Abstract
Background
Enlarged facial pores are one of the common skin signs of photoaging that patients seek treatment for. However, objective data and long‐term assessment on the efficacy and safety of therapeutic procedures for this condition are limited.
Objective
To objectively evaluate the efficacy and safety of a 1064‐nm picosecond laser with microlens array (MLA) for pore tightening.
Methods
Twenty‐five patients with enlarged pores received three treatments with a 1064‐nm picosecond laser coupled with MLA at 4‐week intervals. Patients were evaluated using objective (measurement of pore volume using three‐dimensional photography) and subjective (clinical evaluation by two blinded dermatologists) assessments at baseline and at the 1‐, 3‐, and 6‐month follow‐ups. Adverse effects were also recorded during each visit.
Results
After three treatments, there was a significant reduction of pore size from baseline (p < 0.001). The improvement in pore size appearance significantly continued from the 1‐month to the 6‐month follow‐up visits (p = 0.013). The total average pore size was 1.15652 ± 0.614322 and 0.8087 ± 0.50515 at baseline and at 6 months after the final treatment, respectively, resulting in an average of 30% reduction in pore size. No cases of dyspigmentation, textural alteration, or scarring were documented.
Conclusion
Fractional 1064‐nm picosecond laser appears to be effective and safe for reducing pore size in Asians with minimal transient side effects.
Keywords: 1064‐nm, dilated pores, enlarged pores, facial pores, fractional picosecond laser, microlens array, picosecond laser
INTRODUCTION
“Enlarged” or “dilated” pores is defined as the visible topographic feature on the skin surface corresponding to enlarged openings of pilosebaceous follicles. 1 Enlarged facial pores are considered as one of the skin signs of photoaging. 2 , 3 There are several major clinical causes of enlarged facial pores, including high sebum production, decreased elasticity around pores, and increased hair follicle volume. 4 , 5 Certain exogenous and endogenous factors likewise influence the widening of pores, which includes chronic sun exposure, male gender, age, and genetic predisposition. Impairment of skin architectural components, such as collagen and elastin, around the pores can cause slackening of the pore wall. Treatment of enlarged facial pores includes chemical peeling, topical retinoic acid, oral isotretinoin, microdermabrasion, photorejuvenation, laser skin resurfacing, and fractional laser treatments, each yielding variable results. 4 , 6 Because of its multifactorial nature, treatment of enlarged facial pores has proved to be challenging as they tend to recur after discontinuation of intervention. 4 Various lasers and energy‐based devices (EBDs) have been applied in an attempt to deliver targeted thermal or ultrasound energy to the skin. 4 , 6 , 7 , 8 Their proposed mechanism of action is through the remodelling of collagen fibers near the pilosebaceous openings, resulting in diminished pore size. Lasers 9 , 10 , 11 , 12 , 13 , 14 , 15 and EBDs 16 , 17 , 18 with established collagen remodeling effects have been previously explored. However, available published data on their long‐term efficacy are limited and are usually based on subjective rather than objective assessment methods.
Fractionated picosecond handpieces have been recently developed for skin resurfacing. The high energy delivered by the fractional picosecond domain of the 1064‐ and 532‐nm Nd:YAG and 755‐nm alexandrite lasers are absorbed by intraepidermal melanin within the epidermal focal zone. Within these localized zones, an electron avalanche breakdown alternatively termed “laser‐induced optical breakdown” (LIOB) produces focal vacuoles in the epidermis in a non‐thermal manner as a result of the propagation of focal pressure waves. 19 , 20 LIOB triggers the tissue repair process and modifies cell signaling by converting energy into a pressure wave that is propagated into the dermis. This barotrauma leads to changes in the dermis, resulting in neocollagenesis and neoelastinogenesis. 20 , 21
Fractional picosecond lasers have been proven effective for the treatment of atrophic acne scars, 22 , 23 , 24 , 25 striae, 21 , 26 , 27 photodamaged skin, 14 , 28 and enlarged pores. 14 The purpose of this study then is to objectively evaluate the long‐term safety and efficacy of 1064‐nm picosecond laser with microlens array (MLA) for pore tightening in Asians.
