Abstract
Objective
We aimed to identify the main barriers to integrated care (IC) as reported by healthcare stakeholders from various linguistic regions and health system specificities, according to their reality of practice.
Methods
Information was gathered through an open‐ended question from a national survey conducted in Switzerland in 2019. Responses were analysed qualitatively with the IRaMuTeQ software.
Results
Answers from 410 respondents were obtained. Respondents reported barriers at two levels: the system and professional level. Threat to financial benefits, concerns for patient data sharing and tensions between quality of care and benefits for patients versus costs were mentioned at the professional level, in their activity and in patient care. At the system level, limitations at the political level due to federalism and the lack of support and training for professionals were important barriers, in addition to the lack of recognition and compensation for professionals and the fragmented functioning of the health care system.
Conclusion
Our study underlines the importance of implementing innovative funding strategies and reimbursement schemes, as well as political willingness to move towards IC. The alignment between federal policies and cantonal specificities also appears as necessary to achieve involvement of professionals, promote integration of services and coordination of professionals for continuous and efficient care.
Keywords: barriers, healthcare stakeholders, integrated care, Switzerland
1. INTRODUCTION
From the increased specialization and compartmentalization of health services, shortages in financial resources and personnel, to the increasing life expectancy and growing prevalence of non‐communicable diseases in the population requiring multidisciplinary chronic management, health systems are facing a number of challenges. 1 Approaches promoting the integration and coordination of care to counter the latter have been implemented to improve population health, patient outcomes, and greater efficiency. 1 , 2 , 3 Integrated care (IC) aims to respond to these goals. Even though the definition of IC tends to vary between stakeholders and health care systems, it brings together key elements of fragmented health care systems, in terms of design and delivery to provide care, in the sense of delivering assistance or treatment to patients in need. 4 Despite the growing number of IC initiatives being implemented in Europe, they remain context‐dependent according to the specificities of each health system, and their scaling up challenging. 1 , 5
In Switzerland, the development and implementation of IC has been growing in the past years. 1 Concomitantly, national initiatives such as the Federal Council's 2020–2030 health strategy that specifically targets care quality and coordination, and the 2017‐2024 National strategy to tackle non‐communicable diseases to develop common frameworks to managing these conditions, as well as national programs such as the 2015 National project on the coordination of care, have been developed. Despite these, Switzerland remains behind in the development and implementation of IC initiatives in comparison to other European countries. In Switzerland, the particular configuration of health management through centralized and decentralized logics, with responsibilities divided between the federal, cantonal and municipal levels, leads to considerable disparities and specificities of health systems between cantons. 1 In this context, IC initiatives continue to be diverse and heterogeneous in Switzerland, and mostly implemented as individual initiatives at cantonal or communal levels according to local specificities.
Barriers and facilitators to IC have been explored in different contexts and healthcare systems, through interviews and focus groups, as well as with literature reviews and case studies. 6 , 7 , 8 Funding and policy, delivery structures, information technology, relationships between services and professionals, and skills and attitudes towards change and innovation have been mostly reported, among others. 6 , 7 , 8 , 9 Considering that barriers to IC are context‐specific and that the healthcare context has evolved a lot during the past decade, in terms of the burden of chronic diseases and the required shift in the chronic care paradigm, health policy targets and initiatives, an updated exploration of barriers to IC is appropriate to explore specificities in the swiss healthcare context. 10
The SCIROCCO tool, based on the B3‐Maturity Model, 11 has been used to evaluate the maturity of health systems to deliver IC, by revealing their strengths, weaknesses and areas for improvement, through stakeholders' perspectives. 10 , 12 , 13 Recently, the SCIROCCO tool was included in a national survey to assess the “maturity” of the Swiss health system for IC. 10 Results from this survey confirmed, at the national level, a rather low maturity of the Swiss health system to implement IC on each of the 12 dimensions. The objective of the current study is to understand these quantitative results. More specifically, by using an open‐ended question included in this national survey, we aimed to identify the current main barriers to IC in Switzerland as reported by stakeholders from various linguistic regions and health system specificities, according to their current everyday work and practice. Obtaining current healthcare stakeholders' perspectives on IC, would allow to better grasp challenges and difficulties from those involved in the reality of practice.
