x.1977.tb01900.x [DOI] [PubMed] [Google Scholar]
- Figueira, E. A. , de Rezende, M. L. , Torres, S. A. , Garlet, G. P. , Lara, V. S. , Santos, C. F. , Avila‐Campos, M. J. , da Silva, J. S. , & Campanelli, A. P. (2009). Inhibitory signals mediated by programmed death‐1 are involved with T‐cell function in chronic periodontitis. Journal of Periodontology, 80, 1833–1844. 10.1902/jop.2009.090057 [DOI] [PubMed] [Google Scholar]
- Freitas, A. O. , Marquezan, M. , Nojima, M. D. A. C. , Alviano, D. S. , & Maia, L. C. (2014). The influence of orthodontic fixed appliances on the oral microbiota: A systematic review. Dental Press Journal of Orthodontics, 19, 46–55. 10.1590/2176-9451.19.2.046-055.oar [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garat, J. A. , Gordillo, M. E. , & Ubios, A. M. (2005). Bone response to different strength orthodontic forces in animals with periodontitis. Journal of Periodontal Research, 40, 441–445. 10.1111/j.1600-0765.2005.00809.x [DOI] [PubMed] [Google Scholar]
- Gkantidis, N. , Christou, P. , & Topouzelis, N. (2010). The orthodontic periodontic interrelationship in integrated treatment challenges: A systematic review. Journal of Oral Rehabilitation, 37, 377–390. 10.1111/j.1365-2842.2010.02068.x [DOI] [PubMed] [Google Scholar]
- Guyatt, G. H. , Oxman, A. D. , Schünemann, H. J. , Tugwell, P. , & Knottnerus, A. (2011). GRADE guidelines: A new series of articles in the Journal of Clinical Epidemiology. Journal of Clinical Epidemiology, 64, 380–382. 10.1016/j.jclinepi.2010.09.011 [DOI] [PubMed] [Google Scholar]
- Han, J.‐Y. (2015). A comparative study of combined periodontal and orthodontic treatment with fixed appliances and clear aligners in patients with periodontitis. Journal of Periodontal and Implant Science, 45, 193–204. 10.5051/jpis.2015.45.6.193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins, J. P. T. , Thompson, S. G. , Deeks, J. J. , & Altman, D. G. (2003). Measuring inconsistency in meta‐analyses. BMJ, 327, 557–560. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins, J. P. T. , Thomas, J. , Chandler, J. , Cumpston, M. , Li, T. , Page, M. J. , & Welch, V. A. (Eds.). (2020). Cochrane handbook for systematic reviews of interventions version 6.1. Cochrane; www.training.cochrane.org/handbook [Google Scholar]
- Hoffmann, T. , Al‐Machot, E. , Meyle, J. , Jervøe‐Storm, P. M. , & Jepsen, S. (2016). Three‐year results following regenerative periodontal surgery of advanced intrabony defects with enamel matrix derivative alone or combined with a synthetic bone graft. Clinical Oral Investigations, 20, 357–364. 10.1007/s00784-015-1522-4 [DOI] [PubMed] [Google Scholar]
- Ioannidis, J. P. (2008). Interpretation of tests of heterogeneity and bias in meta‐analysis. Journal of Evaluation in Clinical Practice, 14, 951–957. 10.1111/j.1365-2753.2008.00986.x [DOI] [PubMed] [Google Scholar]
- Jepsen, S. , Caton, J. G. , Albandar, J. M. , Bissada, N. F. , Bouchard, P. , Cortellini, P. , Demirel, K. , de Sanctis, M. , Ercoli, C. , Fan, J. , Geurs, N. C. , Hughes, F. J. , Jin, L. , Kantarci, A. , Lalla, E. , Madianos, P. N. , Matthews, D. , McGuire, M. K. , Mills, M. P. , … Yamazaki, K. (2018). Periodontal manifestations of systemic diseases and developmental and acquired conditions: Consensus report of workgroup 3 of the 2017 World Workshop on the Classification of Periodontal and Peri‐Implant Diseases and Conditions. Journal of Clinical Periodontology, 45(Suppl 20), S219–S229. 10.1111/jcpe.12951 [DOI] [PubMed] [Google Scholar]
- Kaldahl, W. B. , Kalkwarf, K. L. , Patil, K. D. , Molvar, M. P. , & Dyer, J. K. (1996). Long‐term evaluation of periodontal therapy: I. Response to 4 therapeutic modalities. Journal of Periodontology, 67, 93–102. 10.1902/jop.1996.67.2.93 [DOI] [PubMed] [Google Scholar]