METHODS
This was a prospective, single‐arm, nonrandomized study that aimed to investigate the safety and efficacy of a 1064‐nm picosecond laser with MLA attachment for pore tightening.
Study Population
Twenty‐five subjects with visible pores on the nose and both sides of the cheeks, as assessed by a board‐certified dermatologist, were enrolled in this study. Ages ranged from 25 to 40 years (mean age: 33.0 ± 4.2 years). Exclusion criteria included prior use of topical retinoids within the past 6 months, an immunocompromised state, photosensitivity, and history of keloid scar formation. This study was approved by the Siriraj Institutional Review Board (SIRB), Faculty of Medicine Siriraj Hospital's human research review committee, Mahidol University, Thailand (Si 379/2019), and conformed to the guidelines of the 1975 Declaration of Helsinki. Written informed consent was obtained from all study subjects before study initiation. This clinical study was registered at www.clinicaltrials.gov with identification code NCT04471948.
Intervention
A topical anesthetic, a mixture of 2.5% lidocaine and 2.5% prilocaine cream (EMLA; AstraZeneca LP), was applied to both cheeks and nose for 45 minutes before treatment. All treatment sessions were performed by an experienced laser dermatologist who was not involved in lesion assessment (A. K.). A 1064‐nm picosecond laser with MLA attachment (Enlighten; Cutera) was used. Treatment parameters were as follows: fluence, 0.8 J/cm2; spot size, 8 mm; repetitive rate, 5 Hz for two passes with approximately 15–20% of pulse overlapping. The MLA handpiece delivers an array of 180 μm diameter microbeams, containing 460 microbeams per cm2 within an 8‐mm diameter area. All subjects received three consecutive laser treatments at 4‐week intervals. Only the areas of the skin with enlarged pores present were laser irradiated. The total number of pulses received by the patients at the end of the treatment period was approximately 500–1500 depending on the extent of the pores. The endpoint of treatment was moderate erythema with mild‐to‐moderate swelling of the treated facial skin and mild‐to‐moderate purpura. A fragrance‐free and noncomedogenic moisturizing cream (Cetaphil moisturizing cream; Laboratoires Galderma) was applied four times daily for 1 week. Subjects were instructed to avoid excessive sun exposure and to wear a broad‐spectrum sunscreen with a sun protection factor (SPF) of 50 all throughout the study period after crusting had completely healed.
Evaluation
Objective assessment
Pore volume was objectively evaluated using a skin imaging device (Antera® 3D CS; Miravex Limited). A designated area with visibly enlarged pores was marked on every patient and mapped with a translucent sheet on the first visit to ensure consistency of location. The assessments were done at baseline and 1, 3, and 6 months after the final treatment.
Subjective assessment
Photographic documentation using identical camera settings, lighting, and patient positioning were obtained at baseline, and at 1, 3, and 6 months after the final treatment. All digital photographs were taken with a facial photo fixture using a Canon PowerShot G9 stand‐off camera (OMNIA Imaging System; Canfield Scientific, Inc.). Two board‐certified dermatologists (W. M. and K. C.) performed blinded clinical assessments of pore size improvement on the treatment areas using comparative photographs. The evaluators were asked to perform two actions—first, to identify the photographs that showed better pore appearance; and second, to rate the difference in the severity of the pore size enlargement using a quartile grading system. In such cases wherein the raters identified the incorrect order of the photographs, the assessment was recorded as worse. When the raters correctly identified the order of the photographs, the quartile grading scales reflected an improvement in pore size appearance (<25% difference = minimal improvement, 25–50% = moderate improvement, 51–75% = marked improvement, and 76–100% = excellent improvement).
During treatment, patients were asked to evaluate pain levels using a visual analog scale (VAS) ranging from 0 (no pain) to 10 (severe pain). Adverse events reported include erythema, postinflammatory hyperpigmentation (PIH), or hypopigmentation, and were examined by the same physician at every follow‐up visit. Patients likewise evaluated their own degree of pore size improvement from baseline photographs at 1, 3, and 6 months after the final treatment, and graded the improvement using the abovementioned quartile grading scale.
Statistical analyses
Repeated measures analysis of variance test was used to evaluate pore volume at each follow‐up visit. A p value less than 0.05 was considered to be statistically significant. All statistical data analyses were performed using PASW Statistics (formerly SPSS) version 18.0 (SPSS, Inc.).