2. METHOD
2.1. Study design and measures
The open‐ended question was included in a cross‐sectional national survey conducted in Switzerland in the fall of 2019, with local healthcare stakeholders selected for their potential knowledge and experience of integrated care. 10 The survey was composed of three sections. A first section included the French, German and Italian versions of the SCIROCCO tool, to evaluate the maturity of healthcare systems for integrated care according to 12 dimensions. 11 , 12 The following sections included questions to evaluate healthcare stakeholders' opinions towards IC (nine items) and the Swiss healthcare system (single item). 14 Barriers to IC were evaluated in the third section, comprised of an open‐ended question: “In your opinion, what are the main barriers to the implementation of integrated care in Switzerland?”. Finally, sociodemographic and professional information were collected.
2.2. Population and setting
A list of stakeholders was established by the integrated care unit of the Swiss Federal Office of Public Health, the Swiss Forum for Integrated Care, and included representatives of cantonal public health departments. Invitations to take part in the survey were sent by email to approximately 5500 healthcare stakeholders in Switzerland. Information about the study aim (to assess the maturity of the Swiss Health system to implement IC) and a link to the survey, were provided in the email.
2.3. Data analysis
Textual data from the open‐ended question were analysed using the IRaMuTeQ software (version 0.7 alpha 2, 2008–2014 Pierre Ratinaud), a Computer Assisted Qualitative Data Analysis Software. 15 This type of software, specifically dedicated to conduct lexicographic content analysis on large amounts of text 16 such as open‐ended survey questions, allows to identify recurring themes using word or expression co‐occurrences. It thus seeks underlying common narrative structures in a body of textual data. 16 Following the Reinert method, 17 the software first creates a dictionary of words in the texts. Words are then reduced to their shortest form (lemmatization) to create families of words. The texts are then partitioned into elementary contextual units (i.e., sentences) which serve as units for the analysis. Finally, two Hierarchical descending classification of words by ECU are carried out to generate a classification of words in thematic classes and a tree graph showing associations between these classes in the texts. Each extracted thematic class is associated with a typical vocabulary, and typical extracts to ease the identification and labelling of themes. Once the classification is done, it is up to the researchers to identify and label the classes according to the typical words and extracts. They can also analyse connections between classes thanks to the tree graph and a Factor analysis of correspondence. In our case two researchers (IG, SL) specialized in qualitative methods and in the use of this software took part to the IRaMuTeQ analyses (identification and labelling of thematic classes; analyses of connections between classes). Both researchers first conducted their analysis separately and then confronted the latter to reach a consensus, both on the identification/labelling of themes and on connections between classes. No discrepancy between researchers' analyses had to be resolved. The following variables of interest were considered in the analyses: type of healthcare professional, main setting for professional activity, linguistic region in which respondents worked, involvement in IC programs and attitude towards IC and the Swiss healthcare system.
3. RESULTS
3.1. Respondents' characteristics.
Of the 642 survey respondents, 410 answered the open‐ended question about IC barriers. Characteristics of the 410 respondents as well as these of the whole survey respondents are reported in Table 1. Both samples showed close characteristics. Among respondents of the open‐ended question, the mean age was 55.9 years old, 44.6% were women and 42.5% were not involved in integrated care activities. Nearly 30% of the respondents were directors of institutions, approximately a third were healthcare providers and just over four out of 10 worked in healthcare institutions.
Table 1.