- Kassebaum, N. J. , Bernabé, E. , Dahiya, M. , Bhandari, B. , Murray, C. J. , & Marcenes, W. (2014). Global burden of severe periodontitis in 1990‐2010: A systematic review and meta‐regression. Journal of Dental Research, 93, 1045–1053. 10.1177/0022034514552491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwok, V. , & Caton, J. G. (2007). Commentary: Prognosis revisited: A system for assigning periodontal prognosis. Journal of Periodontology, 78, 2063–2071. 10.1902/jop.2007.070210 [DOI] [PubMed] [Google Scholar]
- Langan, D. , Higgins, J. P. T. , Jackson, D. , Bowden, J. , Veroniki, A. A. , Kontopantelis, E. , & Simmonds, M. (2019). A comparison of heterogeneity variance estimators in simulated random‐effects metaanalyses. Research Synthesis Methods, 10, 83–98. 10.1002/jrsm.1316 [DOI] [PubMed] [Google Scholar]
- Liu, X. F. , Pan, X. G. , & Shu, R. (2008). A preliminary study of combined periodontal‐orthodontic approach for treating labial displacement of incisors in patients with periodontal diseases. Shanghai Kou Qiang Yi Xue, 17, 264–266. [PubMed] [Google Scholar]
- Martin, C. , Celis, B. , Ambrosio, N. , Bollain, J. , Antonoglou, G. N. , & Figuero, E. (2021). Effect of orthodontic therapy in periodontitis and non‐periodontitis patients: A systematic review with meta‐analysis. Journal of Clinical Periodontology. 10.1111/jcpe.13487 [DOI] [PubMed] [Google Scholar]
- Martinez‐Canut, P. , Carrasquer, A. , Magán, R. , & Lorca, A. (1997). A study on factors associated with pathologic tooth migration. Journal of Clinical Periodontology, 24, 492–497. 10.1111/j.1600-051x.1997.tb00217.x [DOI] [PubMed] [Google Scholar]
- McKiernan, E. X. , McKiernan, F. , & Jones, M. L. (1992). Psychological profiles and motives of adults seeking orthodontic treatment. The International Journal of Adult Orthodontics and Orthognathic Surgery, 7, 187–198. [PubMed] [Google Scholar]
- Nibali, L. , Koidou, V. P. , Nieri, M. , Barbato, L. , Pagliaro, U. , & Cairo, F. (2020). Regenerative surgery versus access flap for the treatment of intra‐bony periodontal defects: A systematic review and meta‐analysis. Journal of Clinical Periodontology, 47(Suppl 22), 320–351. 10.1111/jcpe.13237 [DOI] [PubMed] [Google Scholar]
- Ogihara, S. , & Wang, H. L. (2010). Periodontal regeneration with or without limited orthodontics for the treatment of 2‐ or 3‐wall infrabony defects. Journal of Periodontology, 81, 1734–1742. 10.1902/jop.2010.100127 [DOI] [PubMed] [Google Scholar]
- Page, M. J. , Moher, D. , Bossuyt, P. M. , Boutron, I. , Hoffmann, T. C. , Mulrow, C. D. , Shamseer, L. , Tetzlaff, J. M. , Akl, E. A. , Brennan, S. E. , Chou, R. , Glanville, J. , Grimshaw, J. M. , Hróbjartsson, A. , Lalu, M. M. , Li, T. , Loder, E. W. , Mayo‐Wilson, E. , McDonald, S. , … McKenzie, J. E. (2021). PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. British Medical Journal, 372, n160. 10.1136/bmj.n160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papageorgiou, S. N. (2014a). Meta‐analysis for orthodontists: Part I—How to choose effect measure and statistical model. Journal of Orthodontics, 41, 317–326. 10.1179/1465313314Y.0000000111 [DOI] [PubMed] [Google Scholar]
- Papageorgiou, S. N. (2014b). Meta‐analysis for orthodontists: Part II—Is all that glitters gold? Journal of Orthodontics, 41, 327–336. 10.1179/1465313314Y.0000000110 [DOI] [PubMed] [Google Scholar]
- Papageorgiou, S. N. , Antonoglou, G. N. , Martin, C. , & Eliades, T. (2019). Methods, transparency and reporting of clinical trials in orthodontics and periodontics. Journal of Orthodontics, 46, 101–109. 10.1177/1465312519842315 [DOI] [PubMed] [Google Scholar]
