Abstract
Aim
Aim of this study is to systematically review and synthesize available evidence to identify the association between nurse staffing methodologies and nurse and patient outcomes.
Design
Systematic review and narrative synthesis.
Data sources
A search of MEDLINE (EBSCO), CINAHL (EBSCO) and Web of Science was conducted for studies published in English between January 2000 and January 2020.
Review methods
The reporting of this review and narrative synthesis was guided by the preferred reporting items for systematic and meta‐analysis guidelines (PRISMA) statement and data synthesis guided by the Synthesis Without Meta‐analysis (SWiM) guideline. The quality of each article was assessed using the Mixed Methods Appraisal Tool.
Results
Twenty‐two studies met the inclusion criteria. Twenty‐one used the mandated minimum nurse‐to‐patient ratio methodology and one study assessed the number of nurse hours per patient day staffing methodology. Both methodologies were mandated. All studies that reported on nurse outcomes demonstrated an improvement associated with the implementation of mandated minimum nurse‐to‐patient ratio, but findings related to patient outcomes were inconclusive.
Conclusions
Evidence on the impact of specific nurse staffing methodologies and patient and nurse outcomes remains highly limited. Future studies that examine the impact of specific staffing methodologies on outcomes are required to inform this fundamental area of management and practice.
Keywords: nurse outcomes, nurse staffing, patient outcomes, systematic review, workload methodologies
What problem did the study address?
The review extends knowledge on the impact of the implementation of specific nurse staffing methodologies and the impact on patient or nurse outcomes.
What were the main findings?
Nurse related outcomes improved following the implementation of mandated minimum nurse‐to‐patient ratios, however, findings related to patient outcomes were inconclusive.
Where and on whom will the research have an impact?
Refinement of research design and measures of patient and nurse outcomes are needed for the field to advance.
1. INTRODUCTION
For over two decades, research has extensively examined the link between nurse staffing, nursing workloads, skill mix and quality of patient care (Aiken et al., 2014; Duffield et al., 2011; Kane et al., 2007; Needleman et al., 2011). This work has been facilitated by the development and adoption of Nurse Sensitive Outcomes (NSOs), as a direct measure of a nurse's contribution to quality patient care. An NSO is defined as a hospital acquired patient event that is considered sensitive to nurse staffing levels (Kane et al., 2007; Needleman et al., 2002). NSOs include central nervous system (CNS) complications, deep vein thrombosis (DVT), pressure injury, Gastro‐intestinal (GI) bleeding, pneumonia, sepsis, shock/cardiac arrest, Urinary tract infection (UTI), failure to rescue, mortality, length of stay, physiologic/metabolic derangement, pulmonary failure and surgical wound infection (Needleman et al., 2001).
Evidence suggests inadequate nurse staffing creates an increase in nursing workload and the ability of nurses to provide the necessary oversight in care, leading to an increase in adverse events related to NSOs (Duffield et al., 2006). For example, lower nurse staffing levels on a ward has been associated with a higher rate of drug administration errors, more episodes of care left undone and more episodes of missed nursing care (Ball et al., 2018; Griffiths et al., 2018a). In the United States of America, a 2% increase in the rate of patient death was identified for patients exposed to a shift with eight or more hours below the defined target staffing level (Needleman et al., 2011). Likewise, in 168 adult general hospitals the addition of one more patient per nurse, increased the rate of motility within 30 days of admission by 7% and increased the risk of failure to rescue (Aiken et al., 2002).
In addition, having adequate hours of care provided by a registered nurse (RN) is important for the early recognition and management of patient deterioration (Dalton et al., 2018). Needlemen et al. (2002), identified that higher number of care hours provided by a registered nurse resulted in a reduction in the rate of failure to rescue. Similarly, in an Australian study the rate of seven NSOs reduced as a result of increasing RN hours by 10% (Roche et al., 2012). Kane et al., (2007) identified that an increase in 1 RN per patient day was associated with a decrease in the odds of hospital acquired pneumonia, unplanned extubation, respiratory failure and a lower risk of failure to rescue in surgical patients and a reduction in the length of stay for intensive care patients. Therefore, the ability to determine adequate nurse staffing levels required in a given setting over time is vital in order to provide safe, quality and affordable care (Saville et al., 2019).
2. BACKGROUND
A number of reviews describe the myriad of approaches available to determine adequate nurse staffing levels (Duffield et al., 2006; Fasoli & Haddock, 2010; Griffiths et al., 2020; Twigg & Duffield, 2009). These include, but are not limited to, professional judgement, simple volume‐based methods (such as patient‐to‐nurse ratios), benchmarking, inpatient prototype classification (such as safer nursing care tool) and timed‐task approaches (Griffiths et al., 2020). Despite the existence of many nurse staffing methods, an international consensus on the most appropriate and effective method to determine optimal nurse staffing across settings does not exist (Whitehead & Myers, 2016). As such, institutions around the world have adopted different methods to manage nurse staffing levels.
California was the first state in the United States that introduced minimum nurse‐to‐patient ratios across hospitals (Coffman et al., 2002). The method shows a 1:3 ratio of one nurse to three patients, which became mandated by law in 1999 (Donaldson et al., 2005; Olley et al., 2019). The method gained international acceptance, due to its simplicity, being implemented in two Australian states, Victoria and Queensland in 2001 and 2016 respectively (Gerdtz & Nelson, 2007; Lasman et al., 2019; Olley et al., 2019). In Australia, nurse‐ to‐ patient ratios are established at the ward level with the intention to reflect patient acuity, in that the more acutely unwell patients are assigned to nurses with fewer patients (Duffield et al., 2006). However, the difficulty with this method is determining the optimal ratio of nurses for each ward based on patient and staffing characteristics. For example, Duffield et al., (2019) conducted a study of nurses working on a ward mandated with a 1:4 nurse‐to‐patient ratios and identified an inconsistency in the allocation of patients with some nurses being allocated four very sick patients. As a result, the workload of some nurses was higher than those of others.
In 2002, The Nursing Hours Per Patient Day (NHPPD) method was introduced in the state of Western Australia (Twigg & Duffield, 2009). This method was mandated by the Australian industrial relations commission in response to industrial unrest amongst nursing staff (Australian Industrial Relations Commission, 2002). The method uses a bottom up approach and classifies each setting (e.g., ward) into seven categories based on the complexity of patient care required. From the ward categorization the number of nurse hours can be determined (Department of Health, 2019). The Department of Health Ireland is in the developmental stages of implementing the WA NHPPD model into adult hospitals (Drennan et al., 2018).
Other countries have adopted staffing tools and patient clarification systems to assist with nurse staffing decision making. In England, the National Health Service (NHS) uses the “Safer Nursing Care Tool”. The tool is designed to support decision making around nurse staffing required on a given ward, however, it is not mandated (Department of Health, 2018; National Quality Board, 2016). In 2016, Wales introduced a Nurse Staffing Levels Act into hospitals where the nurse‐to‐patient ratio is allocated based on professional judgement, patient acuity and quality indicators (Welsh Government, 2016). Most Nordic countries use a patient classification system, known as RAFAELA, to determine the staffing level required to deliver an acceptable intensity of nursing work for a given set of patients in a given setting (Fagerström & Rauhala, 2007). Despite the different methodologies and tools used across the globe, all approaches hold central the aim of creating working conditions that allow nurses to provide safe and effective care.