RESULTS
Twenty‐five patients [6 (26%) males and 19 (74%) females] with Fitzpatrick skin types (FSTs) III (19/25, 76%) and IV (6/25, 24%) were enrolled in this study and completed all treatment and follow‐up sessions. After 3 treatments, there was a significant reduction of average pore volumes from baseline as measured by Antera® 3D CS (p < 0.001; Figure 1). Average pore volumes were 1.15652 ± 0.614322 and 0.8087 ± 0.50515 at baseline and at 6 months after the final treatment, resulting in an average of 30% reduction in pore size (Figure 2).
Figure 1.
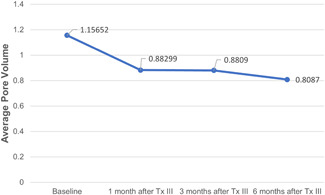
Measurement of average pore volume using Antera® 3D CS at baseline, 1 month, 3 months, and 6 months after the last treatment
Figure 2.
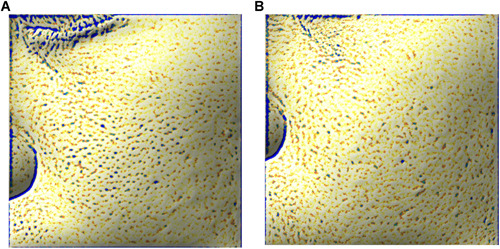
Three‐dimensional images under the small filter mode showing a topographic appearance of pores in a 34‐year‐old subject (FST IV) measured using Antera® 3D CS. (A) At baseline and (B) at 6 months after 3 monthly treatments with a 1064‐nm picosecond laser with MLA
The assessment performed by two board‐certified dermatologists revealed a weighted κ value of 0.875. None of the patients were rated to have worsening of their pore appearance after completion of all laser treatments. At 1 month after the last treatment, more than 50% of the patients showed at least 25% improvement of their pore appearance from baseline. At 6 months follow‐up after the last treatment, 48% and 28% of the patients were rated to have 25–50% and over 50% improvement of the pore size, respectively (Figures 3 and 4). The clinical improvement in the appearance of the pore size significantly continued from the 1‐month follow‐up to the 6‐month visit (p = 0.013). The average pain score during treatments was 3.205 ± 1.702 (1–10 scale).
Figure 3.
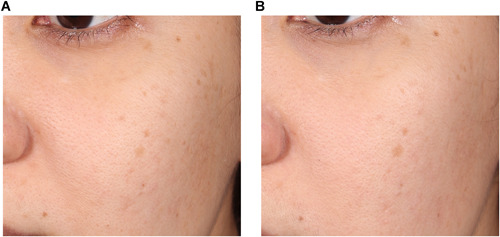
Corresponding clinical appearance of the same subject in Figure 2. (A) at baseline and (B) at 6 months after 3 monthly treatments with a 1064‐nm picosecond laser with a microlens array
Figure 4.
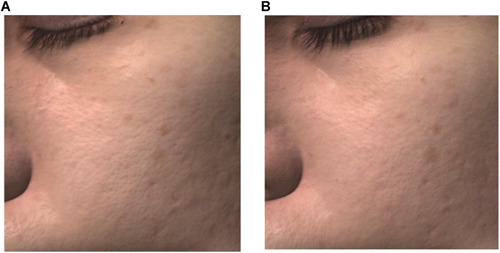
Corresponding three‐dimensional images demonstrating the clinical appearance of the same subject in Figure 2. (A) at baseline and (B) at 6 months after 3 monthly treatments with a 1064‐nm picosecond laser with a microlens array
Immediately after treatment, all patients experienced moderate erythema and mild‐to‐moderate swelling for an average of 4 days. Some purpuric spots were noted to last for 5–7 days. Patient's self‐assessment of overall pore size improvement showed that 52% of the participants rated themselves as having at least 25–50% (moderate) improvement at the 1‐month follow‐up. At the 6‐month follow‐up, 76% of the patients rated themselves as having at least moderate improvement of their pore size while 28% rated themselves as having over 50% improvement. All of the patients reported significant pore size improvement.