- Papageorgiou, S. N. , Antonoglou, G. N. , Michelogiannakis, D. , Kakali, L. , Eliades, T. , & Madianos, P. (2020). Orthodontic treatment of teeth with pathological tooth flaring, drifting, and elongation among periodontitis patients: A systematic review with meta‐analysis [dataset]. Zenodo. 10.5281/zenodo.3992750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papageorgiou, S. N. , Gölz, L. , Jäger, A. , Eliades, T. , & Bourauel, C. (2016). Lingual vs. labial fixed orthodontic appliances: Systematic review and meta‐analysis of treatment effects. European Journal of Oral Sciences, 124, 105–118. 10.1111/eos.12250 [DOI] [PubMed] [Google Scholar]
- Papageorgiou, S. N. , Koletsi, D. , Iliadi, A. , Peltomaki, T. , & Eliades, T. (2020). Treatment outcome with orthodontic aligners and fixed appliances: A systematic review with meta‐analyses. European Journal of Orthodontics, 42, 331–343. 10.1093/ejo/cjz094 [DOI] [PubMed] [Google Scholar]
- Papageorgiou, S. N. , Koretsi, V. , & Jäger, A. (2017). Bias from historical control groups used in orthodontic research: A meta‐epidemiological study. European Journal of Orthodontics, 39, 98–105. 10.1093/ejo/cjw035 [DOI] [PubMed] [Google Scholar]
- Papageorgiou, S. N. , Papadelli, A. A. , & Eliades, T. (2018). Effect of orthodontic treatment on periodontal clinical attachment: A systematic review and meta‐analysis. European Journal of Orthodontics, 40, 176–194. 10.1093/ejo/cjx052 [DOI] [PubMed] [Google Scholar]
- Papageorgiou, S. N. , Xavier, G. M. , & Cobourne, M. T. (2015). Basic study design influences the results of orthodontic clinical investigations. Journal of Clinical Epidemiology, 68, 1512–1522. 10.1016/j.jclinepi.2015.03.008 [DOI] [PubMed] [Google Scholar]
- Papageorgiou, S. N. , Xavier, G. M. , Cobourne, M. T. , & Eliades, T. (2018). Effect of orthodontic treatment on the subgingival microbiota: A systematic review and meta‐analysis. Orthodontics and Craniofacial Research, 21, 175–185. 10.1111/ocr.12237 [DOI] [PubMed] [Google Scholar]
- Papapanou, P. N. , Sanz, M. , Buduneli, N. , Dietrich, T. , Feres, M. , Fine, D. H. , Flemmig, T. F. , Garcia, R. , Giannobile, W. V. , Graziani, F. , Greenwell, H. , Herrera, D. , Kao, R. T. , Kebschull, M. , Kinane, D. F. , Kirkwood, K. L. , Kocher, T. , Kornman, K. S. , Kumar, P. S. , … Tonetti, M. S. (2018). Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri‐Implant Diseases and Conditions. Journal of Periodontology, 89(Suppl 1), S173–S182. 10.1002/JPER.17-0721 [DOI] [PubMed] [Google Scholar]
- Re, S. , Cardaropoli, D. , Abundo, R. , & Corrente, G. (2004). Reduction of gingival recession following orthodontic intrusion in periodontally compromised patients. Orthodontics & Craniofacial Research, 7, 35–39. 10.1111/j.1601-6343.2004.00277.x [DOI] [PubMed] [Google Scholar]
- Reynolds, M. A. , Kao, R. T. , Camargo, P. M. , Caton, J. G. , Clem, D. S. , Fiorellini, J. P. , Geisinger, M. L. , Mills, M. P. , Nares, S. , & Nevins, M. L. (2015). Periodontal regeneration ‐ Intrabony defects: A consensus report from the AAP Regeneration Workshop. Journal of Periodontology, 86, S105–S107. 10.1902/jop.2015.140378 [DOI] [PubMed] [Google Scholar]
- Roccuzzo, M. , Marchese, S. , Dalmasso, P. , & Roccuzzo, A. (2018). Periodontal regeneration and orthodontic treatment of severely periodontally compromised teeth: 10‐year results of a prospective study. International Journal of Periodontics and Restorative Dentistry, 38, 801–809. 10.11607/prd.3756 [DOI] [PubMed] [Google Scholar]
- Sanz, I. , Alonso, B. , Carasol, M. , Herrera, D. , & Sanz, M. (2012). Nonsurgical treatment of periodontitis. The Journal of Evidence‐Based Dental Practice, 12, 76–86. 10.1016/S1532-3382(12)70019-2 [DOI] [PubMed] [Google Scholar]