Whilst the evidence widely acknowledges that in a broad sense, staffing impacts on the quality and safety of patient care, this review has focussed on studies that investigated the impact of staffing as informed by a staffing methodology on patient and nurse outcomes. It extends the knowledge generated through earlier reviews that focused on the impact of minimum nurse‐to‐patient ratios on patient and nurse outcomes (Donaldson & Shapiro, 2010; Serratt, 2013a, 2013b) and were restricted to the inclusion of studies conducted in California from 2004 to 2012. This paper presents a comprehensive review of the association between nurse staffing methodologies and patient and nurse outcomes that extends beyond the focus of earlier reviews.
3. THE REVIEW
3.1. Aim
Aim of this study is to systematically review and synthesize available evidence to identify the association between the implementation of a nurse staffing methodology and nurse and patient outcomes.
3.2. Design
The study protocol was registered with PROSPERO, international prospective register of systematic reviews [CRD42020156717]. The reporting of this systematic review was guided by the Preferred Reporting Items for Systematic Reviews and Meta analyses (PRISMA) guidelines (Moher et al., 2015). For the intervention, this review considered studies that addressed nurse staffing methods, such as nurse‐to‐patient ratios, nursing hours per patient data, acuity‐based staffing and their impact on patient safety and nurse workforce outcomes. Studies with a focus on nursing skill‐mix were not considered in the review. The comparators were existing nurse staffing levels or nurse staffing strategy.
3.3. Search methods
A health information librarian was consulted during the development of the search strategy and Medical Subject Headings (MeSH) (see online resources for a list of terms used). Studies were identified through searching the following electronic databases, Medline (EBSCO), CINAHL (EBSCO) and Web of Science. In addition, an EBSCO host Alert Notification and a Web of Science Search Alert were set up to capture any new publications. Forward citation searching and hand searching of reference lists of included studies were also conducted.
Inclusion criteria were studies that assessed patient and/or nurse outcomes pre and post implementation of the specific nurse staffing methodology or studies that compared patient and nurse outcomes between two comparable organizations implementing different nurse staffing methodologies; written in English and published between from January 1, 2000, to March 2020; conducted in a hospital or aged care setting; conducted in high income countries according to the 2016 World Bank classification system; and outcomes reported as quantitative data. Excluded from this current review were studies conducted in the community, research presented as editorials, letters and at conferences and grey literature. Also excluded were studies that focused on staffing tools or patient classification systems.
3.4. Search outcomes
The initial search resulted in a total of 8474 articles. After removing duplicates in Endnote, 6837 titles and abstracts were exported to Rayyan QCRI for title/abstract screening (Ouzzani et al., 2016). Each title/abstract was independently screened against the inclusion criteria by three reviewers, 6733 articles were excluded. At the title/abstract stage, 104 studies were eligible for full text screening. Two reviewers independently reviewed each full text article. Any disagreement between the reviewers was resolved by discussion. One additional article was included via hand searching resulting in 23 articles for data abstraction (Figure 1).
FIGURE 1.
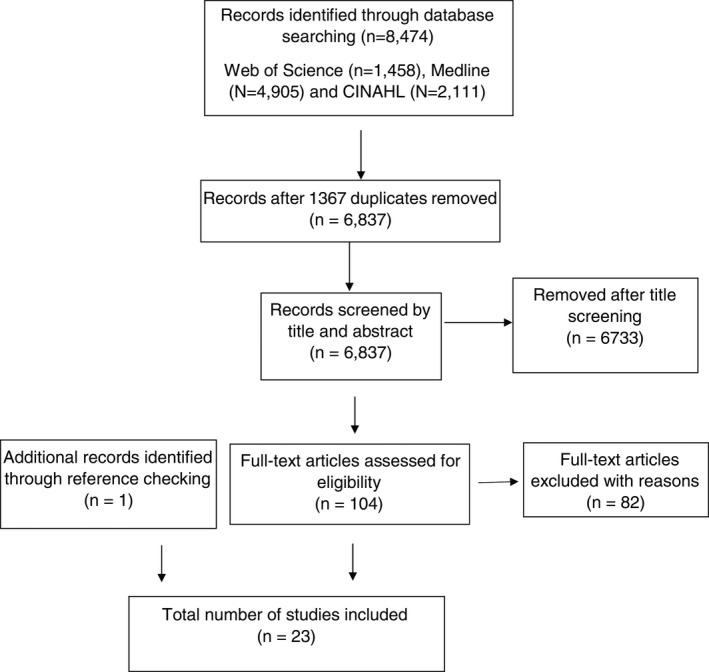
Search and retrieval process
3.5. Quality appraisal
Twenty‐two eligible studies were critically appraised by two independent reviewers using the Mixed Methods Appraisal Tool (MMAT) (Hong et al., 2018). The tool is not limited to the appraisal of mixed methods studies and is able to accommodate a variety of study designs. We used the screening items for quantitative nonrandomized studies.
Two reviewers completed the assessment of methodological quality of each paper review independently and then compared and discussed the ratings and discrepancies. Six discrepancies were noted where one reviewer assessed the item as “can't tell” and the other “no”. Following robust discussion, agreement was reached on all items. Any discrepancies in the appraisal were resolved with discussion. The quality appraisal is reported by item for each paper (Table 1).
TABLE 1.
Quality appraisal report for included studies
| Are there clear research questions? | Do the collected data allow to address the research question? | Are the participants representative of the target population? | Are measurements appropriate regarding both the outcome and intervention (or exposure)? | Are there complete outcome data? | Are the confounders accounted for in the design and analysis? | During the study period, is the intervention administered (or exposure occurred) as intended? | |
|---|---|---|---|---|---|---|---|
| Burnes & Bolton (2007) | Yes | Yes | Can’t tell | Yes | Yes | Yes | Yes |
| Bowblis & Ghattas, (2017) | Yes | Yes | Can’t tell | Yes | Yes | Yes | Yes |
| Chan et al., (2010) | Yes | Yes | Yes | No | Yes | Yes | Yes |
| Chen, (2015) | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Cook et al., (2012) | Yes | Yes | Yes | Yes | Can’t tell | Yes | Yes |
| Cox et al., (2005) | Yes | Yes | Can’t tell | Yes | Can’t tell | No | Yes |
| Donaldson et al., (2005) | Yes | Yes | Can’t tell | Yes | Yes | Yes | Yes |
| Hickey et al., (2011) | Yes | Yes | Can’t tell | Yes | Can’t tell | Yes | Yes |
| Hodgson et al., (2016) | Yes | Yes | Can’t tell | Yes | Yes | Yes | Yes |
| Law et al., (2018) | Yes | Yes | Can’t tell | Yes | Yes | Yes | Yes |
| Leigh et al., (2015) | Yes | Yes | Yes | Yes | Can’t tell | Yes | Yes |
| Mark et al., (2013) | Yes | Yes | Yes | No | Can’t tell | Yes | Yes |
| Matsudaira, (2014) | Yes | Yes | Can’t tell | Yes | Yes | Yes | Yes |
| Park & Stearns, (2009) | Yes | Yes | Yes | Yes | Can’t tell | Yes | Yes |
| Spetz et al., (2008) | Yes | Yes | Can’t tell | Yes | Can’t tell | Yes | Yes |
| Spetz & Herrera, (2010) | Yes | Yes | Can’t tell | No | Can’t tell | Yes | Yes |
| Spetz et al., (2013) | Yes | Yes | Can’t tell | Yes | Can’t tell | Yes | Yes |
| Tellez, (2012) | Yes | Yes | Can’t tell | Yes | Can’t tell | No | Yes |
| Tellez & Seago, (2013) | Yes | Yes | Can’t tell | Yes | Can’t tell | No | Yes |
| Twigg et al., (2011) | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Weichenthal & Hendry, (2011) | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Zhang & Grabowski, (2004) | Yes | Yes | Can’t tell | Yes | Yes | Yes | Yes |
3.6. Data abstraction
The following data were abstracted from eligible studies; country, setting, study population, aim, study design, nurse staffing methodology, patient and nurse outcomes, type of analysis, factors controlled for in the analysis and general findings.