Characteristics of the respondents to the survey (n = 642) and to the open‐ended question on IC barriers (n = 410)
| Respondents to the survey (n = 642) | Respondents to the open‐ended question (n = 410) | |||
|---|---|---|---|---|
| Variables | (n) | Mean (SD) or % | (n) | Mean (SD) or % |
| Age | (610) | 53.7 (10.5) | (393) | 55.9 (10.7) |
| Women | (617) | 42.5% | (176) | 44.6% |
| Profession | (625) | (402) | ||
| Practicing physicians | 19.8% | 18.2 | ||
| Non‐physician practicing healthcare professionals | 16.0% | 16.2 | ||
| Directors | 27.7% | 29.9 | ||
| Administration | 9.6% | 10.0 | ||
| Project management | 15.4% | 15.7 | ||
| Other | 11.5% | 10.2 | ||
| Professional activity | (597) | (389) | ||
| Independent | 19.4% | 15.7 | ||
| Public administration | 11.6% | 11.9 | ||
| Foundation/association | 12.2% | 11.8 | ||
| Insurance | 5.7% | 5.1 | ||
| Private clinic | 3.2% | 2.1 | ||
| University hospital | 22.1% | 20.6 | ||
| Cantonal hospital | 11.2% | 10.0 | ||
| Medical home | 9.2% | 12.1 | ||
| Other | 5.4% | 10.7 | ||
| Region of professional activity | (627) | (407) | ||
| German‐speaking Switzerland | 60.0% | 59.8% | ||
| French‐speaking Switzerland | 20.7% | 19.6% | ||
| Italian‐speaking Switzerland | 3.2% | 3.4% | ||
| Nation‐wide | 16.1% | 17.2% | ||
| Involvement in integrated care | (628) | (407) | ||
| No, never | 46.5% | 42.5% | ||
| Yes, once | 18.8% | 17.7% | ||
| Yes, several times | 34.7% | 39.8% | ||
| Attitude towards the Swiss healthcare system | (610) | (405) | ||
| Complete change needed | 8.2% | 9.9% | ||
| Major changes | 76.9% | 76.3% | ||
| Minor changes | 14.9% | 13.1% | ||
3.2. Lexicographic content analysis
The textual analysis showed that stakeholders identified seven themes. These main barriers to IC intervened at two levels: 1) at the professional level, on their activity and on patient care, and 2) at the system level, due to political constraints at national or cantonal level. Analyses showed that themes were evoked irrespectively of stakeholders' profession, setting of activity, region, or their involvement in or attitude towards IC. The classification and corresponding typical words and extracts are presented in Figure 1.
Figure 1.
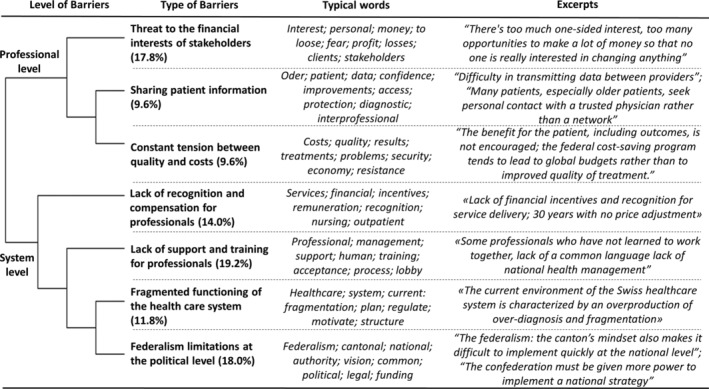
Main barriers to IC as reported by healthcare stakeholders, with corresponding typical words and excerpts. Note: Percentages in brackets represent the proportion of analysed texts in relation to each barrier
Barriers at the professional level. Three main barriers were cited at this level. The first concerned financial apprehensions. Respondents reported that IC represented a threat to the financial benefits of some stakeholders in the current system, particularly for physicians, which led to resistance to change and hampered support for an alternative model. The second concerned sharing patient information. This included the lack of upstream thinking regarding an IT system for patient data sharing, considered key for IC implementation, as well as the difficulty of transmitting data between providers, and the lack of clear protocols for data sharing. Some respondents reported that an interprofessional platform would be useful for discussing opinions and needs for data sharing. However, a concern was the integration of all patients with the use of IT solutions, as providers considered that some patients would be reluctant to rely on networks and prefer direct contact with their already known and trusted physicians. Providers mentioned that this would be especially problematic for elderly patients, which tended to be more unfamiliar with these tools. Respondents raised this concern as a potential limitation that could affect patient participation and self‐determination in care, considered a central aim in IC. The third barrier, often evoked with the previous one, corresponded to the constant tension felt between quality of care and costs (mostly mentioned by clinicians), where cost savings are put forward instead of the improvement of quality and benefits for the patient.