- Schünemann, H. J. , Cuello, C. , Akl, E. A. , Mustafa, R. A. , Meerpohl, J. J. , Thayer, K. , Morgan, R. L. , Gartlehner, G. , Kunz, R. , Katikireddi, S. V. , Sterne, J. , Higgins, J. P. , Guyatt, G. , & GRADE Working Group . (2019). GRADE guidelines: 18. How ROBINS‐I and other tools to assess risk of bias in nonrandomized studies should be used to rate the certainty of a body of evidence. Journal of Clinical Epidemiology, 111, 105–114. 10.1016/j.jclinepi.2018.01.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serio, F. G. , & Hawley, C. E. (1999). Periodontal trauma and mobility. Diagnosis and treatment planning. Dental Clinics of North America, 43, 37–44. [PubMed] [Google Scholar]
- Shi, J. , Zhou, Y. , & Fu, M. (2003). Computer tomograghy study on periodontal patients with anterior displaced teeth before and after combined orthodontic‐periodontal treatment. Beijing Da Xue Xue Bao. Yi Xue Ban, 35, 659–662. [PubMed] [Google Scholar]
- Sideri, S. , Papageorgiou, S. N. , & Eliades, T. (2018). Registration in the international prospective register of systematic reviews (PROSPERO) of systematic review protocols was associated with increased review quality. Journal of Clinical Epidemiology, 100, 103–110. 10.1016/j.jclinepi.2018.01.003 [DOI] [PubMed] [Google Scholar]
- Sterne, J. A. , Hernán, M. A. , Reeves, B. C. , Savović, J. , Berkman, N. D. , Viswanathan, M. , Henry, D. , Altman, D. G. , Ansari, M. T. , Boutron, I. , Carpenter, J. R. , Chan, A. W. , Churchill, R. , Deeks, J. J. , Hróbjartsson, A. , Kirkham, J. , Jüni, P. , Loke, Y. K. , Pigott, T. D. , … Higgins, J. P. (2016). ROBINS‐I: A tool for assessing risk of bias in non‐randomised studies of interventions. BMJ, 355, i4919. 10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterne, J. A. C. , Savović, J. , Page, M. J. , Elbers, R. G. , Blencowe, N. S. , Boutron, I. , Cates, C. J. , Cheng, H. Y. , Corbett, M. S. , Eldridge, S. M. , Emberson, J. R. , Hernán, M. A. , Hopewell, S. , Hróbjartsson, A. , Junqueira, D. R. , Jüni, P. , Kirkham, J. J. , Lasserson, T. , Li, T. , … Higgins, J. P. T. (2019). RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ, 366, l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- Wennström, J. L. , Lindhe, J. , Sinclair, F. , & Thilander, B. (1987). Some periodontal tissue reactions to orthodontic tooth movement in monkeys. Journal of Clinical Periodontology, 14, 121–129. 10.1111/j.1600-051x.1987.tb00954.x [DOI] [PubMed] [Google Scholar]
- Weston, P. , Yaziz, Y. A. , Moles, D. R. , & Needleman, I. (2008). Occlusal interventions for periodontitis in adults. Cochrane Database of Systematic Reviews, 3. 10.1002/14651858.CD004968.pub2 [DOI] [PubMed] [Google Scholar]
- Zasciurinskiene, E. , Lund, H. , Lindsten, R. , Jansson, H. , & Bjerklin, K. (2019). Outcome of periodontal‐orthodontic treatment in subjects with periodontal disease. Part II: a CBCT study of alveolar bone level changes. European Journal of Orthodontics, 41, 565–574. [DOI] [PubMed] [Google Scholar]
- Zasciurinskiene, E. , Baseviciene, N. , Lindsten, R. , Slotte, C. , Jansson, H. , & Bjerklin, K. (2018). Orthodontic treatment simultaneous to or after periodontal cause‐related treatment in periodontitis susceptible patients. Part I: Clinical outcome. A randomized clinical trial. Journal of Clinical Periodontology, 45, 213–224. 10.1111/jcpe.12835 [DOI] [PubMed] [Google Scholar]
- Zhang, J. , Zhang, A.‐M. , Zhang, Z.‐M. , Jia, J.‐L. , Sui, X.‐X. , Yu, L.‐R. , & Liu, H.‐T. (2017). Efficacy of combined orthodontic‐periodontic treatment for patients with periodontitis and its effect on inflammatory cytokines: A comparative study. American Journal of Orthodontics and Dentofacial Orthopedics, 152, 494–500. 10.1016/j.ajodo.2017.01.028 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Supplementary information.
Data Availability Statement
All data from this study are openly available through Zenodo (http://doi.org/10.5281/zenodo.3992750).