Adverse effects
Acneiform eruptions were observed in 14% of a total of 75 treatment sessions. All subjects with acneiform eruptions reported that the condition developed within the first 24–48 hours after laser irradiation, which spontaneously resolved a day after. No cases of postinflammatory hyperpigmentation and hypopigmentation were observed. Similarly, no incidents of scar formation were recorded.
DISCUSSION
Although the underlying causes of enlarged facial pores remain unclear, there are several potential factors that contribute to enlarged skin pores, including excessive sebum production, decreased elasticity around the pores, and increased hair follicle volume. 4 Chronic recurrent acne, sex hormones, and personal skincare regimen preferences may also affect pore size. 5 , 29 Given these different possible causes for enlarged pores, therapeutic modalities should be individualized for each patient. In fact, it is possible that multiple factors orchestrally affect the pore structure of an individual. 4 , 29 Therefore, multiple treatment modalities focusing on different modes of action may be applied for better and long‐lasting outcomes.
There are various lasers and EBDs exerting their mechanisms of action through the induction of collagen remodeling, which has been proven effective in improving the appearance of enlarged facial pores. 15 , 16 , 30 , 31 This study demonstrates the continuing improvement of the enlarged facial pores following 1064‐nm fractional picosecond laser treatment up to 6 months after the final treatment. It has been suggested that skin surface and internal structures surrounding pore openings are related to the enlargement of pore appearance. We, therefore, hypothesize that the mechanism of action for this modality involves induction of collagen remodeling around the dilated pilosebaceous openings, resulting in pore size shrinkage and smoothening of the perifollicular surface, which progressively takes place over the period of 6 months.
The average pore reduction rate following laser treatments is relatively superior to that of intense pulsed light treatment. The average pore reduction rate of 15–37%, 30%, and 40% was objectively documented following a single fractional CO2 laser, 32 three fractional 1064‐nm picosecond laser (the present study), and four 1565‐nm nonablative fractional laser 33 treatments, respectively, while the average pore reduction rate of 2.8% was reported after broadband light therapy. 18 However, the duration of the recovery time and the risk of side effects should be balanced with the efficacy of each individual treatment modality.
Due to its demonstrated effect on neocollagenesis induction, 1064‐nm Nd:YAG lasers have been widely investigated in the treatment of enlarged pores. Multiple trials have focused on varying parameters, especially pulse duration and energy density to maximize clinical outcomes. 10 , 11 , 12 , 13 , 34 Interestingly, a previous study by Roh et al. 12 showed that the Q‐switched and quasi long‐pulsed 1064‐nm Nd:YAG lasers significantly reduced both pore size and sebum output compared to the untreated control. The authors proposed that the new dermal collagen deposition in the perifollicular area is responsible for the reduction of pore size and the direct effect of the laser is accountable for the long‐term maintenance of reduced pore size and sebum level.
Using the concept of combining multiple approaches to address the different factors that influence enlarged pore appearance to achieve better outcomes, Cho et al. 9 investigated the efficacy of combined laser modalities with the expected sebaceous injury effect of a 1450‐nm diode laser, tightening effect of a Q‐switched and quasi long‐pulsed 1064‐nm Nd:YAG, and the smoothening effect of a 10,600‐nm carbon dioxide (CO2) laser. Four months after the final treatment, two treatments each of the 1450‐nm diode, Q‐switched and quasi long‐pulsed 1064‐nm Nd:YAG, and ablative fractional 10,600‐nm carbon dioxide lasers, respectively, the condition of the patient's pores were rated to have 51–75% improvement. However, the recovery time spent, the risk of adverse effects, and the cost of treatment must be taken into account with the benefit of using these multiple treatment modalities.
Theoretically, RF is another EBD that aims to manage several possible causes of enlarged pores. 16 , 35 , 36 The simultaneous thermal effect on surrounding tissues and/or the pilosebaceous unit due to tissue impedance to electrical currents aims to stimulate neocollagenesis for pore tightening and reduction of sebum secretion. 36 , 37 This assumption was confirmed by a previous study by Kim et al., 16 which demonstrated significant improvement in skin elasticity with an increase in the levels of procollagen types I and III, as well as elastin at 3 months after four bipolar fractional RF treatments.