Barriers at the system level. Four main barriers were mentioned. The first concerned the lack of recognition and compensation for professionals. IC requires additional administrative tasks and time for interprofessional coordination, which remain unrecognized and under‐funded. The second barrier concerned the lack of support and training for professionals, which created difficulties in the practice of collaboration. It was also mentioned that IC trainings should be more often proposed to professionals and newly graduated students. The fragmented functioning of the health care system and federalism limitations at the political level were mentioned as closely related barriers. The lack of political will to change the entire system, and more particularly to support the launch of IC pilot projects was underlined. According to respondents, IC requires uniform funding and a unified political vision. However, inter‐cantonal differences result in a lack of a clear national vision of the health care system, unfavourable to the implementation of a more global system.
4. DISCUSSION
The main reported barriers provide a perspective on IC at the national level, according to perceived difficulties and opinions from a variety of healthcare stakeholders working in different linguistic regions with contextual specificities. System level barriers remained the most mentioned by respondents as affecting IC. The federalist political organization, already mentioned in other studies, 1 , 18 is an important factor limiting the development and implementation of a global and national IC strategy in Switzerland. National political initiatives, including funding, supportive regulation, flexible administrative reorganization, as well as financial benefits and reimbursement schemes 19 are essential conditions for IC and are still lacking in Switzerland. Our results also highlight that professionals need to feel supported and be provided with training, which was also mentioned in other contexts. 7 , 8 Another important aspect was for professionals to perceive political willingness for change, as already reported by Lauvergeon et al. a few years ago. 18 This appears as particularly important to favour professionals' involvement. 18 Finally, patient data sharing, a key enabler to the implementation of IC 7 , 19 also remained an issue of concern for professionals in the Swiss context.
Even though identified barriers remained similar to those reported in other contexts, it is possible that national initiatives promoting integrated care in a broader sense, and new models of care for NCDs, among others, 1 may be too recent to have yet deployed their effects. Nevertheless, our study underlines that, between federal decisions and regional necessities, the implementation of innovative funding strategies 1 and reimbursement schemes (such as incentives) would encourage professional involvement and address feelings of threat and fears of losing actual benefits. Commitment to IC at the macro and meso levels (system, organizations and institutions) is required to achieve alignment with the micro level (professionals' activity and practice) and promote institutional and clinical cultures towards IC. 19 These conditions appear as essential to overcome identified barriers in the Swiss context and provide continuous, efficient and cost controlled care through well‐implemented IC initiatives. 19
CONFLICT OF INTEREST
The authors declare having no conflict of interest.
AUTHORS CONTRIBUTION
I.P.B. conceptualized the study, I.P.B. and I.G. designed the study and collected the data, I.G. and S.L. performed the qualitative analysis and C.R., I.G. and S.L. wrote the paper. All authors reviewed and edited the draft manuscript.
ACKNOWLEDGEMENTS
We thank Séverine Schusselé Filliettaz, Peter Berchtold and Andrea Pavlickova for their contributions to the National survey from which the data presented here was extracted. We also thank Michelle Grossglauser, Chantal Arditi, Federico Cathieni, Anita Savidan, Lea von Wartburg, Adriana de Giorgi, Tania Weng Bornholt and Urs Zanoni for their participation in the SCIROCCO adaptation–translation process, and all respondents who took part in the survey. This research received no specific grant from any funding agency in the public, commercial or not‐for‐profit sectors. Open access funding provided by Universite de Lausanne.
Rawlinson C, Lesage S, Gilles I, Peytremann‐Bridevaux I. Healthcare stakeholders' perspective on barriers to integrated care in Switzerland: Results from the open‐ended question of a nationwide survey. J Eval Clin Pract. 2022;28:129-134. 10.1111/jep.13605
Cloé Rawlinson and Saphir Lesage are co‐first authors.