3.7. Synthesis
Due to the heterogeneity of study designs used and the outcomes measured, a meta‐analysis of the data could not be conducted. Instead a narrative synthesis of the data is presented guided by the Synthesis Without Meta‐analysis guideline (Campbell et al., 2020). We grouped studies according to the staffing method intervention (mandated minimum nurse‐to‐patient ratio methodology and the number of nurse hours per patient day staffing methodology) and the outcomes (impact on patient outcomes, impact on staff outcomes). The studies were highly variable in how they reported outcomes (the metric for each outcome). Where p values were reported these were included. Where there was a similarity in the outcomes reported and the method of reporting, these findings were compared. Where they differed, the outcomes were grouped by type of outcomes, for example, wound infection, and the direction of the finding reported. The nature of the data did not allow for an examination of heterogeneity in reported effects or an assessment of the certainty of the synthesized findings. The limitations of the methods of synthesis have been included and how these have affected the conclusions drawn.
4. RESULTS
4.1. Included studies and their characteristics
Twenty‐two studies assessed the mandated minimum nurse‐to‐patient ratios and one study assessed the impact of Nursing Hours Per Patient Day. The characteristics of the included studies are summarized and presented in Table 2 (a detailed table of study characteristics can be found in the online resources). The included studies (n = 22) were conducted in a range of settings including general medical, general surgical, combined medical/surgical, step down units, emergency departments, intensive care and nursing homes/aged care. Twenty‐one studies were conducted in the United States, predominantly California and one study were conducted in Western Australia.
TABLE 2.
Summary of the characteristics of the included stusdies (a full list of all study characteristics can be viewed online)
| Author, year, country, study design | Aims | Key findings |
|---|---|---|
| Nursing hours per patient day | ||
|
(Twigg et al., 2011) Australia Retrospective cohort study |
To determine the impact of implementing the NHPPD staffing method on the incidence of nursing‐sensitive outcomes. | The study found a significant decrease in the rates of nine nurse‐sensitive outcomes following implementation of NHPPD; mortality, central nervous system complications, pressure ulcers, deep vein thrombosis, sepsis, ulcer/gastritis/upper gastrointestinal bleed shock/cardiac arrest, pneumonia and average length of stay. |
| Minimum nurse to patient ratios | ||
|
(Bowblis & Ghattas, 2017) USA Retrospective cohort |
To identify the impact of minimum quality standard regulations on nursing home staffing, quality, and exit decisions. | Higher staffing levels were associated with a statistically significant reduction in contractures and the use of physical restraint. All other quality measures showed no statistically significant impact post implementation of staffing regulations. |
|
(Burnes Bolton et al., 2007) USA Cross sectional survey |
To examine the impact of mandated nursing ratios in California on key measures of nursing quality among adults in acute care hospitals. | The study found no significant improvement in the rate of falls or falls with injury; hospital‐acquired pressure ulcers; or restraint use post regulation |
|
(Chan et al., 2010) USA Prospective Cohort Observational comparative study |
To evaluate the effect of mandated nurse–patient ratios (NPRs) on emergency department (ED) patient flow after 1year implementation. "Within the mandate ratio" vs "outside the mandate ratio". | A shorter wait time to be seen was observed when the emergency department was within the mandated ratio. Care time for patients seen in an “out of ratio” environment was 37% longer than those patients seen in an environment “within ratio. |
|
(Chen & Grabowski, 2015) USA Longitudinal |
To explore the causal relationship between the imposition of minimum nurse staffing standards in nursing homes and outcomes including nursing home staffing and quality of care in California/Ohio compared to other states. |
Staffing regulations in California/Ohio were found to improve contractures, but other quality measures (physical restraints, antipsychotic medications, pressure ulcers, and catheters) remained unchanged post implementation of minimum staffing standards. |
|
(Cook et al., 2012) USA Cross sectional study |
To evaluate the impact of California Assembly Bill 394, which mandated maximum levels of patients per nurse in the hospital setting. | The study did not identify any significant change between the rates of pressure sore and failure to rescue post implementation of the mandated nurse to patient ratios. |
|
(Cox et al., 2005) USA Cross‐sectional |
To evaluate the influence of nursing workforce regulation on nurses’ perceptions of their work environment. | Nurses working in California reported greater satisfaction but no difference in “intent to stay” post implementation of the mandated nurse‐to‐patient ratios. |
|
(Donaldson et al., 2005) USA Cross‐sectional |
To assess the unit‐level impact of California's mandated nurse‐to‐ patient ratios on licensed nurse staffing and patient care quality in medical, surgical and definitive observation units. | The study found no significant improvement in falls and falls with injury; hospital‐acquired pressure ulcers; restraint use post implementation of mandated ratios. |
|
(Hickey et al., 2011) USA Retrospective cohort |
To examine the impact of staffing ratios on risk‐adjusted outcomes for paediatric cardiac surgery programs in California and relative other states combined. | Compared to hospitals in other states, California hospitals experienced a decrease in standardized mortality ratios but an increase of in standardized complication ratios. |
|
(Hodgson et al., 2016) USA Quasi‐experiment |
To compare anxiety and mood disorder secondary diagnoses among patients who were admitted for pneumonia before and after implementation of mandated patient‐to‐nurse ratios. | Hospitals in California, post implementation of mandated ratios, reported improvement in the detection of secondary depression and anxiety in patients with pneumonia. The increase in the number of secondary diagnosis was related to the reduction in the number of patients per nurse. |
|
(Law et al., 2018) USA Retrospective cohort |
To assess whether Massachusetts legislation directed at Intensive care unit (ICU) nurse staffing was associated with improvements in patient outcomes. | The study reported no changes in rate of mortality or complications post implementation of stat‐wide staffing regulations. |
|
(Leigh et al., 2015) USA Retrospective cohort |
To determine whether state‐mandated minimum nurse‐to‐patient staffing ratios in California hospitals had an effect on reported occupational injury and illness rates as compared to 49 other states and the district of Columbia | Nurse‐to‐patient ratios were associated with 55.57 and 93.23 fewer occupational injuries and illnesses per 10,000 registered nurses and licensed practical nurses per year, respectively, as compared to 49 other states and the district of Columbia, without such ratios. |
|
(Mark et al., 2013) USA Cross sectional |
To determine whether, following implementation of California's minimum nurse staffing legislation, changes in acuity‐adjusted nurse staffing and quality of care in California hospitals outpaced similar changes in hospitals in comparison states without such regulations. | Infections, due to medical care, increased significantly in some Californian hospitals compared to hospitals in other states without mandated nurse‐to‐patient ratios. Postoperative sepsis was not significantly different in the Californian based hospitals when compared to hospitals in other states that had not implemented nurse‐to‐patient ratios. However, failure to rescue decreased significantly in some California hospitals in comparison to other states during 2000–2006 following the California minimum nurse staffing legislation. |
|
(Matsudaira, 2014) USA Retrospective cohort |
To assess the causal impact of a law requiring a minimum threshold of nurse staff per patient on the quality of health care provided by nursing homes in California. | There was no statistically significant change in the use of restraints, pressure sores or the use of urinary catherization post implementation of minimum staffing legislation for nursing homes. |