Intense focused ultrasound is another EBD that provided favorable outcomes in reducing facial pores. 17 A previous trial reported the mean improvement scores of 1.7 ± 1.0 (1, 0–25%; 2, 26–50%; 3, 51–75%; and 4, >75% improvement) for 1.5‐mm transducer and 1.9 ± 0.8 for 3.0‐mm transducer, respectively after a single treatment. The improvement in skin elasticity as measured by a Cutometer and the reduction of sebum output as evaluated by a Sebumeter were hypothesized to be the underlying mode of action for this observation. 17
The role of seborrhea and high sebum output on pore size enlargement has gradually been explored. Recently, intradermal injection of botulinum toxin type A (BoNT‐A) has shown significant improvement of enlarged facial pores and seborrhoea lasting an average of 4 months in a controlled, split‐face study. 38 At the 1‐month assessment, both sides showed a significant reduction in sebum and pore scores, with significantly more visible improvement on the botulinum toxin‐treated side. Dermoscopy demonstrated a significant decrease in the average size of facial pores, while the optical coherence topography (OCT) demonstrated a significant increase in dermal thickness with a nonsignificant difference between BoNT‐A and saline‐treated sides. Four months after treatment, the BoNT‐A‐treated side maintained its improvement in both scores. The underlying mode of action on the decrease in sebum level was hypothesized to be the neurologic modulation and vascular regulation of BoNT‐A on sebaceous activity. 39 , 40
One shortcoming of this study and probably of most of the previous studies available is subject selection. Similar to our own protocol, most of the studies in literature did not recruit study subjects who had the same and/or single etiological cause of enlarged facial pores into the trial. This confounding factor might explain the deviated or temporary therapeutic outcomes observed. Our recent study on the treatment of enlarged pores using a variable square pulse erbium:YAG laser noted that the observed therapeutic outcomes dropped significantly at 6 months after discontinuing the treatment. This short‐term improvement may be explained by the inability of lasers and EBDs to correct all underlying causes of this condition. 30
CONCLUSIONS
This study used objective analysis to demonstrate the long‐term efficacy of using a 1064‐nm picosecond laser with MLA for the treatment of enlarged pores in dark‐skinned patients. This treatment modality appears to be safe with therapeutic outcomes persisting up to 6 months after the completion of three laser sessions.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
Palawisuth S, Manuskiatti W, Apinuntham C, Wanitphakdeedecha R, Cembrano KAG. Quantitative assessment of the long‐term efficacy and safety of a 1064‐nm picosecond laser with fractionated microlens array in the treatment of enlarged pores in Asians: A case‐control study. Lasers Surg Med. 2022;54:348–354. 10.1002/lsm.23449
Dr. Palawisuth is currently affiliated with the Department of Medicine, Panyananthaphikkhu Chonprathan Medical Center, Srinakharinwirot University, Nonthaburi, Thailand.
REFERENCES
- 1. Pierard GE, Pierard‐Franchimont C, Marks R, Paye M, Rogiers V. EEMCO guidance for the in vivo assessment of skin greasiness. The EEMCO Group. Skin Pharmacol Appl Skin Physiol. 2000;13(6):372–89. 10.1159/000029945 [DOI] [PubMed] [Google Scholar]