DATA AVAILABILITY STATEMENT
Data are available upon reasonable request. The datasets used during the study are available from the corresponding author on reasonable request.
REFERENCES
- 1. Filliettaz SS, Berchtold P, Kohler D, Peytremann‐Bridevaux I. Integrated care in Switzerland: results from the first nationwide survey. Health Policy. 2018;122(6):568‐576. [DOI] [PubMed] [Google Scholar]
- 2. Shaw S, Rosen R, Rumbold B. What is integrated care. London: Nuffield Trust. 2011;7:1‐23. [Google Scholar]
- 3. Valentijn PP, Schepman SM, Opheij W, Bruijnzeels MA. Understanding integrated care: a comprehensive conceptual framework based on the integrative functions of primary care. Int J Integr Care. 2013;13:1‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Goodwin N. Understanding integrated care. Int J Integr Care. 2016;16(4):1‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Amelung V, Stein V, Goodwin N, Balicer R, Nolte E, Suter E. Handbook Integrated Care. Cham: Springer International Publishing; 2017. [Google Scholar]
- 6. Busetto L, Luijkx K, Calciolari S, Ortiz LGG, Vrijhoef HJM. Barriers and facilitators to workforce changes in integrated care. Int J Integr Care. 2018;18(2):1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ling T, Brereton L, Conklin A, Newbould J, Roland M. Barriers and facilitators to integrating care: experiences from the English integrated care pilots. Int J Integr Care. 2012;12(5):1‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Auschra C. Barriers to the integration of care in inter‐organisational settings: a literature review. Int J Integr Care. 2018;18(1):1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. De Stampa M, Vedel I, Trouve H, Jean O, Ankri J, Somme D. Factors facilitating and impairing implementation of integrated care. Revue Epidemiol Sante Publ. 2013;61(2):145‐153. [DOI] [PubMed] [Google Scholar]
- 10. Peytremann‐Bridevaux I, Filliettaz SS, Berchtold P, Grossglauser M, Pavlickova A, Gilles I. Healthcare system maturity for integrated care: results of a Swiss nationwide survey using the SCIROCCO tool. BMJ Open. 2021;11(2):e041956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Grooten L, Borgermans L, Vrijhoef HJ. An instrument to measure maturity of integrated care: a first validation study. Int J Integr Care. 2018;18(1):1‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pavlickova A SCIROCCO tool to support delivery of integrated care in Europe. Int J Integr Care. 2017;17(5).
- 13. Grooten L, Vrijhoef HJM, Calciolari S, et al. Assessing the maturity of the healthcare system for integrated care: testing measurement properties of the SCIROCCO tool. BMC Med Res Methodol. 2019;19(1):63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Merçay C Expérience de la population âgée de 18 ans et plus avec le système de santé–Situation en Suisse et comparaison internationale. Analyse Int Health Policy Surv Sur Mand Office fédéral de la santé Publique (OFSP)(Obsan Dossier 56) Neuchâtel: Observat Suisse Santé. 2016.
- 15. Fielding N, Cisneros‐Puebla CA. CAQDAS‐GIS convergence: toward a new integrated mixed method research practice? J Mixed Methods Res. 2009;3(4):349‐370. [Google Scholar]
- 16. Stoneman P, Sturgis P, Allum N. Exploring public discourses about emerging technologies through statistical clustering of open‐ended survey questions. Public Underst Sci. 2013;22(7):850‐868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Reinert M. Alceste une méthodologie d'analyse des données textuelles et une application: Aurelia De Gerard De Nerval. Bull Sociol Methodol/Bull méthodol Sociol. 1990;26(1):24‐54. [Google Scholar]
- 18. Lauvergeon S, Burnand B, Peytremann‐Bridevaux I. Chronic disease management: a qualitative study investigating the barriers, facilitators and incentives perceived by Swiss healthcare stakeholders. BMC Health Serv Res. 2012;12(1):176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Maruthappu M, Hasan A, Zeltner T. Enablers and barriers in implementing integrated care. Health Syst Reform. 2015;1(4):250‐256. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request. The datasets used during the study are available from the corresponding author on reasonable request.