|
(Park & Stearns, 2009) USA Natural experiment |
To investigate the impact of state minimum staffing standards on the level of staffing and quality of nursing home care. | None of the quality of care outcomes: pressure ulcers, contractures, or incontinence, catheter use was significantly associated with an increase in minimum standards of staffing. The use of urinary catheters as a process of care was also not significantly significant. The rate of restraint use declined significantly post increase of minimum standards. |
|
(Spetz, 2008) USA Cross sectional study |
This article examines whether nurses who work in hospitals in California have perceived improvements in their working conditions. | There was a significant increase in overall job satisfaction (in other specific satisfaction variables) between 2004 and 2006 |
|
(Spetz & Herrera, 2010) USA Cross sectional |
To examine whether there were improvements in the satisfaction of hospital‐employed registered nurses (RNs) in the mid−2000s. | The odds of a nurse being satisfied or very satisfied with their job overall were higher in 2008 than in 2004 |
|
(Spetz et al., 2013) USA Longitudinal study |
To test whether changes in staffing following the implementation of mandated patient‐to‐nurses ratios led to change in patient safety. | The implementation of the staffing mandate in California, resulted in, a significant increase in six NSOs in hospitals with the lowest pre‐regulation staffing as compared to hospitals with the highest pre‐regulation staffing. |
|
(Tellez, 2012) USA Cross sectional |
To evaluate the effect of the nurse‐to‐patient ratios law on nurse job satisfaction in order to advance the debate over the merits of the law. | The enactment of mandated minimum nurse‐to‐patient ratios in Californian hospitals has proven to be effective in improving nurse outcomes, such as intention to stay, job satisfaction. |
|
(Tellez & Seago, 2013) USA Cross sectional |
To explore the effects on the minimum nurse‐patient staffing legislation on the demographic, human capital, and work characteristics of the working RN population, focusing specifically on direct care nurses in the acute care setting. | An increase in nurse satisfaction was observed after the minimum staffing law was implemented. |
|
(Weichenthal & Hendey, 2011) USA Retrospective cohort |
The aim of the study was to look at the association between nursing ratios and quality of care in an urban teaching Emergency Department (ED). | Overall there was a decrease in patients that left without being seen, a decrease in the time to give antibiotics to patients with pneumonia and no significant difference in the number of reported medication errors or the rate of aspirin administration for acute coronary syndrome patients. Some unexpected negative consequences were identified with all wait times increasing post implementation. |
|
(Zhang & Grabowski, 2004) USA Retrospective cohort |
To examine whether the nursing home reform Act (NHRA) improved nursing home staffing and quality. | There was a significant decrease in the proportion of residents with pressure ulcers, physical restraints, and urinary catheters following the implementation of the NHRA. |
The study design used in the studies varied where: Nine studies used a cross‐sectional design (Burnes Bolton et al., 2007; Cook et al., 2012; Cox et al., 2005; Donaldson et al., 2005; Mark et al., 2013; Spetz, 2008; Spetz & Herrera, 2010; Tellez, 2012; Tellez & Seago, 2013), eleven were cohort studies (Bowblis & Ghattas, 2017; Chan et al., 2010; Chen & Grabowski, 2015; Hickey et al., 2011; Law et al., 2018; Leigh et al., 2015; Matsudaira, 2014; Spetz et al., 2013; Twigg et al., 2011; Weichenthal & Hendey, 2011; Zhang & Grabowski, 2004) and two quasi experimental studies (Hodgson et al., 2016; Park & Stearns, 2009).
Nearly two thirds of the studies (14/22) did not provide enough background information on the study sample to allow an assessment of whether the participants were representative of the target population. Studies mostly drew from existing databases that required institutions to report data on an annual basis. An overview of representation at the data collection level was often not provided. In addition, a number of studies excluded subsets of data according to their inclusion/exclusion criteria but did not report on the impact of this in relation to representation. The majority of the studies described the measurements used and these were assessed as being appropriate regarding both the outcome and the exposure. The reviewers were unable to determine whether complete outcome data were reported in nearly half (11/22) papers. This was related to a lack of detail provided for the reviewers to assess whether this criterion was met or not. The majority of studies identified confounders and reported on how they accounted for these in the design and the analysis of the data. All studies were assessed as meeting the requirement that exposure occurred as intended and any possible unintended exposure was adjusted for or the potential impact discussed.
4.1.1. Minimum nurse to patient ratios (staffing standard)
This section summarizes the fifteen studies that investigated the impact of the mandated minimum nurse‐to‐patient ratios on patient and nurse outcomes. These studies specified the required minimum number of nurses to patients at a ward or unit level. Studies that assessed the impact of the Nursing Home Reform act to have a registered nurse (RN) on duty at least 8 h a day, 7 days a week; and a licensed nurse (RN or LPN) on duty 24 h a day were also included under this heading.
Patient outcomes in hospitals
Ten studies explored the impact of the mandated minimum nurse to patient ratios on patient outcomes in a hospital setting. Chan et al., (2010) explored the effect of patient wait time in the emergency department post implementation of mandated ratios. The study reported that a shorter wait time to be seen was observed when the emergency department was within the mandated ratio compared to when the emergency department was outside the mandated ratio. In addition, they found care time (in minutes) for patients seen in an “out of ratio” environment was 37% longer than those patients seen in an environment “within ratio (Chan et al., 2010).
Weichenthal and Hendey (2011) also explored the effect of mandated minimum nurse‐to‐patient ratios in the emergency department. The study identified an overall decrease in patients that left without being seen from 11.9% to 11.2%, a decrease in the time to give antibiotics to patients with pneumonia (from 103 to 62 min) and found no significant difference in the number of reported medication errors or the rate of aspirin administration for acute coronary syndrome patients. However, it was identified that the implementation resulted in some unexpected negative consequences with all wait times increasing post implementation, including wait time (from 79 to 123 min), throughput time (from 365 to 397 min), and admission time (from 447 to 552 min) (Weichenthal & Hendey, 2011).
Burnes Bolton et al., (2007) and Donaldson et al., (2005) explored trends, over time, in patient outcomes as a result of the mandated minimum nurse to patient ratios. The initial analysis compared patient outcomes prior to the implementation of mandated minimum patient to nurse ratios in 2002 to a 6 month 2004 post ratio implementation period (Burnes Bolton et al., 2007). Donaldson et al., (2005) undertook a secondary analysis comparing post regulation ratios data from 2004 and 2006. The studies identified no statistically significant change in the rate of falls, pressure sores or the use of restraints post implementation of mandated ratios.
One study explored the implementation of Californian nurse staffing legislation, changes in acuity‐adjusted nurse staffing and the quality of care between hospitals with mandated minimum nurse‐to‐patient ratios and similar changes in hospitals in comparison states with no regulations (Mark et al., 2013). The study identified that infections, due to medical care, increased significantly in some Californian hospitals compared to hospitals in other states without such regulations. Postoperative sepsis was not significantly different in the Californian based hospitals when compared to hospitals in other states that had not implemented nurse‐to‐patient ratios. However, failure to rescue decreased significantly in some California hospitals in comparison to other states during 2000–2006 following the California minimum nurse staffing legislation (Mark et al., 2013).