- 2. Bitter PH. Noninvasive rejuvenation of photodamaged skin using serial, full‐face intense pulsed light treatments. Dermatol Surg. 2000;26(9):835–42; discussion 43. 10.1046/j.1524-4725.2000.00085.x [DOI] [PubMed] [Google Scholar]
- 3. Hernandez‐Perez E, Khawaja HA, Alvarez TY. Oral isotretinoin as part of the treatment of cutaneous aging. Dermatol Surg. 2000;26(7):649–52. 10.1046/j.1524-4725.2000.99210.x [DOI] [PubMed] [Google Scholar]
- 4. Lee SJ, Seok J, Jeong SY, Park KY, Li K, Seo SJ. Facial pores: definition, causes, and treatment options. Dermatol Surg. 2016;42(3):277–85. 10.1097/dss.0000000000000657 [DOI] [PubMed] [Google Scholar]
- 5. Sugata K, Nishijima T, Kitahara T, Takema Y. Confocal laser microscopic imaging of conspicuous facial pores in vivo: relation between the appearance and the internal structure of skin. Skin Res Technol. 2008;14(2):208–12. 10.1111/j.1600-0846.2007.00281.x [DOI] [PubMed] [Google Scholar]
- 6. Dong J, Lanoue J, Goldenberg G. Enlarged facial pores: an update on treatments. Cutis. 2016;98(1):33–6. [PubMed] [Google Scholar]
- 7. Elmorsy EH, Elgarem YF, Sallam ES, Taha AAA. Fractional carbon dioxide laser versus carboxytherapy in treatment of striae distensae. Lasers Surg Med. 2021. 10.1002/lsm.23418 [DOI] [PubMed] [Google Scholar]
- 8. Seong GH, Jin EM, Ryu TU, Kim MH, Park BC, Hong SP. Fractional radiofrequency microneedling combined with fractional carbon dioxide laser treatment for striae distensae. Lasers Surg Med. 2021;53(2):219–26. 10.1002/lsm.23264 [DOI] [PubMed] [Google Scholar]
- 9. Cho SB, Noh S, Lee SJ, Kang JM, Kim YK, Lee JH. Combination of Q‐switched and quasi long‐pulsed 1064‐nm Nd:YAG laser, non‐ablative 1450‐nm diode laser, and ablative 10 600‐nm carbon dioxide fractional laser for enlarged pores. J Dermatolog Treat. 2010;21(4):258–60. 10.3109/09546630903410141 [DOI] [PubMed] [Google Scholar]
- 10. Chung H, Goo B, Lee H, Roh M, Chung K. Enlarged pores treated with a combination of Q‐switched and micropulsed 1064 nm Nd:YAG laser with and without topical carbon suspension: a simultaneous split‐face trial. Laser Ther. 2011;20(3):181–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lee CN, Kim YJ, Lee HS, Kim HS. Effects of Q‐switched and long‐pulsed 1064 nm Nd:YAG laser on enlarged facial pores. Photodermatol Photoimmunol Photomed. 2009;25(6):328–30. 10.1111/j.1600-0781.2009.00466.x [DOI] [PubMed] [Google Scholar]
- 12. Roh MR, Chung HJ, Chung KY. Effects of various parameters of the 1064 nm Nd:YAG laser for the treatment of enlarged facial pores. J Dermatolog Treat. 2009;20(4):223–28. 10.1080/09546630802647244 [DOI] [PubMed] [Google Scholar]
- 13. Schmults CD, Phelps R, Goldberg DJ. Nonablative facial remodeling: erythema reduction and histologic evidence of new collagen formation using a 300‐microsecond 1064‐nm Nd:YAG laser. Arch Dermatol. 2004;140(11):1373–76. 10.1001/archderm.140.11.1373 [DOI] [PubMed] [Google Scholar]
- 14. Yim S, Lee YH, Choi YJ, Kim WS. Split‐face comparison of the picosecond 1064‐nm Nd:YAG laser using a microlens array and the quasi‐long‐pulsed 1064‐nm Nd:YAG laser for treatment of photoaging facial wrinkles and pores in Asians. Lasers Med Sci. 2020;35(4):949–56. 10.1007/s10103-019-02906-1 [DOI] [PubMed] [Google Scholar]
- 15. Suh DH, Chang KY, Lee SJ, Song KY, Choi JH, Shin MK, et al. Treatment of dilated pores with 1410‐nm fractional erbium‐doped fiber laser. Lasers Med Sci. 2015;30(3):1135–9. 10.1007/s10103-015-1719-4 [DOI] [PubMed] [Google Scholar]