The rate of complications post implementation of state‐wide intensive care unit staffing requirements was measured by Law et al., (2018). The study reported on patient mortality and patient complications. Complications was the overall measure of central line‐associated bloodstream infections, catheter‐associated urinary tract infections, hospital acquired pressure ulcers and patient falls with an injury. The study reported no changes in rate of mortality or complications post implementation of the staffing regulations (Law et al., 2018).
Cook et al., (2012) explored the effect of hospital nurse staffing on patient health outcomes. The study did not identify any significant change between the rates of pressure sores and failure to rescue post implementation of the mandated nurse to patient ratios.
One study investigated the detection of depression and anxiety, as a secondary condition, in patients hospitalized for pneumonia (Hodgson et al., 2016). This study found that hospitals in California post implementation of ratios reported improvement in the detection of secondary depression and anxiety in patients with pneumonia. The increase in the number of secondary diagnosis was related to the reduction in the number of patients per nurse.
The impact of mandated staffing ratios on the risk adjusted outcomes of paediatric cardiac surgery programs, were explored by Hickey et al., (2011). The outcomes variables of interest were mortality and patient complications. Complications were defined as untoward harm associated with therapeutic or diagnostic healthcare intervention. The study reported that the standardized complication ratio among children who underwent congenital heart surgery increased in Californian hospitals by 5% but decreased by 5% for hospitals in other states. The study also reported a 33% decrease in paediatric cardiac mortality in California after ratios were introduced compared to a 29% decrease in all other states in the USA (Hickey et al., 2011).
Spetz et al., (2013) explored the relationship between nursing and hospital quality using minimum nurse staffing requirements. The study identified that the implementation of the staffing mandate in California, resulted in, a significant increase in six NSOs in hospitals with the lowest pre‐regulation staffing as compared to hospitals with the highest pre‐regulation staffing.
Three studies assessed as being of lower methodological quality (Hickey et al., 2011; Mark et al., 2013; Spetz et al., 2013) contributed to this outcome.
Patient outcomes in nursing homes
Five studies explored the impact of nursing home reform on patients’ outcomes. Bowblis and Ghattas (2017) explored staffing and the percentage of residents that acquired a pressure ulcer, contracture or physical restraint, as a measure of quality. The study identified that higher staffing levels were associated with a statistically significant reduction in contractures and the use of physical restraint. All other quality measures showed no statistically significant impact post implementation of staffing regulations (Bowblis & Ghattas, 2017).
One study observed a significant decrease in the proportion of residents with pressure ulcers, the use of restraint and the proportion of urethral catherization, following the implementation of the Nursing Home Reform act (Zhang & Grabowski, 2004).
As a result of adoption of minimum hours per resident day regulations in nursing homes in California/Ohio, Chen (2015) identified a significant decline in the rate of contractures post implementation. The other quality measures used in the study namely, physical restraints, pressure ulcers, urethral catherization and psychoactive medication use were not found to be statistically significant post implementation of minimum staffing standards.
Matsurdaria (2014) identified no statistically significant change in the use of restraints, pressure sores or the use of urinary catherization post implementation of minimum staffing legislation for nursing homes.
The impact of state minimum staffing standards on the level of staffing and quality of nursing home care was measured in one study (Park & Stearns, 2009). Quality of care outcomes were measured by the rate of pressure sores, contractures and bladder incontinence. The use of restraint and urethral catheterization were considered to be a measure of the process of care. None of the quality of care outcomes were significantly associated with the increase in minimum standards of staffing. The use of urinary catheters as a process of care was also not significantly significant. Although the rates of restraint use declined significantly post increase of minimum standards (Park & Stearns, 2009).
Nurse outcomes
Six studies (Cox et al., 2005; Leigh et al., 2015; Spetz, 2008; Spetz & Herrera, 2010; Tellez, 2012; Tellez & Seago, 2013) assessed mandated nurse‐to‐patient ratios and nurse outcomes. Five studies (Cox et al., 2005; Spetz, 2008; Spetz & Herrera, 2010; Tellez, 2012; Tellez & Seago, 2013) were assessed as being of lower methodological quality.
The studies assessed nurse satisfaction, intent to stay, complaints and verbal abuse, burn out, staff illness and occupational injury. Four studies investigated the impact of nurse‐to‐patient ratios and job satisfaction. All four studies reported that nurse staffing ratios in the hospital setting was associated with a significant increase in nurses’ job satisfaction (Cox et al., 2005; Spetz, 2008; Spetz & Herrera, 2010; Tellez, 2012). Three studies used the same cross‐sectional survey data from the California board of registered nursing surveys (Spetz, 2008; Spetz & Herrera, 2010; Tellez & Seago, 2013), which assessed job satisfaction over time following the implementation of the staffing law. Despite an improvement in satisfaction, Cox et al., (2005) identified no difference in intention to stay post implementation of mandated nurse‐to‐patient ratios.
Leigh et al., (2015) investigated the impact of the Californian mandated minimum nurse to patient ratios on occupational injury and illness rates among nurses. The study reported that nurse to patient ratios were associated with 55.57 and 93.23 fewer occupational injuries and illnesses per 10,000 registered nurses and licensed practical nurses per year, respectively, as compared to 49 other states and the district of Columbia, without such ratios.
4.1.2. Nursing hours per patient day
One study assessed the impact of Nursing Hours Per Patient Day (NHPPD) on nurse sensitive outcomes within a public hospital in Western Australia (Twigg et al., 2011). The NHPPD staffing method, group's wards into seven categories based on a range of indicators such as patient turnover, emergency/elective patient mix and intervention levels, all of which influence nurse workloads. The study found a significant decrease in the rates of nine patient outcomes post implementation. These were mortality, central nervous system complications, pressure ulcers, deep vein thrombosis, sepsis, ulcer/gastritis/upper gastrointestinal bleed shock/cardiac arrest, pneumonia and average length of stay. No difference was reported for the following outcomes wound infections, pulmonary failure, physiologic/metabolic derangement and failure to rescue.
5. DISCUSSION
This review focused on studies that examined the impact of implementing a specific nurse staffing methodology, on patient and nurse outcomes. The findings from this present review highlighted the limited and inconsistent evidence regarding the impact that nurse staffing methodologies have on patient and nurse outcomes. The methodological quality of the papers highlighted the need for authors to provide adequate background information on the study sample to allow an assessment of whether the participants were representative of the target population and on whether complete outcome data were reported.
The majority of studies were conducted in California and investigated the impact of minimum nurse‐to‐patient ratios in hospital or aged care settings. Only one Australian study (Twigg et al., 2011) evaluated the Nurse Hours Per Patient Day staffing method and did find improvements in several patient outcomes including mortality, pressure injury and sepsis. None the less, the evidence on this topic remains limited.
The enactment of mandated minimum nurse‐to‐patient ratios in Californian hospitals has proven to be effective in improving nurse outcomes, such as intention to stay, job satisfaction (Tellez, 2012) and reducing illness and rates of occupational injury (Leigh et al., 2015). However, the question remains whether improvements are related to achieving an effective ratio as a result of mandated ratios or simply better staffing in itself. There is an extensive body of work that identifies an association between higher nurse staffing levels and improved nurse outcomes (Shin et al., 2018; Wynendaele et al., 2019) and these may explain the outcomes noted in this review.
The evidence regarding nurse‐to‐patient ratios and patient outcomes such as mortality and failure to rescue is ambivalent. Numerous studies were cross‐sectional in design making the assessment of causality challenging. Studies that included a longitudinal or cohort design reported inconclusive results. Furthermore, the majority of studies were conducted in California, and therefore, the results may not be directly applicable to other jurisdictions where legislation, nurse education, working conditions, and the healthcare system are likely to be different.