- 16. Kim JE, Lee HW, Kim JK, Moon SH, Ko JY, Lee MW, et al. Objective evaluation of the clinical efficacy of fractional radiofrequency treatment for acne scars and enlarged pores in Asian skin. Dermatol Surg. 2014;40(9):988–95. 10.1097/01.DSS.0000452625.01889.c3 [DOI] [PubMed] [Google Scholar]
- 17. Lee HJ, Lee KR, Park JY, Yoon MS, Lee SE. The efficacy and safety of intense focused ultrasound in the treatment of enlarged facial pores in Asian skin. J Dermatolog Treat. 2015;26(1):73–7. 10.3109/09546634.2013.868862 [DOI] [PubMed] [Google Scholar]
- 18. Yu W, Han Y, Wu X, Shang Y, Ying H, Ma G, et al. A split‐face randomized controlled trial of treatment with broadband light for enlarged facial pores. J Dermatolog Treat. 2019:1–5. 10.1080/09546634.2019.1698701 [DOI] [PubMed] [Google Scholar]
- 19. Kim H, Hwang JK, Jung M, Choi J, Kang HW. Laser‐induced optical breakdown effects of micro‐lens arrays and diffractive optical elements on ex vivo porcine skin after 1064 nm picosecond laser irradiation. Biomed Opt Express. 2020;11(12):7286–98. 10.1364/BOE.410991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tanghetti EA. The histology of skin treated with a picosecond alexandrite laser and a fractional lens array. Lasers Surg Med. 2016;48(7):646–52. 10.1002/lsm.22540 [DOI] [PubMed] [Google Scholar]
- 21. Fusano M, Galimberti MG, Bencini M, Guida S, Bencini PL. Picosecond laser treatment of striae distensae: in vivo evaluation of results by 3D analysis, reflectance confocal microscopy, and patient's satisfaction. Lasers Surg Med. 2021. 10.1002/lsm.23401 [DOI] [PubMed] [Google Scholar]
- 22. Tanghetti Md E , Jennings J. A comparative study with a 755 nm picosecond Alexandrite laser with a diffractive lens array and a 532 nm/1064 nm Nd:YAG with a holographic optic. Lasers Surg Med. 2018;50(1):37–44. 10.1002/lsm.22752 [DOI] [PubMed] [Google Scholar]
- 23. Chayavichitsilp P, Limtong P, Triyangkulsri K, Pratumchart N. Comparison of fractional neodymium‐doped yttrium aluminum garnet (Nd:YAG) 1064‐nm picosecond laser and fractional 1550‐nm erbium fiber laser in facial acne scar treatment. Lasers Med Sci. 2020;35(3):695–700. 10.1007/s10103-019-02891-5 [DOI] [PubMed] [Google Scholar]
- 24. Dai YX, Chuang YY, Chen PY, Chen CC. Efficacy and safety of ablative resurfacing with a high‐energy 1,064 Nd‐YAG picosecond‐domain laser for the treatment of facial acne scars in Asians. Lasers Surg Med. 2020;52(5):389–95. 10.1002/lsm.23151 [DOI] [PubMed] [Google Scholar]
- 25. Zhang M, Fang J, Wu Q, Lin T. Evaluation of the safety and efficacy of a picosecond alexandrite laser with DLA for acne scars in Chinese patients. Lasers Surg Med. 2020;52(2):176–81. 10.1002/lsm.23177 [DOI] [PubMed] [Google Scholar]
- 26. Haimovic A, Brauer JA, Cindy Bae YS, Geronemus RG. Safety of a picosecond laser with diffractive lens array (DLA) in the treatment of Fitzpatrick skin types IV to VI: a retrospective review. J Am Acad Dermatol. 2016;74(5):931–6. 10.1016/j.jaad.2015.12.010 [DOI] [PubMed] [Google Scholar]
- 27. Zaleski‐Larsen LA, Jones IT, Guiha I, Wu DC, Goldman MP. A comparison study of the nonablative fractional 1565‐nm Er: glass and the picosecond fractional 1064/532‐nm Nd: YAG lasers in the treatment of striae alba: A split body double‐blinded trial. Dermatol Surg. 2018;44(10):1311–16. 10.1097/DSS.0000000000001555 [DOI] [PubMed] [Google Scholar]