Given the limited evidence on staffing methodologies mandated nurse staffing ratios are not easily supported in hospital settings (Olley et al., 2019). None the less, California still employs the mandated nurse‐to‐patient ratio methodology and two states in Australia, Victoria and Queensland have introduced this legislation in 2001 and 2016 respectively (Olley et al., 2019). This may be because nurse‐to‐patient ratios are easy to regulate and monitor, however they are far less sensitive to the complexity of the patient mix, and tend to minimize professional judgement in day to day staffing decisions (Griffiths et al., 2020). The Australian study on Nurse Hours Per Patient Day did find improvements in some patient outcomes and has attempted to assess complexity of the patient mix in its design, allowing for professional judgement in daily staffing decisions (Twigg & Duffield, 2009; Twigg et al., 2011). However, further research on this staffing method is needed before generalizing the results to other jurisdictions.
In addition, one study identified improvements in patient outcomes following the implementation of the Nursing Home Reform act in aged care (Zhang & Grabowski, 2004). Finally, there are other staffing tools and patient classification systems in existence and in use across healthcare services in developed countries. This includes, for example, the Safer Nursing Care tool, used in the England (Department of Health, 2018; National Quality Board, 2016) and RAFELA (Fagerström & Rauhala, 2007) used in Finland, to name a few. These tools and systems have shown to assist with staffing decisions and have been shown to improve patient outcomes (Fagerström et al., 2018; Griffiths et al., 2018b, 2019; Junttila et al., 2016). However, were not the focus of this present study. Future research is needed to improve knowledge on nurse staffing methodologies, with an emphasis on the refinement of research design and measures of patient and nurse outcomes.
6. LIMITATIONS
This is the first systematic review to explore the impact of nurse staffing methodologies on patient and nurse outcomes. However, as in any systematic review, there is always a potential for selection bias. We did not include grey literature or studies conducted in nondeveloped countries or studies not published in English. However, we believe that the studies included in our analysis are representative of the available literature.
7. CONCLUSION
Despite the importance of the question and the large volume of publications on nurse staffing, evidence on the impact of adopting a specific nurse staffing methodology and the subsequent impact on patient and nurse outcomes remains limited. The current evidence regarding staffing methodologies cannot point to any methodology as being superior in improving patient and nurse outcomes. Rather, the review supports improvements in nurse staffing levels, which has the associated benefit of improving nurse and patient outcomes. However, the ability to determine the number of nurses required over time remains problematic. The available evidence suggests that more registered nurses (RN) hour results in better patient outcomes, but existing staffing methodologies are yet to determine how many hours provided by an RN is needed in order to provide safe, quality and affordable care. Comparative studies with robust research methodology and clearly defined staffing parameters are needed to better understand how nurse staffing methodologies impact on patient and nurse outcomes.
CONFLICTS OF INTEREST
No conflict of interest has been declared by the author(s).
DATA AVAILABILITY STATEMENT
Author elects to not share data.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/jan.14909.
Supporting information
Table S1
Table S2
ACKNOWLEDGEMENT
We would like to acknowledge Laura Emery as a contributing author. Laura undertook secondary title screening (N = 6837).
Twigg DE, Whitehead L, Doleman G, et al. The impact of nurse staffing methodologies on nurse and patient outcomes: A systematic review. J Adv Nurs. 2021;77:4599–4611. 10.1111/jan.14909
Funding information
This work was supported by the Department of Health Western Australia. The funder was not involved in the development of the review methodology or the conduct and write‐up of the review findings.
Contributor Information
Diane E. Twigg, Email: d.twigg@ecu.edu.au.
Gemma Doleman, Email: g.doleman@ecu.edu.au.
References
- Aiken, L. H. , Clarke, S. P. , & Sloane, D. M. (2002). Hospital staffing, organization, and quality of care: Cross‐national findings. International Journal for Quality in Health Care, 14(1), 5–14. 10.1093/intqhc/14.1.5 [DOI] [PubMed] [Google Scholar]
- Aiken, L. H. , Sloane, D. M. , Bruyneel, L. , Van den Heede, K. , Griffiths, P. , Busse, R. , Lesaffre, E. (2014). Nurse staffing and education and hospital mortality in nine European countries: a retrospective observational study. The Lancet, 383(9931), 1824–1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Australian Industrial Relations Commission (2002).
- Ball, J. E. , Bruyneel, L. , Aiken, L. H. , Sermeus, W. , Sloane, D. M. , Rafferty, A. M. , … Consortium, R. C. (2018). Post‐operative mortality, missed care and nurse staffing in nine countries: A cross‐sectional study. International Journal of Nursing Studies, 78, 10–15. 10.1016/j.ijnurstu.2017.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowblis, J. R. , & Ghattas, A. (2017). The impact of minimum quality standard regulations on nursing home staffing, quality, and exit decisions. Review of Industrial Organization, 50(1), 43–68. 10.1007/s11151-016-9528-x [DOI] [Google Scholar]
- Burnes Bolton, L. , Aydin, C. E. , Donaldson, N. , Storer Brown, D. , Sandhu, M. , Fridman, M. , & Udin Aronow, H. (2007). Mandated nurse staffing ratios in California: A comparison of staffing and nursing‐sensitive outcomes pre‐and postregulation. Policy, Politics, & Nursing Practice, 8(4), 238–250. 10.1177/1527154407312737 [DOI] [PubMed] [Google Scholar]
- Campbell, M. , McKenzie, J. E. , Sowden, A. , Katikireddi, S. V. , Brennan, S. E. , Ellis, S. , Hartmann‐Boyce, J. , Ryan, R. , Shepperd, S. , Thomas, J. , Welch, V. , & Thomas, J. (2020). Synthesis without meta‐analysis (SWiM) in systematic reviews: Reporting guideline. BMJ, 368, 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan, T. C. , Killeen, J. P. , Vilke, G. M. , Marshall, J. B. , & Castillo, E. M. (2010). Effect of mandated nurse–patient ratios on patient wait time and care time in the emergency department. Academic Emergency Medicine, 17(5), 545–552. 10.1111/j.1553-2712.2010.00727.x [DOI] [PubMed] [Google Scholar]
- Chen, M. M. , & Grabowski, D. C. (2015). Intended and unintended consequences of minimum staffing standards for nursing homes. Health Economics, 24(7), 822–839. 10.1002/hec.3063 [DOI] [PubMed] [Google Scholar]
- Coffman, J. M. , Seago, J. A. , & Spetz, J. (2002). Minimum nurse‐to‐patient ratios in acute care hospitals in California. Health Affairs, 21(5), 53–64. 10.1377/hlthaff.21.5.53 [DOI] [PubMed] [Google Scholar]
- Cook, A. , Gaynor, M. , Stephens, M. Jr , & Taylor, L. (2012). The effect of a hospital nurse staffing mandate on patient health outcomes: Evidence from California's minimum staffing regulation. Journal of Health Economics, 31(2), 340–348. 10.1016/j.jhealeco.2012.01.005 [DOI] [PubMed] [Google Scholar]
- Cox, K. S. , Anderson, S. C. , Teasley, S. L. , Sexton, K. A. , & Carroll, C. A. (2005). Nurses’ work environment perceptions when employed in states with and without mandatory staffing ratios and/or mandatory staffing plans. Policy, Politics, & Nursing Practice, 6(3), 191–197. 10.1177/1527154405279091 [DOI] [PubMed] [Google Scholar]
- Dalton, M. , Harrison, J. , Malin, A. , & Leavey, C. (2018). Factors that influence nurses’ assessment of patient acuity and response to acute deterioration. British Journal of Nursing, 27(4), 212–218. 10.12968/bjon.2018.27.4.212 [DOI] [PubMed] [Google Scholar]
- Department of Health . (2018). Framework for safe nurse staffing and skill mix in general and specialist medical and surgical care settings in Ireland 2018. London Department of Health.
- Department of Health . (2019). NHpPD application manual: guiding principles. Department of Health. [Google Scholar]
- Donaldson, N. , Bolton, L. B. , Aydin, C. , Brown, D. , Elashoff, J. D. , & Sandhu, M. (2005). Impact of California’s licensed nurse‐patient ratios on unit‐level nurse staffing and patient outcomes. Policy, Politics, & Nursing Practice, 6(3), 198–210. 10.1177/1527154405280107 [DOI] [PubMed] [Google Scholar]
- Donaldson, N. , & Shapiro, S. (2010). Impact of California mandated acute care hospital nurse staffing ratios: A literature synthesis. Policy, Politics, & Nursing Practice, 11(3), 184–201. 10.1177/1527154410392240 [DOI] [PubMed] [Google Scholar]
- Drennan, J. , Duffield, C. , Scott, A. P. , Ball, J. , Brady, N. M. , Murphy, A. , Dahly, D. , Savage, E. , Corcoran, P. , Hegarty, J. , Griffiths, P. (2018). A protocol to measure the impact of intentional changes to nurse staffing and skill‐mix in medical and surgical wards. Journal of Advanced Nursing, 74(12), 2912–2921. 10.1111/jan.13796 [DOI] [PubMed] [Google Scholar]
- Duffield, C. , Gardner, G. , Doubrovsky, A. , & Wise, S. (2019). Manager, clinician or both? Nurse managers’ engagement in clinical care activities. Journal of Nursing Management, 27(7), 1538–1545. 10.1111/jonm.12841 [DOI] [PubMed] [Google Scholar]
- Duffield, C. , Roche, M. A. , Blay, N. , Thoms, D. , & Stasa, H. (2011). The consequences of executive turnover in Australian hospitals. Journal of Reserach in Nursing, 16(6), 503–514. 10.1177/1744987111422419 [DOI] [Google Scholar]
- Duffield, C. , Roche, M. , & Merrick, E. T. (2006). Methods of measuring nursing workload in Australia. Collegian, 13(1), 16–22. 10.1016/S1322-7696(08)60512-0 [DOI] [PubMed] [Google Scholar]
- Fagerström, L. , Kinnunen, M. , & Saarela, J. (2018). Nursing workload, patient safety incidents and mortality: An observational study from Finland. British Medical Journal Open, 8(4), e016367. 10.1136/bmjopen-2017-016367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagerström, L. , & Rauhala, A. (2007). Benchmarking in nursing care by the RAFAELA patient classification system–a possibility for nurse managers. Journal of Nursing Management, 15(7), 683–692. 10.1111/j.1365-2934.2006.00728.x [DOI] [PubMed] [Google Scholar]
- Fasoli, D. R. , & Haddock, K. S. (2010). Results of an integrative review of patient classi cation systems. Annual Review of Nursing Research, 28(1), 295–316. 10.1891/0739-6686.28.295 [DOI] [PubMed] [Google Scholar]
- Gerdtz, M. F. , & Nelson, S. (2007). 5–20: A model of minimum nurse‐to‐patient ratios in Victoria. Australia. Journal of Nursing Management, 15(1), 64–71. 10.1111/j.1365-2934.2006.00657.x [DOI] [PubMed] [Google Scholar]
- Griffiths, P. , Ball, J. , Bloor, K. , Böhning, D. , Briggs, J. , Dall’Ora, C. , Iongh, A. D. , Jones, J. , Kovacs, C. , Maruotti, A. , Meredith, P. , Prytherch, D. , Saucedo, A. R. , Redfern, O. , Schmidt, P. , Sinden, N. , & Smith, G. (2018). Nurse staffing levels, missed vital signs and mortality in hospitals: retrospective longitudinal observational study. Health Services and Delivery Research, 6(38), 1–120. [PubMed] [Google Scholar]
- Griffiths, P. , Ball, J. , Bloor, K. , Böhning, D. , Briggs, J. , Dall'Ora, C. , Maruotti, A. (2018a). Nurse staffing levels, missed vital signs observations and mortality in hospital wards: Retrospective longitudinal observational study. Health Services and Delivery Research, 6(38). [PubMed] [Google Scholar]
- Griffiths, P. , Maruotti, A. , Recio Saucedo, A. , Redfern, O. C. , Ball, J. E. , Briggs, J. , Dall'Ora, C. , Schmidt, P. E. , & Smith, G. B. (2019). Nurse staffing, nursing assistants and hospital mortality: Retrospective longitudinal cohort study. BMJ Quality & Safety, 28(8), 609–617. 10.1136/bmjqs-2018-008043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths, P. , Saville, C. , Ball, J. , Jones, J. , Pattison, N. , Monks, T. , & Group, S. N. C. S. (2020). Nursing workload, nurse staffing methodologies and tools: A systematic scoping review and discussion. International Journal of Nursing Studies, 103, 103487. 10.1016/j.ijnurstu.2019.103487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hickey, P. A. , Gauvreau, K. , Jenkins, K. , Fawcett, J. , & Hayman, L. (2011). Statewide and national impact of California's staffing law on pediatric cardiac surgery outcomes. JONA: the Journal of Nursing Administration, 41(5), 218–225. 10.1097/NNA.0b013e3182171b2e [DOI] [PubMed] [Google Scholar]
- Hodgson, A. , Morgan, D. , & Peterson, R. (2016). Does better nurse staffing improve detection of depression and anxiety as secondary conditions in hospitalized patients with pneumonia? Nursing Economics, 34(3), 134. [PubMed] [Google Scholar]
- Hong, Q. N. , Pluye, P. , Fàbregues, S. , Bartlett, G. , Boardman, F. , Cargo, M. , Nicolau, B. (2018). Mixed methods appraisal tool (MMAT), version 2018. Registration of copyright, 1148552.
- Junttila, J. K. , Koivu, A. , Fagerström, L. , Haatainen, K. , & Nykänen, P. (2016). Hospital mortality and optimality of nursing workload: A study on the predictive validity of the RAFAELA Nursing Intensity and Staffing system. International Journal of Nursing Studies, 60, 46–53. 10.1016/j.ijnurstu.2016.03.008 [DOI] [PubMed] [Google Scholar]
- Kane, R. L. , Shamliyan, T. , Mueller, C. , Duval, S. , & Wilt, T. J. (2007). Nurse staffing and quality of patient care. Evidence Report Technology Assessment (Full Report), 151(1), 115. [PMC free article] [PubMed] [Google Scholar]
- Lasman, B. , Aroozoo, M. , & Petrie, A. (2019). Safe patient care (nurse to patient and midwife to patient ratios) ammendment bill 2018: Parliment of Victoria.