- 28. Weiss RA, McDaniel DH, Weiss MA, Mahoney AM, Beasley KL, Halvorson CR. Safety and efficacy of a novel diffractive lens array using a picosecond 755 nm alexandrite laser for treatment of wrinkles. Lasers Surg Med. 2017;49(1):40–4. 10.1002/lsm.22577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kim BY, Choi JW, Park KC, Youn SW. Sebum, acne, skin elasticity, and gender difference—Which is the major influencing factor for facial pores? Skin Res Technol. 2013;19(1):e45–53. 10.1111/j.1600-0846.2011.00605.x [DOI] [PubMed] [Google Scholar]
- 30. Phothong W, Manuskiatti W, Cembrano KAG, Wanitphakdeedecha R, Bowornsathitchai N. The efficacy and safety of a variable square pulse (VSP) Erbium:YAG laser for treatment of enlarged pores in Asians. Lasers Surg Med. 2020;53(5):597–42. 10.1002/lsm.23342 [DOI] [PubMed] [Google Scholar]
- 31. Saedi N, Petrell K, Arndt K, Dover J. Evaluating facial pores and skin texture after low‐energy nonablative fractional 1440‐nm laser treatments. J Am Acad Dermatol. 2013;68(1):113–8. 10.1016/j.jaad.2012.08.041 [DOI] [PubMed] [Google Scholar]
- 32. Park CS, Park JH, Kim CR, Lee JH. Objective analysis of volume restoration in atrophic acne scars and skin pores: a split study using human stem cell‐conditioned media. J Dermatolog Treat. 2021;32(1):73–7. 10.1080/09546634.2019.1628915 [DOI] [PubMed] [Google Scholar]
- 33. Yu W, Zhu J, Ma G, Yang J, Qiu Y, Chen Y, et al. Randomized split‐face, controlled comparison of treatment with 1565‐nm nonablative fractional laser for enlarged facial pores. Br J Dermatol. 2018;178(4):e271–e2. 10.1111/bjd.16115 [DOI] [PubMed] [Google Scholar]
- 34. Wattanakrai P, Rojhirunsakool S, Pootongkam S. Split‐face comparison of long‐pulse‐duration neodymium‐doped yttrium aluminum garnet (Nd:YAG) 1,064‐nm laser alone and combination long‐pulse and Q‐switched Nd:YAG 1,064‐nm laser with carbon photoenhancer lotion for the treatment of enlarged pores in Asian women. Dermatol Surg. 2010;36(11):1672–80. 10.1111/j.1524-4725.2010.01717.x [DOI] [PubMed] [Google Scholar]
- 35. Cho SI, Chung BY, Choi MG, Baek JH, Cho HJ, Park CW, et al. Evaluation of the clinical efficacy of fractional radiofrequency microneedle treatment in acne scars and large facial pores. Dermatol Surg. 2012;38(7 Pt 1):1017–24. 10.1111/j.1524-4725.2012.02402.x [DOI] [PubMed] [Google Scholar]
- 36. Lee KR, Lee EG, Lee HJ, Yoon MS. Assessment of treatment efficacy and sebosuppressive effect of fractional radiofrequency microneedle on acne vulgaris. Lasers Surg Med. 2013;45(10):639–47. 10.1002/lsm.22200 [DOI] [PubMed] [Google Scholar]
- 37. Park JY, Lee EG, Yoon MS, Lee HJ. The efficacy and safety of combined microneedle fractional radiofrequency and sublative fractional radiofrequency for acne scars in Asian skin. J Cosmet Dermatol. 2016;15(2):102–7. 10.1111/jocd.12195 [DOI] [PubMed] [Google Scholar]
- 38. Sayed KS, Hegazy R, Gawdat HI, Abdel Hay RM, Ahmed MM, Mohammed FN, et al. The efficacy of intradermal injections of botulinum toxin in the management of enlarged facial pores and seborrhea: a split face‐controlled study. J Dermatolog Treat. 2020;1–7. 10.1080/09546634.2019.1708241 [DOI] [PubMed] [Google Scholar]
- 39. Wang J, Rieder EA. A systematic review of patient‐reported outcomes for cosmetic indications of botulinum toxin treatment. Dermatol Surg. 2019;45(5):668–88. 10.1097/DSS.0000000000001878 [DOI] [PubMed] [Google Scholar]
- 40. Zouboulis CC, Baron JM, Böhm M, et al. Frontiers in sebaceous gland biology and pathology. Exp Dermatol. 2008;17(6):542–51. 10.1111/j.1600-0625.2008.00725.x [DOI] [PubMed] [Google Scholar]