- Law, A. C. , Stevens, J. P. , Hohmann, S. , & Walkey, A. J. (2018). Patient outcomes after the introduction of statewide intensive care unit nurse staffing regulations. Critical Care Medicine, 46(10), 1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh, J. P. , Markis, C. A. , Iosif, A.‐M. , & Romano, P. S. (2015). California’s nurse‐to‐patient ratio law and occupational injury. International Archives of Occupational and Environmental Health, 88(4), 477–484. 10.1007/s00420-014-0977-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mark, B. A. , Harless, D. W. , Spetz, J. , Reiter, K. L. , & Pink, G. H. (2013). California's minimum nurse staffing legislation: Results from a natural experiment. Health Services Research, 48(2pt1), 435–454. 10.1111/j.1475-6773.2012.01465.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsudaira, J. D. (2014). Government regulation and the quality of healthcare evidence from minimum staffing legislation for nursing homes. Journal of Human Resources, 49(1), 32–72. 10.1353/jhr.2014.0003 [DOI] [Google Scholar]
- Moher, D. , Shamseer, L. , Clarke, M. , Ghersi, D. , Liberati, A. , Petticrew, M. , Shekelle, P. , Stewart, L. A. (2015). Preferred reporting items for systematic review and meta‐analysis protocols (PRISMA‐P) 2015 statement. Systematic Reviews, 4(1), 1. 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Quality Board . (2016). Supporting NHS providers to deliver the right staff, with the right skills, in the right place at the right time: safe, sustainable and productive staffing: National Quality Board (NQB).
- Needleman, J. , Buerhaus, P. , Mattke, S. , Stewart, M. , & Zelevinsky, K. (2001). Nurse staffing and patient outcomes in hospitals: Harvard School of Public Health Boston.
- Needleman, J. , Buerhaus, P. , Mattke, S. , Stewart, M. , & Zelevinsky, K. (2002). Nurse‐staffing levels and the quality of care in hospitals. The New England Journal of Medicine, 346(22), 1715–1722. 10.1056/NEJMsa012247 [DOI] [PubMed] [Google Scholar]
- Needleman, J. , Buerhaus, P. , Pankratz, V. S. , Leibson, C. L. , Stevens, S. R. , & Harris, M. (2011). Nurse staffing and inpatient hospital mortality. New England Journal of Medicine, 364(11), 1037–1045. 10.1056/NEJMsa1001025 [DOI] [PubMed] [Google Scholar]
- Olley, R. , Edwards, I. , Avery, M. , & Cooper, H. (2019). Systematic review of the evidence related to mandated nurse staffing ratios in acute hospitals. Australian Health Review, 43(3), 288–293. 10.1071/AH16252 [DOI] [PubMed] [Google Scholar]
- Ouzzani, M. , Hammady, H. , Fedorowicz, Z. , & Elmagarmid, A. (2016). Rayyan—a web and mobile app for systematic reviews. Systematic Reviews, 5(1), 210. 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park, J. , & Stearns, S. C. (2009). Effects of state minimum staffing standards on nursing home staffing and quality of care. Health Services Research, 44(1), 56–78. 10.1111/j.1475-6773.2008.00906.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roche, M. , Duffield, C. , Aisbett, C. , Diers, D. , & Stasa, H. (2012). Nursing work directions in Australia: Does evidence drive the policy? Collegian, 19(4), 231–238. 10.1016/j.colegn.2012.03.006 [DOI] [PubMed] [Google Scholar]
- Saville, C. E. , Griffiths, P. , Ball, J. E. , & Monks, T. (2019). How many nurses do we need? A review and discussion of operational research techniques applied to nurse staffing. International Journal of Nursing Studies, 97, 7–13. 10.1016/j.ijnurstu.2019.04.015 [DOI] [PubMed] [Google Scholar]
- Serratt, T. (2013a). California’s nurse‐to‐patient ratios, Part 1: 8 years later, what do we know about nurse‐level outcome? JONA: the Journal of Nursing Administration, 43(9), 475–480. 10.1097/NNA.0b013e3182a23d6f [DOI] [PubMed] [Google Scholar]
- Serratt, T. (2013b). California’s nurse‐to‐patient ratios, part 3: Eight years later, what do we know about patient level outcomes? JONA: The Journal of Nursing Administration, 43(11), 581–585. 10.1097/01.NNA.0000434505.69428.eb [DOI] [PubMed] [Google Scholar]
- Shin, S. , Park, J.‐H. , & Bae, S.‐H. (2018). Nurse staffing and nurse outcomes: A systematic review and meta‐analysis. Nursing Outlook, 66(3), 273–282. 10.1016/j.outlook.2017.12.002 [DOI] [PubMed] [Google Scholar]
- Spetz, J. (2008). Nurse satisfaction and the implementation of minimum nurse staffing regulations. Policy, Politics, & Nursing Practice, 9(1), 15–21. 10.1177/1527154408316950 [DOI] [PubMed] [Google Scholar]
- Spetz, J. , Harless, D. W. , Herrera, C.‐N. , & Mark, B. A. (2013). Using minimum nurse staffing regulations to measure the relationship between nursing and hospital quality of care. Medical Care Research and Review, 70(4), 380–399. 10.1177/1077558713475715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spetz, J. , & Herrera, C. (2010). Changes in nurse satisfaction in California, 2004 to 2008. Journal of Nursing Management, 18(5), 564–572. 10.1111/j.1365-2834.2010.01117.x [DOI] [PubMed] [Google Scholar]
- Tellez, M. (2012). Work satisfaction among California registered nurses: A longitudinal comparative analysis. Nursing economic$, 30(2), 73–81. [PubMed] [Google Scholar]
- Tellez, M. , & Seago, J. A. (2013). California nurse staffing law and RN workforce changes. Nursing Economics, 31(1), 18. [PubMed] [Google Scholar]
- Twigg, D. , & Duffield, C. (2009). A review of workload measures: A context for a new staffing methodology in Western Australia. International Journal of Nursing Studies, 46(1), 132–140. 10.1016/j.ijnurstu.2008.08.005 [DOI] [PubMed] [Google Scholar]
- Twigg, D. , Duffield, C. , Bremner, A. , Rapley, P. , & Finn, J. (2011). The impact of the nursing hours per patient day (NHPPD) staffing method on patient outcomes: A retrospective analysis of patient and staffing data. International Journal of Nursing Studies, 48(5), 540–548. 10.1016/j.ijnurstu.2010.07.013 [DOI] [PubMed] [Google Scholar]
- Weichenthal, L. , & Hendey, G. W. (2011). The effect of mandatory nurse ratios on patient care in an emergency department. The Journal of Emergency Medicine, 40(1), 76–81. 10.1016/j.jemermed.2009.02.037 [DOI] [PubMed] [Google Scholar]
- Welsh Government . (2016). Nurse staffing levels act 2016. Welsh Government. [Google Scholar]
- Whitehead, L. C. , & Myers, H. (2016). The effect of hospital nurse staffing models on patient and staff‐related outcomes. International Journal of Nursing Practice, 22(4), 330–332. 10.1111/ijn.12463. [DOI] [PubMed] [Google Scholar]
- Wynendaele, H. , Willems, R. , & Trybou, J. (2019). Systematic review: Association between the patient–nurse ratio and nurse outcomes in acute care hospitals. Journal of Nursing Management, 27(5), 896–917. 10.1111/jonm.12764 [DOI] [PubMed] [Google Scholar]
- Zhang, X. , & Grabowski, D. C. (2004). Nursing home staffing and quality under the nursing home reform act. The Gerontologist, 44(1), 13–23. 10.1093/geront/44.1.13 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1
Table S2
Data Availability Statement
Author elects to not share data.


